Abstract
Improving the built environment (BE) is viewed as one strategy to improve community diets and health. The present goal is to review the literature on the effects of BE on health, highlight its limitations, and explore the growing use of natural experiments in BE research, such as the advent of new supermarkets, revitalized parks, or new transportation systems. Based on recent studies on movers, a paradigm shift in built-environment health research may be imminent. Following the classic Moving to Opportunity study in the US, the present Moving to Health (M2H) strategy takes advantage of the fact that changing residential location can entail overnight changes in multiple BE variables. The necessary conditions for applying the M2H strategy to Geographic Information Systems (GIS) databases and to large longitudinal cohorts are outlined below. Also outlined are significant limitations of this approach, including the use of electronic medical records in lieu of survey data. The key research question is whether documented changes in BE exposure can be linked to changes in health outcomes in a causal manner. The use of geo-localized clinical information from regional health care systems should permit new insights into the social and environmental determinants of health.
Keywords: Built environment (BE), Geographic information systems (GIS), Electronic medical records, Natural experiments, Obesity, Diabetes, Residential mobility
Highlights
-
•
The present Moving to Health approach represents a new type of a “natural experiment”
-
•
While built environment (BE) is fixed in place, moving to a new residential location can change one’s BE virtually overnight.
-
•
The question is whether such a shift in BE exposure have any long-term impact on health, body weight or diabetes outcomes.
1. Introduction
Where people live affects their health and well-being. Studies have pointed to multiple links between residential location, the surrounding built environment (BE), and the risk of non-communicable diseases (NCD), including obesity and type 2 diabetes (T2D) (Dearry, 2004, Drewnowski et al., 2014a, Drewnowski et al., 2014b, Ewing et al., 2003, Gibson, 2011, Laska et al., 2010, Moore et al., 2008).
Health-smart urban planning requires a better understanding of which aspects of the BE are most likely to have a measurable impact on obesity rates. Among neighborhood features thought to influence weight and health are walkability (Creatore et al., 2016, Duncan et al., 2015; Hajna et al., 2016; Lee & Moudon, 2006a; Lovasi, Grady, & Rundle, 2011; Moudon et al., 2007; Rundle et al., 2008), proximity to parks and trails (Cohen et al., 2006a, Cohen et al., 2006b, Edwards et al., 2014, Kaczynski et al., 2014, Rundle et al., 2013, Spoon, 2012, Van Cauwenberg et al., 2015), and access to physical activity (Berke et al., 2007, Ding and Gebel, 2012, Frank et al., 2007, Lee and Moudon, 2004; Lee et al., (2009); McCormack, 2017; Nelson & Woods, 2009). The food environment, often defined by the density of and proximity to supermarkets, grocery stores, farmers’ markets, fast food stores, or convenience stores has also been linked to diet quality, obesity, and T2D risk (Aggarwal et al., 2014, Babey et al., 2008, Caspi et al., 2012, Drewnowski et al., 2012, Jiao et al., 2015a, Jiao et al., 2015b, Leal and Chaix, 2011, Zenk et al., 2017).
The study of BE and health has been facilitated by recent advances in geographic information systems (GIS) and global positioning systems (GPS) technologies (Cetateanu et al., 2016b). Spatially-referenced data at a high level of resolution have now become the norm in studies of BE and health outcomes. Aggregate BE data for US counties, health planning areas, and ZIP codes have given way to higher-resolution data such as census tracts, census blocks, or individual tax parcel lots (Drewnowski, Rehm, & Solet, 2007, Drewnowski, Rehm, & Arterburn, 2014b; Lovasi et al., 2013; Stark et al., 2013; Stewart, Moudon, Fesinmeyer, Zhou, & Saelens, 2016; Zenk et al., 2017). Novel variables, including area residential property values, have allowed for a better characterization of area SES in relation to body weight and other health outcomes. That in turn allowed for exploration of geographic disparities in obesity rates, sometimes at the neighborhood level (Drewnowski et al., 2007, Drewnowski et al., 2009, Drewnowski et al., 2014c, Drewnowski et al., 2014d, Ewing et al., 2003, Jackson et al., 2005). Both diet quality and obesity have now been mapped at US census tract and at census block levels (Drewnowski et al., 2009, Drewnowski et al., 2014a, Mayne et al., 2015).
To date, most studies on the impact of BE on body weight have been cross-sectional, pointing to some interesting associations but not allowing for any causal inferences to be made (Alexander et al., 2013, Berry et al., 2010a, Berry et al., 2010b, Jiao et al., 2016). Only longitudinal cohort studies can address the critical and still unanswered question: does the residential BE have a causal effect on body weight trajectories and on overall health? More specifically, can the neighborhood BE variables predict the risk of obesity, T2D, or metabolic syndrome; and can they predict the likelihood of weight loss or weight gain?
Only large, longitudinal cohort studies can answer the further question: do different components of BE, some modifiable and others not, have a direct impact on health outcomes that is independent of area socioeconomic status (SES)? A focus on the modifiable aspects of the BE would inform policy-level decisions about how future neighborhoods ought to be designed.
The present Moving to Health conceptual model was inspired to a significant extent by the classic Moving to Opportunity Study, a randomized social experiment sponsored by the US Department of Housing and Urban Services in the 1990s (Ludwig et al., 2011). The Moving to Opportunity Study tried to answer the question whether moving from a high-poverty to a lower-poverty neighborhood improved the social and economic prospects of the lower-income families in the long term. The present and more health-focused question is whether moving to a different residential location can have a long-term impact on body weight trajectories and obesity risk.
This conceptual note also calls for a paradigm shift. The currently popular “natural experiments” examine the health impact of changes in the BE (Mayne at al., 2015). For the most part, those changes were based on the introduction of a new supermarket, a new or refurbished park or playing field, or a new light rail system. In all those cases, it was the BE that was modified, whereas the people stayed put.
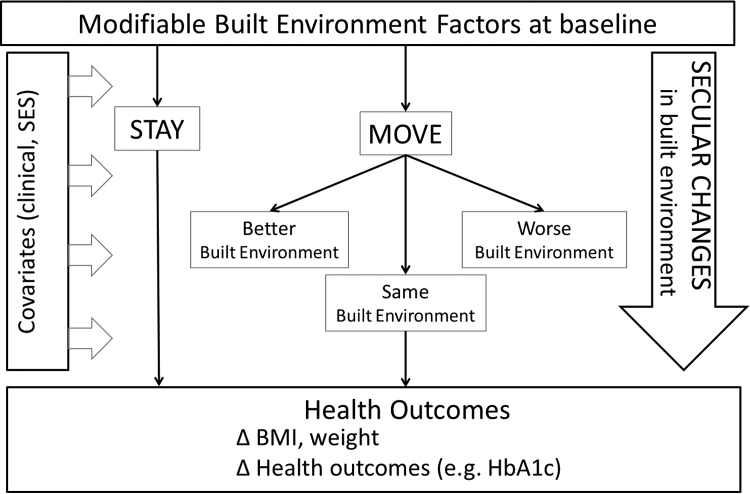
The conceptual scheme of the new research strategy is shown in Fig. 1. In general, it is the real estate that is immobile; it is people who are more likely to move. The mere act of moving to another house in a different neighborhood may change the proximal BE (including the food environment) virtually overnight. Many of the standard BE variables, commonly linked to health outcomes in past research, are likely to change. Neighborhood walkability, proximity to parks and trails, access to supermarkets, farmers’ markets, fast foods, and convenience stores can all change dramatically from one day to the next.
Fig. 1.
.
The critical question is – does any of it make any difference to body weights, or a wide variety of health outcomes?
2. The built environment and health
The BE is said to be a powerful predictor of population health (Dearry, 2004; Diez Roux, 2001; Macintyre, Ellaway, & Cummins, 2002). Reflecting on the impact of place on health, the National Academy of Sciences (NAS) has called on researchers and policymakers to address any modifiable environmental factors that might contribute to health inequalities at the neighborhood level (Health US, 2013). Among those were disparities in access to healthy foods (Laska et al., 2010, Moore et al., 2008, Morland et al., 2002) and opportunities for physical activity (Lee and Moudon, 2004, Lovasi et al., 2008, Macintyre et al., 2002, Saelens et al., 2003a, Saelens et al., 2003b).
2.1. The impact of physical activity and food environments on health
The physical activity (PA) environment is normally conceptualized in terms of density of or distance to parks and trails (Cohen et al., 2006a, Cohen et al., 2006b, Edwards et al., 2014, Ewing and Cervero, 2010, Kaczynski et al., 2014, Rundle et al., 2013, Spoon, 2012, Van Cauwenberg et al., 2015), and recreational facilities (Alexander et al., 2013), the length of sidewalks and street-block size (Berke et al., 2007, Ding and Gebel, 2012, Frank et al., 2007, McCormack, 2017, Stafford et al., 2007, Stewart et al., 2016, Yan et al., 2010). More recent studies, including some natural experiments, have explored the impact on PA of living close to light rail or other public transport as well as the impact of active commuting, and bus ridership (Lee and Moudon, 2004, Lee and Moudon, 2006a, Lee and Moudon, 2006b, MacDonald et al., 2010; Moudon, Hess, Snyder, & Stanilov, 1997; Moudon et al., 2007). In general, more walking has been associated with better transportation infrastructure, measured as intersection, street, and sidewalk density, as well as with traffic conditions, measured by traffic volume and bus ridership (Mitchell Hess, Vernez Moudon, & Logsdon, 2001). Opportunities for PA have also been measured as access to fitness and recreation facilities (Alexander et al., 2013, Lee and Moudon, 2004, Lee and Moudon, 2006a, Lee and Moudon, 2006b, Moudon et al., 1997, Moudon et al., 2007).
The walkability of BE has the potential to influence physical activity (Duncan et al., 2015, Hajna et al., 2016, Lovasi et al., 2008, Lovasi et al., 2011, Moudon et al., 2007, Rundle et al., 2008, Saelens et al., 2003a, Saelens et al., 2003b). Overall, there has been consensus that more walkable BEs are associated with higher levels of PA activity (Creatore et al., 2016, Duncan et al., 2015, Hajna et al., 2016, Lovasi et al., 2011, Rundle et al., 2008). The extent of recreation-based PA has been related to proximity to parks and trails (Cohen et al., 2006a, Cohen et al., 2006b, Edwards et al., 2014, Ewing and Cervero, 2010, Kaczynski et al., 2014, Spoon, 2012, Van Cauwenberg et al., 2015). A study of 6,376 same-sex twins provided evidence that higher neighborhood walkability was associated with more walking, and that more walking was associated with lower BMI (Duncan et al., 2015). A meta-analysis showed that a 1% reduction in distance to a food store was associated with a 25% increase in walking trips (Duncan, Spence, & Mummery, 2005). It is suggested by cross sectional studies that persons living near parks, hiking or walking trails, and other recreational activity centers have more PA (Alexander et al., 2013, Berry et al., 2010a, Berry et al., 2010b, Cohen et al., 2006a, Cohen et al., 2006b, Edwards et al., 2014, Kaczynski et al., 2014, Rundle et al., 2013, Van Cauwenberg et al., 2015).
The food environment has been conceptualized in terms of density of or distance to food sources within a certain distance of home (Caspi et al., 2012, Drewnowski et al., 2014c, Drewnowski et al., 2014d, Gibson, 2011, Jiao et al., 2012, Li et al., 2009, Moore et al., 2008, Zenk et al., 2017). Food sources thought to be most relevant to diet quality and health were supermarkets, grocery stores, fast food restaurants, and convenience stores (An and Sturm, 2012, Bodor et al., 2008, Caspi et al., 2012, Fraser and Edwards, 2010, Hickson et al., 2011, Jiao et al., 2015a, Jiao et al., 2015b, Drewnowski, 2015; Moudon et al., 2013). In some studies, proximity to supermarkets, grocery stores, and traditional restaurants was associated with better diets and better health (Bodor et al., 2008, Gase et al., 2014, Morland et al., 2006, Treuhaft and Karpyn, 2010). By contrast, proximity to convenience stores/fast-food restaurants was associated with poor diets and impaired health (Apparicio et al., 2007, Burdette and Whitaker, 2004, Caspi et al., 2012, Jiao et al., 2015a, Jiao et al., 2015b, Laska et al., 2010, Sharkey and Horel, 2008, Smoyer-Tomic et al., 2006).
However, not all studies produced consistent results. Some studies found that people living closer to full-service supermarkets had lower body weights (Caspi et al., 2012, Laska et al., 2010, Morland and Evenson, 2009, Powell et al., 2007, Rundle et al., 2008, Stafford et al., 2007) but other studies did not (Drewnowski et al., 2012, Fiechtner et al., 2013, Gase et al., 2014, Hattori et al., 2013). Some studies found that people living closer to fast foods and convenience stores were more likely to be obese (Fraser and Edwards, 2010, Hickson et al., 2011, Leung et al., 2011, Mellor et al., 2011, Morland and Evenson, 2009) but other studies did not (Burdette and Whitaker, 2004, Fiechtner et al., 2013, Hattori et al., 2013). The distinction between the physical aspects of the BE and its underlying economic characteristics was not always made clear (An & Sturm, 2012).
For example, perceived proximity to supermarkets, farmers’ markets and cafes, as opposed to fast foods, gas stations and convenience stores is likely to be reflected in the value of real estate and the purchasing power of the neighborhood. In general, the desirability of a given residential area is captured precisely by neighborhood property values. Several studies have now reported links between proximity to specific food sources and area socioeconomic status. In general, perceived proximity to fast foods and convenience stores has been associated with lower property values (Aggarwal et al., 2011, Drewnowski et al., 2012, Drewnowski et al., 2014b, Drewnowski et al., 2015, Jiao et al., 2016), whereas perceived proximity to parks and cafes has been associated with higher property values (An and Sturm, 2012, Burdette and Whitaker, 2004, Leung et al., 2011; Morland & Evenson, 2009; Rundle et al., 2008). Higher property values have been linked, in turn, with lower obesity risk (An and Sturm, 2012, Burdette and Whitaker, 2004, Leung et al., 2011, Morland and Evenson, 2009, Rundle et al., 2008).
2.2. Some limitations of current approaches
When it comes to the food environment, the limitations of the current evidence base can be summarized as follows. First, the data on the underlying area SES is often lacking, while data on residential property values comes from limited studies. Complementing education and incomes, residential property values better capture accumulated wealth, a useful proxy for economic resources and social class. Evidence is accumulating that geo-localized residential property values provide the useful bridge between area SES and health outcomes.
Second, the choice of residence and the composition of the neighborhood is subject to multiple influences. People may self-select their residential locations based on multiple – and usually unmeasured - social and economic variables (Drewnowski et al., 2014b, James et al., 2015, Macintyre et al., 2003). For example, studies have suggested that activity-conscious individuals may be more likely to move to neighborhoods with higher walkability and higher physical activity (Berry et al., 2010a, Berry et al., 2010b; Lee et al., 2009). Lee et al., suggests that people who are more active may be more aware of exercise facilities, which may influence their choice of neighborhood.
Both social capital and social context are also likely to play a part (Drewnowski et al., 2014b, Powell-Wiley et al., 2014, Powell-Wiley et al., 2015, Sharkey and Horel, 2008). Very few health-oriented studies have examined social capital, social context, or area resources in relation to area socioeconomic status. Very few studies on diets and health have asked why people moved into a given neighborhood in the first place or asked about the cost of rent or mortgage (Berry et al., 2010a, Berry et al., 2010b, Rummo et al., 2017).
Third, many studies have been conducted at a crude level of aggregation. Local health jurisdictions are in critical need of geo-localized health data that is actionable and sufficiently fine-grained for developing targeted interventions. Cross-sectional data aggregated to large geographic units (state, county, or metropolitan area) can provide only limited insights into the geographic distribution of obesity and T2D (Alexander et al., 2013, Berry et al., 2010a, Berry et al., 2010b, Cadwell et al., 2010, Control, 2009, Control, 2011, Jiao et al., 2016; Control and Prevention, 2011). Although analyses by ZIP code have been useful for shaping some local policies and programs; the geography of obesity does not follow crude administrative boundaries (Drewnowski et al., 2007, Drewnowski et al., 2014c, Drewnowski et al., 2014d, Lovasi et al., 2013, Stark et al., 2013, Stewart et al., 2016, Zenk et al., 2017). As a result, it has proven difficult to identify those BE elements that are modifiable and most likely to be associated with positive health outcomes (Berke & Vernez-Moudon, 2014). GIS analyses based on higher resolution data may be required to inform legal and regulatory changes in the BE, such as changes in zoning, street standards, or transportation systems (Berke & Moudon, 2014).
There is no question that small area studies point to sharp disparities in diets and health at the local level. For example, spatial epidemiologic studies, based on 59,767 insured adults in King County WA, aggregated by census tract (CT), showed that the prevalence of obesity and T2D varied more than 2.7-fold across county CTs. Crude obesity rates varied from 16% to 44%, whereas T2D rates varied from 7% to 21%, depending on where people lived (Dearry, 2004, Diez Roux, 2001). Lower rates of obesity and T2D were associated with higher area SES, the latter captured by residential property values at the tax parcel level (Drewnowski et al., 2014a, Drewnowski et al., 2014b). About 70% of variance in CT obesity rates and 39% of variance in CT T2D in King County was predicted by the proportion of college educated adults, median household incomes, and residential property values. Lower residential property values were associated with higher obesity rates among women (Drewnowski et al., 2007, Drewnowski et al., 2009, Drewnowski et al., 2014a, Drewnowski et al., 2014b, Rehm et al., 2012).
2.3. Does the built environment affect weight change?
We identified a number of observational studies of BE that included weight or BMI as an outcome (Carter et al., 2013, Ewing et al., 2006, Hirsch et al., 2014a, Hirsch et al., 2014b, Joost et al., 2016, Lippert, 2016, Powell-Wiley et al., 2015, Rachele et al., 2018, Stafford et al., 2010). Of these, several studies explored the impact of baseline BE on the cohort's weight gain over time (Carter et al., 2013, Ewing et al., 2006; Hirsch et al., 2014a, Hirsch et al., 2014b; Hoyt et al., 2014; Joost et al., 2016; Lippert, 2016; Powell-Wiley et al., 2015; Rachele et al., 2018; Stafford et al., 2010). Some of those studies explored the impact of the BE on weight change, usually over a period of 3 to 12 years (Carter et al., 2013, Ewing et al., 2006, Hoyt et al., 2014, Joost et al., 2016, Powell-Wiley et al., 2014). Only three of those studies explored the impact of neighborhood environments on weight and obesity risk (Carter et al., 2013, Ewing et al., 2006, Hoyt et al., 2014, Joost et al., 2016). In general, living in lower SES or deprived neighborhoods was associated with a greater risk of obesity and with increased weight gain among children and adolescents (Carter et al., 2013, Ewing et al., 2006, Hoyt et al., 2014).
One hypothesis was that the lack of parks, trails, and physical activity locations in lower SES areas could contribute to excessive weight gain (Cohen et al., 2006a, Cohen et al., 2006b, Edwards et al., 2014, Ewing and Cervero, 2010, Kaczynski et al., 2014, Van Cauwenberg et al., 2015). That view has been supported by studies that explored physical activity levels by neighborhood (Creatore et al., 2016, Duncan et al., 2015, Hajna et al., 2016, Lovasi et al., 2011, Rundle et al., 2008, Saelens et al., 2003a, Saelens et al., 2003b) or examined the correlations between physical activity and neighborhood BE (Duncan et al., 2015, Hajna et al., 2016, Lovasi et al., 2011, Lovasi et al., 2008; Moudon et al., 2007; Rundle et al., 2008; Saelens et al., 2003a, Saelens et al., 2003b).
Strong associations between changes in neighborhood walkability and weight gain or loss were reported in three studies (Hirsch et al., 2014a, Hirsch et al., 2014b, MacDonald et al., 2010). Hirsch et al., 2014a, Hirsch et al., 2014b found that people who moved to an area with increased walkability experienced a decrease in BMI. There was further evidence that persons who moved into neighborhoods with more walking destinations had lower BMIs prior to their move (Michimi & Wimberly, 2010). Macdonald et al. (2010) found that persons who used a newly installed light rail system walked more and lost more weight.
Data on the impact of the food environment on body weight trajectories were much more limited (Hoyt et al., 2014). A study of 174 adolescents found that living in areas with a high density of food sources was associated with increased obesity risk (Hoyt et al., 2014). As with physical activity, more longitudinal studies are needed to draw causal connections between changes in the food environment and body weight.
2.4. What is the impact of natural experiments on health?
Natural experiments are thought to offer some advantages over traditional observational studies (Mayne et al., 2015). The stated goal of natural experiments has been to assess the impact of changes to the BE on community health (Mayne et al., 2015).
Typically, natural experiments have assessed changes in the BE caused by third party groups, whether by urban development or by private or government action (Mayne et al., 2015). Those BE modifications have included the construction of new supermarkets, new light rail systems, or new park improvements (Hirsch et al., 2018, MacDonald et al., 2010, Mayne et al., 2015). The general assumption has been that positive changes in the BE can benefit the neighborhood and have a direct and measurable impact on the residents’ health. While researchers did not have control over the BE interventions themselves, they were able to study PA or health outcomes (Mayne et al., 2015). Manipulation was minimal as investigators simply sampled individuals within a population before and after any third-party BE intervention.
Mayne et al., (2015) analyzed a number of natural experiment studies that assessed environmental changes and their effects on physical activity, nutrition, and obesity or BMI. Of these, 17 investigated the impact of the modified BE (parks, trails, schoolyards) on self-reported PA and body weight (Mayne et al., 2015). In one study, continuing urbanization was linked to a lower risk for obesity (Hirsch et al., 2014a). A study of newly introduced light rail transit in Charlotte, NC, found that residents using the light rail system showed a decrease in BMI and reduced obesity risk (MacDonald et al., 2010). However, there was no consensus in the literature that improved public transportation increased PA (Mayne et al., 2015).
18 additional studies, reviewed by Mayne et al., (2015), examined the impact of changing BE on diets. However, only three of those explored the impact of BE on obesity and body weight (Mayne et al., 2015). There was no evidence that changes in the BE following a natural experiment improved diets or impacted body weight (Mayne et al., 2015).
The underlying assumption of many natural experiments has been that the BE changes while people stay in place, at least for long enough to experience health changes due to changing BE exposures. However, while studies were conducted in the same area, study samples before and after a given BE interventions were not necessarily the same (Dubowitz et al., 2015). Furthermore, the construction of new supermarkets and transportation systems does not guarantee their use by the surrounding community. In the Pittsburgh PHRESH study, the opening of a new supermarket in a former food desert was associated with greater neighborhood satisfaction and with improved neighborhood diets (Dubowitz et al., 2015). However, those improvements could not be tied to the supermarket itself; indeed, the use of the new supermarket was not associated with any dietary changes or lower body weight. Nonetheless, the researchers recommended continuing policies to incentivize food retail in food deserts, while cautioning that the mechanisms by which diet is improved were imperfectly understood (Dubowitz et al., 2015).
The present position is that any analyses of long term changes in the BE, conducted by third parties, take too long and are confounded by market forces. The building of a new supermarket does not alter the purchasing power of the neighborhood. As a result, neighborhood dietary patterns are unlikely to change.
There is clearly a need for a paradigm shift. Natural experiments are one way to study the impact of changing BE on health. Researchers have advocated for even more natural experiments in obesity research, arguing that studying changes in BE would strengthen the evidence base for local obesity-related policies and local interventions (Mayne et al., 2015). We propose a different type of a natural experiment built around people who change their proximal BE by moving to a different residential location. The U.S. Census Bureau has estimated that 14% of people move annually and 25% move within a 5-year period. Out of those, more than 50% moved within the same county (Bureau, 2016).
3. An imminent paradigm shift in built environment research
3.1. The moving to opportunity study
The classic Moving to Opportunity (MTO) study in the US stands apart as the sole randomized controlled trial (RCT) that studied improvement in neighborhood variables (Ludwig et al., 2011). The study included 5,000 participants, aged 18 y and older, who lived in five major US cities and were followed for a mean of 12.6 years. Participants were randomized into conditions, with some receiving vouchers allowing them to relocate to areas with improved neighborhood SES. The study concluded that participants who were randomly assigned the opportunity to move to a higher SES neighborhood experienced lower incident obesity and T2D.
While highly important because of its randomized design, the MTO study had no measures of the physical BE (Ludwig et al., 2011). Those components of neighborhood BE that potentially had the greatest impact on weights and health could not be identified. By focusing on people who move, the present Moving to Health research strategy (Section 4 below) borrows the central premise of the MTO study, adding a rich array of BE variables. The present goal was to explore a similar type of natural experiment, but to examine how abrupt changes in the neighborhood BE may affect long term health outcomes.
3.2. A focus on residential mobility
There is research literature on residential mobility and the impact of health outcomes of movers versus stayers. We identified ten key studies of movers that are summarized in Table 1 (Berry et al., 2010a, Berry et al., 2010b, Braun et al., 2016, Ewing et al., 2006, Hirsch et al., 2014a; Lee et al., 2009; Lippert, 2016; Mayne et al., 2015; Powell-Wiley et al., 2015; Rachele et al., 2018; Stafford et al., 2010). These studies were based on a total of 37,276 mover participants, of whom 3,667 were children (12–17 y) (Ewing et al., 2006), and with a mean follow-up duration of ~7 y. People who moved away from low SES or deprived neighborhoods had lower BMIs and lower obesity risk (Berry et al., 2010a, Berry et al., 2010b, Lippert, 2016, Mayne et al., 2015, Powell-Wiley et al., 2015, Rachele et al., 2018, Stafford et al., 2010).
Table 1.
Selected studies of residential mobility and obesity that examined movers versus stayers.
| Author & Year | # participants | Follow-up (y) | Key Findings |
|---|---|---|---|
| A focus on people who move | |||
| Ewing-2006 | 3667 | 7 | Adolescents living in sprawling counties more likely to be overweight or at risk of obesity. Changes in BMI not associated with movers. |
| Lee-2009 | 3448 | 5 | Moving to a more or less-sprawling area was not associated with change in BMI. |
| Berry-2010 | 572 | 6 | Participants in lowest SES neighborhoods had largest increases in BMI; moving not significantly associated. |
| Stafford-2010 | 8151 | 11 | Women who resided in neighborhoods with low SES had higher BMI at baseline and greater weight gain over 10 years. No effect in men. |
| Ludwig-2011 | 4498 | 13 | The MTO study. Subjects randomized; opportunity to move from low to high SES neighborhood experienced reductions in the prevalence of obesity and diabetes. |
| Hirsch-2014a | 934 | 6 | Analyzed movers only. Moving to a location with a higher walkability score was associated with a 0.06 lower BMI. |
| Powell-Wiley-2015 | 1835 | 7 | Moving to an area with higher deprivation correlated with weight gain. A longer duration of living in the deprived area associated with increased weight gain. |
| Braun- 2016 | 1079 | 6 | Greater walkability in neighborhoods corresponded with preferable health outcomes like lower blood pressure. Results subject to bias with regard to neighborhood self-selection. |
| Lippert 2016 | 12,164 | 15 | Adolescents who grew up and stayed in low SES neighborhoods had higher risks for obesity compared to individuals stay in moderate-high SES neighborhoods. |
| Rachele - 2018 | 928 | 6 | Changes in the level of neighborhood disadvantage were not associated with BMI changes in women who moved. |
| Total # Subjects | 37,276 |
Four studies investigated the impact of moving to different BEs and the subsequent changes in body weight (Braun et al., 2016, Ewing et al., 2006, Hirsch et al., 2014a; Lee et al., 2009). In a study of 5,506 adults (934 movers) aged 45–84 y in several US cities, Hirsch et al., (2014a) found that moving to an area with a 10-point higher walkability score was associated with a 0.06 lower BMI. Higher walking destination density, population density, and lower percent residential were all linked to a decrease in BMI. In contrast, other studies (one of adults and one of adolescents) found that moving to a more or less-sprawling area (variably defined) was not associated with a change in BMI or BMI z-score (Ewing et al., 2006; Lee et al., 2009). Braun et al., (2016) found no association between changes in walkability and change in BMI among 1,079 movers.
Powell-Wiley et al. (2015) found that adults who moved to more deprived neighborhoods (measured by a novel neighborhood deprivation index or NDI) gained more weight compared to other movers. Longer duration of living in a high NDI area was associated with more weight gain (Powell-Wiley et al., 2015).
4. The Moving to Health (M2H) approach to natural experiment research
US Census Bureau data on geographic mobility show that naturally occurring residential moves are frequent (Bureau, 2016). Access to a well-characterized longitudinal cohort of health care users, confined to a well described geographic area, would be one way to study the impact of the BE on body weights and health. Implementing the M2H approach could take advantage of anonymized electronic medical records (EMR) from a large health system. Some of the conceptual and technical requirements for this research strategy, as suggested by the literature are outlined below.
4.1. A need for geo-localized participant health data
Precise geo-location of participants is necessary to allow greater insight into the complex relations among BE and health outcomes, that are often mediated by individual or area SES.
Geocoded health data are finding their way into the literature (Zandbergen, 2014). Aggregated health data tend to be provided at different levels, from county and metropolitan areas, to health planning areas, ZIP codes, census tracts, or nearest intersections (Zandbergen, 2014). While individual addresses are optimal, precautions need to be taken to assure anonymity and removal of any identifying information (Drewnowski et al., 2007, Drewnowski et al., 2014a, Drewnowski et al., 2014b, Zandbergen, 2014). This is critically important when electronic medical records (EMR) are involved.
4.2. A need for BE metrics at fine level of resolution
Joining vast amounts of EMR data with detailed BE data requires using state-of-the-art GIS methodologies, while developing new methods of spatial analysis. In past studies, the BE has been characterized in a variety of ways. Many of the methods, but not all, have aggregated BE elements by administrative boundaries (Diez Roux, 2004, Macintyre et al., 2003).
SmartMaps, defined below, represent a departure from data aggregated by US county or census tract. Instead, SmartMaps operationalize the measurement of neighborhood context at the individual tax parcel level (Casey et al., 2016, Hurvitz and Moudon, 2012, Hurvitz et al., 2014; Moudon et al., 2014; Lee, Moudon, & Courbois, 2006).
To aid in the creation of SmartMaps, the UW Urban Form Lab (UFL) has assembled GIS databases capturing changes in more than 40 BE characteristics in King County since 2005 (KC; area 5500 km2) using data from various sources not traditionally used in health research. Tax parcel polygon and residential property value data came from the KC tax assessor. KC GIS services provided street and regional trail data, while bus ridership data came from KC Metro, and traffic data came from the Puget Sound Regional Council (the region's municipal planning agency). The UW-UFL developed food establishment data based on geocoded food permits obtained from Public Health-Seattle KC; the UFL compiled park data from individual jurisdiction GIS layers, and geocoded PA and fitness facility data from InfoUSA. BE factors measured at the home neighborhood level for KPWA members will be linked to EMR data, thus creating datasets which are entirely novel.
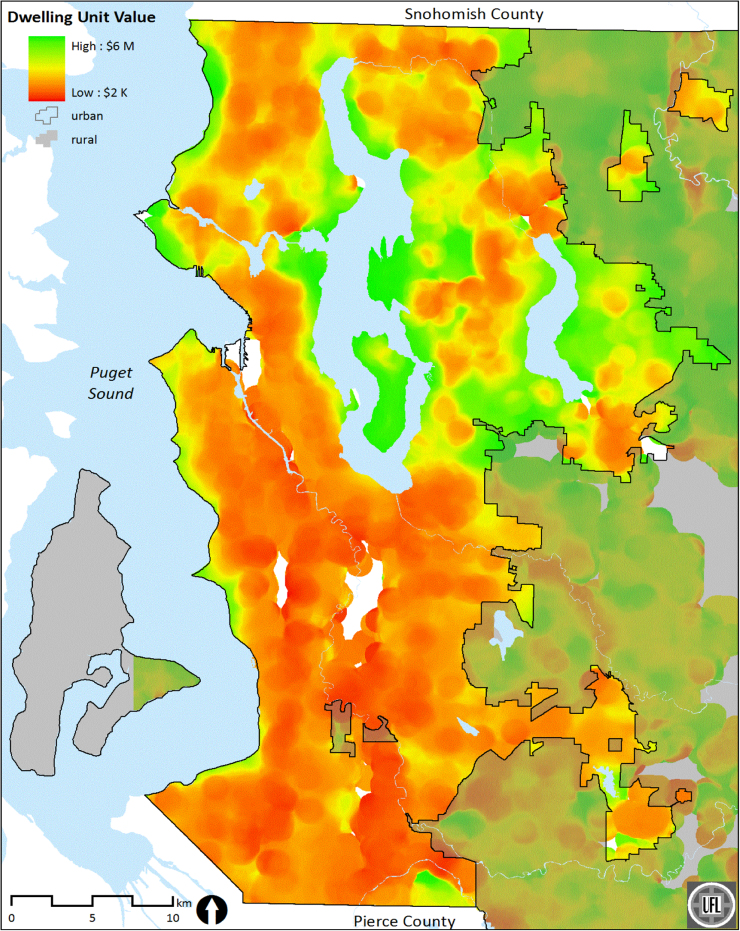
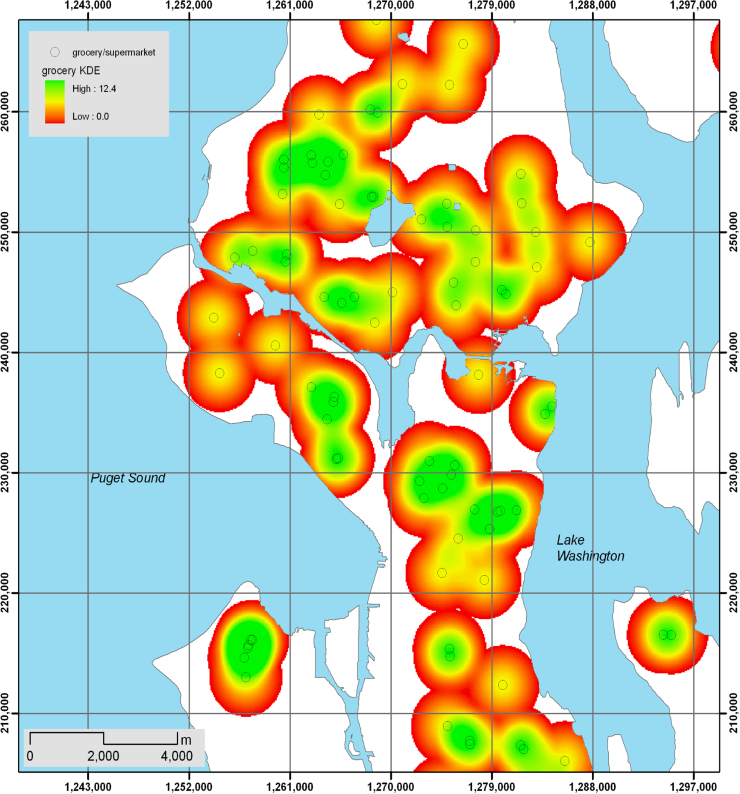
SmartMaps use a range of distances from home to define a participant neighborhood, with 800 m being a commonly used measure that corresponds to the distance that can be walked in 10 minutes (Lovasi et al., 2011). To calculate a SmartMap of residential unit counts, parcels are first converted to a 30 m raster grid, where the value of each cell represents the fraction of residential units within the cell (e.g., a 9000 m2 parcel containing 20 residential units yielded 10 cells with a value of 2 units per cell). The process then sums the values of all cells within each focal “neighborhood” to estimate the number of residential units. Typically, the geocoded home address will correspond to one focal cell, which will be extracted using ArcGIS Surface Spot method. Fig. 2, Fig. 3 show SmartMaps of residential property values and supermarket density, respectively, in King County.
Fig. 2.
SmartMap of residential property values.
Fig. 3.
SmartMap of supermarket density.
Access to healthy foods has been measured in terms of distance to food sources from the participant's home or work. Distance measures have included estimates of the shortest travel time and the shortest physical distance along the road network. These measures were typically taken using the Network Analyst within ArcGIS, employing NAVTEQ or HERE Maps data, which realistically model the street network, including features such as one-way streets, freeway entrances and exits, and limited access roadways (e.g., freeways, pedestrian-only segments).
Walkability was typically indexed as a composite measure of neighborhood development density; mixed uses to insure walking destinations within the neighborhood; and intersection density to provide direct routes between homes and neighborhood destinations (Duncan et al., 2015). The UFL has produced several such indices in the past which have been translated into SmartMaps (Berke and Vernez-Moudon, 2014, Drewnowski et al., 2014c, Drewnowski et al., 2014d, Lee and Moudon, 2006b, Moudon et al., 2011a, Moudon et al., 2011b). Table 2 summarizes the SmartMaps that will be created for BE domains and variables.
Table 2.
Neighborhood built environment (BE) variables in the Moving to Health research strategy.
| Variable Domain | Built environment variable, measures and data sources |
|---|---|
| Variables related to environments that support utilitarian or recreational PA | |
| Neighborhood composition | Residential density (count of residential units/km2) from KC GIS and KC Assessor |
| Employment density (count jobs/km2) from Dept. of Labor statistics | |
| Topography | Terrain slope (% area >5% slope) from digital terrain models |
| Transportation system | Street density (km/km2) from KC GIS transportation roadway data |
| Intersection density (count/km2) from KC GIS transportation roadway data | |
| Sidewalk coverage (sidewalk length; as percent of street length) from UW-UFL data | |
| Transit stop density (count/km2) from KC Metro | |
| Bus ridership per stop (count/km2) from KC Metro | |
| Traffic volume (length of street) from Puget Sound Regional Council | |
| Social and recreation environment | Public parks, (count, % area) from UW-UFL data |
| Trails (km/km2) from KC GIS | |
| Density/distance to fitness centers, playgrounds, swimming areas from InfoUSA, KC GIS | |
| Densities/distances to community centers from KC GIS | |
| Neighborhood services | Densities/distances to stores & neighborhood shopping centers from KC GIS and InfoUSA |
| Densities/distances to medical facilities (hospitals, clinics, HMO sites) from KC GIS | |
| Variables related to environmental food sources | |
| Food environment | Densities/distance to supermarkets, grocery stores, farmers’ markets from UW-UFL/KC GIS |
| Densities/distance to convenience stores from UW-UFL and KC GIS | |
| Densities/distance to full service, fast food, quick service restaurants from UW-UFL/KC GIS | |
4.3. A need for measures of individual and area SES
Knowing whether people move to higher-, lower- or equivalent SES neighborhoods allows for novel measures of exposure. In past studies, we have used assessed property values as a direct measure of individual-level SES (Drewnowski et al., 2016, Moudon et al., 2011a, Moudon et al., 2011b). Property value metrics have been tested previously against typical SES measures, using a representative sample of 2000 participants for King County population. Neighborhood-level SES indicators typically include the mean residential property value within 800 m buffer of respondents’ home, as well as area-weighted mean education attainment, household income, and neighborhood race/ethnicity composition – the latter three variables from US Census data.
SmartMaps of residential property values complement the standard indices of SES: education and incomes (Drewnowski et al., 2016, Moudon et al., 2011a, Moudon et al., 2011b). Since WA State has no income tax, taxation on real property is an essential source of revenue and tax rolls are both accurate and up to date. In Seattle-King County, local variation in residential property values is not captured by CT level data.
It has to be recognized that as people move into a new neighborhood and are abruptly exposed to the new BE, the BE itself may be changing albeit at a slower rate. Moving to a new area does not preclude a new supermarket, a new park, or a new transportation system from being built. Furthermore, those enhancement of the BE are not going to be uniform across neighborhoods. For that reason, studies on the impact of BE on health in a long term cohort, need to include some historical data on how the BE had changed over time.
4.4. A need for long term health and weight outcomes
Long term health and weight outcomes have been used in many prior studies (Arterburn et al., 2013, Drewnowski et al., 2014c, Drewnowski et al., 2014d, Nichols et al., 2012). First clinically-measured height, weight, and clinically diagnosed diabetes provide greater confidence in outcomes of interest and greater ability to access repeated measures within individuals. Based on KPWA data, 37% of adults and 13% of children and adolescents were obese during the study period, which is consistent with national estimates for adults and slightly lower for children. Prevalence of T2D among adults was 9.6%, which is consistent with recent published national estimates (9.3%) (Control & Prevention, 2014). Few children had T2D (0.5%).
Based on KPWA data, more than 86% of adults and children have at least one BMI measurement in the EMR. Furthermore, >210,000 adults and 62,000 children have 2+ BMI measures occurring at least 1 year apart. More than 54,000 adults and 30,000 children have 2 or more weight measures occurring at least 9 years apart. The mean (13) and median (7) number of BMI measures per patient is high. Among adults with T2D, the mean number of HbA1c measures is 9 with a median of 7.
4.5. The limitations of M2H approach
People move for any number of reasons. The use of insurance data as the principal source of both residential location and electronic medical records (EMR) does not permit the study of motivations for such a move. EMR data may identify a change in address and insurance coverage, but do not provide motivations for moving to a different residential address. This is an important limitation, given that a move to a different neighborhood may reflect (or be a proxy for) a shift in individual socioeconomic status. People who move away from a deprived neighborhood may have the means to do so; those who move into a poorer neighborhood may have experienced economic insecurity. Diet quality and health outcomes can be influenced by neighborhood resources, but are also driven by household purchasing power. Residential self-selection bias is one issue that needs to be addressed in full.
Second, address coded EMR data are by definition home-centric. No data on where people shopped for food, exercised, or ate in restaurants are available. Living in a given neighborhood does not necessarily predict full use of that neighborhood's resources (Sharp, Denney, & Kimbro, 2015). For that reason, recent studies on BE and health have turned away from the home-centric “residential trap”, preferring to use GPS tracking devices to establish individual food activity spaces (Chaix, 2018, Kestens et al., 2018) The use of large scale geocoded EMR precludes those options. Whereas the use of GPS tracking to estimate activity spaces is still relatively new (Cetateanu & Jones, 2016a), it holds promise as a means of assessing exposure to the food environment in both time and space. However, daily selective mobility bias (Chaix et al., 2013) may complicate the drawing of causal inferences as to the relation between environmental exposure and health.
Third, insurance EMRs do not permit explorations of intermediate pathways related to energy balance such as diet quality or physical activity behaviors. Without intermediate pathways, the ability of the proposed analyses to advance our understanding of the impact of BE in obesity related outcomes is significantly reduced.
Finally, studying insured households (and those that maintained insurance through a move), means that understanding the impact of BE on the health of vulnerable groups is not possible. Loss of insurance through job loss would in some instances remove participants from the study. The generalizability of such findings to other households can be improved by ensuring that the population under study does include Medicare.
Additional data from other studies may be necessary to complement the M2H approach. For example the ongoing prospective Seattle Obesity Study is collecting GPS, accelerometer, and dietary intakes data for a longitudinal cohort of 1,000 adults in Western WA State over a 24-month period. One focus of the SOS is to explore mechanisms for socioeconomic disparities between King and Pierce Counties, and Yakima County, with a predominantly Hispanic population of lower education and incomes. Since the SOS also collects data on dietary intakes, shopping patterns, dietary behaviors and food assistance, it is able to delineate the behavioral pathways between diverse aspects of the local food environment, obesity and other health outcomes. By contrast, the Moving to Health cohort lacks survey data, but can rely on a very large sample, a sufficient number of movers, and a decade's worth of exposure. Both types of studies are needed to assess the likely impact of neighborhood BE on health.
We will also address the potential for unobserved confounding through a series of sensitivity analyses. Furthermore, any behavioral measures of diet and PA lie on the causal pathway between the BE and our outcomes and should not be adjusted for in our models.
5. Implications of M2H strategy for health-smart urban development
Learnings from large scale cohort studies based on geo-localized clinical data from regional health care systems and linked to aspects of the BE can be useful to urban planners and health policy makers. Such studies can track the changing relationship between the BE and obesity and T2D, at the very high levels of geographic resolution.
There are a number of health related questions that will need to be addressed. The first question is whether BE variables, measured at baseline, can predict longitudinal changes in 1) body weight and 2) HbA1c during up to 12 years follow-up, independent of baseline measures of socioeconomic status (SES; e.g., individual residential property value and neighborhood-level median household income), demographic variables (e.g., age, gender, race/ethnicity, insurance type), and comorbid health conditions (e.g., smoking, asthma, arthritis, hypertension, dyslipidemia).
The second question is whether overnight moving-induced changes in BE variables have any impact on body weight, obesity and T2D that is independent of SES. The third question is whether slower changes in the BE can predict changes in health outcomes among people who do not move residence, independent of changes in SES and other covariates.
This new natural experiment examining sudden (for movers) and gradual (for non-movers) changes in the BE for a very large cohort will provide unprecedented insights into the impact of different places on health. Armed with our findings, urban planners and policymakers will be able to target different BE features for intervention, based on local and regional realities. At the same time, the data will help inform individual residential location decisions and help to create demand for those neighborhood features that are most likely to be supportive of health.
6. Conclusions
Urban developers, policy makers, health authorities, and health care consumers would all benefit from studies on which aspects of the BE are linked to health outcomes, ideally in a causal manner. In the absence of RCTs, longitudinal designs with repeated clinical follow-ups and periodic assessments of the changing BE provide greater ability for drawing causal inferences. Analyzing naturally occurring residential moves in a well characterized longitudinal cohort represents a paradigm shift and a different type of natural experiment in studies of the impact on BE on body weights and health.
Ethics approval
Ethics approval not required.
Acknowledgments
Supported by NIH grants 1 R01 DK 114196-01 and 5 R01 DK076608-10.
References
- Aggarwal A., Cook A.J., Jiao J., Seguin R.A., Vernez Moudon A., Hurvitz P.M., Drewnowski A. Access to supermarkets and fruit and vegetable consumption. American Journal of Public Health. 2014;104(5):917–923. doi: 10.2105/AJPH.2013.301763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aggarwal A., Monsivais P., Cook A.J., Drewnowski A. Does diet cost mediate the relation between socioeconomic position and diet quality? European Journal of Clinical Nutrition. 2011;65(9):1059. doi: 10.1038/ejcn.2011.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander D.S., Huber L.R.B., Piper C.R., Tanner A.E. The association between recreational parks, facilities and childhood obesity: A cross-sectional study of the 2007 National Survey of Children's Health. Journal of Epidemiology and Community Health. 2013 doi: 10.1136/jech-2012-201301. (jech-2012-201301) [DOI] [PubMed] [Google Scholar]
- An R., Sturm R. School and residential neighborhood food environment and diet among California youth. American Journal of Preventive Medicine. 2012;42(2):129–135. doi: 10.1016/j.amepre.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apparicio P., Cloutier M.-S., Shearmur R. The case of Montreal's missing food deserts: Evaluation of accessibility to food supermarkets. International Journal of Health Geographics. 2007;6(1):4. doi: 10.1186/1476-072X-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arterburn D.E., Bogart A., Sherwood N.E., Sidney S., Coleman K.J., Haneuse S., McCulloch D. A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obesity surgery. 2013;23(1):93–102. doi: 10.1007/s11695-012-0802-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babey, S.H., Diamant, A.L., Hastert, T.A., & Harvey, S. (2008). Designed for disease: the link between local food environments and obesity and diabetes.
- Berke E.M., Koepsell T.D., Moudon A.V., Hoskins R.E., Larson E.B. Association of the built environment with physical activity and obesity in older persons. American Journal of Public Health. 2007;97(3):486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berke E.M., Vernez-Moudon A. Built environment change: A framework to support health-enhancing behaviour through environmental policy and health research. Journal of Epidemiology and Community Health. 2014:2012–201417. doi: 10.1136/jech-2012-201417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry T.R., Spence J.C., Blanchard C.M., Cutumisu N., Edwards J., Selfridge G. A longitudinal and cross-sectional examination of the relationship between reasons for choosing a neighbourhood, physical activity and body mass index. International Journal of Behavioral Nutrition and Physical Activity. 2010;7(1):57. doi: 10.1186/1479-5868-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry T.R., Spence J.C., Blanchard C.M., Cutumisu N., Edwards J., Selfridge G. A longitudinal and cross-sectional examination of the relationship between reasons for choosing a neighbourhood, physical activity and body mass index. International Journal of Behavioral Nutrition and Physical Activity. 2010;7:57. doi: 10.1186/1479-5868-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodor J.N., Rose D., Farley T.A., Swalm C., Scott S.K. Neighbourhood fruit and vegetable availability and consumption: The role of small food stores in an urban environment. Public Health Nutrition. 2008;11(4):413–420. doi: 10.1017/S1368980007000493. [DOI] [PubMed] [Google Scholar]
- Braun L.M., Rodriguez D.A., Song Y., Meyer K.A., Lewis C.E., Reis J.P., Gordon-Larsen P. Changes in walking, body mass index, and cardiometabolic risk factors following residential relocation: Longitudinal results from the CARDIA study. Journal of Transport Health. 2016;3(4):426–439. doi: 10.1016/j.jth.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdette H.L., Whitaker R.C. Neighborhood playgrounds, fast food restaurants, and crime: Relationships to overweight in low-income preschool children. Preventive Medicine. 2004;38(1):57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- Bureau, U.C. (2016). Americans Moving at Historically Low Rates, Census Bureau Reports. Retrieved from 〈https://www.census.gov/newsroom/press-releases/2016/cb16-189.html〉.
- Cadwell B., Thompson T., Boyle J., Barker L. Bayesian small area estimates of diabetes prevention by US county. Journal of Data Science. 2010 [PMC free article] [PubMed] [Google Scholar]
- Carter M.A., Dubois L., Tremblay M.S., Taljaard M. The influence of place on weight gain during early childhood: A population-based, longitudinal study. Journal of Urban Health. 2013;90(2):224–239. doi: 10.1007/s11524-012-9712-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey J.A., Schwartz B.S., Stewart W.F., Adler N.E. Using electronic health records for population health research: A review of methods and applications. Annual Review of Public Health. 2016;37:61–81. doi: 10.1146/annurev-publhealth-032315-021353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi C.E., Sorensen G., Subramanian S., Kawachi I. The local food environment and diet: A systematic review. Health place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cetateanu A., Jones A. How can GPS technology help us better understand exposure to the food environment? A systematic review. Social Science Medicine – Population Health. 2016;2:196–205. doi: 10.1016/j.ssmph.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cetateanu A., Luca B.A., Popescu A.A., Page A., Cooper A., Jones A. A novel methodology for identifying environmental exposures using GPS data. International Journal of Geographical Information Science. 2016;30(10):1944–1960. [Google Scholar]
- Chaix B. Mobile sensing in environmental health and neighborhood research. Annual Review of Public Health. 2018;39:367–384. doi: 10.1146/annurev-publhealth-040617-013731. [DOI] [PubMed] [Google Scholar]
- Chaix B., Méline J., Duncan S., Merrien C., Karusisi N., Perchoux C., Lewin A., Labadi K., Kestens Y. GPS tracking in neighborhood and health studies: A step forward for environmental exposure assessment, a step backward for causal inference? Health Place May. 2013;21:46–51. doi: 10.1016/j.healthplace.2013.01.003. (Epub 2013 Jan 17) [DOI] [PubMed] [Google Scholar]
- Cohen, D., Sehgal, A., Williamson, S., Sturm, R., McKenzie, T.L., Lara, R., & Lurie, N. (2006a). Park use and physical activity in a sample of public parks in the city of Los Angeles.
- Cohen D.A., Ashwood J.S., Scott M.M., Overton A., Evenson K.R., Staten L.K., Catellier D. Public parks and physical activity among adolescent girls. Pediatrics. 2006;118(5):e1381–e1389. doi: 10.1542/peds.2006-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Control, C.F.D. (2009). Estimated County-level prevalence of diabetes and obesity - United States, 2007. Retrieved from: 〈http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5845a2.htm〉. [PubMed]
- Control, C.F.D. (2011). Diabetes Public Health Resource: CDC identified Diabetes Belt. Retrieved from: 〈http://www.cdc.gov/diabetes/news/docs/diabetes_belt.htm〉.
- Control, C.F.D., & Prevention (2011). Diabetes data & trends: county level estimates of diagnosed diabetes.
- Control C. f D., Prevention . US Department of Health and Human Services; Atlanta, GA: 2014. National diabetes statistics report: Estimates of diabetes and its burden in the United States, 2014. (2014) [Google Scholar]
- Creatore M.I., Glazier R.H., Moineddin R., Fazli G.S., Johns A., Gozdyra P., Booth G.L. Association of neighborhood walkability with change in overweight, obesity, and diabetes. Jama. 2016;315(20):2211–2220. doi: 10.1001/jama.2016.5898. [DOI] [PubMed] [Google Scholar]
- Dearry A. Impacts of our built environment on public health. Environmental Health Perspectives. 2004;112(11):A600. doi: 10.1289/ehp.112-a600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A.V. Investigating neighborhood and area effects on health. American Journal of Public Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A.V. The study of group-level factors in epidemiology: Rethinking variables, study designs, and analytical approaches. Epidemiologic Reviews. 2004;26(1):104–111. doi: 10.1093/epirev/mxh006. [DOI] [PubMed] [Google Scholar]
- Ding D., Gebel K. Built environment, physical activity, and obesity: What have we learned from reviewing the literature? Health Place. 2012;18(1):100–105. doi: 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- Drewnowski A., Aggarwal A., Cook A., Stewart O., Moudon A.V. Geographic disparities in healthy eating index scores (HEI–2005 and 2010) by residential property values: Findings from Seattle obesity study (SOS) Preventive Medicine. 2016;83:46–55. doi: 10.1016/j.ypmed.2015.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Aggarwal A., Hurvitz P.M., Monsivais P., Moudon A.V. Obesity and supermarket access: Proximity or price? American Journal of Public Health. 2012;102(8):e74–e80. doi: 10.2105/AJPH.2012.300660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Aggarwal A., Tang W., Moudon A.V. Residential property values predict prevalent obesity but do not predict 1‐year weight change. Obesity. 2015;23(3):671–676. doi: 10.1002/oby.20989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Moudon A.V., Jiao J., Aggarwal A., Charreire H., Chaix B. Food environment and socioeconomic status influence obesity rates in Seattle and in Paris. International Journal of Obesity. 2014;38(2):306. doi: 10.1038/ijo.2013.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Rehm C., Kao C., Goldstein H. Poverty and childhood overweight in California Assembly districts. Health Place. 2009;15(2):631–635. doi: 10.1016/j.healthplace.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Rehm C.D., Arterburn D. The geographic distribution of obesity by census tract among 59 767 insured adults in King County, WA. International Journal of Obesity. 2014;38(6):833. doi: 10.1038/ijo.2013.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Rehm C.D., Moudon A.V., Arterburn D. The geography of diabetes by census tract in a large sample of insured adults in King County, Washington, 2005–2006. Preventing Chronic Disease. 2014;11:E125. doi: 10.5888/pcd11.140135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Rehm C.D., Moudon A.V., Arterburn D. Peer reviewed: The geography of diabetes by census tract in a large sample of insured adults in King County, Washington, 2005–2006. Preventing Chronic Disease. 2014:11. doi: 10.5888/pcd11.140135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Rehm C.D., Solet D. Disparities in obesity rates: Analysis by ZIP code area. Social Science Medicine. 2007;65(12):2458–2463. doi: 10.1016/j.socscimed.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz T., Ghosh-Dastidar M., Cohen D.A., Beckman R., Steiner E.D., Hunter G.P., Sloan J.C. Changes in diet after introduction of a full service supermarket in a food desert. Health Affairs (Project Hope) 2015;34(11):1858. doi: 10.1377/hlthaff.2015.0667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan G.E., Cash S.W., Horn E.E., Turkheimer E. Quasi-causal associations of physical activity and neighborhood walkability with body mass index: A twin study. Preventive Medicine. 2015;70:90–95. doi: 10.1016/j.ypmed.2014.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan M.J., Spence J.C., Mummery W.K. Perceived environment and physical activity: A meta-analysis of selected environmental characteristics. International Journal of Behavioral Nutrition and Physical Activity. 2005;2(1):11. doi: 10.1186/1479-5868-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards N.J., Giles-Corti B., Larson A., Beesley B. The effect of proximity on park and beach use and physical activity among rural adolescents. Journal of Physical Activity and Health. 2014;11(5):977–984. doi: 10.1123/jpah.2011-0332. [DOI] [PubMed] [Google Scholar]
- Ewing R., Brownson R.C., Berrigan D. Relationship between urban sprawl and weight of United States youth. American Journal of Preventive Medicine. 2006;31(6):464–474. doi: 10.1016/j.amepre.2006.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing R., Cervero R. Travel and the built environment: A meta-analysis. Journal of the American Planning Association. 2010;76(3):265–294. [Google Scholar]
- Ewing R., Schmid T., Killingsworth R., Zlot A., Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. American Journal of Health Promotion. 2003;18(1):47–57. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- Fiechtner L., Block J., Duncan D.T., Gillman M.W., Gortmaker S.L., Melly S.J., Taveras E.M. Proximity to supermarkets associated with higher body mass index among overweight and obese preschool-age children. Prev Med. 2013;56(3-4):218–221. doi: 10.1016/j.ypmed.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank L.D., Saelens B.E., Powell K.E., Chapman J.E. Stepping towards causation: Do built environments or neighborhood and travel preferences explain physical activity, driving, and obesity? Social Science Medicine. 2007;65(9):1898–1914. doi: 10.1016/j.socscimed.2007.05.053. [DOI] [PubMed] [Google Scholar]
- Fraser L.K., Edwards K.L. The association between the geography of fast food outlets and childhood obesity rates in Leeds, UK. Health Place. 2010;16(6):1124–1128. doi: 10.1016/j.healthplace.2010.07.003. [DOI] [PubMed] [Google Scholar]
- Gase L.N., DeFosset A.R., Smith L.V., Kuo T. The association between self-reported grocery store access, fruit and vegetable intake, sugar-sweetened beverage consumption, and obesity in a racially diverse, low-income population. Frontiers in Public Health. 2014;2:229. doi: 10.3389/fpubh.2014.00229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson D.M. The neighborhood food environment and adult weight status: Estimates from longitudinal data. American Journal of Public Health. 2011;101(1):71–78. doi: 10.2105/AJPH.2009.187567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajna S., Kestens Y., Daskalopoulou S.S., Joseph L., Thierry B., Sherman M., Walkablilty Study G. Neighbourhood walkability and home neighbourhood-based physical activity: An observational study of adults with type 2 diabetes. BMC Public Health. 2016;16:957. doi: 10.1186/s12889-016-3603-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattori A., An R., Sturm R. Peer reviewed: neighborhood food outlets, diet, and obesity among California Adults, 2007 and 2009. Preventing Chronic Disease. 2013;10 doi: 10.5888/pcd10.120123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health US . The National Academies Press; Washington, DC: 2013. International Perspective: Shorter Lives, Poorer Health. [PubMed] [Google Scholar]
- Hickson D.A., Diez Roux A.V., Smith A.E., Tucker K.L., Gore L.D., Zhang L., Wyatt S.B. Associations of fast food restaurant availability with dietary intake and weight among African Americans in the Jackson Heart Study, 2000–2004. American Journal of Public Health. 2011;101(S1):S301–S309. doi: 10.2105/AJPH.2010.300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch J.A., DeVries D.N., Brauer M., Frank L.D., Winters M. Impact of new rapid transit on physical activity: A meta-analysis. Preventive Medicine Reports. 2018 doi: 10.1016/j.pmedr.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch J.A., Diez Roux A.V., Moore K.A., Evenson K.R., Rodriguez D.A. Change in walking and body mass index following residential relocation: The multi-ethnic study of atherosclerosis. American Journal of Public Health. 2014;104(3):e49–e56. doi: 10.2105/AJPH.2013.301773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch J.A., Moore K.A., Barrientos‐Gutierrez T., Brines S.J., Zagorski M.A., Rodriguez D.A., Diez Roux A.V. Built environment change and change in BMI and waist circumference: Multi‐ethnic S tudy of A therosclerosis. Obesity. 2014;22(11):2450–2457. doi: 10.1002/oby.20873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyt L.T., Kushi L.H., Leung C.W., Nickleach D.C., Adler N., Laraia B.A., Yen I.H. Neighborhood influences on girls' obesity risk across the transition to adolescence. Pediatrics. 2014 doi: 10.1542/peds.2014-1286. (peds. 2014-1286) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurvitz P.M., Moudon A.V. Home versus nonhome neighborhood: Quantifying differences in exposure to the built environment. American Journal of Preventive Medicine. 2012;42(4):411–417. doi: 10.1016/j.amepre.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurvitz P.M., Moudon A.V., Kang B., Saelens B.E., Duncan G.E. Emerging technologies for assessing physical activity behaviors in space and time. Frontiers in Public Health. 2014;2:2. doi: 10.3389/fpubh.2014.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J.E., Doescher M.P., Jerant A.F., Hart L.G. A national study of obesity prevalence and trends by type of rural county. Journal of Rural Health. 2005;21(2):140–148. doi: 10.1111/j.1748-0361.2005.tb00074.x. [DOI] [PubMed] [Google Scholar]
- James P., Hart J.E., Arcaya M.C., Feskanich D., Laden F., Subramanian S. Neighborhood self-selection: The role of pre-move health factors on the built and socioeconomic environment. International Journal of Environmental Research and Public Health. 2015;12(10):12489–12504. doi: 10.3390/ijerph121012489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao J., Drewnowski A., Moudon A.V., Aggarwal A., Oppert J.-M., Charreire H., Chaix B. The impact of area residential property values on self-rated health: A cross-sectional comparative study of Seattle and Paris. Preventive Medicine Reports. 2016;4:68–74. doi: 10.1016/j.pmedr.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao J., Moudon A., Kim S., Hurvitz P., Drewnowski A. Health implications of adults' eating at and living near fast food or quick service restaurants. Nutrition Diabetes. 2015;5(7):e171. doi: 10.1038/nutd.2015.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao J., Moudon A.V., Kim S.Y., Hurvitz P.M., Drewnowski A. Health Implications of Adults' Eating at and Living near Fast Food or Quick Service Restaurants. Nutrition Diabetes. 2015;5:e171. doi: 10.1038/nutd.2015.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao J., Moudon A.V., Ulmer J., Hurvitz P.M., Drewnowski A. How to identify food deserts: Measuring physical and economic access to supermarkets in King County, Washington. American Journal of Public Health. 2012;102(10):e32–e39. doi: 10.2105/AJPH.2012.300675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joost S., Duruz S., Marques-Vidal P., Bochud M., Stringhini S., Paccaud F., Waeber G. Persistent spatial clusters of high body mass index in a Swiss urban population as revealed by the 5-year GeoCoLaus longitudinal study. BMJ Open. 2016;6(1):e010145. doi: 10.1136/bmjopen-2015-010145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaczynski A.T., Besenyi G.M., Stanis S.A.W., Koohsari M.J., Oestman K.B., Bergstrom R., Reis R.S. Are park proximity and park features related to park use and park-based physical activity among adults? Variations by multiple socio-demographic characteristics. International Journal of Behavioral Nutrition and Physical Activity. 2014;11(1):146. doi: 10.1186/s12966-014-0146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kestens Y., Thierry B., Shareck M., Steinmetz-wood M., Chaix B. Integrating activity spaces in health research: Comparing the VERITAS activity space questionnaire with 7-day GPS tracking and prompted recall. Spatial and Spatio-temporal Epidemiology. 2018;25:1–9. doi: 10.1016/j.sste.2017.12.003. [DOI] [PubMed] [Google Scholar]
- Laska M.N., Hearst M.O., Forsyth A., Pasch K.E., Lytle L. Neighbourhood food environments: Are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutrition. 2010;13(11):1757–1763. doi: 10.1017/S1368980010001564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leal C., Chaix B. The influence of geographic life environments on cardiometabolic risk factors: A systematic review, a methodological assessment and a research agenda. Obesity Reviews. 2011;12(3):217–230. doi: 10.1111/j.1467-789X.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- Lee C., Moudon A.V. Physical activity and environment research in the health field: Implications for urban and transportation planning practice and research. Journal of Planning Literature. 2004;19(2):147–181. [Google Scholar]
- Lee C., Moudon A.V. The 3Ds+ R: Quantifying land use and urban form correlates of walking. Transportation Research Part D: Transport and Environment. 2006;11(3):204–215. [Google Scholar]
- Lee C., Moudon A.V. Correlates of walking for transportation or recreation purposes. Journal of Physical Activity and Health. 2006;3(s1):S77–S98. doi: 10.1123/jpah.3.s1.s77. [DOI] [PubMed] [Google Scholar]
- Lee C., Moudon A.V., Courbois J.-Y.P. Built environment and behavior: Spatial sampling using parcel data. Annals of Epidemiology. 2006;16(5):387–394. doi: 10.1016/j.annepidem.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Lee I-Min. The built environment and physical activity levels: The Harvard Alumni Health Study. American Journal of Preventive Medicine. 2009;37(4):293–298. doi: 10.1016/j.amepre.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung C.W., Laraia B.A., Kelly M., Nickleach D., Adler N.E., Kushi L.H., Yen I.H. The influence of neighborhood food stores on change in young girls' body mass index. American Journal of Preventive Medicine. 2011;41(1):43–51. doi: 10.1016/j.amepre.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F., Harmer P., Cardinal B.J., Bosworth M., Johnson-Shelton D. Obesity and the built environment: Does the density of neighborhood fast-food outlets matter? American Journal of Health Promotion. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippert A.M. Stuck in unhealthy places: How entering, exiting, and remaining in poor and nonpoor neighborhoods is associated with obesity during the transition to adulthood. Journal of Health and Social Behavior. 2016;57(1):1–21. doi: 10.1177/0022146515627682. [DOI] [PubMed] [Google Scholar]
- Lovasi G.S., Grady S., Rundle A. Steps forward: Review and recommendations for research on walkability, physical activity and cardiovascular health. Public Health Reviews. 2011;33(2):484. doi: 10.1007/BF03391647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovasi G.S., Moudon A.V., Pearson A.L., Hurvitz P.M., Larson E.B., Siscovick D.S., Psaty B.M. Using built environment characteristics to predict walking for exercise. International Journal of Health Geographics. 2008;7(1):10. doi: 10.1186/1476-072X-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovasi G.S., Schwartz-Soicher O., Quinn J.W., Berger D.K., Neckerman K.M., Jaslow R., Rundle A. Neighborhood safety and green space as predictors of obesity among preschool children from low-income families in New York City. Preventive Medicine. 2013;57(3):189–193. doi: 10.1016/j.ypmed.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig J., Sanbonmatsu L., Gennetian L., Adam E., Duncan G.J., Katz L.F., Whitaker R.C. Neighborhoods, obesity, and diabetes—a randomized social experiment. New England Journal of Medicine. 2011;365(16):1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald J.M., Stokes R.J., Cohen D.A., Kofner A., Ridgeway G.K. The effect of light rail transit on body mass index and physical activity. American Journal of Preventive Medicine. 2010;39(2):105–112. doi: 10.1016/j.amepre.2010.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S., Ellaway A., Cummins S. Place effects on health: How can we conceptualise, operationalise and measure them? Social Science Medicine. 2002;55(1):125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Macintyre S., McKay L., Der G., Hiscock R. Socio-economic position and health: What you observe depends on how you measure it. Journal of Public Health. 2003;25(4):288–294. doi: 10.1093/pubmed/fdg089. [DOI] [PubMed] [Google Scholar]
- Mayne S.L., Auchincloss A.H., Michael Y.L. Impact of policy and built environment changes on obesity‐related outcomes: A systematic review of naturally occurring experiments. Obesity Reviews. 2015;16(5):362–375. doi: 10.1111/obr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack G.R. Neighbourhood built environment characteristics associated with different types of physical activity in Canadian adults. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice. 2017;37(6):175–185. doi: 10.24095/hpcdp.37.6.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellor J.M., Dolan C.B., Rapoport R.B. Child body mass index, obesity, and proximity to fast food restaurants. International Journal of Pediatric Obesity. 2011;6(1):60–68. doi: 10.3109/17477161003777433. [DOI] [PubMed] [Google Scholar]
- Michimi A., Wimberly M.C. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. International Journal of Health Geographics. 2010;9(1):49. doi: 10.1186/1476-072X-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell Hess P., Vernez Moudon A., Logsdon M. Measuring land use patterns for transportation research. Transportation Research Record: Journal of the Transportation Research Board. 2001;(1780):17–24. [Google Scholar]
- Moore L.V., Diez Roux A.V., Nettleton J.A., Jacobs D.R., Jr Associations of the local food environment with diet quality—a comparison of assessments based on surveys and geographic information systems: The multi-ethnic study of atherosclerosis. American Journal of Epidemiology. 2008;167(8):917–924. doi: 10.1093/aje/kwm394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K., Roux A.V.D., Wing S. Supermarkets, other food stores, and obesity: The atherosclerosis risk in communities study. American Journal of Preventive Medicine. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Morland K., Wing S., Roux A.D. The contextual effect of the local food environment on residents' diets: The atherosclerosis risk in communities study. American Journal of Public Health. 2002;92(11):1761–1768. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K.B., Evenson K.R. Obesity prevalence and the local food environment. Health Place. 2009;15(2):491–495. doi: 10.1016/j.healthplace.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moudon A., Hess P., Snyder M., Stanilov K. Effects of site design on pedestrian travel in mixed-use, medium-density environments. Transportation Research Record: Journal of the Transportation Research Board. 1997;(1578):48–55. [Google Scholar]
- Moudon A.V., Cook A.J., Ulmer J., Hurvitz P.M., Drewnowski A. A neighborhood wealth metric for use in health studies. American Journal of Preventive Medicine. 2011;41(1):88–97. doi: 10.1016/j.amepre.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moudon A.V., Drewnowski A., Duncan G.E., Hurvitz P.M., Saelens B.E., Scharnhorst E. Characterizing the food environment: Pitfalls and future directions. Public Health Nutrition. 2013;16(7):1238–1243. doi: 10.1017/S1368980013000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moudon A.V., Lee C., Cheadle A.D., Garvin C., Johnson D.B., Schmid T.L., Weathers R.D. Attributes of environments supporting walking. American Journal of Health Promotion. 2007;21(5):448–459. doi: 10.4278/0890-1171-21.5.448. [DOI] [PubMed] [Google Scholar]
- Moudon A.V., Sohn D., Kavage S.E., Mabry J.E. Transportation-efficient land use mapping index (TELUMI), a tool to assess multimodal transportation options in metropolitan regions. International Journal of Sustainable Transportation. 2011;5(2):111–133. [Google Scholar]
- Nelson N.M., Woods C.B. Obesogenic environments: Are neighbourhood environments that limit physical activity obesogenic? Health Place. 2009;15(4):917–924. doi: 10.1016/j.healthplace.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Nichols G.A., Desai J., Lafata J.E., Lawrence J.M., O’Connor P.J., Pathak R.D., Silverman B.G. Construction of a multisite DataLink using electronic health records for the identification, surveillance, prevention, and management of diabetes mellitus: The SUPREME-DM project. Preventing Chronic Disease. 2012;9 doi: 10.5888/pcd9.110311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell-Wiley T.M., Ayers C., Agyemang P., Leonard T., Berrigan D., Ballard-Barbash R., Hoehner C.M. Neighborhood-level socioeconomic deprivation predicts weight gain in a multi-ethnic population: Longitudinal data from the Dallas Heart Study. Preventive Medicine. 2014;66:22–27. doi: 10.1016/j.ypmed.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell-Wiley T.M., Cooper-McCann R., Ayers C., Berrigan D., Lian M., McClurkin M., Leonard T. Change in neighborhood socioeconomic status and weight gain: Dallas Heart Study. American Journal of Preventive Medicine. 2015;49(1):72–79. doi: 10.1016/j.amepre.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell L.M., Auld M.C., Chaloupka F.J., O’Malley P.M., Johnston L.D. Associations between access to food stores and adolescent body mass index. American Journal of Preventive Medicine. 2007;33(4):S301–S307. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Rachele J.N., Kavanagh A., Brown W.J., Healy A.M., Turrell G. Neighborhood disadvantage and body mass index: A study of residential relocation. American Journal of Epidemiology. 2018:kwx390. doi: 10.1093/aje/kwx390. [DOI] [PubMed] [Google Scholar]
- Rehm C.D., Moudon A.V., Hurvitz P.M., Drewnowski A. Residential property values are associated with obesity among women in King County, WA, USA. Social Science Medicine. 2012;75(3):491–495. doi: 10.1016/j.socscimed.2012.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rummo P.E., Guilkey D.K., Shikany J.M., Reis J.P., Gordon-Larsen P. How do individual-level sociodemographics and neighbourhood-level characteristics influence residential location behaviour in the context of the food and built environment? Findings from 25 years of follow-up in the CARDIA Study. Journal of Epidemiology and Community Health. 2017;71(3):261–268. doi: 10.1136/jech-2016-207249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rundle A., Neckerman K.M., Freeman L., Lovasi G.S., Purciel M., Quinn J., Weiss C. Neighborhood food environment and walkability predict obesity in New York City. Environmental Health Perspectives. 2008;117(3):442–447. doi: 10.1289/ehp.11590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rundle A., Quinn J., Lovasi G., Bader M.D., Yousefzadeh P., Weiss C., Neckerman K. Associations between body mass index and park proximity, size, cleanliness, and recreational facilities. American Journal of Health Promotion. 2013;27(4):262–269. doi: 10.4278/ajhp.110809-QUAN-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelens B.E., Sallis J.F., Black J.B., Chen D. Neighborhood-based differences in physical activity: An environment scale evaluation. American Journal of Public Health. 2003;93(9):1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelens B.E., Sallis J.F., Black J.B., Chen D. Neighborhood-based differences in physical activity: An environment scale evaluation. American Journal of Public Health. 2003;93(9):1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey J.R., Horel S. Neighborhood socioeconomic deprivation and minority composition are associated with better potential spatial access to the ground-truthed food environment in a large rural area. Journal of Nutrition. 2008;138(3):620–627. doi: 10.1093/jn/138.3.620. [DOI] [PubMed] [Google Scholar]
- Sharp G., Denney J.T., Kimbro R.T. Multiple contexts of exposure: Activity spaces, residential neighborhoods, and self-rated health. Social Science Medicine. 2015;146:204–213. doi: 10.1016/j.socscimed.2015.10.040. [DOI] [PubMed] [Google Scholar]
- Smoyer-Tomic K.E., Spence J.C., Amrhein C. Food deserts in the prairies? Supermarket accessibility and neighborhood need in Edmonton, Canada. The Professional Geographer. 2006;58(3):307–326. [Google Scholar]
- Spoon, C. (2012). Infographic: The Role of Parks and Recreation in Promoting Physical Activity. from 〈https://activelivingresearch.org/blog/2012/10/infographic-role-parks-and-recreation-promoting-physical-activity〉.
- Stafford M., Brunner E.J., Head J., Ross N.A. Deprivation and the development of obesity: A multilevel, longitudinal study in England. American Journal of Preventive Medicine. 2010;39(2):130–139. doi: 10.1016/j.amepre.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Stafford M., Cummins S., Ellaway A., Sacker A., Wiggins R.D., Macintyre S. Pathways to obesity: Identifying local, modifiable determinants of physical activity and diet. Social Science Medicine. 2007;65(9):1882–1897. doi: 10.1016/j.socscimed.2007.05.042. [DOI] [PubMed] [Google Scholar]
- Stark J.H., Neckerman K., Lovasi G.S., Konty K., Quinn J., Arno P., Bader M.D. Neighbourhood food environments and body mass index among New York City adults. Journal of Epidemiology and Community Health. 2013;67(9):736–742. doi: 10.1136/jech-2013-202354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart O.T., Moudon A.V., Fesinmeyer M.D., Zhou C., Saelens B.E. The association between park visitation and physical activity measured with accelerometer, GPS, and travel diary. Health place. 2016;38:82–88. doi: 10.1016/j.healthplace.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treuhaft, S., & Karpyn, A. (2010). The Grocery Gap: Who Has Access to Healthy Food and Why It Matters.
- Van Cauwenberg J., Cerin E., Timperio A., Salmon J., Deforche B., Veitch J. Park proximity, quality and recreational physical activity among mid-older aged adults: Moderating effects of individual factors and area of residence. International Journal of Behavioral Nutrition and Physical Activity. 2015;12(1):46. doi: 10.1186/s12966-015-0205-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan A.F., Voorhees C.C., Clifton K., Burnier C. Do you see what I see?–Correlates of multidimensional measures of neighborhood types and perceived physical activity–related neighborhood barriers and facilitators for urban youth. Preventive Medicine. 2010;50:S18–S23. doi: 10.1016/j.ypmed.2009.08.015. [DOI] [PubMed] [Google Scholar]
- Zandbergen P.A. Ensuring confidentiality of geocoded health data: Assessing geographic masking strategies for individual-level data. Advances in Medicines. 2014;2014:567049. doi: 10.1155/2014/567049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk S.N., Mentz G., Schulz A.J., Johnson-Lawrence V., Gaines C.R. Longitudinal associations between observed and perceived neighborhood food availability and body mass index in a multiethnic urban sample. Health Education Behavior. 2017;44(1):41–51. doi: 10.1177/1090198116644150. [DOI] [PMC free article] [PubMed] [Google Scholar]