INTRODUCTION
Scale-up of access to anti-retroviral therapy (ART) in low-income countries has, by many measures, been one of the signal successes of global public health. The magnitude and impact of this scale-up has been remarkable, saving the lives of millions of persons living with HIV (PLWH), and leading to improvements in overall health and well-being [1]. To fulfill the potential of ART to enhance health at the population-level, however, it is necessary to recognize that health is produced by communities and health systems, not just by individuals. Growing recognition of the need for structural interventions to improve adherence and HIV care has motivated research and advocacy on how addressing poverty, housing insecurity, and food insecurity could improve ART outcomes, but there has been little exploration of the connections between HIV care and inadequate water/sanitation.
Inequities in access to safe water and sanitation rank as one of the great moral and technological failures in global health. Recent estimates from UNICEF/WHO suggest that 780 million people lack access to improved water sources and 2.5 billion lack improved sanitation [2]. Inadequate water and sanitation account for 4% of all deaths and 5.7% of the total disease burden worldwide [3], and in developing countries one-third of deaths are associated with the consumption of contaminated water [4]. This issue is particularly acute in sub-Saharan Africa, where only 19 of 50 countries are on track to meet the 2015 Millennium Development Goal of reducing the proportion of people without sustainable access to safe drinking water and basic sanitation [2]. Despite significant improvements, and varying degrees of progress, this region lags behind most of the world with only about 61% coverage for improved water supply and 30% coverage for sanitation [2].
Insufficient access to water/sanitation challenges PLWH in multiple ways: insufficient coverage has been shown to affect hygiene practices, like the ability to bathe and wash soiled clothes and linens; to increase caregiver burden; to limit the ability to swallow medications safely; and to exacerbate poor HIV health-related outcomes, especially opportunistic infections, like diarrheal and skin diseases, which lead to greater morbidity and mortality among PLWH [5–10]. In addition to being necessary for health and the activities of daily living, better water and sanitation can enhance the comfort and dignity of PLWH [10]. PLWH are more prone to certain pathogens with about 90% of PLWH in Africa suffering from chronic diarrhea stemming from water-borne infections [10]. Households with PLWH may need an additional 20 to 80 liters of water per day, depending on the severity of diarrhea, for cleaning and sanitation purposes [9]. Studies have also noted that access to potable water, and water more generally, may be an important predictor of ART adherence and HIV outcomes [11–13].
Improvements in water and sanitation can also benefit household members of PLWH [13], especially caregivers who may face tremendous burdens as a result of providing HIV care. Women and children bear a disproportionate amount of the time and resource burden of both water/sanitation management and caring for PLWH. The physical, emotional, and opportunity costs to women are substantial, and while the social arrangements that place women as primary resource managers and caregivers within the home are often treated as “natural”, they are part of a broader social order organized around gender that structures both labor and power [14].
Gender, as conceptualized by Connell [14], encompasses more than just ‘gender roles’ (shared ideas about how appropriate and valued behavior differs for men and women), which are discussed fairly frequently in biomedical research [15–18]. Connell proposes instead that social institutions (such as family, health care systems, schools) have gender regimes that are comprised of the gendered division of labor, gendered access to power (both physical power and decision-making capacity), and cathexis (gendered ideals for emotion and social relations). This broad notion of gender has been applied with considerable power in research on HIV prevention [19, 20].
In this paper, we discuss the ways that gender overlaps with both water and sanitation and with HIV caregiving, applying Connell’s theorization to explore the full range of ways in which HIV caregiving and water and sanitation practices are shaped by gender relations and gendered social structures. We then propose a conceptual framework that integrates Connell’s theory of gender [14] with a public health approach of systems science, which frames public health problems as embedded in larger social systems and emphasizes the intertwining of multiple social determinants with diverse health outcomes [21]. Together, gender theory and systems science allow us to describe the gendered pathways between water/sanitation and HIV treatment outcomes and to articulate how improved water/sanitation would create positive synergies in the household and community production of health.
GENDERED BURDEN OF WATER AND SANITATION
Considering water/sanitation practices as a gendered institution means attending to the allocation of work - that is, the gendered division of labor - but also to questions of power and social ideals. A substantial body of research has shown that globally, women are responsible for the majority of domestic water work. At the household level, water work is largely directed toward drinking, cooking, cleaning and hygiene purposes and involves water collection, storage and treatment, maintenance of sanitation facilities, and small-scale production activities for family income-generation [22].
Women spend hours each day fetching water and travel great distances, sometimes multiple times per day, to reach water sources [23–25]. The physical strain associated with such work may negatively impact women’s health [23]: in some mountainous regions of East Africa, women spend up to 27% of their caloric intake procuring water [26]. Collecting water can be particularly burdensome for elderly women or young girls when water supply points are far away, pump handles are high or heavy, and if they are ill or weak [27]. Physical strain is further compounded by heat and long queues at water sources [25]. Men play a less prominent role in domestic water management. For example, in Tanzania 13% of boys fetched water, while only 9% of men (fathers) were involved, and only where distances to water sources were deemed too great for women to travel [23].
While water is necessary for the social production of health, access to water for commercial purposes can bring desperately-needed economic resources into the household through livestock-watering, brick-molding, subsistence-farming, dairying, and construction [25, 28]. In addition, whereas women are often depicted in policy and programs as less involved in the commercial use of water, to the contrary, studies demonstrate that women play multiple roles in water, and are frequently the users, managers and guardians of household water as well as key players in income-generating activities [25, 28]. Women’s access to water for productive activities is limited by water scarcity, access to resources like land, credit, training, and transportation, and their primary social obligations to care for their home and family [25, 29].
Women’s water-related labor also has opportunity costs as it competes with other domestic and economic work, reduces the time that women have available for other activities, makes it difficult for girls to continue their schooling [30], and prevents women from caring for themselves or family and from engaging in remunerative activities [27, 29]. Water work can also present the risk of rape or violence if they are required to go to a remote place to fetch water [27].
A focus only on gendered patterns of labor, however, fails to fully capture the ways that the labor associated with water is gendered. Within households, women may have less power than men to make decisions regarding water, including decisions about the allocation of water resources, and may be poorly positioned to negotiate for a more equitable division of labor [23, 24]. While improved water/sanitation is likely to be a high priority for women, household-level power inequalities may make women either reluctant or unable to suggest allocating a greater portion of domestic resources to improved access to water/sanitation, especially since the expense would largely benefit them by decreasing their household work burden [24].
GENDERED BURDEN OF HIV CARE
There are similar gendered inequalities in the allocation of labor and time in HIV caregiving. While the importance of gender in relation to HIV risk has received substantial attention [31, 32], our focus here is on the gendered nature of informal HIV care, which shapes both the burden on HIV caregivers and the burden to social systems. The improved health outcomes produced by the remarkable scale-up of HIV care and treatment in many parts of the world has fundamentally altered the nature of caregiving by family members. While prior to availability of HIV care and treatment, family and home-based caregiving was largely focused on end of life care during advanced HIV disease stages with largely homebound patients, currently this is centered on support for access and retention in care and for adherence with treatment. Nonetheless, family caregivers lack training, bear the physical and emotional burdens associated with caregiving, and face high opportunity costs [33–35]. For those without access to clinic-based care, home-based care plays a critical role in the HIV epidemic; indeed, for many, care by family in the home is the only option [36, 37]. Women are the primary caregivers: studies show that in Southern Africa, 78% to 94% of HIV caregivers were female relatives [35]. Men on occasion take up the responsibility of caring for ill family members [38], but less commonly, and the limited research on this topic suggests that this occurs primarily when women are unavailable [33, 39]. Men often lack the knowledge, skills and confidence to do so effectively, and perform different activities than women, like instrumental activities of daily living [35, 36, 40]. Reluctance by men to provide such care may stem from perception that women are “natural” caregivers, and that it is not a masculine activity [35, 41].
A great deal of research demonstrates the considerable physical demands on caregivers, including pain, increased risk of infections, and overall higher morbidity and mortality [8, 35, 41–43]. Care can involve bathing and carrying patients, toileting, mood management, emotional support, and assistance with instrumental activities of daily living [8, 33, 35, 44]. These activities are likely made more difficult by insufficient access to clean water in large quantities and proper sanitation.
The mental health of caregivers is affected as well, as watching family members suffer and die and facing anxiety about the patient’s well-being and the ability to provide sufficient care while navigating the challenges presented by stigma and discrimination [8, 35, 41, 45], can all produce psychological distress [46]. Caregiving is also disruptive to social life and caregivers report that they lose social contact and support, facing stigma from close family members and their community [8, 41, 42, 46]. While these processes can certainly affect men, they are not involved in care to the same extent as women and men are not always present in HIV-affected households. It should also be noted that women’s lower status relative to men and gendered household power dynamics mean that women may give priority to the needs of male household members, ignoring their own health [44].
HIV caregivers are also at risk of losing their jobs or hours of work, which can dramatically decrease income and exacerbate poverty [35, 41, 46]. Many caregivers become financially dependent on support from family, friends, and neighbors [41], but relatives are not always willing or able to help, limiting caregivers’ ability to provide food or medications [47]. For younger caregivers, time spent on care can interfere with schooling [33, 35]. As men fall ill or die, economic burdens increasingly fall on women, who have limited access to resource-generating opportunities [34, 35], resulting in increases in women’s economic marginality [41]. It must be noted, however, that these effects are greatly mitigated by access to ARTs, as they have dramatic effects on improved wellness for PLWH and their ability to care for themselves and their families [48].
It is important to note, however, that a fully gendered analysis of HIV care acknowledges that men too are gendered subjects; in contrast to men’s greater access to informal home-based care, women tend to have better access to formal systems of health care, are more likely to seek health care, and more likely to receive HIV treatment [49–53]. Nonetheless, it is evident that the work of water/sanitation management and the work of HIV care intersect to disproportionately affect the lives of women.
INTEGRATING SYSTEMS SCIENCE AND GENDER THEORY
To conceptualize the pathways between gender, water/sanitation and HIV care and treatment, we draw upon the systems science approach and the social science of gender. In particular, we take two messages from systems science. First, moving away from a ‘single-exposure, single-outcome’ approach to thinking about public health problems encourages us to consider the potential impacts of improved water and sanitation on HIV care outcomes [21, 54]. The goal is not to justify improved access to water and sanitation, since ample evidence already exists for the substantial population-level benefits of safer water and sanitation; rather, it is to provoke those in the field of HIV care and policy to think more broadly about possible population-level, non-biomedical interventions to improve HIV-related health outcomes. Second, systems science emphasizes the web of interconnected social factors that shape health outcomes. Our use of gender is emblematic of this approach: focusing on the complex processes through which health is created, we have in this paper highlighted gender as one specific element of social organization, and used a social science theorization of gender as a heuristic to more fully conceptualize the pathways between HIV and water/sanitation.
Grounded in this integration of gender and systems science, we propose that the potential impact of improving water and sanitation on HIV treatment outcomes only comes clearly into focus by considering the profound ways in which both home-based HIV care and water/sanitation are generally considered to be women’s activities. We further propose that water/sanitation is an important leverage point for enhancing HIV treatment outcomes, but we raise salient questions about the form of delivery of such interventions. There are ongoing debates in public health about the balance between individual-level behavior change interventions and broader population-level structural interventions [55–58]. In terms of water/sanitation, economic and infrastructural challenges have meant that water/sanitation interventions over the past few decades have focused primarily on behavior change and improvements within households. Yet, when we take a gendered perspective on water and HIV, we question whether household-level interventions - for instance, improved water collection, storage vessels, and access to individual-level devices for chemical and mechanical water purification - would have the same impact as the development of effective water/sanitation systems that are designed to improve access to clean water for entire communities, especially in areas hit hardest by HIV and shortages of potable water and where the work of both falls primarily on women and girls.
TOWARDS A FRAMEWORK ON GENDER, WATER AND SANITATION, AND HIV
Improvements in water/sanitation could lead to improved HIV outcomes for PLWH, reductions in the gendered burden of care and resource management, and have an impact on more distal outcomes at the population level. As seen in Figure 1, inadequate water/sanitation can aggravate vulnerabilities and health outcomes associated with HIV, impede proper treatment and care, and increase the socioeconomic impacts of HIV [59]. Due to the greater water needs of PLWH, improved water and sanitation could lead directly to better HIV outcomes by enhancing people’s ability to be adherent to ART, reducing co-morbidities, improving infant feeding practices, and increasing the dignity of those who are ill. At the same time, better water/sanitation could ease the burden of care on women, particularly if it were made available via infrastructure as opposed to household-level interventions that may still involve considerable work on the part of women. Reducing the burden of care that women face would allow them to have more time to devote to higher quality care for PLWH, income-generating work, and to keeping children in school. These pathways, in turn, have a synergistic impact on the health and economic situation of individuals and families affected by HIV. Infrastructural improvements to water/sanitation could also build local economies, reduce the enteric-disease related burden on health systems, enhance the ability of health systems to care for PLWH, improve overall individual and community health, and contribute to longer-term goals and concerns around the provision of HIV care and treatment through the strengthening of formal and informal systems of care.
Figure 1:
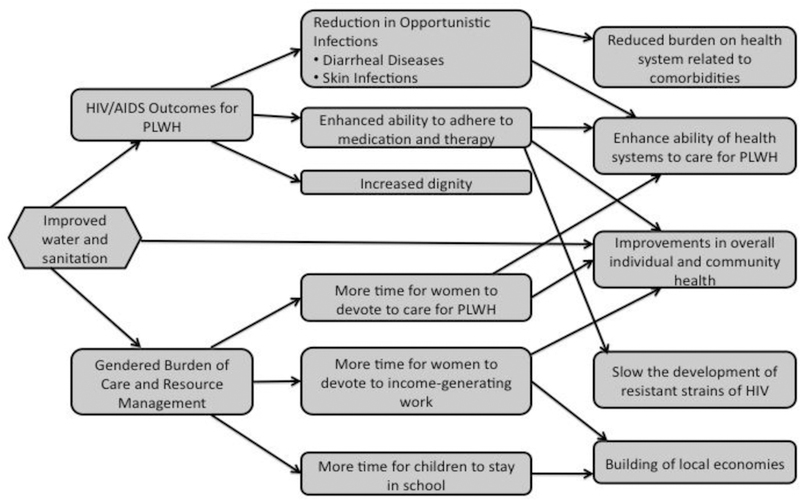
Pathways Between Gender, Water and Sanitation, and HIV
Based on this framework, we posit that community level water/sanitation programs should be considered part of the basic package of care for PLWH, particularly in areas where there is overlap between high HIV prevalence and inadequate systems of water/sanitation, as evident in sub-Saharan Africa (Figure 2). In this region, only a quarter of the population had water on their premises in 2010 and it is home to about 22.5 million people living with HIV, which in 2009 represented about 68% of the global HIV burden [60]. Further, in sub-Saharan Africa, women or girls are responsible for water collection in 71% of all households and enormous amounts of time and labor are expended to manage water/sanitation resources [2].
Figure 2:
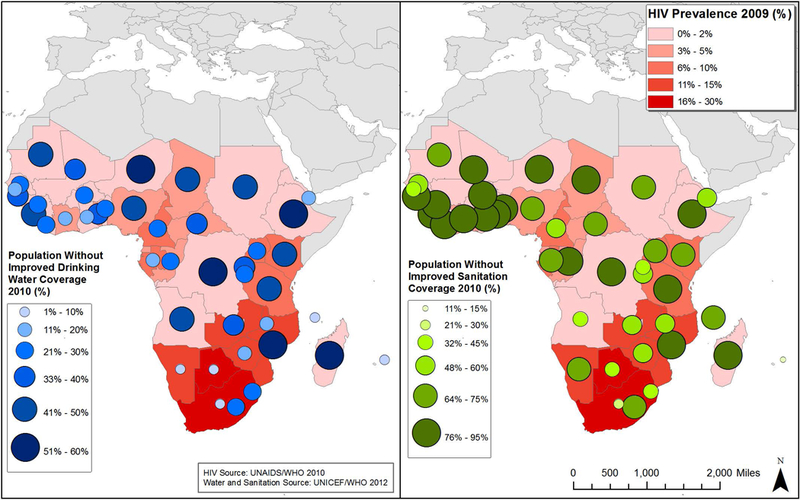
HIV Prevalence and Water and Sanitation Coverage in sub-Saharan Africa
Infrastructural improvements in water and sanitation, beyond individual-level interventions, would, no doubt, represent a substantial cost - a cost that is perhaps difficult to consider given the magnitude of necessary commitments to sustaining and expanding access to ART. Structural interventions of this nature could include building latrines, investments in sanitation systems in urban and periurban areas, digging wells, and ideally, the construction of water purification plants where appropriate. Our assessment of the literature, however, suggests that the potential positive synergies of investing in water and sanitation in communities in which access to ART is being expanded would be significant, with health multiplying effects that go far beyond the individual level and instead have an impact on entire communities.
As we describe above, there are multiple paths through which improved water/sanitation could potentially improve HIV-related outcomes; however, there is a need for new and better ways to reduce the gender burden of water/sanitation and HIV care, to increase access to improved water/sanitation sources, and to improve HIV treatment outcomes. In order to make this a reality, however, there is a need for greater coordination among water/sanitation and HIV researchers and programmers to develop mutually beneficial and effective interventions. Table 1 shows priorities for further research in this area.
Table 1:
Priority research areas on gender, water and HIV
| 1) Association of access to clean water/sanitation, ART adherence, comorbidities, and the role of gender in HIV-related outcomes. |
| 2) Mathematical modeling to assess the potential impact of improved water/sanitation on HIV-related outcomes. |
| 3) Effect of water/sanitation interventions on HIV-related health and social outcomes. |
| 4) Role of men in household production of health for both water/sanitation and HIV and development of interventions to promote and support such a role. |
| 5) Evolution of gender roles in HIV care with expansion of HIV care and treatment |
CONCLUSIONS
In both HIV caregiving and water/sanitation management, the responsibility for improvements has been largely delegated to households and individuals, with a disproportionate burden falling on women and girls. In the context of HIV programs, home-based care has been utilized as a less-costly and more culturally appropriate alternative to hospital and terminal care and as a means to reduce the strain on overwhelmed health systems. This analysis, though, fails to consider the substantial burden on predominantly female caregivers and the value of their unpaid labor [35]. In water/sanitation, women’s instrumental role in resource management is also frequently taken for granted. While behavioral interventions can be beneficial to the health of the household, they do not necessarily reduce the work of water management itself, leaving the very real potential for women’s workloads to increase rather than easing existing burdens. Boiling, purifying, or otherwise filtering water, or walking farther to fetch water that is clean rather than using closer-by water that is dirty, may be less unpleasant work than caring for someone suffering the health consequences of inadequate water/sanitation—but it is work nonetheless. Rather than relying on programs that push the work of public health onto the public, particularly women and children, water/sanitation needs to move beyond the home to the population level. This not only has the power to reach the greatest number of people, but also begins to remedy one of public health’s greatest failures: the lack of basic infrastructure provision in the form of water and sanitation.
The gendered burdens of HIV care and water/sanitation management do not exist in isolation from each other. By examining HIV care and water/sanitation management in relation to the gendered nature of labor, power, and ideals for emotion and social relations, we demonstrate how these processes and their interconnections shape and are shaped by complex social systems. We further demonstrate that the gendered burdens of resource management and HIV care are exponentially increased by the lack of water infrastructure and by overburdened health systems. Similarly, HIV treatment outcomes are shaped by access to care and adequate water/sanitation. Taken together, the “perfect storm” of the intertwining burdens of HIV care and inadequate water/sanitation slows progress towards both improved HIV outcomes and gender equity. Thus, funding for water/sanitation cannot be at the expense of funding for HIV treatment, but should instead complement it as it has the potential to both enhance health and alleviate women’s time burden. Tackling the intersections of water/sanitation, HIV, and gender will allow for a critical examination of the broader systems in which health and social relationships occur and this knowledge can then be used to design public health interventions that will work for all members of a community, rather than just create more work for some.
REFERENCES
- 1.PEPFAR. Celebrating Life: Fifth Annual Report to Congress on PEPFAR 2009.
- 2.UNICEF and World Health Organization. Progress on Drinking Water and Sanitation: 2012 Update. WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; 2012.
- 3.Pruss A, Kay D, Fewtrell L, Bartram J. Estimating the burden of disease from water, sanitation, and hygiene at a global level. Environ Health Perspect 2002. May;110(5):537–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. Guidelines for Drinking Water Quality, Second Edition Geneva: WHO; 1997. [Google Scholar]
- 5.UNAIDS. Report on the global AIDS Epidemic 2004.
- 6.Kiongo J The Millenium Development Goal on Poverty and the Links with Water Supply, Sanitation, Hygiene and HIV/AIDS: A case study from Kenya: IRC International Water and Sanitation Center 2005.
- 7.WaterAid. Assessment of the Adequacy of Water, Sanitation, and Hygiene Facilities in Resource-poor Areas of Nigeria in Relation to the Needs of Vulnerable People Abuja, Nigeria: WaterAid Nigeria; 2006. [Google Scholar]
- 8.Chimwaza AF, Watkins SC. Giving care to people with symptoms of AIDS in rural sub-Saharan Africa. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv 2004. October;16(7):795–807. [DOI] [PubMed] [Google Scholar]
- 9.Ngwenya BN, Kgathi DL. HIV/AIDS and access to water: A case study of home-based care in Ngamiland, Botswana. Physics and Chemistry of the Earth 2006(15–16):669–80. [Google Scholar]
- 10.Obi CL, Onabolu B, Momba MNBet al. The interesting cross-paths of HIV/AIDS and water in Southern Africa with special reference to South Africa. Water SA 2006. July;32(3):323–43. [Google Scholar]
- 11.Davies MA, Boulle A, Fakir T, Nuttall J, Eley B. Adherence to antiretroviral therapy in young children in Cape Town, South Africa, measured by medication return and caregiver self-report: a prospective cohort study. BMC Pediatr 2008. September;8:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy DA, Roberts KJ, Martin DJ, Marelich W, Hoffman D. Barriers to antiretroviral adherence among HIV-infected adults. Aids Patient Care STDS 2000. January;14(1):47–58. [DOI] [PubMed] [Google Scholar]
- 13.Lule JR, Mermin J, Ekwaru JP, et al. Effect of home-based water chlorination and safe storage on diarrhea among persons with human immunodeficiency virus in Uganda. Am J Trop Med Hyg 2005. November;73(5):926–33. [PubMed] [Google Scholar]
- 14.Connell R Gender and Power: Society, the Person and Sexual Politics Stanford: Stanford University Press; 1987. [Google Scholar]
- 15.Manji A, Pena R, Dubrow R. Sex, condoms, gender roles, and HIV transmission knowledge among adolescents in Leon, Nicaragua: implications for HIV prevention. AIDS Care 2007. September;19(8):989–95. [DOI] [PubMed] [Google Scholar]
- 16.O’Sullivan LF, Hoffman S, Harrison A, Dolezal C. Men, multiple sexual partners, and young adults’ sexual relationships: understanding the role of gender in the study of risk. Journal of Urban Health 2006. July;83(4):695–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santana MC, Raj A, Decker MR, La Marche A, Silverman JG. Masculine gender roles associated with increased sexual risk and intimate partner violence perpetration among young adult men. Journal of Urban Health 2006. July;83(4):575–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sarna A, Chersich M, Okal J, et al. Changes in sexual risk taking with antiretroviral treatment: influence of context and gender norms in Mombasa, Kenya. Culture, Health & Sexuality 2009. November;11(8):783–97. [DOI] [PubMed] [Google Scholar]
- 19.Hirsch J, Wardlow H, Smith D, Phinney H, Parikh S, Nathanson C. The Secret: Love, Marriage and HIV Nashville, Tennessee: Vanderbilt University Press; 2009. [Google Scholar]
- 20.Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav 2000. October;27(5):539–65. [DOI] [PubMed] [Google Scholar]
- 21.Leischow SJ, Milstein B. Systems Thinking and Modeling for Public Health Practice. Am J Public Health 2006. March;96(3):403–05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Women Ray I., Water and Development. Annu Rev Environ Resour 2007;32:421–49. [Google Scholar]
- 23.Buor D Water needs and women’s health in the Kumasi metropolitan area, Ghana. Health & Place 2004. March;10(1):85–103. [DOI] [PubMed] [Google Scholar]
- 24.Women Rathgeber E., Men, and Water-Resource Management in Africa. In: Rached E, Rathgeber E, Brooks D, editors. Water Management in Africa and the Middle East: Challenges and Opportunities: IDRC; 1996.
- 25.Upadhyay B Gendered livelihoods and multiple water use in North Gujarat. Agric Human Values 2005. Win;22(4):411–20. [Google Scholar]
- 26.Lewis N Safe Womanhood: A Discussion Paper. Toronto, ON: International Federation of Institutes for Advanced Study; 1994. [Google Scholar]
- 27.Wegelin-Schuringa M, Kamminga E. HIV/AIDS and Water, Sanitation and Hygiene: IRC International Thematic Overview Paper 2003.
- 28.Makoni FS, Manase G, Ndamba J. Patterns of domestic water use in rural areas of Zimbabwe, gender roles and realities. Physics and Chemistry of the Earth 2004;29:1291–94. [Google Scholar]
- 29.Sijbesma C, Verhagen J, Nanavaty R, James AJ. Impacts of domestic water supply on gender and income: results from a participatory study in a drought-prone region in Gujarat, India. Water Policy 2009;11(1):95–105. [Google Scholar]
- 30.Devnarain B, Matthias C. Poor access to water and sanitation: Consequences for girls at a rural school. Agenda: Empowering Women for Gender Equity 2011;25(2):27–34. [Google Scholar]
- 31.Dworkin S, Ehrhardt A. Going Beyond ABC to Include GEM (Gender Relations, Economic Contexts, and Migration Movements): Critical Reflections on Progress in the HIV/AIDS Epidemic. Am J Public Health 2007;97:13–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Higgins JA, Hoffman S, Dworkin SL. Rethinking Gender, Heterosexual Men, and Women’s Vulnerability to HIV/AIDS. Am J Public Health 2010. March;100(3):435–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kipp W, Tindyebwa D, Rubaale T, Karamagi E, Bajenja E. Family Caregivers in Rural Uganda: The Hidden Reality. Health Care for Women International 2007;28:856–71. [DOI] [PubMed] [Google Scholar]
- 34.Taylor L, Seeley J, Kajura E. Informal care for illness in rural southwest Uganda: the central role that women play. Health Transition Review 1996;6:49–56. [PubMed] [Google Scholar]
- 35.Akintola O Unpaid HIV/AIDS Care in Southern Africa: Forms, Context, and Implications Fem Econ 2008;14(4):117–47. [Google Scholar]
- 36.Akintola O A Gendered Analysis of the Burden of Care on Family and Volunteer Caregivers in Uganda and South Africa: Health Economics and HIV/AIDS Research Division (HEARD), University of KwaZuluNatal, Durban, South Africa: 2004. [Google Scholar]
- 37.Peacock D, Weston M. Men and Care in the Context of HIV and AIDS: Structure, Political Will and Greater Male Involvement Geneva: United Nations Division for the Advancement of Women; 2008, October 6–9 Contract No.: EGM/ESOR/2008/EP.1. [Google Scholar]
- 38.Peacock D, Stemple L, Sawires S, Coates TJ. Men, HIV/AIDS, and Human Rights. J Acquir Immune Defic Syndr 2009. July;51(Suppl 3):S119–S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Luker V AIDS and the burden of care: Mainstreaming gender or ‘main-themeing’ women? Development Bulletin 2004;64:78–81. [Google Scholar]
- 40.Akintola O Gendered Home-based Care: More Trouble for the Troubled. African Journal of AIDS Research 2006;5(3):237–47. [DOI] [PubMed] [Google Scholar]
- 41.Tarimo EAM, Kohi TW, Outwater A, Blystad A. Gender Roles and Informal Care for Patients With AIDS A Qualitative Study From an Urban Area in Tanzania. J Transcult Nurs 2009. January;20(1):61–68. [DOI] [PubMed] [Google Scholar]
- 42.Kipp W, Nkosi TM. Factors associated with the self-reported health status of female caregivers of AIDS patients. Western Journal of Nursing Research 2008. February;30(1):20–33. [DOI] [PubMed] [Google Scholar]
- 43.Bachmann MO, Booysen FLR. Health and economic impact of HIV/AIDS on South African households: a cohort study. BMC Public Health 2003. April;3:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bharat S, Aggleton P. Facing the challenge: household responses to HIV/AIDS in Mumbai, India. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV 1999. February;11(1):31–44. [DOI] [PubMed] [Google Scholar]
- 45.Feng MC, Feng JY, Chen TC, Lu PL, Ko NY, Chen YH. Stress, needs, and quality of life of family members caring for adults living with HIV/AIDS in Taiwan. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV 2009;21(4):482–89. [DOI] [PubMed] [Google Scholar]
- 46.Orner P Psychosocial impacts on caregivers of people living with AIDS. AIDS Care 2006;18(3):236–40. [DOI] [PubMed] [Google Scholar]
- 47.Seeley J, Kajura E, Bachengana C, Okongo M, Wagner U, Mulder D. The extended family and support for people with AIDS in a rural-population in Southwest Uganda - A safety net with holes. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV 1993;5(1):117–22. [DOI] [PubMed] [Google Scholar]
- 48.Beard J, Feeley F, Rosen S. Economic and quality of life outcomes of antiretroviral therapy for HIV/AIDS in developing countries: a systematic literature review. AIDS Care 2009;21(11):1343–56. [DOI] [PubMed] [Google Scholar]
- 49.Braitstein P BA, Nash D et al. Gender and the use of antiretroviral treatment in resource-constrained settings: findings from a multicenter collaboration. Journal of Women’s Health 2008;17:47–55. [DOI] [PubMed] [Google Scholar]
- 50.Chen SCC YJ, Harries AD, Bong CN, Kolola-Dzimadzi R, Tok TS, King CC, and Wang JD. Increased mortality of male adults with AIDS related to poor compliance to antiretroviral therapy in Malawi. Tropical Medicine & International Health 2008;13:513–19. [DOI] [PubMed] [Google Scholar]
- 51.Cornell ML MR, Kaplan L, Bekker G, and Wood R. The impact of gender and income on survival and retention in a South African antiretroviral therapy programme. Tropical Medicine & International Health 2009;14:722–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.ART-LINC Collaboration of the International Databases to Evaluate AIDS (IeDEA). Antiretroviral therapy in resource-limited settings 1996 to 2006: patient characteristics, treatment regimens and monitoring in Sub-Saharan Africa, Asia and Latin America. Tropical Medicine & International Health 2008;13:87–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mills E, Ford N, Mugyenyi P. Expanding HIV care in Africa: making men matter. Lancet 2009;374:275–76. [DOI] [PubMed] [Google Scholar]
- 54.Homer J, Hirsch G. System dynamics for modeling public health: background and opportunties. Am J Public Health 2006;96:452–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blankenship K, Friedman S, Dworkin S, Mantell J. Structural Interventions: Concepts, Challenges and Opportunities for Research. J Urban Health 2006;83(1):59–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carter RC, Tyrrel SF, Howsam P. The impact and sustainability of community water supply and sanitation programmes in developing countries. Water and Environment Journal 1999;13(4):292–96. [Google Scholar]
- 57.Green L, Kreuter M. Health promotion as public health strategy for the 1990s. Annu Rev Public Health 1990;11:319–34. [DOI] [PubMed] [Google Scholar]
- 58.Roberts M Public Health and Health Psychology: Two Cats of Kilkenny? Professional Psychology: Research and Practice 1987. April;18(2):145–49. [Google Scholar]
- 59.UNHABITAT. HIV/AIDS Checklist for Water and Sanitation Projects Nairobi: United Nations Human Settlements Programme; 2006. [Google Scholar]
- 60.UNAIDS. Global Report Fact Sheet: Sub-Saharan Africa 2010.


