Abstract
From its earliest days, Buddhism has been closely intertwined with the practice of medicine, both being concerned in their own way in the alleviation and prevention of human suffering. However, while the connection between Buddhism and healthcare has long been noted, there is scarce literature on how Buddhist philosophy can guide health-care practitioners in their professional as well as personal lives. In the sutras, we find analogies that describe the Buddha as a doctor, knowledge of Dharma as the treatment, and all lay people as patients. The occurrence of disease is closely related to one's mental, physical and spiritual health, society, culture, and environment. It is not enough to approach medicine in a manner that simply eradicates symptoms; the psychosocial aspects of disease and its mind based causes and remedies must be a primary consideration. Holistic care involves harmonization of all these elements, and the Buddhist philosophy offers great insight for the physician. The Buddhist medical literature lays out moral guidelines and ethics for a health-care practitioner and this has corollaries in the principles of medical ethics: nonmaleficence, benevolence, justice, and autonomy. There is emphasis on loving-kindness, compassion, empathy, and equanimity as key attributes of an ideal physician. The practice of medicine is a stressful profession with physician burnout an often neglected problem. Mindfulness meditation, as developed in Buddhism, can help health-care professionals cope up with the stress and develop the essential attributes to improve patient care and self-care. This article outlines the spiritual and ethical values which underlie Buddhist concern for the sick and gives an overview of lessons which health-care practitioners can imbibe from Buddhism.
Keywords: Buddhism, equanimity, health-care practitioner, holistic care, loving kindness, medical ethics, mindfulness meditation, mindfulness-based stress reduction, physician burnout, physician's vows, self-compassion
INTRODUCTION
In Buddhist tradition, the first and primordial healer was the Buddha himself. In his first sermon at Sarnath, Gautam Buddha elucidated the Four Noble Truths – there is suffering (dukkha), the cause of suffering is clinging and ignorance (dukkha samudaya), it is possible to overcome suffering (dukkha nirodha) and the way to do so is the practice of the Eightfold Noble Path (dukkha nirodha marga).
“And what have I taught? This is stress. This is the origination of stress. This is the cessation of stress. This is the path of practice leading to the cessation of stress”[1]
“Both formerly and now, it is only stress that I describe, and the cessation of stress.”[2]
The Buddha's Four Noble Truths are a path toward healing, for in them lies the recognition of disease, its etiology, its prognosis, and the remedy. These four components form the very basis of any physician's practice. The Dictionary of Medical Ethics points out that “The principles governing Buddhism and the practice of medicine have much in common.”[3] Both focus on the alleviation and prevention of suffering.
Buddha has often referred to medicine as the most suitable analogy for the Noble Truths:
Know the sickness, Abandon the cause of the sickness, Aspire the cure and Rely upon the medical treatment.
In the same way one should:
Know the suffering, Abandon the cause, Obtain the cessation And follow the Path.
Indeed Buddha was considered a great physician and psychotherapist due to his compassion and wisdom to diagnose and treat the root cause of all mental and physical malaise.[4] His teachings can be considered a course of therapy and Buddhist meditation techniques have been abundantly utilized in modern-day psychotherapy for several mental and other chronic illnesses.[5] R L Soni writes “It is indeed a matter of supreme interest that the noble profession of medicine and the corpus of thought known as Buddhism are both concerned in their own way in the alleviation, control and ultimately the removal of human sufferings.”[6]
The health-care practitioner has a lot to learn from Buddha's teachings and the practice of Buddhist precepts, which would aid him/her in not only fulfilling their role as a physician but also in living wholesome lives.
The medicine buddha/Bhaisajyaguru
The Medicine Buddha, Bhaisajyaguru, Yakushi Nyora, i or the Buddha of Healing is described in Mahayana Buddhist texts and usually represented seated with his right hand raised in vadra mudra (the hand and finger gesture symbolizing giving and compassion), and the left hand rested on his lap, holding a jar of medicine. In illustrations, he is shown surrounded by various healing plants and innumerable sages, depicted as the Paradise of the Medicine Buddha that represents an idealized universe where remedies exist for every ailment, something that modern medical research is ever striving to attain.
The Medicine Buddha is described as a healer who cures suffering and disease, both physical and mental. The Sutra of the Medicine Buddha is a common sutra to recite in Eastern Buddhist temples and monasteries.[7] He is believed to have revealed the teachings which constitute the Four Medical Tantras of Buddhist medical literature. The Four Medical Tantras have elaborated on the cause, nature and signs of various ailments, the methods of healing and medicines, and precise explanations on medical ethics, delineating the qualities of a physician.
The health-care practitioner in Buddhism
The doctors, nurses, and others involved in care of the sick are held in high esteem in Buddhist cultures. The doctor is referred to as bhisakka, vejja, or tikicchaka. The Buddha saw the physician's role as a vital one. The Buddha said:
“Those who tend the sick are of great benefit (to others).”[8]
“Nursing the sick was much praised by the Great Compassionate One and is it a wonder that he would do so? For the Sage sees the welfare of others as his own and thus that he should act as a benefactor is no surprise. This is why attending to the sick has been praised by the Buddha. One practicing great virtue should have loving concern for others”.[9]
For over 2000 years, Buddhism has had a close involvement in the treatment of the sick and was instrumental in institutionalization of medicine in the East. The Pali Canon is replete with information about sickness and health, healing, medicine, medical care, and medical ethics. Practice of medicine was included as a scholastic discipline in the monasteries. Monasteries often served as hospices and infirmaries.
The three jewels: The physician as a guide
In Buddhism, an individual takes refuge in the Three Jewels– the Buddha (the spiritual guide), the Dharma (the practice), and the Sangha (the community). The role of the physician and spiritual guide are considered very similar. The one who guides individuals in overcoming negative states of the mind and develop positive potential is regarded as a Spiritual Master, and the one who takes care of the individual by giving them medical treatment to overcome their physical and mental ailments and stay healthy is referred to as a physician or medical doctor. The aim of both is to free individuals from their suffering.
The analogy given is that of a patient relying upon the right treatment.[10] It is said:
Take refuge in the Three Jewels, See Buddha as the most qualified physician, See the Dharma as a faultless medicine And the Sangha as medical attendants.
Just as one should be careful in seeking spiritual guidance from someone with true knowledge (the spiritual guide), in the field of medicine, it is crucial that the patient should not rely on quack practitioners but seek guidance from those adequately qualified (the healthcare practitioner). Moreover, it is the responsibility of the physician to be well-informed so that he/she can make the right decisions and also to take assistance from the Sangha. The Sangha in medical community would include other individuals involved in the care of the patient including other specialists, diet counselors and patient educators, psychologists, pharmacists, family members and friends, pharmaceutical companies, research groups and the civic society, institutions and government.
Buddha considered it a good practice to resolve conflicts or differences in ideas by discussion within the Sangha. To date, Buddhist monastic communities conduct their business and resolve disagreements by a majority vote. Similarly, medical community has sought the coming together of ideas and sharing of experiences with consensus meetings among experts and formulation of practice guidelines.
Holistic, patient-centered care, and the five great sciences
Within the Buddhist worldview, health and disease involve the overall state of a human being and are interwoven with many nonmedical factors, such as economics, education, social and cultural milieu, and ethics or morality. All of these conditional factors need to be seriously taken into account in the understanding of health and disease. Health is, therefore, to be understood in its wholeness. It is the expression of harmony-within oneself, in one's social relationships, and in relation to the natural environment.[11] To be concerned about a person's health means to be concerned with the whole person: his or her physical, mental, and moral dimensions; social, familial, and work relationships; as well as the environment in which the person lives. Thus, the work of a physician is of a complete wholesome nature.
A Bodhisattva is someone who is driven by great compassion and is determined to attain enlightenment for the sake of all sentient beings. The central point of the teaching is not the Buddha or any divine being or philosophical entity, but sentient beings. Similarly, for a physician, the central point of attention and care is the patient. Everything must be formulated around the patient: most guidelines emphasize the need to move from a “paternalistic approach” in modern medicine to this “patient-oriented approach”. The Buddha taught that one must follow the Middle Path (madhyampratipada), avoiding extremes of indulgence and self-denial. The doctor–patient relationship too rests on seeking a middle ground between the physician's knowledge and the patient's perceptions and experiences. The physician must not only bear theoretical knowledge, but should be able to skillfully gather information about patient's health, should be capable of analyzing that information and share it with the patient, and engage in informed decision-making process to determine the course of therapy.
It is described that a Boddhisattva must master the Five Great Sciences:
The science of art
The science of medicine
The science of language
The science of logic
The inner science of mental training.
The same would be true for those involved in healthcare-the physician must master the science and the art of medicine, the art of communication, the ability to analyze and use logic, and also developmental training.[12,13]
The six perfections/Paramitas and the four Immeasurables/Brahmaviharas
A health-care practitioner shoulders great responsibility and he/she needs to develop and inculcate several characteristics to be able to deliver their duties. Fulfilling the task of a perfect physician requires the practice of the Six Perfections/Paramitas and the four immeasurables/Brahmaviharas [Table 1].
Table 1.
The key attributes of a physician-the six perfections and the four immeasurables
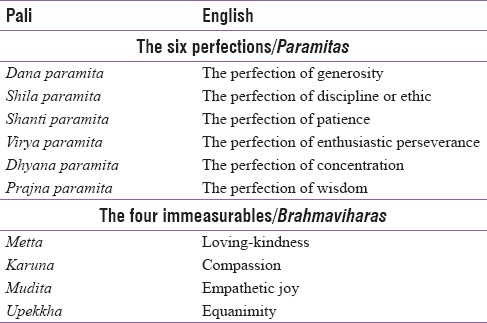
Health-care practitioners need to exhibit sincere compassion and generosity (Dana Paramita) toward the patient and not be limited in their approach by material benefits in the form of wealth, fame, or position. Altruism or selfless concern for the well-being of others is of utmost importance in healthcare, and it is an opportunity to experience our interconnectedness to other beings and become aware of our own mortality. The diligent health-care professional, who works selflessly for the health of persons seeking her/his guidance, can accumulate good karma as well. Greed, hatred, and delusion have been described as the “Three Bitter Poisons” by Buddha and the physician should avoid these. The basic Buddhists tenets can take a physician from a confused, ignorant, and deluded state to a state of great compassion, wisdom, and love.
The Shila Paramita is encompassed in the Noble Eightfold Path [Table 2]. The Buddha taught:
Table 2.
The noble eightfold path for a healthcare practitioner

“Now what, monks, is the Noble Eightfold Path? Right view, right resolve, right speech, right action, right livelihood, right effort, right mindfulness, right concentration.”[14]
The physician must endeavor to seek right theoretical knowledge, approach patients with right intent, communicate with right and kind speech (piya vaca) and manifest right conduct in choosing appropriate therapy, lifestyle modification, and medications.
The Buddha emphasized:
“Whatever words we utter should be chosen with care”.
“Better than a thousand hollow words, is one word that brings peace.”
He/she should refrain from unethical practice and strive toward right livelihood and right effort. Mindfulness at work and meditation aid the practitioner in stress management, prevent errors in judgment, and ensure the strengthening of a healthy doctor-patient relationship. A practitioner must exhibit patience (Shanti paramita), genuine interest, and enthusiasm (Virya paramita) and concentration (Dhyana paramita) and strive toward wisdom and up-to-date knowledge in medical field (Prajna paramita). The Buddha, during his last sermon before his parinirvana, rightly pointed out:
“Within the light of wisdom, destroy the darkness of ignorance.”
The four immeasurable abodes/Brahmaviharas, namely, loving-kindness (metta or maitri), compassion (karuna), empathetic joy (mudita), and equanimity (upekkha) are pivotal to the role of a health-care professional. Compassion is recognized as a vital trait for a healthcare professional and is defined in recent medical literature as the ability to understand another person's suffering, combined with a willingness to help and promote the well-being of that person.[15] The ability to feel the suffering of others and responding with warmth and compassion helps one mobilize the boundless power of healing. In the art of medicine, there is a constant need to strike a balance between the biomedical needs of the patient while respecting his/her psychosocial concerns. The practice of medicine is one of the most stressful professions and a significant proportion of practitioners suffer compassion fatigue and burnout. It is imperative that while one is focused inpatient care, a practitioner's circle of kindness, and compassion must include themselves.
Medical ethics and Buddhism
The Buddhist text Dhammapada (verse 183) guides the practitioner:
“Not to do any evil
To cultivate what is good
To purify one's mind
This is the teaching of the Buddhas.”
It is interesting to note that these moral principles described in ancient Buddhist literature are incorporated as the four basic moral principles described as biomedical ethics in modern medicine, namely, nonmaleficence, beneficence, justice, and autonomy.[16] The first and foremost teaching “not to do any evil” is the principle of nonmaleficence, which means to not be the cause of any harm. Primum nonnocere is indeed a key guiding principle for all health-care practitioners. The second principle of beneficence is reflected as “to cultivate what is good”. A practitioner should act in the best interest of the patient. The remaining two principles can be summed up as “to purify one's mind” and include respect for Autonomy, i.e., the patient has the right to refuse or choose treatment and Justice, i.e., fairness and equality in dealing with patients and in distribution of health-care resources.
Physician's vow/Vejjavatapada
The Vejjavatapada or Physician's Vow[13] is composed of verses attributed to the Buddha, from the Pali Canon, dating between 5th and 3rd centuries BC. It serves as an ethical commitment, undertaken by Buddhist doctors and others working with the sick. It is the equivalent of the Western Hippocratic Oath.
Rendered in English, this is translated as shown in Box 1. The seven vows in the Vejjavatapada are very relevant to the practice of medicine, and every physician should abide by them:
Box 1.
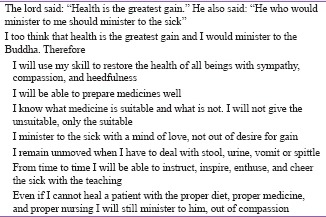
Buddhist physician's vow/Vejjavatapada
Care (hita), kindness (daya), and compassion (anukampa) in the healing process
Responsibility to be fully trained and skilled in his discipline
Not do any harm (ahimsa). Whatever benefits the patient truly should be pursued by all means and whatever is harmful must be avoided
Put the welfare of the patient above one's personal gain– benevolent attitude
It may be necessary to deal with loathsome aspects of human body and physician should do so with detachment and not humiliate or embarrass the patient. Detachment would also help the physician maintain their own mental balance in the face of bad outcomes
Providing counseling and comfort are crucial to healing process
Minister to patients even if they will probably die – terminal and palliative care.
Medical care must be extended to even those individuals who may be terminally ill. Buddha described three kinds of sick people – one who will recover whether or not he receives treatment, one who will not recover even with treatment, and ones who will recover only if they get proper treatment. All of them need to be attended to because there is a chance they may actually turn out to need and benefit from the care.[17]
Physician burnout and self-compassion
The medical profession is a high-stress profession, and physician burnout is a significant but often ignored issue. Burnout is characterized by physical, emotional, and mental fatigue and multiple studies have indicated a high prevalence of burnout among physicians, with almost one-third of them being affected at some point in their career.[18,19] In a recent study from the US, 45.8% physicians reported having at least one symptom of burnout.[20]
Prolonged exposure to stress may result in compassion fatigue with a loss of enthusiasm for work, feeling of helplessness and defeat, and the lack of a sense of personal achievement. This may lead to the physician becoming alienated or depersonalized, wherein the health-care provider may begin to treat patients indifferently, objectify them and develop a negative attitude toward the profession. It affects the quality of patient care, exerts a strain on the doctor–patient relationship and inter-personal relationship with colleagues as well. In addition, the tendency of most health-care professionals to give suboptimal attention to self-wellness is likely to affect their own health and personal life.[21] However, within the medical culture, very little emphasis is placed on clinician's well-being, and the impact of compassion fatigue and burnout overlooked.
As per Buddhist thought, responsible persons should themselves be in a harmonious state of body and mind, and the medical practitioner needs to remember this constantly. The Buddha said:
“You, yourself, as much as anybody in the entire universe, deserve your love and affection.”
Self-acceptance, self-kindness, and self-compassion have become a central focus of intervention in psychology practice. Self-compassion entails being warm toward one's own self when encountering pain and personal shortcomings, rather than ignoring them or hurting oneself with self-criticism. It also involves the recognition that suffering and personal failure is a part of the shared human experience. At the same time, Buddhist thought encourages the process of reflection on one's actions in an attempt to improve on them:
“A mirror is for reflection. A person should also reflect on their acts– whether physical, verbal or mental and assess whether they cause affliction to themselves or others. Repeated reflection is how you train yourself.”[22]
Role of Buddhist meditation practices for the physician
Mindfulness meditation is a technique of mental training that enables one to experience current reality in a nonjudgmental and nonreactive way and constitutes one of the most important meditation practices in Buddhism.[23] It is a self-directed practice for relaxing the body and calming the mind through focusing on present-moment awareness:
“Peace comes from within. Do not seek it without.”
“Those who are vigilant, who train their minds day and night and strive continually for nirvana, enter the state of peace beyond all selfish passions.”
“Hard it is to train the mind, which goes where it likes and does what it wants. But a trained mind brings health and happiness. The wise can direct their thoughts, subtle and elusive, wherever they choose: A trained mind brings health and happiness.”
Through mindfulness, unhelpful habitual thoughts and behaviors can be recognized, and new creative ways of responding to challenging situations developed. Mindfulness helps cultivate clear thinking, equanimity, compassion, and empathy – attributes that have been repeatedly stressed in Buddhist philosophy and necessary to cultivate for a healthcare provider.
“Our life is shaped by our mind; we become what we think. Joy follows a pure thought like a shadow that never leaves.”
“If you meditate earnestly, pure in mind and kind in deeds, leading a disciplined life in harmony with the dharma, you will grow in glory. If you meditate earnestly, through spiritual disciplines you can make an island for yourself that no flood can overwhelm.”
Of the various meditation techniques, mindfulness is particularly suitable for physician burnout. It is nonreligious, secular and has academic appeal and a solid scientific foundation. Mindfulness-based stress reduction (MBSR) is a well-researched and clinically useful program of psychotherapy widely recognized as a tool for stress reduction. MBSR has been used for management of chronic pain syndromes, depression, anxiety, substance abuse, sleep disorders, blood pressure, and diabetes management.[23]
Several small studies have reported that mindfulness-based interventions can help reduce work-related stress, improve compassion scores and reduce burnout among physicians, nurses, residents, and medical students.[24,25,26] Goodman and Schorling demonstrated significant improvements in the areas of emotional exhaustion, depersonalization, personal accomplishment, and mental well-being using formal mindfulness practices of walking meditation, sitting meditation, body scans, and mindfulness movement.[27] Others have reported reduction in psychological distress and improved quality of life with MBSR.[28,29,30] An 8-week mindfulness-based program was used in resilience training (RT) for health-care professionals with current depressive symptoms and demonstrated a 63%–70% reduction in depression, 48% reduction in stress, and 23% reduction in anxiety, with benefits persisting for up to 2 months after completion of the RT program.[31]
In a recent systematic review and meta-analysis[32] of meditative interventions among informal caregivers and health professionals, statistically significant improvements were reported in depression (effect size 0.49, 95% confidence interval [CI] 0.24–0.75), anxiety (effect size 0.53, 95% CI 0.06–0.99), stress (effect size 0.49, 95% CI 0.21–0.77), and self-efficacy (effect size 0.86, 95% CI 0.5–1.23) after 8 weeks of intervention. Another meta-analysis demonstrated that cognitive, behavioral, and mindfulness-based approaches are effective in reducing stress, anxiety, and burnout in medical students and practicing physicians.[33]
CONCLUSION
In this text, we have tried to present Buddhist teachings that can assist and guide the health-care practitioners in their work. The doctrine presented in this humble communication provides a spiritual and moral compass for our profession. Modern medical care needs to internalize age-old Buddhist philosophy and draw inspiration from Modern medical fraternity needs to internalize age-old Buddhist philosophy and draw inspiration from Buddhist values, in order to regain their internal self-esteem and their respect among society.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.SN 56.3 PTS: M i 426 Cula-Malunkyovada Sutta: The Shorter Instructions to Malunkya. Translated from the Pali by Bhikkhu T. 1998. [Last accessed on 2017 Dec 06]. Available from: https://www.accesstoinsight.org/tipitaka/mn/mn.063.than.html .
- 2.SN 22.86 PTS: S iii 116 CDB i 936 Anuradha Sutta: To Anuradha. Translated from the Pali by Bhikkhu T. 2004. [Last accessed on 2017 Dec 06]. Available from: https://www.accesstoinsight.org/tipitaka/sn/sn22/sn22.086.than .
- 3.Duncan AS, Dunstan GR, Welbourm RB. Dictionary of Medical Ethics. London: Darton, Longman and Todd; 1981. [Google Scholar]
- 4.Aich TK. Buddha philosophy and Western psychology. Indian J Psychiatry. 2013;55:S165–70. doi: 10.4103/0019-5545.105517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cullen M. Mindfulness-based interventions: An emerging phenomenon. Mindfulness. 2011;2:186–93. [Google Scholar]
- 6.Soni RL. Buddhism in relation to the profession of medicine. In: Millard DW, editor. Religion and Medicine. Vol. 3. London: SCM Press; 1976. pp. 135–51. [Google Scholar]
- 7.Thanh M, Leigh PD. Translated Under the Guidance of Dharma Master Hsuan Jung. Sutra of the Medicine Buddha. Buddhanet's Book Library. International Buddhist Monastic Institute. (2nd ed) 2001 [Google Scholar]
- 8.Bronkhorst J. Api Ca Gilanupatthaka Bahupakara, Vinaya I. Buddhism in the Shadow of Brahmanism: Handbook of Oriental Studies, South Asia. Asian Studies E-Books Online, Collection. 2011;24:303. Sec 2. [Google Scholar]
- 9.Morris R. Sadddhamopayana. Translated by Hazlewood AA, Saddhamopayana (The Gift-Offering of the True Dhamma) J Phys Ther Sci. 1887:35–98. [Google Scholar]
- 10.Bhikkhu T. Beyond Coping: V. Teaching by Example. Access to Insight Legacy Edition. 2013. Nov 30, Available from: http://www.accesstoinsight.org/lib/study/beyondcoping/examples.html .
- 11.Ratanakul P. Buddhism, health and disease. Eubios J Asian Int Bioeth. 2004;15:1620164. [Google Scholar]
- 12.Donden Y. Ithaca, New York: Snow Lion Publication; 1986. Health Through Balance – An Introduction to Tibetan Medicine. [Google Scholar]
- 13.Kenneth GZ. Studies in traditional Indian medicine in the Pali Canon: Jivaka and Ayurveda, Kenneth G. J Int Assoc Buddhist Stud. 1982;5:309–13. [Google Scholar]
- 14.SN 45.8 Tipitaka Samyutta Nikaya SN 45.8 PTS: S v 2 CDB ii 1524 Magga-Vibhanga Sutta: An Analysis of the Path. Translated from the Pali by Bhikkhu T. 1996. [Last accessed on 2017 Dec 06]. Available from: https://www.accesstoinsight.org/tipitaka/sn/sn45/sn45.008.than.html .
- 15.Perez-Bret E, Altisent R, Rocafort J. Definition of compassion in healthcare: A systematic literature review. Int J Palliat Nurs. 2016;22:599–606. doi: 10.12968/ijpn.2016.22.12.599. [DOI] [PubMed] [Google Scholar]
- 16.Gillon R. Medical ethics: Four principles plus attention to scope. Br Med J. 1994;309:184–188. doi: 10.1136/bmj.309.6948.184. Doi: 10.11336/bmj. 3096948.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.AN 3.22 PTS: A i 120 Gilana Sutta: Sick People. Translated from the Pali by Bhikkhu T. 1997. [Last accessed on 2017 Dec 06]. Available from: https://www.accesstoinsight.org/tipitaka/an/an03/an03.022.than.html .
- 18.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: A missing quality indicator. Lancet. 2009;374:1714–21. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 19.Romani M, Ashkar K. Burnout among physicians. Libyan J Med. 2014;9:23556. doi: 10.3402/ljm.v9.23556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 21.McKinlay JB, Marceau L. New wine in an old bottle: Does alienation provide an explanation of the origins of physician discontent? Int J Health Serv. 2011;41:301–35. doi: 10.2190/HS.41.2.g. [DOI] [PubMed] [Google Scholar]
- 22.Tipitaka Majjhima Nikaya MN 61 PTS: M i 414Ambalatthika-rahulovada Sutta: Instructions to Rahula at Mango Stone. Translated from the Pali by Bhikkhu T. Availabel from: https://www.accesstoinsight.org/tipitaka/mn/mn.061.than.html . [Google Scholar]
- 23.Zou T, Wu C, Fan X. The clinical value, principle, and basic practical technique of mindfulness intervention. Shanghai Arch Psychiatry. 2016;28:121–30. doi: 10.11919/j.issn.1002-0829.216060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bond AR, Mason HF, Lemaster CM, Shaw SE, Mullin CS, Holick EA, et al. Embodied health: The effects of a mind-body course for medical students. Med Educ Online. 2013;18:20699. doi: 10.3402/meo.v18i0.20699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thimmapuram J, Pargament R, Sibliss K, Grim R, Risques R, Toorens E, et al. Effect of heartfulness meditation on burnout, emotional wellness, and telomere length in health care professionals. J Community Hosp Intern Med Perspect. 2017;7:21–7. doi: 10.1080/20009666.2016.1270806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang SJ, Kwak EY, Hahm BJ, Seo SH, Lee da W, Jang SJ, et al. Effects of a meditation program on nurses’ power and quality of life. Nurs Sci Q. 2016;29:227–34. doi: 10.1177/0894318416647778. [DOI] [PubMed] [Google Scholar]
- 27.Goodman MJ, Schorling JB. A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med. 2012;43:119–28. doi: 10.2190/PM.43.2.b. [DOI] [PubMed] [Google Scholar]
- 28.Shanafelt TD. Enhancing meaning in work: A prescription for preventing physician burnout and promoting patient-centered care. JAMA. 2009;302:1338–40. doi: 10.1001/jama.2009.1385. [DOI] [PubMed] [Google Scholar]
- 29.Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness based stress reduction for health care professionals: Results from a randomized trial. Int J Stress Manag. 2005;12:164–76. [Google Scholar]
- 30.Martín-Asuero A, García-Banda G. The mindfulness-based stress reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. Span J Psychol. 2010;13:897–905. doi: 10.1017/s1138741600002547. [DOI] [PubMed] [Google Scholar]
- 31.Johnson JR, Emmons HC, Rivard RL, Griffin KH, Dusek JA. Resilience training: A Pilot study of a mindfulness-based program with depressed healthcare professionals. Explore (NY) 2015;11:433–44. doi: 10.1016/j.explore.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Dharmawardene M, Givens J, Wachholtz A, Makowski S, Tjia J. A systematic review and meta-analysis of meditative interventions for informal caregivers and health professionals. BMJ Support Palliat Care. 2016;6:160–9. doi: 10.1136/bmjspcare-2014-000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: A review and meta-analysis. J Nerv Ment Dis. 2014;202:353–9. doi: 10.1097/NMD.0000000000000130. [DOI] [PubMed] [Google Scholar]


