Abstract
Background and Aim
There is a need to improve utilization of cessation assistance in low- and middle-income countries (LMICs), and tobacco cessation research has been identified as priority in LMICs. This study evaluates the relationship between health care provider intervention and cessation assistance utilization in LMICs.
Methods
Data from 13 967 participants (aged ≥15 years, 90.3% males) of the Global Adults Tobacco Survey conducted in 12 LMICs (74.3%–97.3% response rates) were analyzed with utilization of counseling/cessation clinic, WHO-recommended medications, and quitline as outcome variables. Health care provider intervention (“no intervention,” only “tobacco screening,” “quit advice”) was the exposure variable. Weighted multiple logistic regression models were used to examine the relationship between each outcome variable and the exposure variable, adjusting for other covariates. Adjusted odds ratios (ORs) with 95% confidence intervals (CIs) are reported.
Results
Approximately 52%, 8%, and 40% of participants received no intervention, only tobacco screening, and advice to quit, respectively. Overall, 0.4%, 1.9%, 3.0%, and 4.5% used quitline, WHO-recommended medications, counseling/cessation clinic, and any cessation assistance, respectively. Compared with no intervention, quit advice was associated with increased utilization of quitline (OR = 2.24, 95% CI = 1.2 to 4.4), WHO-recommended medications (OR = 1.67, 95% CI = 1.2 to 2.3), counseling/cessation clinic (OR = 4.41, 95% CI = 3.2 to 6.1), and any assistance (any of the three types) (OR = 2.80, 95% CI = 2.2 to 3.6).
Conclusion
The findings of this study suggest that the incorporation of quit advice by health care providers in tobacco control programs and health care systems in LMICs could potentially improve utilization of cessation assistance to improve smoking cessation in LMICs.
Implications
This first study of association between health care provider intervention and the utilization of cessation assistance in LMICs reports that there was a missed opportunity to provide quit advice to about 60% of smokers who visited a health care provider in the past year. The odds of utilization of counseling/cessation clinic, WHO-recommended medications, and quitline were significantly increased in participants who were advised to quit smoking. The results suggest that effective integration and implementation of advice to quit in tobacco control programs and the national health care systems may increase the use of cessation assistance to quit smoking.
Introduction
Tobacco smoking continues to be the leading preventable cause of deaths and contributes to over 1 trillion dollars in economic costs; yet, over 1 billion people aged 15 years and above continue to smoke worldwide.1 Of these worldwide smokers, over 80% currently reside in low- and middle-income countries (LMICs) and the increasing tobacco consumption threatens the health and lives of many people.2 Additionally, such a trend poses a major threat to sustainable economic development in light of the loss of potential years of productive life attributed to smoking,3 and direct and indirect medical cost due to smoking.1 Evidence indicates that half of persistent tobacco users die from the habit,4 and smokers on average die more than 10 years earlier than nonsmokers;5 hence, the critical need for smoking cessation services.
Smoking cessation is one of the pillars of a comprehensive tobacco control program, which can save the lives of millions of smokers in a few decades,1 and protect nonsmokers from the deleterious effects of secondhand tobacco smoke exposure.6 However, quit rates in LMICs are still low,7 and tobacco dependence treatment and cessation research have been identified as a priority in these countries.8 Therefore, there is a gap in the literature to understand factors that promote tobacco cessation in LMICs, including the role of health care providers. The Global Adult Tobacco Survey (GATS) has been implemented as a standard tool for monitoring tobacco control8 in countries with high smoking prevalence, which provides opportunity to understand tobacco dependence treatment in LMICs. This study aimed to fill a research gap by using GATS to estimate the relationship between health care provider intervention and utilization of cessation assistance in LMICs.
There is a critical need for cessation assistance in LMICs because the addictive nature of tobacco smoking makes it difficult for smokers to quit.9 Although a significant number of smokers quit unaided or “cold turkey,”10 there are many who will require assistance to successfully give up smoking due to nicotine and psychological addiction.9 Research suggests that cessation interventions such as counseling by the health care provider and the use of nicotine replacement therapy (NRT) are cost-effective,11,12 and they could help to control tobacco smoking in LMICs, if they are readily available and acceptable to the population. However, the rates of utilization of cessation assistance are low in LMICs (from 4% in Ukraine to 27% in Vietnam).13 Thus, increased utilization of cessation assistance is needed to increase cessation rates14 and curtail the increasing trend of tobacco use in LMICs.
Health care professionals play crucial roles in tobacco cessation interventions. The clinical setting provides a direct opportunity where physicians can counsel and support tobacco users to quit.15 Evidence indicates that a brief clinician intervention can increase tobacco cessation and that there is a dose–response relationship between the intensity of the clinician intervention and tobacco cessation.16 In a systematic review involving 17 randomized control trials, it was found that smokers who received physician quit advice had 66% greater chance of smoking cessation than those who did not.17 For this reason, the WHO Framework Convention for Tobacco Control (WHO FCTC), the first international treaty for tobacco control,18 has recognized the significant role of health care professionals by encouraging routine tobacco screening and advice to quit smoking by these professionals.2
Although almost all LMICs have signed and ratified the WHO FCTC, the development of policies and programs to address tobacco smoking is slow,19,20 and tobacco dependence treatment is low in LMICs.21 Several sociodemographic and economic factors22–24 increase the utilization of cessation assistance among smokers; however, there is a scarcity of research on the extent to which health care provider advice to quit is associated with utilization of cessation assistance in LMICs. Thus, this study assessed associations between health care provider interventions and utilization of cessation assistance in 12 tobacco high-burdened LMICs. The study results will serve as evidence to inform efforts to incorporate the role of health care providers in tobacco control programs and to strengthen health care provider tobacco use screening and advice to quit smoking in health care systems of LMICs.
Methods
Participants and Procedure
GATS data from 2009 to 2013 were utilized for this study. GATS is a component of the Global Tobacco Surveillance System (GTSS), which aims at helping countries to monitor key indicators of tobacco use and control programs. Details of the survey have been published elsewhere.25,26 Briefly, it is a multistage area clustered-probability sampling of civilian noninstitutionalized adults aged 15 years and older in each participating country. Firstly, countries are divided into sampling units in proportion to size, based on a recent census data and/or administrative records. Households are then sampled, and one adult is randomly selected from eligible adults in each household to answer survey questions. The survey is designed to obtain nationally representative data. The use of standardized study protocol allows for cross-country comparisons of the core tobacco control indicators and pooled data analysis.
Publicly available GATS data from 18 LMICs were retrieved for the present study. Countries were included if they asked questions about all the three types of the cessation assistance considered in this study and there was at least one positive response on usage of each assistance types or the WHO implementation reports indicate availability of the cessation services in the country at the time of the survey. Twelve countries meeting the above criteria (Bangladesh [2009], Egypt [2009], Mexico [2009], China [2010], India [2010], Vietnam [2010], Malaysia [2011], Romania [2011], Thailand [2011], Argentina [2012], Turkey [2012], and Panama [2013]) were included in the study and six countries that did not meet the criteria (Cameroon, Indonesia, Nigeria, Philippines, Uganda, and Ukraine) were excluded from the study. The overall response rates ranged from 74.3% in Argentina to 97.3% in Egypt (Table 1).
Table 1.
Characteristics and proportions of health care provider intervention in study participants (N = 13 967)
| Country | Year of survey | Overall response rate (%) | Sample sizea | Female (W%) | Male (W%) | 15–24 years (W%) | 25–44 years (W%) | 45–64 years (W%) | 65+ years (W%) | No intervention (W%) | Tobacco screening (W%) | Advice to quit (W%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Argentina | 2012 | 74.3 | 747 | 41.7 | 58.3 | 21.3 | 35.5 | 34.3 | 8.9 | 19.8 | 19.7 | 60.6 |
| Bangladesh | 2009 | 93.6 | 836 | 2.0 | 98.0 | 13.8 | 47.9 | 28.6 | 9.7 | 44.3 | 3.1 | 51.6 |
| China | 2010 | 96 | 1453 | 5.9 | 94.1 | 9.6 | 36.9 | 37.5 | 16.0 | 59.5 | 6.9 | 33.6 |
| Egypt | 2009 | 97.3 | 956 | 3.2 | 96.8 | 12.7 | 44.1 | 33.5 | 9.8 | 26.0 | 7.1 | 66.9 |
| India | 2010 | 91.8 | 4944 | 11.4 | 88.6 | 11.5 | 41.1 | 36.1 | 11.3 | 46.5 | 6.7 | 46.8 |
| Malaysia | 2011 | 85.3 | 301 | 2.8 | 97.2 | 16.8 | 48.5 | 28.5 | 6.2 | 33.3 | 15.2 | 53.4 |
| Mexico | 2009 | 82.5 | 483 | 32.5 | 67.5 | 38.8 | 41.7 | 20.8 | 6.7 | 36.6 | 44.4 | 19.0 |
| Panama | 2013 | 88.4 | 297 | 28.1 | 71.9 | 13.9 | 34.5 | 36.7 | 14.8 | 31.4 | 14.3 | 54.3 |
| Romania | 2011 | 88.5 | 561 | 39.2 | 60.8 | 12.5 | 47.7 | 32.9 | 6.8 | 17.8 | 14.7 | 67.5 |
| Thailand | 2011 | 94.2 | 1604 | 8.5 | 91.5 | 14.8 | 34.6 | 38.6 | 12.0 | 34.7 | 9.5 | 55.9 |
| Turkey | 2012 | 90.1 | 1071 | 31.7 | 68.3 | 13.2 | 55.8 | 26.8 | 4.3 | 48.6 | 8.5 | 42.9 |
| Vietnam | 2010 | 92.8 | 714 | 4.1 | 95.9 | 14.3 | 44.7 | 30.6 | 10.4 | 65.3 | 5.0 | 26.7 |
| Total | 2009–2013 | 13 967 | 9.7 | 90.3 | 11.4 | 39.8 | 35.7 | 13.1 | 51.9 | 7.8 | 40.4 |
W% = weighted percentage.
Data source: GATS 2009–2013.
aParticipants included in this study.
The eligible participants comprised current smokers, and transitioning smokers (former smokers who had quit for less than 12 months) who visited a health-care provider in the past year. A total of 38 898 current or transitioning smokers participated in the survey, and 14 286 (36.7%) of them indicated that they visited health care providers in the past year. Of these 14 286 eligible participants, 319 (2.2%) had missing data points and were excluded from the analysis. Thus, the analytic sample for this study comprised 94.7% (13 215/13 967) current smokers and 5.3% (752/13 967) transitioning smokers aged 15 years and above.
Measures
Outcome Variables
The outcome variables were the utilization of three recommended cessation assistance: (1) counseling/cessation clinic, (2) WHO-recommended medications (eg, bupropion, nicotine patch, nicotine gum, etc)27, and (3) quitline in the past year. A fourth outcome variable was created as “any cessation assistance,” defined as a report of utilization of any of the three types of cessation assistance. Utilization of cessation assistance was assessed with the question “During the past 12 months, did you use any of the following to try to stop tobacco smoking?” Responses were coded as 1 = yes and 0 = no.
Exposure Variable
The exposure variable was health care provider behavioral intervention, categorized into “no intervention,” “only tobacco screening,” and “advice to quit smoking. ” Current smokers and transitioning smokers were asked whether they visited any health care provider in the past year (yes/no). Those who answered in affirmative were further asked, “During any visit to a doctor or health-care provider in the past 12 months, were you asked if you smoke tobacco?” (yes/no). Those who answered “yes” were further asked, “During any visit to a doctor or health-care provider in the past 12 months, were you advised to quit smoking tobacco?” (yes/no). If a doctor or health care provider did not ask about tobacco smoking, it was classified as “no intervention.” If a doctor or health care provider asked about smoking status but did not offer quit advice, it was categorized as “only tobacco screening,”28 and if a doctor or health care provider asked about smoking status and also advised to quit smoking, it was considered to be “advice to quit smoking.”
Covariates
Based on the literature22–24,29 and available information in the GATS data, sex, age, education level, exposure to health warnings on cigarette packages, knowledge about smoking harm, home smoking rules, and exposure to anti-smoking media messages were included as covariates. Age was categorized as 15–24, 25–44, 45–64, and 65+ years old as recommended by the GATS Collaborative Group.30 Education level was categorized into below high school, high school, and above high school education. Exposure to health warnings on cigarette packages was assessed with the question, “In the last 30 days, did you notice any health warnings on cigarette packages?” (yes/no). Exposure to anti-smoking media messages was assessed by the question, “In the last 30 days, have you noticed information about the dangers of smoking cigarettes or that encourages quitting in any of the following places?” (Newspapers or magazines, television, radio, and billboards). The exposure to anti-smoking media messages was categorized as “no exposure,” “exposure in only one media channel,” and “exposure in more than one media channel” to be consistent with literature.28 Home smoking rules were classified into “smoking allowed” (participants reported that there were no rules or smoking was allowed at home), “smoking restriction” (smoking generally not allowed but with exception), and “smoke-free” (smoking completely not allowed at home).
Because availability of affordable cessation services can influence the use of these services, information in the WHO FCTC implementation reports31,32 was utilized to create a dummy variable, “National cessation service availability and affordability,” and included in the model as a covariate. The variable classified the countries in the study into three groups according to the availability of the services: (1) NRT and/or some cessation services (none of them is cost-covered; Bangladesh, China, India, Egypt, and Vietnam); (2) NRT and/or some cessation services with at least one cost-covered (Argentina, Malaysia, Mexico, and Thailand); and (3) National quitline and both NRT and some cessation services cost-covered (Panama, Romania, and Turkey).
Statistical Analysis
Data management and analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC). Sampling weights, accounting for sampling effects and nonresponses, were used in each analysis to ensure that the estimates would be generalizable. Similar to previous studies,33,34 a country dummy variable (country of survey) was included in all analyses to adjust for countries’ sociocultural, environmental and population differences, and variance estimations accounted for the stratified and clustered sampling design. Descriptive analysis was conducted to estimate the proportions of each outcome in the categories of the exposure variable and covariates.
Four multiple logistic regression models were fitted to examine the relationship between health care provider behavioral intervention and each of the four outcome variables (counseling/cessation clinic, quitline/telephone support, WHO-recommended medications, and any cessation assistance). Model diagnostics were evaluated for each model, and no significant violations of the assumptions of the logistic regression model were found; the sample size was large enough, no multicollinearity, no influential data points, and model fits were adequate. Because both advice to quit smoking and anti-smoking media messages offer direct communication and encouragement to quit smoking, interaction between health care provider intervention and exposure to anti-smoking media messages was tested in each model. The interaction term was excluded from the final models because it did not improve any of the four models. The significance of all analyses was set a priori at p-value of .05. Odds ratios (ORs) and associated 95% confidence intervals (CIs) are reported.
Results
Sample Characteristics and Prevalence of Health Care Provider Intervention and Utilization of Cessation Assistance
Table 1 shows the characteristics of the study participants and prevalence of health care provider intervention. Of the 13 967 total participants included, 90.3% were males, more than half (51%) were under the age of 45 years, and 13% were ≥65 years old. Overall, 51.9%, 7.8%, and 40.4% of participants received no intervention, only tobacco screening, and advice to quit, respectively. Among current smokers, 51.9%, 7.9%, and 40.2% received no intervention, only tobacco screening, and advice to quit, respectively, compared with 50.8%, 4.9%, and 44.3% of transitioning smokers who received no intervention, only tobacco screening, and advice to quit, respectively. While the proportion of participants who received only tobacco screening ranged from 3.1% in Bangladesh to 44.4% in Mexico, those who received advice to quit ranged from 19.0% in Mexico to 67.5% in Romania.
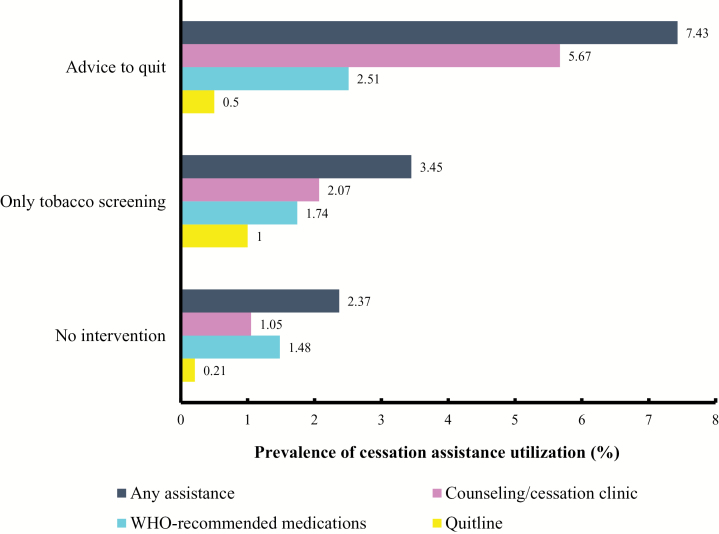
Table 2 illustrates cessation assistance utilization by covariates. Prevalence of cessation assistance utilization in the pooled data was 0.4%, 1.9%, 3.0%, and 4.5% for quitline, WHO-recommended medications, counseling/cessation clinic, and any cessation assistance, respectively. Utilization of any cessation assistance was higher in transitioning smokers (9.2%) than current smokers (4.2%). Overall, 3.8%, 0.5%, and 0.2% of the participants used only one type, two types, and all the three types of cessation assistance, respectively. Figure 1 shows prevalence of cessation assistance utilization by health care provider intervention. Prevalence of any cessation assistance utilization was 2.4%, 3.5%, and 7.4% in participants who received no intervention, only tobacco screening, and advice to quit, respectively. In all cessation assistance types, prevalence of utilization was highest in those who received advice to quit, except quitline, where the utilization was highest among those who received only tobacco screening (Figure 1).
Table 2.
Prevalence of cessation assistance utilization in the categories of covariates (N = 13 967)
| Variable | Quitline or telephone W% (95% CI) | WHO-recommended medications W% (95% CI) | Counseling/cessation clinic W% (95% CI) | Any cessation assistance W% (95% CI) |
|---|---|---|---|---|
| Sex | ||||
| Female | 0.4 (0.1–0.6) | 2.8 (1.7–3.9) | 3.4 (1.8–5.0) | 5.4 (3.6–7.2) |
| Male | 0.4 (0.2–0.6) | 1.8 (1.4–2.2) | 3.0 (2.4–3.5) | 4.4 (3.7–5.1) |
| Age | ||||
| 15–24 years | 0.7 (0.0–1.6) | 2.1 (1.2–3.1) | 2.7 (1.4–4.1) | 4.4 (2.7–6.0) |
| 25–44 years | 0.4 (0.2–0.6) | 2.6 (1.8–3.3) | 3.0 (2.3–3.7) | 5.1 (4.0–6.1) |
| 45–64 years | 0.4 (0.1–0.6) | 1.5 (1.1–2.0) | 3.0 (2.3–3.7) | 4.1 (3.3–5.0) |
| 65+ years | 0.1 (0.0–0.2) | 0.8 (0.4–1.3) | 3.3 (2.1–4.5) | 3.9 (2.6–5.2) |
| Education | ||||
| Below high school | 0.4 (0.2–0.7) | 2.0 (1.5–2.4) | 4.1 (3.3–4.9) | 5.6 (4.7–6.5) |
| High school | 0.2 (0.1–0.3) | 1.3 (0.8–1.8) | 1.0 (0.6–1.4) | 2.0 (1.3–2.6) |
| Above high school | 0.8 (0.2–1.2) | 3.7 (2.0–5.3) | 3.0 (1.8–4.1) | 6.0 (4.0–8.1) |
| Seen warning label | ||||
| No | 0.7 (0.1–1.3) | 1.6 (0.9–2.3) | 3.9 (2.6–5.3) | 4.8 (3.4–6.3) |
| Yes | 0.3 (0.2–0.4) | 2.0 (1.6–2.4) | 2.8 (2.3–3.3) | 4.4 (3.7–5.1) |
| Know smoking harm | ||||
| No | 0.3 (0.0–0.6) | 1.3 (0.04–2.6) | 0.8 (0.3–1.4) | 1.8 (0.5–3.2) |
| Yes | 0.4 (0.2–0.6) | 2.0 (1.6–2.4) | 3.4 (2.8–4.0) | 5.0 (4.2–5.7) |
| Home smoking rule | ||||
| Allowed | 0.1 (0.1–0.2) | 1.4 (1.0–1.8) | 1.9 (1.5–2.4) | 3.2 (2.5–3.8) |
| Restriction | 1.3 (0.3–2.3) | 2.9 (1.9–3.9) | 5.7 (3.8–7.5) | 7.7 (5.5–9.9) |
| Smoke free | 1.1 (0.5–1.7) | 4.3 (3.2–5.5) | 7.2 (5.5–9.0) | 10.0 (8.1–11.9) |
| Exposure to anti-smoking media message | ||||
| No exposure | 0.1 (0.0–0.2) | 0.6 (0.3–0.9) | 2.5 (1.8–3.2) | 2.9 (2.1–3.7) |
| Exposure in one channel | 0.6 (0.1–1.0) | 2.2 (1.3–3.0) | 2.6 (1.8–3.4) | 4.4 (3.2–5.6) |
| Exposure in more than one channel | 0.6 (0.3–0.9) | 3.4 (2.6–4.2) | 4.0 (3.1–4.9) | 6.7 (5.4–7.9) |
| Overall | 0.4 (0.2–0.5) | 1.9 (1.5–2.3) | 3.0 (2.5–3.5) | 4.5 (3.8–5.2) |
CI = confidence intervals; W% = weighted prevalence.
Estimates were adjusted for country of survey, sample weight, and clustering and stratification of the sampling design. “Any assistance” means utilization of any of the three recommended cessation aids.
Data source: GATS 2009–2013.
Figure 1.
Health care provider intervention and cessation assistance utilization (N = 13 967).
Relationship Between Health Care Provider Intervention and Utilization of Cessation Assistance
Table 3 shows the results of the multiple logistic regression analyses for the relationship between health care provider intervention and utilization of cessation assistance. The odds of quitline utilization in participants who were advised to quit were significantly more than two times the odds of those who received no intervention (OR = 2.24, 95% CI = 1.2 to 4.4). Odds of WHO-recommended medications utilization was 67% (OR = 1.67, 95% CI = 1.2 to 2.3) higher in those who received advice to quit than those who received no intervention. Compared with no intervention, odds of utilization of counseling/cessation clinic were significantly increased in those who were advised to quit (OR = 4.41, 95% CI = 3.2 to 6.1). For those who received advice to quit smoking, there was approximately twofold significant increase in the odds of any cessation assistance utilization compared with those who received no intervention (OR = 2.80, 95% CI = 2.2 to 3.6).
Table 3.
Relationship between health care provider behavioral intervention and utilization of cessation assistance (N = 13 967)
| Quitline or telephone | WHO-recommended medications | Counseling/cessation clinic | Cessation assistance | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Health provider intervention | ||||||||
| No intervention | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Only tobacco screening | 4.20* | 1.2–14.8 | 0.92 | 0.5–1.6 | 2.06 | 0.9–4.6 | 1.33 | 0.7–2.4 |
| Advice to quit | 2.24* | 1.2–4.4 | 1.67** | 1.2–2.3 | 4.41*** | 3.2–6.1 | 2.80*** | 2.2–3.6 |
| Gender | ||||||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Male | 1.76 | 0.8–4.0 | 0.87 | 0.6–1.3 | 0.76 | 0.4–1.3 | 0.82 | 0.6–1.2 |
| Age | ||||||||
| 15–24 years | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 25–44 years | 0.72 | 0.2–2.1 | 1.31 | 0.8–2.2 | 0.93 | 0.6–1.6 | 1.10 | 0.7–1.7 |
| 45–64 years | 0.70 | 0.2–2.2 | 0.86 | 0.5–1.5 | 0.98 | 0.6–1.7 | 0.97 | 0.6–1.5 |
| 65+ years | 0.19 | 0.03–1.1 | 0.53 | 0.3–1.1 | 1.27 | 0.7–2.4 | 1.08 | 0.7–1.8 |
| Education | ||||||||
| Below high school | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| High school | 0.83 | 0.3–2.1 | 0.93 | 0.5–1.7 | 0.81 | 0.5–1.3 | 0.82 | 0.5–1.2 |
| Above high school | 1.29 | 0.5–3.1 | 1.61 | 0.9–2.8 | 0.97 | 0.6–1.5 | 1.25 | 0.8–1.9 |
| Seen warning label | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.26** | 0.1–0.7 | 0.64 | 0.4–1.1 | 0.68 | 0.5–1.0 | 0.74 | 0.5–1.1 |
| Know smoking harm | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.38 | 0.1–1.7 | 0.56 | 0.2–1.5 | 1.77 | 0.9–3.5 | 1.15 | 0.5–2.5 |
| Home smoking rule | ||||||||
| Allowed | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Restriction | 6.50*** | 2.7–15.9 | 1.40 | 0.9–2.1 | 2.37*** | 1.7–3.4 | 1.83*** | 1.4–2.5 |
| Smoke free | 3.97* | 1.3–12.0 | 1.65* | 1.1–2.5 | 2.49*** | 1.8–3.5 | 1.93*** | 1.5–2.6 |
| Exposure to anti-smoking media message | ||||||||
| No exposure | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Exposure in one channel | 6.20** | 1.7–23.2 | 3.06** | 1.5–6.1 | 1.15 | 0.8–1.7 | 1.57* | 1.1–2.3 |
| Exposure in more than one channel | 5.28* | 1.3–21.0 | 3.42*** | 1.9–6.3 | 1.71** | 1.2–2.4 | 1.98*** | 1.4–2.7 |
| National cessation service availability and affordability | ||||||||
| NRT and/or some cessation services (none cost-covered) | 1.00 | 1.00 | ||||||
| NRT and/or some cessation services with at least one cost-covered | 1.10 | 0.3–4.1 | 0.21*** | 0.1–0.3 | 0.94 | 0.4–2.1 | 0.22 | 0.1–0.4 |
| National quit line, and both NRT and some cessation services cost-covered | 2.80 | 0.8–9.4 | 0.37*** | 0.2–0.6 | 1.38 | 0.6–2.9 | 0.43 | 0.3–0.6 |
*p < .05; **p < .01; ***p < .001.
CI = confidence interval; OR = adjusted odds ratio; NRT = nicotine replacement therapy.
Odds ratios were derived from weighted multiple logistic regression models. Estimates were adjusted for country of survey, and variance estimation accounted for the clustered and stratified sampling design.
Data source: GATS 2009–2013.
In addition to health care provider intervention, living in smoke-free homes and exposure to anti-smoking media messages in more than one media channel were associated with significantly increased odds of utilization of all the three types of cessation assistance considered in this study (Table 3).
Discussion
Strong evidence exists about the health and economic benefits of tobacco smoking cessation.5,14 Cessation can save millions of lives and prevent premature deaths.35 However, tobacco smoking prevalence is still high in some LMICs2 and increasing in many other.36,37 Although tobacco smoking cessation can help to reverse the rising trend of smoking prevalence in LMICs, utilization of evidenced-based cessation assistance remains low in LMICs,13 despite the availability.16 Thus, this study was conducted to examine the relationship between health care provider cessation intervention and the utilization of cessation assistance in LMICs in order to help identify ways of improving utilization of cessation assistance for tobacco smoking cessation.
Overall, more than half of the participants (51%) were neither screened for tobacco smoking nor advised to quit upon seeing a health care provider, and about 8% were asked about their smoking status but not advised to quit smoking in the past year (Table 1). In all types of cessation assistance used, the proportion of usage was highest among participants who received advice to quit, except for quitline utilization in which the highest proportion was seen in those who were only screened for tobacco use. Research suggests that health care provider intervention such as screening or quit advice increases patients’ satisfaction with care,16 and satisfaction with care is associated with increased utilization of health care services.38,39 Thus, these results reinforce the added benefit of tobacco screening and/or quit advice in comprehensive tobacco control programs.
Although utilization of all the three types of cessation assistance was low, quitline, which has been found to be effective in tobacco cessation in high-income countries40 and cost-effective in resource-limited countries,41 was the least utilized cessation assistance by the study participants. This low report of the utilization of quitline may not be due to the absence or accessibility to such services in LMICs. Indeed, at the time of survey, 25% of the countries in the present study had a national tobacco quitline. The odds of quitline utilization among participants from these countries were, however, not significantly different from countries without a national quitline or cost-covered cessation services. With the rise in access to telecommunication in LMICs, it has been expected that quitline could be used to offer cessation counseling in LMICs where resources to provide cessation medications may be limited,41 and there have been calls for studies to evaluate the effectiveness of quitline40 and ways by which the use of quitline can be improved in LMICs.41 The low utilization of quitline observed in this study reinforces the need for scientific investigations into and efforts to increase utilization of telephone-based cessation counseling in LMICs. Despite the low utilization of quitline in this study, it was found that participants who received quit advice were more likely to use quitline. Therefore, the findings in the present study suggest that effective implementation of tobacco screening and advice to quit in the national health care system may be one of the ways by which the use of quitline services can be improved.
Health care provider behavioral intervention has been found to increase the chances of quitting smoking14 and improve the effectiveness of NRT.42 It is an effective but inexpensive tobacco use intervention, which can easily be integrated into the health care system,15 and best practices have been developed to guide the implementation of this intervention.16,43 However, our results show that only 40% of smokers who visited health care providers were advised to quit, although there were between-country variabilities in the rates. This indicates a missed opportunity to encourage quitting in 60% of these smokers and highlights the need to improve tobacco screening and advice to quit in the primary health care system in the studied countries. Health care provider capacity building and reduction in the prevalence of smoking among health care providers in LMICs can increase tobacco screening and advice to quit in these countries.44
The WHO FCTC Article 14 requires integration of tobacco dependence treatment into the health care system and emphasizes health care provider tobacco screening and advice to quit,45 and the current implementation report shows that only two of the 12 countries (Bangladesh and Vietnam) in the present study have not made any progress from having only some cessation services with none cost-covered.46 As of December 31, 2016, 33% of the countries (4/12) in the present study had implemented tobacco dependence treatment policy that provides a national quitline plus both NRT and some cessation services cost-covered to the population.46 India, Mexico, Panama, and Turkey are at the best practice level—presence of a National quit line, and both NRT and some cessation services cost-covered—with its tobacco use cessation services; whereas Argentina, China, Egypt, Malaysia, Romania, and Thailand on the other hand are at a second-best level with the presence of NRT and/or some cessation services (at least one of which is cost-covered).46 While this progress is positive to tobacco control in these countries, our results suggest that the implementation of these policies alone may not improve utilization of cessation assistance and that other factors, such as health care provider tobacco screening and advice to quit may play a critical role in the use of cessation assistance to quit tobacco use. In the current study, there was no evidence that availability of countrywide cost-covered cessation services increased utilization of quitline or counseling/cessation clinics to quit smoking but was associated with decreased odds of utilization of WHO-recommended medications. However, advice to quit was associated with increased utilization of all the three cessation assistant types. Although longitudinal studies are required to establish causation, our findings suggest that a full implementation of health care provider intervention in LMICs could promote tobacco use cessation. However, as a small proportion of current smokers in LMICs (21.6% to 55.8%) reported seeing a health care provider in the past 12 months,47 it is important to also implement other tobacco control policies that encourage utilization of cessation assistance.
The results of the present study support the evidence that components in comprehensive control programs can complement one another.48 In all types of cessation assistance, odds of utilization were significantly increased in participants who reported exposure to anti-smoking messages in the media, especially those who reported exposure to these messages from more than one media channel, although there was no significant interaction between health care provider intervention and exposure to anti-smoking messages in the media. Additionally, those who reported living in homes with either smoking restriction or complete smoke-free rules were more likely to have used assistance to attempt to quit smoking (Table 3). Both home smoking rules and anti-smoking messages were associated with utilization of any cessation assistance. These findings reflect the importance of comprehensive tobacco control programs in LMICs, in which cessation assistance is readily available, accessible, and affordable to those who require help to quit smoking.
The study has some limitations that must be considered in the interpretation of the results. First, all variables were measured by self-report and therefore prone to recall bias or social desirability bias. Second, being a cross-sectional study, temporality cannot be established; hence, the need for longitudinal studies. It may happen that cessation assistance was utilized before visiting health care provider and vice versa; however, we strongly believe that health care providers would not selectively screen or offer advice to quit to those who had utilized cessation assistance in the past year. Also, the utilization of quitline was low, so the analysis may be underpowered. Correcting this limitation by increasing the sample in this category in future studies will strengthen the results found in this study. Despite these limitations, the results can be generalized to more than half of smokers in LMICs because the study uses representative data from 12 countries that account for more than half of the adult tobacco smokers in LMICs.1 Additionally, the robustness of our analysis has helped to minimize the chances of errors in the findings.
Conclusion
Health care provider intervention (advice to quit) was significantly associated with increased utilization of all three types of cessation assistance considered in this study: counseling/cessation clinic, WHO-recommended medications, and quitline. Additionally, home smoking rules (restriction and smoke-free) and exposure to anti-smoking messages were associated with increased utilization of cessation assistance. These findings suggest that quit advice by health care providers should be incorporated into comprehensive tobacco control programs and integrated into the health care system as part of routine health care procedure for all care seekers in LMICs.
Funding
This work was supported in part by the National Cancer Institute of the National Institutes of Health and the Food and Drug Administration (FDA), Center for Tobacco Products (R00CA187460), and the National Institute on Drug Abuse and FDA Center for Tobacco Products (P50DA036128). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Declaration of Interests
None declared.
Acknowledgments
We would like to thank the National Cancer Institute of the National Institutes of Health, the Center for Tobacco Products of Food and Drug Administration, and the National Institutes of Health for their financial support. We would also like to thank the College of Public Health, East Tennessee State University (ETSU), and the School of Public Health, Georgia State University for logistical support.
References
- 1. U.S. NCI and WHO. The Economics of Tobacco and Tobacco Control. National Cancer Institute Tobacco Control Monograph 21. NIH Publication No. 16-CA-8029A. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; and Geneva, CH: World Health Organization; 2016. [Google Scholar]
- 2. WHO. WHO Report on the Global Tobacco Epdemic: The MPOWER Package. Geneva: World Health Organization; 2008. http://whqlibdoc.who.int/publications/2008/9789241596282_jpn.pdf. Accessed February 23, 2018. [Google Scholar]
- 3. Yang MC, Fann CY, Wen CP, Cheng TY. Smoking attributable medical expenditures, years of potential life lost, and the cost of premature death in Taiwan. Tob Control. 2005;14(Suppl 1):i62–i70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ. 1994;309(6959):901–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. [DOI] [PubMed] [Google Scholar]
- 6. WHO. WHO Report on the Global Tobacco Epidemic, 2009: Implementing Smoke-Free Environments. World Health Organization: Geneva; 2009. [Google Scholar]
- 7. Storr CL, Cheng H, Alonso J, et al. Smoking estimates from around the world: data from the first 17 participating countries in the World Mental Health Survey Consortium. Tob Control. 2010;19(1):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McRobbie H, Raw M, Chan S. Research priorities for Article 14—demand reduction measures concerning tobacco dependence and cessation. Nicotine Tob Res. 2013;15(4):805–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. USDHHS. The Health Consequences of Smoking: Nicotine Addiction: A Report of the Surgeon General. Atlanta, GA: US Government Printing Office; 1988. [Google Scholar]
- 10. Leung CMK, Leung AKC, Hon KLE, Kong AYF. Fighting tobacco smoking—a difficult but not impossible battle. Int J Environ Res Public Health. 2009;6(1):69–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. USPSTF. Tobacco Use in Children and Adolescents: Primary Care Interventions https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/tobacco-use-in-children-and-adolescents-primary-care-interventions. Published 2013. Accessed June 5, 2017.
- 12. West R, Raw M, McNeill A, et al. Health-care interventions to promote and assist tobacco cessation: a review of efficacy, effectiveness and affordability for use in national guideline development. Addiction. 2015;110(9):1388–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang L, Jin Y, Lu B, Ferketich AK. A cross-country study of smoking cessation assistance utilization in 16 low and middle income countries: data from the global adult tobacco survey (2008–2012). Nicotine Tob Res. 2016;18(5):1076–1082. [DOI] [PubMed] [Google Scholar]
- 14. Fiore MC, Baker TB, Bailey WC, et al. A clinical practice guideline for treating tobacco use and dependence: 2008 update. Am J Prev Med. 2008;35(2):158–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lancaster T. The role of doctors in smoking cessation : evidence from the cochrane library. SA Heart. 2011;8(1):24–27. [Google Scholar]
- 16. Fiore MC, Jaén CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update—A clinical practice guideline. Diane Publishing: 2008. [Google Scholar]
- 17. Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane database Syst Rev. 2008;2. doi:10.1002/14651858.CD000165.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. WHO FCTC. Framework Convention on Tobacco Control (FCTC). Geneva; 2005. [Google Scholar]
- 19. WHO. 2014 Global Progress Report on the Implementation of the WHO Framework Convention on Tobacco Control. Geneva: World Health Organization; 2014. [Google Scholar]
- 20. WHO. 2016 Global Progress Report on Implementation of the WHO Framework Convention on Tobacco Control. Genevad: World Health Organization; 2016. [Google Scholar]
- 21. Mamudu H, Cairney P, Studlar D. Global public policy: does the new venue for transnational tobacco control challenge the old way of doing things?Public Adm. 2015;93(4):856–873. [Google Scholar]
- 22. Gollust SE, Schroeder SA, Warner KE. Helping smokers quit: understanding the barriers to utilization of smoking cessation services. Milbank Q. 2008;86(4):601–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lillard DR, Plassmann V, Kenkel D, Mathios A. Who kicks the habit and how they do it: socioeconomic differences across methods of quitting smoking in the USA. Soc Sci Med. 2007;64(12):2504–2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Myers MG, Strong DR, Linke SE, Hofstetter CR, Al-Delaimy WK. Predicting use of assistance when quitting: a longitudinal study of the role of quitting beliefs. Drug Alcohol Depend. 2015;149:220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. GATS Collaborative Group. Global Adult Tobacco Survey (GATS): Sample Design Manual, Version 2.0. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 26. Warren CW, Asma S, Lee J, Veronica L, Mackay J.. The Global Tobacco Surveillance System: The GTSS Atlas. Atlanta, GA: CDC Foundation and World Lung Foundation; 2009. [Google Scholar]
- 27. WHO. Tools for Advancing Tobacco Control in the XXIst Century: Policy Recommendations for Smoking Cessation and Treatment of Tobacco Dependence Tools for Public Health. Geneva: World Health Organization; 2003. http://www.who.int/tobacco/resources/publications/en/chapter5_to_annex2.pdf?ua=1. Accessed February 23, 2018. [Google Scholar]
- 28. CDC. Antismoking messages and intention to quit—17 Countries. MMWR Morb Mortal Wkly Rep. 2013;62(21):417–422. [PMC free article] [PubMed] [Google Scholar]
- 29. Gilbert H, Sutton S, Sutherland G. Who calls QUIT? The characteristics of smokers seeking advice via a telephone helpline compared with smokers attending a clinic and those in the general population. Public Health. 2005;119(10):933–939. [DOI] [PubMed] [Google Scholar]
- 30. Global Tobacco Surveillance System (GTSS). Global Adult Tobacco Survey (GATS): Indicator Guidelines. 2009. doi:10.1017/CBO9781107415324.004 [Google Scholar]
- 31. WHO. WHO Report on the Global Tobacco Epidemic: Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship. Geneva: World Health Organization; 2013. http://www.who.int/tobacco/global_report/2013/en/index.html. Accessed February 23, 2018. [Google Scholar]
- 32. WHO. WHO Report on the Global Tobacco Epidemic, 2011: Warning about the Dangers of Tobacco. Geneva: World Health Organization; 2011. http://whqlibdoc.who.int/publications/2011/9789240687813_eng.pdf. Accessed February 23, 2018. [Google Scholar]
- 33. Owusu D, Mamudu HM, John RM, Ibrahim A, Ouma AE, Veeranki SP. Never-smoking adolescents’ exposure to secondhand smoke in Africa. Am J Prev Med. 2016;51(6):983–998. [DOI] [PubMed] [Google Scholar]
- 34. Owusu D, Quinn M, Wang KS, Aibangbee J, Mamudu HM. Intentions to quit tobacco smoking in 14 low- and middle-income countries based on the transtheoretical model. Drug Alcohol Depend. 2017;178:425–429. [DOI] [PubMed] [Google Scholar]
- 35. Jha P, Chaloupka F.. Tobacco Control in Developing Countries. Oxford: Oxford University Press; 2000. [Google Scholar]
- 36. Bilano V, Gilmour S, Moffiet T, et al. Global trends and projections for tobacco use, 1990–2025: an analysis of smoking indicators from the WHO comprehensive information systems for tobacco control. Lancet. 2015;385(9972):966–976. [DOI] [PubMed] [Google Scholar]
- 37. Thun M, Peto R, Boreham J, Lopez AD. Stages of the cigarette epidemic on entering its second century. Tob Control. 2012;21(2):96–101. [DOI] [PubMed] [Google Scholar]
- 38. Fenton JJ. The cost of satisfaction. Arch Intern Med. 2012;172(5):405. [DOI] [PubMed] [Google Scholar]
- 39. Kruk ME, Rockers PC, Varpilah ST, Macauley R. Which doctor?: determinants of utilization of formal and informal health care in postconflict liberia. Med Care. 2011;49(6):585–591. [DOI] [PubMed] [Google Scholar]
- 40. Aquilino ML, Lowe JB. Approaches to tobacco control: the evidence base. Eur J Dent Educ. 2004;8(Suppl 45):11–17. [DOI] [PubMed] [Google Scholar]
- 41. Croyle RT. Increasing the effectiveness of tobacco quitlines. J Natl Cancer Inst. 2010;102(2):72–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Apollonio D, Glantz SA. Tobacco industry research on nicotine replacement therapy: “If anyone is going to take away our business it should be us.” Am J Public Health. 2017;107(10):1636–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. WHO. Code of practice on tobacco control for health professional organisations http://www.who.int/tobacco/communications/events/codeofpractice/en/. Accessed November 24, 2015.
- 44. Abdullah AS, Stillman FA, Yang L, Luo H, Zhang Z, Samet JM. Tobacco use and smoking cessation practices among physicians in developing countries: a literature review (1987–2010). Int J Environ Res Public Health. 2013;11(1):429–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. WHO FCTC/COP4(8). Guidelines for implementation of Article 14 of the WHO Framework Convention on Tobacco Control http://www.who.int/fctc/Guidelines.pdf?ua=1. Published 2010. Accessed January 5, 2016.
- 46. WHO. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 47. Centers for Disease Control and Prevention. Health-care provider screening for tobacco smoking and advice to quit—17 Countries, 2008–2011. Morb Mortal Wkly Rep. 2013;62(46):920–927. [PMC free article] [PubMed] [Google Scholar]
- 48. Centers for Disease Control and Prevention (CDC). Best Practices for Comprehensive Tobacco Control Programs. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]