Sir,
Once the diagnosis of primary hyperparathyroidism (PHPT) has been established, localization of the abnormal gland becomes a priority. Sestamibi (MIBI) scintigraphy combined with the single photon emission computed tomography (SPECT) is the initial test of choice in all cases, as it is the best test to screen both the cervical and mediastinal lesions and has the highest positive predictive value of the available imaging techniques.[1] Additional imaging modalities that have also been used successfully include ultrasound (US), 4D-CT, and 11C-methionine PET-CT.[2] US is highly sensitive in experienced hands and is inexpensive, non-invasive, and reproducible in the operating room. However, the accuracy of US is operator dependent, and needs a skillful eye to pick up small adenomas, “hidden adenomas,” and intra-thyroidal lesions. US combined with MIBI offers the best sensitivity (up to 95%) and positive predictive value in localization of the abnormal gland.[3] Doubtful lesions and intra-thyroidal lesions can be assessed with needle aspirate parathyroid hormone (PTH) which can accurately localize an intra-thyroidal parathyroid adenoma.[4]
We have been performing MIBI and US in all our patients with PHPT in our institution from 2015 till date. We have a single person reading all the MIBI scans (author, Sunil HV) and one operator performing the US (author, Subramanian Kannan). US was performed using a 8–12 Hz probe of a Samsung sono-ACER3 machine. A Dual-Phase 99mTc-Sestamibi protocol with early (10–30 min after injection) and delayed (1.5–2.5 h after injection) high-count images of neck and thorax were obtained after intravenous injection of 15–20 mCi of 99mTc-Sestamibi. Delayed SPECT computed tomography (SPECT CT) images were also acquired on most occasions to aid better localization. We retrospectively reviewed our records of patients who had undergone surgery for PHPT from January 2015 to August 2018 to study our cases in which MIBI was negative.
We had 38 patients with PHPT who were operated 2015 onwards. MIBI and US was done in all patients except three patients (two of them had pancreatitis during pregnancy and one presented with neck mass on the CAT scan) who only underwent US. The mean age of the cohort was 49 ± 15 years with 22 females. All patients (100%) had a positive localization in the US, and 28 patients (74%) were positive on the MIBI. Among those with MIBI negative (10 patients), US localized the abnormal gland in all the cases, among whom two patients had multi-gland adenomas, three had intra-thyroidal adenomas [Table 1]. One patient (AAM) with a left-sided intra-thyroidal adenoma had a positive needle tip PTH >20000 and underwent left hemithyroidectomy. One patient (R) with bilateral thyroid nodules with Bethesda 3 on cytological assessment had cellblock stained positive for PTH and underwent total thyroidectomy. In another patient (S) who had multiple small (4–6 mm) intra-thyroidal lesions, US could not localize which of these thyroid nodules corresponded to the parathyroid adenoma. However, US gave a guiding plan on “what to do next” when the intro-operative PTH (IOPTH) did not drop below 80% of the baseline value. All our patients have been rendered eucalcemic on follow up at 6 months. One patient (S) (who underwent total thyroidectomy) developed permanent hypoparathyroidism.
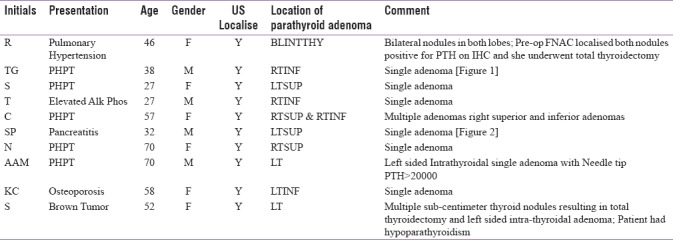
Table 1.
Clinical summary of MIBI-negative patients
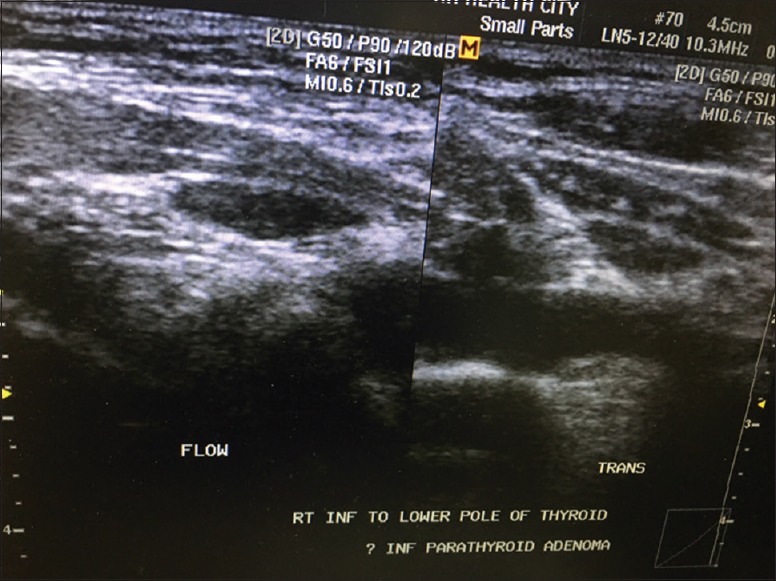
In our institution, US helped localizing parathyroid adenomas in all our MIBI-negative patients. While there are multiple options of imaging in patients with PHPT who are MIBI negative, we feel US is an important, non-invasive imaging step in PHPT. Unlike the nuclear imaging or cross-sectional imaging which give a binary localizing result as adenoma present or absent, the US report by a dedicated sonologist can give a map of the suspected lesions present within the thyroid gland and outside the thyroid gland [Figure 3]. In order of likely possibility of parathyroid adenoma, the sonologist can give the surgeon an exploratory plan for localizing the diseased gland. This helps with the operative plan if the IOPTH did not drop as expected. Our approach of using MIBI + US + IOPTH in all the patients with PHPT during parathyroid exploration provides a balanced approach between focal gland exploration which may miss multi-gland disease and avoid routine 4-gland exploration which has a risk of permanent hypoparathyroidism.
Figure 3.
Ultrasound appearance of intra-thyroidal parathyroid adenoma
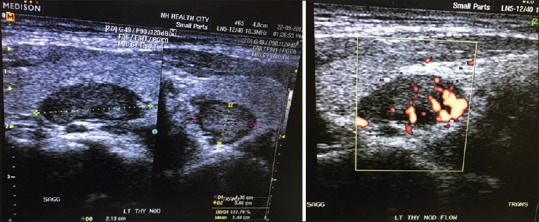
Figure 1.
Ultrasound appearance of parathyroid adenomas in MIBI-negative patients
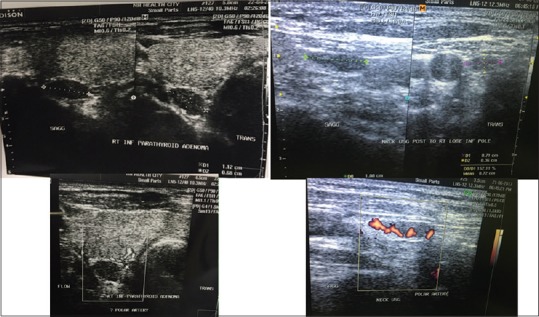
Figure 2.
Ultrasound appearance on patient who was pregnant and presented with pancreatitis and was diagnosed with primary hyperparathyroidism
Dedicated sonologist with experience in parathyroid imaging can effectively localize the abnormal gland in all MIBI-negative cases and in most cases chart a road map for the surgeon intra-operatively. All patients with PHPT should have a neck US by a dedicated sonologist before surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Presentation at a meeting:
Organisation: Submitted as abstract to Foundation of Head & Neck Surgical Oncology & Indian Society of Bone and Mineral Research Society
Place: Kolkatta & Delhi
Date: Nov 2018 & Sep 2018
REFERENCES
- 1.Lew JI, Solorzano CC. Surgical management of primary hyperparathyroidism: State of the art. Surg Clin North Am. 2009;89:1205. doi: 10.1016/j.suc.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 2.Mihai R, Simon D, Hellman P. Imaging for primary hyperparathyroidism-an evidence-based analysis. Langenbecks Arch Surg. 2009;394:765. doi: 10.1007/s00423-009-0534-4. [DOI] [PubMed] [Google Scholar]
- 3.Haber RS, Kim CK, Inabnet WB. Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: Comparison with (99m) technetium sestamibi scintigraphy. Clin Endocrinol (Oxf) 2002;57:241. doi: 10.1046/j.1365-2265.2002.01583.x. [DOI] [PubMed] [Google Scholar]
- 4.Dutta D, Selvan C, Kumar M, Datta S, Das RN, Ghosh S, et al. Needle aspirate PTH in diagnosis of primary hyperparathyroidism due to intrathyroidal parathyroid cyst. Endocrinol Diabetes Metab Case Rep 2013. 2013:130019. doi: 10.1530/EDM-13-0019. [DOI] [PMC free article] [PubMed] [Google Scholar]


