Abstract
Background/objectives
To investigate the relationship between the cross-sectional visceral adipose tissue (VAT) areas at different anatomic sites and the total VAT volume in a healthy Chinese population using quantitative computed tomography (QCT), and to identify the optimal anatomic site for a single slice to estimate the total VAT volume.
Subjects/methods
A total of 389 healthy Chinese subjects aged 19–63 years underwent lumbar spine QCT scans. The cross-sectional area of total adipose tissue and VAT were measured using the tissue composition module of the software (QCT Pro, Mindways) at each intervertebral disc level from T12/L1 to L5/S1, as well as at the umbilical level. The total VAT volume was defined as the fat areas multiplied by the height of vertebral body for all six slices. Statistical analysis was performed to determine the correlation between single-slice VAT areas and the total VAT volume. Moreover, the optimal anatomic site for a single slice to estimate the total VAT volume was identified by multiple regression analysis.
Results
The cross-sectional area of VAT and subcutaneous adipose tissue (SAT) measured at each anatomic site was all highly correlated with the total VAT volume and the total SAT volume (r = 0.89–0.98). Additionally, the VAT area measured at the L2/L3 level showed the strongest correlation with the total VAT volume (r = 0.98, P < 0.001). Covariates including age, gender, BMI, waist, and hypertension make a slight effect on the prediction of the total VAT volume.
Conclusion
It is feasible to perform measurements of VAT area on a single slice at L2/L3 level for estimating the total VAT volume.
Introduction
Obesity has already become a major health problem in the United States and it is now becoming an emerging health issue in China. The prevalence of overweight and obesity in China has increased considerably by 7.3 and 4.8% over the past decade (2002–2012). According to the 2015 national health report from the National Health and Family Planning Commission of China, 30.1% of adults over 18 years old are overweight, 11.9% are obese. With China’s 1.36 billion population, this prevalence would translate to a large number of overweight and obese population in the country. Obesity is associated with insulin resistance (type II) diabetes, atherogenic dyslipidemia, cardiovascular disease, hypertension, cancer, sleep apnea, and metabolic syndrome [1, 2]. It is critical to identify those who are at high risk of obesity-related complications so that early interventions can be taken to prevent them from worsening. Overweight and obesity are often defined by the body mass index (BMI) in clinical practice of China. Waist circumference (WC) and waist to hip ratio are other two frequently used anthropometric measurements to define obesity [3]. However, these two measurements are unable to differentiate visceral adipose tissue (VAT) from subcutaneous adipose tissue (SAT). VAT is thought to be the most important indicator for obesity-related complications [3].
The high-resolution cross-sectional imaging modalities, such as computed tomography (CT) and magnetic resonance imaging (MRI), are widely used during our clinical practice. Both imaging techniques can be used to measure the regional adipose tissue in vivo [2, 4]. Although, MRI is free of radiation, its application is still limited by the high cost and long-scanning time. Adipose tissue can be measured fast and accurately using CT [2, 5, 6]. With the commercially available quantitative computed tomography (QCT) software, bone mineral density (BMD) of the vertebrae and the amount of abdominal adipose tissue can be measured at the same time [7]. Therefore, osteoporosis and obesity can be evaluated simultaneously on a single-CT scan.
By using CT or MRI, it is possible to measure the amount of adipose tissue within the whole abdomen. However, considering the high cost, the long-scanning time, and the high-radiation dosage exposure of multi-slice CT scans, investigators sought to find an optimal anatomic site for single-slice imaging to estimate total abdominal adipose tissue volume [2, 4, 8]. Irlbeck et al. [2] used CT scan to measure VAT and SAT from L1/L2 to L5/S1, as well as at the umbilicus level and concluded that the single-slice measurement made at the L3/L4 was strongly associated with the total VAT and SAT volumes in both men and women. Kuk et al. [8] reported that the measurement made at L1/L2 and L2/L3 levels had strongest correlations with the total VAT volume. In the study of Shen et al. [4], MRI was used to measure VAT and SAT volume at different locations and that the single-slice VAT area measured at 10 cm above the umbilicus for men and at 5 cm above for women was found to best predict the total VAT volume. In an MRI study, Maislin et al. [9] reported that the VAT area measured at L2/L3 level was significantly correlated with the VAT volume stronger than traditional anthropometric variables in both the overweight and obese subjects. These studies suggested that a single slice measurement by CT or MRI at the upper abdominal level might provide better risk assessments for metabolic syndrome or cardiovascular disease in a western population.
It is well known that the Asian people often have a larger amount of VAT volume than Caucasian and African American people even after adjustment of weight or BMI [10]. Asian people are also a diverse ethnical and racial group of different statures, as well as fat distribution. It is therefore important to establish the optimal anatomic site for measurement in the Chinese population. Currently it is unknown yet whether the single upper abdomen slice that best estimates total VAT volume in western populations remains true in a Chinese population. Therefore, the objective of this study was to investigate the relationships between the cross-sectional VAT and SAT areas at different anatomic sites and the total VAT and SAT volumes using QCT in a healthy Chinese population, and to identify the optimal anatomic site for estimating the total VAT and SAT volumes.
Materials and methods
Sample size determination
The sample size was determined by assuming a normal distribution for the desired confidence interval of 95% and fixing the probability of committing type I error (α) at 5% and that of type II error (β) at 20%, thus maintaining the power of the study at 80%. The calculated sample size was ~246.
Subjects
Participants of this study were the subjects recruited from an ongoing spine and knee degeneration study started from June 2014. This spine and knee degeneration study was designed to recruit healthy subjects at baseline and to follow them up for 10 years to investigate the potential development of degeneration and the related risk factors. The present study analyzed the existing data of the spine and knee degeneration study. Informed consent was obtained from all subjects, and the study protocol was approved by the Ethic Committee of Jishuitan hospital.
We included all participants of spine and knee degeneration study with the inclusion criteria as follows: healthy adults; 18–65 years old; and lived in Beijing >5 years. Subjects were defined as healthy based on the results of the questionnaire, physical examinations, and routine blood screening performed by a clinical physician. Subjects were excluded if they have the following conditions: (1) spine or knee disorders due to congenital, tumor or tuberculosis; (2) a history of spine or knee injury or surgery; (3) suffered other major diseases (such as infection, tumor, rheumatic immune disease, renal failure, coronary heart disease, stroke, and mental diseases) and taking bone metabolism regulating drugs; (4) during pregnancy or breastfeed; (5) heart pace maker, coronary stent, orthopedic implants, and implant teeth; and (6) familial hereditary disease. A total of 430 subjects had QCT measurement results. We excluded 2 subjects for missed height and weight data, 8 subjects with BMI <18.5 or >35, and 31 subjects because of the incomplete coverage of T12 to S1 caused by improper positioning of the calibration phantom. Finally, a total of 389 subjects with complete data and complete CT coverage of T12 to S1 were included in the present study.
Anthropometric measurements
Body weight and height were measured with the resolution of 0.1 kg and 0.1 cm with the use of appropriately calibrated scales and stadiometer. WC was measured at 1 cm above the umbilicus with the subjects wearing undergarments and standing with their heels together. Hip circumference was taken at the level of iliac crest. Blood pressure was measured according to the study protocol.
Blood test
Blood samples were taken from all subjects. Complete blood cell count and serum lipids including triglyceride and cholesterol were measured.
CT scan protocol
As part of the protocols of the spine and knee degeneration study, all subjects underwent abdominal QCT scans. All QCT scans and image analyses were performed in the department of Radiology, Beijing Jishuitan Hospital. The details of the QCT acquisition were reported previously [7]. Briefly, a standard abdominal CT scan was performed for each of the subject on a Toshiba 64-slice or on an 80-slice CT scanner with a Mindways QCT pro (Mindways, Austin, TX, USA) calibration phantom positioned under the back.
Adipose tissue measurement
The CT volumetric dataset was transferred to a Mindways QCT workstation and the measurement of abdominal adipose tissue was performed by trained and qualified radiologists. The details of adipose tissue measurement of each slice were described in earlier publications [7]. Briefly, the software automatically positions a closed spline at the subcutaneous margin—the boundary between the subcutaneous fat and abdominal muscle. The resulting spline boundary can be modified by the user, as needed, by moving spline control points. An example where manual adjustment of the spline boundary would be needed is in anterior regions of the abdomen where abdominal muscle may be so thin as to allow the spline boundary to transition into the abdominal cavity. Soft-tissue pixels were segmented on a per-pixel basis by CT value in to a predicted mixture of fat and lean muscle that would be expected to yield the observed CT value. The calculation of CT value from a mixture of fat and lean tissue makes use of the CT calibration data derived from the phantom imaged with the patient and the ICRU (International Commission on Radiation Units and Measurements) Publication 46 average atomic compositions for adult adipose tissue and lean muscle.
Similar to the method introduced by Irlbeck et al. [2], slices at the level of each intervertebral space were selected on the CT-Scout image software for further analyses. As a result, six slices at each intervertebral space from T12/L1 to L5/S1, as well as an extra slice at the umbilicus level were measured. On each 1 mm-thick slice, adipose tissue was segmented and mapped as blue color with default threshold, then the outer contour of abdominal wall was outlined by the software automatically. Total adipose tissue (TAT) and VAT area (cm2) were semi-automatically measured by the Tissue Composition Module of the software (Mindways, Austin, TX, USA), results were exported to Excel format. SAT was calculated as SAT = TAT–VAT, and the VAT/TAT ratio, as well as the SAT/TAT ratio were calculated. The TAT volume (cm3) of each compartment was defined as the sum of fat area (cm2) multiply by the height (cm) between the two adjacent slices. It should be mentioned that there may be interpolation in the process of selecting the slices which can distort image data. As it could be involved in selecting all the 7 slices, interpolation was put aside in our present study, which focused on the optimization of the preferable slice.
The inter-observer and the intra-observer reproducibility of measurements were evaluated by measuring 30 subjects between two radiologists, and repeating the measurements by one radiologist at 1-month’s interval.
Statistical analysis
All continuous variables were expressed as ‘mean ± s.d.’ and examined for normality using the Kolmogorov–Smirnov test. We compared the mean scores between two different groups by two-sided Student’s t-test. One-way analysis of variance and Dunnett’s T3 post hoc tests were employed for multiple comparisons with no adjustments. The intra-class correlation coefficient (ICC) was used to calculate the inter-observer and intra-observer measurement reliability. What deserves to be mentioned is that ICC is employed to evaluate the reliability of manual operation but not to assess segmentation repeatability. Area overlap measurement of actual image segmentation is an appropriate approach [11]. The correlations between the single-slice VAT areas and the total VAT volume were calculated for each slice, and two-sided Steiger’s Z-test was used to identify the optimal anatomic site for measurement [12]. A simple regression model was then applied to separately identify the coefficients for the observed relationships between the total VAT volume and the VAT area for a selected slice. Multiple regression models were then finally applied to detect whether the relationship between the total VAT volume and the VAT area of the selected slice was independent from age, sex, BMI, or WC. All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). A P-value <0.05 was considered to be statistically significant.
Results
Characteristics of subjects
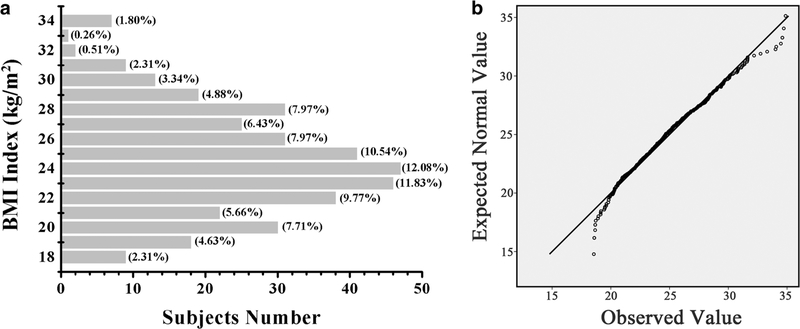
The characteristics of the subjects were presented in Table 1. The BMI of 210 (54.0%) subjects were ranging from 18.5 to 24.9, and the BMI of 147 (37.8%) subjects were ranging from 25.0 to 29.9, and the BMI of the remaining 32 (8.2%) subjects were >30.0 (Fig. 1) (Z = 0.882, P = 0.417).
Table 1.
Characteristics of the subjects
| Variables | Men (n = 161) | Women (n = 228) | P-value |
|---|---|---|---|
| Age (y) | 40.8 ± 8.4 | 40.3 ± 8.6 | 0.544 |
| Height (cm) | 172.3 ± 6.1 | 160.2 ± 5.7 | <0.001 |
| Weight (kg) | 77.7 ± 11.0 | 61.9 ± 9.0 | <0.001 |
| WC (cm) | 91.1 ± 8.5 | 80.0 ± 8.4 | <0.001 |
| HC (cm) | 100.6 ± 5.9 | 96.9 ± 5.8 | <0.001 |
| BMI (kg/m2) | 26.1 ± 3.2 | 24.1 ± 3.4 | <0.001 |
| SBP (mmHg) | 125.2 ± 12.7 | 115.0 ± 14.6 | <0.001 |
| DBP (mmHg) | 78.0 ± 9.91 | 70.9 ± 10.7 | <0.001 |
| Hypertension | 28 (17.4%) | 20 (8.77%) | 0.011 |
WC waist circumference, HC hip circumference, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure
Fig. 1.
BMI distribution of subjects in the study (a) and the Q–Q plot of BMI values (b)
Inter and intra-observer reliabilities of QCT measurement
The inter-observer and intra-observer reliabilities of QCT measurements expressed as ICC were shown in Table 2. The ICC values were ranging from 0.963 to 0.996.
Table 2.
Inter- and intra-observer measurements of abdomen VAT at different locations (cm2, mean ± s.d.)
| Inter-observer
measurements |
Intra-observer
measurements |
|||||
|---|---|---|---|---|---|---|
| A | B | ICC | C1 | C2 | ICC | |
| L2 | 113.65 ± 62.91 | 112.81 ± 62.18 | 0.990 | 111.59 ± 62.26 | 111.19 ± 62.38 | 0.996 |
| L3 | 102.06 ± 49.90 | 102.39 ± 50.64 | 0.996 | 101.43 ± 50.03 | 101.33 ± 51.51 | 0.996 |
| L4 | 87.15 ± 40.45 | 85.79 ± 39.71 | 0.988 | 85.40 ± 38.65 | 86.14 ± 38.17 | 0.988 |
| L5 | 83.15 ± 30.75 | 81.87 ± 29.55 | 0.990 | 83.78 ± 32.67 | 83.23 ± 29.49 | 0.986 |
All P-values for ICC > 0.05
VAT visceral adipose tissue, ICC intra-class correlation coefficient, A measurement results of observer A, B measurement results of observer B, C1 first measurement results of observer C, C2 second measurement results of observer C at 1 month’s interval
Variations of VAT and SAT areas between slices at different anatomic sites
Substantial differences were observed among different anatomic sites for VAT areas, SAT area, as well as the VAT/SAT ratio (Table 3).
Table 3.
VAT and SAT measurements at different anatomic slices
| Variables | Men | Women | Total |
|---|---|---|---|
| VAT | |||
| T12/L1 (cm2) | 171.62 ± 73.96 | 87.29 ± 50.22 | 122.19 ± 73.90a |
| L1/L2 (cm2) | 179.24 ± 71.14 | 99.79 ± 49.31 | 132.67 ± 71.03a |
| L2/L3 (cm2) | 170.00 ± 64.30 | 101.63 ± 48.54 | 129.92 ± 64.96a |
| L3/L4 (cm2) | 141.57 ± 53.96 | 94.81 ± 40.52 | 114.16 ± 51.90a |
| L4/L5 (cm2) | 119.05 ± 39.87 | 90.16 ± 32.09 | 102.11 ± 38.22a |
| L5/S1 (cm2) | 102.58 ± 32.11 | 85.57 ± 26.41 | 92.61 ± 30.06a |
| Umbilicus (cm2) | 127.99 ± 47.97 | 89.83 ± 34.08 | 105.62 ± 44.52a |
| SAT | |||
| T12/L1 (cm2) | 72.15 ± 38.94 | 90.20 ± 43.97 | 82.73 ± 42.84b |
| L1/L2 (cm2) | 88.11 ± 46.17 | 109.24 ± 50.39 | 100.50 ± 49.74b |
| L2/L3 (cm2) | 112.82 ± 53.18 | 131.28 ± 53.24 | 123.64 ± 53.92b |
| L3/L4 (cm2) | 141.87 ± 61.92 | 144.97 ± 57.97 | 143.69 ± 59.58b |
| L4/L5 (cm2) | 167.02 ± 71.13 | 182.76 ± 66.18 | 176.24 ± 68.62b |
| L5/S1 (cm2) | 153.59 ± 67.44 | 210.85 ± 66.08 | 187.15 ± 72.30b |
| Umbilicus (cm2) | 153.92 ± 64.41 | 173.44 ± 67.94 | 165.36 ± 67.11b |
| VAT/SAT | |||
| T12/L1 | 2.77 ± 1.41 | 1.02 ± 0.49 | 1.74 ± 1.30c |
| L1/L2 | 2.38 ± 1.05 | 0.98 ± 0.44 | 1.56 ± 1.02c |
| L2/L3 | 1.73 ± 0.80 | 0.80 ± 0.32 | 1.18 ± 0.73c |
| L3/L4 | 1.11 ± 0.45 | 0.70 ± 0.32 | 0.87 ± 0.43c |
| L4/L5 | 0.79 ± 0.31 | 0.53 ± 0.21 | 0.64 ± 0.29c |
| L5/S1 | 0.76 ± 0.29 | 0.43 ± 0.13 | 0.56 ± 0.27c |
| Umbilicus | 0.90 ± 0.33 | 0.56 ± 0.23 | 0.70 ± 0.32c |
VAT visceral adipose tissue, SAT subcutaneous adipose tissue, VAT/ SAT ratio of VAT to SAT
Levene test: F = 82.975, P < 0.001; one-way analysis of variance (ANOVA): F = 36.084, P < 0.001; Dunnett’s T3 post hoc test: T12/L1 vs. L1/L2, P = 0.610; T12/L1 vs. L2/L3, P = 0.933; T12/L1 vs. L3/L4, P = 0.823; T12/L1 vs. umbilicus, P = 0.003 < 0.05; L1/L2 vs. L2/L3, P = 0.997; all others, P < 0.001
Levene test: F = 20.018, P < 0.001; ANOVA: F = 191.876, P < 0.001; Dunnett’s T3 post hoc test: L4/L5 vs. L5/S1, P = 0.483; L4/L5 vs. umbilicus, P = 0.419; all others, P < 0.001
Levene test: F = 148.207, P < 0.001; ANOVA: F = 144.890, P < 0.001; Dunnett’s T3 post hoc test: T12/L1 vs. L1/L2, P = 0.426; L4/L5 vs. L5/S1, P = 0.003 < 0.05; L4/L5 vs. umbilicus, P = 0.068; all others, P < 0.001
The correlation of measurement between a single slice with the total fat volume
Correlations between VAT and SAT area measurement on a single slice at different anatomic sites with the total volume of VAT and SAT were high (Supplementary Figure S1). Pearson’s correlation coefficient was highest for VAT measurements at L2/L3 level. However, SAT measurements at different anatomic locations did not show statistical significance on Pearson’s correlation coefficients (Table 4).
Table 4.
Pearson’s correlation coefficients for VAT and SAT volume with VAT and SAT areas measured at different anatomic locations
| T12/L1 | L1/L2 | L2/L3 | L3/L4 | L4/L5 | L5/S1 | Umbilicus | |
|---|---|---|---|---|---|---|---|
| Men | |||||||
| VAT areaa | 0.924 | 0.959 | 0.973 | 0.959 | 0.958 | 0.919 | 0.939 |
| SAT areab | 0.941 | 0.957 | 0.967 | 0.969 | 0.976 | 0.942 | 0.948 |
| Women | |||||||
| VAT areaa | 0.892 | 0.953 | 0.973 | 0.978 | 0.951 | 0.911 | 0.951 |
| SAT areab | 0.923 | 0.948 | 0.946 | 0.937 | 0.939 | 0.934 | 0.918 |
| Total | |||||||
| VAT areaa | 0.936 | 0.968 | 0.980 | 0.971 | 0.949 | 0.894 | 0.950 |
| SAT areab | 0.924 | 0.946 | 0.954 | 0.946 | 0.956 | 0.906 | 0.930 |
VAT visceral adipose tissue, SAT subcutaneous adipose tissue
All P-values for Pearson’s correlation coefficients <0.001
Steiger’s Z-test: T12/L1 vs. L1/L2, Z = 9.750, P < 0.01; T12/L1 vs. L2/ L3, Z = 12.24, P < 0.01; T12/L1 vs. L3/L4, Z = 7.71, P < 0.01; T12/L1 vs. L4/L5, Z = 2.24, P < 0.05; T12/L1 vs. L5/S1, Z = 4.84, P < 0.01; T12/ L1 vs. umbilicus, Z = 2.37, P < 0.05; L1/L2 vs. L2/L3, Z = 5.459, P < 0.01; L1/L2 vs. L3/L4, Z = 0.972, P > 0.05; L1/L2 vs. L4/L5, Z = 4.702, P < 0.01; L1/L2 vs. L5/S1, Z = 11.600, P < 0.01; L1/L2 vs. umbilicus, Z = 4.366, P < 0.01; L2/L3 vs. L3/L4, Z = 3.608, P < 0.01; L2/L3 vs. L4/ L5, Z = 9.066, P < 0.01; L2/L3 vs. L5/S1, Z = 15.866, P < 0.01; L2/L3 vs. umbilicus, Z = 8.833, P < 0.01; L3/L4 vs. L4/L5, Z = 6.114, P < 0.01; L3/L4 vs. L5/S1, Z = 12.762, P < 0.01; L3/L4 vs. umbilicus, Z = 6.001, P < 0.01; L4/L5 vs. L5/S1, Z = 9.037, P < 0.01; L4/L5 vs. umbilicus, Z = 0.243, P > 0.05; L5/S1 vs. umbilicus, Z = 8.077, P < 0.01
Steiger’s Z-test: T12/L1 vs. L1/L2, Z= 6.032, P < 0.01; T12/L1 vs. L2/L3, Z= 5.441, P < 0.01; T12/L1 vs. L3/L4, Z= 3.270, P < 0.01; T12/L1 vs. L4/ L5, Z= 5.202, P < 0.01; T12/L1 vs. L5/S1, Z= 2.096, P < 0.05; T12/L1 vs. umbilicus, Z= 0.789, P > 0.05; L1/L2 vs. L2/L3, Z= 1.907, P > 0.05; L1/ L2 vs. L3/L4, Z= 0.105, P > 0.05; L1/L2 vs. L4/L5, Z= 1.962, P < 0.05; L1/L2 vs. L5/S1, Z= 5.363, P < 0.01; L1/L2 vs. umbilicus, Z= 2.480, P < 0.05; L2/L3 vs. L3/L4, Z= 1.5911, P > 0.05; L2/L3 vs. L4/L5, Z= 0.434, P > 0.05; L2/L3 vs. L5/S1, Z= 6.764, P < 0.01; L2/L3 vs. umbilicus, Z= 4.001, P < 0.01; L3/L4 vs. L4/L5, Z= 2.378, P < 0.05; L3/L4 vs. L5/S1, Z = 5.403, P < 0.01; L3/L4 vs. umbilicus, Z= 2.636, P < 0.01; L4/L5 vs. L5/S1, Z= 7.270, P < 0.01; L4/L5 vs. umbilicus, Z= 5.161, P < 0.01; L5/ S1 vs. umbilicus, Z= 2.845, P < 0.01
Estimation of total volume from a single-slice measurement
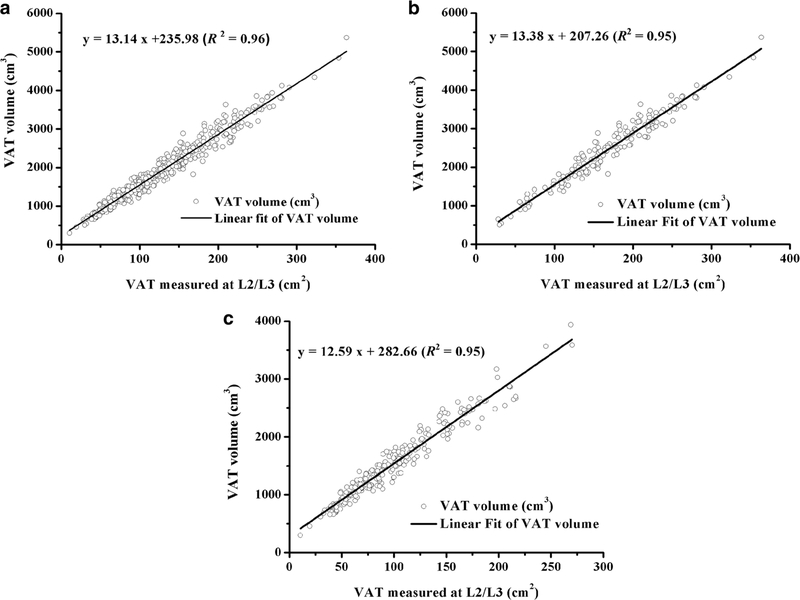
Take L2/L3 slice for example, the estimation of total volume from a single measurement with adjustment of potential covariates was shown in Table 5. Using linear regression models, we investigated the prediction of total VAT volume using the VAT area from L2/L3 and assessed the effect of covariates on the prediction. The L2/L3 slice alone explained 96.1% (94.7% for both men and women, respectively) of the variance in total abdominal VAT volume (Figs. 2, 3), and the addition of covariate terms (although some were significant) did not increase the R2 - <value. Moreover, the model errors were also similar between the L2/L3 slice alone (RMSE = 172.7 cm3 for VAT, CV = 8.89%) and adding additional terms to the L2/ L3 model (RMSE = 170.2 cm3 for VAT, CV = 8.76%).
Table 5.
Regression equations to predict total VAT volume from the VAT area scanned at L2/L3
| Variables in model | R2 | RMSE | CV | AIC |
|---|---|---|---|---|
| L2/L3a | 0.96 | 172.7 | 8.89 | 4010 |
| L2/L3a + agea | 0.96 | 171.6 | 8.83 | 4006 |
| L2/L3a + agea + sexb | 0.96 | 171.1 | 8.81 | 4004 |
| L2/L3a + agea + sexb + BMIb | 0.96 | 171.1 | 8.81 | 4006 |
| L2/L3a + agea + sexb + BMIa + waista | 0.96 | 170.2 | 8.76 | 4003 |
| L2/L3a + agea + sexb + BMIa + waista + hypertensionb | 0.96 | 170.4 | 8.77 | 4004 |
VAT visceral adipose tissue, L2/L3, VAT area measured at L2/L3 level, R2 percentage of variance explained by the regression variables, RMSE root mean squared error, CV coefficient of variation, AIC Akaike information criterion
Term is significant in the model
Term is not significant in the model
Fig. 2.
The scatter plots of VAT measured at L2/L3 with total VAT volume indicate linear correlation for all the participants (a), for men (b), and for women (c)
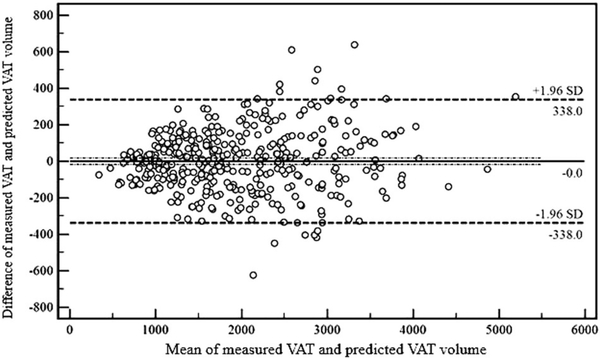
Fig. 3.
Bland–Altman analysis demonstrates that measured VAT volume was in good consistency with predicted VAT volume by L2/L3 slice
Determination coefficients of VAT areas at L2/L3 were higher than those of SAT areas for both sexes (R2 for VAT of 0.947 and 0.947, R2 for SAT of 0.894 and 0.936, for women and men, respectively). The explained variance of total-body VAT volume at L2/L3 reference in women (94.7%) was the same as in men (standard error of estimate: 0.14 L for women, 0.20 L for men). When compared with women, the explained variance of total-body SAT volume at L2/L3 reference in men was 4.2% higher with a lower standard error of estimate (0.30 L for women, 0.26 L for men). Prediction equations for total volumes (V) of VAT and SAT from the slice area (A) at L2/L3 were as follows.
VAT
| (1) |
| (2) |
SAT
| (3) |
| (4) |
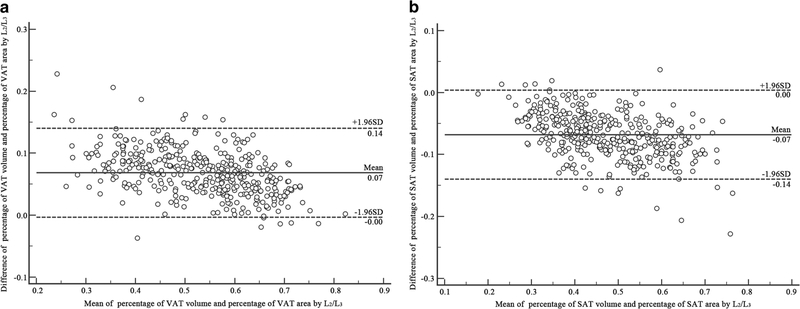
Bland–Altman plots with percentages of VAT and SAT volumes and percentages of VAT and SAT areas at L2/L3 showed the following agreement (Fig. 4).
Fig. 4.
Bland–Altman plots with percentages of adipose tissue volume and percentages of adipose tissue area at L2/L3 slice: (a) VAT, (b) SAT
Discussion
Traditionally, CT or MRI measurement was made at the umbilicus or L4/L5 level for the estimation of the total volume of VAT, partially due to the convenience of locating the umbilicus. Moreover, high-VAT diagnostic criteria of 100 cm2 at the umbilical level using CT scan was proposed for Japanese population [13]. Recently, Jia et al. [14] utilized the MRI to measure the VAT and SAT using a single slice at L4/L5 level and found that both the VAT and SAT were correlated well with the WC and waist to hip ratio in Chinese population.
The present study showed strong correlations (r = 0.89–0.97) between a single-slice VAT area and the total VAT volume in a large healthy Chinese population, which was in consistent with the previous studies performed on western populations [2, 4, 8, 15]. These findings might be helpful for future CT or MRI studies on VAT measurements in larger populations. Moreover, considering the higher radiation dosage exposed in CT scan and the longer scanning time consumed in MRI studies, our results made it possible to estimate the total VAT volume from a single CT or MRI slice and to calculate the cutoff value for the metabolic syndrome or the cardiovascular disease risk assessments.
Previous investigations favored the L4/L5 or the umbilical level for total VAT measurements [4]. However, Demerath et al. [15] claimed that 6 cm above the L4/L5 level (the L3 level) was the optimal anatomic site for total VAT measurements, and this was in accordance with the conclusion of whole-body MRI by Schweitzer et al. [16]. It was revealed that a single-MRI slice at the level of L3 was the best compromise site to assess total tissue volumes of skeletal muscle, VAT and SAT; but L3 did not predict changes in tissue components. Tong et al. [17] reported it was more superiorly located at L3–L4 for VAT measurements to achieve the maximum area-to-volume correlation by the standardized anatomic space method based on a full volume CT scan. Moreover, the anatomic location of maximum correlation derived from nonlinear mapping has more precision (10% higher) than that from simple linear mapping. And this is because the nonlinear mapping approach guaranteeing that the slice with maximum correlation is localized at the same anatomical location irrespective of patient-to-patient anatomical variability [17]. It should be mentioned that both the linear and nonlinear approaches are two methods of assigning landmark labels after segmentation of images, instead of the area-to-volume correlation of VAT.
It was demonstrated in our study that VAT area measurements at L2/L3 slice showed the strongest correlation with the total VAT volume than other slices (Table 4). Difference of results among studies include diversity of population (nation, race), and the region for CT datasets analysis. When choosing the optimal anatomic site, several factors should be considered. We would like to recommend that the L2/L3 intervertebral disc space might be the reasonable optimal anatomic site for a single CT slice measurement. First, the L2/L3 level was shown as the preferable locations for VAT area-to-volume correlations. Second, limiting the CT scanning range to the upper abdomen could reduce the dosage of radiation. Third, with the upper abdominal CT or MRI images available, it was possible to combine the VAT measurements with the BMD, as well as the liver fat assessments in a single exam. More valuable information can be used to analyze the relationship of BMD, VAT and the liver steatosis. However, future studies are still needed to verify the power of this anatomic site in assessing the risk for various visceral fat-related diseases.
Variations in VAT and SAT area were found in slices at different scanning levels, as well as in different subjects. These might weaken the use of a single-slice measurement during our clinical practice. However, Kuk et al. [8] reported that the VAT measurements at different scanning levels all had the power to assess the risk for the metabolic syndrome, with the highest odds ratio found at the L1/L2 level. Nevertheless, future studies with larger sample size are still needed.
Abdominal VAT measurement by QCT was fast and accurate, as well as easy to be performed during our clinical practice. The major concern of using the QCT for VAT measurement was the dosage of radiation. However, we need to justify the use of the CT scan for a medical problem. For instance, in a low-dosage upper abdominal CT scan, the BMD, visceral fat and liver fat could all be accurately measured with a single-CT exam, all of which were important for assessing the risks of osteoporosis, liver steatosis, and cardiovascular diseases. The benefits have over-weighted the side effects of radiation exposure. Moreover, as low as reasonably achievable (ALARA) principle for radiation should always be followed when the CT scan was performed, and there were several ways to reduce the dosage of radiation during the CT scan. First, a reasonable low-dosage scanning parameter should be applied for VAT measurement. Second, the scanning region should be limited to a smaller area. Third, measurements of radiation protection should be taken. Fourth, with the advancement of the CT scanning hardware and the reconstruction algorithm, the dosage of radiation in abdominal CT scan has been significantly reduced. Finally, MRI could be the substitute of CT with a standardization technique to minimize the inter-subject and intra- and inter-scanner variations for the same tissue after image acquisition [18].
There were several limitations in this study. First, CT scan was used in this study to measure the abdominal fat content; radiation exposure was inevitable to the study subjects. However, as the CT data used in the current study were all obtained from the QCT data of an ongoing spine and knee degeneration study, no extra radiation was involved. Second, the subjects were initially recruited not for fat measurements. Third, the software did not exclude the bowel contents from the VAT measurement; this might cause an over-estimation of VAT values. However, considering the small amount of bowel contents compared to the large total VAT volume, the influence might be neglected. Fourth, handling nonlinearity model properly may be even more important for Asian people, considered the diversity of their stature and fat distribution related to different nations and races. However, scatter plots of VAT area-to-volume at the different levels (Supplementary Fig. S1) showed good linearity for the population in the present study. This may be related to the relatively small sample size, or the limited racial variability of our study. Finally, it should be noted that hypertension, diabetes, smoking, physical activity, and other factors are important covariates which may influence VAT and SAT distribution. In our study, hypertension was included and shown no significance in the model. More factors should be considered in the future research to evaluate their influence on VAT and SAT distribution.
In conclusion, the fat tissue could be accurately and reliably measured by using the QCT. Moreover, the VAT and SAT measured in a single slice (L2/L3 level) showed the strongest correlation with the total VAT and SAT volumes in this large sample of Chinese population. We therefore suggested that the L2/L3 level as the optimal anatomic site for abdominal fat measurement in future studies.
Supplementary Material
Acknowledgements
The foundation from the National Natural Science Found of China (No. 81401407), Beijing Bureau of Health 215 Program (No. 2009-2-03) and Capital Health Development Research Program (No. 2014-2-1122).
Footnotes
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of interest.
Electronic supplementary material The online version of this article (https://doi.org/10.1038/s41430-018-0122-1) contains supplementary material, which is available to authorized users.
References
- 1.Tchernof A, Després J-P. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93:359–404. [DOI] [PubMed] [Google Scholar]
- 2.Irlbeck T, Massaro J, Bamberg F, O’Donnell C, Hoffmann U, Fox C. Association between single-slice measurements of visceral and abdominal subcutaneous adipose tissue with volumetric measurements: the Framingham Heart Study. Int J Obes. 2010;34:781–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang F, Wu S, Song Y, Tang X, Marshall R, Liang M, et al. Waist circumference, body mass index and waist to hip ratio for prediction of the metabolic syndrome in Chinese. Nutr Metab Cardiovas. 2009;19:542–7. [DOI] [PubMed] [Google Scholar]
- 4.Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. Visceral adipose tissue: relations between single-slice areas and total volume. Am J Clin Nutr. 2004;80:271–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oda E New criteria for ‘obesity disease’ in Japan. Circ J. 2006;70:150. [DOI] [PubMed] [Google Scholar]
- 6.Sottier D, petit JM, Guiu S, Hamza S, Benhanmiche H, Hillon P, et al. Quantification of the visceral and subcutaneous fat by computed tomography: interobserver correlation of a single slice technique. Diagn Interv Imaging. 2013;94:879–84. [DOI] [PubMed] [Google Scholar]
- 7.Wang L, Wang W, Xu L, Cheng X, Ma Y, Liu D, et al. Relation of visceral and subcutaneous adipose tissue to bone mineral density in Chinese women. Int J Endocrinol. 2013;2013:378632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuk J, Church T, Blair SN, Ross R. Does measurement site for visceral and abdominal subcutaneousadipos tissue alter association with the metabolic syndrome? Diabetes Care. 2006;29:679–84. [DOI] [PubMed] [Google Scholar]
- 9.Maislin G, Ahmed MM, Gooneratne N, Thorne-Fitzgerald M, Kim C, Teff K, et al. Single slice vs. volumetric mr assessment of visceral adipose tissue—reliability and validity among the overweight and obese. Obesity. 2012;20:2124–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, Ross R, et al. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am J Clin Nutr. 2012;96:714–26. [DOI] [PubMed] [Google Scholar]
- 11.Udupa JK, LeBlanc VR, Zhuge Y, Imielinska C, Schmidt H, Currie LM, et al. A framework for evaluating image segmentation algorithms. Comput Med Imaging Graph. 2006;30:75–87. [DOI] [PubMed] [Google Scholar]
- 12.Steiger JH. Tests for comparing elements of a correlation matrix. Psychol Bull. 1980;87:245–61. [Google Scholar]
- 13.Ryo M, Kishida K, Nakamura T, Yoshizumi T, Funahashi T, Shimomura I. Clinical significance of visceral adiposity assessed by computed tomography: a Japanese perspective. World J Radiol. 2014;6:409–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jia WP, Lu JX, Xiang KS, Bao YQ, Lu HJ, Chen L. Prediction of abdominal visceral obesity from body mass index, waist circumference and waist-hip ratio in Chinese adults: receiver operating characteristic curves analysis. Biomed Environ Sci. 2003;16:206–11. [PubMed] [Google Scholar]
- 15.Demerath EW, Shen W, Lee M, Choh AC, Czerwinski SA, Siervogel RM, et al. Approximation of total visceral adipose tissue with a single magnetic resonance image. Am J Clin Nutr. 2007;85:362–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schweitzer L, Geisler C, Pourhassan M, Braun W, Glüer CC, Bosy-Westphal A, et al. What is the best reference site for a single MRI slice to assess whole-body skeletal muscle and adipose tissue volumes in healthy adults? Am J Clin Nutr. 2015;102:58–65. [DOI] [PubMed] [Google Scholar]
- 17.Tong Y, Udupa JK, Torigian DA. Optimization of abdominal fat quantification on CT imaging through use of standardized anatomic space: a novel approach. Med Phys. 2014;41:063501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Udupa JK, Odhner D, Zao L, Tong Y, Matsumoto MMS, Ciesielski KC, et al. Body-wide hierarchical fuzzy modeling, recognition, and delineation of anatomy in medical images. Med Image Anal. 2014;18:752–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.