“The only thing that is constant is change.”
—Greek Philosopher Heraclitus, c.535 – c.475 BCE
Consumer sleep technology (CST) is here to stay,1 but what does it mean for the sleep medicine community? The American Academy of Sleep Medicine's (AASM) recent formation of a Technology Presidential Committee and publication of a position statement on CSTs highlights the importance of this issue to our collective future.2 These actions demonstrate the AASM intends to shape this future rather than react to these imminent changes.
Sleep disorders and the importance of sleep health are under-recognized by primary care physicians and their patients. Conversations with primary care as part of the AASM and Sleep Research Societies' National Healthy Sleep Awareness Project3 to engage them more deeply in sleep medicine care was largely rebuffed, no doubt a result of minimal sleep medicine education in medical school curricula, internships, and residencies and an overburdened primary care workforce. No wonder 85% of people with sleep apnea go undiagnosed and untreated,4 > 30% of the adult population does not get the recommended 7 or more hours of sleep on a nightly basis,5,6 and access to cognitive behavioral therapy for insomnia (CBT-I) is so limited.7 Indeed, only 13% of those with insomnia ever consult a health care provider for this sleep problem.8
CSTs address these shortcomings by empowering those with sleep difficulties with objective data to better understand their sleep problem and provide physician reports to catalyze patient/provider interactions to address these sleep issues (Figure 1).9 These novel objective reports provide previously unobtainable longitudinal and ecologically valid sleep data. The resulting doctor-patient conversations will drive patients into sleep clinics for the care they need.
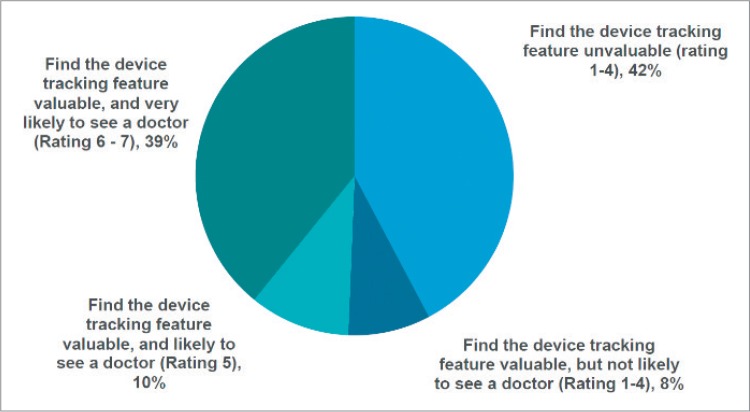
Figure 1. Likelihood of seeing a doctor due to sleep issues.
Likelihood of seeing a doctor due to sleep issues (eg, insomnia, sleep apnea, restless legs syndrome) detected by a consumer sleep technology device or application (n = 2,000; ± 2.19%).9
How do we deal with these increased referrals? With an approximate ratio of one board certified sleep physician for every 46,000 American citizens and vast swaths of the country devoid of sleep medicine expertise, it is clear we already have an access problem.10 The AASM is working to tackle this issue by growing sleep fellowship programs and exploring alternative pathways to board eligibility with the Accreditation Council for Graduate Medical Education through the Innovative Fellowship Model Implementation Presidential Committee.10 But even the best outcomes of these efforts will likely leave us with a shortage of sleep physicians. CSTs help this dilemma by steering people with sleep difficulties to solutions that optimize the sleep environment and facilitate proper sleep hygiene as first steps to address sub-optimal sleep. For example, CSTs can inform the consumer regarding habitual sleep duration and quality, the effect of alcohol, caffeine and nicotine on sleep, and aspects of the individual's sleep environment such as ambient temperature, sound, and light levels. Once this information is collected, some CSTs provide guidance for how to address these potentially problematic sleep issues and advance sleep health. Examples include referring individuals to digital CBT-I11,12 and/or home-based, timed, blue wavelength light suppressing technologies. Interventions such as these may obviate the need for specialist referral and deliver improved sleep health to a broader cross-section of society.
The AASM position statement on CSTs focuses on the need for FDA approval and rigorous validation against current gold standards. This position is appropriate if CSTs seek to advance beyond devices focused on general sleep health and well-being into the realm of screening, diagnosis and treatment of sleep disorders. The AASM sets the bar high and the CST community is taking responsibility as evidenced by the Consumer Technology Association implementing early standardization efforts focused on definitions and methodologies.13,14
The AASM focus on validation and FDA approval is aspirational and well-reasoned, yet it overlooks the complementary nature of CSTs and traditional sleep testing. CSTs assess aspects of a person's sleep life that heretofore were massive blind spots for the sleep medicine community. Polysomnography is a diagnostic test that measures sleep for one night, in a strange environment, in an obtrusive manner. But no two nights of sleep are exactly the same and inter-scorer agreement of polysomnography is just 83% highlighting the imperfection of PSG.15 Home sleep apnea tests are done in the person's typical sleep environment, but otherwise suffer from the same limitations as polysomnography. Actigraphy is an indirect measure of sleep that provides limited data and requires interaction with providers with sleep expertise for interpretation. Thus these traditional tests are far from an accurate representation of one's sleep life. Conversely, CSTs assess sleep longitudinally, in the typical sleep environment, with minimal obtrusiveness. Some devices even measure aspects of the sleep environment itself. Ultimately, CSTs and traditional objective sleep assessment tools are more complementary than competitive.
For decades, polysomnography has been used to diagnose sleep disorders, but do we need all of these data elements to make these diagnoses? Prior meetings and conferences by the AASM and others focused on our collective future have asked this question seeking to demonstrate how the massive amount of data collected by PSG can be utilized to provide additional diagnostic or therapeutic insights for providers and their patients. Yet, the success of home sleep apnea tests suggest patients, payers, and perhaps providers believe sleep diagnostic reductionism is the direction of the future. Years ago, pulse arterial tonometry for the diagnosis of sleep apnea was but a scientific concept, today we use this routinely to diagnose sleep apnea in the patient's home.16 This proved to the sleep medicine community that extensive traditional physiological measurements may not be required to accurately screen or diagnose sleep disorders. Indeed, CSTs that utilize heart rate and/or respiratory signals hold great promise for screening of sleep-disordered breathing and may support screening of other sleep disorders. Universal access to these technologies through smartphones could dramatically increase awareness of sleep disorders across the country. The technological advances represented by CSTs can only help as we seek less expensive, scalable, readily accessible sleep screening, diagnostic and treatment solutions of the future.
There exists substantial variability in the amount of validation of CSTs, yet the AASM position statement lumps these technologies together.2 If the sleep community wishes to promote validation, we must recognize those entities that both share and reject the AASM focus on validation.2 Specifying these differences will encourage entities allocating substantial resources to validation and challenge entities eschewing validation to either step up or fade away.
The possibilities of CSTs are many. By allowing people to objectify their sleep longitudinally CSTs empower the average individual to assess how their behavior impacts sleep quality. Extrapolate this to the clinical environment and these emerging technologies allow providers to assess the impact of their diagnoses and interventions on their patient's long term sleep health. In the end, greater insight into the effectiveness of our interventions through CSTs will make us better sleep providers by expanding our opportunities to understand our patient's habitual sleep patterns and problems. If Heraclitus is right when asserting “the only thing that is constant is change,” then the rise of CSTs is a change for the better.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. No financial support was provided for this manuscript. Dr. Watson is a member of the scientific advisory board of SleepScore Labs. Mr. Lawlor is Chief Executive Officer of SleepScore Labs. Dr. Raymann is Vice President of Sleep Science and Scientific Affairs for SleepScore Labs.
CITATION
Watson NF, Lawlor C, Raymann RJ. Will consumer sleep technologies change the way we practice sleep medicine? J Clin Sleep Med. 2019;15(1):159–161.
REFERENCES
- 1.Ko PR, Kientz JA, Choe EK, Kay M, Landis CA, Watson NF. Consumer sleep technologies: a review of the landscape. J Clin Sleep Med. 2015;11(12):1455–1461. doi: 10.5664/jcsm.5288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khosla S, Deak MC, Gault D, et al. Consumer sleep technology: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2018;14(5):877–880. doi: 10.5664/jcsm.7128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Healthy Sleep Awareness Project. Sleep Education website. [Accessed September 3, 2018]. http://www.sleepeducation.org/healthysleep.
- 4.Fuhrman C, Fleury B, Nguyên XL, Delmas MC. Symptoms of sleep apnea syndrome: high prevalence and underdiagnosis in the French population. Sleep Med. 2012;13(7):852–858. doi: 10.1016/j.sleep.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among adults--United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 6.Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheung JM, Bartlett DJ, Armour CL, Glozier N, Saini B. Insomnia patients' help-seeking experiences. Behav Sleep Med. 2014;12(2):106–122. doi: 10.1080/15402002.2013.764529. [DOI] [PubMed] [Google Scholar]
- 8.Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123–130. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Parks Associates. Sleep and IoT: Behaviors, Awareness, and Opportunities. Parks Associates website. [Accessed September 29, 2018]. https://www.parksassociates.com/services/sleep-iot.
- 10.Watson NF, Rosen IM, Chervin RD Board of Directors of the American Academy of Sleep Medicine. The past is prologue: the future of sleep medicine. J Clin Sleep Med. 2017;13(1):127–135. doi: 10.5664/jcsm.6406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye YY, Chen NK, Chen J, et al. Internet-based cognitive-behavioural therapy for insomnia (ICBT-i): a meta-analysis of randomised controlled trials. BMJ Open. 2016;6(11):e010707. doi: 10.1136/bmjopen-2015-010707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Espie CA, Emsley R, Kyle SD, et al. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiatry. 2018 Sep 25; doi: 10.1001/jamapsychiatry.2018.2745. . [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Consumer Technology Association R6.4 Health & Fitness Technology Subcommittee. ANSI/CTA Standard: Definitions and Characteristics for Wearable Sleep Monitors. Arlington, VA: Consumer Technology Association; 2016. ANSI/CTA-2052.1. [Google Scholar]
- 14.Consumer Technology Association R6.4 Health & Fitness Technology Subcommittee WG 1 Sleep Monitors. ANSI/CTA Standard: Methodology and Measurements for Features in Sleep Tracking Consumer Technology Devices and Applications. Arlington, VA: Consumer Technology Association; 2017. ANSI/CTA-2052.2. [Google Scholar]
- 15.Rosenberg RS, Van Hout S. The American Academy of Sleep Medicine inter-scorer reliability program: sleep stage scoring. J Clin Sleep Med. 2013;9(1):81–87. doi: 10.5664/jcsm.2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayas NT, Pittman S, MacDonald M, White DP. Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med. 2003;4(5):435–442. doi: 10.1016/s1389-9457(03)00111-4. [DOI] [PubMed] [Google Scholar]