Abstract
Background
The use of intravenous recombinant tissue plasminogen activator (IV r-tPA) in early acute ischemic stroke (AIS) management faces a lot of difficulties in developing countries due to lessened guideline development with consecutive pre- and intra-hospital delay.
Objectives
The objective was to identify the barriers facing proper utilization of IV r-tPA for AIS in Tanta University Hospitals.
Methods
The study was conducted on 4124 AIS patients eligible to use IV r-tPA divided to group-I consisting of 442 patients who arrived the hospital within <3.5 h from the stroke onset and group-II consisting of 3682 patients who arrived >3.5 h from the stroke onset. The former group was further subdivided to 238 patients who received IV r-tPA (group-Ia) and 204 patients who did not receive IV r-tPA (group-Ib) due to different obstacles.
Results
The main causes of pre-hospital onset to arrival delay were stroke unawareness, long travel time, incorrect beliefs, non-available neurologists, stroke onset during sleep and multiple causes (18.2%, 20.5%, 12.7%, 9.1%, 16% and 23.5% of cases, respectively). Causes of non-administration of IV r-tPA in eligible patients includes prolonged door-to-needle time, financial restraints, minor strokes, unavailable beds and fear of complications (41.2%, 26%, 12.7%, 11.3% and 8.8%, respectively).
Conclusion
Increasing the chance of utilizing IV r-tPA for AIS patients' needs regular updating of the stroke chain of survival system to get the highest benefits from the available resources.
Keywords: Tissue plasminogen activator, Therapeutic window, Stroke chain of survival, Pre-hospital delay, Door-to-needle time
Highlights
-
•
Stroke management faces a lot of difficulties in developing countries.
-
•
Only 5.8% of those were eligible for received IV thrombolysis.
-
•
Studied patients relatives were not aware about the therapeutic window despite their recognition of stroke symptoms.
-
•
Minor and non-motor strokes defects may mislead the on-duty doctor to withhold IV r-tPA in indicated cases.
1. Introduction
Cerebrovascular stroke (CVS) is the second most common cause of deaths (after ischemic heart disease) and the third most common cause of disability adjusted life years (after ischemic heart disease and cancer) [1]. The overall crude prevalence rate of stroke in Egypt is 963/100,000 inhabitants [2]. In 1996, the Food and Drug Administration (FDA) had approved IV r-tPA as the only therapy for early acute ischemic stroke (AIS) management and since this date, many efforts have been spent to reduce the stroke onset/needle time owing to the narrow therapeutic window of the drug [3].
Improving stroke outcome is based on enhanced care within the first hours of stroke onset through providing a well-organized stroke chain of survival (SCS), which is a dynamic process that needs continuous evaluation and quality assessment, to identify and solve gaps and disparities in providing early stroke care [4]. The American Heart Association/American Stroke Association (AHA/ASA) continuously update protocols and recommendations to assess the quality of SCS in which the pre-hospital onset to arrival time (OAT) and the intra-hospital door-to-needle time (DNT) should not exceed 35 and 60 min, respectively [5]. In developed countries, most hospitals adjust their programs to shorten the time of administrative procedures, clinical assessment, imaging and laboratory investigation for stroke patients to fit these guidelines [6]. While in developing countries, stroke management protocols face a lot of difficulties including low stroke awareness, weak finances and complex administrative procedures with subsequent higher mortalities and greater disabilities among their stroke patients [7].
1.1. Aim of the work
The aim of the work was to identify obstacles facing the proper use of IV r-tPA in AIS management in Tanta University Hospitals (TUHs) and propose possible recommendations to increase its utilization.
2. Patients and methods
The present work was a prospective observational cross-sectional study conducted on 4124 AIS patients eligible to IV r-tPA use and referred to the neurology emergency room (NER) of the Neuropsychiatry Department, TUHs in the period from November 1, 2017 till the end of October 2018. The study's protocol was approved by the local research ethics committee and quality assurance unit, Faculty of Medicine, Tanta University. Informed consents were obtained from all patients' or their first-degree relative.
Exclusion criteria encompassed patients with transient ischemic attacks (TIAs) who showed complete regression of the neurological deficit within 1-h and AIS patients with baseline contraindications for IV r-tPA (head trauma, stroke, myocardial infarction, major surgery or internal bleeding in the preceding 3 months as well as NIHSS > 22 and Alberta Stroke Program Early CT Score < 7).
Tanta University Hospitals are tertiary referral hospitals under the management of the Faculty of Medicine, Tanta University administered by the Ministry of Higher Education of Egypt. The hospitals have inpatients neurovascular units (NVUs) within the Neuropsychiatry Department as well as the Center of Neurology and Psychiatry which have 41 inpatients beds in a state of constant readiness for admission of AIS patients and administration of IV r-tPA. The NVUs had applied the AHA/ASA guidelines for early management of patients with AIS, 2018 [8] except in extending the time window of IV r-tPA use to 4.5 h relied on the European guidelines for AIS management [9]. During the period of the study, NVUs of TUHs are the only governmental place providing IV r-tPA in a 50-km radius area inhabitant by approximately 10 million Egyptian Citizens (one of the highest density population areas in Egypt). The hospitals are in the center of Tanta City, the capital of Gharbia Governorate which include seven other cities with their related villages. Tanta is approximately 10-km radius in the center of the Lower Egypt Nile Delta. The medical services of TUHs extend to parts of Al-Mennofia, Kafr El-Sheikh and Al-Behera Governorate.
The pre-hospital EMS transfer system is under the management of Directorate of Health Affairs in Gharbia Governorate which deliver AIS patients to the front emergency hospital in TUHs where the on-duty internal medicine residents assess the patients and then refer them to the NER in the main hospital located in another building 200 m away. The patients are reassessed by the on-duty neurology staff who applies NIHSS assessment and vital signs stabilization and then order CT brain imaging, which in turn; carried out in the diagnostic radiology department located in a third building 70 m away from the NER. After that, patients return to the NER and if IV r-tPA is indicated, the patients' relatives undergo the administrative procedures during which laboratory investigations are done in clinical pathology department in the above-mentioned emergency hospital. Patients’ relatives had to pay about 550 dollars to purchase r-tPA vials as the drug is provided in a paid service.
During the period of the study, 15,832 patients were delivered to the NER including 7125 (45%) cases with possible diagnosis of cerebrovascular accidents. The latter group consisted of 4836/7125 (67.9%) AIS patients, 216/7125 (3%) TIAs cases, 1716/7125 (24.1%) had hemorrhagic stroke and 357/7125 (5%) had stroke mimics state (functional hemiparesis, post-epileptic Todd's paralysis, syncope, hypoglycemia and brain tumors). 712/4836 (14.7%) AIS cases had baseline r-tPA contraindication and the remaining 4124/4836 (85.3%) cases were eligible to use IV r-tPA. The latter group was divided to group-I consisting of 442/4124 (10.7%) had OAT < 3.5 h from the stroke onset and group-II consisting of 3682/4124 (89.3%) with OAT > 3.5 h from the stroke onset. The former group was further subdivided to 238/442 (53.8%) patients who received IV r-tPA (group-Ia) and 204/442 (46.2%) patients did not receive IV r-tPA despite arrival within the attended OAT (group-Ib).
The attended arrival time in this study was <3.5 h from stroke onset, i.e. 1-h before expiry of the therapeutic window which is the DNT limit recommended by the AHA/ASA [6].
Stroke awareness was assessed in the patients or their relatives by asking them about recognition of stroke warning signs and limit of the therapeutic window. Subjects were asked about their knowledge of the items of the acronym FAST (face dropping, arm weakness, speech difficulty and time to call EMS service) and they were considered unaware if they did not know either stroke warning sign and/or the length of the therapeutic window.
Statistical analysis was conducted using SPSS Prism, version 20, 2013 created by IBM, Illinois, Chicago, USA. Statistical differences between the studied groups were tested using Chi-square for categorical variables and student t-test for numerical variables. P-value <.05 was considered statistically significant.
3. Results
The study had determined that, the mean pre-hospital onset arrival time (OAT) and intra-hospital door-to-needle time (DNT) for the studied patients were 147.2 ± 42.5 and 87.5 ± 16.4 min, respectively. The DNT in TUHs was spent as follows; emergency hospital assessment and NER transfer time was 17.6 ± 6.2 min, NER assessment and imaging transfer time was 19.3 ± 5.8 min, CT brain assessment and return to NER time was 34.9 ± 11.7 min, investigation time 18.4 ± 7.5 min and the administrative procedures time was 16.9 ± 6.4 min.
The study showed statistically significant increase in stroke awareness among patients and/or relatives of AIS patients with OAT < 3.5 h (group-I) compared to those arrived after expiry of this time (group-II) with p-value < .05. At the same time, group-I showed statistically significant decrease in the percent of patients from rural areas, those who live >10 km away from TUHs and nocturnal onset strokes patients with p-values < .05. On the other hand, there were statistically non-significant differences between group-I and group-II patients regarding their age, sex and site of stroke (whether anterior or posterior circulation) with p-value > .05 (Table 1).
Table 1.
Comparison between acute stroke patients who arrived 1-h before expiry of the IV r-tPA therapeutic window (group I) and those arrived after this time (group II).
| Group I (n: 442) | Group II (n: 3682) | Chi-square |
|||
|---|---|---|---|---|---|
| X2-value | p-value | ||||
| Age (mean ± SD) | 60.4 ± 5.7 | 59.6 ± 8.9 | 0.662 | 0.558 | |
| Sex | Male n (%) | 205 (46.4%) | 1899 (51.6%) | 4.2621 | 0.0389 |
| Female n (%) | 237 (53.6%) | 1783 (48.4%) | |||
| Residence | Urban n (%) | 316 | 1968 | 51.997 | <0.0001a |
| Rural n (%) | 126 | 1714 | |||
| Scene to hospital distance | <10 km n (%) | 278 | 1352 | 23.707 | <0.0001a |
| >10 km n (%) | 164 | 2330 | |||
| Stroke site | ACI n (%) | 327 | 2593 | 2.417 | 0.12 |
| PCI n (%) | 115 | 1089 | |||
| Stroke awareness | Aware n (%) | 374 | 1584 | 273.8 | <0.0001a |
| Unaware n (%) | 68 | 2098 | |||
| Stroke onset | Diurnal | 308 | 2244 | 12.587 | 0.0004a |
| Nocturnal | 134 | 1434 | |||
Significant, ACI: anterior circulation infarction, PCI: posterior circulation infarction.
The results of the present study showed that, stroke unawareness either due to non-recognition of stroke warning signs or therapeutic window limits was determined in 669/3682 (18.2%) of group-II patients who had OAT > 3.5 h. At the same time, 753/3682 (20.5%) of these patients had long travel time due to pre-arrival multiple consultation of stroke non-ready hospitals, weak and slow EMS services as well as strokes happened in rural and distant places. Incorrect beliefs were a third cause of pre-hospital delay occurred in 468/3682 (12.7%) included thinking that management is hopeless, waiting for spontaneous recovery and believing that the use of large dose of aspirin may liquefy the thrombus. Other causes of extraordinary prolonged OAT were non-available neurological guidance during holidays in 335/3682 (9.1%) of cases, stroke onset during sleep in 589/3682 (16%) of cases and multiple pre-mentioned factors in 868/3682 (23.5%) of cases (Fig. 1)
Fig. 1.
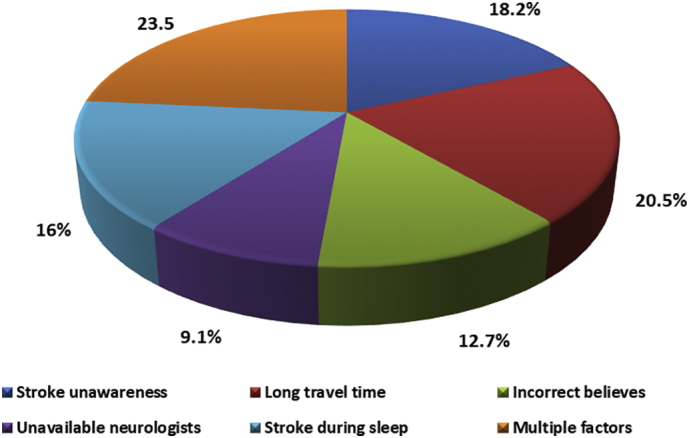
Main causes of pre-hospital onset arrival delay.
The study had also showed that, causes of non-administration of IV r-tPA in group-Ib patients despite their arrival within <3.5 h from stroke onset were as follows; 84/204 (41.2%) had prolonged DNT > 60 min, 53/204 (26%) had patients' financial restraints, 26/204 (12.7%) had minor motor (NIHSS ≤ 5) or non-motor stroke, 23/204 (11.3%) did not find available stroke ready beds and 18/204 (8.8%) had feared of hemorrhagic transformation (Fig. 2).
Fig. 2.
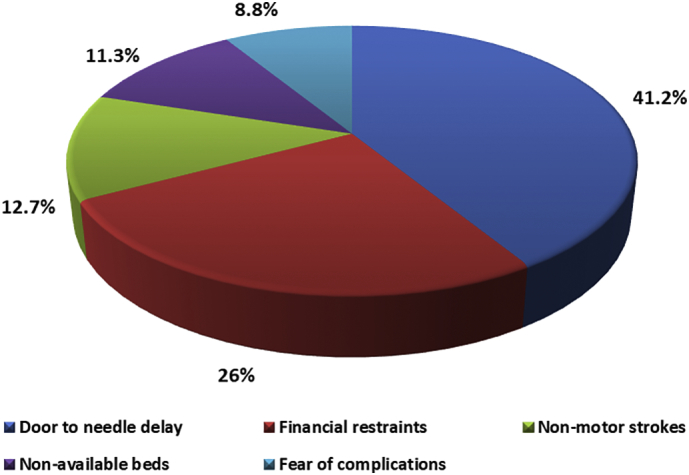
Causes of IV r-tPA non-administration despite arrival within the therapeutic window.
4. Discussion
Great advancements had occurred in AIS management in Egypt during the last years, but the usage of IV thrombolysis (<1%) is still very far away from the proposed rate [2]. The drug is one of the few evidence-based managements of AIS with the earlier initiation of therapy, the better the clinical response and the lower degree of disabilities [10].
The study revealed that AIS patients who received IV r-tPA constituted only 5.8% of those were eligible for receiving IV thrombolysis. This result is very close to that of Cheng and colleagues [11] who estimated the proportion of patients received IV thrombolysis to be 5.3% of their studied stroke patients and explained this lower percentage to delays in activating the EMS services and the suboptimal hospital infrastructure.
The results of the present study showed that better recognition of stroke warning signs and awareness of the limits of the narrow therapeutic window represent the most important cause of OAT lessening, which resulted in rapid contact with the EMS services and prompt hospital transfer. At the same time, many studied patients or their relatives were not aware about the extent of the therapeutic window despite their recognition of early stroke symptoms. These results are in accordance with that of Dombrowski and colleagues [12] as well as Nishijima and colleagues [13] who identified that stroke symptoms recognition, previous experience of dealing with stroke patients and follow-up public as well as TV educational programs are associated with pre-hospital time reduction.
The study had also declared that, wrong beliefs and bad medical performances like the concept that big dose of aspirin may dissolve the thrombus were one of the causes of wasting the golden hours of the therapeutic window. These results are passing with that of Farrag and colleagues [14] as well as Ruiz and colleagues [15] who stated that delayed calling of the EMS services as well as poorly organized ambulance services were important causes of pre-hospital delay of AIS patients.
The study determined that pre-hospital delay is more common among rural patients and those lived far away from the hospital due to delayed recognition of stroke symptoms, narrow villages' alleys handicapping the arrival of EMS services, lack of nearby ambulances and absence of thrombolysis in nearby hospitals. These results are parallel with that of Abu-Hegazy and colleagues [16] who stated that AIS patients from rural areas showed significant prolongation of OAT due to long distances and weak transport network with severe difficulties in transporting AIS cases especially those with nocturnal onset symptoms. On the other hand, Hansen and colleagues [17] determined non-significant differences in alarm-to-door time between Canadian rural and urban areas due to efficient EMS system and application of the bypass as well as drip and ship protocols.
The results of this study also revealed that, economic constraints may be a serious obstacle that decreased the usage of IV r-tPA which is noticed in the sector of patients who could not utilize IV r-tPA despite their arrival within the permissible therapeutic window due to financial problems. This result is in accordance with that of Ghandehari [18] who determined that financial limitation and lack governmental as well as health insurance support are very important factors that limit the use of IV thrombolysis in developing countries.
The study showed that, minor motor as well as non-motor strokes like hemiataxia, hemi-hypoesthesia or visual field defects may mislead the on-duty doctor to withhold IV r-tPA in indicated cases. Powers and colleagues [8] had rectified this problem while proposing the AHA/ASA, 2018 for early AIS management as they cautioned against non-administration of IV thrombolysis in patients with mild or non-motor disabilities who will greatly benefit from its use.
The study had also determined that, the non-available beds within NVUs were one of the barriers that limited the use of IV r-tPA in some eligible cases. This result is passing with the work of Paul and colleagues [19] who recommended that improved rate of r-tPA use needs financial incentives, quality-improvement approaches, increases the hospital infrastructures including the hospital size as well as the number of beds, accessibility of on-duty qualified staff on a 24-h basis and tele-stroke services for hospital pre-notification systems.
Intra-hospital delay is also an important cause of narrow therapeutic window consumption. The study showed that multiple referrals, doing steps in consecutive rather than simultaneous manners and complex administrative procedures are very important causes of prolonged DNT. These results are in harmony with the results of Fernandes and Umasankar [20] who stated that weak hospitals organization, delayed doctors' arrival, CT delay, tied up stroke nurse with another patient and delayed decisions are the main causes of intra-hospital DNT prolongation.
4.1. Recommendations
Increasing IV r-tPA utilization for AIS patients' needs the following proposals:
-
1.
Increasing social awareness about the early stroke recognition and the value of early arrival in stroke-ready hospitals before the expiry of the therapeutic window.
-
2.
Repeated training of the EMS personnel about their vital role in saving the OAT, how to identify stroke warning signs, assess their severities, bypass stroke non-ready hospitals to the nearest ready one and how to utilize tele-stroke pre-arrival hospital notification.
-
3.
Arrangement with the Directorate of Health Affairs in Gharbia Governorate to set up the general hospitals under their management to be certified as acute primary stroke-ready hospitals which could immediately administer IV r-tPA and then transfer patients to NVUs of TUHs with better stroke treatment facilities (drip and ship strategy).
-
4.
More financial support is needed from the government, third-party agencies and the civil society institutions for free accessibility of the r-tPA vials and to improve the hospital infrastructures to avoid the possibility of unavailable beds or busy unattainable staff.
-
5.
During future reconstruction of the hospital, the NER, imaging and laboratory investigations as well as the administrative procedures must be offered in the same building location.
5. Conclusion
While building or adjusting the SCS system, do not look for the unreachable solutions, but always adjust the system regarding the available resources. The administrative procedures, laboratory investigations and imaging steps could be done in simultaneous rather than consecutive steps.
6. Limitations
Acute ischemic stroke patients delivered to some private hospitals in the studied area were missed in the present study but their number was statistically negligible compared to those arrived to TUHs.
References
- 1.Feigin V.L., Norrving B., Mensah G.A. Global burden of stroke. Circ. Res. 2017;120:439–448. doi: 10.1161/CIRCRESAHA.116.308413. [DOI] [PubMed] [Google Scholar]
- 2.Zakaria M.F., Aref H., Abd ElNasser A. Egyptian experience in increasing utilization of reperfusion therapies in acute ischemic stroke. Int. J. Stroke. 2018 Jul;13(5):525–529. doi: 10.1177/1747493017711949. [DOI] [PubMed] [Google Scholar]
- 3.Badachi S., Mathew T., Prabhu A. Hurdles in stroke thrombolysis: experience from 100 consecutive ischemic stroke patients. Ann. Indian Acad. Neurol. 2015;18(4):415–418. doi: 10.4103/0972-2327.165460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valenzuela Espinoza A.V., Van Hooff R.J., De Smedt A. Development and pilot testing of 24/7 in-ambulance telemedicine for acute stroke: prehospital stroke study at the Universitair Ziekenhuis Brussel-Project. Cerebrovasc Dis. 2016;42(1–2):15–22. doi: 10.1159/000444175. [DOI] [PubMed] [Google Scholar]
- 5.Fonarow G.C., Smith E.E., Saver J.L. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–758. doi: 10.1161/CIRCULATIONAHA.110.974675. [DOI] [PubMed] [Google Scholar]
- 6.Caplan L.R. Primary stroke centers vs comprehensive stroke centers with interventional capabilities: which is better for a patient with suspected stroke? JAMA Neurol. 2017;74(5):504–506. doi: 10.1001/jamaneurol.2017.0006. [DOI] [PubMed] [Google Scholar]
- 7.Kassebaum N.J., Arora M., Barber R.M. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–1658. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Powers W.J., Rabinstein A.A., Ackerson T. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49 (eXXX–eXXX) [Google Scholar]
- 9.Meschia J.F., Brott T. Ischaemic stroke. Eur. J. Neurol. 2018;25:35–40. doi: 10.1111/ene.13409. [DOI] [PubMed] [Google Scholar]
- 10.Puolakka T., Strbian D., Harve H. Prehospital phase of the stroke chain of survival: a prospective observational study. J. Am. Heart. Assoc. 2016;5 doi: 10.1161/JAHA.115.002808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng N.T., Kim A.S. Intravenous Thrombolysis for acute ischemic stroke within 3 hours versus between 3 and 4.5 hours of symptom onset. Neurohospitalist. 2015;5(3):101–109. doi: 10.1177/1941874415583116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dombrowski S.U., Ford G.A., Morgenstern L.B. Differences between US and UK adults in stroke preparedness: evidence from parallel population-based community surveys. Stroke. 2015;46:3220–3225. doi: 10.1161/STROKEAHA.115.009997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishijima H., Ueno T., Tomiyama M. Effects of educational television commercial on pre-hospital delay in patients with ischemic stroke wore off after the end of the campaign. J. Neurol. Sci. 2017:381117–381118. doi: 10.1016/j.jns.2017.08.3236. [DOI] [PubMed] [Google Scholar]
- 14.Farrag M.A., Oraby M.I., Ghali A.A. Public stroke knowledge, awareness, and response to acute stroke: multi-center study from 4 Egyptian governorates. J. Neurol. Sci. 2018;384:46–49. doi: 10.1016/j.jns.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Ruiz R.G., Fernández J.S., Ruiz R.M.G. Response to symptoms and prehospital delay in stroke patients. Is it time to reconsider stroke awareness campaigns? J. Stroke Cerebrovasc. Dis. 2018;27(3):625–632. doi: 10.1016/j.jstrokecerebrovasdis.2017.09.036. [DOI] [PubMed] [Google Scholar]
- 16.Abu-Hegazy M., Elmenshawi I., Saad M. Barriers for acute ischemic stroke treatment using recombinant tissue plasminogen activator in Mansoura Emergency Hospital: prehospital and in hospital delay factors. Egypt. J. Neurol. Psychiatry Neurosurg. 2016;53:263–267. [Google Scholar]
- 17.Hansen G., Bal S., Schellenberg K.L. Prehospital management of acute stroke in rural versus urban responders. J. Neurosci. Rural Pract. 2017;8(1):S33–S36. doi: 10.4103/jnrp.jnrp_2_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghandehari K. Barriers of thrombolysis therapy in developing countries. Stroke Res. Treat. 2011;2011 doi: 10.4061/2011/686797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paul C.L., Ryan A., Rose S. How can we improve stroke thrombolysis rates? A review of health system factors and approaches associated with thrombolysis administration rates in acute stroke care. Implement. Sci. 2016;11 doi: 10.1186/s13012-016-0414-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernandes D., Umasankar U. Improving door to needle time in patients for thrombolysis. BMJ Qual. Improv. Rep. 2016;5 doi: 10.1136/bmjquality.u212969.w5150. [DOI] [PMC free article] [PubMed] [Google Scholar]


