Abstract
Postoperative pain after breast surgery is difficult to manage owing to its complex innervation. Recently, erector spinae plane (ESP) block, an interfacial block, has been described to provide pain relief after thoracic and abdominal surgeries, multiple rib fractures, and neuropathic thoracic pain. Local anesthetic injected in the erector spinae muscle sheath at the level of the 5th thoracic transverse process is distributed cranially and caudally along the sheath, and to the paravertebral space through apertures in the anterior sheath wall. This may block the dorsal and ventral rami of the thoracic spinal nerves at multiple vertebral levels and the rami communicantes transmitting autonomic fibers to and from the sympathetic ganglia, causing multidermatomal somatic and visceral analgesia. The present case report demonstrates the adequate perioperative analgesia provided by the ultrasound-guided ESP block in patients undergoing various breast surgeries.
Keywords: Breast surgery, erector spinae plane block, ultrasound
Introduction
The complex innervation of breast tissues poses a great challenge for the anesthesiologists to provide adequate perioperative analgesia. Multimodal analgesia techniques including various regional blocks are the preferred choice. Recently, erector spinae plane (ESP) block has been described to provide perioperative analgesia covering the dermatomes from T2 to T9 when local anesthesia (LA) is injected at the level of the 5th thoracic transverse process. To the best of our knowledge, there are no reports in the literature demonstrating the use of this block for perioperative analgesia in breast surgeries. We describe our experience of preinduction ESP block at the level of T5 (thoracic) transverse process in 10 patients undergoing breast surgery under general anesthesia (GA).
Case Report
The ESP block was administered in 10, American Society of Anesthesiologists (ASA) I and II female patients aged between 35 and 70 years (median 46 years), weighing 40–90 kg (median 56.5 kg) undergoing breast surgery under GA as a part of a multimodal analgesic technique. Written informed consent was taken from all patients after explaining the block procedure. The block was performed in preanesthesia room after attaching all the ASA standard monitors and securing intravenous (IV) access. All patients were administered 1 mg midazolam IV, oxygen by facemask administered at a flow rate 4 l/min. Patients were positioned lateral with little forward bending and operative site up. T5 spinous process was palpated and marked; another point 3 cm lateral to the midline was also marked after cleaning and draping [Figure 1a]. Then, a high-frequency (6–13 Hz) linear ultrasonographic probe (Sonosite M-Turbo; Sonosite Inc, Bothell, WA) was placed longitudinally over the lateral marking. The three muscles of the back were identified (from superficial to deep) as trapezius, rhomboid major, and erector spinae [Figure 1b] overlying the acoustic shadow of the transverse process. The puncture site was injected with 3 ml of 2% lignocaine hydrochloride. A 22G, 10 cm echogenic needle (Pajunk Sonoplex, Geisingen, Germany) was then inserted “in-plane” from cranial to caudal direction [Figure 2a], to make contact with the transverse process. A volume of 1–2 ml of normal saline was injected to hydrodissect the plane following which 20 ml of ropivacaine (0.375%) was deposited lifting the erector spinae muscle off the transverse process [Figure 2b].
Figure 1.
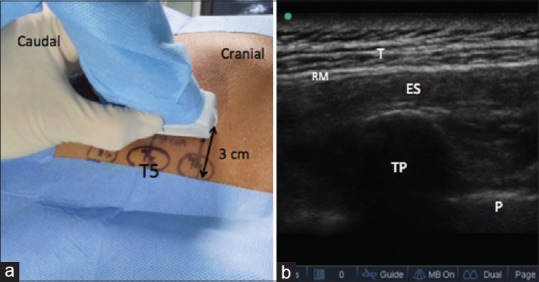
(a) High-frequency probe placed 3 cm lateral to T5 spinous process, (b) T – Trapezius, RM – Rhomboid major, ES – Erector spinae, TP – Transverse process, and P – Pleura
Figure 2.
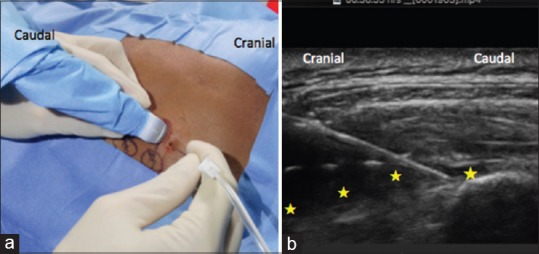
(a) Needle entry in craniocaudal direction, (b) Local anesthetic deposit below Erector spinae muscle * Local anesthetic
GA was induced with fentanyl 2 mcg/kg, propofol 2–3 mg/kg, and atracurium 0.5 mg/kg. The airway was secured with an endotracheal tube or Proseal laryngeal mask airway. 1 mcg/kg of fentanyl was administered if there was a pain response. Paracetamol 1 g and ketorolac 30 mg IV were administered toward the end of surgery along with ondansetron 4 mg IV for antiemesis. The residual neuromuscular blocker was reversed at the end of surgery. Patients were extubated once they were conscious and were following verbal commands.
Postoperatively, all patients received paracetamol 1 g IV 6th hourly and diclofenac sodium 75 mg IV 12th hourly. All patients were monitored in postanesthesia care unit (PACU) for 6 h and then shifted to the wards. Postoperatively, the pain was assessed by 11-point numeric pain rating scale (NRS) from 0 to 10 and fentanyl 25 mcg IV was administered as rescue analgesia if NRS score >4 at any time in PACU. Tramadol 50 mg IV was prescribed as a rescue analgesic in the wards if the patients NRS score exceed 4.
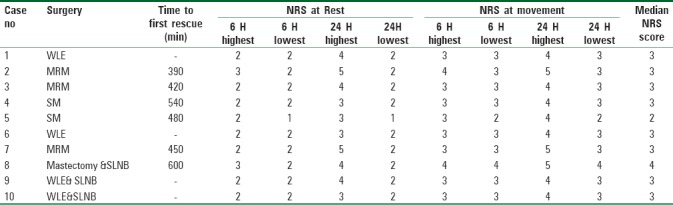
Out of 10 patients, three had undergone modified radical mastectomy and rest were either simple mastectomy or wide local excision with or without sentinel lymph node biopsy. The mean intraoperative fentanyl consumption was 148 mcg. Six patients had intraoperative pain response; however, it was not persistent and well managed with fentanyl only. All patients had a smooth recovery and were pain free at the time of shifting to PACU. The median NRS score in first 6 h was 2 at rest and 3 with movement [Table 1]. The highest median NRS score in 24 h was 4 and six patients received rescue analgesic in the wards. The median time to the first rescue analgesia was 465 min. None of the patients had any procedure related or surgical complications.
Table 1.
Type of surgery and numerical pain rating scale (NRS) score in the first 24 H after surgery
Discussion
We started giving this block in breast surgeries after reviewing the following literature. Forero et al.[1] gave the ESP block in two patients with intractable thoracic neuropathic pain and in two patients for video-assisted thoracoscopic surgery (VATS). The authors observed excellent pain relief in patients with neuropathic pain. The patients with VATS had numbness over posterior and anterolateral thorax till 24 h covering dermatomes T3–T9. We also found similar results and the intraoperative median fentanyl consumption was only 148 mcg although we administered both paracetamol and ketorolac as routine intraoperative nonsteroidal anti-inflammatory drugs. We observed there were raised hemodynamics when surgeons were doing cautery in the infraclavicular area and in the vicinity of pectoral nerves, which is most likely to be spared being branches of brachial plexus. Postoperatively, six of our patients complained of pain on movement, which was controlled with single dose of tramadol 50 mg IV. However, the median NRS score was 4. Similar results were also observed by Chin et al.,[2,3] who performed perioperative bilateral ESP block at T7 level in three patients for laparoscopic bariatric surgery and four patients of ventral hernia repair. In one patient of bariatric surgery, the author placed catheter preoperatively that provided good perioperative analgesia limiting the total opioid requirements. Hamilton et al. did use this block as a standalone anesthetic technique in multiple rib fractures.[4]
Based on cadaver studies, the injection of LA below the erector spinae muscle and closer to the costotransverse foramina would help the spread of LA readily to the paravertebral space.[1] Technically, we found this block is safe and easier compared to paravertebral block; as needle end point being the transverse process poses lesser risk of pleural puncture. The ESM extends along the length of the thoracolumbar spine; this interfacial plane can allow the spread of LA in more extensive manner than the thoracic paravertebral block. To conclude, the ESP block is a safe, simple, and versatile technique. The single facial plane offers analgesia to thoracic, abdominal, and probably for lower limb surgery. Thus, more studies are needed to establish its efficacy.
Financial support and sponsorship
All drugs and equipment used in the case series are our hospital resources (All India Institute of Medical Sciences, New Delhi).
Conflicts of interest
There are no conflicts of interest.
References
- 1.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A Novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 2.Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: A Report of 3 cases. Reg Anesth Pain Med. 2017;42:372–6. doi: 10.1097/AAP.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 3.Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–60. doi: 10.1111/anae.13814. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118:474–5. doi: 10.1093/bja/aex013. [DOI] [PubMed] [Google Scholar]


