Abstract
Introduction:
Anaplastic thyroid cancers (ATCs) usually present in the sixth to seventh decades of life and little is known about the disease in young patients. The aim was to analyze the clinicopathological characteristics diagnosed with ATC in an iodine-deficient area.
Material and Methods:
The medical records of 100 patients diagnosed with ATC at a tertiary care hospital between 1991 and 2013 were reviewed.
Results:
The mean age of patient was 58 years. About 34 patients were ≤50 years. The common presentation was that of a rapidly growing fixed and hard mass (64%). Due to rapid expansion, 27% patients experienced severe pain. About one-third presented as sudden enlargement of pre-existing goiter over few weeks. The median duration of symptoms before diagnosis was 3 months. About 41% presented with lymph node enlargement and 31% with distant metastasis. The diagnosis was established with fine-needle aspiration or core biopsy. Histopathology was available in 32 patients and showed four major patterns: spindle cell (9), giant cell (7), epithelioid (5), squamoid (1), mixed type in 10 patients. Eight patients presenting with stridor required emergency tracheostomy for airway control. Total thyroidectomy with or without lymph node dissection was possible in 21 patients. Patients received radiotherapy with or without chemotherapy. Median overall survival was 3 months. Overall survival was significantly better in patients receiving some form of treatment.
Conclusion:
ATC in endemic goiter areas presents at an earlier age. One-third of ATC is due to anaplastic transformation of pre-existing goiter and majority of the patients refuse treatment due to dismal outcome.
Keywords: Anaplastic, carcinoma, thyroid
INTRODUCTION
Although <2% of all thyroid carcinomas are anaplastic thyroid cancer (ATCs), it account for 14%–39% of thyroid carcinoma deaths.[1,2] The incidence of ATC has decreased after the introduction of iodination of salt,[3,4] suggesting that a low-iodine diet may contribute to the higher incidence of ATC.
The aggressive nature and rarity of ATC make it difficult to determine patient outcome, especially in single-institution studies with small cohorts and short follow-up. In fact, ATC is classified as Stage IV thyroid carcinoma according to the American Joint Committee on Cancer (AJCC), regardless of the tumor size or the presence of lymph node or distant metastasis.[5] ATC presents in the sixth to seventh decades of life[6,7] with <5% of cases seen in patients aged <40 years[7] and little is known about the disease in young patients.
The aim of this study was to analyze the clinico-pathological characteristics of patients who were diagnosed with ATC in an iodine-deficient area, for which we reviewed the medical records of ATC patients treated in our hospital.
MATERIALS AND METHODS
The medical records of 100 patients diagnosed with ATC at SGPGI between 1991 and 2013 were reviewed. The diagnosis was confirmed by dedicated pathologists through histological analysis of surgical specimens in operated cases. For nonoperated cases, diagnosis was made through cytology or core biopsy. We collected data on demographic characteristics of patients including age, gender, place of residence, duration of disease before diagnosis, presence of pre-existing goiter, and whether the operation was done or just fine-needle aspiration (FNA) biopsy. Staging was done according to AJCC. Special attention was focused on the histopathological findings in the operated patients and the presence of pre-existing well-differentiated thyroid cancer. Treatment offered and treatment accepted by the patient was also noted.
Follow-up data on whether patients were still alive or when they died were gathered through interviews of patients or their families through postal or telephonic media. Overall survival was defined as the time from the first day to the date of death from any cause. Survival curves were estimated using the Kaplan–Meier method.
RESULTS
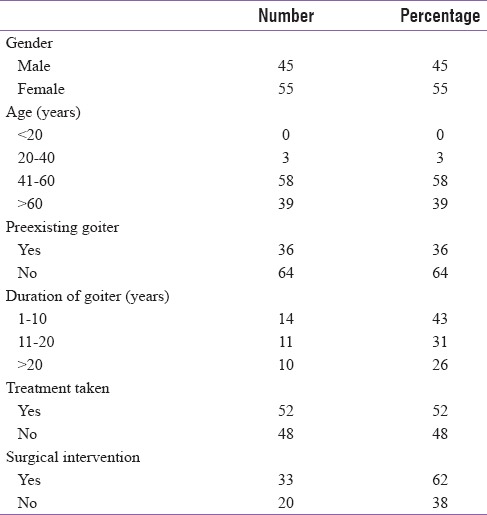
Basic demographic and clinical characteristics of ATC patients are shown in Table 1. The age of patients was ranged from 36 to 80 years (mean: 58 years). About 34 patients were ≤50 years and only 3 patients were <40 years. The youngest patient was 36-year old. There were 45 male and 55 female patients, yielding a ratio of 1:1.2 [Table 1].
Table 1.
Demographic and clinical characteristics
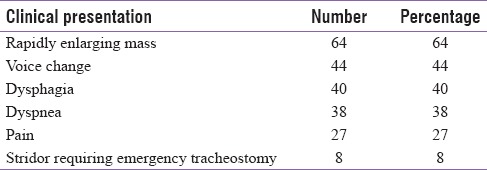
The most common presentation was that of a rapidly growing fixed and hard mass (64%). Due to rapid expansion, 27% patients experienced severe pain. About one-third of patients (36%) presented as sudden enlargement of pre-existing goiter over few weeks. Associated signs and symptoms are presented in Table 2. The median duration of symptoms before diagnosis was 3 months (range 8 days to 60 months). About 41% presented with lymph node enlargement. At the time of diagnosis, 31% presented with distant metastasis, most frequent site being lungs (70%). Tumor was 5–10 cm in 61%, >10% in 36%, whereas rest had tumor <5 cm.
Table 2.
Clinical presentation
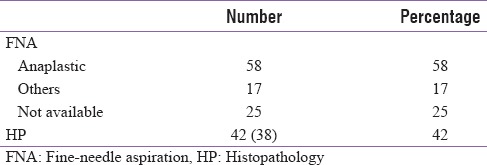
The diagnosis was established with either FNA or core biopsy [Table 3]. Cytological results were available in 75 patients, 58 patients were given the diagnosis of anaplastic carcinoma, whereas 17 had a different diagnosis given on FNA (seven had poorly differentiated, three were medullary thyroid, two were suggestive of either poorly differentiated or medullary, two follicular variant of PTC, one each for colloid and squamous cell, whereas cytology of one patient was suspicious of malignancy). In these 17 patients, the diagnosis of ATC was established by histopathology (core biopsy or surgical specimen). The cytological pattern obtained by FNA was based on the presence of pleomorphic cellular population in a necrotic background. The tumor cells were bizarre, oval- to spindle-shaped, dyscohesive elements showing anisocytosis, and irregular sometimes multiple nuclei.
Table 3.
FNA and HP correlation
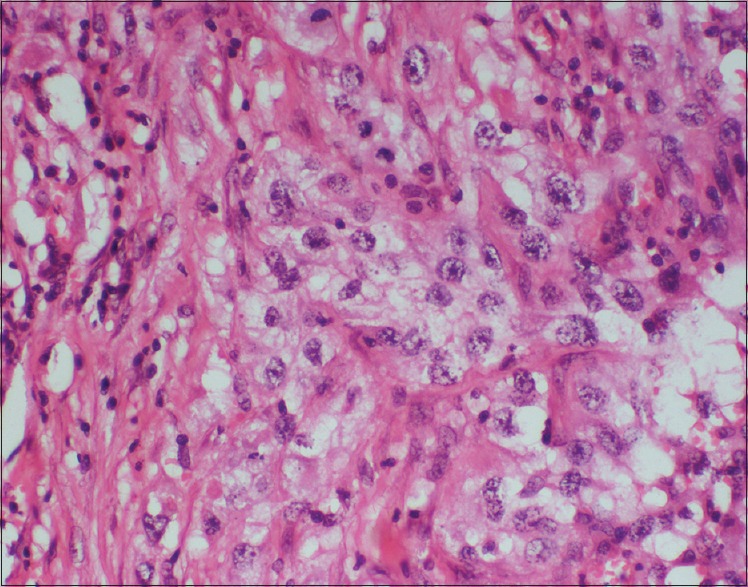
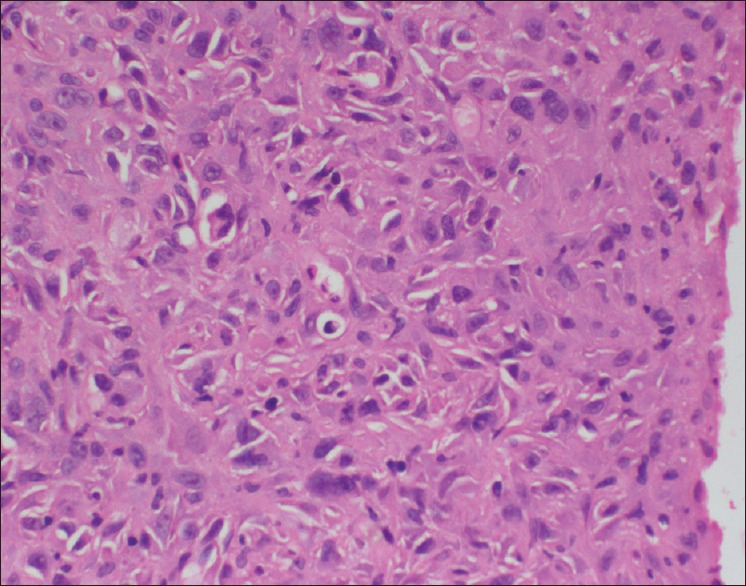
Histopathology was available in 32 patients and showed four major patterns: spindle cell (n = 9) [Figure 1], giant cell (n = 7), epithelioid (n = 5), squamoid [Figure 2] (n = 1), mixed spindle and giant (n = 9), and mixed squamoid + spindle (n = 1). Squamoid pattern was characterized by formation of distinct nests of irregular configuration with moderate pleomorphism. When the tumor was predominantly composed of spindle cells [Figures 1 and 4], the cells had a sarcomatoid appearance often arranged in fascicles resembling a sarcoma. The giant cell pattern was characterized by a high degree of pleomorphism than that of other patterns with numerous giant cells with large anaplastic cells containing single or multiple hyperpyknotic nuclei and eosinophilic cytoplasm. Epithelioid types [Figure 3] are characterized by polygonal cells with a clearly epithelial appearance, growing in solid nests, intermingled by desmoplastic stroma. All four patterns had high mitotic activity, large foci of necrosis, and high-degree invasiveness. Seven tumors contained residual foci of well-differentiated (three papillary, one follicular) or poorly differentiated tumors (n = 3).
Figure 1.
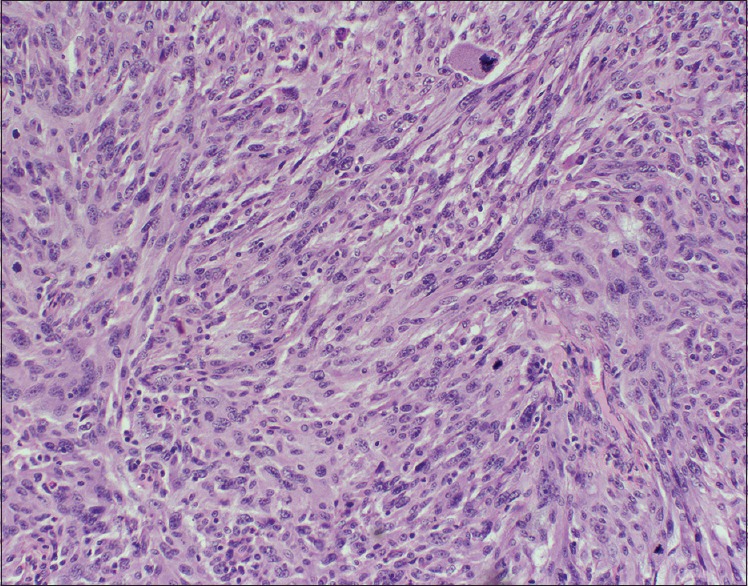
Microphotograph from anaplastic carcinoma thyroid shows spindle cells present in short fascicles infiltrated by lymphomonuclear inflammatory infiltrate and frequent mitotic figures including atypical mitosis (H and E stain, 200× magnification)
Figure 2.
Microphotograph shows islands of squamous cells with clear cytoplasm (H and E stain, 400× Magnification)
Figure 4.
Spindle cell component of anaplastic carcinoma showing marked nuclear pleomorphism (H and E stain, 400× magnification)
Figure 3.
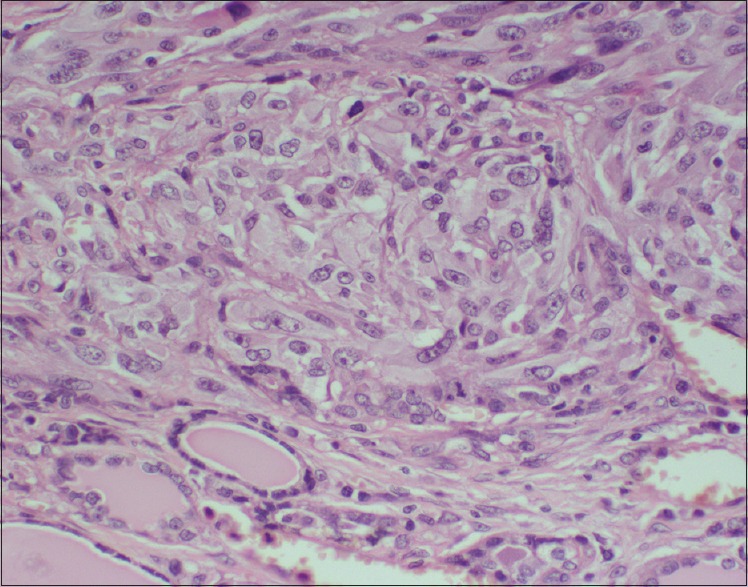
Microphotograph showing epithelial component with irregular vesicular nuclei and abundant cytoplasm (H and E stain, 400× magnification)
Patients underwent either all or some of the following investigations, like chest x-ray, indirect laryngoscopy, neck ultrasound, bone scan, Contrast enhanced computed tomography (CECT) neck, and mediastinum, for determining the extent of locoregional invasion and feasibility of resection.
Eight patients presented with stridor and required emergency tracheostomy for airway control. Five patients underwent debulking surgery for relief of airway obstruction. In all these five cases, the thyroid was found to be densely adhered to strap muscles and trachea and complete resection was not possible; three of them underwent tracheostomy intraoperatively.
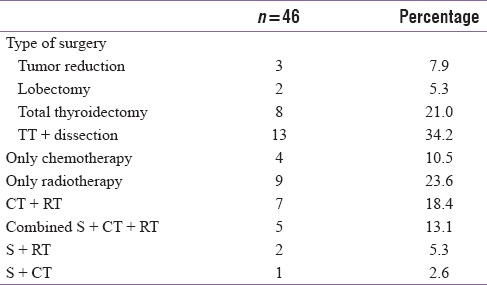
Total thyroidectomy was possible in 8 [Table 4] patients, whereas total thyroidectomy with some form of lymph node dissection was done in 13 patients.
Table 4.
Treatment
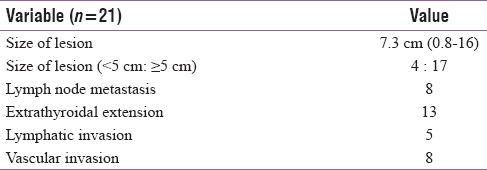
Out of 21 patients that underwent total thyroidectomy, 14 of them had pre-existing goiter. The mean duration of symptoms before presentation was 4.6 months. Ten (47%) patients had initial cytology other than anaplastic. Five patients had differentiated and poorly differentiated component on histopathology. Pathological characteristics are described in Table 5.
Table 5.
Pathological characteristics of operated patients
Patients received radiotherapy with or without chemotherapy (cisplatin/adriamycin). Radiotherapy was given with either palliative intent where dose of 20–30 Gy given in 5–10 fractions or radical intent where the thyroid bed and the neck was given 50–70 Gy by either conventional fractionation or hyper fractionated radiotherapy. Seven patients received hyper fractionated radiotherapy with chemotherapy. Eight patients who had undergone surgery (total thyroidectomy) received some sort of adjuvant therapy. Survival data were available in 36 patients. Median overall survival was 3 months. Overall survival was significantly better in patients receiving some form of treatment [Figure 5].
Figure 5.
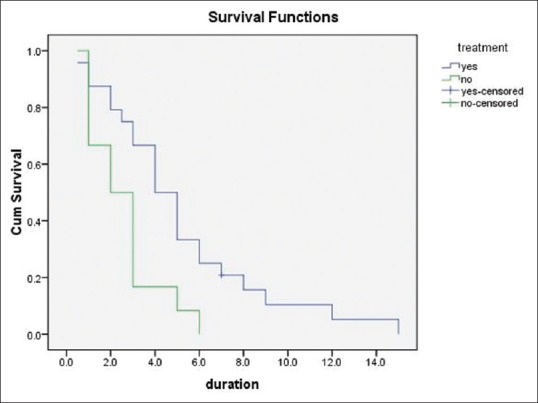
Survival image
DISCUSSION
ATC is one of the most aggressive solid tumors to affect humans with average 5-year survival of around only 3.6%.[8] The aim of this paper was to study the clinic-pathological profile of ATC from an endemic goiter area. More than 90% of all patients in the reported literature are >50 years.[9,10] Infact, anaplastic carcinoma is rare under 40 years of age.[11] Age has been found to be an independent prognostic factor in ATC. However, the mean age of our patients was 58 years and 34% were ≤50 years of age. This is in contrast to world literature, where the ATCs affect patients a decade later.[12] Tennvall et al.[13] reported that the median duration of symptoms before diagnosis was 1.5 months, whereas in our series, the median duration of symptoms was 3 months. The most common presentation was that of a rapidly growing fixed and hard mass as seen in 64% of our patients. This is similar to the study by Giuffrida et al.[14] Regional lymph node swelling (41%) and neck pain (27%) along with usual systemic symptoms of anorexia and weight loss that are commonly present at the time of diagnosis were similar to other reported literature.[15] In ATC, distant metastases are observed in 20%–50% of cases at the time of diagnosis. In study by Hundahl et al.,[1] metastases are found in half of patients at presentation with one-fourth developing metastasis during the course of disease and lungs being the most common sites of metastasis.[8] In our study, 31% presented with distant metastasis at the time of diagnosis and the most frequent site being lungs (70%). Pre-existing goiter or a family history of goiter[16] and previously undetected long-standing thyroid cancers have been identified as risk factors for ATC. One-third of our patients had pre-existing goiter for mean duration of 16 years.
The diagnosis of ATC is usually made by FNA cytology. However, FNA may sometimes be inconclusive in view of extensive necrosis, in which case core biopsy may be needed. In our study, FNA was available in 75 cases and a diagnosis of ATC was correctly made in 58 cases (77%).
The histopathological type depends on the admixture of four main patterns: spindle cell, giant cell, and squamoid and epithelioid. These patterns often coexist and are not predictive of patients’ outcome. The sarcomatoid type (spindle or giant type) predominated in 25 specimens (78%).
Only 51% patients accepted some form of treatment. The rest did not accept any form of treatment once the diagnosis and prognosis was explained. Treatment modalities for ATC include combination therapy with surgical resection for local control, external beam radiotherapy, and chemotherapy. The combination of surgery and radiotherapy is the most effective treatment available in controlling local disease.[17,18] Radical resection of tumor is considered to be an important therapy in tumors that are locally advanced.[19] Total thyroidectomy with or without lymph node dissection was possible in 21 patients. Out of these patients that underwent total thyroidectomy, 66% of them had pre-existing goiter. The mean size of lesion was 7.3 cm. About 47% patients had initial cytology other than anaplastic. The initial cytology was papillary, follicular, medullary thyroid, and poorly differentiated types in these 10 patients. The decision of total thyroidectomy in 10 patients was based on cytology report of a tumor with better prognosis. In the remaining 11 patients with an FNA diagnosis of ATC, total thyroidectomy was possible without causing excessive morbidity.
The best results are obtained by multimodal treatment.[9,10,20] Only five of our patients received combined multimodality treatment (surgery + chemotherapy and radiotherapy).
CONCLUSION
ATC may present a decade earlier in iodine-deficient areas; otherwise, the clinico-pathological profile of our patients is not different from that of iodine-sufficient areas. Patients with clinical suspicion of ATC should undergo core biopsy. Total thyroidectomy may be offered upfront if it can be performed without causing significant morbidity. When end of life issues are discussed, most patients opt for comfort care rather than entering into an active treatment program.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hundahl SA, Fleming ID, Fremgen AM, Menck HR. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985–1995. Cancer. 1998;83:2638–48. doi: 10.1002/(sici)1097-0142(19981215)83:12<2638::aid-cncr31>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 2.Kitamura Y, Shimizu K, Nagahama M, Sugino K, Ozaki O, Mimura T, et al. Immediate causes of death in thyroid carcinoma: Clinicopathological analysis of 161 fatal cases. J Clin Endocrinol Metab. 1999;84:4043–49. doi: 10.1210/jcem.84.11.6115. [DOI] [PubMed] [Google Scholar]
- 3.Besic N, Hocevar M, Zgajnar J. Lower incidence of anaplastic carcinoma after higher iodination of salt in Slovenia. Thyroid. 2010;20:623–6. doi: 10.1089/thy.2009.0404. [DOI] [PubMed] [Google Scholar]
- 4.Dijkstra B, Prichard RS, Lee A, Kelly LM, Smyth PP, Crotty T, et al. Changing patterns of thyroid carcinoma. Ir J Med Sci. 2007;176:87–90. doi: 10.1007/s11845-007-0041-y. [DOI] [PubMed] [Google Scholar]
- 5.Greene FL, Page DL, Fleming ID. Thyroid. AJCC Cancer Staging Manual. 6th ed. New York: Springer-Verlag; 2002. p. 77. [Google Scholar]
- 6.Smallridge RC, Copland JA. Anaplastic thyroid carcinoma: Pathogenesis and emerging therapies. Clin Oncol. 2010;22:486–97. doi: 10.1016/j.clon.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wein RO, Weber RS. Anaplastic thyroid carcinoma: Palliation or treatment? Curr Opin Otolaryngol Head Neck Surg. 2011;19:113–8. doi: 10.1097/MOO.0b013e328343af3d. [DOI] [PubMed] [Google Scholar]
- 8.Nel CJ, van Heerden JA, Goellner JR, Gharib H, McConahey WM, Taylor WF, et al. Anaplastic carcinoma of the thyroid: A clinicopathologic study of 82 cases. Mayo Clin Proc. 1985;60:51–8. doi: 10.1016/s0025-6196(12)65285-9. [DOI] [PubMed] [Google Scholar]
- 9.Sugitani I, Kasai N, Fujimoto Y, Yanagisawa A. Prognostic factors and therapeutic strategy for anaplastic carcinoma of the thyroid. World J Surg. 2001;25:617–22. doi: 10.1007/s002680020166. [DOI] [PubMed] [Google Scholar]
- 10.Hadar T, Mor C, Shvero J, Parmentier J, Remick SC. Anaplastic carcinoma of the thyroid. Eur J Surg Oncol. 1993;19:511–6. [PubMed] [Google Scholar]
- 11.Pichardo-Lowden A, Durvesh S, Douglas S, Todd W, Bruno M, Goldenberg D. Anaplastic thyroid carcinoma in a young woman: A rare case of survival. Thyroid. 2009;19:775–9. doi: 10.1089/thy.2009.0025. [DOI] [PubMed] [Google Scholar]
- 12.Akaishi J, Sugino K, Kitagawa W, Nagahama M, Kameyama K, Shimizu K, et al. Prognostic factors and treatment outcomes of 100 cases of anaplastic thyroid carcinoma. Thyroid. 2011;21:1183–9. doi: 10.1089/thy.2010.0332. [DOI] [PubMed] [Google Scholar]
- 13.Tennvall J, Lundell G, Wahlberg P, Bergenfelz A, Grimelius L, Akerman M, et al. Anaplastic thyroid carcinoma: Three protocols combining doxorubicin, hyperfractionated radiotherapy and surgery. Br J Cancer. 2002;86:1848–53. doi: 10.1038/sj.bjc.6600361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giuffrida D, Gharib H. Anaplastic thyroid carcinoma: Current diagnosis and treatment. Ann Oncol. 2000;11:1083–9. doi: 10.1023/a:1008322002520. [DOI] [PubMed] [Google Scholar]
- 15.Nagaiah G, Hossain A, Mooney CJ, Parmentier J, Remick SC. Anaplastic thyroid cancer: A review of epidemiology, pathogenesis, and treatment. J Oncol 2011. 2011:542358. doi: 10.1155/2011/542358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hundahl SA, Cady B, Cunningham MP, Mazzaferri E, McKee RF, Rosai J, et al. Initial results from a prospective cohort study of 5583 cases of thyroid carcinoma treated in the united states during 1996. U.S. and German Thyroid Cancer Study Group. An American College of Surgeons Commission on Cancer Patient Care Evaluation study. Cancer. 2000;89:202–17. doi: 10.1002/1097-0142(20000701)89:1<202::aid-cncr27>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 17.Siironen P, Hagström J, Mäenpää HO, Louhimo J, Heikkilä A, Heiskanen I, et al. Anaplastic and poorly differentiated thyroid carcinoma: Therapeutic strategies and treatment outcome of 52 consecutive patients. Oncology. 2010;79:400–8. doi: 10.1159/000322640. [DOI] [PubMed] [Google Scholar]
- 18.Haigh PI, Ituarte PHG, Wu HS, Treseler PA, Posner MD, Quivey JM, et al. Completely resected anaplastic thyroid carcinoma combined with adjuvant chemotherapy and irradiation is associated with prolonged survival. Cancer. 2001;91:2335–42. [PubMed] [Google Scholar]
- 19.Perri F, Lorenzo GD, Scarpati GD, Buonerba C. Anaplastic thyroid carcinoma: A comprehensive review of current and future therapeutic options. World J Clin Oncol. 2011;2:150–7. doi: 10.5306/wjco.v2.i3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Venkatesh YS, Ordonez NG, Schultz PN, Hickey RC, Goepfert H, Samaan NA. Anaplastic carcinoma of the thyroid. A clinicopathologic study of 121 cases. Cancer. 1990;66:321–6. doi: 10.1002/1097-0142(19900715)66:2<321::aid-cncr2820660221>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]


