Abstract
Background:
Yoga has its origin from the ancient times. It is an integration of mind, body, and soul. Besides, mindfulness emphasizes focused awareness and accepting the internal experiences without being judgemental. These techniques offer a trending new dimension of treatment in various psychiatric disorders.
Aims:
We aimed to review the studies on the efficacy of yoga and mindfulness as a treatment modality in severe mental illnesses (SMIs). SMI includes schizophrenia, major depressive disorder (MDD), and bipolar disorder (BD).
Methods:
We conducted a literature search using PubMed, Google Scholar, and Cochrane Library with the search terms “yoga,” “meditation,” “breathing exercises,” “mindfulness,” “schizophrenia spectrum and other psychotic disorders,” “depressive disorder,” and “bipolar disorder” for the last 10-year period. We also included relevant articles from the cross-references.
Results:
We found that asanas and pranayama are the most commonly studied forms of yoga for schizophrenia. These studies found a reduction in general psychopathology ratings and an improvement in cognition and functioning. Some studies also found modest benefits in negative and positive symptoms. Mindfulness has not been extensively tried, but the available evidence has shown benefits in improving psychotic symptoms, improving level of functioning, and affect regulation. In MDD, both yoga and mindfulness have demonstrated significant benefit in reducing the severity of depressive symptoms. There is very sparse data with respect to BD.
Conclusion:
Both yoga and mindfulness interventions appear to be useful as an adjunct in the treatment of SMI. Studies have shown improvement in the psychopathology, anxiety, cognition, and functioning of patients with schizophrenia. Similarly, both the techniques have been established as an effective adjuvant in MDD. However, more rigorously designed and larger trials may be necessary, specifically for BD.
Keywords: Bipolar disorder, major depressive disorder, mindfulness, schizophrenia, severe mental illnesses, yoga
Introduction
The term “yoga” stands for “union.” It is a philosophical science seeking unity of an individual's soul with absolute reality. Yoga is gaining importance across the world. While the western world views yoga as a form of physical exercise (PE), the eastern world recognizes yoga more holistically as a means of integration of the body and the mind.[1]
Yoga has been demonstrated to have several positive effects on the cardiorespiratory performance,[2] glucose tolerance,[3] and musculoskeletal system.[4] Similarly, recent evidence has shown promising results of yoga in various psychiatric disorders.
Basically, three forms of yogic practices, namely asana-based (bodily), breathing-based (breath), and meditation-based (mental), are inherent to any form of yoga. An asana-based practice involves various bodily postures coordinated with breathing. Meditation-based yoga involves dissociating oneself from the disturbing thoughts and focusing on breathing. Thirdly breathing-based yoga, which is referred to as “pranayama,” involves slow and focused breathing providing designated time for inhalation and exhalation.
Similar to yoga, another age-old technique that is gaining special attention in the recent years is mindfulness. Mindfulness is an ancient practice from the Buddhist culture, and it emphasizes on the focused attention of present moment, acceptance of internal experiences, and being nonjudgemental.[5] Evidence is favoring positive effects of mindfulness on mental health such as improvement in coping and self-compassion and reduction of stress, anxiety,[6] depression,[7] and obsessions.[8]
Schizophrenia is a severe mental disorder with heterogeneous cluster of symptoms. It is a challenge to attain complete remission in most patients with the current pharmacological agents. The drawback of side effects and minimal effect on cognitive deficits with medications have necessitated the use of yoga and mindfulness in schizophrenia. Similarly, the persistence of depressive symptoms in patients with major depressive disorder (MDD) has led to the trials of complementary therapies, including yoga and mindfulness.[9]
These complementary therapies are finding importance in bipolar disorder (BD) which is one among the severe mental disorders due to similar difficulties.
Here, we aimed at reviewing the available literature for the role of yoga and mindfulness interventions in severe mental illnesses (SMIs) such as schizophrenia, MDD, and BD.
Methods
We conducted an independent search on MEDLINE through PubMed, Google Scholar, and Cochrane Library. The keywords are specific medical subject heading terms, namely “yoga” or “breathing exercises” or “meditation” or “mindfulness.” A time limit of 10 years has been specified, and we restricted the search to English-language articles. We also used the Boolean operator with these terms to combine with “schizophrenia spectrum and other psychotic disorders” yielding 106 results and combining with “bipolar disorder” yielded 22 results. We also used the search term “depressive disorder” and obtained 827 articles. Few studies (n = 6) has been included for the review from the cross-references of these articles.
We screened these results based on title and abstract for suitability to be included in the review. We included all types of human studies such as clinical trials, randomized trials, and nonrandomized trials, as well as open-label studies, case–control studies, and case reports. We excluded opinions expressed on the subject in the form of correspondence and review papers. We specifically excluded the studies on depression that included only depressive symptoms and done in special population with comorbid medical conditions as the feasibility and fidelity of the intervention were doubtful. We also excluded studies that reported mindfulness-based cognitive-behavioral therapy (MBCT) as we believed that these studies were more in the domain of psychotherapies and CBT, which imbibed only some principles from yoga and mindfulness.
We got a total of 49 studies based on the above steps as demonstrated in the flow diagram of Figure 1. The full text of these studies was obtained, and two authors independently extracted the available data using a common format. We assessed the available information and presented under various themes.
Figure 1.
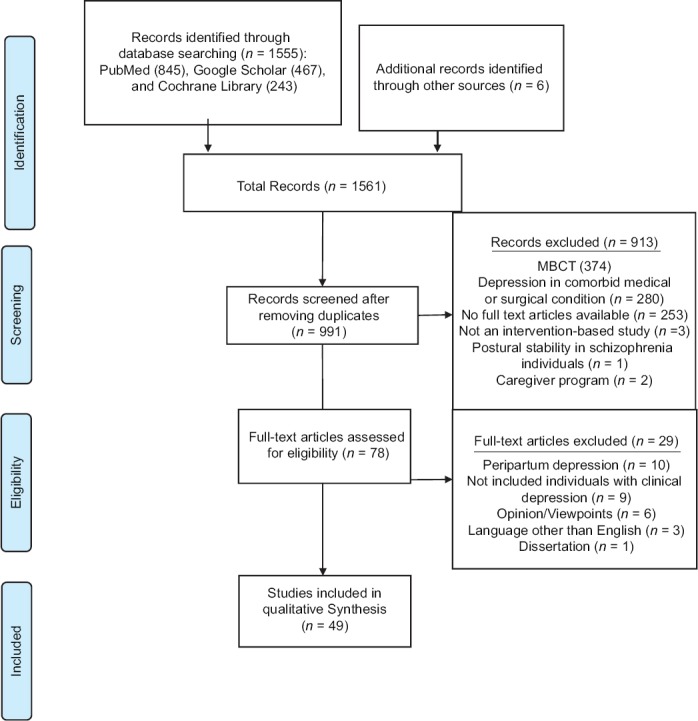
Flow chart of the study-selection process
Results
Forty-nine eligible studies were reviewed for studying the role of yoga and mindfulness in SMI.
Sample characteristics
Sample size in the yoga therapy (YT) studies ranged from 19[10] to 286[11] and in the mindfulness-based intervention (MBI) studies ranged from 5[12] to 340.[13] The above-mentioned sample size range is not inclusive of case report or case series type of studies. Sample size calculation has been mentioned only in a few studies.[13,14,15,16,17,18,19,20] The mean age ranged from 21.50 ± 3.21[21] to 65.5 ± 4.8[20] years in the YT studies and from 23.8 ± 6.8[13] to 53.2 ± 6.1[12] years in the MBI studies. YT and MBI studies included both genders, but few YT studies included either men[18,22] or women,[17,23] and one MBI study included only men.[6] Number of women in MBI studies ranged from 1[12] to 66.[13] The patient group comprised mostly individuals with a diagnosis of either schizophrenia, MDD, or BD as per the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, except for a few studies which used the ICD-10 criteria.[18,22,24,25] Apart from individuals with schizophrenia, a few studies included certain other disorders such as schizoaffective disorder,[6,12,17,26,27] unspecified psychosis,[7,17,21,28] schizophreniform, brief psychotic and delusional disorders,[17] and psychotic depression.[14,29] In YT studies, baseline mean total positive and negative syndrome scale (PANSS) score varied from 47.5 ± 15.4[17] to 85.10 ± 19.82[10] and positive subscale score ranged from 10.2 ± 3.7[17] to 21.60 ± 5.99.[10] Vancampfort et al. have included schizophrenia individuals with a clinical global impression-severity (CGI-S) score ≥4.[30] Few of the YT studies included participants with the mean baseline total scale for the assessment of positive symptoms and scale for the assessment of negative symptoms scores ranging from 6.6 ± 2.3 and 10 ± 4.7[31] to 12.44 ± 11.50 and 23.58 ± 18.09,[11] respectively. In the MBI studies, baseline mean total PANSS score ranged from 77.2 ± 13.7[12] to 88.5 ± 15.8[13] and the positive subscale score ranged from 17.4 ± 2.8[12] to 26.9 ± 8.3.[13] Few studies on MBIs used the brief psychiatric rating scale (BPRS) to assess the severity of the illness and the range varied from 30.6 ± 7.5[16] to 41.83 ± 13.59.[7] YT and MBI studies on depression that used standardized scales are described in Table 1a and b, respectively. Baseline depression severity ranged from 12.5[32] to 26.20 ± 6.60[35] in YT studies and from 7.62 ± 3.92[34] to 30 ± 9.1[35] in MBI studies. Murray et al. have recruited individuals with a baseline mean total young mania rating scale of 2.45 ± 3.00 and Hamilton depression rating scale (HDRS) score of 8.03 ± 9.02.[15]
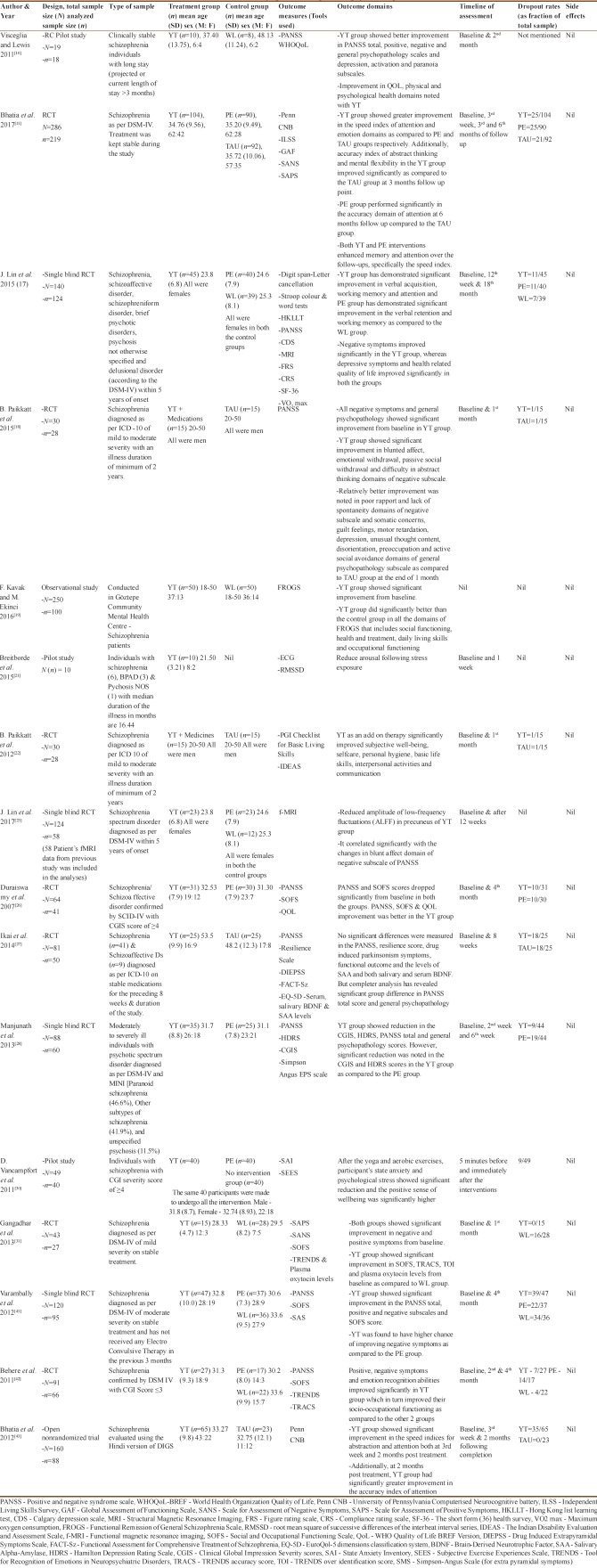
Table 1a.
Details of the studies of yoga in major depressive disorder
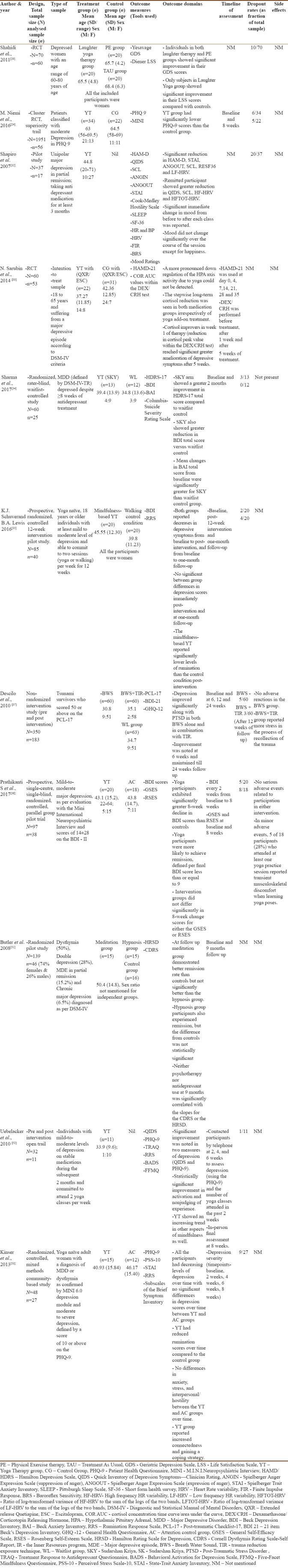
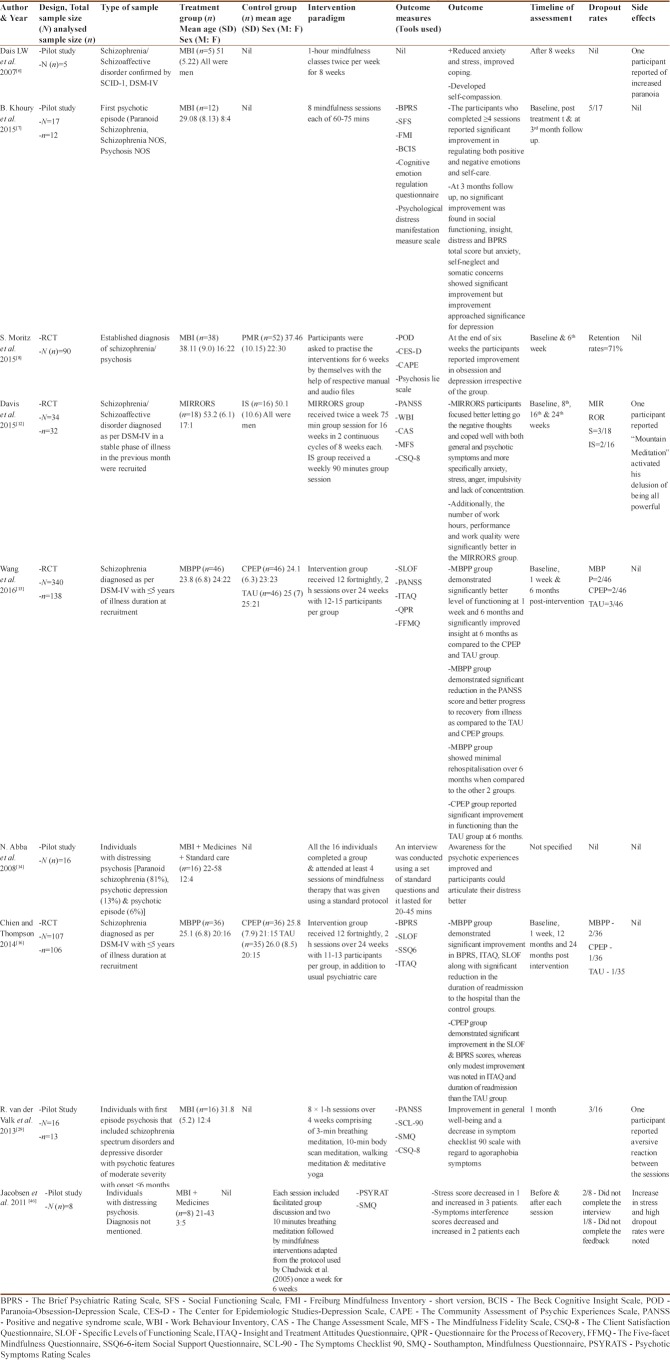
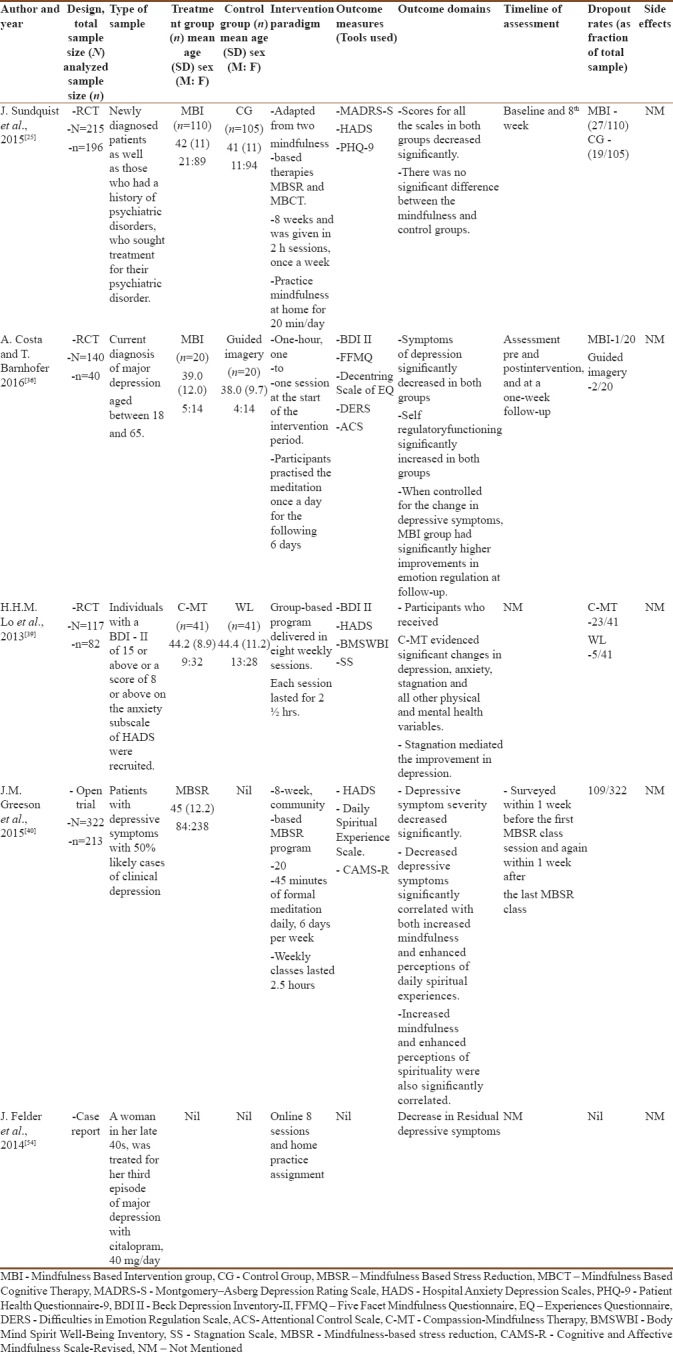
Table 1b.
Details of the studies of mindfulness in major depressive disorder
Intervention paradigm
Details of the YT are described in Table 2. MBI paradigm are included in Tables 3a and 1b. In majority of the studies, the training for the intervention groups has been offered by experts. The duration of sessions ranged from 40 to 90 min and 60 to 120 min in the YT and MBI groups, respectively. Training sessions were either completed during the 1st week or conducted at the frequency of one/two sessions per week. During other days, participants were encouraged to practice the intervention in their homes.
Table 2.
Details of the yoga postures and duration of the intervention including the training period
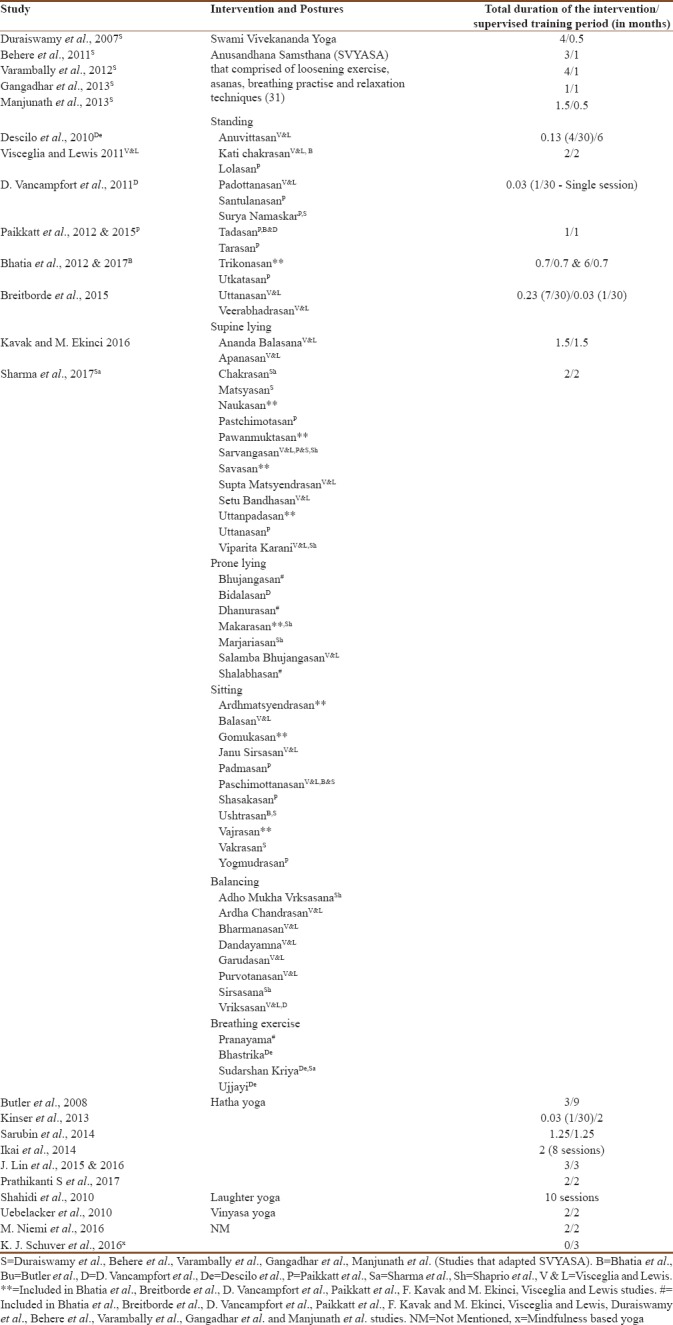
Table 3a.
Details of the studies of mindfulness in schizophrenia/psychotic spectrum disorder
Effects of yoga in schizophrenia and other psychotic spectrum disorders
The results of various studies on YT in schizophrenia are described in Table 4a. Evidence has clearly demonstrated that YT has benefited individuals with schizophrenia.
Table 4a.
Details of the studies of yoga in schizophrenia/psychotic spectrum disorder
Yoga and psychopathology
YT demonstrated a significant improvement in PANSS total score,[26,28,36] positive subscale,[10,31,37] negative subscale,[10,17,18,31,36,37] and general psychopathologic subscale.[10,18,28] A few of the aforementioned studies have identified a significant improvement in specific domains of PANSS negative subscales such as blunted affect, emotional withdrawal, passive social withdrawal, and difficulty in abstract thinking with relatively better improvement in poor rapport and lack of spontaneity.[18] Similarly, in the general psychopathologic subscale, somatic concerns, guilt feelings, motor retardation, depression, unusual thought content, disorientation, preoccupation, and active social avoidance domains showed a significant improvement.[18] Manjunath et al. have reported significant improvement in CGI-S and HDRS of YT group as compared to the PE group.[28]
Yoga and functional outcome
YT has shown promising results in improving functional outcome of schizophrenia individuals, which includes better social and occupational functioning,[26,31,36] quality of life,[26] achieving functional remission,[19] subjective well-being, personal hygiene, life skills, interpersonal activities, and communication.[22] Individuals on YT demonstrated better scores in Tool for Recognition of Emotions in Neuropsychiatric Disorders (TRENDS) accuracy score[31,37] and TRENDS over identification score.[31]
Yoga and cognition
In schizophrenia individuals, YT has demonstrated significant improvement in speed index of attention and emotion domains and accuracy index of abstract thinking and mental flexibility domains.[11,38] Both YT and PE have enhanced memory and attention over the follow-ups, specifically the speed index.[11] YT enhances plasma oxytocin levels, which has been implicated in social cognition.[31]
Yoga, brain imaging, and other markers
Findings of functional magnetic resonance imaging and serum and salivary markers in YT studies are reported in Table 4a.[23,27]
Yoga and physical exercise
Combination of yoga and aerobic exercises in moderately ill individuals with schizophrenia produced a significant reduction in the state anxiety and stress with significant improvement in the positive sense of well-being.[30]
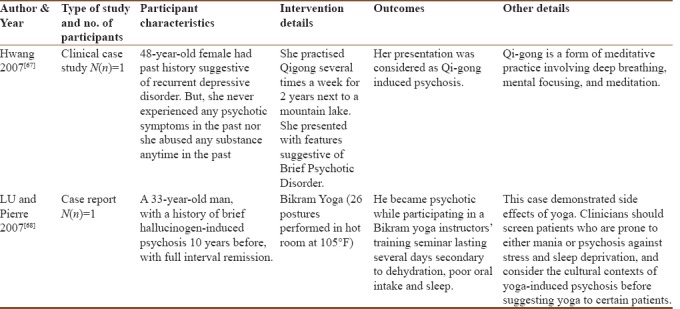
The details of case reports of yoga-induced psychosis are described in Table 4b.
Table 4b.
Details of the case studies of yoga and schizophrenia/psychotic spectrum disorder
Effects of mindfulness technique in schizophrenia and other psychotic spectrum disorders
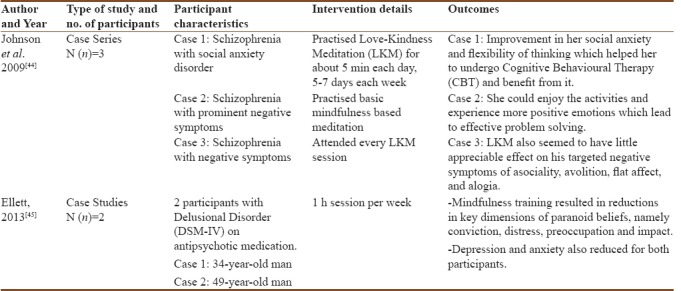
The results of various studies and case reports on mindfulness interventions in schizophrenia are described in Table 3a and b, respectively.
Table 3b.
Details of the case studies of mindfulness and schizophrenia/psychotic spectrum disorder
Mindfulness and illness-related variables
MBI has demonstrated significant reduction of stress, anxiety,[6,12] depression, obsession,[8] anger, impulsivity, lack of concentration,[12] and agoraphobic symptoms.[29] It also improves the awareness of the psychotic experiences and helps individuals to articulate their distress.[14]
Mindfulness-based psychoeducation program (MBPP) has significantly reduced the PANSS score with faster recovery. Further, the number of rehospitalizations[13] and the duration of readmissions[16] decreased over time with MBPP.
MBI has demonstrated significant improvement in certain domains of BPRS, such as anxiety, self-neglect, and somatic concerns, and improvement approached significance for depression, despite having mixed results for total BPRS score.[7]
There are a few case reports implicating the positive role of mindfulness meditation in improving social anxiety, flexibility of thinking, experiencing more positive emotions, and minimal effect on negative symptoms in individuals with schizophrenia.[39] In addition, another case series has demonstrated reduction of paranoid beliefs apart from depression and anxiety in individuals with delusional disorder.[40]
Mindfulness and individual related variables
MBI has demonstrated significant improvement in self-maintenance and community living skill[16] apart from better coping skills, self-compassion,[6] self-care,[7] and general well-being.[29] Further, there have been mixed reports for social functioning and insight.[7,16] A study has demonstrated an increase in stress levels in some patients immediately following the intervention.[41]
Mindfulness and regulation of emotions
In patients, mindfulness has been associated with significant improvement in regulating negative emotions such as self-blaming, rumination, and catastrophizing and developing more adaptive emotion regulation.[7,42]
Yoga and mindfulness in bipolar disorder
We could find only one study of YT and three studies that assessed the role of mindfulness in BD.
Hatha yoga
Uebelacker et al. conducted a qualitative study on yoga practice and the impact of yoga among 70 self-identified yoga practitioners with BD. Positive effects of yoga have been described under cognitive, emotional, and physical domains. Cognitive effects include better-focusing ability, ability to distract from negative thoughts, and a sense of accomplishment. Emotional effects include relaxation and reduction in both anxiety and depression. Moreover, physical effects are the improvement in circulation, heart rate, sleep, weight reduction, and increased energy. In addition, certain negative effects such as agitation with rapid breathing, transition from hypomania to mania with heated energetic yoga style, increased depression-like symptoms with meditation, and physical injury or increased pain have been suggested.[43]
Mindfulness
Chadwick et al. studied 12 stable individuals with BD diagnosed as per the ICD-10, and all the participants received treatment as usual (TAU). They all attended at least six weekly mindfulness sessions, each lasting for 90 min. The participants reported that it enables them to integrate it into all aspects of life and respond wisely. Furthermore, it has been reported to minimize the impact of mood change and prevent further relapse.[44]
Muray et al. studied the role of online MBI like online, recovery-focused, bipolar individual therapy (ORBIT) in 26 clinically stable individuals with late-stage BD with at least six or more episodes. ORBIT focused chiefly on emotion regulation, relationship to self, and improving sleep quality. Sixteen completers demonstrated significant improvement in the quality of life, but the improvement in anxiety did not reach significance (P = 0.06). No significant negative effects have been reported.[45]
Self-management strategies
Murray et al. studied 33 clinically stable individuals with BD Type I or II adapting various self-management strategies. We focused mainly on the reflective and meditative practices among the various self-management strategies which included Tai Chi, yoga, mindfulness, meditation, inspirational reading, and praying. Individuals who practiced Tai Chi and yoga reported that it provided a ground of stability enabling them to manage symptoms of BD well. Moreover, those who engaged in mindfulness cited that it facilitated them in reframing negative thoughts.[15]
Yoga and mindfulness in major depressive disorder
Effects of yoga in major depressive disorder
Results of YT studies in MDD are described in Table 1a. Yoga has demonstrated significant improvement in depression as an adjuvant to antidepressants in several trials.[24,32,33,46,47,48,49,50] Other demonstrated advantages of yoga in depression are improvement in anxiety,[32,50] behavioral activation, and nonjudging facet of mindfulness.[47] Shahidi et al. have established significant improvement in depression and life satisfaction in elderly depressed women as compared to the TAU control group but not against the PE group.[20] A study by Descilo et al. have demonstrated significant improvement in depression among patients with posttraumatic stress disorder. Breathing interventions alone and in combination with exposure therapy in real-life situations were both useful in the improvement of symptoms.[51] Sarubin et al. have demonstrated that in depressed individuals, YT neither demonstrated significant benefit in regulating hypothalamus–pituitary axis nor has any additional benefit over the control group.[52] Similarly, Butler et al. did not demonstrate a significant benefit of YT over group therapy with hypnosis.[46]
Effects of mindfulness in major depressive disorder
MBI other than mindfulness-based cognitive therapy (MBCT) has demonstrated significant improvement in depression.[25,34] An adaptation of MBI from mindfulness-based stress reduction/MBCT, namely compassion-mindfulness therapy, also demonstrated significant improvement in depression.[53] In the study by Costa and Barnhofer, depression improved significantly with both MBI and guided imagery groups. However, the maintenance of the effects required continued practice of mindfulness skills.[35] Although Sundquist et al.'s study demonstrated significant reduction in depressive symptoms from baseline with MBI, no significant advantage has been demonstrated over the TAU control group. In the mindfulness group, those who underwent at least 6–8 sessions have demonstrated significant reduction in depressive symptoms.[25] Another study has established that improvement in depressive symptoms appear to be directly related to the baseline magnitude of depression and may not be related to religious affiliation, spiritual experiences, sex, or age.[36]
Case report of mindfulness mood program (MMB), adapted from MBCT, was found to be cost-effective approach targeting residual depressive symptoms.[54]
Discussion
Yogic practices, though ancient, are being rediscovered by modern medicine. As per the principles of evidence-based medicine, any method of treatment has to prove its efficacy in treating a disorder against a placebo or another preexisting effective treatment. Hence, several medical specialties are conducting studies on the effectiveness of yoga as an intervention so as to be able to recommend it to their patients. In accordance with this trend, yoga is being increasingly used in psychiatric disorders. Commonly, it is used for anxiety and other neurotic disorders; however, there have been several trials in recent times that have studied the efficacy of yoga in SMI.
The studies reviewed have shown that yoga as an add-on to antipsychotics was beneficial in reducing psychopathology and improving socio-occupational functioning. Most studies have included patients with mild-to-moderate levels of current psychopathology as evidenced by PANSS total scores.
Yoga has been shown to improve both positive and negative symptoms of schizophrenia, thereby decreasing the illness severity.[10,17,18,26,28,38,39] This could possibly be explained by the psychobiological changes of yogasanas as evident by reduced amplitude of low-frequency fluctuations in the precuneus which correlated significantly with the PANSS – blunted affect subscore.[23] Further studies are required to replicate the findings on a larger scale to identify whether yoga is associated with similar psychobiological changes.
YT has also been found to significantly improve the facial emotion recognition deficits (FERDs) and socio-occupational functioning.[31,39] FERD can affect socio-occupational functioning by impairing the ability to interact in social situations.[55,56] The finding of increased oxytocin levels in the patients assigned to YT gives a biological basis to the observed behavioral improvements.[31] The use of oxytocin in improving social cognition deficits has been demonstrated in earlier studies.[57]
Both YT and PE interventions showed significant improvement in several cognitive domains including attention and working memory.[11,17] Yoga has a larger effect on verbal acquisition than PE.[17] Yoga can improve cognitive functions possibly by the emphasis on mental concentration and control of the body movements, which can lead to alterations in brain structures and immune functions enhancing cognitive abilities.[58] Cognitive improvement with a brief intervention sustained even after a duration of unsupervised period and certain cognitive domains have also demonstrated delayed improvement.[11] Hence, to have the maximum benefit, yoga must be practiced for certain period. Most of the studies described here have a maximum intervention period of 6 months.
It is still not clear how each of the various postures used in these studies has produced a therapeutic effect. Attention is an inherent component of yoga as it involves synchronizing of bodily postures and breathing pattern. Cognitive remediation techniques use attention-enhancing tasks, and its significance has been well established in schizophrenia.[59] This could be an additional benefit of yoga over PEs. Yogasanas could cause beneficial effects by stimulation of vagal afferents through the pressure receptors and diaphragmatic receptors. These vagal afferents through their projections to limbic system influence the mood and affect regulation.[60]
In MDD, YT has demonstrated to be an effective adjuvant to antidepressants, except for few studies. The lack of an advantage of yoga over group therapy with hypnosis in the study by Butler et al. could be due to poor motivation levels and poor adherence to treatment. Similarly, the study by Shahidi et al. failed to demonstrate benefit of yoga over PE. However, instead of conventional asanas, this study used laughter yoga as the intervention. Many of the other studies have methodological issues such as single-group outcome study without any placebo or control arm.[32,49]
Other studies like that of Schuver and Lewis used visual media for instruction rather than sessions by a therapist. This would have limited the participant learning and practice greatly. The lack of a waitlist control group[35,50] and the low frequency of yoga training (once or twice per week)[33,35,53] may have been responsible for failure of YT in few studies. Hence, it is difficult to comment on the number of sessions per week for effective yoga intervention in depression due to methodological issues in the aforementioned studies. However, the duration of the intervention in the included studies ranged from 5 weeks[52] to 9 months.[48]
A study with a waitlist control group and the yoga group receiving interventions by trained professionals with at least two supervised sessions per week and ensuring home-based continuation of the yoga sessions during rest of the days in a week has clearly demonstrated benefit of yoga as an add-on treatment for depression.[50] Therefore, future studies of yoga intervention could have two or more weekly sessions of personal instruction from a trained yoga therapist. There could also be instructions for regular practice of yoga at home with a method to measure adherence to the therapy during the period of intervention.
Possible mechanisms by which the yoga improves depression include positive self-talk and self-acceptance. It minimizes negative thinking bias, enhances self-confidence, and promotes more adaptive thinking.[9] Other possible mechanisms include increasing gamma-aminobutyric acid neurotransmitter in the brain,[61,62] improving sleep,[63] decreasing ruminations,[64] and promoting behavioral activation.[49]
Similarly, in the recent times, mindfulness technique has been gaining importance as an integrated approach in schizophrenia, MDD, and BD. In schizophrenia individuals, mindfulness interventions are found to be effective in various symptom domains of the illness. However, methodologically, rigorous randomized clinical trials (RCTs) were only few in number.[8,12,13,16] A study by Davis et al. demonstrated that MBI may work synergistically with vocational rehabilitation for improving work persistence and performance. They predominantly involved male samples, and they were employed in a basic-level job with low pay.[12] Hence, the generalizability is limited. Moritz et al. did not establish the superiority of mindfulness over progressive muscle relaxation technique for reducing depressive symptoms in individuals with psychosis possibly due to lack of proper training, lengthy manuals, and difficulty in ensuring adherence.[8] Findings of Jacobsen et al.'s study of increase in stress levels immediately following the intervention must be viewed with caution as the study involved only a small sample size.[43] Mindfulness techniques modulate the individual's relationship with psychotic experiences either by increasing patient's acceptance and awareness of the nature of symptoms, or by minimizing subjective distress. It also facilitates developing self-compassion, regulating negative emotions, and removing guilt feelings.[6,7]
In depression, while the effectiveness of MBCT is well established, other MBIs have also been showing promising results. It has been shown that mindfulness can lead to improvement in depression, anxiety, physical distress, positive affect, and daily functioning.[53]
Possible mechanisms for such improvement may include decentering from negative thinking and reducing the difficulties in emotion regulation. Mindfulness techniques are known to increase meta-cognitive awareness and facilitate decentering. Although such gains may be seen even with guided imagery, the gains are maintained in patients who are able to employ principles of mindfulness even during follow-up. Another mechanism could be the development of non-judgemental, observing stance to the ruminations, thereby facilitating the ruminators to disengage and mitigate the maintaining effect of ruminations in depression.[65]
Recent literature cautions the use of meditative practices in patients with psychosis as it might exacerbate the psychotic experiences.[66] While concerns are raised by the case reports of precipitation of acute psychotic states after certain yogic practices,[67,68] none of the controlled studies involving a larger number of patients have demonstrated such adverse effects with either yoga or MBI. Hence, it appears to be a feasible intervention for individuals with psychotic symptoms and it has been replicated in a few studies.[7,29]
However, we must note that the studies of YT and MBI in schizophrenia and MDD have included patients who had a low level of symptom severity.
One major limitation of RCTs is that double-blinding is not feasible. Compliance in the intervention group after training was not assessed rigorously, except a few studies which used log book, but this has its own limitations. Willingness and attitude toward such alternatives might also influence the outcome significantly. There is often criticism that the observed benefits of yoga may be due to the placebo effect. However, some of the studies have found that there are definite changes in biological markers such as oxytocin increase corresponding to improved social cognition. Such use of biomarkers in the trials of yoga is essential to demonstrate that the effects are specific, genuine, and not merely due to chance or placebo effects.
This review attempts to provide a comprehensive narrative review of two most commonly used complementary therapies in psychiatric disorders, yoga and mindfulness which enable the readers to have a complete understanding of both these interventions. Furthermore, all the included studies were independently reviewed by two authors to extract relevant data and concur on the findings. Limitations include lack of systemic analysis and heterogeneity in the studies. Thus, we have written a narrative review rather than attempt a meta-analysis.
Conclusion
We would like to highlight the importance of integrating yoga and mindfulness interventions as add-on therapy for major mental health disorders. The mental health professionals should work in close association with the therapists to cater the needs of the patients. It is interesting to note that hardly few patients in the included studies had few adverse effects and worsening of positive symptoms during the intervention. This probably suggests that yoga and mindfulness techniques can be practiced by patients with schizophrenia, MDD, and BD without much worsening of symptoms. Further systematic studies are needed to study the beneficial effects and potential neurobiological mechanisms of yoga and mindfulness intervention in patients with schizophrenia, MDD, and BD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.De Michelis E. A History of Modern Yoga: Patanjali and Western Esotericism. London; Continuum: A and C Black; 2005. p. 301. [Google Scholar]
- 2.Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, et al. Effects of hatha yoga and omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10:261–8. doi: 10.1089/107555304323062257. [DOI] [PubMed] [Google Scholar]
- 3.Hunter SD, Dhindsa M, Cunningham E, Tarumi T, Alkatan M, Tanaka H, et al. Improvements in glucose tolerance with Bikram yoga in older obese adults: A pilot study. J Bodyw Mov Ther. 2013;17:404–7. doi: 10.1016/j.jbmt.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Phoosuwan M, Kritpet T, Yuktanandana P. The effects of weight bearing yoga training on the bone resorption markers of the postmenopausal women. J Med Assoc Thai. 2009;92(Suppl 5):S102–8. [PubMed] [Google Scholar]
- 5.Lang AJ. Mindfulness in PTSD treatment. Curr Opin Psychol. 2017;14:40–3. doi: 10.1016/j.copsyc.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Davis LW, Strasburger AM, Brown LF. Mindfulness: An intervention for anxiety in schizophrenia. J Psychosoc Nurs Ment Health Serv. 2007;45:23–9. doi: 10.3928/02793695-20071101-06. [DOI] [PubMed] [Google Scholar]
- 7.Khoury B, Lecomte T, Comtois G, Nicole L. Third-wave strategies for emotion regulation in early psychosis: A pilot study. Early Interv Psychiatry. 2015;9:76–83. doi: 10.1111/eip.12095. [DOI] [PubMed] [Google Scholar]
- 8.Moritz S, Cludius B, Hottenrott B, Schneider BC, Saathoff K, Kuelz AK, et al. Mindfulness and relaxation treatment reduce depressive symptoms in individuals with psychosis. Eur Psychiatry. 2015;30:709–14. doi: 10.1016/j.eurpsy.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Kinser PA, Goehler LE, Taylor AG. How might yoga help depression? A neurobiological perspective. Explore (NY) 2012;8:118–26. doi: 10.1016/j.explore.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: A randomized, controlled pilot study. J Altern Complement Med. 2011;17:601–7. doi: 10.1089/acm.2010.0075. [DOI] [PubMed] [Google Scholar]
- 11.Bhatia T, Mazumdar S, Wood J, He F, Gur RE, Gur RC, et al. A randomised controlled trial of adjunctive yoga and adjunctive physical exercise training for cognitive dysfunction in schizophrenia. Acta Neuropsychiatr. 2017;29:102–14. doi: 10.1017/neu.2016.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis LW, Lysaker PH, Kristeller JL, Salyers MP, Kovach AC, Woller S, et al. Effect of mindfulness on vocational rehabilitation outcomes in stable phase schizophrenia. Psychol Serv. 2015;12:303–12. doi: 10.1037/ser0000028. [DOI] [PubMed] [Google Scholar]
- 13.Wang LQ, Chien WT, Yip LK, Karatzias T. A randomized controlled trial of a mindfulness-based intervention program for people with schizophrenia: 6-month follow-up. Neuropsychiatr Dis Treat. 2016;12:3097–110. doi: 10.2147/NDT.S123239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abba N, Chadwick P, Stevenson C. Responding mindfully to distressing psychosis: A grounded theory analysis. Psychother Res. 2008;18:77–87. doi: 10.1080/10503300701367992. [DOI] [PubMed] [Google Scholar]
- 15.Murray G, Suto M, Hole R, Hale S, Amari E, Michalak EE, et al. Self-management strategies used by ‘high functioning’ individuals with bipolar disorder: From research to clinical practice. Clin Psychol Psychother. 2011;18:95–109. doi: 10.1002/cpp.710. [DOI] [PubMed] [Google Scholar]
- 16.Chien WT, Thompson DR. Effects of a mindfulness-based psychoeducation programme for Chinese patients with schizophrenia: 2-year follow-up. Br J Psychiatry. 2014;205:52–9. doi: 10.1192/bjp.bp.113.134635. [DOI] [PubMed] [Google Scholar]
- 17.Lin J, Chan SK, Lee EH, Chang WC, Tse M, Su WW, et al. Aerobic exercise and yoga improve neurocognitive function in women with early psychosis. NPJ Schizophr. 2015;1:15047. doi: 10.1038/npjschz.2015.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paikkatt B, Singh AR, Singh PK, Jahan M, Ranjan JK. Efficacy of yoga therapy for the management of psychopathology of patients having chronic schizophrenia. Indian J Psychiatry. 2015;57:355–60. doi: 10.4103/0019-5545.171837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kavak F, Ekinci M. The effect of yoga on functional recovery level in schizophrenic patients. Arch Psychiatr Nurs. 2016;30:761–7. doi: 10.1016/j.apnu.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 20.Shahidi M, Mojtahed A, Modabbernia A, Mojtahed M, Shafiabady A, Delavar A, et al. Laughter yoga versus group exercise program in elderly depressed women: A randomized controlled trial. Int J Geriatr Psychiatry. 2011;26:322–7. doi: 10.1002/gps.2545. [DOI] [PubMed] [Google Scholar]
- 21.Breitborde NJ, Dawley D, Bell EK, Vanuk JR, Allen JJ, Lane RD, et al. A personalized paced-breathing intervention to increase heart rate variability among individuals with first-episode psychosis following stress exposure. Schizophr Res. 2015;169:496–7. doi: 10.1016/j.schres.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 22.Paikkatt B, Singh AR, Singh PK, Jahan M. Efficacy of yoga therapy on subjective well-being and basic living skills of patients having chronic schizophrenia. Ind Psychiatry J. 2012;21:109–14. doi: 10.4103/0972-6748.119598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin J, Geng X, Lee EH, Chan SK, Chang WC, Hui CL, et al. Yoga reduces the brain's amplitude of low-frequency fluctuations in patients with early psychosis results of a randomized controlled trial. Schizophr Res. 2017;184:141–2. doi: 10.1016/j.schres.2016.11.040. [DOI] [PubMed] [Google Scholar]
- 24.Niemi M, Kiel S, Allebeck P, Hoan le T. Community-based intervention for depression management at the primary care level in Ha Nam province, Vietnam: A cluster-randomised controlled trial. Trop Med Int Health. 2016;21:654–61. doi: 10.1111/tmi.12674. [DOI] [PubMed] [Google Scholar]
- 25.Sundquist J, Lilja Å, Palmér K, Memon AA, Wang X, Johansson LM, et al. Mindfulness group therapy in primary care patients with depression, anxiety and stress and adjustment disorders: Randomised controlled trial. Br J Psychiatry. 2015;206:128–35. doi: 10.1192/bjp.bp.114.150243. [DOI] [PubMed] [Google Scholar]
- 26.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia – A randomized controlled trial. Acta Psychiatr Scand. 2007;116:226–32. doi: 10.1111/j.1600-0447.2007.01032.x. [DOI] [PubMed] [Google Scholar]
- 27.Ikai S, Suzuki T, Uchida H, Saruta J, Tsukinoki K, Fujii Y, et al. Effects of weekly one-hour hatha yoga therapy on resilience and stress levels in patients with schizophrenia-spectrum disorders: An eight-week randomized controlled trial. J Altern Complement Med. 2014;20:823–30. doi: 10.1089/acm.2014.0205. [DOI] [PubMed] [Google Scholar]
- 28.Manjunath RB, Varambally S, Thirthalli J, Basavaraddi IV, Gangadhar BN. Efficacy of yoga as an add-on treatment for in-patients with functional psychotic disorder. Indian J Psychiatry. 2013;55:S374–8. doi: 10.4103/0019-5545.116314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van der Valk R, van de Waerdt S, Meijer CJ, van den Hout I, de Haan L. Feasibility of mindfulness-based therapy in patients recovering from a first psychotic episode: A pilot study. Early Interv Psychiatry. 2013;7:64–70. doi: 10.1111/j.1751-7893.2012.00356.x. [DOI] [PubMed] [Google Scholar]
- 30.Vancampfort D, De Hert M, Knapen J, Wampers M, Demunter H, Deckx S, et al. State anxiety, psychological stress and positive well-being responses to yoga and aerobic exercise in people with schizophrenia: A pilot study. Disabil Rehabil. 2011;33:684–9. doi: 10.3109/09638288.2010.509458. [DOI] [PubMed] [Google Scholar]
- 31.Jayaram N, Varambally S, Behere RV, Venkatasubramanian G, Arasappa R, Christopher R, et al. Effect of yoga therapy on plasma oxytocin and facial emotion recognition deficits in patients of schizophrenia. Indian J Psychiatry. 2013;55:S409–13. doi: 10.4103/0019-5545.116318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shapiro D, Cook IA, Davydov DM, Ottaviani C, Leuchter AF, Abrams M, et al. Yoga as a complementary treatment of depression: Effects of traits and moods on treatment outcome. Evid Based Complement Alternat Med. 2007;4:493–502. doi: 10.1093/ecam/nel114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarubin N, Nothdurfter C, Schüle C, Lieb M, Uhr M, Born C, et al. The influence of hatha yoga as an add-on treatment in major depression on hypothalamic-pituitary-adrenal-axis activity: A randomized trial. J Psychiatr Res. 2014;53:76–83. doi: 10.1016/j.jpsychires.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 34.Sharma A, Barrett MS, Cucchiara AJ, Gooneratne NS, Thase ME. A breathing-based meditation intervention for patients with major depressive disorder following inadequate response to antidepressants: A randomized pilot study. J Clin Psychiatry. 2017;78:e59–63. doi: 10.4088/JCP.16m10819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schuver KJ, Lewis BA. Mindfulness-based yoga intervention for women with depression. Complement Ther Med. 2016;26:85–91. doi: 10.1016/j.ctim.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 36.Costa A, Barnhofer T. Turning towards or turning away: A comparison of mindfulness meditation and guided imagery relaxation in patients with acute depression. Behav Cogn Psychother. 2016;44:410–9. doi: 10.1017/S1352465815000387. [DOI] [PubMed] [Google Scholar]
- 37.Descilo T, Vedamurtachar A, Gerbarg PL, Nagaraja D, Gangadhar BN, Damodaran B, et al. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 South-East Asia tsunami. Acta Psychiatr Scand. 2010;121:289–300. doi: 10.1111/j.1600-0447.2009.01466.x. [DOI] [PubMed] [Google Scholar]
- 38.Prathikanti S, Rivera R, Cochran A, Tungol JG, Fayazmanesh N, Weinmann E, et al. Treating major depression with yoga: A prospective, randomized, controlled pilot trial. PLoS One. 2017;12:e0173869. doi: 10.1371/journal.pone.0173869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lo HH, Ng SM, Chan CL, Lam KF, Lau BH. The Chinese medicine construct “stagnation” in mind-body connection mediates the effects of mindfulness training on depression and anxiety. Complement Ther Med. 2013;21:348–57. doi: 10.1016/j.ctim.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 40.Greeson JM, Smoski MJ, Suarez EC, Brantley JG, Ekblad AG, Lynch TR, et al. Decreased symptoms of depression after mindfulness-based stress reduction: Potential moderating effects of religiosity, spirituality, trait mindfulness, sex, and age. J Altern Complement Med. 2015;21:166–74. doi: 10.1089/acm.2014.0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Varambally S, Gangadhar BN, Thirthalli J, Jagannathan A, Kumar S, Venkatasubramanian G, et al. Therapeutic efficacy of add-on yogasana intervention in stabilized outpatient schizophrenia: Randomized controlled comparison with exercise and waitlist. Indian J Psychiatry. 2012;54:227–32. doi: 10.4103/0019-5545.102414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Behere RV, Arasappa R, Jagannathan A, Varambally S, Venkatasubramanian G, Thirthalli J, et al. Effect of yoga therapy on facial emotion recognition deficits, symptoms and functioning in patients with schizophrenia. Acta Psychiatr Scand. 2011;123:147–53. doi: 10.1111/j.1600-0447.2010.01605.x. [DOI] [PubMed] [Google Scholar]
- 43.Bhatia T, Agarwal A, Shah G, Wood J, Richard J, Gur RE, et al. Adjunctive cognitive remediation for schizophrenia using yoga: An open, non-randomized trial. Acta Neuropsychiatr. 2012;24:91–100. doi: 10.1111/j.1601-5215.2011.00587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnson DP, Penn DL, Fredrickson BL, Meyer PS, Kring AM, Brantley M, et al. Loving-kindness meditation to enhance recovery from negative symptoms of schizophrenia. J Clin Psychol. 2009;65:499–509. doi: 10.1002/jclp.20591. [DOI] [PubMed] [Google Scholar]
- 45.Ellett L. Mindfulness for paranoid beliefs: Evidence from two case studies. Behav Cogn Psychother. 2013;41:238–42. doi: 10.1017/S1352465812000586. [DOI] [PubMed] [Google Scholar]
- 46.Jacobsen P, Morris E, Johns L, Hodkinson K. Mindfulness groups for psychosis; key issues for implementation on an inpatient unit. Behav Cogn Psychother. 2011;39:349–53. doi: 10.1017/S1352465810000639. [DOI] [PubMed] [Google Scholar]
- 47.Tabak NT, Horan WP, Green MF. Mindfulness in schizophrenia: Associations with self-reported motivation, emotion regulation, dysfunctional attitudes, and negative symptoms. Schizophr Res. 2015;168:537–42. doi: 10.1016/j.schres.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Uebelacker LA, Weinstock LM, Kraines MA. Self-reported benefits and risks of yoga in individuals with bipolar disorder. J Psychiatr Pract. 2014;20:345–52. doi: 10.1097/01.pra.0000454779.59859.f8. [DOI] [PubMed] [Google Scholar]
- 49.Chadwick P, Kaur H, Swelam M, Ross S, Ellett L. Experience of mindfulness in people with bipolar disorder: A qualitative study. Psychother Res. 2011;21:277–85. doi: 10.1080/10503307.2011.565487. [DOI] [PubMed] [Google Scholar]
- 50.Murray G, Leitan ND, Berk M, Thomas N, Michalak E, Berk L, et al. Online mindfulness-based intervention for late-stage bipolar disorder: Pilot evidence for feasibility and effectiveness. J Affect Disord. 2015;178:46–51. doi: 10.1016/j.jad.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 51.Butler LD, Waelde LC, Hastings TA, Chen XH, Symons B, Marshall J, et al. Meditation with yoga, group therapy with hypnosis, and psychoeducation for long-term depressed mood: A randomized pilot trial. J Clin Psychol. 2008;64:806–20. doi: 10.1002/jclp.20496. [DOI] [PubMed] [Google Scholar]
- 52.Uebelacker LA, Tremont G, Epstein-Lubow G, Gaudiano BA, Gillette T, Kalibatseva Z, et al. Open trial of vinyasa yoga for persistently depressed individuals: Evidence of feasibility and acceptability. Behav Modif. 2010;34:247–64. doi: 10.1177/0145445510368845. [DOI] [PubMed] [Google Scholar]
- 53.Kinser PA, Bourguignon C, Whaley D, Hauenstein E, Taylor AG. Feasibility, acceptability, and effects of gentle hatha yoga for women with major depression: Findings from a randomized controlled mixed-methods study. Arch Psychiatr Nurs. 2013;27:137–47. doi: 10.1016/j.apnu.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Felder J, Dimidjian S, Beck A, Boggs JM, Segal Z. Mindful mood balance: A case report of web-based treatment of residual depressive symptoms. Perm J. 2014;18:58–62. doi: 10.7812/TPP/14-019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hooker C, Park S. Emotion processing and its relationship to social functioning in schizophrenia patients. Psychiatry Res. 2002;112:41–50. doi: 10.1016/s0165-1781(02)00177-4. [DOI] [PubMed] [Google Scholar]
- 56.Kee KS, Green MF, Mintz J, Brekke JS. Is emotion processing a predictor of functional outcome in schizophrenia? Schizophr Bull. 2003;29:487–97. doi: 10.1093/oxfordjournals.schbul.a007021. [DOI] [PubMed] [Google Scholar]
- 57.Pedersen CA, Gibson CM, Rau SW, Salimi K, Smedley KL, Casey RL, et al. Intranasal oxytocin reduces psychotic symptoms and improves theory of mind and social perception in schizophrenia. Schizophr Res. 2011;132:50–3. doi: 10.1016/j.schres.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 58.Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65:564–70. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- 59.Lewandowski KE, Eack SM, Hogarty SS, Greenwald DP, Keshavan MS. Is cognitive enhancement therapy equally effective for patients with schizophrenia and schizoaffective disorder? Schizophr Res. 2011;125:291–4. doi: 10.1016/j.schres.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 60.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression. Part II – Clinical applications and guidelines. J Altern Complement Med. 2005;11:711–7. doi: 10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 61.Streeter CC, Jensen JE, Perlmutter RM, Cabral HJ, Tian H, Terhune DB, et al. Yoga asana sessions increase brain GABA levels: A pilot study. J Altern Complement Med. 2007;13:419–26. doi: 10.1089/acm.2007.6338. [DOI] [PubMed] [Google Scholar]
- 62.Streeter CC, Whitfield TH, Owen L, Rein T, Karri SK, Yakhkind A, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: A randomized controlled MRS study. J Altern Complement Med. 2010;16:1145–52. doi: 10.1089/acm.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khalsa SB. Treatment of chronic insomnia with yoga: A preliminary study with sleep-wake diaries. Appl Psychophysiol Biofeedback. 2004;29:269–78. doi: 10.1007/s10484-004-0387-0. [DOI] [PubMed] [Google Scholar]
- 64.Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW, et al. Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. J Psychiatr Pract. 2010;16:22–33. doi: 10.1097/01.pra.0000367775.88388.96. [DOI] [PubMed] [Google Scholar]
- 65.Desrosiers A, Vine V, Klemanski DH, Nolen-Hoeksema S. Mindfulness and emotion regulation in depression and anxiety: Common and distinct mechanisms of action. Depress Anxiety. 2013;30:654–61. doi: 10.1002/da.22124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McGee M. Meditation and psychiatry. Psychiatry (Edgmont) 2008;5:28–41. [PMC free article] [PubMed] [Google Scholar]
- 67.Hwang WC. Qi-gong psychotic reaction in a Chinese American woman. Cult Med Psychiatry. 2007;31:547–60. doi: 10.1007/s11013-007-9065-z. [DOI] [PubMed] [Google Scholar]
- 68.Lu JS, Pierre JM. Psychotic episode associated with Bikram yoga. Am J Psychiatry. 2007;164:1761. doi: 10.1176/appi.ajp.2007.07060960. [DOI] [PubMed] [Google Scholar]