Abstract
Aim
To describe the registry design of the Osaka Emergency Information Research Intelligent Operation Network system (ORION) and its profile of hospital information, patient and emergency medical service characteristics, and in‐hospital outcomes among all patients transported to critical care centers and emergency hospitals in Osaka Prefecture, Japan.
Methods
The Osaka Prefecture Government has developed and introduced an information system for emergency patients (the ORION system) that uses a smartphone application (app) for hospital selection by on‐scene emergency medical service personnel and has been accumulating all ambulance records. Since January 2015, medical institutions have obtained information on the diagnosis and outcome of patients transported to medical institutions, and the ORION system merged these data with ambulance records including smartphone app data.
Results
From January 2015 to December 2016, 753,301 eligible patients were registered. The mean age was 58.7 years, and 51.5% of patients were male. After hospital arrival, 39.7% were hospitalized, 58.2% were discharged from hospital, 1.1% changed hospital, and 1.0% died. The most common diagnoses were injury, poisoning, and certain other consequences of external causes. Among the hospitalized patients, 29.2% were continuously hospitalized, 59.0% discharged, 5.2% changed hospital, and 5.8% were dead at 21 days after hospitalization. The most common confirmed diagnosis was diseases of the circulatory system.
Conclusion
Using the ORION system developed and operated by Osaka Prefecture since January 2015, we described the epidemiological data of all emergency patients transported to emergency hospitals. Analysis using the ORION database in the future could lead to improvements in the emergency transport system and patient outcomes.
Keywords: Ambulance, diagnosis, emergency medical service, information technology, survival
Introduction
Recently, the number of emergency patients transported to hospitals by emergency medical service (EMS) personnel has been increasing and exceeding the hospital capacity in Japan. Therefore, it is very difficult for hospitals to accept emergency patients smoothly and appropriately, especially critically ill patients and pregnant women.1 However, digital information devices such as smartphones and tablet computers have also been dramatically advancing in recent years, and various medical information systems for EMS and/or medical institutions have also been introduced with the use of these devices. For example, we showed that sharing information between an ambulance and a hospital by using a smartphone application (app) at the scene was associated with decreased difficulty in obtaining hospital acceptance.2
In the Senshu medical control area in Osaka, Japan, Nakao and colleagues reported descriptive results of all emergency patients for whom fire departments had selected medical institutions, but they pointed out that there were excessive limitations to registering them when using a handwritten‐based registry.3 In contrast, multicenter registry research has been undertaken with the use of information technology,4, 5 and the establishment of databases that linked ambulance records with in‐hospital information has been also achieved in some areas.6, 7, 8, 9 Importantly, however, most of these databases were hospital‐based, and there were few population‐based registries at the regional or national level. Thus, to evaluate the effectiveness of the emergency medical system, records after hospital arrival of emergency patients, such as diagnosis and outcome, and information on ambulance records are essential at the population level. For this purpose, it is important to make effective use of smartphones and tablet computers.
Since January 2013, the Osaka Prefecture Government has developed and introduced an information system for emergency patients (the Osaka Emergency Information Research Intelligent Operation Network [ORION] system) using a smartphone app for hospital selection by on‐scene EMS personnel and has been accumulating all ambulance records. Furthermore, since January 2015, medical institutions obtained information on the diagnosis and outcome of emergency patients transported to medical institutions, and the ORION system merged these data with ambulance records and smartphone app data. This report describes the ORION system and its profile of hospital information, EMS characteristics, and in‐hospital diagnoses and outcomes between January 2015 and December 2016.
Methods
Study design, population, and setting
This is a descriptive epidemiological observation of data from the population‐based emergency patient database collected by the ORION system. The study period was the 2 years from January 2015 to December 2016. Osaka Prefecture is located in the central area of western Japan and covers an area of 1,905 km2.10 The proportion of male inhabitants was 48.1% and that of elderly people (aged ≥65 years) was 26.1% in 2015 (Table 1). There are 519 hospitals (106,273 beds) in Osaka Prefecture,11 of which 288 are emergency hospitals including 16 critical care centers that are designated to accept patients with life‐threatening emergency diseases such as severe trauma and sepsis.12 Among the secondary medical control areas (Table 2), Osaka City has the biggest area with 75 ambulances, and it accounts for 26.2% of the number of ambulances in Osaka prefecture.
Table 1.
Basic information about Osaka prefecture
| Osaka Prefecture | 2015 |
|---|---|
| Area, km2 | 1,905 |
| Population | 8,839,469 |
| Male | 42,56,049 (48.1) |
| Female | 45,83,420 (51.2) |
| Children aged 0–14 years | 10,93,111 (12.5) |
| Adults aged 15–64 years | 53,41,654 (61.3) |
| Elderly aged ≥65 years | 22,78,324 (26.1) |
| Secondary medical control area | |
| Toyono | 10,09,956 (11.4) |
| Mishima | 7,42,670 (8.4) |
| Kita‐Kawachi | 11,82,487 (13.4) |
| Naka‐Kawachi | 8,53,278 (9.7) |
| Minami‐Kawachi | 6,34,159 (7.2) |
| Sakai City | 8,39,518 (9.5) |
| Senshu | 9,19,836 (10.4) |
| Osaka City | 26,57,565 (30.0) |
| Population density, population/km2 | 4640.1 |
| Critical emergency medical centers | 16 |
Data are expressed as n or n (%).
Table 2.
Basic information about fire departments and medical control in Osaka prefecture
| Osaka Prefecture | 2015 |
|---|---|
| Number of participating fire departments | 27 |
| Toyono area | 4 (14.8) |
| Mishima area | 4 (14.8) |
| Kita‐Kawachi area | 4 (14.8) |
| Naka‐Kawachi area | 3 (11.1) |
| Minami‐Kawachi area | 4 (14.8) |
| Sakai City area | 1 (3.7) |
| Senshu area | 6 (22.2) |
| Osaka City area | 1 (3.7) |
| Number of ambulances | 286 |
| Toyono area | 35 (12.2) |
| Mishima area | 28 (9.8) |
| Kita‐Kawachi area | 42 (14.7) |
| Naka‐Kawachi area | 31 (10.8) |
| Minami‐Kawachi area | 19 (6.6) |
| Sakai City area | 33 (11.5) |
| Senshu area | 23 (8.0) |
| Osaka City area | 75 (26.2) |
Data are expressed as n or n (%).
This study included emergency patients with data that linked ambulance records with in‐hospital information in these hospitals and excluded those patients without data in emergency hospitals, those not transported to hospitals, those with only smartphone app data, those transported to hospitals other than emergency hospitals in Osaka Prefecture, those with inconsistent information regarding gender between the ambulance and emergency hospital, those whose age differed by ≥3 years between the ambulance and the emergency hospital, and those with inappropriate data as judged by Osaka Prefecture.
Emergency medical service systems and hospitals in Osaka Prefecture
The EMS system is basically the same as that used in other areas of Japan, as previously described.13 After the introduction of the ORION system, emergency dispatchers in Osaka Prefecture did not make telephone calls to hospitals for patient acceptance; rather, EMS personnel at the scene selected appropriate hospitals and transported patients to the hospitals including critical care centers during the study period.
The ORION system
Information on the system configuration of ORION was previously described in detail.2 Emergency medical service personnel at the scene operate the ORION smartphone app for each emergency patient. All of the data input into the smartphone app, such as vital signs and the time of the call to the hospital for acceptance, are also recorded (Fig. 1). The smartphone app data are accumulated in the ORION cloud server, and in cooperation with the dispatched EMS personnel, data managers at each fire department directly input or upload the ambulance record of each emergency patient so that it can be connected with the app data. Furthermore, the operators of each hospital also directly input or upload the patient's data, such as diagnoses and outcomes, after hospital acceptance (Fig. 2). The results of aggregated data in the ORION system are fed back to every fire department and emergency hospital. The department of public health of Osaka Prefecture can also analyze the effects of health policy on the emergency medical system using these collected data. The ORION system has been in place in all fire departments and emergency hospitals in Osaka Prefecture since January 2015.
Figure 1.
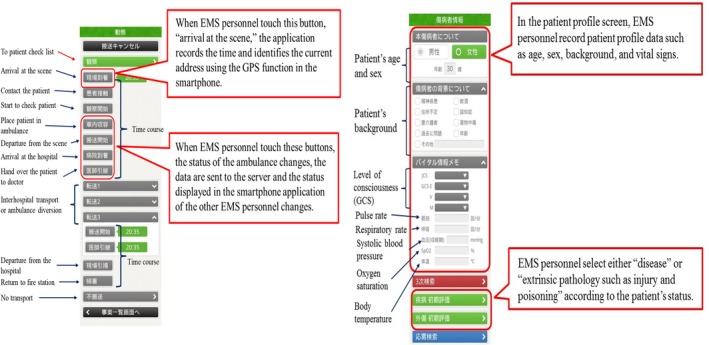
Configuration of the Osaka Emergency Information Research Intelligent Operation Network system (ORION) smartphone application.2
Figure 2.
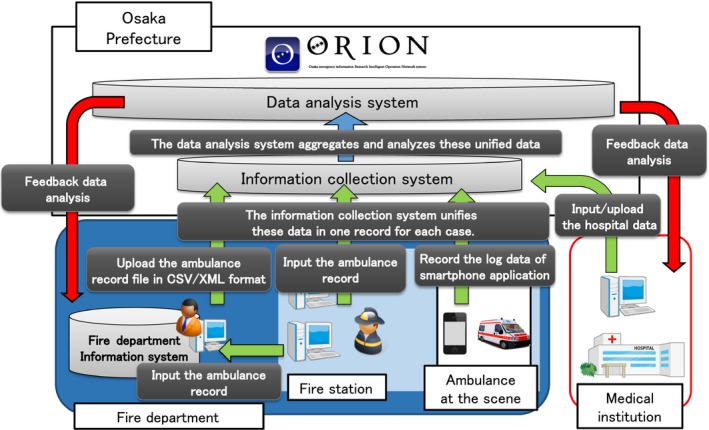
System configuration of the Osaka Emergency Information Research Intelligent Operation Network (ORION). All data consisting of the smartphone application data, ambulance records, and hospital data are merged in the ORION server and managed as one large database in Osaka Prefecture, Japan.2
Data collection and quality control
The ORION system collects data about all ambulance dispatches in Osaka Prefecture. Emergency medical service personnel operate the smartphone app during the emergency activities and input the smartphone app data before they return to each fire station. After returning, they input the ambulance record into the information system of each fire department or the ORION system. At this time, the information system of each fire department or the ORION system logically checks for errors in the inputted data, and EMS personnel correct them, if necessary. The data managers of each fire department output comma separated value (CSV) files or extended markup language (XML) files converted in the format specified by the Fire and Disaster Management Agency of Japan from the data input into the information system of each fire department. They can also upload the output file to the ORION system, and these data are connected to smartphone app data with a specific anonymized number in the ORION system.
The patient data registered by the smartphone app is displayed on the website of the ORION system, and the staff of each emergency hospital can select the displayed patient data and input the in‐hospital data from the Web form. In the ORION system, Osaka Prefecture Government decided to use 21‐day survival as the follow‐up period so that emergency hospitals including critical care centers could input the patient's information by the end of next month after hospital arrival. The ORION system checks for errors in the inputted in‐hospital data, and the staff of each emergency hospital can correct them, if necessary. Through these tasks, smartphone app data, ambulance records, and the in‐hospital data such as diagnosis and prognosis can be comprehensively registered for each patient transported by an ambulance. The registered data is cleaned and analyzed by the Working Group to analyze the emergency medical care system in Osaka Prefecture.
The ORION data are composed of the following:
Smartphone app information
The items concerning each emergency patient at the scene are registered by the EMS personnel operating the smartphone app as follows: age, gender, time course before hospital arrival (arrival at the scene, patient contact, departure from the scene, and hospital arrival), Glasgow Coma Scale, pulse rate (b.p.m.), frequency of respiration (breaths/min), systolic and diastolic blood pressure at the scene (mmHg), oxygen saturation (%), body temperature (°C), and other information.
Ambulance record
The records for ambulance dispatches are primarily composed of information regulated by the Fire and Disaster Management Agency of Japan as follows:14 name of fire department, accident type, date of ambulance dispatch, detailed time course before hospital arrival (119 call, ambulance dispatch, arrival at the scene, patient contact, patient accommodation in the ambulance, departure from the scene, and hospital arrival), age, age group classified by EMS, gender, accident location, total number of phone calls by EMS personnel at the scene to hospitals, evaluation of the urgency by the on‐scene EMS personnel, severity judged by the doctor, Utstein information (only for patients with out‐of‐hospital cardiac arrest),15 and other information.
Hospital information
The staff of each emergency hospital input the following items: age, gender, date and time of transport, treating department at hospital admission, treating department after hospitalization, patient's background such as drug abuse and elderly who need care, International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD‐10) diagnosis at hospital admission, ICD‐10 diagnosis at 21 days after hospitalization, urgency of the patient as judged by doctors at hospital admission, patient outcome at hospital admission, outcome at 21 days after hospitalization, and other information.
Statistical analysis
Continuous variables are indicated by mean (standard deviation) and median (interquartile range), and categorical variables are indicated by percentage. Statistical analyses were carried out using spss version 23.0J (IBM, Armonk, NY, USA). This study was approved by the ethics committees of Osaka University Graduate School of Medicine (approval no. 15003; Osaka, Japan). Because the ORION data is anonymized without specific personal data, such as the patient's name, date of birth, and address, the requirement of obtaining patients’ informed consent was waived.
Results
In 2015 (Fig. 3A), a total of 578,402 emergency patients were registered with the ORION system, and 325,769 emergency patients were confirmed after excluding 76,559 without transport to a hospital, 91,842 transported to other than emergency hospitals, 65,294 without linked data between the ambulance and a hospital, and 18,938 with only smartphone app data. Of them, 315,327 were eligible for our analysis after excluding patients with inconsistent data such as that for sex and age and those with unknown key factors such as outcomes. Although the number of emergency patients with only smartphone app data in Kita‐Kawachi and Naka‐Kawachi areas was great, there were no basic differences in patient characteristics between analytic and non‐analytic cohorts in 2015 (Table S1). In 2016 (Fig. 3B), a total of 573,384 emergency patients were registered, and 437,974 emergency patients were eligible for our analysis, and the number of patients without linked data between the ambulance and a hospital was 20,008.
Figure 3.
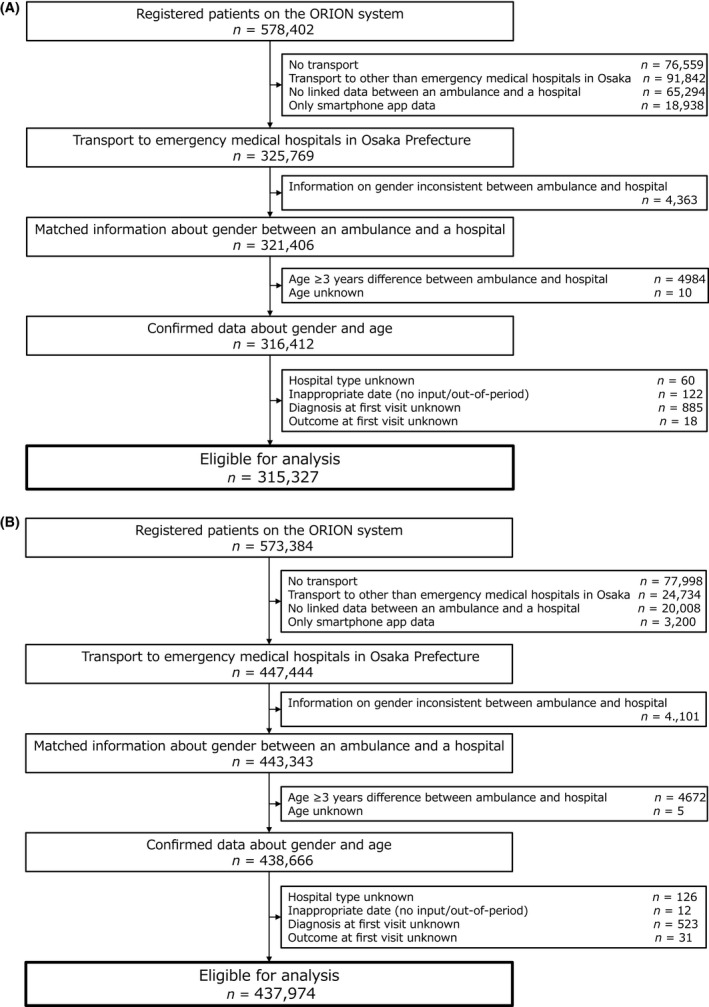
Patient flow of the Osaka Emergency Information Research Intelligent Operation Network (ORION) registry between 2015 (A) and 2016 (B), including all patients transported to critical care centers and emergency hospitals in Osaka Prefecture, Japan.
Table 3 shows the prehospital baseline characteristics of the patients. The mean patient age was 58.7 years, and the proportion of male patients was 51.5%. The most frequent reason for the ambulance call was acute diseases (66.4%), followed by other injury (15.3%) and traffic accidents involving car, ship, or aircraft (9.0%). The most frequent location of occurrence was the home (58.4%), followed by a public space (22.7%), and a road (15.4%). The mean time intervals from ambulance call to arrival at the scene and to arrival at the hospital were 7 and 31 min, respectively.
Table 3.
Prehospital baseline characteristics of emergency patients registered with the Osaka Emergency Information Research Intelligent Operation Network system, 2015–2016
| Total (n = 753,301) | 2015 (n = 315,327) | 2016 (n = 437,974) | |
|---|---|---|---|
| Number of patients by area, n (%) | |||
| Toyono | 50,413 (6.7) | 9,812 (3.1) | 40,601 (9.3) |
| Mishima | 59,684 (7.9) | 25,828 (8.2) | 33,856 (7.7) |
| Kita‐Kawachi | 80,995 (10.8) | 31,523 (10.0) | 49,472 (11.3) |
| Naka‐Kawachi | 76,932 (10.2) | 28,512 (9.0) | 48,420 (11.1) |
| Minami‐Kawachi | 30,258 (4.0) | 13,744 (4.4) | 16,514 (3.8) |
| Sakai City | 84,695 (11.2) | 39,632 (12.5) | 45,063 (10.3) |
| Senshu | 75,387 (10.0) | 35,933 (11.4) | 39,454 (9.0) |
| Osaka City | 2,94,937 (39.2) | 1,30,343 (41.3) | 1,64,594 (37.6) |
| Age, years; mean (SD) | 58.7 (26.2) | 58.3 (26.2) | 59.0 (26.3) |
| Age, years; median (IQR) | 67 (40–80) | 66 (40–79) | 67 (41–80) |
| Age groups, n (%) | |||
| Newborn infant, <28 days | 1,502 (0.2) | 107 (0.0) | 1,395 (0.3) |
| Young child, ≥28 days and <7 years | 41,551 (5.5) | 17,976 (5.7) | 23,575 (5.4) |
| Older child, ≥7 years and <18 years | 29,917 (4.0) | 12,683 (4.0) | 17,234 (3.9) |
| Adult, ≥18 years and <65 years | 2,74,711 (36.5) | 1,17,343 (37.2) | 1,57,368 (35.9) |
| Elderly, ≥65 years | 4,05,620 (53.8) | 1,67,218 (53.0) | 2,38,402 (54.4) |
| Male gender, n (%) | 3,87,716 (51.5) | 1,62,510 (51.5) | 2,25,206 (51.4) |
| Reason for ambulance call, n (%) | |||
| Fire accident | 614 (0.1) | 250 (0.1) | 364 (0.1) |
| Natural disaster | 23 (0.0) | 11 (0.0) | 12 (0.0) |
| Water accident | 85 (0.0) | 42 (0.0) | 43 (0.0) |
| Traffic accident involving car, ship, or aircraft | 67,891 (9.0) | 29,122 (9.2) | 38,769 (8.9) |
| Injury, poisoning, and disease due to industrial accident | 6,871 (0.9) | 2,904 (0.9) | 3,967 (0.9) |
| Disease and injury due to sports | 4,782 (0.6) | 2,092 (0.7) | 2,690 (0.6) |
| Other injury | 1,15,460 (15.3) | 47,872 (15.2) | 67,588 (15.4) |
| Trauma due to assault | 5,879 (0.8) | 2,691 (0.9) | 3,188 (0.7) |
| Self‐induced injury | 5,280 (0.7) | 2,320 (0.7) | 2,960 (0.7) |
| Acute disease | 4,99,875 (66.4) | 2,08,837 (66.2) | 2,91,038 (66.5) |
| Interhospital transport | 46,363 (6.2) | 19,119 (6.1) | 27,244 (6.2) |
| Other | 178 (0.0) | 67 (0.0) | 111 (0.0) |
| Location, n (%) | |||
| Home | 4,40,040 (58.4) | 1,83,914 (58.3) | 2,56,126 (58.5) |
| Public space | 1,70,861 (22.7) | 70,720 (22.4) | 1,00,141 (22.9) |
| Workspace | 17,906 (2.4) | 7,691 (2.4) | 10,215 (2.3) |
| Road | 1,15,656 (15.4) | 49,156 (15.6) | 66,500 (15.2) |
| Other | 8,727 (1.2) | 3,737 (1.2) | 4,990 (1.1) |
| Unknown | 111 (0.0) | 109 (0.0) | 2 (0.0) |
| Urgency as judged by EMS personnel, n (%) | |||
| High | 51,934 (6.9) | 20,430 (6.5) | 31,504 (7.2) |
| Middle | 4,06,107 (53.9) | 1,62,931 (51.7) | 2,43,176 (55.5) |
| Low | 8,637 (1.1) | 3,993 (1.3) | 4,644 (1.1) |
| Not urgent | 2,86,623 (38.0) | 1,27,973 (40.5) | 1,58,650 (36.2) |
| Time interval from ambulance call to arrival at the scene, min; mean (SD) | 7 (6–9) | 7 (6–9) | 7 (6–9) |
| Time interval from ambulance call to arrival at the hospital, min; mean (SD) | 31 (26–39) | 31 (26–39) | 31 (26–39) |
EMS, emergency medical service; IQR, interquartile range; SD, standard deviation.
Table 4 shows the diagnostic classifications and the clinical outcome at hospital arrival for the 753,301 transported patients. The most frequent diagnostic classification listed was “injury, poisoning and certain other consequences of external causes (S + T)” (26.2%), followed by “symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified (R)” (14.6%) and “diseases of the circulatory system (I)” (12.3%). Patient outcomes were “hospitalized” in 39.7% and “discharged” in 58.2% of the patients.
Table 4.
Diagnoses and outcomes at hospital arrival of emergency patients registered with the Osaka Emergency Information Research Intelligent Operation Network, 2015–2016
| Total (n = 753,301) | 2015 (n = 315,327) | 2016 (n = 437,974) | |
|---|---|---|---|
| Diagnoses (ICD‐10), n (%) | |||
| Certain infectious and parasitic diseases (A + B) | 32,714 (4.3) | 13,495 (4.3) | 19,219 (4.4) |
| Neoplasms (C) | 10,831 (1.4) | 4,699 (1.5) | 6,132 (1.4) |
| Diseases of the blood and blood‐forming organs and certain disorders involving the immune mechanism (D) | 5,398 (0.7) | 2,457 (0.8) | 2,941 (0.7) |
| Endocrine, nutritional, and metabolic diseases (E) | 27,704 (3.7) | 11,697 (3.7) | 16,007 (3.7) |
| Mental and behavioral disorders (F) | 26,656 (3.5) | 11,670 (3.7) | 14,986 (3.4) |
| Diseases of the nervous system (G) | 24,670 (3.3) | 10,761 (3.4) | 13,909 (3.2) |
| Diseases of the eye and adnexa (H00‐59) | 829 (0.1) | 346 (0.1) | 483 (0.1) |
| Diseases of the ear and mastoid process (H60‐96) | 13,907 (1.8) | 5,945 (1.9) | 7,962 (1.8) |
| Diseases of the circulatory system (I) | 92,486 (12.3) | 38,726 (12.3) | 53,760 (12.3) |
| Diseases of the respiratory system (J) | 63,412 (8.4) | 26,384 (8.4) | 37,028 (8.5) |
| Diseases of the digestive system (K) | 54,799 (7.3) | 23,651 (7.5) | 31,148 (7.1) |
| Diseases of the skin and subcutaneous tissue (L) | 4,171 (0.6) | 1,751 (0.6) | 2,420 (0.6) |
| Diseases of the musculoskeletal system and connective tissue (M) | 23,529 (3.1) | 9,486 (3.0) | 14,043 (3.2) |
| Diseases of the genitourinary system (N) | 26,961 (3.6) | 11,385 (3.6) | 15,576 (3.6) |
| Pregnancy, childbirth, and the puerperium (O) | 3,384 (0.4) | 1,376 (0.4) | 2,008 (0.5) |
| Certain conditions originating in the perinatal period (P) | 380 (0.1) | 193 (0.1) | 187 (0.0) |
| Congenital malformations, deformations, and chromosomal abnormalities (Q) | 388 (0.1) | 164 (0.1) | 224 (0.1) |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R) | 1,10,105 (14.6) | 45,321 (14.4) | 64,784 (14.8) |
| Injury, poisoning and certain other consequences of external causes (S + T) | 1,97,161 (26.2) | 83,670 (26.5) | 1,13,491 (25.9) |
| External causes of morbidity and mortality (V + W + X + Y) | 15,252 (2.0) | 7,178 (2.3) | 8,074 (1.8) |
| Factors influencing health status and contact with health services (Z) | 920 (0.1) | 502 (0.2) | 418 (0.1) |
| Others (U) | 1 (0.0) | 0 (0) | 1 (0.0) |
| Unknown | 18,145 (2.4) | 4,972 (1.6) | 13,173 (3.0) |
| Outcomes, n (%) | |||
| Hospitalized | 2,99,004 (39.7) | 1,24,014 (39.3) | 1,74,990 (40.0) |
| Discharged | 4,38,333 (58.2) | 1,84,690 (58.6) | 2,53,643 (57.9) |
| Changed hospital | 8,239 (1.1) | 3,302 (1.0) | 4,937 (1.1) |
| Death | 7,707 (1.0) | 3,321 (1.1) | 4,386 (1.0) |
| Unknown | 18 (0.0) | 0 (0) | 18 (0.0) |
| Clinical department, n (%) | |||
| Internal medicine | 2,06,031 (27.4) | 84,254 (26.7) | 1,21,777 (27.8) |
| Respiratory medicine | 10,052 (1.3) | 4,459 (1.4) | 5,593 (1.3) |
| Cardiology | 33,949 (4.5) | 14,498 (4.6) | 19,451 (4.4) |
| Gastroenterology | 21,378 (2.8) | 9,226 (2.9) | 12,152 (2.8) |
| Nephrology | 1,099 (0.1) | 491 (0.2) | 608 (0.1) |
| Neurology | 8,601 (1.1) | 3,650 (1.2) | 4,951 (1.1) |
| Endocrinology and metabolism | 1,570 (0.2) | 704 (0.2) | 866 (0.2) |
| Hematology | 1,062 (0.1) | 480 (0.2) | 582 (0.1) |
| Dermatology | 820 (0.1) | 340 (0.1) | 480 (0.1) |
| Allergy and rheumatology | 420 (0.1) | 205 (0.1) | 215 (0.0) |
| Pediatrics | 39,210 (5.2) | 16,835 (5.3) | 22,375 (5.1) |
| Psychiatry | 706 (0.1) | 336 (0.1) | 370 (0.1) |
| Surgery | 57,276 (7.6) | 22,472 (7.1) | 34,804 (7.9) |
| Thoracic surgery | 499 (0.1) | 220 (0.1) | 279 (0.1) |
| Cardiovascular surgery | 1,223 (0.2) | 496 (0.2) | 727 (0.2) |
| Gastrointestinal surgery | 2,738 (0.4) | 1,214 (0.4) | 1,524 (0.3) |
| Urology | 6,030 (0.8) | 2,620 (0.8) | 3,410 (0.8) |
| Neurosurgery | 71,460 (9.5) | 30,920 (9.8) | 40,540 (9.3) |
| Orthopedic surgery | 79,381 (10.5) | 33,251 (10.5) | 46,130 (10.5) |
| Plastic and reconstructive surgery | 3,318 (0.4) | 1,610 (0.5) | 1,708 (0.4) |
| Ophthalmology | 643 (0.1) | 266 (0.1) | 377 (0.1) |
| Otorhinolaryngology – head and neck surgery | 4,782 (0.6) | 2,083 (0.7) | 2,699 (0.6) |
| Pediatric surgery | 878 (0.1) | 417 (0.1) | 461 (0.1) |
| Obstetrics and gynecology | 7,166 (1.0) | 3,071 (1.0) | 4,095 (0.9) |
| Emergency department | 1,55,457 (20.6) | 65,401 (20.7) | 90,056 (20.6) |
| Oral and maxillofacial surgery | 268 (0.0) | 108 (0.0) | 160 (0.0) |
| Emergency and critical care center | 33,387 (4.4) | 14,128 (4.5) | 19,259 (4.4) |
| Unknown | 50 (0.0) | 21 (0.0) | 29 (0.0) |
| Others | 3,847 (0.5) | 1,551 (0.5) | 2,296 (0.5) |
ICD‐10, International Statistical Classification of Diseases and Related Health Problems, 10th Revision.
The diagnostic classification, clinical department, and outcome at 21 days after hospitalization of the 299,004 hospitalized patients are shown in Table 5. The diagnostic classification of “diseases of the circulatory system (I)” was highest at 20.3%, followed by “injury, poisoning and certain other consequences of external causes (S + T)” at 19.2% and “diseases of the respiratory system (J)” at 13.8%. Patient outcomes at 21 days after hospitalization were “discharged” in 59.0% and “hospitalized” in 29.2% of the patients.
Table 5.
Confirmed diagnoses and outcomes after hospitalization of emergency patients registered with the Osaka Emergency Information Research Intelligent Operation Network, 2015–2016
| Total (n = 299,004) | 2015 (n = 124,014) | 2016 (n = 174,990) | |
|---|---|---|---|
| Diagnoses (ICD‐10), n (%) | |||
| Certain infectious and parasitic diseases (A + B) | 10,531 (3.5) | 4,276 (3.4) | 6,255 (3.6) |
| Neoplasms (C) | 11,930 (4.0) | 5,153 (4.2) | 6,777 (3.9) |
| Diseases of the blood and blood‐forming organs and certain disorders involving the immune mechanism (D) | 3,480 (1.2) | 1,579 (1.3) | 1,901 (1.1) |
| Endocrine, nutritional, and metabolic diseases (E) | 11,106 (3.7) | 4,600 (3.7) | 6,506 (3.7) |
| Mental and behavioral disorders (F) | 4,952 (1.7) | 2,047 (1.7) | 2,905 (1.7) |
| Diseases of the nervous system (G) | 11,515 (3.9) | 4,901 (4.0) | 6,614 (3.8) |
| Diseases of the eye and adnexa (H00‐59) | 152 (0.1) | 68 (0.1) | 84 (0.0) |
| Diseases of the ear and mastoid process (H60‐96) | 4,817 (1.6) | 1,993 (1.6) | 2,824 (1.6) |
| Diseases of the circulatory system (I) | 60,565 (20.3) | 25,124 (20.3) | 35,441 (20.3) |
| Diseases of the respiratory system (J) | 41,259 (13.8) | 17,180 (13.9) | 24,079 (13.8) |
| Diseases of the digestive system (K) | 33,765 (11.3) | 14,503 (11.7) | 19,262 (11.0) |
| Diseases of the skin and subcutaneous tissue (L) | 1,888 (0.6) | 786 (0.6) | 1,102 (0.6) |
| Diseases of the musculoskeletal system and connective tissue (M) | 7,922 (2.6) | 3,138 (2.5) | 4,784 (2.7) |
| Diseases of the genitourinary system (N) | 12,253 (4.1) | 4,987 (4.0) | 7,266 (4.2) |
| Pregnancy, childbirth, and the puerperium (O) | 2,775 (0.9) | 1,115 (0.9) | 1,660 (0.9) |
| Certain conditions originating in the perinatal period (P) | 235 (0.1) | 112 (0.1) | 123 (0.1) |
| Congenital malformations, deformations, and chromosomal abnormalities (Q) | 281 (0.1) | 110 (0.1) | 171 (0.1) |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R) | 12,735 (4.3) | 5,320 (4.3) | 7,415 (4.2) |
| Injury, poisoning, and certain other consequences of external causes (S + T) | 57,308 (19.2) | 23,964 (19.3) | 33,344 (19.0) |
| External causes of morbidity and mortality (V + W + X + Y) | 735 (0.2) | 352 (0.3) | 383 (0.2) |
| Factors influencing health status and contact with health services (Z) | 178 (0.1) | 93 (0.1) | 85 (0.0) |
| Others (U) | 1 (0.0) | 0 (0.0) | 1 (0.0) |
| Unknown | 8,621 (2.9) | 2,613 (2.1) | 6,008 (3.4) |
| Outcomes, n (%) | |||
| Hospitalized | 87,417 (29.2) | 36,392 (29.3) | 51,025 (29.2) |
| Discharged | 1,76,274 (59.0) | 72,829 (58.7) | 103,445 (59.1) |
| Changed hospital | 15,560 (5.2) | 6,209 (5.0) | 9,351 (5.3) |
| Death | 17,226 (5.8) | 7,217 (5.8) | 10,009 (5.7) |
| Unknown | 2,527 (0.8) | 1,367 (1.1) | 1,160 (0.7) |
| Clinical departments, n (%) | |||
| Internal medicine | 73,377 (24.5) | 29,700 (23.9) | 43,677 (25.0) |
| Respiratory medicine | 12,595 (4.2) | 5,294 (4.3) | 7,301 (4.2) |
| Cardiology | 27,460 (9.2) | 11,420 (9.2) | 16,040 (9.2) |
| Gastroenterology | 23,357 (7.8) | 9,756 (7.9) | 13,601 (7.8) |
| Nephrology | 2,408 (0.8) | 1,009 (0.8) | 1,399 (0.8) |
| Neurology | 8,700 (2.9) | 3,521 (2.8) | 5,179 (3.0) |
| Endocrinology and metabolism | 1,979 (0.7) | 813 (0.7) | 1,166 (0.7) |
| Hematology | 1,388 (0.5) | 586 (0.5) | 802 (0.5) |
| Dermatology | 538 (0.2) | 224 (0.2) | 314 (0.2) |
| Allergy and rheumatology | 607 (0.2) | 253 (0.2) | 354 (0.2) |
| Pediatrics | 10,120 (3.4) | 4,556 (3.7) | 5,564 (3.2) |
| Psychiatry | 546 (0.2) | 254 (0.2) | 292 (0.2) |
| Surgery | 15,073 (5.0) | 6,239 (5.0) | 8,834 (5.0) |
| Thoracic surgery | 799 (0.3) | 336 (0.3) | 463 (0.3) |
| Cardiovascular surgery | 1,808 (0.6) | 706 (0.6) | 1,102 (0.6) |
| Gastrointestinal surgery | 3,612 (1.2) | 1,543 (1.2) | 2,069 (1.2) |
| Urology | 4,290 (1.4) | 1,802 (1.5) | 2,488 (1.4) |
| Neurosurgery | 35,866 (12.0) | 15,174 (12.2) | 20,692 (11.8) |
| Orthopedic surgery | 37,744 (12.6) | 15,459 (12.5) | 22,285 (12.7) |
| Plastic and reconstructive surgery | 1,174 (0.4) | 505 (0.4) | 669 (0.4) |
| Ophthalmology | 162 (0.1) | 64 (0.1) | 98 (0.1) |
| Otorhinolaryngology – head and neck surgery | 2,202 (0.7) | 953 (0.8) | 1,249 (0.7) |
| Pediatric surgery | 224 (0.1) | 99 (0.1) | 125 (0.1) |
| Obstetrics and gynecology | 4,670 (1.6) | 1,915 (1.5) | 2,755 (1.6) |
| Emergency department | 11,970 (4.0) | 5,458 (4.4) | 6,512 (3.7) |
| Oral and maxillofacial surgery | 139 (0.0) | 61 (0.0) | 78 (0.0) |
| Emergency and critical care center | 10,710 (3.6) | 4,306 (3.5) | 6,404 (3.7) |
| Others | 2,145 (0.7) | 729 (0.6) | 1,416 (0.8) |
| Unknown | 3,341 (1.1) | 1,279 (1.0) | 2,062 (1.2) |
ICD, International Statistical Classification of Diseases and Related Health Problems, 10th Revision.
Discussion
The ORION system was launched in January 2015, and since then it has been prospectively collecting data on all emergency patients transported to critical care centers or emergency hospitals in Osaka Prefecture, including diagnoses and outcomes after hospital arrival along with ambulance records and on‐scene smartphone app data. This report described the ORION profile and briefly presented the characteristics of 753,301 emergency patients registered during the first 2 years of the system's operation between January 2015 and December 2016.
To improve the survival of emergency patients by improving the emergency medical care system, it is necessary to evaluate the actual situation of the medical system at the population level. In accordance with the recent increase in the number of emergency transports, the time interval from EMS call to hospital arrival has lengthened since 2000,1 but the only number included in the public data was for all patients. Importantly, ambulances were dispatched not only for highly urgent diseases such as acute myocardial infarction, stroke, out‐of‐hospital cardiac arrest, and severe trauma, whose prehospital time courses would affect outcome, but also for diseases of low urgency such as slight fever and minor injuries. To evaluate whether the entire emergency medical care system from ambulance call to patient admission in medical institutions works effectively, it is also important to evaluate whether the time interval from ambulance call to hospital arrival affects the outcome of emergency patients, especially those with highly urgent conditions. The ORION system enabled us to comprehensively and individually collect data at the population level.
Research using the ORION system has several strengths. First, in the registry preceding ORION, most researchers could only evaluate emergency patients who visited participating medical institutions, and thus not all targeted subjects in the target region were assessed. Because the ORION system has been collecting data on all emergency patients transported to emergency medical institutions and critical care centers by ambulance in Osaka Prefecture, patient selection bias is small. In addition, with a total population of approximately 8.8 million people in our target area of Osaka Prefecture, the target population for all emergency dispatches is, to our knowledge, the largest in the world. Second, most of the preceding multicenter registries of emergency and intensive treatments collected and analyzed patients through hospital‐based collaboration, and data on emergency activities before hospital arrival were not based on ambulance records. The ORION system collects much information during the period from ambulance call to hospital discharge, and there are no similar registries in other areas. Finally, data collection has been carried out in cooperation with fire departments and medical institutions, but administrative agencies organized uniform explanations about data input for their staff during the study period. Indeed, although there were some deficiencies in the collected data in 2015 (e.g., the amount of linked data between an ambulance and a hospital), the quality improved exceedingly in 2016, the second year of data collection. Thus, one of the strengths of the present study is that the quality of data collection was guaranteed by administrative organizations, fire departments, and medical institutions.
This study showed that approximately 40% of emergency patients who were transported to emergency institutions by ambulance in Osaka Prefecture were hospitalized, and the remaining 60% were discharged to home. The use of ambulances is a public service in Japan and is basically free of charge. Therefore, the general public can easily call an ambulance even in cases of low urgency, which is one of the reasons for the increased use of ambulances in recent years. Furthermore, “injury, poisoning and certain other consequences of external causes” were the most frequent diagnoses at hospital admission, which suggests that most patients and bystanders do not have enough knowledge to take measures against injury or poisoning. Therefore, regular first aid education at the school or community level would lead to the better practice of first aid and to a decrease in ambulance calls for such cases.
In contrast, among the emergency patients who were transported, “diseases of the circulatory system” such as heart failure, myocardial infarction, and hypertension were the most frequent admitting diagnoses at hospitalization. Although the reason for this is unclear in the present study, it might be partially explained by the recent super‐aging society in Japan because these diseases increase with increasing age.16 The detailed diagnostic classification in the ORION system is recorded according to ICD‐10 coding, and carrying out a detailed analysis based on these codes is the next issue to be addressed. The real‐world evidence from Osaka, Japan indicates that the ORION system is suitable for improving emergency transport systems and patient outcomes.
Limitations
This study has some limitations. First, the ORION system obtains data on emergency medical institutions and critical care centers in Osaka Prefecture but cannot obtain data on clinics or non‐emergency institutions or on patients transported outside Osaka Prefecture because the ORION system is operated only within Osaka Prefecture. In the future, similar interoperable information systems will be needed across many areas. Second, we could not obtain data on emergency patients not transported by EMS personnel or on those with interhospital transport. Finally, we did not have detailed patient history such as medications, pregnancy, and development before the ambulance call. Because it is difficult for fire departments and medical institutions to collect baseline individual data, linkage of the ORION database with personal health records will also be required in the future.
Conclusion
Using the ORION system developed and operated by Osaka Prefecture since January 2015, we described the epidemiological data of all emergency patients transported to emergency hospitals in the first 2 years of ORION's operation. In the near future, further analysis of the ORION database is expected to lead to improvements in the emergency transport system and patient outcomes.
Disclosure
Approval of the research protocol: The protocol was approved by the Ethics Committee of Osaka University as the corresponding institution.
Informed consent: The requirement for informed consent of patients was waived.
Registry and the registration no. of the study/trial: This study was not registered.
Animal studies: N/A.
Conflict of interest: None.
Supporting information
Table S1. Characteristics of patients transported to critical care centers and emergency hospitals in Osaka Prefecture, Japan, by data availability of the Osaka Emergency Information Research Intelligent Operation Network in 2015
Acknowledgments
The Osaka Prefecture Government is deeply indebted to all of the Emergency Medical System personnel and concerned physicians in Osaka Prefecture and to the Osaka Medical Association for their indispensable cooperation and support. This study was supported by the Japan Society for the Promotion of Science KAKENHI (grant no. JP18H02902). This article was supported by the Clinical Investigator's Research Project of the Osaka University Graduate School of Medicine.
Funding Information
No funding information provided.
References
- 1. Ambulance Service Planning Office of Fire and Disaster Management Agency of Japan: effect of first aid for emergency patients in 2017. [cited 30 May 2018]. Available from: http://www.fdma.go.jp/neuter/topics/kyukyukyujo_genkyo/h29/01_kyukyu.pdf.
- 2. Katayama Y, Kitamura T, Kiyohara K et al Improvements in patient acceptance by hospitals following the introduction of a smartphone app for the emergency medical service system: a population‐based before‐and‐after observational study in Osaka City, Japan. JMIR Mhealth Uhealth 2017; 5(9): e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nakao S, Kawaguchi R, Mizushima Y et al Availabilities and problems of a revised regional emergency medical system. J. Jpn. Soc. Emerg Med. 2013; 16: 817–25. (in Japanese). [Google Scholar]
- 4. Japan Trauma Care and Research. Japan Trauma Data Bank annual report 2016 (2011‐2015). [cited 21 Aug 2017]. Available from: https://www.jtcr-jatec.org/traumabank/dataroom/data/JTDB2016.pdf.
- 5. Yamada T, Kitamura T, Hayakawa K et al Rationale, design, and profile of Comprehensive Registry of In‐Hospital Intensive Care for OHCA Survival (CRITICAL) study in Osaka, Japan. J. Intensive Care 2016; 4: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nakao S, Matsuoka T, Nakata T et al Availabilities of emergency patient registration system using information and communication technology. J. Jpn. Assoc. Acute Med. 2014; 25: 693–702. (in Japanese). [Google Scholar]
- 7. Katayama Y, Kitamura T, Kiyohara K et al Factors associated with the difficulty in hospital acceptance at the scene by emergency medical service personnel: a population‐based study in Osaka City, Japan. BMJ Open 2016; 6(10): e013849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Katayama Y, Kitamura T, Kiyohara K et al Evaluation of factors associated with the difficulty in finding receiving hospitals for traffic accident patients at the scene treated by emergency medical services: a population‐based study in Osaka City, Japan. Acute Med. Surg. 2017; 4(4): 401–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Matsuyama T, Kitamura T, Kiyohara K et al Characteristics and outcomes of emergency patients with self‐inflicted injuries: a report from ambulance records in Osaka City, Japan. Scand. J. Trauma Resusc. Emerg. Med. 2016; 24: 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Statistics Bureau, Ministry of Internal Affairs and Communications of Japan . National census in 2015. [cited 30 May 2018]. Available from: http://www.stat.go.jp/data/kokusei/2015/kekka/kihon1/pdf/gaiyou2.pdf.
- 11. Ministry of Health, Labour and Welfare of Japan . Medical facility survey in 2013. [cited 30 May 2018]. Available from: http://www.e-stat.go.jp/SG1/estat/List.do?lid=000001126755.
- 12. Emergency Medical Council in Osaka Prefecture . Certification of emergency medical institutions in 2017. [cited 30 May 2018]. Available from: http://www.pref.osaka.lg.jp/iryo/qq/kyuutaishin_kaisai.html; http://www.pref.osaka.lg.jp/iryo/qq/kyukyu_3ji_taisei.html.
- 13. Irisawa T, Iwami T, Kitamura T et al An association between systolic blood pressure and stroke among patients with impaired consciousness in out‐of‐hospital emergency settings. BMC Emerg. Med. 2013; 13: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ambulance Service Planning Office of Fire and Disaster Management Agency of Japan . Supplementary explanation about ambulance records. [cited 30 May 2018]. Available from: http://www.fdma.go.jp/html/new/pdf/150326_hou/7.pdf.
- 15. Jacobs I, Nadkarni V, Bahr J et al Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004; 110: 3385–97. [DOI] [PubMed] [Google Scholar]
- 16. Mitchell GF, Guo CY, Benjamin EJ et al Cross‐sectional correlates of increased aortic stiffness in the community, the Framingham Heart Study. Circulation 2007; 115: 2628–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of patients transported to critical care centers and emergency hospitals in Osaka Prefecture, Japan, by data availability of the Osaka Emergency Information Research Intelligent Operation Network in 2015


