Abstract
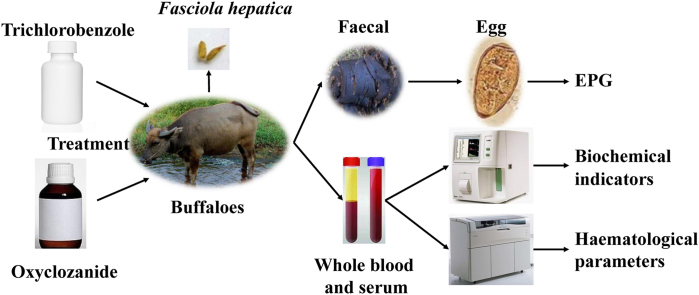
Fasciola hepatica is a common parasite of grazing livestock in Guangxi Zhuang Autonomous Region in China, but its prevalence has not been studied. While triclabendazole is commonly used to treat F. hepatica infection in China, oxyclozanide has never been used. This study investigated the prevalence of F. hepatica infections in buffaloes in the Guangxi and evaluated the efficacy of oxyclozanide and triclabendazole as treatments. In the prevalence study, a total of 767 individual faecal samples were obtained from 58 farms in Guangxi to detect the prevalence of F. hepatica, and the total rate of infection was 87.35%. A subset of 277 infected buffaloes from these farms were randomly divided into 3 groups. Group 1 (n = 101) was treated with oxyclozanide at 10 mg/kg.bw; group 2 (n = 94) was treated with triclabendazole (12 mg/kg.bw); and group 3 (n = 82) was untreated. Faecal samples were taken on days 0, 7, 14, 21 and 28. Whole blood and serum were collected on days 0 and 14. Anthelmintic efficacy was assessed using faecal egg count reduction (FECR), buffaloes positive by coprology reduction (BPCR) as well as post-treatment improvement in biochemical and haematological indicators. After 28 days treatment, group 1 and 2 showed FECR% values above 98%, and BPCR% values of 97.03% and 77.66%, respectively. In addition, the biochemical indicators and haematological parameters were improved at 14 days post-treatment compared with those before treatment. These results indicate a high prevalence of F. hepatica in Guangxi, demonstrate that oxyclozanide and triclabendazole are effective against F. hepatica infection in buffaloes, and indicate that oxyclozanide could be used in China as an alternative drug.
Keywords: Fasciola hepatica, Buffaloes, Prevalence, Oxyclozanide, Triclabendazole, Efficacy
Abbreviations: F. hepatica, Fasciola hepatica; F. gigantica, Fasciola gigantica; FECR, faecal egg count reduction; BPCR, buffaloes positive by coprology reduction; EPG, eggs per gram; EDTA, ethylenediaminetetraacetic acid; RBCs, red blood cells; Hb, haemoglobin; PCV, packed cell volume; WBCs, white blood cells; EOS, eosinophils; TP, total protein; A, albumin; AST, aspartate aminotransferase; ALT, alanine aminotransferase; GGT, γ-glutamyl transpeptidase; LDH, lactate dehydrogenase; GLU, glucose; ALP, alkaline phosphatase
Graphical abstract
Highlights
-
•
The prevalence of F. hepatica infections in 767 buffaloes was 87.35% on 58 farms from 8 districts in Guangxi Zhuang Autonomous Region in China.
-
•
Oxyclozanide and triclabendazole effectively restored the health of infected buffaloes and reduced the EPG of F. hepatica.
1. Introduction
Fasciolosis is a parasitic disease, caused by Fasciola hepatica (F. hepatica) and Fasciola gigantica (F. gigantica), leading to substantial financial losses and affecting human health (Zhang et al., 2004). It is estimated that 2.4–7 million people are infected and 90 million people are at risk (Keiser and Utzinger, 2005). More than 700 million domestic animals are at risk worldwide, with economic losses exceeding US$ 2 billion per year (Spithill and Dalton, 1998). Fasciolosis is geographically widely dispersed in Africa, Asia, Europe, the Americas and Oceania, as well as other temperate countries and regions (Mas-Coma et al., 2005; Mehmood et al., 2017). In China, it is prevalent throughout the north to Heilongjiang Province, south to Yunnan and Guangdong Provinces, east to Jiangsu and Taiwan Provinces, and west to Gansu and Xinjiang Provinces (Yuan et al., 2016). Approximately 28.5% of sheep were infected by F. hepatica in Heilongjiang Province from 1999 to 2003 (Wang et al., 2006). The prevalence of F. hepatica and F. gigantica in buffaloes in Hunan Province was 44.7% and 24.9%, respectively (Liu et al., 2009). Gansu Province has a prevalence F. hepatica ranging from 21.8% to 39.1% in yaks (Zhang et al., 2017). The cattle in Haikou have a seropositive rate of 19.92% (Wang, 2012, in Chinese). Moreover, fascioliasis outbreaks caused by F. gigantica have been reported in Yunnan (Chen et al., 2013).
Guangxi Zhuang Autonomous Region is located in the southern part of China (Sohn et al., 2009), and has one of the largest buffalo populations in China. Both F. hepatica and F. gigantica infection are frequently found in buffaloes in Guangxi Province; the serum positive rate of buffaloes infected with F. gigantica in suburbs of Qinzhou city in Guangxi was 38.57% (He et al., 2010, in Chinese). Indirect ELISA showed that the seropositive rates of buffaloes infected with Fasciola in most areas in Guangxi were between 60% and 80% (Passi et al., 2009, in Chinese). These reports were all published in Chinese journals, but the information about the prevalence of F. hepatica in buffaloes is limited. The objective of the present study was to investigate the prevalence of F. hepatica infection in Guangxi Province and provide baseline information for estimating the effectiveness of control and treatment strategies against F. hepatica infection in buffaloes in Guangxi.
Currently, the control of fasciolosis in animals relies on the use of anthelmintic drugs, such as albendazole, rafoxanide, and triclabendazole. Triclabendazole is commonly used to treat fascioliasis in China (Zhang et al., 2010; Wang, 2012; Feng, 2011; Zhang, 2011; Li et al., 2017; Wang et al., 2016; in Chinese). Oxyclozanide is also widely used to treat infections caused by F. gigantica and F. hepatica as well as other intestinal trematodes and gastrointestinal nematodes (Alam et al., 2015; Arafa et al., 2015; Foreyt and Todd, 1974; Paraud et al., 2009a, 2009b; Rolfe and Boray, 1987; Shokier et al., 2013); however, oxyclozanide has never been used in China. The present study also evaluated the efficacy of triclabendazole and oxyclozanide against F. hepatica in naturally infected buffaloes.
2. Materials and methods
2.1. Site location and sample collection for the prevalence study
F. hepatica infection is determined in epidemiological surveys via faecal egg detection. A total of 767 individual faecal samples for F. hepatica egg detection testing were collected from the rectums of randomly selected buffaloes on 58 farms from Wuzhou, Liuzhou, Yizhou, Jiangzhou, Yulin, Baise, Guilin and Chongzuo in Guangxi Zhuang Autonomous Region. The samples were stored at 4 °C in self-sealing polyethylene bags labelled with the management number of each buffalo. The presence of F. hepatica eggs in the faeces was determined using a modified sedimentation technique (Arafa et al., 2015; Mooney et al., 2009).
All experimental methods, animal care and the barn environment in this study were in strict accordance with the Guide for the Care and Use of Laboratory Animals, Lanzhou Institute of Husbandry and Pharmaceutical Sciences, China. All efforts were made to minimize suffering.
2.2. Evaluation of drug efficacy
In a preliminary experiment aiming to determine the optimal dosage of oxyclozanide, a dose confirmation test of oxyclozanide was performed before the anthelmintics efficacy test. Sixty buffaloes infected with F. hepatica were randomly divided into 4 groups, with 15 buffaloes in each group, and treated with oxyclozanide at 5 mg/kg, 10 mg/kg, 20 mg/kg or without treated as control, respectively. Accordingly, the optimate dosage of oxyclozanide is 10 mg/kg.bw (Table S1).
Two-hundred seventy-seven buffaloes that had been naturally infected with F. hepatica from the above 58 farms were used to evaluate the efficacy of anti-fasciolosis drugs. The buffaloes were of both sexes, ranged in age from 1.5 to 3 years, and weighed between 200 and 300 kg. The buffaloes examined had not been treated recently. The buffaloes were randomly divided into 3 groups (Table 1). Group 1 was administered oxyclozanide (10 mg/kg.bw, n = 101), group 2 was administered triclabendazole (12 mg/kg.bw, n = 94) (Elitok et al., 2006), and group 3 was untreated and considered the control group (n = 82). The animals were administered the drugs once orally, and the dose was based on live weight. All buffaloes were maintained under nearly identical conditions, and enough water and food were provided. The efficacy of anthelmintics was assessed according to the FECR, buffaloes positive by coprology reduction (BPCR) based on the values on days 21 and 28 as well as improvements in biochemical indicators and haematological parameters post-treatment.
Table 1.
Experimental drugs, groups and doses.
| Groups | Number of animals | Anthelmintics | Dosage (mg/kg.bw) |
|---|---|---|---|
| 1 | 101 | Oxyclozanide | 10 mg/kg.bw |
| 2 | 94 | Triclabendazole | 12 mg/kg.bw |
| 3 | 82 |
2.2.1. Eggs per gram (EPG), FECR and BPCR
During the experimental period, clinical manifestations were observed. Individual faecal samples were examined at days 0 (before treatment), 7, 14, 21 and 28 after treatment. Eggs per gram (EPG) was ascertained using the sedimentation technique as described above. FECR for each group as calculated using three different methods described by Brockwell et al. (2014): Method 1 is the technique recommended by the World Association of the Advancement of Veterinary Parasitology, which compares post-treatment arithmetic means of treated and control groups (Coles et al., 1992); Method 2 uses means of individual animal pre- and post-treatment counts to derive individual FECR reductions (Pook et al., 2002); Method 3 uses changes in the untreated control group means to correct for changes in FECR between collection dates using arithmetic means (Dash et al., 1988). Buffaloes positive by coprology reduction (BPCR) is the % of animals with no eggs after treatment and were determined using the following formulas (Arias et al., 2013; Athar et al., 2011):
| (1) |
Positive buffaloespre-treatment is the total number of infected buffaloes before treatment. Positive buffaloespost-treatment is the number of infected buffaloes after treatment. The efficacy of anthelmintics were determined based on the values on days 21 and 28 (Wood et al., 1995), and the difference in EPG between days 21 or 28 and 0 were calculated.
2.2.2. Haematological and biochemical analysis
To evaluate the changes in haematological and biochemical parameters after drug treatment, two venous blood samples were aseptically obtained from each buffalo on day 0 (before treatment) and day 14 (post-treatment). One sample was immediately transferred into a vacutainer containing ethylenediaminetetraacetic acid (EDTA) anticoagulant and maintained at 4 °C, and the other was collected into a vacutainer without anticoagulant and centrifuged at 3000 rpm for 10 min to separate the serum. Serum samples were then frozen at −20 °C.
The whole blood samples with EDTA anticoagulant were transferred to the laboratory, and haematological studies were performed using a veterinary automatic blood cell analyser (BC-2800Vet, Shenzhen Mindray Bio-Medical Electronics Co., Ltd, China). The following haematological parameters were measured: red blood cells (RBCs), haemoglobin (Hb), packed cell volume (PCV), white blood cells (WBCs) and eosinophils (EOS).
The concentrations of total protein (TP), albumin (A), aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyl transpeptidase (GGT), lactate dehydrogenase (LDH), glucose (GLU), and alkaline phosphatase (ALP) were measured in the serum samples using commercially available kits (Ningbo Meikang Biotechnology Co., Ltd, China) and an automatic biochemical analyser (XL-640, Erbe China Ltd, China).
2.3. Statistical analysis
Descriptive data are presented as means ± standard deviations (SD). Significant differences were determined using the Mann-Whitney test for variance at P < 0.05 using the SPSS 13.0 Windows statistical package (2004).
3. Results
3.1. Faecal egg detection test and prevalence study
The results in Table 2 indicate that the districts in Guangxi were positive for F. hepatica, with infection rates ranging from 71.91 to 95.65%. These rates suggest that relatively high F. hepatica burdens are present. The total rate of infection in all 767 buffaloes was 87.35%.
Table 2.
Prevalence of F. hepatica infection in each district based on the faecal egg detection.
| Districts | Number of farms | Mean buffaloes/farm | Number of animals/district | Animals positive | Prevalence (%) |
|---|---|---|---|---|---|
| Wuzhou | 8 | 11.13 | 89 | 64 | 71.91 |
| Liuzhou | 8 | 14.75 | 118 | 104 | 88.14 |
| Yizhou | 12 | 20.50 | 246 | 211 | 85.77 |
| Jiangzhou | 4 | 8.25 | 33 | 29 | 87.88 |
| Yulin | 6 | 11.50 | 69 | 66 | 95.65 |
| Baise | 4 | 15.50 | 62 | 56 | 90.32 |
| Guilin | 10 | 10.00 | 100 | 95 | 95.00 |
| Chongzuo | 6 | 8.33 | 50 | 45 | 90.00 |
| Total | 58 | 13.22 | 767 | 670 | 87.35 |
3.2. Flukicidal efficacy test
During the flukicidal efficacy test, the clinical signs observed in the affected buffaloes were anorexia and persistent diarrhoea. The buffaloes recovered from their illness within 28 days post-treatment. There was an improvement in body weight following the administration of flukicide. Table 3 shows the mean EPG in faeces of each group on each day, and EFCR% was calculated at days 21 and 28 using 3 different methods. The treatment groups showed a significant (P < 0.05) reduction in EPG on days 7–28. All three methods of calculation were in agreement that the FECR% values in groups 1 and 2 were up to 98%, which indicated the good efficacy of the drugs. Furthermore, the majority of the oxyclozanide-treated buffaloes had nearly zero EPG at the end of the experiment according to the BPCR of 97.03%, whereas the BPCR% in the triclabendazole treatment group was 77.66%. The EPG for group 3 (untreated) did not show a significant change throughout the experimental period.
Table 3.
Eggs per gram (EPG), faecal egg count reduction (FECR) and buffaloes positive by coprology reduction (BPCR).
| Days | EPG ± SD |
FECR% (day 21) |
FECR% (day 28) |
BPCR (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-treatment |
Post-treatment |
Methods |
Methods |
|||||||||
| 0 | 7 | 14 | 21 | 28 | 1 | 2 | 3 | 1 | 2 | 3 | ||
| Group1 | 106.21 ± 41.19 | 42.34 ± 22.19∗ | 3.33 ± 8.77∗ | 1.53 ± 5.14∗ | 0.28 ± 1.67∗ | 98.56 | 98.56 | 98.55 | 99.73 | 99.74 | 99.73 | 97.03 |
| Group 2 | 100.89 ± 45.46 | 27.69 ± 20.91∗ | 17.45 ± 17.72∗ | 1.39 ± 3.04∗ | 1.63 ± 3.87∗ | 98.69 | 98.62 | 98.61 | 98.46 | 98.38 | 98.37 | 77.66 |
| Group 3 | 106.74 ± 41.02 | 101.69 ± 24.23 | 96.85 ± 20.50 | 107.14 ± 23.04 | 106.02 ± 17.76 | |||||||
The mean EPG of buffaloes from each group was counted at days 0, 7, 14, 21 and 28 after treatment. FECR% were calculated at days 21 and 28 by the three methods (Method 1 was the WAAVP method; Method 2 calculated individual buffalo reductions followed by transformation and averaging; Method 3 accounted for changes in control values over time and used group means).
Significant differences of EPG between pre-treatment and post-treatment in each group were determined using the Mann-Whitney test.
* = Significant at the 5% level (P < 0.05).
3.3. Haematological and biochemical analyses
Table 4 summarizes the haematological parameters of buffaloes in each group on days 0 and 14 post-treatment. F. hepatica infection in group 3 exhibited a decreasing trend in Hb, RBC, and PCV values between days 0 and 14. WBC and EOS levels were elevated in group 3 (day 14: 12.9 ± 1.8 and 0.009 ± 0.019, respectively) compared to values obtained before the experiment (day 0: 12.5 ± 1.7 and 0.006 ± 0.009, respectively). However, for the oxyclozanide and triclabendazole treatment, there were increased trends in Hb, RBC and PCV with respect to the values obtained before the experiment in groups 1 and 2, and the drug treatment also caused a decreased trend in WBC and EOS levels on day 14 compared to those on day 0, although these changes were not significant compared with those at day 0.
Table 4.
Haematological parameters of the buffaloes on days 0 and 14 post-treatment.
| Groups | Day | WBC (109/L) | EOS (109/L) | RBC (1012/L) | Hb (g/L) | PCV (%) |
|---|---|---|---|---|---|---|
| 1 | 0 | 12.8 ± 2.6 | 0.009 ± 0.011 | 5.7 ± 1.2 | 111 ± 15 | 34.8 ± 6.6 |
| 14 | 12.5 ± 2.0 | 0.004 ± 0.005∗ | 6.1 ± 1.2 | 115 ± 14 | 37.1 ± 5.6 | |
| 2 | 0 | 12.2 ± 1.1 | 0.006 ± 0.011 | 5.8 ± 0.6 | 115 ± 15 | 34.1 ± 3.4 |
| 14 | 12.1 ± 1.2 | 0.005 ± 0.007 | 5.9 ± 0.7 | 116 ± 10 | 36.5 ± 6.2 | |
| 3 | 0 | 12.5 ± 1.7 | 0.006 ± 0.009 | 5.8 ± 0.7 | 115 ± 11 | 33.7 ± 3.3 |
| 14 | 12.9 ± 1.8 | 0.009 ± 0.019 | 5.5 ± 0.8 | 113 ± 13 | 32.2 ± 5.0 |
The above values represent the mean ± SD of buffaloes from each group.
Significant differences between days 0 and 14 in each group were determined.
* = Significant at the 5% level (P < 0.05).
Table 5 shows the biochemical parameters of buffaloes in each group on days 0 and 14 post-treatment. Mean values for TP, A, and GLU decreased over time in group 3, while AST (P < 0.05), ALT, GGT, LDH and ALP (P < 0.05) values increased. Treatment with oxyclozanide or triclabendazole resulted in improvements trend in these values on day 14 of the experiment compared with the day 0 values; in particular, the concentrations of GGT were significantly decreased (P < 0.05) in groups 1 and 2.
Table 5.
Biochemical parameters of the buffaloes on days 0 and 14 post-treatment.
| Groups | Day | TP (g/L) | A (g/L) | AST (U/L) | ALT (U/L) | GGT (U/L) | LDH (U/L) | GLU (mmol/L) | ALP (μmol/L) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 0 | 72.4 ± 8.8 | 22.9 ± 2.9 | 207 ± 35 | 36.0 ± 14.0 | 29.3 ± 7.5 | 828 ± 147 | 0.5 ± 0.3 | 182 ± 31 |
| 14 | 72.9 ± 9.2 | 23.9 ± 3.3 | 198 ± 38 | 34.9 ± 9.0 | 25.1 ± 7.2∗ | 821 ± 129 | 0.6 ± 0.2 | 180 ± 45 | |
| 2 | 0 | 73.1 ± 15.2 | 23.5 ± 2.9 | 198 ± 93 | 33.9 ± 4.7 | 30.0 ± 5.0 | 815 ± 102 | 0.5 ± 0.2 | 163 ± 57 |
| 14 | 74.0 ± 8.6 | 25.3 ± 3.7∗ | 187 ± 34 | 32.9 ± 7.7 | 25.2 ± 5.8∗ | 812 ± 81 | 0.5 ± 0.3 | 162 ± 41 | |
| 3 | 0 | 74.8 ± 10.0 | 23.0 ± 3.1 | 209 ± 35 | 33.3 ± 7.0 | 29.6 ± 6.1 | 835 ± 167 | 0.5 ± 0.2 | 161 ± 50 |
| 14 | 73.6 ± 11.0 | 22.7 ± 4.3 | 241 ± 32∗ | 36.6 ± 7.6 | 31.9 ± 5.2 | 860 ± 80 | 0.3 ± 0.1 | 167 ± 30∗ |
The above values represent the mean ± SD of buffaloes from each group.
Significant differences between days 0 and 14 in each group were determined.
* = Significant at the 5% level (P < 0.05).
4. Discussion
Temperature, water and snail are important factors in the epidemicity of F. hepatica. At the same time, rainfall has a positive effect on the development of F. hepatica and reproduction of the snail intermediate host (Mas-Coma et al., 2009; Novobilsky et al., 2014; Qin et al., 2016). The present study confirmed 87.35% prevalence of F. hepatica infections in buffaloes on 58 farms from 8 districts in Guangxi, this is consistent with the results of F.gigantica in Guangxi reported by Passi et al. (2009, in Chinses). This high prevalence may be due to the favourable climate, abundance of aquatic sources and rainfall in Guangxi, which make it a good habitat for F. hepatica's intermediate snail host. Furthermore, local buffaloes are mostly raised in a free-range way, which exposes buffaloes more access to intermediate hosts (He et al., 2010, in Chinese). In addition, buffaloes are most susceptible to severe infections when they are reared and grazed in narrow and humid paddy fields for a long time. Domestic buffaloes can also be infected by mowing grass from low-lying wet pastures (Wang, 2012. in Chinese). As buffaloes are the main labour animal, buffalo farming constitutes an important agricultural sector in Guangxi Province; buffaloes are raised and kept as economically important animals because they provide milk, meat and hides of good quality (Yang et al., 1998). F. hepatica infection of buffaloes is common and may cause considerable economic losses to the buffalo industries and farming communities as a consequence of the death of infected animals and reduced weight gains (Charlier et al., 2014; Chen et al., 2000; Schweizer et al., 2005). Therefore, the high prevalence of infection indicates that control strategies must be implemented.
Effective drugs to control fasciolosis are in urgent need. According to the guidelines from the World Association for the Advancement of Veterinary Parasitology for fasciolosis diagnosis, efficacy is determined by comparing faecal egg counts from treated and untreated animals shortly before or at the time of treatment and not less than 3 weeks later (Wood et al., 1995). Other researchers have estimated the efficacy of anthelmintics against Fasciola spp. at two weeks post-treatment (Arafa et al., 2015; Mooney et al., 2009; Ortiz et al., 2013; Shokier et al., 2013). However, eggs can be stored in the gall bladder for several weeks, even after removal of the adult flukes. Therefore, the measurement interval must be long enough to ensure that any eggs in the gall bladder are expelled from the animals following drug treatment (Arafa et al., 2015). The efficacy of anthelmintics against F. hepatica was evaluated over a period of 28 days in this clinical trial.
As an uncoupling agent, the antihelminth efficacy test clearly showed that oxyclozanide has high efficacy against fascioliasis yielded a 98.55% reduction in FECR on day 21 post-treatment and up to a 99.74% reduction in FECR on day 28, this finding is consistent with the results of Shokier et al. (2013). Additionally, the positive by coprology reduction can be used to determine whether the eggs have been completely removed. The animals in the oxyclozanide treated group were close to egg-free following the maximum BPCR of 97.03%, which indicated the eggs in most buffaloes had been completely removed. This high efficacy may be due to oxyclozanide blocks oxidative phosphorylation and inhibits ATP production in the mitochondria of this parasite, causing it to die due to energy metabolism disorders (Corbett and Goose, 1971; Probert et al., 1981; Shaheen, 2013; Veenendaal and de Waal, 1974). However, triclabendazole, which targets both the tissue-damaging immature stages and the mature adult stages of the parasites (Cwiklinski et al., 2016), showed the BPCR% was 77.66% after 28 days treatment, which is lower than that in oxyclozanide treatment group. This may be due to triclabendazole treatment did not repelled all F. hepatica in individual buffaloes. Although the resistance to this drug has been frequently reported in other areas (Elliott et al., 2015; Hanna, 2015; Kelley et al., 2016; Morphew et al., 2012; Nzalawahe et al., 2018; Olaechea et al., 2011; Ortiz et al., 2013; Toet et al., 2014), our study indicated that triclabendazole is still effective against F. hepatica infection in Guangxi Province based on the FECR of up to 98%. Furthermore, oxyclozanide may be an alternative drug for fascioliasis in China.
In addition, F. hepatica parasitizes the intrahepatic bile duct, causing liver or bile duct damage, which influences the normal values of biochemical indicators and haematological parameters. In infected untreated group 3, there were minor decreases in the mean values of RBC, Hb, PCV, TP, A, and GLU. The changes in RBC, Hb and PCV may due to the secretory toxins of F. hepatica, which exert haemolytic effects and haemorrhage, leading to anaemia, anaemia also results from blood digestion by adult flukes. The decreases in TP and A levels are likely due to the reduced albumin synthesis and increased plasma protein leakage into the gut associated with fasciolosis. AST, GGT and ALT levels are important indicators of the degree of cholestasis and the synthetic capacity of the liver (Shrimali et al., 2016). Elevated levels of the serum enzymes AST and ALT were observed in the infected buffaloes, possibly due to extensive damage to the liver parenchyma, the production of hepatotoxins and cellular necrosis. Furthermore, the marked increase in GGT level associated with cholestasis and bile duct damage. Damage to the bile duct epithelium causes the release of GGT into the circulation, which increases the GGT level in serum mainly after flukes have entered the bile duct (Matanovic et al., 2007). Additionally, elevated levels of LDH and ALP, which are also indicators of damage to the liver parenchyma and bile ducts, are caused by the migration of F. hepatica (Mooney et al., 2009). In F. hepatica-infected hosts, hepatic parenchymal injury and abnormal hepatic function not only decrease the concentration of GLU but also cause an immune response in the host, leading to increased WBC, particularly in EOS (Escamilla et al., 2016). However, gradual decreases in the mean values of WBC, EOS, AST, ALT, GGT, LDH and ALP were recorded along with gradual increases in the mean values of RBC, Hb, PCV, TP, A, and GLU in the oxyclozanide and triclabendazole treatment groups. These results are consistent with previous studies (Roy et al., 2004; Shaheen, 2013; Shokier et al., 2013; Shrimali et al., 2016).The recovery of altered biochemical indicators and haematological parameters may have been due to flukicide activity of oxyclozanide and triclabendazole.
5. Conclusion
This study has demonstrated a high prevalence in Guangxi Province of F. hepatica, and revealed that oxyclozanide and triclabendazole effectively restored the health of infected buffaloes and reduced the EPG of F. hepatica by killing the parasite. Oxyclozanide could be a useful alternative drug for F. hepatica infection in China.
Declarations of interest
All authors declare the absence of any financial or personal interests that could inappropriately influence the current work. The final article has been approved by all authors.
Author contributions
Hong-Fei Si, Xiao-Fei Shang, Xu-Zheng Zhou and Bing Li participated in the clinical trial. Ji-Yu Zhang designed the study and critically revised the manuscript. Ji-Li Zhang supervised the experiments and wrote the manuscript. All authors read and approved the final manuscript.
Conflicts of interest
All authors declare the absence of any financial or personal interests that could inappropriately influence the current work. The final article has been approved by all authors.
Role of the funding source
This work was supported by the Key Project in the National Science and Technology Pillar Program during the Twelfth Five-year Plan Period (2015BAD1101) and by the earmarked fund for the China Agriculture Research System (CAR-37).
Acknowledgements
The authors are grateful to the staff in the Veterinary Research Institute of Guangxi Zhuang Autonomous Region for their help.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijppaw.2018.12.010.
Contributor Information
Ji-Li Zhang, Email: zhangjlzjl@sina.com.
Hong-Fei Si, Email: shf5162629@163.com.
Xu-Zheng Zhou, Email: zhxuzheng@163.com.
Xiao-Fei Shang, Email: shangxf928@126.com.
Bing Li, Email: pharm2005bl@126.com.
Ji-Yu Zhang, Email: infzjy@sina.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alam N., Islam M., Howlader M., Lucky N. Effects of oxyclozanide (Tremacid®) preparation against fascioliasis on clinical and haematological parameters in cattle of Bangladesh. Int. J. Biol. Res. 2015;3:46–55. [Google Scholar]
- Arafa W.M., Shokeir K.M., Khateib A.M. Comparing an in vivo egg reduction test and in vitro egg hatching assay for different anthelmintics against Fasciola species, in cattle. Vet. Parasitol. 2015;214:152–158. doi: 10.1016/j.vetpar.2015.09.023. [DOI] [PubMed] [Google Scholar]
- Arias M.S., Sanchis J., Francisco I., Francisco R., Pineiro P., Cazapal-Monteiro C., Cortinas F.J., Suarez J.L., Sanchez-Andrade R., Paz-Silva A. The efficacy of four anthelmintics against Calicophoron daubneyi in naturally infected dairy cattle. Vet. Parasitol. 2013;197:126–129. doi: 10.1016/j.vetpar.2013.06.011. [DOI] [PubMed] [Google Scholar]
- Athar L.A., Khan M.N., Sajid M.S., Tauseef ur R., Khan I.A. Cost benefits analysis of anthelmintic treatment of cattle and buffaloes. Pakistan Vet. J. 2011;31:149–152. [Google Scholar]
- Brockwell Y.M., Elliott T.P., Anderson G.R., Stanton R., Spithill T.W., Sangster N.C. Confirmation of Fasciola hepatica resistant to triclabendazole in naturally infected Australian beef and dairy cattle. Int. J. Parasitol. Drugs Drug Resist. 2014;4:48–54. doi: 10.1016/j.ijpddr.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlier J., Vercruysse J., Morgan E., van Dijk J., Williams D.J. Recent advances in the diagnosis, impact on production and prediction of Fasciola hepatica in cattle. Parasitology. 2014;141:326–335. doi: 10.1017/S0031182013001662. [DOI] [PubMed] [Google Scholar]
- Chen J.X., Chen M.X., Ai L., Xu X.N., Jiao J.M., Zhu T.J., Su H.Y., Zang W., Luo J.J., Guo Y.H., Lv S., Zhou X.N. An Outbreak of Human Fascioliasis gigantica in Southwest China. PLoS One. 2013;8 doi: 10.1371/journal.pone.0071520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Daugschies A., Wang B., Mao X. Blood eicosanoids and immune indices during fasciolosis in water buffaloes. Parasitol. Int. 2000;49:273–278. doi: 10.1016/s1383-5769(00)00056-8. [DOI] [PubMed] [Google Scholar]
- Coles G.C., Bauer C., Borgsteede F.H., Geerts S., Klei T.R., Taylor M.A., Waller P.J. World Association for the Advancement of Veterinary Parasitology (W.A.A.V.P.) methods for the detection of anthelmintic resistance in nematodes of veterinary importance. Vet. Parasitol. 1992;44:35–44. doi: 10.1016/0304-4017(92)90141-u. [DOI] [PubMed] [Google Scholar]
- Corbett J.R., Goose A.J. The biochemical mode of action of the fasciolicides nitroxynil, hexachlorophane and oxyclozanide. Biochem. J. 1971;121 doi: 10.1042/bj1210041pa. 41P. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cwiklinski K., O'Neill S.M., Donnelly S., Dalton J.P. A prospective view of animal and human Fasciolosis. Parasite Immunol. 2016;38:558–568. doi: 10.1111/pim.12343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dash K.M., Hall E., Barger I.A. The role of arithmetic and geometric mean worm egg counts in faecal egg count reduction tests and in monitoring strategic drenching programs in sheep. Aust. Vet. J. 1988;65:66–68. doi: 10.1111/j.1751-0813.1988.tb07359.x. [DOI] [PubMed] [Google Scholar]
- Elitok B., Elitok O.M., Kabu M. Field trial on comparative efficacy of four fasciolicides against natural liver fluke infection in cattle. Vet. Parasitol. 2006;135:279–285. doi: 10.1016/j.vetpar.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Elliott T.P., Kelley J.M., Rawlin G., Spithill T.W. High prevalence of fasciolosis and evaluation of drug efficacy against Fasciola hepatica in dairy cattle in the Maffra and Bairnsdale districts of Gippsland, Victoria, Australia. Vet. Parasitol. 2015;209:117–124. doi: 10.1016/j.vetpar.2015.02.014. [DOI] [PubMed] [Google Scholar]
- Escamilla A., Bautista M.J., Zafra R., Pacheco I.L., Ruiz M.T., Martinez-Cruz S., Mendez A., Martinez-Moreno A., Molina-Hernandez V., Perez J. Fasciola hepatica induces eosinophil apoptosis in the migratory and biliary stages of infection in sheep. Vet. Parasitol. 2016;216:84–88. doi: 10.1016/j.vetpar.2015.12.013. [DOI] [PubMed] [Google Scholar]
- Feng L.X. Comprehensive control measures of Fasciola hepatica in cattle and sheep. Gansu Anim. Husb. Vet. Med. 2011;41(6):17–18. In Chinese. [Google Scholar]
- Foreyt W.J., Todd A.C. Efficacy of rafoxanide and oxyclozanide against Fascioloides magna in naturally infected cattle. Am. J. Vet. Res. 1974;35:375–377. [PubMed] [Google Scholar]
- Hanna R. Fasciola hepatica: histology of the reproductive organs and differential effects of triclabendazole on drug-sensitive and drug-resistant fluke isolates and on flukes from selected field cases. Pathogens. 2015;4:431–456. doi: 10.3390/pathogens4030431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S.H., Bankman Guo Y.F. Investigation and analysis of Fasciola megafasciola infection in buffaloes in suburbs of Qinzhou City, Guangxi. J. South. Agri. 2010;41(11):1237–1239. In Chinese. [Google Scholar]
- Keiser J., Utzinger J. Emerging foodborne trematodiasis. Emerg. Infect. Dis. 2005;11:1507–1514. doi: 10.3201/eid1110.050614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley J.M., Elliott T.P., Beddoe T., Anderson G., Skuce P., Spithill T.W. Current threat of triclabendazole resistance in Fasciola hepatica. Trends Parasitol. 2016;32:458–469. doi: 10.1016/j.pt.2016.03.002. [DOI] [PubMed] [Google Scholar]
- Li C.Y., Jiao W.L., Wen J.F. Research and application status of trichlorobenzole at home and abroad. Chin. Anim. Husb. Vet. Abstr. 2017;33:63–64. In Chinese. [Google Scholar]
- Liu Y., Li F., Liu W., Dai R.S., Tan Y.M., He D.S., Lin R.Q., Zhu X.Q. Prevalence of helminths in water buffaloes in Hunan Province, China. Trop. Anim. Health Prod. 2009;41:543–546. doi: 10.1007/s11250-008-9219-1. [DOI] [PubMed] [Google Scholar]
- Mas-Coma S., Bargues M.D., Valero M.A. Fascioliasis and other plant-borne trematode zoonoses. Int. J. Parasitol. 2005;35:1255–1278. doi: 10.1016/j.ijpara.2005.07.010. [DOI] [PubMed] [Google Scholar]
- Mas-Coma S., Valero M.A., Bargues M.D. Climate change effects on trematodiases, with emphasis on zoonotic fascioliasis and schistosomiasis. Vet. Parasitol. 2009;163:264–280. doi: 10.1016/j.vetpar.2009.03.024. [DOI] [PubMed] [Google Scholar]
- Matanovic K., Severin K., Martinkovic F., Simpraga M., Janicki Z., Barisic J. Hematological and biochemical changes in organically farmed sheep naturally infected with Fasciola hepatica. Parasitol. Res. 2007;101:1657–1661. doi: 10.1007/s00436-007-0709-2. [DOI] [PubMed] [Google Scholar]
- Mehmood K., Zhang H., Sabir A.J., Abbas R.Z., Ijaz M., Durrani A.Z., Saleem M.H., Ur Rehman M., Iqbal M.K., Wang Y., Ahmad H.I., Abbas T., Hussain R., Ghori M.T., Ali S., Khan A.U., Li J. A review on epidemiology, global prevalence and economical losses of fasciolosis in ruminants. Microb. Pathog. 2017;109:253–262. doi: 10.1016/j.micpath.2017.06.006. [DOI] [PubMed] [Google Scholar]
- Mooney L., Good B., Hanrahan J.P., Mulcahy G., de Waal T. The comparative efficacy of four anthelmintics against a natural acquired Fasciola hepatica infection in hill sheep flock in the west of Ireland. Vet. Parasitol. 2009;164:201–205. doi: 10.1016/j.vetpar.2009.05.017. [DOI] [PubMed] [Google Scholar]
- Morphew R.M., Eccleston N., Wilkinson T.J., McGarry J., Perally S., Prescott M., Ward D., Williams D., Paterson S., Raman M., Ravikumar G., Khalid Saifullah M., Abbas Abidi S.M., McVeigh P., Maule A.G., Brophy P.M., LaCourse E.J. Proteomics and in silico approaches to extend understanding of the glutathione transferase superfamily of the tropical liver fluke Fasciola gigantica. J. Proteome Res. 2012;11:5876–5889. doi: 10.1021/pr300654w. [DOI] [PubMed] [Google Scholar]
- Novobilsky A., Engstrom A., Sollenberg S., Gustafsson K., Morrison D.A., Hoglund J. Transmission patterns of Fasciola hepatica to ruminants in Sweden. Vet. Parasitol. 2014;203:276–286. doi: 10.1016/j.vetpar.2014.04.015. [DOI] [PubMed] [Google Scholar]
- Nzalawahe J., Hannah R., Kassuku A.A., Stothard J.R., Coles G., Eisler M.C. Evaluating the effectiveness of trematocides against Fasciola gigantica and amphistomes infections in cattle, using faecal egg count reduction tests in Iringa Rural and Arumeru Districts, Tanzania. Parasites Vectors. 2018;11:384. doi: 10.1186/s13071-018-2965-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaechea F., Lovera V., Larroza M., Raffo F., Cabrera R. Resistance of Fasciola hepatica against triclabendazole in cattle in Patagonia (Argentina) Vet. Parasitol. 2011;178:364–366. doi: 10.1016/j.vetpar.2010.12.047. [DOI] [PubMed] [Google Scholar]
- Ortiz P., Scarcella S., Cerna C., Rosales C., Cabrera M., Guzman M., Lamenza P., Solana H. Resistance of Fasciola hepatica against Triclabendazole in cattle in Cajamarca (Peru): a clinical trial and an in vivo efficacy test in sheep. Vet. Parasitol. 2013;195:118–121. doi: 10.1016/j.vetpar.2013.01.001. [DOI] [PubMed] [Google Scholar]
- Paraud C., Fournier E., Robergeot V., Kulo A., Pors I., Baudry C., Chartier C. Calicophoron daubneyi infection in grazing goats: results from a cross-sectional coprological survey in France. Small Rumin. Res. 2009;82:66–68. [Google Scholar]
- Paraud C., Gaudin C., Pors I., Chartier C. Efficacy of oxyclozanide against the rumen fluke Calicophoron daubneyi in experimentally infected goats. Vet. J. 2009;180:265–267. doi: 10.1016/j.tvjl.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Passi R.S.L.D., Wang Dongying, Zhang Weiyu. Indirect ELISA survey of the epidemiological situation of buffalo Flagelliasis in Guangxi. Guangxi Anim. Husb. Vet. Med. 2009;25(4):214–215. In Chinese. [Google Scholar]
- Pook J.F., Power M.L., Sangster N.C., Hodgson J.L., Hodgson D.R. Evaluation of tests for anthelmintic resistance in cyathostomes. Vet. Parasitol. 2002;106:331–343. doi: 10.1016/s0304-4017(02)00093-6. [DOI] [PubMed] [Google Scholar]
- Probert A.J., Sharma R.K., Singh K., Saxena R. The effect of five fasciolicides on malate dehydrogenase activity and mortality of Fasciola gigantica, Fasciolopsis buski and Paramphistomum explanatum. J. Helminthol. 1981;55:115–122. doi: 10.1017/s0022149x0002558x. [DOI] [PubMed] [Google Scholar]
- Qin H., Gao X., Wang H., Xiao J. Relative importance of meteorological and geographical factors in the distribution of Fasciola hepatica infestation in farmed sheep in Qinghai province, China. Parasite. 2016;23:59. doi: 10.1051/parasite/2016070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolfe P.F., Boray J.C. Chemotherapy of paramphistomosis in cattle. Aust. Vet. J. 1987;64:328–332. doi: 10.1111/j.1751-0813.1987.tb06060.x. [DOI] [PubMed] [Google Scholar]
- Roy M., Galdhar C.N., Roy S. Efficacy of oxyclozanide against paramphistomiasis in buffaloes. Indian Vet. J. 2004;81:588–589. [Google Scholar]
- Schweizer G., Braun U., Deplazes P., Torgerson P.R. Estimating the financial losses due to bovine fasciolosis in Switzerland. Vet. Rec. 2005;157:188–193. doi: 10.1136/vr.157.7.188. [DOI] [PubMed] [Google Scholar]
- Shaheen H. Evaluation of oxyclozanide and niclosamide combination as alternative antiparamphistomal therapy in buffaloes. Afr. J. Pharm. Pharmacol. 2013;7:2157–2166. [Google Scholar]
- Shokier K.M., Aboelhadid S.M., Waleed M.A. Efficacy of five anthelmintics against a natural Fasciola species infection in cattle. Beni-Suef Univ. J. Basic Appl. Sci. 2013;2:41–45. [Google Scholar]
- Shrimali R.G., Patel M.D., Patel R.M. Comparative efficacy of anthelmintics and their effects on hemato-biochemical changes in fasciolosis of goats of South Gujarat. Vet. World. 2016;9:524–529. doi: 10.14202/vetworld.2016.524-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn W.M., Eom K.S., Min D.Y., Rim H.J., Hoang E.H., Yang Y., Li X. Fishborne trematode metacercariae in freshwater fish from Guangxi Zhuang Autonomous Region, China. Kor. J. Parasitol. 2009;47:249–257. doi: 10.3347/kjp.2009.47.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spithill T.W., Dalton J.P. Progress in development of liver fluke vaccines. Parasitol. today. 1998;14:224–228. doi: 10.1016/s0169-4758(98)01245-9. [DOI] [PubMed] [Google Scholar]
- Toet H., Piedrafita D.M., Spithill T.W. Liver fluke vaccines in ruminants: strategies, progress and future opportunities. Int. J. Parasitol. 2014;44:915–927. doi: 10.1016/j.ijpara.2014.07.011. [DOI] [PubMed] [Google Scholar]
- Veenendaal G.H., de Waal M.J. Uncoupling activity of the anthelmintic oxyclozanide in rodents. Br. J. Pharmacol. 1974;50:435–437. doi: 10.1111/j.1476-5381.1974.tb09622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Chen Q.S., Zeng F.Q. Prevention and control of fascioliasis of sheep. Sichuan Anim. Husb. Vet. Med. 2016;43(2) 50-50. In Chinese. [Google Scholar]
- Wang C.R., Qiu J.H., Zhu X.Q., Han X.H., Ni H.B., Zhao J.P., Zhou Q.M., Zhang H.W., Lun Z.R. Survey of helminths in adult sheep in Heilongjiang Province, People's Republic of China. Vet. Parasitol. 2006;140:378–382. doi: 10.1016/j.vetpar.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Wang S.M. Survey and control of fascioliasis of bovine. Cattle Sci. China. 2012;38:67–68. In Chinese. [Google Scholar]
- Wood I.B., Amaral N.K., Bairden K., Duncan J.L., Kassai T., Malone J.B., Jr., Pankavich J.A., Reinecke R.K., Slocombe O., Taylor S.M. World Association for the Advancement of Veterinary Parasitology (W.A.A.V.P.) second edition of guidelines for evaluating the efficacy of anthelmintics in ruminants (bovine, ovine, caprine) Vet. Parasitol. 1995;58:181–213. doi: 10.1016/0304-4017(95)00806-2. [DOI] [PubMed] [Google Scholar]
- Yang Q., Mao W.H., Ferre I., Bayon J.E., Mao X.Z., Gonzalez-Gallego J. Plasma aspartate aminotransferase (AST), glutamate dehydrogenase (GLDH) and gamma-glutamyl transpeptidase (GGT) activities in water buffaloes with experimental subclinical fasciolosis. Vet. Parasitol. 1998;78:129–136. doi: 10.1016/s0304-4017(98)00134-4. [DOI] [PubMed] [Google Scholar]
- Yuan W., Liu J.M., Lu K., Li H., Duan M.M., Feng J.T., Hong Y., Liu Y.P., Zhou Y., Tong L.B., Lu J., Zhu C.G., Jin Y.M., Cheng G.F., Lin J.J. Molecular identification and seasonal infections of species of Fasciola in ruminants from two provinces in China. J. Helminthol. 2016;90:359–363. doi: 10.1017/S0022149X15000383. [DOI] [PubMed] [Google Scholar]
- Zhang W., Moreau E., Huang W., Chauvin A. Comparison of humoral response in sheep to Fasciola hepatica and Fasciola gigantica experimental infection. Parasite. 2004;11:153–159. doi: 10.1051/parasite/2004112153. [DOI] [PubMed] [Google Scholar]
- Zhang X.L., Hou F.Q., Wang H.F. Diagnosis and control of fascioliasis in animals. Hubei Anim. Husb. Vet. Med. 2010;9:42–43. [Google Scholar]
- Zhang X.X., Feng S.Y., Ma J.G., Zheng W.B., Yin M.Y., Qin S.Y., Zhou D.H., Zhao Q., Zhu X.Q. Seroprevalence and risk factors of fascioliasis in yaks, bos grunniens, from three counties of Gansu Province, China. Kor. J. Parasitol. 2017;55:89–93. doi: 10.3347/kjp.2017.55.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.Q. Fasciola and fasciolasis. Guangxi Anim. Husb. Vet. Med. 2011;27:373–377. In Chinese. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.