Abstract
Osteochondromas rarely induce vascular complications by mechanical compression. We present the case of a subclavian artery pseudoaneursym caused by an osteochondroma of the scapula in a 67-year-old male. The diagnosis was based on a previous history of multiple exostoses, computed tomography and magnetic resonance imaging, as well as the local vascular clinical status of the lesion. Surgical treatment consisted of vascular and orthopaedic intervention. First, the vascular surgeon implanted a bypass of the subclavian artery from the ventral aspect, enabling the orthopaedic surgeon to resect the osteochondroma from the dorsal aspect. The patient recovered with full function. Vascular pseundoaneurysms should be taken into consideration in patients with osteochondromas, especially with a known history of multiple hereditary exostoses.
Keywords: Osteochondroma, pseudoaneurysm, scapula, subclavian artery
Introduction
Osteochondromas represent about one-third of benign bone tumours. They can present as solitary lesions or rarely as multiple hereditary exostoses. They occur most commonly in the metaphyses and diametaphyses of long bones, mainly the femur and tibia, and are covered with a soft cartilaginous cap which undergoes ossification.1
Vascular complications such as arterial pseudoaneurysms induced by mechanical compression of bone tumours are rare.2 To our knowledge, this is the first case report presenting a pseudoaneurysm of the subclavian artery induced by mechanical compression of an osteochondroma of the scapula.
Case presentation
A 67-year-old male patient was referred from a state hospital to our orthopaedic outpatient department with an expansive mass in the left scapula and a differential diagnosis of a chondrosarcoma. The patient presented with a 2-month history of progressive pain in the left scapula, which radiated to the elbow. In the previous 2 weeks the pain had been accompanied by oedema of the entire left arm and gradual loss of muscle strength. Upper extremity strength testing of the left arm showed slightly reduced muscle strength in comparison to the right arm (4/5). The patient did not exhibit any sensory disturbances. The radial pulse was palpable. At the time of referral, the patient’s visual analogue pain score (VAS) was 9/10 despite analgesic therapy with intravenous opioid patient-controlled analgesia, oral opioids (Hydromorphone) and non-opioid analgesics. Computed tomography (CT) and magnetic resonance imaging (MRI) of the left scapula showed a 7-cm long bone spur on the ventro-cranial aspect of the scapula, with 3 cm of soft tissue surrounding the exostosis (Figures 1 and 2). MRI was performed without contrast medium due to the patient’s massive pain and inability to remain still during the imaging, which resulted in poor image quality (Figure 3). According to the radiology report, the soft tissue mass was thought to be a large cartilaginous cap. Since the patient had a history of multiple hereditary exostoses and a scapular cartilage resection performed in 2011, the primary differential diagnosis was a chondrosarcoma. On the ventral aspect, the tumour mass was in direct contact with the subclavian artery and vein. The patient was informed of the necessity of performing a biopsy of the tumour as well as further diagnostic methods and was admitted to our department. First, bone scintigraphy revealed increased tracer uptake at the superior angle of the left scapula. The subsequent MRI was again unsuccessful, as the patient was unable to remain still. We proceeded with the core-needle biopsy under ultrasound guidance, which was uneventful. The histology report of the biopsy showed an old blood coagulum with no signs of malignancy.
Figure 1.
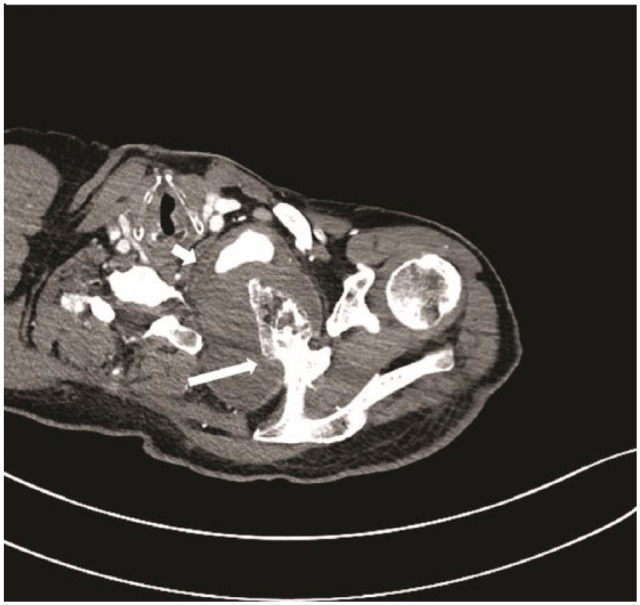
Computed tomography: horizontal view of the left scapula. Long arrow: 7-cm long bone spur; short arrow: 3 cm of soft tissue surrounding the exostosis.
Figure 3.
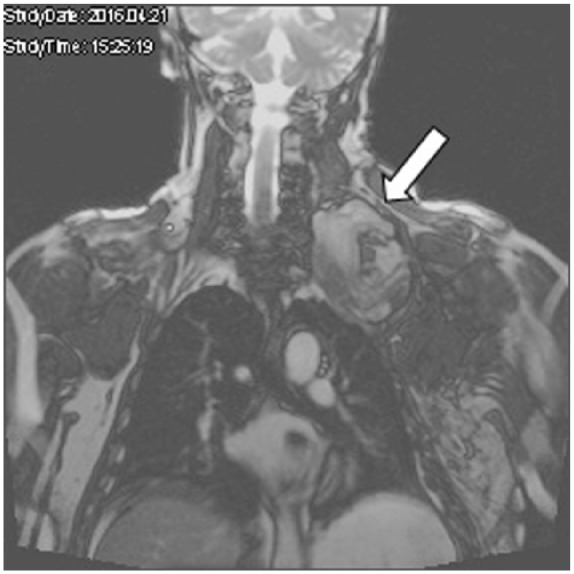
Magnetic resonance imaging: coronal view of the left scapula. Arrow: tissue surrounding soft tissue.
Figure 2.

Computed tomography: sagittal view of the left scapula. Long arrow: 7-cm long bone spur; short arrow: 3 cm of soft tissue surrounding the exostosis.
For further clarification, a new CT was performed. Analysis of the new CT images set the suspicion of a pseudoaneurysm of the subclavian artery with an expansion of 4.3 × 4 cm2 in the ventral aspect of the lesion. Due to the proximity of the subclavian vessels, a vascular surgeon was consulted prior to tumour resection. Clinical examination revealed pulsation of the soft tissue portion of the ventral side of the tumour, the portion which was initially thought to be a chondral cap. The planned surgical treatment consisted of vascular and orthopaedic intervention. Initially, a ventral approach was taken through the subclavian triangle and axillary fossa, using a GORE-TEX® 8 mm Vascular Graft (Figure 4) in the setting of the subclavian artery. Afterwards, a dorsal approach was taken to resect the osteochondroma and remove the surrounding haematoma. The histology report of the surgical specimen showed bone tissue with reactive changes, oedema, chronic inflammation and focal enchondral ossification but no prominent cartilage cap (Figure 5). After the operation, the patient had a normal palpable peripheral pulse. At the latest follow-up 6 months after the operation, the patient exhibited full shoulder function with no evidence of any vascular or neurological sequelae.
Figure 4.

Subclavian-axillary bypass grafting short arrows (GORE-TEX® 8 mm Vascular Graft) made by ventral approach through jugulum and axillary fossa.
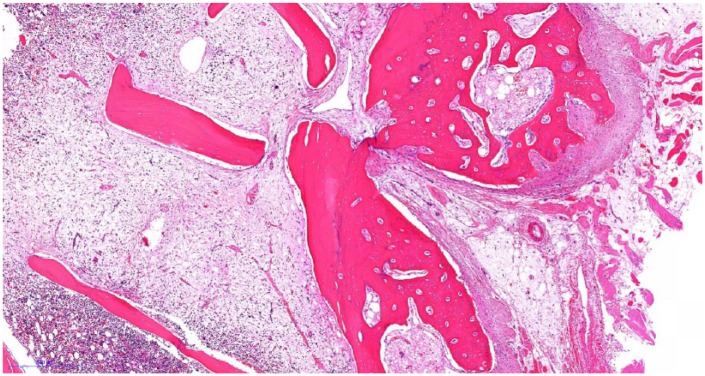
Figure 5.
Histopathological evaluation of the surgical specimen showed bone tissue with reactive changes, oedema, chronic inflammation and focal enchondral ossification but no prominent cartilage cap (hematoxylin and eosin staining, magnification 4×).
Discussion
To our knowledge, this is the first case report presenting a pseudoaneurysm of the subclavian artery induced by mechanical compression of a tumour of the scapula. The risk of mechanical compression of a vessel by a bone exostosis such as an osteochondroma is unknown. Arterial damage is represented in 91% of vascular complications,2 including pseudoaneurysms and aneurysms, intermittent compression, thrombosis and stenosis while venous damage is presented with venous thrombosis or compression.2–4 Pseudoaneurysms are rare and mainly occur after the end of enchondral ossification phase, when the cartilage cap becomes firm and rigid.2 The mean age at which vascular complications usually occur is 22.6 years,2 in contrast to our patient, who was 67 years of age. The most common site of a pseudoaneurysm-associated osteochondroma was the femur (86%), with the popliteal artery as the most commonly injured vessel (77%).2 The main complication in osteochondromas is malignant transformation, with incidence rising from 1 to 10 with multiple hereditary exostoses.2 Vascular complications in the arm or upper torso are extremely rare, with only two cases of compression of the subclavian artery described due to the first rib and clavicle,5,6 few cases of pseudoaneurysm of the brachial artery7–11 and one case of subclavian vein thrombosis.12 In 36% of cases, patients had a history of multiple hereditary exostoses.13 A delayed brachial artery pseudoaneurysm was described 3 and 13 years after the excision of a humeral osteochondroma.7,9 Since our patient was 67 years of age with a previously performed osteochondroma resection 5 years previously, we endorse the need for a long-term postoperative follow-up of patients at any age, especially with a history of multiple hereditary exostoses.
When conventional radiology is sufficient for the diagnosis of osteochondroma, further demonstration of adjacent structures is presented by MRI and CT scans. MRI provides excellent visualisation of arterial and venous compromise and is the most accurate method for measuring cartilaginous cap thickness. When the cartilaginous cap thickness exceeds 2 cm in adults and 3 cm in children, malignant transformation should be considered.14
The diagnosis of an arterial lesion should be confirmed with duplex ultrasonography, CT, magnetic resonance angiography (MRA) or conventional angiogram.2,8 These methods were not used in our case due to sufficient supporting clinical, histological and radiological evidence. Depending on the degree of vessel damage, end-to-end anastomosis, autologous saphenous vein graft or synthetic graft placement can be performed.2,13 In our case, the vascular surgeon deemed the extent of the subclavian artery pseudoaneurysm as un-reparable and opted for a synthetic graft.
Conclusion
Due to the proximity to the tumour, the mechanical damage to vessels, pseudoaneurysm is a plausible differential diagnosis and should be taken into consideration. The collaboration of vascular and orthopaedic surgeons in the reconstruction of major blood vessels in proximity of bone tumours is recommended.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymised information to be published in this article.
References
- 1. Hakim DN, Pelly T, Kulendran M, et al. Benign tumours of the bone: a review. J Bone Oncol 2015; 4(2): 37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vasseur MA, Fabre O. Vascular complications of osteochondromas. J Vasc Surg 2000; 31(3): 532–538. [PubMed] [Google Scholar]
- 3. Lucarelli DD, Subram A. Type IV popliteal arterial entrapment associated with an osteochondroma. J Vasc Surg Cases Innov Tech 2017; 3(2): 66–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ruales Romero AM, Doiz Artazcoz E, Craven-Bartle Coll A, et al. Thrombosed popliteal artery pseudoaneurysm as herald of tibial osteochondroma. EJVES Short Rep 2016; 33: 27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kobayashi H, Ikegami M, Ushiku T, et al. Secondary chondrosarcoma presenting with symptoms similar to thoracic outlet syndrome. Case Rep Orthop 2018; 2018: 9347145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gokkus K, Atmaca H, Sagtas E, et al. Osteochondromas originating from unusual locations complicating orthopedic discipline: case series. Eklem Hastalik Cerrahisi 2015; 26(2): 100–109. [DOI] [PubMed] [Google Scholar]
- 7. Scotti C, Marone EM, Brasca LE, et al. Pseudoaneurysm overlying an osteochondroma: a noteworthy complication. J Orthop Traumatol 2010; 11(4): 251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Koenig SJ, Toth AP, Martinez S, et al. Traumatic pseudoaneurysm of the brachial artery caused by an osteochondroma, mimicking biceps rupture in a weightlifter: a case report. Am J Sports Med 2004; 32(4): 1049–1053. [DOI] [PubMed] [Google Scholar]
- 9. Tobias AM, Chang B. A rare brachial artery pseudoaneurysm 13 years after excision of a humeral osteochondroma. Ann Plast Surg 2004; 52(4): 419–422. [DOI] [PubMed] [Google Scholar]
- 10. Villanueva-Garcia E, Bas-Hermida P, Espinosa-Lledo C. Pseudoaneurysm of the brachial artery caused by an osteochondroma. A report of two cases. Int Orthop 1995; 19(4): 248–250. [DOI] [PubMed] [Google Scholar]
- 11. Papacharalampous G, Galyfos G, Geropapas G, et al. False arterial aneurysm due to long bone exostosis: presentation of two cases and update on proper management. Ann Vasc Surg 2015; 29(4): 842.e19–842.e22. [DOI] [PubMed] [Google Scholar]
- 12. Mollano AV, Hagy ML, Jones KB, et al. Unusual osteochondroma of the medial part of the clavicle causing subclavian vein thrombosis and brachial plexopathy. J Bone Joint Surg Am 2004; 86-A(12): 2747–2750. [DOI] [PubMed] [Google Scholar]
- 13. Raherinantenaina F, Rakoto-Ratsimba HN, Rajaonanahary TM. Management of extremity arterial pseudoaneurysms associated with osteochondromas. Vascular 2016; 24(6): 628–637. [DOI] [PubMed] [Google Scholar]
- 14. Woertler K, Lindner N, Gosheger G, et al. Osteochondroma: MR imaging of tumor-related complications. Eur Radiol 2000; 10(5): 832–840. [DOI] [PubMed] [Google Scholar]