Abstract
Background:
Recurrence rates are high for patients who have undergone two-stage hepatectomy (TSH) for bilateral colorectal liver metastases, and there is no established treatment approach for recurrent disease. This study aimed to determine the feasibility, safety, and prognostic impact of surgical resection for recurrence after TSH and the prognostic role of RAS mutation in this cohort.
Methods:
The study included 137 patients intended to undergo TSH for bilateral colorectal metastases during 2003–2016. Clinicopathologic factors were compared using univariate and multivariate analysis.
Results:
One hundred eleven patients (81%) completed TSH. The median recurrence-free survival in these patients was 12 months. Of the 83 patients with subsequent recurrence, 31 (37%) underwent resection for recurrence, and 11 underwent multiple resections for recurrence. Forty-eight operations were performed for recurrence: 23 repeat hepatectomies, 14 pulmonary resections, 5 locoregional resections, and 6 concurrent resections in multiple organ sites. The median overall survival (OS) among patients with recurrence was 143 months for patients who underwent resection and 49 months for those who did not (P<0.001). On multivariate analysis, resection for recurrence (hazard ratio [HR] 0.25; 95% CI 0.10–0.54, P<0.001) was associated with better OS, whereas RAS mutation (HR 2.25; 95% CI 1.16–4.50, P=0.016) and first recurrence in multiple sites (HR 2.28; 95% CI 1.17–4.37, P=0.016) were independent predictors of worse overall survival.
Conclusions:
In patients who have undergone TSH for bilateral colorectal liver metastases, recurrence is frequent and should be treated with resection whenever possible. Patients with wild-type RAS fare particularly well with resection for recurrence.
Keywords: colorectal neoplasms, hepatectomy, neoplasm metastases, recurrence
INTRODUCTION
Initially described by Adam et al. in 2000, two-stage hepatectomy (TSH) is a safe and effective technique for the treatment of bilateral colorectal liver metastases (CLM) [1–3]. Many patients whose liver disease would have been deemed unresectable in the past can be cured of disease after combined TSH and systemic chemotherapy, which produces 5-year overall survival (OS) rates nearing 50% [2–4]. With the use of portal vein embolization (PVE) combined with advances in surgical technique, rates of morbidity and mortality associated with TSH are low in experienced centers [3, 5, 6]. As more cases of advanced CLM are managed with TSH, a distinct group of patients with a high risk of recurrence is emerging.
Recurrence after TSH is frequent and often early, likely due to the overall burden of disease in patients that undergo TSH [3, 4]. TSH is unique in that the staged approach uses the test of time to evaluate tumor biology. After the first stage of TSH, the findings on pathologic examination of the surgical specimen indicate the response to preoperative chemotherapy [7, 8]. Subsequently, the time interval between stages of TSH allows for disease progression to present itself, particularly if interval chemotherapy is not used. While patients successfully completing TSH have less aggressive disease than those in whom TSH cannot be completed, patients completing TSH are still a group with aggressive cancer. This raises the question of how to manage disease recurrence in this patient population. A key question is whether surgical resection for recurrence after successful TSH improves OS.
The aim of this study, performed in a center with extensive experience in the management of bilateral CLM, was to determine the feasibility, safety, and prognostic impact of surgical resection for recurrence after TSH. As previous evidence from our institution demonstrated that RAS mutation status is predictive of worse OS after TSH [2], we also aimed to determine whether this remained the case in patients who underwent further surgical resections for recurrence after TSH.
MATERIALS AND METHODS
Study Population and Data Collection
The Institutional Review Board at The University of Texas MD Anderson Cancer Center approved this study (PA15–0203, RCR01–116). Of 1768 patients who underwent resection of CLM from November 2003 to November 2016, 137 patients were planned for TSH. For all patients, computerized medical records were queried retrospectively for clinicopathologic factors. Factors related to the primary tumor were collected when available, including the tumor location, nodal status, timing of diagnosis and resection, and the institution performing the resection. Synchronous CLM presentation was defined as CLM diagnosed within 365 days of primary tumor diagnosis. Extra-hepatic disease was defined as the presence of other metastatic disease at the time of the TSH, discovered either preoperatively on imaging or intraoperatively. Preoperative chemotherapy regimens were recorded for each patient when available, together with the timing of administration, and the number of cycles administered.
Data collected for each stage of TSH included extent of resection, presence of concurrent procedures, and estimated blood loss. Pathologic factors were also evaluated, including surgical margin status and number and size of CLM. Pathologic response to preoperative chemotherapy was described as complete (no viable tumor cells), major (1–49% viable tumor cells), or minor (≥50% viable tumor cells) [7]. This response was based on the specimen from the first stage of TSH. RAS mutation status was captured when available, either from the primary tumor or from the liver tumor specimen itself, given the high rates of concordance in mutation status between primary tumor and liver metastases [9]. Morbidity related to TSH was assessed according to the Clavien-Dindo classification, with grade III complications or greater classified as major [10]. Hepatic insufficiency was defined as peak total bilirubin level > 7 mg/dL [11].
The institutional approach for TSH has been well described [2]. After completion of the second stage, adjuvant chemotherapy was typically recommended to total 12 pre- and postoperative cycles. Data regarding recurrence, date of last follow-up, and survival were collected for all patients. For patients who had disease recurrence after completion of TSH, additional data were recorded, including the location of the recurrence and whether or not surgical resection was performed. “Multiple sites” of first recurrence was defined as newly diagnosed disease in more than one anatomic location. If a patient underwent resection for recurrence, details regarding the timing and site of the resection were recorded, along with peri-procedural data. Surgical resection for recurrence was categorized by site of operation as locoregional, liver, lung, or multiple organ sites. Recurrences were classified as locoregional if they occurred in the pelvis, retroperitoneum, or at the site of primary anastomosis. Hyperthermic intraperitoneal chemotherapy (HIPEC) and debulking was included in the “multiple organ sites” category. Survival in patients with recurrence after TSH was analyzed from time of the first stage resection and was analyzed again using the date of recurrence as the start time to avoid any impact of timing of recurrence on surgical planning.
Statistical Analysis
Categorical variables are expressed as numbers and percentages and were compared using the Fisher’s exact or chi-square test, as appropriate. Continuous variables are expressed as the median (interquartile range [IQR]) and were compared using the Mann-Whitney U test. The Kaplan-Meier method was used to construct survival curves, which were compared using the log-rank test. OS was calculated from the time of the first stage of TSH or from the time of recurrence after completion of TSH. Factors with P<0.10 in a Cox proportional hazard model as a univariate analysis were entered into multivariate Cox analysis for OS. All P values were two-sided and P<0.05 was deemed statistically significant. All statistical analysis was performed using JMP Pro software (version 12; SAS Institute Inc., Cary, NC).
RESULTS
Clinicopathologic Characteristics of Patients Undergoing TSH
A total of 137 patients were intended for TSH from November 2003 to November 2016, 89 (65%) male and 48 (35%) female. The median age for this entire cohort was 52 years (IQR, 45–61). The median number of CLM was 6 (IQR, 4–10) and the median maximum tumor diameter was 33 mm (IQR, 22–55). Among the 137 patients intended for TSH, 111 patients (81%) successfully completed both stages; 26 patients (19%) were unable to complete the second stage. Patients unable to complete TSH received a higher number of preoperative chemotherapy cycles (median 12 vs. 6, P=0.003) and were more likely to receive interval chemotherapy (81% vs. 37%, P <0.001). There were no significant differences between the groups with respect to other demographic, histopathologic, or perioperative factors.
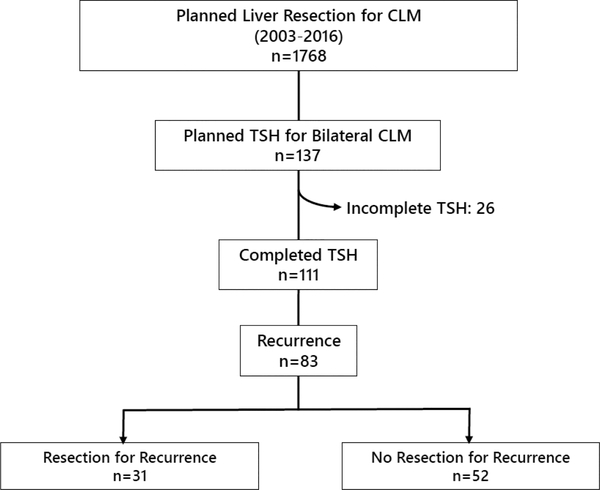
Of the 111 patients who completed TSH, 83 patients (75%) subsequently experienced disease recurrence. Thirty-one of these patients (37%) underwent at least one surgical resection for recurrence after TSH and 52 patients did not (63%) (Figure 1). Clinicopathologic factors for patients with recurrence are reported in Table 1. All factors assessed were similar between patients who did and those who did not undergo resection for recurrence. The majority of patients presented with synchronous CLM and a primary tumor in the colon with positive nodal involvement. Most patients underwent portal vein embolization. Within this cohort, major complications after either stage of TSH were seen in 19 patients (23%), of whom 15 (79%) experienced an intra-abdominal fluid collection or biloma requiring drainage by interventional radiology. One patient experienced postoperative hepatic insufficiency as well as a biloma requiring drainage; one patient developed a pulmonary embolism while on anticoagulation therapy and required placement of an inferior vena cava filter; and another patient developed a pneumothorax after a second-stage procedure that included a partial diaphragm resection and ultimately required videoscopic-assisted pleurodesis. Finally, one patient experienced a wound infection necessitating operative debridement after a combined abdominoperineal resection and partial hepatectomy as the first-stage procedure. The majority of patients in both groups underwent preoperative as well as adjuvant chemotherapy.
Figure 1.
Patient selection. CLM, colorectal liver metastases; TSH, two-stage hepatectomy.
Table 1.
Clinicopathologic characteristics of patients with recurrence after two-stage hepatectomy overall and by resection status*
| Characteristic | Total | Resection for recurrence |
No resection for recurrence |
P† |
|---|---|---|---|---|
| No. of patients | 83 | 31 (37) | 52 (63) | |
| Age, median (IQR), years | 52 (45–61) | 52 (45–61) | 53 (45–61) | 0.989‡ |
| Sex, male | 55 (66) | 21 (68) | 34 (65) | 0.826 |
| Preoperative chemotherapy | 82 (99) | 30 (97) | 52 (100) | 0.374¶ |
| >6 cycles | 29 (35) | 11 (35) | 18 (35) | 0.936 |
| Completion within 8 weeks of first stage§ | 62 (78) | 23 (77) | 39 (80) | 0.756 |
| Rectal primary tumor | 30 (36) | 13 (42) | 17 (33) | 0.397 |
| Primary tumor nodal status | 0.394¶ | |||
| Positive | 63 (76) | 24 (77) | 39 (75) | |
| Negative | 13 (16) | 6 (19) | 7 (13) | |
| Unknown | 7 (8) | 1 (3) | 6 (12) | |
| Synchronous CLM presentation | 72 (87) | 26 (84) | 46 (88) | 0.551 |
| Presence of extrahepatic metastases | 16 (19) | 7 (23) | 9 (17) | 0.556 |
| Number of CLM on preoperative imaging, median (IQR) | 6 (5–9) | 6 (5–7) | 7 (5–10) | 0.206‡ |
| Maximum CLM diameter, median (IQR), mm | 33 (20–45) | 29 (19–44) | 35 (22–49) | 0.194‡ |
| Pathologic response | 1.000¶ | |||
| Complete | 11 (15) | 4 (15) | 7 (15) | |
| Major | 46 (61) | 17 (63) | 29 (60) | |
| Minor | 18 (24) | 6 (22) | 12 (25) | |
| Positive surgical margin at either stage of TSH | 29 (35) | 10 (32) | 19 (37) | 0.646 |
| RAS mutation** | 36 (46) | 13 (42) | 23 (48) | 0.602 |
| Portal vein embolization | 59 (71) | 21 (68) | 38 (73) | 0.604 |
| Interval chemotherapy | 31 (37) | 14 (44) | 18 (35) | 0.505 |
| Major complication†† | 19 (23) | 7 (23) | 12 (23) | 0.959 |
| Adjuvant chemotherapy‡‡ | 54 (70) | 20 (69) | 34 (71) | 0.862 |
| Time to recurrence after completion of TSH, median (IQR), mo. | 10 (7–15) | 11 (7–16) | 10 (7–13) | 0.251 |
| Location of first recurrence | 0.239¶ | |||
| Liver | 33 (40) | 16 (52) | 17 (33) | |
| Lung | 15 (18) | 6 (19) | 9 (17) | |
| Locoregional | 7 (8) | 3 (10) | 4 (8) | |
| Peritoneum | 3 (4) | 1 (3) | 2 (4) | |
| Multiple sites | 25 (30) | 5 (16) | 20 (38) |
IQR, interquartile range; CLM, colorectal liver metastases; TSH, two-stage hepatectomy.
Values in table are number of patients (percentage) unless otherwise indicated.
χ2 test unless otherwise indicated.
Mann-Whitney U test.
Fisher’s exact test.
Missing data in 4 patients: 1 with resection and 3 without resection.
Missing data in 4 patients: 0 with resection and 4 without resection.
Clavien-Dindo grade ≥ III complication after either stage.
Missing data in 6 patients: 2 with resection and 4 without resection.
Clinicopathologic Characteristics of Patients Undergoing Resection for Recurrence
Of the 31 patients who underwent at least one surgical resection for recurrence after TSH, 11 patients (35%) underwent multiple operations, for a total of 48 operations performed for recurrence. Surgical outcomes for all resections for recurrence by location are summarized in Table 2. In two of the five patients with locoregional recurrences, the primary tumor resection was performed at an outside institution. The median time to first surgical resection for recurrence was 17 months (IQR, 11–27). Complications occurred after 16 operations (33%) and most were grade I or II. Major complications occurred in four patients (8%). Two patients developed a postoperative fluid collection requiring drainage by interventional radiology, one after a repeat hepatectomy and the other after resection of a locoregional recurrence. The other two patients required re-laparotomy. One of these two patients experienced wound dehiscence after a repeat hepatectomy, and the other developed infected ascites after the excision of a pelvic mass with retroperitoneal lymphadenectomy.
Table 2.
Surgical outcomes after resection of recurrence after two-stage hepatectomy, by location of resection
| All resections (n=48) | Locoregional (n=5) | Liver (n=23) | Lung (n=14) | Multiple organ sites (n=6) | |
|---|---|---|---|---|---|
| Time to resection, median (IQR), mo. |
17 (11–27) | 22 (18–28) | 15 (10–22) | 25 (14–39) | 11 (5–23) |
| Estimated blood loss, median (IQR), cc |
200 (100–300) | 250 (60–350) | 200 (150–350) | 100 (49–178) | 328 (219–600) |
| Operative time, median (IQR), min |
201 (145–294) | 191 (130–267) | 224 (176–301) | 129 (102–155) | 334 (267–360) |
| Positive surgical margin | 10 (21) | 1 (20) | 6 (26) | 1 (7) | 2 (33) |
| Any complication | 16 (33) | 4 (80) | 5 (22) | 3 (21) | 4 (67) |
| Major complication* | 4 (8) | 2 (40) | 1 (4) | 0 (0) | 1 (17) |
| Postoperative chemotherapy† | 20 (43) | 0 (0) | 13 (57) | 3 (21) | 4 (67) |
Values in table recorded as number of patients (percentage) unless otherwise indicated IQR, interquartile range
Clavien-Dindo grade ≥ III
Missing data for 1 patient.
Survival Outcomes
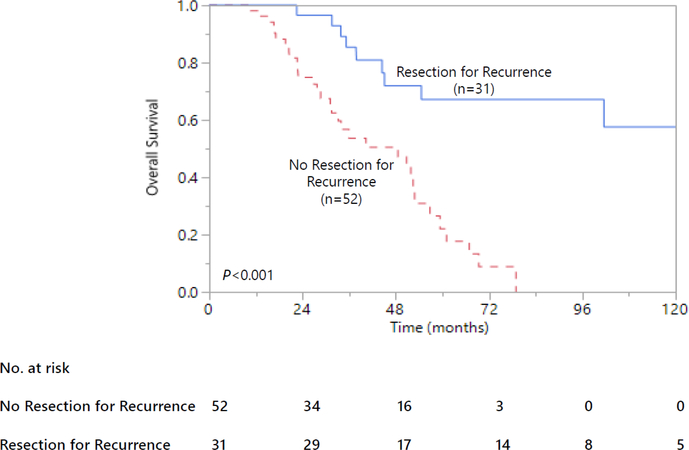
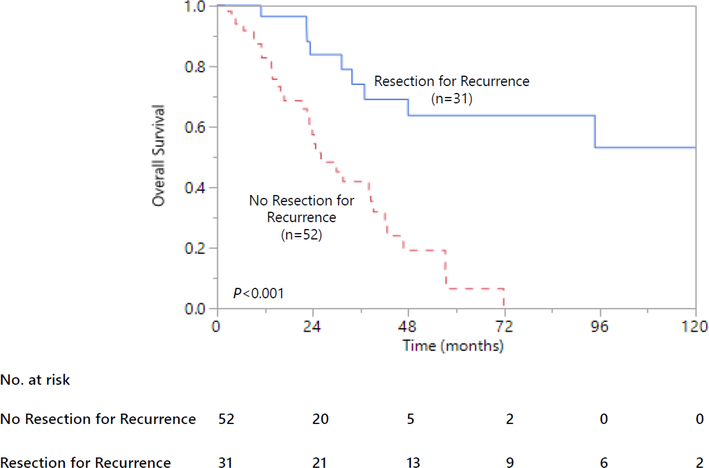
The median duration of follow-up for the entire cohort of patients was 32 months. The median OS from time of first-stage resection was 57 months for patients who completed TSH and 20 months for patients who were unable to complete TSH (P<0.001). For patients who completed TSH, the 5-year OS rate was 47% and the median recurrence-free survival was 12 months. Among the 83 patients with recurrence after completion of TSH, the median OS was 143 months for patients who underwent resection for recurrence and 49 months for those who did not undergo resection for recurrence (Figure 2A, P<0.001). When OS was re-assessed with the time of first recurrence used as the starting point, OS remained significantly longer for patients who underwent resection (Figure 2B, P<0.001).
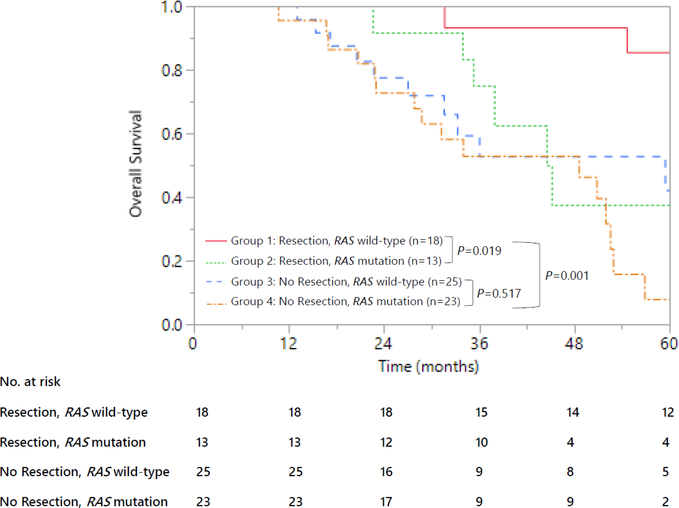
Figure 2.
Overall survival in patients with recurrence after two-stage hepatectomy. (a) Overall survival from time of first-stage hepatectomy, by resection status. (b) Overall survival from time of recurrence, by resection status. (c) Overall survival from time of first-stage hepatectomy, by resection status and RAS mutation status.
Survival Impact of RAS Mutation
Thirteen of 31 patients (42%) who underwent resection for recurrence and 23 of 48 patients (48%) who did not undergo resection for recurrence had a RAS mutation (P=0.602). Four patients with recurrence did not have genomic analysis performed and thus were excluded from this part of the analysis. Kaplan-Meier curves stratified by both resection status and RAS mutation status are shown in Figure 2C. Patients who underwent resection for recurrence and had RAS wild-type disease did markedly better than all other groups. Patients who did not undergo resection for recurrence and had a RAS mutation fared by far the worst, with a 5-year OS rate of only 8%. The 5-year OS rates for patients with wild-type RAS who underwent resection and patients with RAS mutation who underwent resection were 86% and 38%, respectively (P=0.019). Among the patients with a RAS mutation (n=36), survival did not differ by resection status (P=0.139).
Factors Associated with Overall Survival
Univariate analysis of clinicopathologic factors associated with OS demonstrated that RAS mutation, having a first recurrence in multiple sites, and surgical resection for recurrence were the only variables strongly associated with OS (Table 3). On multivariate analysis, resection for recurrence (hazard ratio [HR] 0.25; 95% CI 0.10–0.54, P<0.001) was associated with substantially better OS, whereas RAS mutation (HR 2.25; 95% CI 1.16–4.50, P=0.016) and first recurrence in multiple sites (HR 2.28; 95% CI 1.17–4.37, P=0.016) were independent risk factors for OS.
Table 3.
Univariate and multivariate analysis of overall survival for patients with recurrence after two-stage hepatectomy
| Variable | N(%) | 5-year survival rate, % |
Univariate P value |
Hazard ratio |
95% confidence interval |
Multivariate P value |
|---|---|---|---|---|---|---|
| All patients | 83 | 42 | ||||
| Preoperative factors | ||||||
| Age, >60 years | 55 (66) | 47 | 0.798 | |||
| Preoperative chemotherapy | 82 (99) | 41 | 0.110 | |||
| Rectal primary tumor | 30 (36) | 37 | 0.264 | |||
| Positive primary tumor nodal status |
63 (75) | 46 | 0.569 | |||
| Synchronous presentation | 72 (87) | 41 | 0.929 | |||
| Extra-hepatic disease | 16 (19) | 38 | 0.764 | |||
| Histopathologic factors | ||||||
| Total number of tumors > 5 | 51 (61) | 33 | 0.306 | |||
| Largest tumor diameter > 5 cm | 18 (22) | 33 | 0.817 | |||
| Positive surgical margin at either stage of TSH |
29 (35) | 39 | 0.900 | |||
| Complete pathologic response | 11 (15) | 44 | 0.665 | |||
| RAS mutation | 36 (46) | 19 | 0.006 | 2.25 | 1.16–4.50 | 0.016 |
| Postoperative factors | ||||||
| Portal vein embolization | 59 (71) | 40 | 0.980 | |||
| Interval chemotherapy | 31 (37) | 28 | 0.994 | |||
| Major complication at either Stage of TSH |
19 (23) | 34 | 0.287 | |||
| Adjuvant chemotherapy | 54 (70) | 44 | 0.973 | |||
| Recurrence-related factors | ||||||
| First recurrence at multiple sites | 25 (30) | 24 | 0.005 | 2.28 | 1.17–4.37 | 0.016 |
| Resection for recurrence | 31 (37) | 67 | <0.001 | 0.25 | 0.10–0.54 | <0.001 |
| TSH, two-stage hepatectomy | ||||||
DISCUSSION
This analysis of long-term outcomes in a large group of patients treated over nearly a decade and a half demonstrated that surgical resection for recurrence after TSH was feasible and safe. Patients who underwent resection for recurrence had a substantially improved OS compared to those who did not, and on multivariate analysis, resection for recurrence was the most significant prognostic factor for OS. The results of this analysis agree with results previously reported by Imai et al., showing that aggressive surgical management of recurrent disease in patients who have undergone TSH can result in improved survival rates [12]. The current study also serves as an update to previous institutional data confirming that TSH itself is feasible, safe, and associated with higher long-term OS rates than best medical therapy [2, 3].
This study demonstrated that RAS mutation was associated with lower long-term survival rates in patients with recurrence after TSH. RAS mutation has a known prevalence of 18 to 52% in patients undergoing resection of CLM, and is associated with worse OS after CLM resection [13–16]. Passot et al. demonstrated that RAS mutation was independently associated with shorter OS in patients who underwent TSH [2]. The present study confirms the negative prognostic implications of RAS mutation in a new context: patients undergoing resection for recurrence after TSH. However, our analysis showed no survival difference between RAS mutant patients who did or did not undergo resection for recurrence, meaning that the benefit of resection for recurrence in patients with RAS mutation remains unclear.
Importantly, the current study demonstrates the safety and efficacy of repeat surgical resection in patients who have previously undergone TSH. The staged approach to resection of bilateral CLM can be a demanding and emotionally exhausting process for the patient and healthcare team. It is critical to know that surgical resection for recurrence after a patient has previously undergone TSH is safe and efficacious before suggesting it as a management strategy. In our study, 48 operations were performed for recurrence after TSH with acceptable operative times and blood loss, and a major complication rate of only 8%. Repeat hepatectomy, which for some patients was a fourth or even fifth liver resection, was particularly safe and associated with low morbidity and appropriate rates of return to other oncologic therapy.
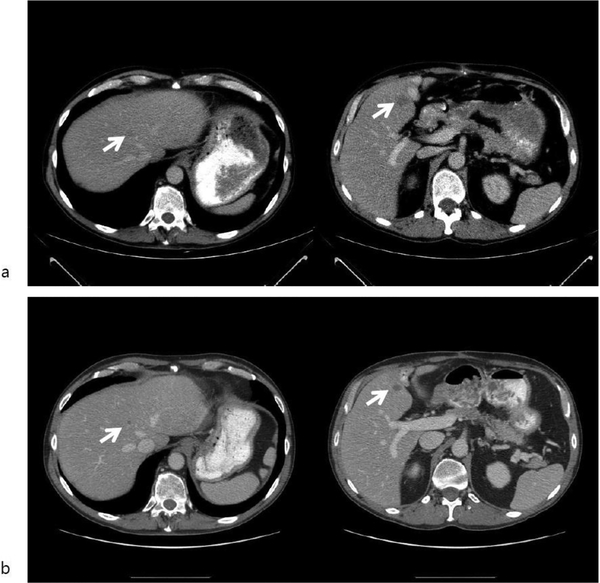
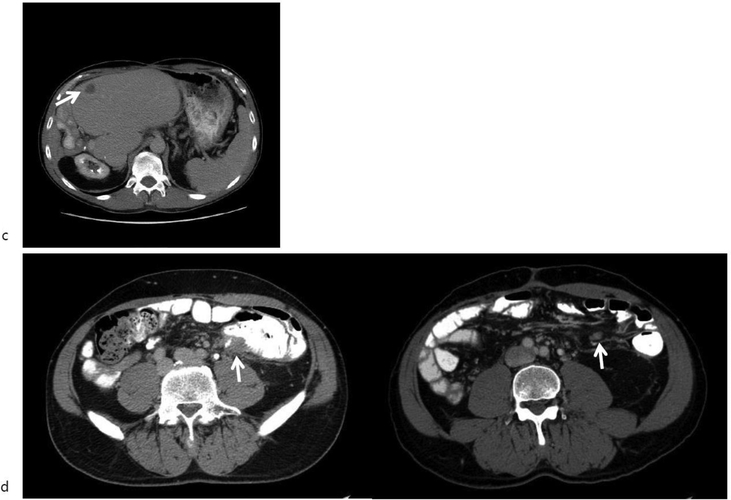
The management of disease recurrence after TSH is challenging. For liver recurrence, the three primary therapeutic options are chemotherapy, ablation, and resection. While ablation is preferred for early recurrences that are small and located in the periphery, those that occur late or cannot be ablated are more suited for surgical resection. For pulmonary metastases, the standard approach for lesions amenable to resection is pulmonary metastastectomy. Several studies have shown that patients with RAS mutations have a higher incidence of lung metastases [13, 17–19], leading to a more complex clinical picture. Finally, although less common, locoregional recurrence of colorectal cancer is being observed with increasing frequency as improvements in systemic therapy extend OS. Locoregional recurrence is more common with primary rectal disease and after margin-positive tumor resection [20, 21], which argues for total mesorectal excision (or complete mesocolic excision for colon primary tumors), even in patients with stage IV disease at presentation [22]. Resection for locoregional recurrence remains the best chance for cure; however, repeat operations in the pelvis are technically challenging and can be associated with significant morbidity. Importantly, the operative intent should be for an R0 resection, as this leads to significant survival benefits for locally recurrent colorectal cancer. Multimodal therapy, including a combination of systemic chemotherapy, radiotherapy, and surgical resection appears to provide the greatest benefit [23, 24]. Figure 3 shows representative images from a patient who underwent sequential resections for liver and locoregional recurrences.
Figure 3.
Computed tomography scans from a 52-year-old patient who underwent two-stage hepatectomy (TSH) after subtotal colectomy for cecal cancer and synchronous bilateral colorectal liver metastases. (a) Representative images at presentation reveal bilateral liver involvement, indicated by the arrows. (b) Images obtained after the patient underwent six cycles of FOLFOX + bevacizumab with arrows indicating tumor shrinkage. This was followed by TSH (partial hepatectomy of segment 3, interval portal vein embolization, and extended right hepatectomy). (c) Isolated hepatic recurrence (arrow) 8 months after completion of TSH. This was treated with FOLFIRI + bevacizumab, followed by partial hepatectomy of the segment III lesion. (d) Anastomotic and regional lymph node recurrence (arrows) 27 months after TSH. The patient underwent resection of the ileocolonic anastomosis en bloc with the tumor mass and ileocolonic nodes, with retroperitoneal lymphadenectomy and ileorectal anastomosis.
This study has several limitations. First, patients analyzed in this study represent a very select cohort of patients with CLM. Given the retrospective design and selection bias for patients who could tolerate not only a TSH but also subsequent resection for recurrence, we conclude that patients who can undergo resection for disease recurrence survive longer than those who cannot. Brouquet et al. previously reported that TSH was associated with improved survival compared to best medical therapy [3]. Our present study shows that the benefit is even greater if the patient can undergo surgical resection when diagnosed with recurrence. In addition, we grouped together various types of disease recurrence in colorectal cancer and we acknowledge that recurrences at different sites are clinically and possibly biologically distinct. The surgical operations required for recurrences at different sites also differ with regard to technique and difficulty. However, it would be difficult to compare each group separately due to the small numbers of patients.
CONCLUSION
Recurrence in patients who previously underwent TSH for bilateral CLM should be managed according to the specific characteristics of the recurrent disease. Aggressive surgical therapy should not be withheld on the basis of previous TSH, as resection for recurrence may offer significantly improved survival. RAS mutation status remains an important negative prognostic factor and should be considered when discussing surgical planning.
Acknowledgements
The authors thank Stephanie Deming (Department of Scientific Publications, MD Anderson Cancer Center) for copyediting the manuscript and Ruth J Haynes (Department of Surgical Oncology, MD Anderson Cancer Center) for secretarial assistance in the preparation of the manuscript.
Funding Sources: Dr. Heather Lillemoe is supported by National Institutes of Health grant T32CA009599–29 and the MD Anderson Cancer Center support grant (P30 CA016672).
Dr. Heather Lillemoe is supported by National Institutes of Health grant T32CA009599–29.
Footnotes
This study will be presented on June 5, 2018 at the 59th Annual Meeting of the Society for Surgery of the Alimentary Tract, Washington, DC.
References
- 1.Adam R, Laurent A, Azoulay D et al. Two-stage hepatectomy: A planned strategy to treat irresectable liver tumors. Ann Surg 2000; 232: 777–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Passot G, Chun YS, Kopetz SE et al. Predictors of Safety and Efficacy of 2-Stage Hepatectomy for Bilateral Colorectal Liver Metastases. J Am Coll Surg 2016; 223: 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brouquet A, Abdalla EK, Kopetz S et al. High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. J Clin Oncol 2011; 29: 1083–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wicherts DA, Miller R, de Haas RJ et al. Long-term results of two-stage hepatectomy for irresectable colorectal cancer liver metastases. Ann Surg 2008; 248: 994–1005. [DOI] [PubMed] [Google Scholar]
- 5.Narita M, Oussoultzoglou E, Jaeck D et al. Two-stage hepatectomy for multiple bilobar colorectal liver metastases. Br J Surg 2011; 98: 1463–1475. [DOI] [PubMed] [Google Scholar]
- 6.Lam VW, Laurence JM, Johnston E et al. A systematic review of two-stage hepatectomy in patients with initially unresectable colorectal liver metastases. HPB (Oxford) 2013; 15: 483–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blazer DG 3rd, Kishi Y, Maru DM et al. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol 2008; 26: 5344–5351. [DOI] [PubMed] [Google Scholar]
- 8.Passot G, Vauthey JN. In favor of two-stage hepatectomy (TSH). Eur J Surg Oncol 2015; 41: 1566–1567. [DOI] [PubMed] [Google Scholar]
- 9.Vakiani E, Janakiraman M, Shen R et al. Comparative genomic analysis of primary versus metastatic colorectal carcinomas. J Clin Oncol 2012; 30: 2956–2962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mullen JT, Ribero D, Reddy SK et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg 2007; 204: 854–862; discussion 862–854. [DOI] [PubMed] [Google Scholar]
- 12.Imai K, Benitez CC, Allard MA et al. Impact of Surgical Treatment for Recurrence After 2-Stage Hepatectomy for Colorectal Liver Metastases, on Patient Outcome. Ann Surg 2017. [DOI] [PubMed] [Google Scholar]
- 13.Vauthey JN, Zimmitti G, Kopetz SE et al. RAS mutation status predicts survival and patterns of recurrence in patients undergoing hepatectomy for colorectal liver metastases. Ann Surg 2013; 258: 619–626; discussion 626–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schirripa M, Bergamo F, Cremolini C et al. BRAF and RAS mutations as prognostic factors in metastatic colorectal cancer patients undergoing liver resection. Br J Cancer 2015; 112: 1921–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chun YS, Passot G, Yamashita S et al. Deleterious Effect of RAS and Evolutionary High-risk TP53 Double Mutation in Colorectal Liver Metastases. Ann Surg 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Margonis GA, Spolverato G, Kim Y et al. Effect of KRAS Mutation on Long-Term Outcomes of Patients Undergoing Hepatic Resection for Colorectal Liver Metastases. Ann Surg Oncol 2015; 22: 4158–4165. [DOI] [PubMed] [Google Scholar]
- 17.Kemeny NE, Chou JF, Capanu M et al. KRAS mutation influences recurrence patterns in patients undergoing hepatic resection of colorectal metastases. Cancer 2014; 120: 3965–3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim MJ, Lee HS, Kim JH et al. Different metastatic pattern according to the KRAS mutational status and site-specific discordance of KRAS status in patients with colorectal cancer. BMC Cancer 2012; 12: 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pereira AA, Rego JF, Morris V et al. Association between KRAS mutation and lung metastasis in advanced colorectal cancer. Br J Cancer 2015; 112: 424–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carlsson U, Lasson A, Ekelund G. Recurrence rates after curative surgery for rectal carcinoma, with special reference to their accuracy. Dis Colon Rectum 1987; 30: 431–434. [DOI] [PubMed] [Google Scholar]
- 21.Yeo HL, Paty PB. Management of recurrent rectal cancer: practical insights in planning and surgical intervention. J Surg Oncol 2014; 109: 47–52. [DOI] [PubMed] [Google Scholar]
- 22.Adam R, de Gramont A, Figueras J et al. Managing synchronous liver metastases from colorectal cancer: a multidisciplinary international consensus. Cancer Treat Rev 2015; 41: 729–741. [DOI] [PubMed] [Google Scholar]
- 23.You YN, Skibber JM, Hu CY et al. Impact of multimodal therapy in locally recurrent rectal cancer. Br J Surg 2016; 103: 753–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colibaseanu DT, Mathis KL, Abdelsattar ZM et al. Is curative resection and long-term survival possible for locally re-recurrent colorectal cancer in the pelvis? Dis Colon Rectum 2013; 56: 14–19. [DOI] [PubMed] [Google Scholar]