Abstract
Background:
Malaria contributes significantly to under-5 morbidity and mortality in Sub-Saharan African countries including Nigeria. The rollback malaria (RBM) initiative and millennium developmental goal 6 are the programs targeted at reduction in malaria burden. The target year here is 2015; it would be needful to determine the impact of these programs on lives of at-risk population.
Objectives:
To determine caregivers’ perception and utilization of insecticide-treated mosquito net (ITN) for their children/wards under 5 years of age.
Methods:
It was a cross-sectional, descriptive, hospital-based study conducted at Federal Teaching Hospital, Abakaliki, between April 1, 2014, and October 31, 2014. A structured questionnaire was used to assess caregivers’ perception and utilization of ITN. Relevant information collected from the respondents included awareness of what ITN is and its use, ownership, source and utilization of ITN, and frequency of antimalaria use for febrile episodes. Data were analyzed using Statistical Package for the Social Sciences (SPSS) Windows Program (SPSS Inc., Chicago, IL, USA) version 20.0 while the level of statistical significance was set at P < 0.05.
Results:
A total of 410 caregivers were interviewed; 362 (88.3%) were mothers. Three-hundred and eighty-four (93.7%) participants knew that ITN prevents mosquito bite that cause malaria infection, 81.2% (333/410) have at least one ITN in their homes, but only 215 (52.4%) use the ITN every night. Caregivers who used ITN regularly used antimalaria for their under-5 quarterly (34.9%) and rarely (33.9%). A significant relationship existed among socioeconomic class, knowledge of ITN, source of knowledge of ITN, frequency of anti-malaria use, and utilization of ITN.
Conclusion:
The study observed that awareness and ownership of ITN are high among study participants, but its utilization was suboptimal compared to RBM target for 2010 (80.0%). Health education and free distribution of ITNs should be further strengthened particularly among mothers of childbearing age and younger children.
Keywords: Caregivers perception, insecticide-treated nets, malaria, utilization, des moustiquaires imprégnées d’insecticide (MII), les connaissances, l’utilisation, le paludisme, les OMD, LA GESTION AXÉE SUR LES RÉSULTATS
Résumé
Arriére-plan:
Le paludisme contribue de manière significative à sous-5 Taux de morbidité et de mortalité au Nigéria. Le programme Faire reculer le paludisme (RBM) et objectif de développement du millénaire 6 (OMD 6), ont été des programmes ciblés sur la lutte contre le paludisme fardeau. L’année cible 2015 est ici, il serait nécessaire de déterminer l’impact de ces programmes sur la vie des populations à risque.
Objectif:
évaluer les connaissances des intervenants en soins de santé et l’utilisation des MII pour leurs enfants/pupilles de <5 ans.
Méthodes:
Il s’agissait d’une étude basée sur l’hôpital descriptive effectuée dans FETHA entre avril et octobre 2014. Un questionnaire structuré a été utilisé pour évaluer les connaissances des intervenants en soins de santé et l’utilisation des MII. Critères utilisés comprenaient la conscience de ce que MII et son utilisation, la propriété, la source et l’utilisation des MII et de la fréquence de l’anti-malaria utiliser pour les épisodes fébriles. L’analyse a été effectuée à l’aide de SPSS version 20. Niveau de signification a été P < 0.05.
Résultats:
un total de 410 personnes soignantes ont été interviewés, 362 (88,3%) étaient des femmes. Trois cent quatre-vingt-quatre (93,7%) participants savaient qu’ITN empêche piqûre de moustique qui causent l’infection palustre, 81,2% (333/410) ont au moins une MII dans leurs foyers mais seulement 215 (52,4%) utilisent l’ITN chaque nuit. Les aidants naturels qui utilisaient régulièrement de MII utilisé contre la malaria pour leurs enfants de moins de cinq ans (34,9%) trimestriel et rarement (33,9%). Une relation significative existe entre la classe socio-économique, la connaissance de l’ITN, source de connaissance de l’ITN, la fréquence d’utilisation de lutte contre le paludisme et l’utilisation des MII.
Conclusion:
l’étude a observé que la sensibilisation et la propriété de l’ITN est élevée parmi les participants à l’étude, mais son utilisation est encore sous-optimale par rapport à faire reculer le paludisme Cible pour 2010 (80,0%).
INTRODUCTION
Malaria infection is caused by a protozoan (Plasmodiae). Malaria infection occurs when favorable environmental conditions of temperature, rainfall, and humidity are created for the female Anopheles mosquitoes, carrying the Plasmodium, to bite a susceptible host.[1] Malaria infection is endemic in Nigeria, with a prevalence of 919 per 10,000 of population; it remains one of the leading causes of morbidity and mortality.[2]
It accounts for seven out of ten outpatient visits in Nigerian hospitals as well as being responsible for about 20% and 30% of infant and under-5 mortality rate, respectively.[3]
The renewed Abuja, Nigeria, target for roll back malaria (RBM), a control program for malaria, targets 80.0% of children <5 years of age and pregnant women to use insecticide-treated mosquito nets (ITN) between 2006 and 2010.[4]
The millennium development goal 6 has a target of halting and beginning to reverse the incidence of malaria in 2015. These control programs are aimed at reducing the morbidity and mortality, resulting from malaria infections in at-risk groups (pregnant women and under-fives). The past decades have witnessed an increase in international funding for malaria control. This increased funding has led to an increase in accessing ITN in Sub-Saharan Africa.[5]
At the end of 2010, approximately 289 million ITNs were delivered to the Sub-Saharan African region; this is enough to take care of 76% of the 765 million persons at risk.[5]
ITN is currently one of the most cost-effective options for reducing malaria-related morbidity and mortality and has been reported to reduce malaria mortality by 17% in children <5 years of age.[6,7] The World Health Organization recommends the use of ITN and long-lasting ITNs for the prevention of malaria.[6]
The RBM program has brought about an increase in awareness of malaria preventive measures such as ITN use, indoor residual spraying, environmental sanitation, and use of window and door nettings. Hanson et al.,[8] in Tanzania, reported an increase in net ownership and usage from 44% to 65% and from 33% to 56%, respectively, between 2005 and 2007 after implementing malaria intervention programs. Kimbi et al.[9] observed that awareness of malaria was high in both rural (98.04%) and urban (98.97%) settings and subjects had good perception of ITN as a means of malaria prevention (99.0%). Baume and Marin[10] conducted a survey within some selected countries in Sub-Saharan Africa with Nigeria inclusive between 2000 and 2004; they reported that bed net use among children younger than 5 years within households with at least one-bed net ranged from 48% to 73%. Epidemiological surveys have shown significant differences between awareness, ownership, and usage of ITN.[9,11,12] Atieli et al.[11] in Uganda reported ownership rate of 71.0% as against usage of 56.3%. In Cameroun, Kimbi et al.[9] reported ownership rate of 47.0% and usage of 69.7%.
A Nigerian study by Edelu et al.[12] reported a high awareness rate of 80.0% but the utilization rate of ITN was markedly low (26.1%). Other studies in Nigeria reported rates of ITN usage as 53.0% and 49.8%, respectively.[13,14]
The most important determining factor of ITN usage is ownership. People who are aware of the benefits of using ITN and are willing to use it but cannot access it are not better than the ignorant ones. Various other factors also determine utilization of ITN. Nankinga et al.[15] carried out a study on the prevalence of ITN utilization among children seeking health care in a health center; they found a low prevalence rate of 34.2%. This prevalence rate was significantly influenced by source of the nets, formal employment by head of household, number of children <12 years of age, and sharing bed with parents. Iloh et al.[13] observed that the most common reason for nonuse of ITN was inconvenience of sleep. Other reasons for nonusage of ITN as documented by Edelu et al.[12] included having window and door nets while social class did not seem to influence the use of net in their study. Okafor and Odeyemi[16] observed a high ITN use rate in their study (61.8%), and it was significantly influenced by caregiver marital status and the number of children under 5 years of age in the household; however, educational level of caregiver and occupation of the head of the household were not significant determinants.
Sleeping regularly under ITNs has been shown to be the most effective, proven way to prevent malaria infection. Koudou et al.[17] reported a significant decrease in the mean Plasmodium falciparum rate over a year period when intervention using ITN was instituted among children aged 6–59 months. Osondu and Jerome[18] compared the effectiveness of ITN with the traditional bed nets; they observed that ITN was 62.8% more effective in reducing febrile episodes and 84.1% more effective in reducing marked levels of malaria parasitemia in the cohort that used it.
The study locale, Abakaliki, Ebonyi State, is a fairly new state capital in Nigeria with high indices of infant and under-five mortality, of which severe malaria is among the common causes. With availability of ITN nationwide,[19] similar studies have been conducted in different parts of Nigeria[12,13,14,16,18] to determine the impact of usage of ITN on childhood malaria. To the knowledge of the researchers, no study on ITN usage in children has been conducted in the whole state, hence the need to assess the impact through a pilot, hospital-based questionnaire-based study.
The objectives of the study were to determine caregivers’ perception and utilization of ITN for their children/wards under 5 years of age.
METHODS
The study was conducted in children outpatient clinic of the Federal Teaching Hospital Abakaliki (FETHA), Ebonyi State, Nigeria. It was a cross-sectional descriptive study carried out from 1st April to 31st October, 2014. Consecutive recruitment of caregivers was done in the clinic at presentation after informed written consent was obtained from them for the study. A structured interviewer-administered questionnaire was used to collect information from the caregivers. The questionnaire sought information such as sociodemographic, ITN ownership, source of ITN, its use, and reasons for nonusage and use of antimalaria.
The study sample size was determined by the formula for sample size appropriate for an infinite population (i.e., >10,000),[20] n = z2pq/d2:
where n = The sample size when the population is > 10,000
z = The standard normal deviate, usually set at 1.96 (which corresponds to 95% confidence interval)
p = The proportion in the target population estimated to have a particular characteristic.
=0.50 (assumed that 50% have and use ITN)
Q = 1 − P = 1 − 0.50 = 0.50
D = Degree of accuracy desired, which for this study is set at 0.05 (proportion of the sampling error tolerated)
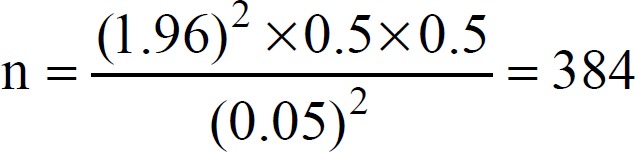
Attrition rate of 5% was added and the sample size was approximated to 410 caregivers.
Ethical approval was sought and obtained from the health and ethical management committee of the FETHA before the commencement of the study.
Socioeconomic classification of caregivers into upper, lower, and middle classes was determined by the criteria proposed by Oyedeji.[21]
Annual health education and health promotion were usually organized by a non- governmental organization (NGO), Maternal and Child Care Initiative (MCCI) organizing health talks and distributed free ITNs, Vitamin A, anti-helminthic, and soaps to health centers and local government areas (LGAs) in Ebonyi State, Southeast Nigeria (study locale), between 2007 and 2014.
Data were analyzed using Statistical Package for the Social Sciences, (SPSS) Windows Program (SPSS Inc., Chicago, IL, USA) version 20.0. Chi-square test was used to compare the proportions with the level of statistical significance being set at P < 0.05.
RESULTS
A total of 410 caregivers of children <5 years were studied during the 7 month study period, out of which 362 were females (88.3%). The age range of caregivers was 16–47 years, with a mean age of 30.03 ± 5.6 years.
Knowledge that ITN can prevent mosquito bites that cause malaria was high in this study (93.6%). A total of 333 (81.2%) of the subjects owned at least one ITN in their homes. A significant relationship was observed between knowledge of ITN and its ownership thereof as shown in Table 1.
Table 1.
Insecticide-treated net ownership versus knowledge of insecticide-treated net
| Ownership of ITN | Knowledge of ITN | Total, n (%) | |
|---|---|---|---|
| Prevent mosquito bites, n (%) | Do not know, n (%) | ||
| Yes | 329 (80.2) | 4 (0.97) | 333 (81.2) |
| No | 55 (13.4) | 22 (5.4) | 77 (18.8) |
| Total | 384 (93.6) | 26 (6.4) | 410 (100.0) |
χ2=78.88, df=1, P=0.000. ITN=Insecticide-treated net
Majority of the caregivers were of the lower social class (43.4%), while those who belonged to the middle and upper classes were 42.0% and 14.6% of the study population, respectively. A total of 215 (52.4%) of the caregivers that presented to the children outpatient clinic during the study period used ITN for their children <5 years of age every night, 28.0% (115) use ITN sometimes, while 19.5% (80) of subjects never used ITN for their children less 5 years of age. Majority of the caregivers were married (98.3%). The health center was the major source of information about ITN for regular users of ITN (50.2%). Of the 333 caregivers who owned ITN, 302 (90.7%) were obtained free of charge from LGA secretariats and health centers as shown in Table 2.
Table 2.
Factors influencing the use of insecticide-treated net
| Determining factors | Utilization of insecticide-treated mosquito nets | Statistical indices (χ2, df, P) | ||
|---|---|---|---|---|
| Every night (n=215) | Sometimes (n=115) | Never (n=80) | ||
| Knowledge of ITN | ||||
| Yes | 213 | 105 | 65 | 34.30, 2, 0.000 |
| No | 2 | 10 | 15 | |
| Source of information | ||||
| H/center | 108 | 48 | 31 | 39.40, 10, 0.000 |
| Media | 28 | 21 | 9 | |
| Friends | 6 | 7 | 10 | |
| Others | 63 | 29 | 15 | |
| Not aware | 1 | 10 | 15 | |
| Source of ITN | ||||
| H/center | 124 | 72 | 2 | 124.86, 8, 0.000 |
| LGA | 69 | 34 | 1 | |
| Market | 19 | 6 | 0 | |
| Others | 3 | 3 | 0 | |
| No ITN | 0 | 0 | 77 | |
| Marital status of caregivers | ||||
| Married | 213 | 113 | 77 | 5.34, 4, 0.234 |
| Single | 1 | 2 | 3 | |
| Divorced | 1 | 0 | 0 | |
| Social class | ||||
| Upper | 41 | 10 | 9 | 10.92, 4, 0.027 |
| Middle | 94 | 45 | 33 | |
| Lower | 80 | 60 | 38 | |
| Number of children | ||||
| <4 | 164 | 91 | 39 | 6.21, 6, 0.400 |
| 4–5 | 41 | 16 | 33 | |
| >5 | 10 | 8 | 8 | |
ITN=Insecticide-treated net, LGA=Local government area
A total of 294 (71.7%) caregivers interviewed in this study had three children and below who were <12 years of age. Utilization of ITN was influenced by knowledge of ITN being able to prevent mosquito bites (P = 0.000), source of the knowledge (P = 0.000), source of ITN (P = 0.000), and social class of caregivers (0.027) while marital status of caregivers (0.234) and the number of children in the households <12 years of age did not influence ITN use (0.400) as shown in Table 2.
Reasons why caregivers never used ITN or used it sometimes are seen in Table 3. ITN causing heat was the major reason reported by caregivers (13.7%). A total of 46 (11.2%) caregivers blamed their nonusage of ITN to not being able to access it. Other reasons for nonusage included that ITN causes rash (9.0%), inconveniences sleep (4.6%), and having window/door nets (7.8%). Five respondents (1.2%) did not have any reason for nonusage of ITN as shown in Table 3.
Table 3.
Reasons obtained from caregivers for not using insecticide-treated net for their under fives
| Reasons for ITN nonusage | Utilization of ITN | Total | ||
|---|---|---|---|---|
| Every night | Sometimes | Never | ||
| Not applicable | 215 (52.4) | 0 (0.0) | 0 (0.0) | 215 (52.4) |
| Causes rash | 0 (0.0) | 28 (6.8) | 9 (2.2) | 37 (9.0) |
| Inconvenience sleep | 0 (0.0) | 10 (2.4) | 9 (2.2) | 19 (4.6) |
| Have window/door nets | 0 (0.0) | 21 (5.1) | 11 (2.7) | 32 (7.8) |
| Causes heat | 0 (0.0) | 54 (13.2) | 2 (0.5) | 56 (13.7) |
| Do not have ITN | 0 (0.0) | 0 (0.0) | 46 (11.2) | 46 (11.2) |
| No reason | 0 (0.0) | 2 (0.5) | 3 (0.7) | 5 (1.2) |
| Total | 215 (52.4) | 115 (28.0) | 80 (19.5) | 410 (100.0) |
χ2=176.49, df=10, P=0.000. ITN=Insecticide-treated net
Comparison of antimalaria use with ITN utilization is represented in Table 4. Majority of those who had monthly need for antimalarial (50.0%) never used ITN.
Table 4.
Comparison of insecticide-treated net utilization with the frequency of anti-malaria use
| Frequency of anti-malaria use | Utilization of ITN | Total, n (%) | ||
|---|---|---|---|---|
| Every night, n (%) | Sometimes, n (%) | Never, n (%) | ||
| Monthly | 27 (12.5) | 55 (47.8) | 40 (50.0) | 122 (29.8) |
| Bi-monthly | 40 (18.6) | 26 (22.6) | 14 (17.5) | 80 (19.5) |
| Quarterly | 75 (34.9) | 22 (19.1) | 17 (20.3) | 114 (27.8) |
| Rarely | 73 (33.9) | 12 (10.4) | 9 (11.3) | 94 (22.9) |
| Total | 215 (52.4) | 115 (28.0) | 80 (19.5) | 410 (100.0) |
χ2=78.04, df=6, P=0.000. ITN=Insecticide-treated net
The least number of subjects requiring monthly antimalarial used ITN every night (12.5%) as shown in Table 4. Further, Table 4 shows that those subjects whose caregivers used ITN for them every night made use of antimalarial quarterly (34.9%) and rarely (33.9%). A significant relationship existed between antimalaria use and utilization of ITN (P = 0.000).
DISCUSSION
The awareness of ITN is able to prevent mosquito bites that cause malaria is high among the participants (93.6%) in the current study. This is comparable to that obtained in Cameroun by Kimbi et al.[9] (99.0%) but higher than findings by Edelu et al.,[12] 5 years ago (80.0%) in Enugu, Southeast Nigeria. This may be explained by the sustained health education and health promotion by a NGO, MCCI that organized health talks and distributed free ITNs, Vitamin A, anti-helminthic, and soaps to health centers and LGA secretariats in the Ebonyi State (study locale) between 2007 and 2014 predating the current study.
Similarly, ownership of ITN is also high (81.2%), reason being that majority of the subjects obtained their ITN from health centers and LGA secretariats (90.7%) free of charge. This is higher than that reported by Atieli et al.[11] (71.0%) and Kimbi et al.[9] (47.0%).
Regular ITN utilization for children <5 years of age in this study was 52.4%. This is far lower than the RBM target of 2010 which is 80.0% usage of ITN for children <5 years of age, but is comparable to ITN usage rate reported by Iloh et al.[13] in Southeast Nigeria (53.0%), and lower than that observed by Okafor and Odeyemi[16] in Lagos, Southwest Nigeria (61.8%). This difference in ITN usage rate may be explained by high literacy level and social class of their study participants when compared to the respondents in the current study. Lower ITN usage was reported by Auta[14] (49.8%), Nankinga et al.[15] (34.2%), and Edelu et al.[12] (26.1%) working differently.
ITN ownership in this study did not translate to its usage. This has been corroborated by several other researchers working differently.[12,14,15] Hence, there is need to implement the hang up and keep up campaign strategies, where health workers visit homes of people who had received ITN to ensure proper usage. This also provides opportunities for health education on the importance and benefits of ITN and helps to demonstrate the proper net usage.
Utilization of ITN in this study was significantly influenced by socioeconomic class, knowledge of ITN, source of knowledge of ITN, and source of ITN. This is consistent with the findings by Nankinga et al.,[15] who observed that source of net and social class of caregiver were significant determinants to ITN usage. However, other workers did not observe any significant influence of socioeconomic class on ITN use.[12,16]
The number of children <12 years of age, households, and marital status of caregivers were significant determinants to ITN use in studies by Nankinga et al.[15] and Okafor and Odeyemi.[16] These however did not influence the ITN use in the current study. The most common reason for nonuse of ITN in the present study was that it causes heat (13.7%). Previous workers observed inconvenience to sleep as a major reason for nonusage.[12,13] Other reasons for nonuse of ITN in this study were possession of window and door nets as has been previously reported in a similar study in Enugu, Nigeria.[12]
Effectiveness of ITN in malaria prevention was also observed in this study. The least number of caregivers requiring antimalarial monthly for febrile episodes for their under-fives was observed among regular users of ITN. A significant relationship was observed between ITN usage and frequency of antimalaria for febrile episodes. This was comparable to the study by Koudou et al.,[17] who reported a significant decrease in the mean P. falciparum rate with use of ITN, and Osondu and Jerome,[18] who reported that ITN was 62.8% more effective in reducing febrile episodes compared to ordinary nets.
CONCLUSION
The knowledge and ownership of ITN in the current study are high; however, regular ITN usage rate was observed to be low.
Strategies to improve utilization should be put in place so that the gains of improved access to ITN will be matched with an attendant outcome of malaria prevention through regular usage to save lives.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ogala WN. Malaria. In: Azubuike JC, Nkanginieme KEO, editors. Paediatrics and Child Health in a Tropical Region. 2nd ed. Owerri, Nigeria: African Educational Services; 2007. pp. 596–603. [Google Scholar]
- 2.Abebe E, Mosanya ME, Amajoh C, Otsemobor O, Ezedinachi EN, Afolabi BM, et al. Nigeria Roll Back Malaria Consultative Mission: Essential Actions to Support the Attainment of the Abuja Targets. 2003. [Last accessed on 2018 Jul 12]. Available from: http://www.rollbackmalaria.org/partnership/country/docs/WAfrica/reaping nigeria.pdf .
- 3.Federal Ministry of Health (FMOH). National Antimalarial Treatment Policy. Abuja, Nigeria: Malaria and Vector Control Division, FMOH; 2005. pp. 1–66. [Google Scholar]
- 4.WHO. World Malaria Report 2010. Geneva, Switzerland: World Health Organization; 2010. [Last accessed on 2018 Jul 24]. Available from: http://wwwwho.int/iris/handle/10885/44451 . [Google Scholar]
- 5.Roll Back Malaria, Global Strategic Plan: Roll Back Malaria, 2005-2015. Roll Back Malaria Partnership. Geneva, Switzerland: WHO; 2005. [Last accessed on 2018 Jul 04]. Available from: http://www.cdbh.org . [Google Scholar]
- 6.World Health Organization. Insecticide Treated Mosquito Nets. WHO Position Statement. Geneva: World Health Organization; 2008. [Last accessed on 2018 Jul 07]. Available from: http://www.ivcc.com . [Google Scholar]
- 7.Lengeler C. insecticide – treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004;2:CD 000363. doi: 10.1002/14651858.CD000363.pub2. DOI: 10.1002/14651858. CD 000363. Pub 2. [DOI] [PubMed] [Google Scholar]
- 8.Hanson K, Marchant T, Nathan R, Mponda H, Jones C, Bruce J, et al. Household ownership and use of insecticide treated nets among target groups after implementation of a national voucher programme in the United Republic of Tanzania: Plausibility study using three annual cross sectional household surveys. BMJ. 2009;339:b2434. doi: 10.1136/bmj.b2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kimbi HK, Nkesa SB, Ndamukong-Nyanga JL, Sumbele IU, Atashili J, Atanga MB, et al. Socio-demographic factors influencing the ownership and utilization of insecticide-treated bed nets among malaria vulnerable groups in the Buea Health District, Cameroon. BMC Res Notes. 2014;7:624. doi: 10.1186/1756-0500-7-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baume CA, Marin MC. Intra-household mosquito net use in Ethiopia, Ghana, Mali, Nigeria, Senegal, and Zambia: Are nets being used. Who in the household uses them? Am J Trop Med Hyg. 2007;77:963–71. [PubMed] [Google Scholar]
- 11.Atieli HE, Zhou G, Afrane Y, Lee MC, Mwanzo I, Githeko AK, et al. Insecticide-treated net (ITN) ownership, usage, and malaria transmission in the highlands of Western Kenya. Parasit Vectors. 2011;4:113. doi: 10.1186/1756-3305-4-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edelu BO, Ikefuna AN, Emodi JI, Adimora GN. Awareness and use of insecticide-treated bed nets among children attending outpatient clinic at UNTH, Enugu – The need for an effective mobilization process. Afr Health Sci. 2010;10:117–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Iloh GU, Amadi AN, Obiukwu CE, Njoku PU, Ofoedu JN, Okafor GO, et al. Family biosocial variables influencing the use of insecticide treated nets for children in Eastern Nigeria. J Family Community Med. 2013;20:12–9. doi: 10.4103/2230-8229.108178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Auta A. Demographic factors associated with insecticide treated net use among Nigerian women and children. N Am J Med Sci. 2012;4:40–4. doi: 10.4103/1947-2714.92903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nankinga Z, Muliira JK, Kalyango J, Nankabirwa J, Kiwuwa S, Njama-Meya D, et al. Factors associated with utilization of insecticide-treated nets in children seeking health care at a Ugandan hospital: Perspective of child caregivers. J Community Health. 2012;37:1006–14. doi: 10.1007/s10900-012-9546-z. [DOI] [PubMed] [Google Scholar]
- 16.Okafor IP, Odeyemi KA. Use of insecticide-treated mosquito nets for children under five years in an urban area of Lagos state, Nigeria. Niger J Clin Pract. 2012;15:220–3. doi: 10.4103/1119-3077.97325. [DOI] [PubMed] [Google Scholar]
- 17.Koudou BG, Ghattas H, Essé C, Nsanzabana C, Rohner F, Utzinger J, et al. The use of insecticide-treated nets for reducing malaria morbidity among children aged 6-59 months, in an area of high malaria transmission in Central Côte d’Ivoire. Parasit Vectors. 2010;3:91. doi: 10.1186/1756-3305-3-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Osondu NB, Jerome OO. Effectiveness of insecticide treated bed nets (ITN) in malaria prevention among children aged 6 months to 5 years in a rural community in Imo state, Nigeria. Int J Trop Med. 2009;4:41–9. [Google Scholar]
- 19.National Population Commission (NPC) [Nigeria] and ICF International 2014 Nigeria Demographic and Health Survey 2013. Abuja, Nigeria and Rockville, Maryland, USA: NPC and ICF International. 2013. [Last accessed on 2018 Jul 16]. Available from: http://www.dhsprogram.com .
- 20.Araoye MO. research methodology with statistics for health and social sciences. Ilorin: Nathadox Publishers; 2004. Sample size determination; pp. 115–22. [Google Scholar]
- 21.Oyedeji GA. Socio-economic and cultural background of hospitalized children in Ilesha. Niger J Paediatr. 1985;12:111–17. [Google Scholar]


