Abstract
Objective:
To explore the relations between trauma exposure and anxiety and depression among college students, and to determine whether trait mindfulness may moderate these relations.
Participants:
Self-report survey data from 2,336 college sophomores was drawn from a larger university-wide study (“Spit for Science”).
Methods:
We constructed multiple linear regression models using past-year trauma exposure, trait mindfulness, and their multiplicative interaction to predict current anxiety and depressive symptom severity, while controlling for covariates.
Results:
Mindfulness was associated with lower levels of depression and anxiety symptom severity. Trauma was a significant predictor of anxiety, but not depression, and high levels of mindfulness attenuated the association between trauma exposure and higher anxiety symptom severity.
Conclusions:
These results have implications for the treatment and prevention of anxiety among trauma-exposed college students and provides a basis for further research into the mechanisms through which mindfulness may facilitate positive mental health.
Keywords: anxiety, depression, internalizing, trauma, mindfulness
Anxiety disorders, characterized by uncontrollable feelings of fear and anxiety, and depressive disorders, characterized by depressed mood, anhedonia, and irritability, both cause impairments in everyday physical and psychological functioning, from decreased energy to deficits in cognitive functioning.1,2 Depressive disorders and anxiety disorders have been shown to be highly comorbid, especially in adolescence,3 and have been commonly conceptualized as being contained within a broad group of internalizing psychiatric disorders, which share similar symptomology, comorbidity, and genetic and environmental etiology.4
These internalizing disorders, along with other severe mental health problems, have been increasing among college students in recent years.5,6 During an often-unstable period of transition between adolescence and adulthood, college students may be particularly susceptible to the negative effects of mental health problems. Recent data from the American College Health Association-National College Health Assessment shows that 16.9% of respondents had been treated for or diagnosed with anxiety and 13.2% with depression within the 12 months prior to the survey.5 In addition to the challenges posed to university administration and family members of sufferers, those diagnosed with anxiety and depressive disorders are at risk for reductions in academic success, increases in substance use, and, tragically, increases in suicidal ideation and attempts.5,6
Additionally, anxiety and depression are markedly elevated in those who have experienced a traumatic event,7 making college students who have experienced trauma an even more at-risk population. In one study by Frazier et al.,8 85% of undergraduate students reported experiencing a traumatic event at some point in their lives, with 21% experiencing one over just a two-month period while in college. Although posttraumatic stress disorder (PTSD) is the signature trauma-related disorder, trauma is a transdiagnostic risk factor and is also associated with anxiety and depression, which are often comorbid with PTSD.7,9 It has been postulated that this association may be due to an increased risk of trauma exposure in anxiety and depression sufferers, a causal link between PTSD and comorbid disorders, or shared genetic and environmental risk factors between PTSD and internalizing disorders.7 Given the association between trauma and internalizing symptoms and the complex nature of trauma exposure risk, research aimed at elucidating potential moderating factors on the relationship between trauma and internalizing symptoms in college students has important implications for reducing psychological distress and suffering.
The unique properties of mindfulness, a non-judgmental awareness of and attention to one’s present experience,10 may aid those suffering from internalizing disorders by altering their experience of distress and fear, which have been shown to be predictive of these disorders.11 Mindfulness has been linked to a number of measures of positive well-being, is negatively correlated with depression and anxiety, and has shown promise in the treatment of many psychological disorders, including anxiety and depression.10 Two meta-analyses examining mindfulness-based therapies, performed by Hofmann, Sawyer, Witt, and Oh12 and Vollestad, Nielsen, and Nielsen,13 showed large effect sizes for reduction in depression and anxiety symptoms among clinical populations. These therapies focus on altering a patient’s relationship to internal experiences, i.e. reframing how they view and evaluate these experiences. There is evidence that following such interventions, individuals show increased levels of trait mindfulness,14,15 demonstrating that this is a trait that may be cultivated.
With mindfulness showing clear efficacy as a treatment for some common psychiatric conditions and trauma being a common antecedent, it is of interest to understand how mindfulness might provide resilience to the development of psychiatric disorders following a traumatic event. Thompson, Arnkoff, and Glass16 present a mindfulness- and acceptance-based conception of trauma resilience and propose a mechanism by which mindfulness may confer these benefits. From this perspective, experiential avoidance (attempts to avoid unwanted internal experiences) and a dissociative predisposition (lapsing in normal mental processing) are central to the development and maintenance of PTSD and other comorbid disorders, including anxiety and depression. Mindfulness, with its focus on attention to and awareness of one’s present experience, is thought to confer resilience to trauma by facilitating acceptance and emotion processing following a traumatic event, thus reducing dissociative and avoidant tendencies. Vollestad and colleagues13 proposed that these interventions reduce distress from anxiety disorders by addressing an individual’s relations to their distressing thoughts and behaviors by viewing them with acceptance and compassion rather than attempting to avoid, control or suppress their symptoms. Avoidance and suppression of negative thoughts and emotions are associated with elevated levels of internalizing symptomology among trauma-exposed individuals,17 suggesting that mindfulness may provide specific benefits to trauma-exposed individuals by reducing these tendencies and their related internalizing symptoms. Mindfulness, therefore, should provide a reduced risk for developing severe mental health issues, and increased resilience following a trauma.
Thus far, a single study18 has empirically examined this link, studying the role of mindfulness in the mental health of individuals exposed to trauma. Although they found that low levels of mindfulness were not indicative of vulnerability to anxiety, depression, or PTSD following a trauma, high levels of mindfulness were linked to resilience after experiencing a trauma. However, the study was limited by its sample, which lacked racial/ethnic diversity and was composed only of smokers, and was also limited by its lack of temporal order linking the traumatic event to psychopathology and mindfulness. The lack of a discernable order of events could lead to interpretational difficulties related to reverse causation. Further, this study did not conduct an explicit test of interaction or include individuals without trauma exposure for comparison.
“Spit for Science” (S4S), a longitudinal study focusing on the genetic, environmental and developmental factors related to substance use and emotional health in college students,19 provides an avenue for exploring the link between mindfulness and psychopathology following trauma and for addressing the limitations of previous research. This study includes a large, diverse sample, a clearly discernable timeline for examining anxiety and depression symptoms following a traumatic event, and provides genetic data for potential use in future studies. Research on the role of mindfulness in mental health following trauma has thus far concentrated on adult populations. With its focus on emerging adult, college-aged individuals, the present study provides a novel examination of an understudied population in this area of research. The present study aims to determine whether trait mindfulness moderates the effect of trauma exposure on depression and anxiety. We hypothesized that individuals exposed to a traumatic event and reporting higher trait mindfulness would show lower levels of depression and anxiety symptom severity than those exposed to trauma and reporting lower trait mindfulness.
Methods
Participants
The data used in the present analysis was collected as part of S4S, a larger longitudinal study measuring a number of behavioral and psychological self-report measures.19 A sample of undergraduate students from a large, urban, mid-Atlantic university were recruited through a mass mailing and email announcement sent to all incoming students aged 18 or older from four consecutive cohorts (2011–2014) at the beginning of the fall semester of each cohort’s freshman year. Eligible students were sent a link to a confidential online survey using REDCap data management software.20 This protocol was approved by the university Institutional Review Board, and participants provided informed consent online prior to beginning the survey. After their completion of the online survey portion of the study, participants were compensated with a t-shirt and $10. Participants were also given the opportunity to provide an optional DNA sample, for which they received an additional $10. Approximately 70% of the eligible freshman student population enrolled in the parent S4S sample (N = 9,889). Students who enrolled in the study were invited to participate in a follow-up survey each subsequent spring semester that they were in attendance at the university.
Inclusion in the present study was predicated on the completion of four measures of interest (described below), collected during the freshman and sophomore spring survey waves. Specifically, the mindfulness items were assessed for only two of the four cohorts of students, meaning that the total target sample for the present analyses was N = 4260 individuals from the parent study. After initial enrollment and completion of the freshman year survey, 56% of these individuals also completed the sophomore follow-up survey, which included measures used in this study. Students were also given the option to choose not to respond to questions. With these factors considered, we had a final analytic sample size of n = 2236 (52% of the target sample). The participants in our sample ranged in age from 18 to 27 years old (mean = 19.9). Thirty-three percent of our sample was male and 66% female, and the responses to the self-reported race/ethnicity item in our sample are summarized in Table 1. A chi-square goodness of fit test revealed that the proportions of gender (χ2 = 22.31, p < 0.001) and ethnicity (χ2 = 26.42, p < 0.001), of our sample differed significantly from the overall S4S sample, which is likely due to attrition following the initial survey. Our subsample appears to over-represent females and those who identify as Asian and Black or African American, while underrepresenting those who identify as white, as compared to the full sample of participants. T-tests revealed no significant differences in anxiety symptom severity (t(4375.2) = 1.67, p = 0.09) or depression symptom severity (t(4426.9) = −0.48, p = 0.63) between freshman and sophomore year within our subsample.
Table 1.
Self-reported race and ethnicity in study sample of college students.
| Ethnicity | N | Percent |
|---|---|---|
| American Indian/Alaska Native | 9 | 0.38% |
| Asian | 470 | 19.68% |
| Black/African American | 496 | 20.77% |
| Hispanic/Latino | 140 | 5.86% |
| More than one race | 145 | 6.07% |
| Native Hawaiian/Other Pacific | 15 | 0.63% |
| Islander | ||
| Unknown | 7 | 0.29% |
| White | 1066 | 44.64% |
| Choose not to answer | 40 | 1.68% |
Measures
Trauma exposure.
Past-year dichotomous traumatic event exposure (TE) was measured in participants’ sophomore year follow-up survey using the Life Events Checklist,21 which asked participants to indicate whether or not they have experienced any of the following potentially traumatic events in the past 12 months: natural disaster, physical assault, sexual assault, other unwanted or uncomfortable sexual experience, transportation accident. This scale shows adequate temporal stability, with a one-week retest correlation of r = 0.82, and convergent validity with an established trauma exposure measure (r = −0.55, with lower scores on the life events checklist indicating more severe exposure in this study) as well as measures of psychopathology associated with traumatic event exposure (r = −0.27 to −0.43)21. Participants’ responses were recoded for our analysis, creating a new dichotomous measure of trauma-exposed and non-trauma exposed individuals dependent upon their endorsement of exposure to any of these traumatic events in the past year.
Mindfulness.
Items from the Mindful Attention Awareness Scale (MAAS),10 were used in participants’ sophomore follow-up survey to measure levels of a basic operationalization of dispositional mindfulness, conceptualized as a sustained attention to and awareness of one’s present experience. The seven items (α = 0.88) used were derived from Item Response Theory analysis in an independent sample of 2292 students from the same university population.22 Examples of these items included: “I could be experiencing some emotion and not be conscious of it until sometime later.” and “I do jobs or tasks automatically, without being aware of what I’m doing” (rated on a Likert scale from 1 = Almost Always to 6 = Almost Never). This scale has previously demonstrated high reliability, with an interclass correlation of 0.81 and no significant difference between mean MAAS scores across a 4-week interval10. Convergent and discriminative validity of the MAAS has also been demonstrated through its correlation with a prior measure of mindfulness/mindlessness and other scales conceptually expected to covary with trait mindfulness10. Individuals who answered less than 50% of the items were excluded from analyses; for the remainder, the mean of available responses was computed, with higher scores representing higher levels of trait mindfulness.
Covariates.
Sex, race/ethnicity (from census categories), personality traits, and resilience were measured during participants’ freshman-year survey and included as covariates to control for factors that may differ systematically with the outcomes of interest. For example, levels of anxiety, depression, and risk of trauma exposure differ between males and females23,24, and multiple dimensions of personality are linked to variation in mindfulness and psychopathology as well10,25.
Ethnic group categories with low rates of endorsement in our sample (i.e. American Indian/Alaska Native, Hispanic/Latino, More than one race, Native Hawaiian/Other Pacific Islander, Unknown) were combined for our analyses. The Big-Five trait taxonomy26 was used to measure personality traits of openness, conscientiousness, extraversion, agreeableness, and neuroticism, with three items included for each trait. This scale is an extremely well-validated measure of the five primary domains of personality that have been replicated across decades of research26, with high internal consistency (α > .86)27 and test-retest reliability (r = .86-.91)28. The subset of items included for each scale in our study demonstrated good inter-item consistency (α = 0.60 – 0.80). Two items from the Connor-Davidson Resilience Scale29 were included as a measure of resilience, showing good consistency in our sample (α = 0.61); this scale has shown good reliability, with no significant difference in mean scores across two time periods and an interclass correlation of 0.87, and high validity, correlating positively with hardiness and negatively with perceived stress and stress vulnerability29. Sum scores were calculated for each of these measures of personality and resilience.
Anxiety and Depression Symptoms.
Recent levels of anxiety symptom severity (AS) and depression symptom severity (DS) were measured in participants’ initial freshman year survey and follow-up sophomore survey using the average of participants’ scores on four items each from the anxiety and depression subscales of the Symptoms Checklist 90 (SCL-90).30 The SCL-90 asks participants to describe their level of distress in the 30 days prior to the survey administration caused by various psychological symptoms. Responses were measured on a Likert-type scale with five response options ranging from 1 = “Not at all” to 5 = “Extremely”. Previously, this scale has demonstrated evidence of good construct validity30 and as noted previously, shows good temporal stability in our sample with no significant difference between symptom severity measured during freshman and sophomore year.
In our sample, four items (α = 0.85[freshman year], α = 0.84[sophomore year]) from the SCL-90’s anxiety subscale were used to measure AS, including “nervousness or shakiness inside” and “spells of terror or panic”. Similarly, four items (α = 0.82[freshman year], α = 0.85[sophomore year]) from the depression subscale of the SCL-90 were used to measure DS, including “feeling no interest in things” and “feeling hopeless about the future”. Participants who answered less than 50% of the items on either of the subscales were excluded from analysis and missing data were pro-rated. Scores were created by averaging the four items in each subscale and multiplying by the total number of items. AS and DS were assessed in participants’ sophomore survey as well as in their initial freshman year survey. Initial levels (“baseline AS/DS”) were included in our analyses to control for the potential effects of existing anxiety or depression psychopathology affecting TE and/or self-reported levels of mindfulness in sophomore year.
Statistical Analyses
R version 3.3.131 was used for all statistical analyses and data visualization in the present study. Probable covariates (measured in participants’ initial freshman survey) were analyzed using correlations to determine which were associated with the independent/dependent variables and therefore which should be controlled for in subsequent analyses. For our main aim, two hierarchical multiple linear regression analyses were performed, one each for DS and AS. We used measures from participants’ sophomore survey including TE, mean mindfulness score, and their multiplicative interaction term as predictor variables and mean DS or AS as the dependent variable. Covariates, along with baseline DS or AS levels (from the freshman survey), were statistically controlled by their inclusion in the model. Each analysis consisted of a set of three nested models: 1) covariates only; 2) covariates + main effects of TE and mindfulness; and 3) covariates + main effects + TE-mindfulness interaction term.
Results
Descriptive Statistics
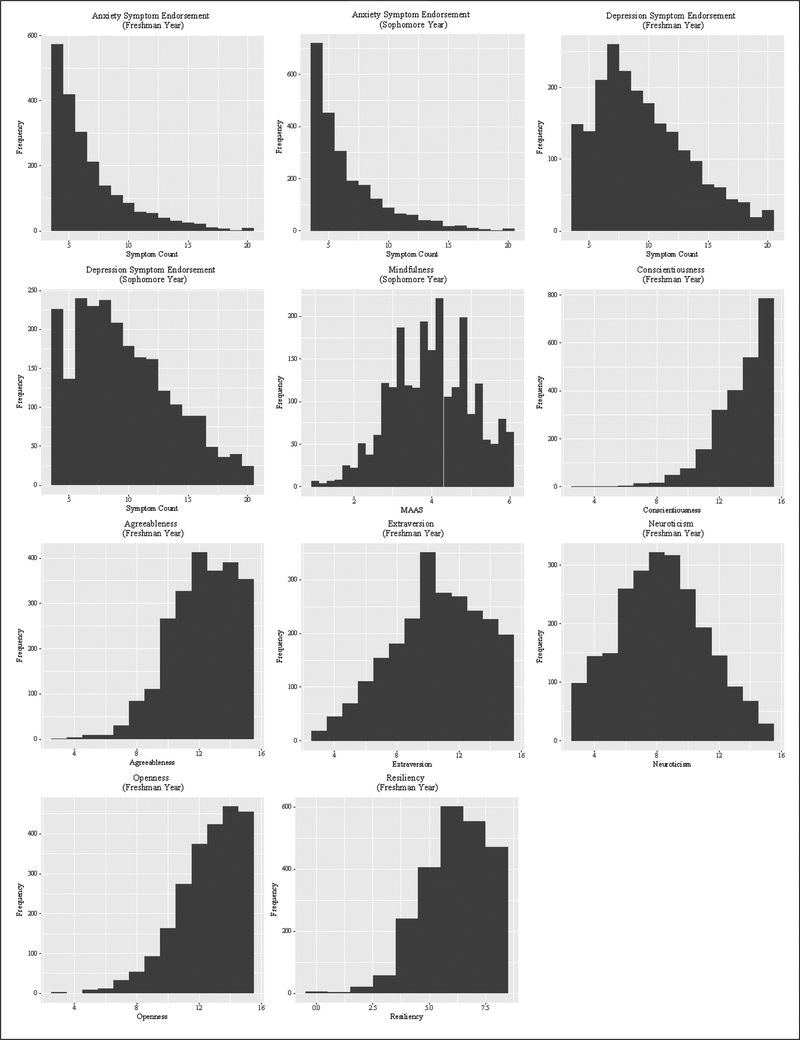
Histograms for our continuous variables of interest are shown in Figure 1. AS and DS in our sample were skewed towards the right, while agreeableness, conscientiousness, openness, and resilience were skewed to the left. Descriptive statistics for the sample are summarized in Table 2. Approximately 32% of participants reported experiencing at least one traumatic event in the year prior to completing their sophomore survey. Correlations between variables used in our analyses are presented in Table 3, showing that the proposed covariates (openness, conscientiousness, extraversion, agreeableness, neuroticism, and resilience) were significantly associated with our outcome of interest and/or one or more predictor variables. AS and DS were positively correlated with each other and negatively correlated with trait mindfulness. Psychopathology was also correlated with higher neuroticism and openness as well as lower conscientiousness, extraversion, agreeableness, and resiliency. Mindfulness showed a negative correlation with neuroticism and positive correlations with conscientiousness, extraversion, agreeableness, and resiliency.
Figure 1.
Histograms for continuous variables included in main analyses.
Table 2.
Descriptive statistics of self-report measures of anxiety symptom severity (AS), depression symptom severity (DS), mindfulness, and trauma exposure (TE) collected from two waves of surveys in a longitudinal sample of college students.
| Survey Wave | Measure | M (SD) | Range | α |
|---|---|---|---|---|
| Freshman Spring | AS | 6.76 (3.16) | 4 – 20 | 0.85 |
| DS | 9.56 (3.86) | 4 – 20 | 0.82 | |
| Sophomore Spring | AS | 6.60 (3.08) | 4 – 20 | 0.84 |
| DS | 9.62 (4.02) | 4 – 20 | 0.85 | |
| Trait Mindfulness | 4.00 (1.03) |
1 – 6 |
0.88 | |
| TE |
N |
Percent |
||
| Non-Exposed | 1596 | 68.18% | ||
| Exposed | 745 | 31.82% |
Note. AS: Past 30-day Anxiety Symptom Severity. DS: Past 30-day Depression Symptom Severity. TE: Past-Year Trauma Exposure.
Table 3.
Correlations between covariates and primary outcome measures.
| Mindfulness | AS(Sophomore) | DS(Sophomore) | AS(Freshman) | DS(Freshman) | Agreeableness | Conscientiousness | Extraversion | Neuroticism | Openness | Resiliency | |
| Mindfulness | 1.00 | ||||||||||
| AS(Sophomore) | −0.37 | 1.00 | |||||||||
| DS(Sophomore) | −0.44 | 0.67 | 1.00 | ||||||||
| AS(Freshman) | −0.28 | 0.50 | 0.37 | 1.00 | |||||||
| DS(Freshman) | −0.33 | 0.44 | 0.55 | 0.69 | 1.00 | ||||||
| Agreeableness | 0.15 | −0.06 | −0.09 | −0.09 | −0.12 | 1.00 | |||||
| Conscientiousness | 0.18 | −0.09 | −0.12 | −0.10 | −0.12 | 0.33 | 1.00 | ||||
| Extraversion | 0.04 | −0.09 | −0.16 | −0.07 | −0.16 | 0.00 | 0.11 | 1.00 | |||
| Neuroticism | −0.20 | 0.31 | 0.35 | 0.34 | 0.40 | −0.18 | −0.15 | −0.10 | 1.00 | ||
| Openness | −0.03 | 0.08 | 0.07 | 0.10 | 0.06 | 0.11 | 0.09 | 0.15 | −0.05 | 1.00 | |
| Resiliency | 0.12 | −0.12 | −0.14 | −0.16 | −0.20 | 0.15 | 0.26 | 0.21 | −0.41 | 0.14 | 1.00 |
Note. Bold indicates p-value < 0.05. AS: Past 30-day Anxiety Symptom Severity. DS: Past 30-day Depression Symptom Severity. TE: Past-Year Dichotomous Trauma Exposure
Linear Models
The results of a hierarchical multiple linear regression analysis (Analysis 1) predicting DS are summarized in Table 4. The base Model 1, including only covariates and baseline DS, explained 33% of the variance in current DS. Baseline DS was a significant predictor of current DS (β = 0.49, p<0.001), along with certain covariates (ethnicity, personality, and resilience; see Table 4). The addition of TE and mindfulness in Model 2 explained a significant increase of 7% in DS variance. Mindfulness (β = −1.09, p<0.001) was a significant predictor of DS, while TE was marginally significant at p=0.10 (β = 0.24). A TE x mindfulness interaction term was included in Model 3, which was not significant and did not result in a significant increase in R2.
Table 4.
Analysis 1: Predictors of past 30-day depression symptom severity (DS) from a hierarchical linear regression model in a sample of college students.
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 = 0.33; F = 90.49*** | R2=0.40; F for ΔR2=115.56*** | R2=0.40; F for ΔR2=0.36 | |||||||
| β | SE | p | β | SE | p | β | SE | p | |
| Intercept | 3.89 | 0.93 | 3.00e–5*** | 8.29 | 0.93 | <2e–16 | 8.44 | 0.96 | <2e–16 |
| Sex (Male = 1) | −0.30 | 0.17 | 0.08 | −0.39 | 0.16 | 0.02* | −0.40 | 0.16 | 0.01* |
| Asian | −0.42 | 0.20 | 0.04* | −0.45 | 0.19 | 0.02* | −0.45 | 0.19 | 0.02* |
| Black/African American | −0.58 | 0.20 | 3.34e–3** | −0.42 | 0.19 | 0.02* | −0.42 | 0.19 | 0.02* |
| Other Ethnicity | −0.38 | 0.23 | 0.09 | −0.34 | 0.22 | 0.11 | −0.34 | 0.22 | 0.11 |
| Agreeableness | 0.02 | 0.04 | 0.61 | 0.06 | 0.04 | 0.12 | 0.05 | 0.04 | 0.12 |
| Conscientiousness | −0.13 | 0.05 | 9.77e–3** | −0.06 | 0.04 | 0.19 | −0.06 | 0.04 | 0.19 |
| Extraversion | −0.10 | 0.03 | 1.68e–4*** | −0.11 | 0.03 | 2.31e–5*** | −0.11 | 0.03 | 2.54e–5*** |
| Neuroticism | 0.21 | 0.03 | 1.15e–10*** | 0.18 | 0.03 | 2.65e–9*** | 0.18 | 0.03 | 3.45e–9*** |
| Openness | 0.11 | 0.04 | 2.15e–3** | 0.09 | 0.03 | 5.32e–3** | 0.09 | 0.03 | 5.75e–3** |
| Resiliency | 0.12 | 0.06 | 0.04* | 0.12 | 0.06 | 0.04* | 0.11 | 0.06 | 0.04* |
| Previous-Year DS | 0.49 | 0.02 | <2e–16*** | 0.40 | 0.02 | <2e–16*** | 0.40 | 0.02 | <2e–16*** |
| Mindfulness | −1.09 | 0.07 | <2e–16*** | −1.12 | 0.09 | <2e–16*** | |||
| TE | 0.24 | 0.15 | 0.10 | −0.09 | 0.58 | 0.88 | |||
| Mindfulness x TE | 0.09 | 0.14 | 0.55 | ||||||
Note. <0.05.
<0.01.
<0.001. DS: Past 30-Day Depression Symptom Severity. TE: Past-Year Dichotomous Trauma Exposure.
A similar hierarchical multiple linear regression analysis (Analysis 2) was performed, this time with AS as the dependent variable; these results are summarized in Table 5. The base Model 1 explained 29% of the variance in AS. Baseline AS (β = 0.41, p<0.001) was a significant predictor of current AS, as were sex, ethnicity, and a number of personality variables (see Table 5). Model 2, which added TE and mindfulness as predictors, explained a significant increase of 5% in the variance in AS accounted for as compared to Model 1. Both TE (β = 0.39, p<0.01) and mindfulness (β = −0.67, p<0.001) significantly predicted AS. Finally, a TE x mindfulness interaction term was included in Model 3, which explained significantly more (1%) variance in AS as compared to Model 2 and was a significant predictor in this model (β = −0.39, p<0.001). This pattern of results remained the same after running the same models with log-transformed AS to account for the variable’s skew, after mean centering the continuous variables, and after log-transforming personality variables that showed a skewed distribution. The interaction term was robust to all variable transformations.
Table 5.
Analysis 2: Predictors of past 30-day anxiety symptom severity (AS) from a hierarchical linear regression model in a sample of college students.
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 = 0.29; F = 75.01*** | R2=0.34; F for ΔR2=76.34*** | R2=0.35; F for ΔR2=11.30*** | |||||||
| β | SE | p | β | SE | p | β | SE | p | |
| Intercept | 3.20 | 0.72 | 9.29e–6*** | 5.71 | 0.73 | 7.89e–15*** | 5.06 | 0.75 | 2.19–e11*** |
| Sex (Male = 1) | −0.36 | 0.13 | 8.29e–3** | −0.40 | 0.13 | 2.17e–3** | −0.38 | 0.13 | 3.18e–3** |
| Asian | −0.40 | 0.16 | 0.01* | −0.39 | 0.15 | 0.01* | −0.38 | 0.15 | 0.01* |
| Black/African American | −0.57 | 0.15 | 2.04e–4*** | −0.51 | 015 | 6.15e–4*** | −0.51 | 0.15 | 6.65e–4*** |
| Other Ethnicity | −0.22 | 0.18 | 0.22 | −0.22 | 0.17 | 0.21 | −0.22 | 0.17 | 0.19 |
| Agreeableness | 0.01 | 0.03 | 0.81 | 0.03 | 0.03 | 0.28 | 0.03 | 0.03 | 0.24 |
| Conscientiousness | −0.08 | 0.04 | 0.03* | −0.04 | 0.04 | 0.27 | −0.04 | 0.03 | 0.25 |
| Extraversion | −0.08 | 0.02 | 2.52e–3** | −0.07 | 0.02 | 1.92e–4*** | −0.08 | 0.02 | 1.22e–4*** |
| Neuroticism | 0.17 | 0.02 | 2.27e–11*** | 0.14 | 0.02 | 9.35e–9*** | 0.14 | 0.02 | 2.54e–9*** |
| Openness | 0.07 | 0.03 | 0.01* | 0.06 | 0.03 | 0.03* | 0.06 | 0.03 | 0.02* |
| Resiliency | 0.07 | 0.05 | 0.12 | 0.07 | 0.04 | 0.14 | 0.07 | 0.04 | 0.10 |
| Previous-Year AS | 0.41 | 0.02 | <2e–16*** | 0.36 | 0.02 | <2e–16*** | 0.35 | 0.02 | <2e–16*** |
| Mindfulness | −0.67 | 0.06 | <2e–16*** | −0.54 | 0.07 | 5.38e–15*** | |||
| TE | 0.39 | 0.12 | 1.50e–3 ** | 1.90 | 0.47 | 4.83e–5*** | |||
| Mindfulness x TE | −0.39 | 0.11 | 7.89e–4*** | ||||||
Note. <0.1.
<0.05.
<0.01.
<0.001. AS: Past 30-day Anxiety Symptom Severity. TE: Past-Year Dichotomous Trauma Exposure.
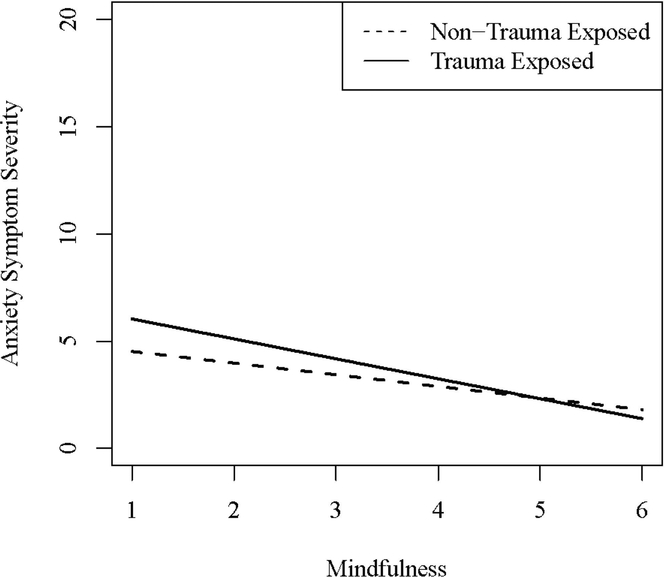
Figure 2 shows sophomore year AS predicted by Analysis 2, Model 3 as a function of mindfulness for individuals with and without trauma exposure. This interaction showed that trauma-exposed individuals scoring low in mindfulness (MAAS scores less than 4) reported an average of 1.18 higher AS than non-trauma exposed individuals with similarly low mindfulness scores, while those trauma-exposed individuals high in mindfulness (MAAS scores greater than 4) reported only 0.45 higher AS than to their non-exposed, high-mindful counterparts. Post-hoc simple slopes analysis indicated that TE was significantly associated with higher AS at low levels of mindfulness, but did not have a significant effect at higher levels of mindfulness (MAAS > 4.7).
Figure 2.
Predicted association between mindfulness and anxiety symptom severity for trauma-exposed and non-trauma exposed individuals, controlling for previous-year symptoms, sex, race, personality traits, and resiliency.
Sensitivity Analyses
Because our measure of TE was rather brief and there are complex relationships between trauma and DS/AS, we conducted sensitivity analyses to investigate whether the observed results were dependent on the specific definition of TE we employed here, and whether they were consistent across subgroups. Epidemiologic studies suggest that while males generally have higher trauma exposure histories compared to females, females are more likely to experience an interpersonal trauma.24 Thus, we conducted post-hoc analyses repeating the hierarchical regression analyses for females and males separately, showing overall similar patterns of results. However, while mindfulness was significantly predictive of lower AS in both males and females (male β = −0.50, p < 0.001, female β = −0.56, p < 0.001), TE (male β = 0.75, p = 0.36, female β = 2.15, p < 0.001) and mindfulness x TE terms (male β = 0.15, p = 0.47, female β = −0.43 p = 0.002) were significant predictors of AS only for females. Additionally, models with the TE measure including only endorsement of interpersonal trauma items (i.e. physical assault, sexual assault, other unwanted sexual experience) showed similar patterns as presented in our results for overall trauma. Finally, similar patterns of significance were seen in models predicting AS using a non-dichotomous trauma exposure variable (i.e. a count of the number of TEs experienced), suggesting that the observed relationships are robust regardless of the number or type of traumatic events experienced. Full results of the sensitivity analyses are available upon request.
Comment
The aim of this study was to understand the relationship between trauma exposure and internalizing symptoms in college students and to test whether mindfulness may have a moderating effect on this relationship. We found that TE exhibited a significant positive association with AS, but that TE was not a significant predictor of DS. Dispositional mindfulness was associated with both lower AS and DS in our sample. Our hypothesis that mindfulness would buffer the effects of trauma exposure on DS and AS was partially supported. Although the mindfulness x TE interaction was not a significant predictor of DS, it was specifically associated with AS, even after controlling for other factors such as previous symptom severity levels that may have provided an alternative explanation for their association. The relationship between TE and AS was moderated by trait mindfulness levels such that the positive association between TE and AS was attenuated among those higher in dispositional mindfulness. Further, we found that multiple dimensions of personality, primarily higher neuroticism and lower extraversion, were associated with higher levels of AS and DS even when accounting for mindfulness and trauma exposure.
Our finding that TE is significantly associated with higher AS is supported by previous studies demonstrating that trauma exposure is a risk factor for anxiety disorders.7,18 However, our results failed to show the predicted relation between trauma exposure and depression revealed in past research. This may be due to the fact that our study utilized different, abbreviated measures of DS. Additionally, since many previous studies have focused on older adult populations, this could indicate variance in the effects of trauma on depression symptoms between younger and older adults. Specifically, this discrepancy could be due to differences in the types of trauma experienced by older adults compared to college students, or differences in the subjective experience of those events. Taken together with the high prevalence of past-year trauma exposure in our sample, our results reinforce the importance of mental health screening and appropriate treatment in college students following a traumatic event.
The results of our study showed a robust negative relation between mindfulness and AS and DS, even when controlling for previous symptom severity and other probable covariates, and is consistent with previous research demonstrating the positive associations between mindfulness and emotional health.10,12,13,18 Although the present results are correlational, the robust literature demonstrating the effects of mindfulness interventions on mental health suggests that mindfulness may exhibit a causal influence in decreasing internalizing symptoms.12,13 The temporal ordering of events, with participants reporting trauma exposure as occurring before our measures of anxiety and depression were taken, reduce the likelihood of reverse causality between trauma exposure and symptom severity, although cannot exclude the possibility of biased trauma exposure reporting among those experiencing higher DS or AS. Overall, our results contribute to the growing body of evidence that mindfulness confers benefits for one’s mental health, regardless of trauma exposure. However, we note that mindfulness and TE jointly accounted for a smaller proportion of the variance in both AS and DS than did other individual characteristics such as sex, ethnicity, personality, and baseline AS/DS, emphasizing that these individual differences are important to consider in the etiology of anxiety and depression. The effects of TE and mindfulness are incremental but considerably less strong predictors than these more inherent individual characteristics.
Although mindfulness demonstrated no moderating effect on DS, our results indicated that there is a significant interaction between TE and mindfulness on AS. These results demonstrate that higher dispositional mindfulness may reduce the effect of trauma exposure in a way that is specific to anxiety disorders. Mindfulness may provide these unique benefits to anxiety symptoms following traumatic events because of the conceptual differences between anxiety and depressive disorders. Since many anxiety disorders are characterized by a tension and vigilance related to future events1, the present-oriented focus afforded by mindfulness may uniquely benefit those suffering from anxiety following a traumatic event compared to depressive disorders by shifting one’s attention from the negative past experience of trauma and the anxiety about future events to present or current events and experiences.
Thompson, Arnkoff, and Glass16 theorized that the present-oriented nature of mindfulness strengthens general resilience to trauma by reducing dissociative and avoidant tendencies that often contribute to anxiety, depression, and PTSD symptoms. Our findings suggest that mindfulness may bolster resilience to trauma, but that these benefits may be especially pronounced in anxiety. More generally, outside of the context of trauma, Desrosiers, Vine, Klemanski, & Nolen-Hoeksema32 suggest differences in mediators of the relation between mindfulness and anxiety versus mindfulness and depression symptoms. These authors found that the relation between mindfulness and depression symptoms was shown to be mediated by rumination and reappraisal, but its relation with anxiety symptoms was mediated by rumination and worry. Therefore, our findings suggest that it may be worry, uniquely important in anxiety, that is increased by trauma exposure and reduced by mindfulness in trauma-exposed college students. Our novel findings warrant further research to uncover the mechanisms through which mindfulness induces resilience to anxiety following a trauma.
Limitations
Our study faces limitations due to possible reporting bias, as our self-report survey included stigma-associated items related to mental health. Our survey also included a brief assessment of anxiety and depression symptom severity and does not provide indication of clinical diagnoses, which were important in previous research of the benefits of mindfulness for clinical patients.12,13 Additionally, since trait mindfulness was measured concurrently with other measures, trauma and/or internalizing symptoms may have influenced participants’ scores on the MAAS items. However, participants were explicitly asked to report on different time frames for each measure – trauma in the past year, internalizing symptoms in the past 30 days, and mindfulness as day-to-day frequency of usual behaviors. Our sample is also limited by attrition from the initial freshman survey. Finally, since our survey did not include thorough measures of PTSD, future research is needed to examine the role of mindfulness in its development following a trauma and whether our results related to anxiety symptoms may be mediated by a diagnosis of PTSD. There are likely additional variables not captured by our survey which may be important in the relation between trauma, mindfulness, and anxiety which should be examined further in future studies.
Conclusions
Our results suggest implications for the prevention and treatment of anxiety following traumatic events in the at-risk college student population, and for the treatment and prevention of internalizing disorders in this population more generally. Our results suggest that following a trauma, those exhibiting anxiety symptoms may benefit more from mindfulness-based therapy than those exhibiting depressive symptoms, but that targeted mindfulness interventions may also be successful in reducing anxiety and depression in college student populations regardless of trauma exposure status. We have shown that mindfulness may provide a unique benefit to trauma-exposed female college students suffering from anxiety, but our findings also illustrated the broad relation of basic trait mindfulness with lower levels of internalizing symptoms regardless of trauma exposure or sex. Experimental research is necessary to test the robustness of these findings and to elucidate the mechanisms by which mindfulness confers these benefits in young adults previously exposed to trauma. Our results help to lay the groundwork for such studies and provide initial support for a new addition to the growing list of the benefits of mindfulness in promoting positive mental health.
Acknowledgements:
Spit for Science: The VCU Student Survey has been supported by Virginia Commonwealth University, P20AA017828, R37AA011408, K02AA018755, and P50AA022537 from the National Institute on Alcohol Abuse and Alcoholism, and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. We would like to thank Kirk Warren Brown, PhD for his feedback during the preparation of this manuscript. We would also like to thank the VCU students for making this study a success, as well as the many VCU faculty, students, and staff who contributed to the design and implementation of the project. JDT is now at the National Institutes of Health. JES is now at Vrije Universiteit Amsterdam.
References
- 1.American Psychiatric Association. Anxiety disorders. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. 2013. 10.1176/appi.books.9780890425596.dsm05 [DOI]
- 2.American Psychiatric Association. Depressive disorders. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. 2013. 10.1176/appi.books.9780890425596.dsm04 [DOI]
- 3.Garber J, Weersing VR. Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clin Psychol. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women.Arch Gen Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929 [DOI] [PubMed] [Google Scholar]
- 5.American College Health Association. National college health assessment II: Undergraduate student reference group data report spring 2016. http://www.acha-ncha.org/docs/NCHA-II%20SPRING%202016%20UNDERGRADUATE%20REFERENCE%20GROUP%20DATA%20REPORT.pdf
- 6.Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46(1):3–10. 10.1016/j.jadohealth.2009.08.008 [DOI] [PubMed] [Google Scholar]
- 7.Breslau N The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10(3):198–210. doi: 10.1177/1524838009334448 [DOI] [PubMed] [Google Scholar]
- 8.Frazier P, Anders S, Perera S, Tomich P, Tennen H, Park C, Tashiro T. Traumatic events among undergraduate students: Prevalence and associated symptoms. J Cons Psychol. 2009;56(3):450–460. doi: 10.1037/a0016412 [DOI] [Google Scholar]
- 9.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- 10.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822 [DOI] [PubMed] [Google Scholar]
- 11.Eaton NR, Krueger RF, Markon KE, et al. The structure and predictive validity of the internalizing disorders. J Abnorm Psychol. 2013;122(1):86–92. doi: 10.1037/a0029598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–183. doi: 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vøllestad J, Nielsen MB, Nielsen GH. Mindfulness- and acceptance-based interventions for anxiety disorders: A systematic review and meta-analysis. Br J Clin Psychol. 2012;51(3):239–260. doi: 10.1111/j.2044-8260.2011.02024.x [DOI] [PubMed] [Google Scholar]
- 14.Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. J Psychosom Res. 2008;64:393–403. doi: 10.1016/j.jpsychores.2007.06.015 [DOI] [PubMed] [Google Scholar]
- 15.Shapiro SL, Brown KW, Thoresen C, Plante TG. The moderation of Mindfulness-based stress reduction effects by trait mindfulness: Results from a randomized controlled trial. J Clin Psychol. 2011;67:267–277. doi: 10.1002/jclp.20761 [DOI] [PubMed] [Google Scholar]
- 16.Thompson RW, Arnkoff DB, Glass CR. Conceptualizing Mindfulness and Acceptance as Components of Psychological Resilience to Trauma. Trauma Violence Abuse. 2011;12(4):220–235. doi: 10.1177/1524838011416375 [DOI] [PubMed] [Google Scholar]
- 17.Amstadter AB, Vernon LL. A preliminary examination of thought suppression, emotion regulation, and coping in a trauma-exposed sample. J Aggress Maltreatment Trauma. 2008;17(3):279–295. doi: 10.1080/10926770802403236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernstein A, Tanay G, Vujanovic AA. Concurrent relations between mindful attention and awareness and psychopathology among trauma-exposed adults: Preliminary evidence of transdiagnostic resilience. J Cogn Psychother. 2011;25(2):99–113. doi: 10.1891/0889-8391.25.2.99 [DOI] [Google Scholar]
- 19.Dick DM, Nasim A, Edwards AC, et al. Spit for science: Launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Front Genet. 2014;5:1–12. doi: 10.3389/fgene.2014.00047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. [DOI] [PubMed] [Google Scholar]
- 22.Brown KW, Rogge R. Item Response Theory analysis of the Mindful Attention Awareness Scale in a young adult population. 2013. Unpublished data, Virginia Commonwealth University. [Google Scholar]
- 23.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, … Kendler KS (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–19. [DOI] [PubMed] [Google Scholar]
- 24.Benjet C, Bromet E, Karam EG, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium.Psychol Med. 2016;46(2):327–343. doi: 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malouff JM, Thorsteinsson EB, & Schutte NS (2005). The Relationship Between the Five-Factor Model of Personality and Symptoms of Clinical Disorders: A Meta-Analysis. Journal of Psychopathology and Behavioral Assessment, 27(2), 101–114. doi: 10.1007/s10862-005-5384-y [DOI] [Google Scholar]
- 26.John OP, Srivastava S. The big-five trait taxonomy: History, measurement and theoretical perspectives In Pervin LA & John OP (Eds.), Handbook of personality: Theory and research (Vol. 2, pp. 102–138). New York: Guilford Press; 1999. [Google Scholar]
- 27.McCrae RR, & Costa PT Jr., (2010). NEO Inventories: Professional manual. Lutz, FL: Psychological Assessment Resources, Inc. [Google Scholar]
- 28.McCrae RR; Costa PT (1983). “Joint factors in self-reports and ratings: Neuroticism, extraversion and openness to experience”. Personality and Individual Differences. 4 (3): 245–255. [Google Scholar]
- 29.Connor KM, Davdison JRT. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. 2003;18:76–82. [DOI] [PubMed] [Google Scholar]
- 30.Derogatis LE, Cleary PA. Confirmation of the dimensional structure of the SCL-90: A study in construct validation. J Clin Psychol. 1977;33(4):981–989. [Google Scholar]
- 31.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: 2016. https://www.R-project.org/ [Google Scholar]
- 32.Desrosiers A, Vine V, Klemanski DH, Nolen-Hoeksema S. Mindfulness and emotion regulation in depression and anxiety: Common and distinct mechanisms of action. Depress Anxiety. 2013;30(7):654–661. doi: 10.1002/da.22124 [DOI] [PMC free article] [PubMed] [Google Scholar]