Abstract
Background
Three-dimensional (3D) navigation techniques can theoretically provide higher accuracy rates and increased safety for pedicle screw (PS) placement than traditional fluoroscopy (FL) guided methods. In this study, we compare the pedicular accuracy of 3D isocentric fluoroscopic navigation (3DFL) versus FL guidance in PS L4-L5-S1 fixation and evaluate the differential cortical purchase and safety of fixation of the S1 PS.
Methods
This is a single-centre retrospective study of 810 PSs placed in open L4-L5-S1 fixation between 2012 and 2017 in 39 patients using standard FL and in 96 patients under 3DFL. Pedicular screw accuracy was determined by postoperative computed tomography (CT) and graded on a 4-tiered classification system according to Gertzbein and Robbins. In addition, sacral screws were evaluated depending on the degree of cortical fixation: monocortical, bicortical or tricortical, and the degree of safety with respect to retroperitoneal structures.
Results
Grade 0 perfect pedicular screw placement was 95% for 3DFL screws compared to 85% for screws placed under fluoroscopy (P<0.05). The number of grade 0 versus grade 1 and higher (breached screws) was statistically significant (P<0.05). Higher S1 cortical screw accuracy [77% versus 51% (P<0.05)] for bi- and tricortical fixation and a lower percentage of “at risk” PSs (P<0.05) were achieved with placement under 3DFL versus FL.
Conclusions
3DFL enhances the accuracy and safety of PS placement in L4-L5-S1 fixation, reducing the rate of misplaced screws and improving S1 cortical fixation.
Keywords: Navigated spine surgery, three-dimensional fluoroscopy, pedicle screw accuracy, sacrum cortical fixation, lumbosacral spine
Introduction
Transpedicular screw L4-L5-S1 fixation is an established, common procedure performed by spine surgeons that requires correct placement of pedicle screws (PSs) to provide biomechanical stability and to avoid injuries in neighbouring neurovascular structures. Even in expert hands, and although these pedicles are the widest of the entire vertebral column, the widespread practice of PS implantation based on surface anatomy combined with conventional fluoroscopy (FL) is associated with high rates of malposition, ranging from 10% to 40% in different series, resulting in a risk of iatrogenic injury and the need for surgical revision (1-3).
From a biomechanical perspective, both the position of the screw relative to the lumbar pedicle and the fixation mode (monocortical, bicortical or tricortical) in S1 fixation affect the stability of segmental fixation and the success of spinal fusion (4-6). The progressive development of image-guided spinal surgery, which involves real-time integration of the three-dimensional (3D) anatomy with instrumental techniques, has enabled improved precision in the placement of PSs while reducing radiation exposure of the surgical team (7-12).
The authors carried out a retrospective study to analyse the accuracy and safety of PS implantation in L4-L5-S1 fixation using fluoroscopy (FL) versus 3D isocentric fluoroscopic navigation (3DFL). To determine the associated biomechanical implications, the placement outcomes with different modes of cortical fixation of PSs in S1 (monocortical, bicortical or tricortical) were evaluated.
Methods
A retrospective study was carried out with a consecutive series of 135 patients who underwent open L4-L5-S1 fixation with PS implantation between 2012 and 2017. The patients were divided into two groups based on the imaging protocol used for transpedicular instrumentation. FL was used until October 2013, date in which a 3D isocentric fluoroscopy navigation system was incorporated that was used systematically in all cases. Group FL included 39 patients (9 males and 30 females, average age of 60.6 years) in whom fluoroscopy was used for screw implantation. Group 3DFL consisted of 96 patients (27 males and 69 females, average age 58.7 years) who underwent navigated insertion of Stryker Xia screws.
Pedicular screw insertion was always performed at the initial phase of the surgery, before an eventual laminectomy in case of stenosis. Laminectomy may increase the intervertebral mobility and thus hinder the transpedicular instrumentation, and in case of navigation it may alter the stability of the reference clamp.
Surgical technique under FL
Under biplanar fluoroscopy, pedicles were cannulated according to the Roy-Camille technique. The trajectory of a palpation probe was verified by the “owl’s eye technique”: after insertion of a metal marker, fluoroscopic exploration was performed with the fluoroscopy beam projected coaxially on the pedicle. A final assessment of the screw was carried out under fluoroscopy in the lateral view.
Surgical technique under 3DFL
Once the patient was placed in the prone position on a carbon fibre table, the procedure was initiated, and the vertebral spaces projected for instrumentation were located by fluoroscopy. The reference clamp for navigation was fixed in the spinous process of the L3 vertebra. Then, with the patient in an apnoeic state for 1 minute and the surgical team outside the operating room, a 3D isocentric fluoroscan was performed by motorized elliptical movement of the fluoroscope with a maximum rotational arc of 135° around the patient (Ziehm Vision FD Vario 3D Imaging, Nuremberg, Germany). We obtained 120 successive 2D fluoroscopic images of the lumbar region to be instrumented, which allowed reconstruction in the coronal, axial and sagittal planes in the fluoroscopy equipment itself, and the reconstructed images were automatically transferred to the navigation platform (System II SpineMap 3D, Stryker, Freiburg, Germany) for multiplanar reconstruction of the vertebral anatomy.
Subsequently, the locations of the navigation instruments were recorded, and the instruments were calibrated with an error margin of less than 0.5 mm.
PSs were implanted under the guidance of the navigation system and then a second 3D fluoroscan was performed to examine the final position of the screws intraoperatively. If the position of a screw was judged to be inadequate, then the screw was replaced and repositioned, followed by another fluoroscan.
Regardless of the imaging system used, the authors attempted to fix the PSs in S1 at the bicortical or tricortical level, which is biomechanically superior to monocortical fixation (4,5).
Assessment of the position of the screws
All patients were examined postoperatively by computed tomography (CT) scans (GE VCT64 with sub-millimeter resolution) and the spatial arrangement of the PSs was analysed by the surgeons using the Dicom viewer Ossirix.
The position of each screw was evaluated both at the pedicular level and in relation to the vertebral body.
For the screw position at the pedicular level, the Gertzbein and Robbins (13) scale was followed, which includes four grades according to the existence of rupture of the pedicle wall and the extent of extracortical displacement in increments of 2 mm:
❖ Grade 0: the screw is completely contained in the pedicle; “perfect position”;
❖ Grade 1: perforation-rupture of the pedicle wall with displacement less than 2 mm; “clinically acceptable position” or safe-zone screws;
❖ Grade 2: moderate displacement between 2 and 4 mm; potentially hazardous;
❖ Grade 3: severe displacement greater than 4 mm; absolutely hazardous.
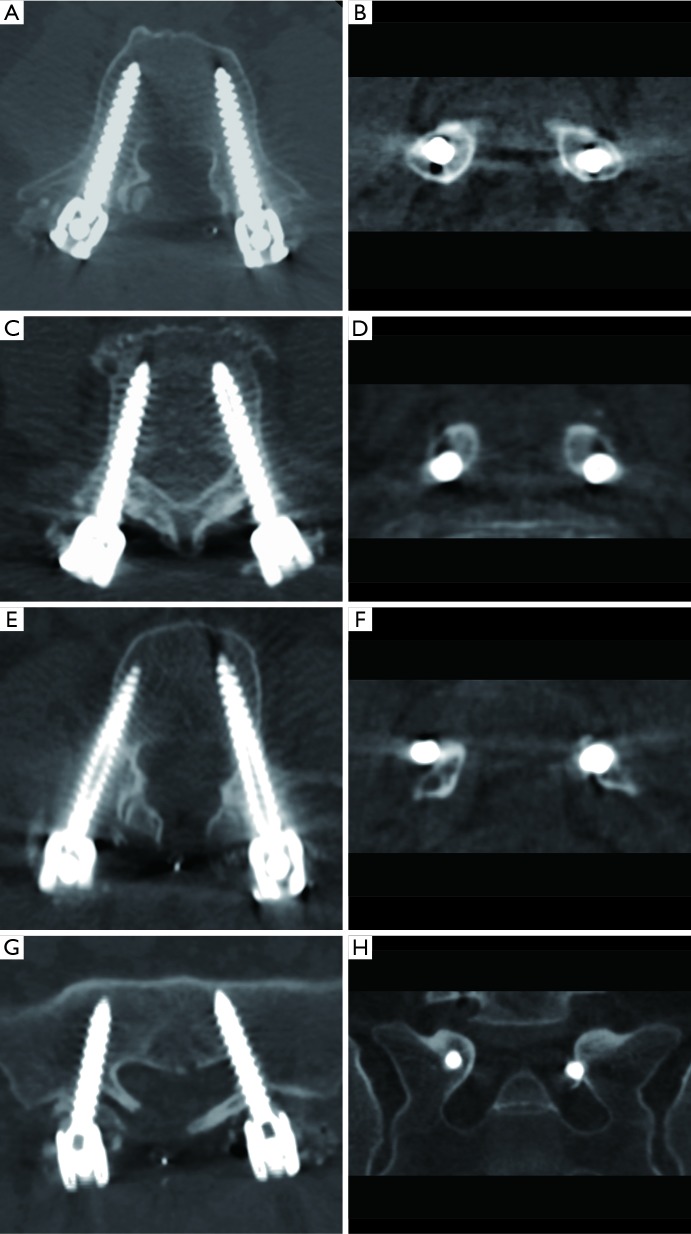
Grade 0 is considered “perfect”, and grades 0 + 1 are considered “clinically acceptable”. Screws with grades 2 and 3 are regarded as a “potential clinical risk” due to the possibility of neurovascular lesions; their deviation was evaluated as medial-inferior or lateral-superior (Figure 1).
Figure 1.
Representative CT images in the axial and coronal planes of grade 0 (A,B), grade 1 (C,D), grade 2 medial and grade 3 lateral (E,F) and grade 3 medial (G,H) pedicle screw placements. CT, computed tomography.
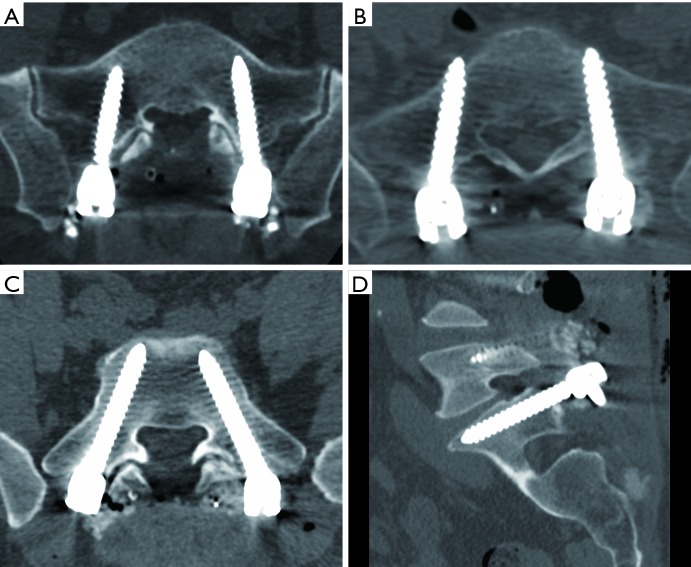
For the screw position in relation to the vertebral body, the existence of anterior cortical perforation, extracortical displacement and the risk of injury to neurovascular structures was assessed. For PSs in S1, the category of fixation was evaluated as monocortical (purchase with posterior cortex penetration alone), bicortical (tapping of the anterior sacral cortex or cranial S1 endplate) and tricortical (penetration of the apex of the sacral promontory) (Figure 2). According to Sarwahi et al. (14), the category of “at risk” was established for cases of anterior protrusion greater than 4 mm (Figure 3).
Figure 2.
Representative images of different cortical fixations of an S1 pedicular screw: monocortical (A), bicortical (B) and tricortical (C,D) purchase.
Figure 3.
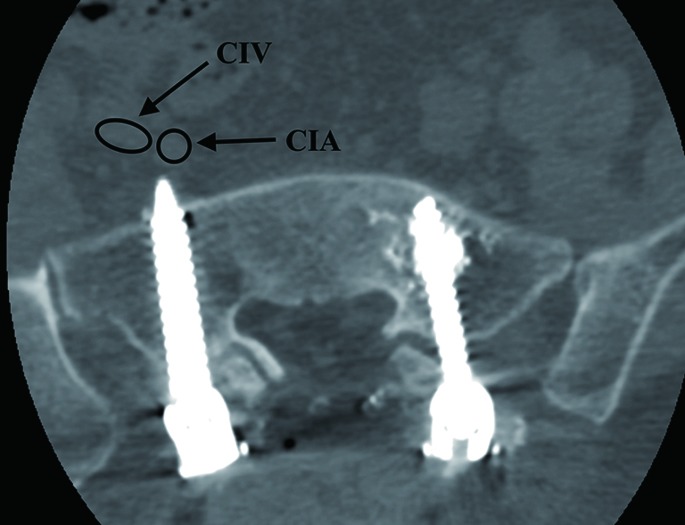
S1 pedicular screw “at risk”: protrusion >4 mm close to the common iliac artery (CIA) and vein (CIV).
Statistical analysis
The positions of the screws and the associated risk were compared using the chi-square test and Fisher’s exact test (two-tailed). Relative risks (RRs), odds ratios (ORs) with 95% confidence intervals, and the number needed to harm (NNH) were calculated.
The analysis was carried out using the software EPIDAT 3.1 (General Directorate of Public Health, 2006), and P values <0.05 were considered significant.
Results
The general characteristics of each group, including demography, body mass index (BMI), preoperative diagnosis and surgical technique, were similar, except for a higher number of revision cases in the 3DFL group (Table 1). A total of 810 screws were implanted, including 234 under FL and 576 under 3DFL.
Table 1. Patient characteristics.
| Variable | Fluoroscopic surgery | 3DFL navigated surgery |
|---|---|---|
| Mean age (years) | 60.6 | 58.7 |
| Females/males | 30/9 | 74/22 |
| Preoperative diagnosis, n | ||
| Degenerative disc disease | 14 | 33 |
| Listhesis | 7 | 13 |
| Stenosis | 16 | 46 |
| Other | 2 | 4 |
| Revision surgery | 6 (15%) | 23 (24%) |
3DFL, three-dimensional isocentric fluoroscopic navigation.
Assessment of the pedicle position of the screws (Table 2)
Table 2. Pedicular screw evaluation.
| Technique | Total screws | Correctly placed | Minor perforation <2 mm | Displaced with potential clinical risk | |||
|---|---|---|---|---|---|---|---|
| 2 to <4 mm (lat–sup) | 2 to ≤4 mm (med–inf) | ≥4 m (lat–sup) | ≥4 m (med–inf) | ||||
| Fluoroscopy | 234 | 200 | 26 | 2 | 3 | 1 | 2 |
| Navigation | 576 | 548 | 24 | 4 | 0 | 0 | 0 |
lat, lateral; sup, superior; med, medial; inf, inferior.
A “perfect” position of the screws (grade 0) was achieved in 85% (200 PSs) of the cases in the FL group compared to 95% (548 PSs) of the cases in the 3DFL group (P=0.001). A “clinically acceptable” position (grades 0 and 1) had an accuracy of 96.6% (226 PSs) in the FL group compared to 99.3% (572 PSs) in the 3DFL group (P=0.004).
In the FL group, a total of 8 deviated L4-L5 PSs (3.4%) presented extrapedicular displacement greater than 2 mm, with moderate displacement (grade 2) of 5 screws, including 3 medially and 2 laterally deviated screws, and severe displacement (grade 3) of 3 screws, including 1 laterally and 2 medially deviated screws. In the immediate postoperative period, no complications arising from the incorrect positions of the screws were noted; however, the 2 PSs with medial displacement greater than 4 mm were revised.
In the 3DFL group, postoperative CT showed 4 deviated L4-L5 PSs (grade 2) with lateral displacement <4 mm and no screws with severe displacement. In this group, 3D intraoperative fluoroscopic imaging showed incorrect positioning of 6 PSs (2.4%), which were repositioned intraoperatively. Postoperative CT confirmed that the original trajectory deviated in the external direction as well as the correct final position of the implant.
The RR of a displaced PS in the FL group was 4.9 times higher, with a NNH of 38 procedures and an OR of 5.03.
Assessment of the position of L4-L5 PSs in relation to the vertebral body
Anterior/lateral protrusion was observed in 4 (2.6%) of the PSs with fluoroscopy and in 5 (1.3%) of the PSs with navigation, which was less than 3 mm in all cases. Postoperative CT scans did not indicate a risk to vascular structures.
Assessment of the cortical fixation of PSs in S1 (Table 3)
Table 3. S1 fixation of pedicular screws.
| Technique | Total screws | Monocortical | Bicortical | Tricortical | At risk |
|---|---|---|---|---|---|
| Fluoroscopy | 78 | 38 | 24 | 16 | 4 |
| Navigation | 192 | 44 | 65 | 83 | 0 |
In the FL group, PS fixation in S1 was monocortical in 38 cases (49%), bicortical in 24 cases (31%) and tricortical in 16 cases (21%) compared with 44 cases (23%), 65 cases (34%) and 83 cases (43%) in the 3DFL group, respectively. Evaluation of anterior protrusion of the bi-tricortical screws revealed 4 “at risk” PSs in the FL group, with anterior protrusion greater than 4 mm and close to the iliac vessels. In the 3DFL group, 9 PSs were revised intraoperatively when unacceptable anterior protrusion was observed on the intraoperative 3D fluoroscan. The differences between both implantation strategies were significant, with a higher percentage of bi-tricortical fixation (P=0.001) and a lower risk (P=0.007) in the 3DFL group and a NNH of 20 procedures.
Discussion
The findings show that implantation of PSs at the L4-L5-S1 level using 3DFL results in significantly greater accuracy and involves less risk than FL, with a perfect position achieved in 95% of the cases and clinically acceptable positioning (displacement <2 mm) with 99.3% accuracy in the 3DFL group compared to 85% and 96% in the FL group, respectively.
Several clinical (11,12,15-17) and experimental (8,18) studies have shown that the positioning accuracy of PSs is significantly better with a navigation system than with FL. In 2013, Waschke et al. (11) retrospectively analysed the data of 1,006 patients: in the lumbar spine, the placement accuracy was 96.4% for 2,422 CT-navigated screws and 93.9% for 2,002 PSs placed under fluoroscopy (P=0.001).
The systematic review by Aoude et al. (19), which included 68 relevant articles with a total of 3,442 patients, 60 cadavers and 43,305 PSs, reports an average accuracy of 91.4% for PSs placed within the safe zone (<2 mm breach) with the free-hand or fluoroscopy technique compared to an average accuracy of 97.3% for PSs placed using navigation (P<0.001).
The greater precision of the navigation technique is related to the important advantage of intraoperative 3D imaging, which allows the surgeon to confirm correct screw placement prior to leaving the operating room and thus reposition or remove screws as necessary. Ryang et al. (20) reported an intraoperative revision rate of 4.9% (36 of 736 PSs) using 3DFL, while Fichtner et al. (7) reported a rate of 3% (230 of 7,548 PSs). In the 3DFL group, 15 PSs (2.6%), including 6 lumbar and 9 sacral screws, were reviewed intraoperatively, and none of the patients required reoperation.
The malpositioning of a PS may not only affect the stability of fixation but also result in clinical repercussions or even necessitate surgical revision (3,7,15,17,21-23).
A literature review indicates that the incidence of complications and the rate of surgical revision are greater with traditional FL than with the various navigation systems. A meta-analysis of 23 spinal instrumentation studies found no neurological complications in the 719 patients that underwent screw placement with navigation, compared with 13 instances of neurological complications (2.3%) in the 569 patients treated without navigation (24). In another meta-analysis of 39 studies (3,062 patients) regarding clinical issues related to PS misplacement in non-navigated procedures, 32 patients in ten studies required further revision surgeries for misplaced PSs, causing neurological problems in 1.04% of the patients (32/3,062) (1).
Fichtner et al. (7) recent retrospective study reports a rate of 1.35% for secondary revision (15/1,112 patients) of screws placed by IsoC-3D navigated fluoroscopy versus 4.38% (49/1,120 patients) with FL, which was indicated for mispositioned screws without neurological complications in 50% of both groups.
Similar to our 0% revision surgery rate in the 3DFL group, 0% rates were also reported by Nakashima et al. (9), who placed 150 percutaneous posterior lumbar PSs, and also using O-arm based navigation by Shin et al. (10) for insertion of 106 PSs.
Regarding sacral fixation, the type of cortical purchase of the PS to use is important to consider. Several in vitro and clinical studies have concluded that both bicortical and tricortical purchases are biomechanically superior to monocortical fixation of the screw (4-6).
To the best of our knowledge, this is the first study in the literature comparing different cortical purchases of S1 PSs (Table 3) between fluoroscopy and the 3D navigation technique.
Our data show that better bi-tricortical positioning of PSs is achieved using fluoroscopic navigation versus FL, which may favour a greater degree of bone consolidation in L4-L5-S1 fixation, although this factor was not assessed in our study. Orita et al. (6) reports a lower risk of loosening of S1 PSs with tricortical fixation versus monocortical fixation, while Kato et al. (25) reports better bone consolidation with tricortical fixation (100% fusion in 98 patients) than with monocortical fixation (10% pseudoarthrosis in 33 patients).
Given the anatomy of the sacrum, this structure is somewhat difficult to assess with FL, including the position of the end of the screw in relation to the anterior sacral cortex (26). However, the literature is controversial, with several studies indicating a “safety margin” with anterior protrusion less than 4 mm in sacral PS placement permitting anterior cortical purchase, while some reports have strongly recommended avoiding anterior cortex penetration because of the risk of neurovascular injury (6,14,27,28). Balling and Blattert (21) mentions the difficulty of achieving correct bicortical fixation in his series of 258 S1 PSs, reporting a total error rate of 5.8%, 3.9% of which was due to excess length, although no clinical lesions were noted.
Fluoroscopic navigation allowed the surgeon to intraoperatively review nine sacral PSs that were found to be excessively long. FL revealed three at-risk PSs with anterior displacement greater than 4 mm on postoperative CT but without clinical repercussions.
The limitations of this study include the retrospective design and the fact that the postoperative scans to evaluate the positions of the PSs were assessed by the surgeons themselves. Although both authors have extensive spinal surgical experience, they cannot exclude the possible influence of the inherent learning curves for FL and the new navigation techniques, which were implemented in consecutive periods.
Conclusions
Placement of L4-L5-S1 pedicular screws under 3DFL was found to be significantly more accurate than placement under FL. This technique may lead not only to less complications and revision surgeries but also to biomechanically superior fixation, especially for bi-tricortical fixation of the S1 vertebra.
Acknowledgements
The authors thank Sonia Pertega of the Clinical Epidemiologic Unit of the University Hospital of A Coruna for her assistance in the statistical analysis.
Ethical Statement: This research article was done with the approval of the local Ethics committees, and written informed consent was obtained from all patients included in the study.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Gautschi OP, Schatlo B, Schaller K, et al. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus 2011;31:E8. 10.3171/2011.7.FOCUS11168 [DOI] [PubMed] [Google Scholar]
- 2.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine 2007;32:E111-20. 10.1097/01.brs.0000254048.79024.8b [DOI] [PubMed] [Google Scholar]
- 3.Saarenpää I, Laine T, Hirvonen J, et al. Accuracy of 837 pedicle screw positions in degenerative lumbar spine with conventional open surgery evaluated by computed tomography. Acta Neurochir 2017;159:2011-7. 10.1007/s00701-017-3289-7 [DOI] [PubMed] [Google Scholar]
- 4.Luk KD, Chen L, Lu WW. A stronger bicortical sacral pedicle screw fixation through the S1 endplate: an in vitro cyclic loading and pull-out force evaluation. Spine 2005;30:525-9. 10.1097/01.brs.0000154649.55589.bf [DOI] [PubMed] [Google Scholar]
- 5.Lehman RA, Kuklo TR, Belmont PJ, et al. Advantage of pedicle screw fixation directed into the apex of the sacral promontory over bicortical fixation: a biomechanical analysis. Spine 2002;27:806-11. 10.1097/00007632-200204150-00006 [DOI] [PubMed] [Google Scholar]
- 6.Orita S, Ohtori S, Eguchi Y, et al. Radiographic evaluation of monocortical versus tricortical purchase approaches in lumbosacral fixation with sacral pedicle screws: a prospective study of ninety consecutive patients. Spine 2010;35:E1230-7. 10.1097/BRS.0b013e3181e5092c [DOI] [PubMed] [Google Scholar]
- 7.Fichtner J, Hofmann N, Rienmüller A, et al. Revision rate of misplaced pedicle screws of the thoracolumbar spine-comparison of three-dimensional fluoroscopy navigation with freehand placement: a systematic analysis and review of the literature. World Neurosurg 2018;109:e24-32. 10.1016/j.wneu.2017.09.091 [DOI] [PubMed] [Google Scholar]
- 8.Mason A, Paulsen R, Babuska JM, et al. (2014) The accuracy of pedicle screw placement using intraoperative image guidance systems. J Neurosurg Spine 2014;20:196-203. 10.3171/2013.11.SPINE13413 [DOI] [PubMed] [Google Scholar]
- 9.Nakashima H, Sato K, Ando T, et al. Comparison of the percutaneous screw placement precision of isocentric C-arm 3-dimensional fluoroscopy-navigated pedicle screw implantation and conventional fluoroscopy method with minimally invasive surgery. J Spinal Disord Tech 2009;22:468-72. 10.1097/BSD.0b013e31819877c8 [DOI] [PubMed] [Google Scholar]
- 10.Shin MH, Ryu KS, Park CK. Accuracy and safety in pedicle screw placement in the thoracic and lumbar spines: comparison study between conventional C-arm fluoroscopy and navigation coupled with O-Arm® guided methods. J Korean Neurosurg Soc 2012;52:204-9. 10.3340/jkns.2012.52.3.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waschke A, Walter J, Duenisch P, et al. CT-navigation versus fluoroscopy-guided placement of pedicle screws at the thoracolumbar spine: single center experience of 4,500 screws. Eur Spine J 2013;22:654-60. 10.1007/s00586-012-2509-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu T, Mi S, He Y, et al. Accuracy of pedicle screw placement in posterior lumbosacral instrumentation by computer tomography evaluation: a multi-centric retrospective clinical study. Int J Surg 2017;43:46-51. 10.1016/j.ijsu.2017.05.041 [DOI] [PubMed] [Google Scholar]
- 13.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine 1990;15:11-14. 10.1097/00007632-199001000-00004 [DOI] [PubMed] [Google Scholar]
- 14.Sarwahi V, Payares M, Wendolowski S, et al. Pedicle screw safety: how much anterior breach is safe?: a cadaveric and CT-based study. Spine 2017;42:E1305-10. 10.1097/BRS.0000000000002153 [DOI] [PubMed] [Google Scholar]
- 15.Gelalis ID, Paschos NK, Pakos EE, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 2012;21:247-55. 10.1007/s00586-011-2011-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luther N, Iorgulescu JB, Geannette C, et al. Comparison of navigated versus non-navigated pedicle screw placement in 260 patients and 1434 screws: screw accuracy, screw size, and the complexity of surgery. J Spinal Disord Tech 2015;28:E298-303. 10.1097/BSD.0b013e31828af33e [DOI] [PubMed] [Google Scholar]
- 17.Noriega DC, Hernandez-Ramajo R, Rodriguez-Monsalve Milano F, et al. Risk-benefit analysis of navigation techniques for vertebral transpedicular instrumentation: a prospective study. Spine J 2017;17:70-5. 10.1016/j.spinee.2016.08.004 [DOI] [PubMed] [Google Scholar]
- 18.Tian W, Lang Z. Placement of pedicle screws using three-dimensional fluoroscopy-based navigation in lumbar vertebrae with axial rotation. Eur Spine J 2010;19:1928-35. 10.1007/s00586-010-1564-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aoude AA, Fortin M, Figueiredo R, et al. Methods to determine pedicle screw placement accuracy in spine surgery: a systematic review. Eur Spine J 2015;24:990-1004. 10.1007/s00586-015-3853-x [DOI] [PubMed] [Google Scholar]
- 20.Ryang YM, Villard J, Obermuller T, et al. Learning curve of 3D fluoroscopy image-guided pedicle screw placement in the thoracolumbar spine. Spine J 2015;15:467-76. 10.1016/j.spinee.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 21.Balling H, Blattert TR. Rate and mode of screw misplacements after 3D-fluoroscopy navigation-assisted insertion and 3D-imaging control of 1547 pedicle screws in spinal levels T10-S1 related to vertebrae and spinal sections. Eur Spine J 2017;26:2898-905. 10.1007/s00586-017-5108-5 [DOI] [PubMed] [Google Scholar]
- 22.Costa F, Villa T, Anasetti F, et al. Primary stability of pedicle screws depends on the screw positioning and alignment. Spine J 2013;13:1934-9. 10.1016/j.spinee.2013.03.046 [DOI] [PubMed] [Google Scholar]
- 23.Stauff MP, Freedman BA, Kim JH, et al. The effect of pedicle screw redirection after lateral wall breach--a biomechanical study using human lumbar vertebrae. Spine J 2014;14:98-103. 10.1016/j.spinee.2013.03.028 [DOI] [PubMed] [Google Scholar]
- 24.Verma R, Krishan S, Haendlmayer K, et al. Functional outcome of computer-assisted spinal pedicle screw placement: a systematic review and meta-analysis of 23 studies including 5,992 pedicle screws. Eur Spine J 2010;19:370-5. 10.1007/s00586-009-1258-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kato M, Taneichi H, Suda K. Advantage of pedicle screw placement into the sacral promontory (Tricortical Purchase) on lumbosacral fixation. J Spinal Disord Tech 2015;28:E336-42. 10.1097/BSD.0b013e31828ffc70 [DOI] [PubMed] [Google Scholar]
- 26.Jain N, Yu E. Intraoperative radiographic technique for visualization of bicortical or tricortical anteromedial sacral screw placement. Clin Spine Surg 2018;31:108-11. 10.1097/BSD.0000000000000561 [DOI] [PubMed] [Google Scholar]
- 27.Akhgar J, Terai H, Rahmani MS, et al. Anatomical location of the common iliac veins at the level of the sacrum: relationship between perforation risk and the trajectory angle of the screw. Biomed Res Int 2016;2016:1457219. 10.1155/2016/1457219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ergur I, Akcali O, Kiray A, et al. Neurovascular risks of sacral screws with bicortical purchase: an anatomical study. Eur Spine J 2007;16:1519-23. 10.1007/s00586-007-0326-x [DOI] [PMC free article] [PubMed] [Google Scholar]