Abstract
Background:
Hospital admission, like hospital discharge, represents a transition-of-care associated with changes in setting, healthcare providers and clinical management. While considerable efforts have focused on improving the quality and safety of hospital-to-home transitions, there has been little focus on transitions into hospital.
Objectives:
Among children hospitalized with ambulatory care sensitive conditions, we aimed to characterize families’ experiences as they transitioned from outpatient to inpatient care, identify hospital admission processes and outcomes most important to families, and determine how parental perspectives differed between children admitted directly and through emergency departments.
Methods:
We conducted semi-structured interviews with parents of hospitalized children at 4 structurally diverse hospitals. We inquired about pre-admission healthcare encounters, how hospital admission decisions were made, and parents’ preferences regarding hospital admission processes and outcomes. Interviews were transcribed verbatim and analyzed using a general inductive approach.
Results:
We conducted 48 interviews. Participants were predominantly mothers (74%); 45% had children with chronic illnesses and 52% were admitted directly. Children had a median of 2 [IQR 1-3] healthcare encounters in the week preceding hospital admission, with 44% seeking care in multiple settings. Patterns of healthcare utilization were influenced by (i) disease acuity and healthcare access; (ii) past experiences; and (iii) varied perspectives about primary care and ED roles as hospital gatekeepers. Participants’ hospital admission priorities included: (i) effective clinical care; (ii) efficient admission processes; (iii) safety and security; (iv) timeliness; and (v) patient- and family-centered processes of care.
Conclusions:
Families received pre-admission care in several settings and described varying degrees of care coordination during their admission processes. This research can guide improvements in hospitals’ admission systems, necessary to achieve health system integration and continuity of care.
INTRODUCTION
Each year approximately 2 million children are admitted to hospitals in the United States (US), incurring costs that represent 40% of pediatric healthcare expenditures nationally.1,2 While numerous studies have characterized variation in physicians’ thresholds to admit children to hospital and called for more standardized approaches to hospital admission decisions, we know correspondingly very little about patients’ and families’ experiences and preferences as they move from outpatient to inpatient care.3–6
Hospital admission, like hospital discharge, reflects a transition of care associated with changes in care setting, healthcare providers and clinical management. While hospital discharge processes and hospital-to-home transitions have been the focus of considerable efforts to improve their quality and safety,7–9 there is a paucity of research about hospital admission processes and healthcare utilization preceding hospitalization. A small number of studies have compared the effectiveness of hospital admissions beginning in emergency departments (EDs) with direct admission to hospital, defined as hospital admission without receiving care in the hospital’s ED.10–12 For example, among children hospitalized with pneumonia, children admitted directly incurred lower healthcare costs and resource utilization with no differences in adverse outcomes.10 Another study found no differences in rates of unplanned transfer for intensive care among children admitted directly and through EDs.12 However, we know very little about parents’ perspectives about hospital admission approaches and outcomes. Understanding families’ perspectives in this arena may provide valuable guidance as we endeavor to improve the value of healthcare delivery and patients’ and families’ experiences across the care continuum. To this end, we aimed to: (i) characterize families’ experiences with the healthcare system as they transitioned from outpatient to inpatient care, (ii) identify hospital admission processes and outcomes most important to families, and (iii) identify how parental perspectives differed between children admitted directly and those admitted through EDs. We limited this work to children hospitalized with ambulatory care sensitive conditions (ACSC), defined as acute conditions for which ambulatory care may prevent disease progression, in order to represent common reasons for pediatric hospitalization at both community hospitals and children’s hospitals for which families might reasonably have contacted their primary care provider (PCP) prior to hospital admission, and thus for whom direct admission could be considered.13,14
METHODS
Study design & setting
We employed qualitative methods to provide rich descriptions of parents’ perspectives and develop a nuanced understanding of parents’ perspectives to inform subsequent research and quality improvement initiatives.15 We conducted semi-structured interviews with parents of hospitalized children at four structurally diverse hospitals in Massachusetts, US, in 2015-2016. Hospitals included one freestanding children’s hospital (with a dedicated pediatric ED), one children’s hospital nested within an adult hospital (with a dedicated pediatric ED from 12pm-12am), and two community hospitals with general pediatric wards (with general EDs). All of these hospitals accept hospital admissions both from their ED and via direct admission, and all have Hospital Medicine services where pediatric hospitalists provide inpatient care. However, the processes to accept direct admissions, and rates of direct admission, varied across these hospitals. With respect to referring healthcare providers, the majority of primary care in Massachusetts is provided by community and hospital-based general pediatricians whose practices include primary care for children with and without chronic conditions. Additional sources of ambulatory care include specialty clinics, urgent care (walk-in) clinics, and EDs.
In addition to interviews, participants completed a questionnaire to document sociodemographic characteristics. To understand patterns of pre-hospital admission clinical care we asked participants’ about their clinical encounters for their child’s illness in the 7 days preceding hospital admission (including primary care, specialty care, urgent care, emergency department care and hospitalizations). Institutional review board approval was received at [redacted].
Study population & sampling plan
Study participants were parents of hospitalized children and adolescents who had been admitted for unplanned hospital stays for common ACSCs (pneumonia, asthma, cellulitis, gastroenteritis/dehydration, urinary tract infections, and ear-nose-throat infections). Eligibility criteria included parent age >18 years, ability to communicate in English with the interviewer, and hospital admission to a general medical-surgical bed within the preceding 48 hours. Recognizing that approximately three-quarters of hospital admissions begin in EDs while one-quarter of children experience direct admissions,11 participants were purposefully sampled to represent both ED and direct admissions. Additionally, we purposefully sampled to represent children with and without co-existing chronic conditions.
Procedures
Interviews at all four hospitals were conducted by one member of the research team trained to conduct semi-structured interviews using a structured guide and associated question probes (PR). Potential participants were purposefully sampled based on the criteria described above to include both direct and ED admissions and children with and without comorbid chronic illnesses at each hospital. Following confirmation from the bedside nurse that the parent was present and that the child was clinically stable, the interviewer approached potential participants during day time hours to explain the study, request participation, and receive verbal consent from parents and assent from adolescents (when applicable). Children/adolescents were encouraged to share their perspectives as age and cognitive development allowed. Interviews were conducted in a private location within the hospital and audio-recorded with permission. To minimize recall bias, all interviews were conducted within 48 hours of hospital admission. Participants received a $10 gift card to recognize their participation. Audiofiles were professionally transcribed and verified for accuracy.
Interview guides were developed by the research team and pilot-tested with parents (not included in the final sample) to ensure that the questions were clear and elucidated nuanced, comprehensive responses. For the purpose of this study, hospital admission was defined as the period beginning upon arrival at the hospital and ending when the child had care initiated and was physically located in his/her hospital room. Interview questions focused on: (i) health care received in the 7 days preceding hospital admission; (ii) how the need for admission was identified; (iii) how the admission was facilitated; (iv) satisfaction with the admission process; (iv) perceptions of differences between direct admissions and ED admissions; (vi) challenges associated with the admission process and areas requiring improvement; and (vii) outcomes thought to be most relevant to quality improvement. Interviews were conducted sequentially, one hospital at a time, and stopped at each hospital when the study team agreed that data saturation was achieved.
Analysis
Using open-coding, an approach rooted in grounded theory, transcripts were reviewed by the research team to identify emergent concepts related to families’ admission experiences and preferences. These concepts and associated definitions were summarized in a jointly-developed coding framework.16,17 Two members of the research team then independently applied codes to a subset of transcripts; areas of coding disagreement were resolved through in-depth discussions of the concepts, corresponding codes, and definitions. Following assurance of coding agreement, transcripts were uploaded to Dedoose, a mixed-methods data management and analysis program, and one member of the research team coded the transcripts, with coding audits performed by the principal investigator.18 Analysis was performed during the interview period, and interviews were continued at each hospital until the research team agreed that no new relevant concepts or insights were emerging from the data (data saturation).19–21 Following open-coding of all interviews, all codes and associated transcript excerpts were reviewed by the research team to group similar concepts into themes. Similar themes were then grouped into domains, which were conceptualized within the context of the quality improvement literature to develop a framework for improving families’ hospital admission experiences. Descriptive statistics were employed to summarize quantitative data.
Participants
We conducted 48 interviews including 26 at community hospitals (n=14 at hospital 1 and n=12 at hospital 2) and 22 at children’s hospitals (n=12 at hospital 3 and n=10 at hospital 4). Each interview focused on the child’s current hospitalization; no parents were interviewed more than once. A total of 25 interviews represented children admitted directly and 23 represented children admitted through EDs. Based on analysis performed during the interview period, the research team agreed that data saturation was achieved at each hospital, with sample sizes falling with the range suggested by qualitative methods guidelines.20–22 Participants were predominantly mothers (75%); 70% were native English speakers and 70% had some college education. Approximately half of children were privately insured; 45% had chronic illnesses and 100% had primary care providers (Table 1).
Table 1.
Sociodemographic characteristics of participants (n=48)#
| Parent characteristics* | n (%) | |
|---|---|---|
| Parent age, years (median, IQR) | 33 [28.5, 42.5] | |
| Relationship to child: | ||
| Mother | 35 | (74%) |
| Father | 11 | (23%) |
| Other relative/guardian | 1 | (2%) |
| Parent race/ethnicity: | ||
| Non-hispanic white | 26 | (57%) |
| Non-hispanic Black | 7 | (15%) |
| Hispanic | 8 | (17%) |
| Asian | 3 | (7%) |
| Other | 2 | (4%) |
| Native English speaker (% yes) | 33 | (70%) |
| Educational attainment: | ||
| ≤ high-school | 14 | (30%) |
| Some college or 2-year degree | 13 | (28%) |
| ≥ 4-year college graduate | 20 | (43%) |
| Child characteristics | ||
| Child age, years (median, IQR) | 2.5 [0.7-7.8] | |
| Child gender (female) | 17 | (36%) |
| Primary payor: | ||
| Private health insurance | 24 | (52%) |
| Public | 22 | (48%) |
| Principal reason for hospitalization: | ||
| Gastroenteritis/dehydration | 17 | (36%) |
| Respiratory illness (asthma, pneumonia) | 14 | (30%) |
| Urinary tract infection | 8 | (17%) |
| Skin/soft tissue infection | 5 | (11%) |
| Other | 3 | (6%) |
| Concurrent chronic illness | 21 | (45%) |
| Has primary care provider | 47 | (100%) |
missing for one participant
RESULTS
Healthcare encounters preceding hospital admission
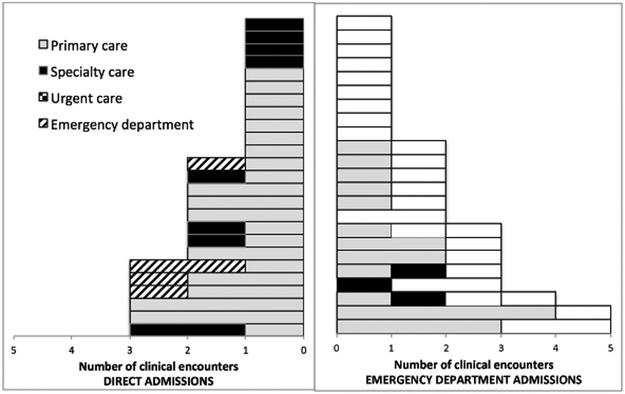
Figure 1 illustrates the ambulatory and ED care received by children in the 7 days preceding hospitalization. During this period, hospitalized children had a median of 2 clinical encounters with PCPs, specialists, urgent care clinics and EDs, with a range from 1 to 5 visits. Approximately half (n=27, 56%) of parents reported that all of their pre-hospitalization visits occurred in one care setting, while 44% (n=21) received care in 2 or more settings. Although children admitted directly reported fewer ED visits and more PCP visits, there were not differences between the groups regarding the number of clinical encounters in the week prior to hospitalization (p=0.45).
Figure 1.
Healthcare encounters in the 7 days preceding hospital admission among children admitted directly and through emergency departments; each row represents one child.
When asked about factors that influenced where they sought care, parents’ responses aligned with three domains: (i) illness acuity and healthcare accessibility; (ii) past experiences with the health care system; and (iii) primary care and ED roles as gatekeepers to hospitalization.
Illness Acuity & Healthcare Accessibility
Parents’ reported that the relative acuity of their child’s illness was a major factor influencing where they sought health care. For example, one parent stated, “We’ve been going to the pediatrician all along. As the symptoms really got significantly worse we decided to take him to the emergency room. It was more acute.” (Participant A3, community hospital). Among children directly admitted to hospital, several parents reported multiple visits to their PCP prior to hospitalization for intensive outpatient management and follow-up, with one parent reporting 3 visits to her child’s PCP in 24 hours for close observation. In contrast, other parents reported that their PCPs directed them to the ED for acute care management, due to both resource limitations for acute care provision within primary care practices as well as the time of day or week. For example, one parent of a child admitted through the ED reported, “The clinic is closed at night, that’s why I go to the Emergency Room. If the clinic is open, I’m going to the clinic.“ (Participant A5, community hospital). Another stated, “No one ever gets sick Monday through Friday during business hours. It is on the weekend or overnight… “ (Participant D7, children’s hospital). In our sample, limited primary care office hours appeared to be the largest barrier to PCP accessibility; relatively few parents reported difficulties scheduling same-day appointments for acute care visits.
Past experiences with the healthcare system
Parents also reported that their past experiences with the healthcare system, either related to their currently hospitalized child or for other family members, influenced where they sought care in advance of their child’s hospitalization. One parent reported, “For my older daughter, when she had a fever of 100.7 and I took her to the clinic first they told me, actually, just go to the ER… So instead of wasting my time there [clinic], I came straight here [ED].“ (Participant D6, children’s hospital). A subset of parents of children with chronic conditions described that they had a written protocol that influenced their choice of healthcare setting, stating, “There’s a protocol of when you go to the pediatrician and when you come to the hospital [ED].“ (Participant Bl, community hospital).
PCP and ED roles as hospital gatekeepers
The most notable difference between parents of children admitted through EDs compared with direct admission related to their perspectives about the roles of PCPs and ED providers as hospital gatekeepers. Parents of children who were directly admitted described that they trusted their PCP and felt that s/he was in the best position to advise them about the most appropriate care. They also described how their PCP’s ability to arrange a direct admission facilitated continuity of care. Representative quotations from parents illustrating this domain are provided in Table 2. These quotes demonstrate that parent of children who were admitted directly had well-established relationships with their PCP and highly valued PCP involvement in all aspects of their child’s healthcare.
Table 2.
Variation in perspective regarding primary care and emergency department providers as gatekeepers to hospital admission.
| Primary care provider as hospital gatekeeper | Emergency department as hospital gatekeeper |
|---|---|
|
“We rely on the doctors to tell us what’s causing the sickness… Any time we fell that she needs to go to the hospital, or she’s sick, we go to the pediatrician first… so they tell us what to do ” (Participant B4, community hospital) “I trust the doctor’s expertise.”. ” (Participant B5, community hospital) “They are in charge of her complete care for the rest of her life, pretty much.”. (Participant C7, children’s hospital) “He’s been his pediatrician since birth, excellent. We trust him one hundred percent.” (Participant A12, community hospital) “We work with the pediatrician. If we were coming to the emergency room every time, we don’t know who we ‘re going to get. It’s basically going through the same thing over and over from the beginning.” (Participant A8, community hospital) We had a feeling that he probably was going to get admitted but we wanted to go through the process of bringing him to the pediatrician and have him do the tests cause… I don’t want to come here and have him admitted if there’s nothing going on, just to do all those tests here if they could do it at the pediatrician. I’d rather have them do the tests and we ‘re coming in with some knowledge of what’s going on. (Participant C8, children’s hospital) |
“I knew that he was going to come in [for admission] before we got to the ER. The point of going to the ER was to get him in… ” Participant B1, community hospital) “I was going to take her to the doctor’s office, but, like, what is the point of going to the doctor’s office. They are not doing nothing for her… So let her go to the hospital. They probably will know what to do better in this situation.” Participant B9, community hospital) Personally, I would rather go to the Emergency vs. having your doctor in the middle. (Participant D4, children’s hospital) … We went to the ER because we weren’t already established here… We were brand new here. (Participant D11, children’s hospital) Because at least they have x-rays or something they can use to at least see what I can’t see to help pinpoint the problem. So yeah. I’m always quick to say let’s go the ER or to the hospital to see what’s wrong. (Participant C3, children’s hospital) “He had been sick with diarrhea and vomiting for 2 weeks so I took him to the doctor, and his doctor referred him to the ER just to check and see if there was anything worse.”. (Participant D9, children’s hospital) |
In contrast, parents of children admitted through EDs were less likely to describe their PCP as a key stakeholder in the hospital admission process, reporting that they didn’t want to have their PCP “in the middle” when their child required hospitalization. They described the ED as “the filter for [access to] the rest of the hospital,” and reported how the ED provided opportunities for a “second opinion,” rapid diagnostic testing, and the opportunity to avoid unnecessary hospital admission. For example, one parent stated, “The pediatrician [primary care provider] might have his worry meter up, saying this person needs to be admitted. What if we get here [ED] and get admitted and then the specialist says you didn’t really have to be in here? … And so they were sort of that middleman. And I think that the ER does that a lot.“ (Participant D9, children’s hospital). These quotations suggest that among children admitted through EDs, several parents were wary that their PCP would be able assist with acute care while in other cases and therefore bypassed PCP involvement. However, for other children admitted through EDs, the PCPs themselves suggested that the ED was the most appropriate venue for acute care management. Among children admitted through EDs, 43% (n=10) reported that they had been directed there by their PCPs.
Processes and outcomes prioritized by families
When asked to describe hospital admission processes and outcomes that were most important to them, parents’ responses encompassed five domains: (i) effective clinical care; (ii) efficiency; (iii) safety and security; (iv) timeliness; and (v) patient- and family-centered care. Minor themes within each of these domains, as well as key concepts discussed by participants, are shown in Table 3.
Table 3.
Domains and associated themes summarizing hospital admission processes and outcomes most valued by parents of hospitalized children.
| Domain | Themes | Key concepts expressed by participants |
|---|---|---|
| Effective clinical care | A. Clinical improvement B. Healthcare team expertise |
• Improvement in symptoms and return to baseline health status • Avoidance of medical errors • Healthcare team that is knowledgeable about pediatric problems and disease management |
| Efficiency | A. Avoid unnecessary hospitalizations B. Avoid unnecessary clinical encounters C. Avoid unnecessary diagnostic testing |
• Referral to the ED provides an opportunity for a second opinion and the potential to avoid hospital admission • Direct admission can decrease the number of healthcare providers involved in care (by bypassing the ED) • Desire to avoid diagnostic testing that is not needed, or that has already been performed in another setting |
| Safety and security | A. Safe physical environment B. Low nosocomial infection risk |
• Ready availability of medications and equipment to address acute health problems • Avoidance of exposure to noise, trauma, ill adults, stressful environment • Avoidance of exposure to other infectious disease risks |
| Timeliness | A. Rapid diagnosis and treatment B. Rapid bed placement |
• Desire to receive diagnostic testing and treatment initiation as quickly as possible • Minimize waiting times to be placed in a hospital room / bed |
| Patient- and family-centered care | A. Respect for parents’ perspectives B. Effective communication & transitions C. Privacy/atmosphere E. Convenience F. Low out-of-pocket costs |
• Parents’ desire to have their concerns taken seriously, and to be respected for their knowledge about how their child’s condition has changed from baseline and what disease management has already occurred • Effective communication with families: healthcare team demonstrates empathy towards parent(s) and child; keep the family updated re. timelines, next steps, and results of diagnostic testing • Effective communication within the healthcare team: effective handoffs between physicians in different departments, including between referring and accepting providers, and over time • Pediatric-friendly waiting room and/or treatment spaces • Quiet and private spaces for child to rest and recover • Receipt of healthcare that is easy and convenient to access; healthcare processes that minimize demands on parent(s) and child • Receipt of healthcare in settings that minimize direct and indirect costs to families |
Although all five domains were described by parents of children who were admitted directly and through EDs, we observed variation between the groups with respect to the minor themes emphasized. Representative quotations, categorized according to admission source, are provided in the Supplement to demonstrate how the hospital admission processes and outcomes most valued by parents varied according to hospital admission source. Within the efficiency domain, parents described how, unlike direct admissions, initiating care in the ED might avoid hospitalization. For example, one parent of a child with a chronic condition stated, “…There’s a chance you ‘re going home when you get admitted into the ER… there’s a 50-50 split whether she bounces back and we can go home…that’s really the most ideal.” (Participant A9, community hospital). In contrast, parents of children admitted directly described efficiency associated with fewer clinical encounters, with one parent describing ED care as “an unnecessary step.”
Parents of children admitted directly and through EDs both prioritized a safe physical environment, with parents of children admitted through EDs valuing the relatively large healthcare staff in the ED and rapid access to medical equipment, and parents of directly admitted children describing the value of security and privacy in their hospital rooms, perceived decreased risk of nosocomial infection and exposure to “other people’s issues,” such as trauma and drug overdoses/toxic ingestions. Parents in both groups valued rapid diagnosis and treatment and rapid bed placement, but had differing perspectives about how these outcomes could be achieved via the different portals of hospitalization. For example, some parents reported that they were able to receive “a lot of the tests a lot faster …in the ED” while other parents reported that diagnostic testing and treatment initiation occurred more quickly via direct admission. These varied responses occurred within the same hospital and across hospitals, and didn’t appear to be related to the chronicity of the child’s medical concerns.
Patient-centered care was also valued by parents in both groups. Direct admission was described as providing more personalized care in a more comfortable environment, with one parent described direct admission as “more 1 to 1 service.” Parents among children admitted directly as well as through EDs both expressed concerns that communication between healthcare providers was often poor, particularly related to “debrief[ing] each other” and consistency in clinical management approaches across healthcare providers, and that updates regarding timelines and next steps were frequently not communicated to them.
DISCUSSION
To our knowledge, this is the first study to examine patterns of and reasons for pediatric preadmission acute care among hospitalized children and to characterize parents’ perspectives and preferences regarding hospital admission processes. We identified quality domains prioritized by parents regarding their child’s hospital admission, generating valuable data to inform initiatives to improve transitions from outpatient to inpatient settings, and to guide efforts to improve health system integration while reducing healthcare utilization.
We found that, among this group of children hospitalized with ACSC, the week preceding hospitalization was a period of substantial healthcare utilization, with the majority of children having more than one clinical encounter during this time, often in multiple settings. Parents reported that recurrent healthcare visits were influenced by both PCPs or specialists requesting close clinical follow-up and by their own ongoing concerns about their child. Our findings highlight that, similar to post-discharge care, pre-admission healthcare utilization is substantial and associated with varied degrees of continuity. While a small number of studies have illustrated associations between continuity of care for well child visits and decreased risk of hospitalization for ACSC, further research is needed to determine if improved continuity of care for acute illnesses is associated with decreased risk of hospitalization and resource utilization during hospital stays.23,24 In addition, our findings raise questions about whether expanding bundled payments for “episodes of care” to include healthcare during the pre-admission period would incentivize high value care across the care continuum.25
The results of this study also expand on the literature about why patients seek acute care in EDs. Although several parents in our sample described their PCP as the first and most appropriate point of contact to access all healthcare services, others viewed the ED as the most appropriate avenue for acute care and did not conceptualize PCPs in this role. Past studies have described how insurance coverage, disease acuity, and PCP access, availability, and affordability are associated with where patients seek care for acute illnesses.26–29 Our results suggest that parental perspectives about PCPs’ roles in acute care management and hospitalization decisions also strongly influence where they seek care. First contact, coordinated care are key principles of the patient-centered medical home;30 increasing parental knowledge about these principles may reduce ED utilization and improve care coordination.
Among children admitted through EDs, PCPs were the first point of contact for approximately 50%; this number is similar to national survey data that found that, among a predominantly adult population, only 42% saw their PCP for “first contact” care for acute conditions.31 In contrast, more than 90% of children admitted directly saw their PCP for initial disease management. These findings speak to the enhanced opportunity for care coordination among directly admitted children. Effective hand-offs from outpatient to inpatient providers, as described by parents in our study, may contribute to lower rates of diagnostic testing and healthcare costs observed in previous studies comparing direct and ED admissions.10,11 Given variation in outpatient clinic hours and accessibility, as well as variation in the resources available in primary care offices to provide acute care, the ED plays an important role in acute care provision. Enhanced handoff between PCPs and EDs, as well as shared electronic health records, may similarly improve care coordination and reduce duplicative diagnostic testing as described in this study.
While considerable research and health policy efforts have been dedicated to develop validated quality measures to evaluate transitional care, transitions into the hospital have received little attention.32–35 Our identification of quality domains prioritized by families lays important groundwork for future quality improvement work in this area. Parents of children admitted through EDs and via direct admission valued effective, efficient, timely, safe and patient-centered care, with several themes within these domains specific to their hospital admission experiences. While some of these domains can be evaluating using existing survey instruments, future work is needed to operationalize the evaluation of other domains emerging in this research. For example, the Child Hospital Consumer Assessment of Healthcare Providers and Systems survey evaluates patient and family experience of care during their hospital stay and includes assessment of communication with parents as well as attention to safety and comfort.36 However, to our knowledge there are not validated quality measures to evaluate parents’ perceptions about the timeliness of diagnosis and treatment, avoidance of duplicative diagnostic testing, or the effectiveness of hand-offs between outpatient, ED and inpatient providers. In addition, we are not aware of any quality measures that are specific to hospital admission procedures that could be applied for both ED and direct admissions. Development of quality measures in these areas are important next steps to evaluate families’ experiences as they transition from outpatient to inpatient care.
STRENGTHS AND LIMITATIONS
Our results should be interpreted in light of its strengths and limitations. Strengths of this study include its multi-center design, incorporating the perspectives of parents admitted to structurally diverse hospitals. The validity and transferability of our work is supported by the consistency of or results across these settings, and among parents of children with and without chronic conditions. By excluding parents who did not speak English we may have missed themes of particular importance to non-English-speaking families. Massachusetts has a very high rate of health insurance coverage for children, and all children represented in this study were insured. Correspondingly, these findings may not be applicable to children without health insurance. Relatedly, 98% of children in the Northeastern United States have a usual source of healthcare; this percentage is somewhat higher than the rest of the country. A referral from an outpatient-based physician to the hospital is required for all direct admissions; as a result our findings may not apply to children without primary care access. In addition, primary care practices vary considerably in their resources available to provide acute care in outpatient settings; this study did not examine how resources available in outpatient settings are related to hospital admission approach. We conducted interviews with parents during their child’s hospitalization, thereby excluding children who were referred to the ED for hospitalization but discharged home. As a result, determining the potential preventability of these pediatric hospitalizations is beyond the scope of this work. Lastly, it is important to note that qualitative research is, by design, hypothesis generating; further studies of representative populations are needed to determine how to optimize hospital admission experiences and pre-admission coordination of care.
CONCLUSIONS
The majority of hospitalized children had at least two encounters with healthcare providers in the week preceding hospitalization, often in multiple settings. Parents prioritized efficient, timely and family-centered hospital admission processes, which were variably achieved. This research may guide improvements in hospitals’ admission systems and inform quality assessment of both ED and direct admissions. Given the national focus on health system integration and continuity of care, these findings are particularly relevant.
Supplementary Material
Acknowledgments
Funding Source: This research was supported by funding from the National Heart, Lung, and Blood Institute (K24HL132008); Agency for Healthcare Research and Quality (K08HS024133); National Center for Advancing Translational Sciences, National Institutes of Health (UL1TR001064). The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ or the NIH.
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
REFERENCES
- 1.Lassman D, Hartman M, Washington B, Andrews K, Catlin A. US health spending trends by age and gender: selected years 2002–10. Health Aff Millwood). 2014:33(5):815–822. doi: 10.1377/hlthaff.2013.1224. [DOI] [PubMed] [Google Scholar]
- 2.Moore B, Levit K, Elixhauser A. Ph D.Costs for Hospital Stays in the United States, 2012. Healthcare Cost and Utilization Project 181. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sbl8l-Hospital-Costs-United-States-2012.pdf. Accessed Septe. [PubMed] [Google Scholar]
- 3.Sabbatini AK, Nallamothu BK, Kocher KE. Reducing variation in hospital admissions from the emergency department for low-mortality conditions may produce savings. Health Aff. 2014;33(9): 1655–1663. doi: 10.1377/hlthaff.2013.1318. [DOI] [PubMed] [Google Scholar]
- 4.Abualenain J, Frohna WJ, Shesser R, Ding R, Smith M, Pines JM. Emergency department physician-level and hospital-level variation in admission rates. Ann EmergMed. 2013;61(6):638–643. doi: 10.1016/j.annemergmed.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Pines JM, Mutter RL ZM. Variation in emergency department admission rates across the United States. Med Care Res Rev. 2013;70(2):218–231. [DOI] [PubMed] [Google Scholar]
- 6.Bourgeois FT, Monuteaux MC, Stack AM, Neuman MI. Variation in Emergency Department Admission Rates in US Children’s Hospitals. Pediatrics. 2014; 134(3):539–545. doi: 10.1542/peds.2014-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians- Society of Academic Emergency Medicine. J Gen InternMed. 2009;24(8):971–976. doi: 10.1007/sl1606-009-0969-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med. 2014;65:471–485. doi: 10.1146/annurev-med-022613-090415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Auger K a, Kenyon CC, Feudtner C, Davis MM. Pediatric hospital discharge interventions to reduce subsequent utilization: a systematic review. J Hosp Med. 2014;9(4):251–260. doi: 10.1002/jhm.2134. [DOI] [PubMed] [Google Scholar]
- 10.Leyenaar JK, Shieh M, Lagu T, Pekow PS, Lindenauer PK. Variation and outcomes associated with direct admission among children with pneumonia in the United States. JAMA Pediatr. 2014;168(9):829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leyenaar J, Shieh M-S, Lagu T, Pekow PS, Lindenauer PK. Direct admission to hospitals among children in the United States. JAMA Pediatr. 2015;169(5):500–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reese J, Deakyne S, Blanchard A, Bajaj L. Rate of preventable early unplanned intensive care unit transfer for direct admissions and emergency department admissions. Hosp Pediatr. 2015;5(1):27–34. [DOI] [PubMed] [Google Scholar]
- 13.Agency for Health Care Research and Quality. Prevention Quality Indicators Overview. Available at: https://www.qualityindicators.ahrq.gov/Modules/pqi_resources.aspx. Accessed May 28, 2017.
- 14.Leyenaar JK, Ralston SL, Shieh M, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of Pediatric Hospitalizations at General Hospitals and Freestanding Children ‘ s Hospitals in the United States. J Hosp Med. 2016;0(0):1–7. doi: 10.1002/jhm.2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sofaer S Qualitative Methods : What Are They and Why Use Them ? Health Serv Res. 1999;34(5): 1101–1118. [PMC free article] [PubMed] [Google Scholar]
- 16.Ulin P, Robinson E, Tolley E. Qualitative Methods in Public Health: A Field Guide for Applied Research. [Google Scholar]
- 17.Seidel JV Qualitative Data Analysis; www.qualisresearch.com (originally published in The Ethnograph v5.0: A Users Guide; Appendix E; 1998; Colorado Springs; Colorado: Qualis Research; ). Accessed April 4, 2016 Ethnogr v4. 1998;(c): 1–15. http://www.qualisresearch.com/DownLoads/qda.pdf. [Google Scholar]
- 18.Dedoose Version 5.0.11, web application for managing, analyzing, and presenting qualitative and mixed method research data (2014). Lsssssos Angeles, CA: SocioCultural Research Consultants, LLC; (www.dedoose.com). [Google Scholar]
- 19.Creswell J, Miller D. Determining validity in qualitative inquiry. Theory Pract. 2000;39(3): 124–130. [Google Scholar]
- 20.Creswell J Qualitative Inquiry and Research Design: Choosing among Five Traditions. 3rd ed Thousand Oaks, CA: Sage Publications Inc.; 2013. [Google Scholar]
- 21.Morse JM. Determining Sample Size. Qual Health Res. 2000;10(1):3–5. [Google Scholar]
- 22.Guest G, Bunce A, Johnson L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field methods. 2006;18(1):59–82. doi: 10.1177/1525822X05279903. [DOI] [Google Scholar]
- 23.Tom J, Tseng C, Davis J, Solomon C, Zhou C, Mangione-Smith R. Missed well-child care visits, low continuity of care, and risk for ambulatory care sensitive hospitalizations in young children. Arch Pediatr Adolesc Med. 2010; 164(11): 1052–1058. doi: 10.1001/archpediatrics.2010.201. MISSED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Enlow E, Passarella M, SA L. Continuity of Care in Infancy and Early Childhood Health Outcomes. Pediatrics. 2017;140(1):e20170339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Medicare and Medicaid Services. Bundled Payments for Care Improvement (BPCI) Initiative: General Information. Available at: https://innovation.cms.gov/initiatives/bundled-payments/. Accessed August 6, 2017.
- 26.Kangovi S, Barg FK, Carter T, Long J a, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood). 2013;32(7):1196–1203. doi: 10.1377/hlthaff.2012.0825. [DOI] [PubMed] [Google Scholar]
- 27.Johnson W, Rimsza M. The Effects of Access to Pediatric Care and Insurance Coverage on Emergency Department Utilization. Pediatrics. 2004; 113(3):483–487. [DOI] [PubMed] [Google Scholar]
- 28.Luo X, Liu G, Frush K, Hey L. Chilren’s Health Insurance Status and Emergency Department Utilization in the United States. Pediatrics. 2003; 112(2):314–319. [DOI] [PubMed] [Google Scholar]
- 29.Racine AD, Alderman EM, Avner JR. Effect of Telephone Calls From Primary Care Practices on Follow-up Visits After Pediatric Emergency Department Visits. Arch Pediatr Adolesc Med. 2009;163(6):505–511. [DOI] [PubMed] [Google Scholar]
- 30.Academy A. American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home. March 2007. :1–3. [Google Scholar]
- 31.Pitts SR, Carrier ER, Rich EC, Kellermann AL. Where Americans get acute care: increasingly, it’s not at their doctor’s office. Health Aff (Millwood). 2010;29(9):1620–1629. doi: 10.1377/hlthaff.2009.1026. [DOI] [PubMed] [Google Scholar]
- 32.Coleman E a, Parry C, Chalmers S, Min S. The Care Transitions Intervention. Arch Intern Med. 2006; 166(17): 1822–1828. doi: 10.1001/archinte.l66.17.1822. [DOI] [PubMed] [Google Scholar]
- 33.Leyenaar JK, Desai AD, Burkhart Q, Parast L, Roth CP. Quality Measures to Assess Care Transitions for Hospitalized Children. Pediatrics. 2016; 138(2): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parast L, Burkhart Q, Desai AD, et al. Validation of New Quality Measures for Transitions Between Sites of Care. Pediatrics. 2017;139(5):e20164178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Desai AD, Burkhart Q, Parast L, et al. Development and Pilot Testing of Caregiver-Reported Pediatric Quality Measures for Transitions Between Sites of Care. Acad Pediatr. 2016;16(8):760–769. doi: 10.1016/j.acap.2016.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Toomey SL, Elliott MN, Zaslavsky AM, et al. Variation in Family Experience of Pediatric Inpatient Care As Measured by Child HCAHPS. 2017;139(4). doi: 10.1542/peds.2016-3372. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.