Abstract
Objective:
To determine the prevalence and CT features of malignancy in incidental focal fundal gallbladder wall thickening.
Methods:
Patients with incidental focal fundal gallbladder wall thickening on CT were included if they had an ultrasound or MRI diagnostic of the etiology (n=19), stability on CT for 1 year (n=84), or pathological correlation (n=13). Morphologies were classified as type 1 (nodular/pinched intramural low attenuation), type 2 (intramural low attenuation), type 3 (homogeneous enhancement), type 4 (nodular/pinched homogeneous enhancement), type 5 (intramural cystic spaces), or type 6 (hyper-enhancing/heterogeneous enhancement).
Results:
116 patients had the following morphologies: type 1 (n=57), type 2 (n=10), type 3 (n=6), type 4 (n=19), type 5 (n=14), type 6 (n=10). Four (3.4%; 95% CI 0.9, 8.6%) cases of malignancy were identified (type 6 in three and type 3 in one).
Conclusions:
Incidental focal fundal gallbladder wall thickening is usually benign. CT features help distinguish benign from malignant etiologies.
Keywords: Gallbladder, fundal, focal wall thickening, adenomyomatosis
Introduction
Focal gallbladder wall thickening may be incidentally encountered on abdominal CT performed for other reasons. The differential diagnosis for focal gallbladder wall thickening includes benign etiologies such as focal adenomyomatosis, benign polyps and localized chronic cholecystitis, as well as malignant etiologies such as gallbladder cancer, lymphoma and metastases 1. In particular, the fundus is the most common location for focal adenomyomatosis, a benign condition that is typically asymptomatic and usually requires no treatment or follow up 2. Adenomyomatosis is also a relatively common entity, seen in 2–8% of cholecystectomy specimens 3. Although gallbladder carcinoma is less common than adenomyomatosis and other benign etiologies of focal gallbladder wall thickening, it is an aggressive cancer with 5 year survival rates of 5–10% 4. However 5 year survival rates up to 100% have been reported for stage T1 tumor following cholecystectomy 5. Thus distinguishing early stage gallbladder cancer from benign disease in crucial.
Unfortunately, the distinction between gallbladder cancer and benign diseases such as adenomyomatosis can be challenging at CT. Gallbladder cancer can present as a polypoid mass or a mass replacing the gallbladder, in which cases the appropriate management has been established 6,7. However, gallbladder cancer can also present as focal or diffuse wall thickening which may have a similar appearance to benign causes of wall thickening. Intramural cystic spaces are the classic feature of adenomyomatosis and are well demonstrated by T2-weighted MRI 8. When the cystic spaces are seen within an area of wall thickening at CT, the diagnosis of adenomyomatosis can be made with confidence 9. However, due to the limited contrast resolution of CT compared to MRI, the cystic spaces are often not seen at CT, and it may not be possible to distinguish adenomyomatosis and gallbladder cancer. The gallbladder wall enhancement pattern has also been a reported feature to distinguish benign from malignant wall thickening 10. The CT features that might help distinguish benign from malignant gallbladder wall thickening specifically confined to the fundus have not been examined. Therefore, the purpose of this study is to determine the prevalence of malignancy in incidental focal fundal gallbladder wall thickening seen at CT, and to determine which CT features, if any, predict malignancy.
Materials Methods
Patient Population
We performed a retrospective study which was approved by our institutional review board and was Health Insurance Portability and Accountability Act compliant. We performed a search of the radiology database for patients 18 years and older who underwent contrast-enhanced CT of the abdomen from April 1, 2002 to January 18, 2017. The phrases “focal fundal,” fundal wall thickening,” “adenomyomatosis,” and “gallbladder mass” were queried. The radiology reports were first reviewed to ensure there was a description of focal fundal gallbladder wall thickening and this yielded 240 patients. One-hundred twenty patients were excluded owing to a lack of follow up imaging. The images were then reviewed to exclude cases of polypoid masses (n=3) or masses with clear invasion into the liver (n=1). The remaining 116 patients (mean age 64.3 years; 49 men, 67 women) were included in the study. The reference standard for the presence or absence of malignancy was follow up ultrasound or MRI diagnostic of the etiology of the wall thickening (n=19), stability on CT for at least 1 year (n=84), or pathological correlation (n=13). The indications for the index CT are presented in table 1.
Table 1.
Indications for index CT examinations.
| Indication | Number of cases |
|---|---|
| History of cancer | 41 |
| Abdominal pain | 38 |
| Cirrhosis | 8 |
| Fever/infection | 5 |
| Trauma | 5 |
| Abdominal mass | 5 |
| Aneurysm | 4 |
| Hernia | 3 |
| Nausea/vomiting | 2 |
| Renal transplant | 2 |
| Biliary dilation | 1 |
| Hematuria | 1 |
| Hematochezia | 1 |
| Total | 116 |
Imaging Technique
Owing to the length of the study period, index CT examinations were performed on a variety of CT scanners. MDCT scanners included GE 16 & 64 detector row scanners (General Electric Medical Systems, Milwaukee, WI) and Siemens 64 and 128 detector row scanners (Siemens Medical System, Forchheim, Germany). All scans were obtained using a fixed kV of 120 and variable mAs using automated dose modulation. The pitch varied across the scanners. All exams were reconstructed at slice thicknesses/intervals of 5/5 mm and 98 exams were also reconstructed at slice thicknesses/intervals 1.25/1.25 mm owing to a change in our protocols during the study period. One hundred twelve index CT exams were performed in the portal venous phase and four were performed in the arterial phase. Omnipaque-350 (GE Healthcare, Cork, Ireland) was injected intravenously at a dose of 100–150 mL using a power injector at a rate of 2–4 mL/second.
The follow up ultrasounds were performed by Registered Diagnostic Medical Sonographer-licensed technologists using Acuson Sequoia (Siemens Medical Solutions, Mountain View, CA) or LOGIQ E9 (GE Healthcare, Milwaukee, WI) ultrasound machines. A variety of probes including curved, linear, and vector (low and high-frequency) were utilized depending on penetration.
Follow up MRIs were performed either on 1.5 Tesla General Electric Signa MRI Scanner systems or 1.5 Tesla General Electric Optima MR 450w (GE Medical Systems, Milwaukee, WI), with phased array torso coils. The exact protocols varied due to the length of the study period, however all included the following sequences: coronal T2-weighted single shot fast spin echo (SSFSE) (field of view (FOV), 38 cm; slice thickness, 5 mm; spacing 6 mm; matrix 288 × 192; TR, 1141 msec; TE, 90 msec, flip angle (FA), 90), axial T2-weighted SSFSE (FOV, 40 cm; slice thickness, 5 mm; spacing 6 mm; matrix 288 × 192; TR, 900 msec; TE, 90 msec; FA, 90), axial fat saturated T2-weighted fast spin echo (FOV, 40 cm; slice thickness, 5 mm; spacing 6 mm; matrix 288 × 192; TR, 2200 msec; TE, 90 msec; echo train length, 25; FA, 90), and axial 2D in/out of phase T1-weighted imaging (FOV, 40 cm; slice thickness, 5 mm; spacing 6 mm; matrix 288 × 160; TR, 150 msec; TE, 2.2/4.4 msec; FA, 90). Pre and post contrast imaging was acquired using axial T1-weighted fat saturated 3D spoiled gradient echo (FOV, 40 cm; slice thickness, 5 mm; spacing 2.5 mm; matrix 288 × 192; TR, 3.1 msec; TE, 1.4 msec; FA, 12) before and after the intravenous administration of 0.1 mmol/Kg of gadodiamide at a rate of 2cc/sec.
Image Analysis
Two radiologists with subspecialty training in abdominal imaging (with 8 and 6 years of post-training experience) independently reviewed the images and categorized the focal fundal gallbladder wall thickening into 1 of 6 morphological types: Type 1 (nodular or pinched appearance with smooth inner layer wall enhancement and homogeneous intramural low attenuation without discrete cystic spaces), Type 2 (smooth inner layer wall enhancement and homogeneous intramural low attenuation without discrete cystic spaces), Type 3 (full thickness homogeneous wall enhancement), Type 4 (nodular or pinched with full thickness homogeneous wall enhancement), Type 5 (definite discrete intramural cystic spaces), and Type 6 (hyper-enhancing or heterogeneous wall enhancement involving any part of the thickened wall without discrete cystic spaces) (figure 1–6). Any discrepancies were resolved by consensus between the same two reviewers. Both axial and coronal images were available for review and thin (1.25 mm) axial images were available for review in 98 cases. The maximal wall thickness was measured on the axial images by a single reviewer. Measurements were taken perpendicular to the wall at the point of maximal thickness.
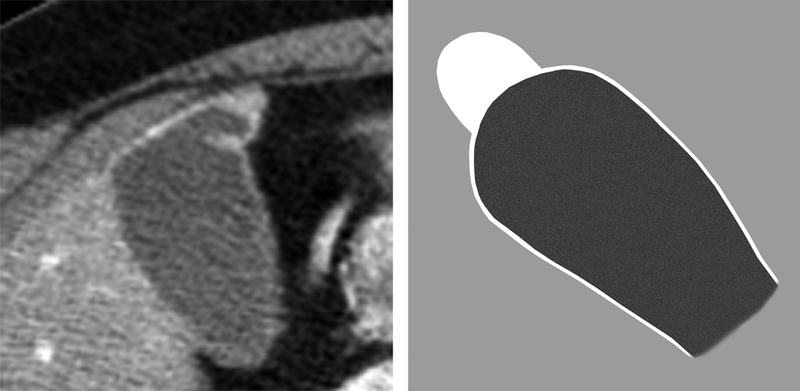
Fig 1.
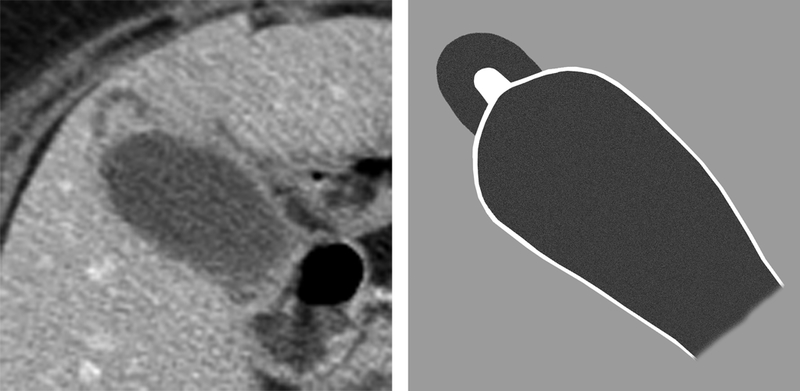
Type 1 focal fundal gallbladder wall thickening. 76 year old female with benign gallbladder wall thickening that was stable for over 2 years. (a) Axial CT reveals a pinched/nodular appearance of the gallbladder fundus with smooth inner layer enhancement and homogeneous low attenuation within the wall. (b) Type 1 diagram.
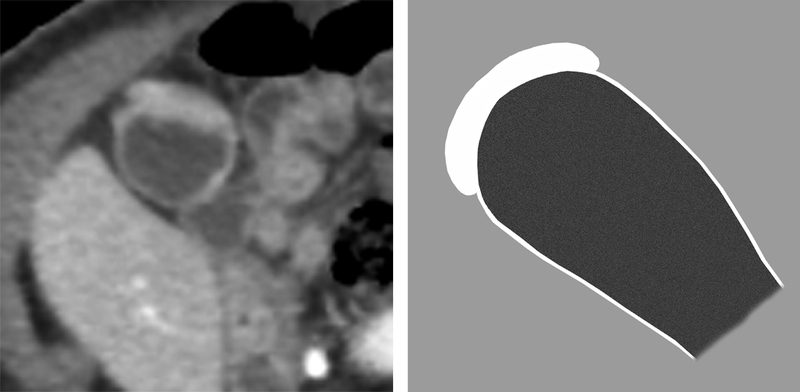
Fig 6.
Type 6 focal fundal gallbladder wall thickening. 67 year old man with gallbladder adenocarcinoma. (a) Axial CT image shows heterogeneous enhancement of the thickened gallbladder fundus. (b) Type 6 diagram.
Imaging Follow up
The original radiology reports and images of any follow up ultrasound (n=5) or MRI (n=14) were reviewed by one radiologist. A definite diagnosis of adenomyomatosis was made on ultrasound if there was focal fundal wall thickening with intramural echogenic foci demonstrating “comet-tail” artifact. A definite diagnosis of adenomyomatosis was made on MRI if there were intramural cystic spaces seen as hyperintense on T2-weighted images within the focal fundal wall thickening. The diagnosis of malignancy was not made on ultrasound alone. The diagnosis of possible malignancy was made on MRI if there was full thickness or heterogeneous wall enhancement without intramural cystic spaces on T2-weighted imaging.
Imaging stability was assessed on follow up CT of the chest (n=6) or abdomen (n=78) that adequately showed the gallbladder fundus. Stability was defined as no change in the degree of wall thickening across the studies with a minimum of 1 year follow up. The mean time to follow up CT was 3.4 years +/− 2.4 years (range 1–10.3 years).
Statistical Analysis
Two-sided 95% confidence intervals were calculated using binomial exact method. For ratios with numerators of 0, one-sided 95% confidence intervals were used. An unpaired student’s t-test was used to compare wall thickness between benign and malignant lesions. Intra-class correlation coefficients (ICC) with 95% confidence intervals were calculated to assess inter-reader agreement for wall thickening type.
Results
There were 116 patients included in the study. The mean thickness of the malignant lesions was 15.8 +/− 8.1 mm (range 8–25 mm), which was significantly greater than that of the benign lesions at 9.0 +/− 3.1 mm (range 4–18 mm) (p<.0001).
The number of benign and malignant or possibly malignant cases for each morphology is presented in Table 2. Malignancy or possible malignancy was seen in 4/116 (3.4%; 95% CI 0.9, 8.6%). Three of the malignant cases had type 6 morphology; one case was pathologically proven gallbladder adenocarcinoma, one had positive peritoneal cytology for GI tract adenocarcinoma in the setting of the gallbladder lesion and was being treated for gallbladder cancer, and the third had a follow up MRI showing an enhancing mass suspicious for malignancy. The other case had type 3 morphology and both a follow up MRI and an endoscopic ultrasound showing a mass suspicious for malignancy. The two patients without any pathologic correlation died before any further follow up was obtained.
Table 2.
Number of malignant cases for each morphology type. Numbers in parentheses are percentages with 95% confidence intervals.
| Morphology Type | # of malignant cases/Total # of cases |
|---|---|
| 1 - nodular or pinched appearance with homogeneous intramural low attenuation |
0/57 (0%; 0.0–5.1%) |
| 2 - homogeneous intramural low attenuation |
0/10 (0%; 0.0–25.9%) |
| 3 - full thickness wall enhancement | 1/6 (16.7%; 0.4–64.1%) |
| 4 - nodular or pinched with full thickness enhancement |
0/19 (0%; 0.0–14.6%) |
| 5 - intramural cystic spaces | 0/14 (0%; 0.0–19.3%) |
| 6 - heterogeneous wall enhancement | 3/10 (30%; 6.7–65.2%) |
| Total | 4/116 (3.4%; 0.9–8.6%) |
The remaining 112 cases were all benign. Pathology was available in 11 benign cases with 6 cases of chronic cholecystitis, 4 cases of adenomyomatosis, and 1 case with no specific diagnosis but negative for malignancy. Follow up imaging with diagnostic results was available in 17 benign lesions (12 MRI and 5 ultrasound) all of which showed adenomyomatosis. The morphologies for the 21 cases of adenomyomatosis (diagnosed by pathology or definitive imaging) were as follows: type 1 (n=12), type 4 (n=4), type 5 (n=3), type 6 (n=2). Follow up CT was performed in 84 patients and the lesions were stable in 81, and resolved in 3.
The ICC for wall thickening type was 0.85 (95% CI 0.81, 0.89) showing good agreement between the two readers. There was a discrepancy in morphology type between the two readers in 15 of 116 cases. All of these 15 cases were benign lesions and there was perfect agreement on the morphology type in all 4 malignant cases.
Discussion
The results of this study confirm that focal fundal gallbladder wall thickening is most often due to benign entities. We propose a morphologic classification system based on contrast-enhanced CT features that helps distinguish benign and malignant etiologies.
Approximately 3% (4/116) of cases of focal fundal gallbladder wall thickening in our study were malignant or potentially malignant. Thirty percent of the cases (3/10) with heterogeneous wall enhancement (type 6) and 17% (1/6) of the cases with full thickness wall enhancement (type 3) were malignant. Therefore, these types should be considered as suspicious for malignancy when encountered, although benign etiologies remain possible. No cases of malignancy were seen when intramural cystic spaces were seen (type 5), and these were most likely cases of focal fundal adenomyomatosis. No cases of malignancy were seen when smooth inner layer enhancement and homogeneous intramural low attenuation was demonstrated, with (type 1, 0/57) or without (type 2, 0/10) a nodular/pinched appearance. These were also likely cases focal fundal adenomyomatosis. This is supported by the finding that 12 cases with type 1 morphology had pathology or imaging confirmation of adenomyomatosis. We hypothesize that the intramural low attenuation actually represents the small cystic spaces that are below the resolution of CT to clearly delineate. No cases (0/19) of malignancy were found with a nodular/pinched with full thickness enhancement appearance (type 4). Some of these cases proved to be focal fundal adenomyomatosis and again, may represent cases where the cystic spaces and even any low attenuation in the wall cannot be visualized by CT. However, the pattern is similar to full thickness wall enhancement (type 3) where one malignant lesion was seen, and due to the small number of lesions in the type 4 group, it is possible that malignancy could also have this appearance.
Malignant focal fundal gallbladder wall thickening was on average, thicker than benign causes however there was significant overlap between the two groups. The smallest thickness in the malignant group was 8 mm and thus minimal wall thickening less than this is likely to be benign. This may be a useful feature as morphologic assessment may be more difficult with lesser degrees of wall thickening.
Although our study is the first to specifically examine the risk of malignancy in focal fundal gallbladder wall thickening, our findings are similar to prior studies evaluating generalized gallbladder wall thickening. Our findings are in keeping with the study by Ching et al. which showed high specificity of intramural cystic spaces seen on CT for gallbladder adenomyomatosis 9. However, when cystic spaces were not visualized, the accuracy of CT was low for distinguishing adenomyomatosis from malignancy in that study. Kim et al. described 5 different patterns of flat gallbladder wall thickening (not isolated to the fundus) and found a heterogeneous pattern of wall enhancement to be associated with malignancy, in keeping with our results 10. That study also found an association with a strongly enhancing inner wall layer to be associated with malignancy and wall hyper-enhancement was included in our type 6 morphology. However, the remainder of patterns in that study did not readily apply to the morphologic types seen with isolated focal fundal gallbladder wall thickening in our study. Yun et al. found greater wall thickness in gallbladder malignancy vs. chronic cholecystitis which is also consistent with our findings 11. That study also found hyper-enhancement of the inner wall on arterial phase CT to be associated with malignancy. Our study did not assess this feature as no arterial phase was acquired with our CT protocols which were portal venous phase only given that our cases were incidentally detected. A study by Kim et al. specifically evaluated focal fundal gallbladder wall thickening on CT and found an oval contour, cystic spaces, and inner layer enhancement more commonly in adenomyomatosis compared to chronic cholecystitis 12. The oval contour likely corresponds to the nodular or pinched appearance described in our study. However our study did not assess the differences between the various benign causes of wall thickening, and the study by Kim et al. did not evaluate the CT features of focal fundal malignancy.
The results of our study will aid in the management of incidentally detected focal fundal gallbladder wall thickening on CT. If focal thickening with benign morphology in encountered, we suggest that no follow up is required. However, if the type 6, type 3, and potentially type 4 patterns are encountered, additional follow up imaging with ultrasound or MRI is warranted. If further tests are not diagnostic of a benign entity, close follow up or surgical resection should be considered. We feel that our classification system can be widely utilized as there was good agreement on morphology type by the two readers. Importantly, there was no disagreement between the readers in malignant cases.
Our retrospective study has limitations. We had a small sample size and pathologic proof was not available for most cases of focal fundal gallbladder wall thickening, including two cases of suspected malignancy. A definitive imaging diagnosis was also not available in most cases and benignity was established by stability in the majority of cases where the underlying etiology of the wall thickening is not known. However, we feel that stability on CT for at least one year (with a mean of 3.4 years in this study) is sufficient to exclude the possibility of an aggressive malignancy such as gallbladder carcinoma. The outcomes of patients without follow up are unknown. The CT protocols including slice thickness was not uniform due to the length of the study.
In conclusion, incidentally detected focal fundal gallbladder wall thickening is most often benign, and CT morphologic features help distinguish benign from malignant etiologies. Heterogeneous or full thickness wall enhancement patterns should raise suspicion for malignancy while smooth inner wall enhancement with homogeneous intramural low attenuation or cystic spaces can be considered benign.
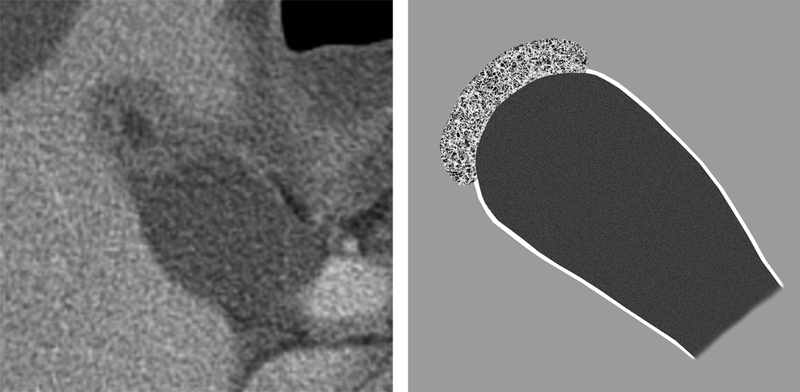
Fig 2.
Type 2 focal fundal gallbladder wall thickening. 72 year old man with benign fundal gallbladder wall thickening. (a) Axial CT shows homogeneous intramural low attenuation within the thickened gallbladder fundus. Follow up CT 2 years later (not shown) revealed stability. (b) Type 2 diagram.
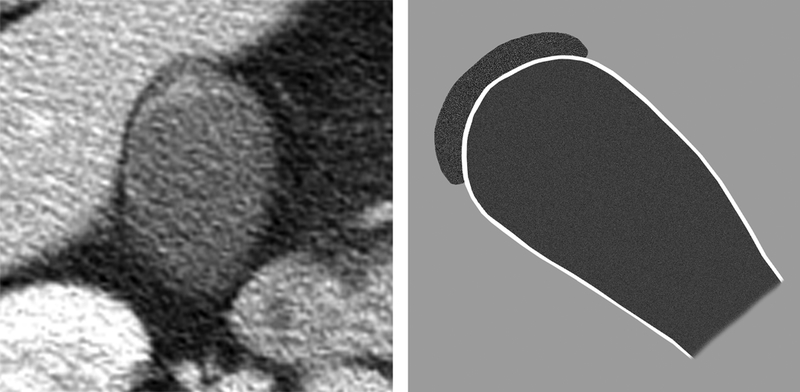
Fig 3.
Type 3 focal fundal gallbladder wall thickening. 83 year old woman with probable gallbladder malignancy. (a) Axial CT shows full thickness enhancement of the gallbladder wall. Follow up MRI (not shown) was suspicious for gallbladder malignancy but was never confirmed pathologically. (b) Type 3 diagram.
Fig 4.
Type 4 focal fundal gallbladder wall thickening. 66 year old woman with benign fundal gallbladder wall thickening. (a) Axial CT shows nodular/pinched appearance with full thickness enhancement. Follow up CT 3 years later (not shown) revealed stability. (b) Type 4 diagram.
Fig 5.
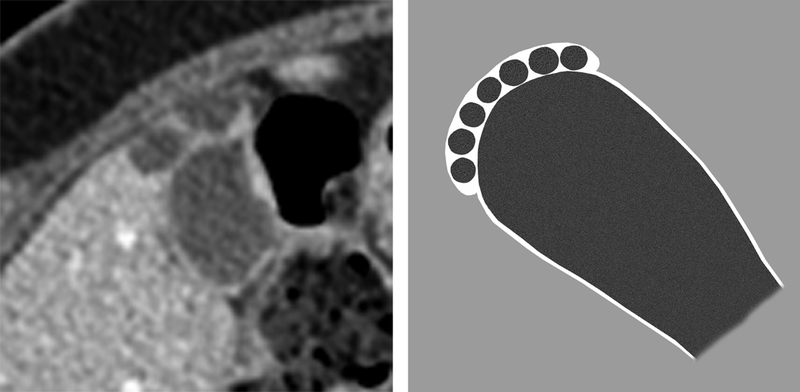
Type 5 focal fundal gallbladder wall thickening. 70 year old woman with benign fundal gallbladder wall thickening. (a) Axial CT shows cystic spaces within the gallbladder fundus. Follow up CT 2 years later (not shown) revealed stability. (b) Type 5 diagram.
Acknowledgments
The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through grant #UL1 TR000002.
References
- 1.Runner GJ, Corwin MT, Siewert B, et al. Gallbladder wall thickening. AJR. American journal of roentgenology January 2014;202(1):W1–W12. [DOI] [PubMed] [Google Scholar]
- 2.Boscak AR, Al-Hawary M, Ramsburgh SR. Best cases from the AFIP: Adenomyomatosis of the gallbladder. Radiographics : a review publication of the Radiological Society of North America, Inc May-Jun 2006;26(3):941–946. [DOI] [PubMed] [Google Scholar]
- 3.Hammad AY, Miura JT, Turaga KK, et al. A literature review of radiological findings to guide the diagnosis of gallbladder adenomyomatosis. HPB : the official journal of the International Hepato Pancreato Biliary Association February 2016;18(2):129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hueman MT, Vollmer CM Jr., Pawlik TM. Evolving treatment strategies for gallbladder cancer. Annals of surgical oncology August 2009;16(8):2101–2115. [DOI] [PubMed] [Google Scholar]
- 5.Kanthan R, Senger JL, Ahmed S, et al. Gallbladder Cancer in the 21st Century. Journal of oncology 2015;2015:967472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy AD, Murakata LA, Rohrmann CA Jr., Gallbladder carcinoma: radiologic-pathologic correlation. Radiographics : a review publication of the Radiological Society of North America, Inc Mar-Apr 2001;21(2):295–314; questionnaire, 549–255. [DOI] [PubMed] [Google Scholar]
- 7.Sebastian S, Araujo C, Neitlich JD, et al. Managing incidental findings on abdominal and pelvic CT and MRI, Part 4: white paper of the ACR Incidental Findings Committee II on gallbladder and biliary findings. Journal of the American College of Radiology : JACR December 2013;10(12):953–956. [DOI] [PubMed] [Google Scholar]
- 8.Yoon JH, Cha SS, Han SS, et al. Gallbladder adenomyomatosis: imaging findings. Abdominal imaging Sep-Oct 2006;31(5):555–563. [DOI] [PubMed] [Google Scholar]
- 9.Ching BH, Yeh BM, Westphalen AC, et al. CT differentiation of adenomyomatosis and gallbladder cancer. AJR. American journal of roentgenology July 2007;189(1):62–66. [DOI] [PubMed] [Google Scholar]
- 10.Kim SJ, Lee JM, Lee JY, et al. Analysis of enhancement pattern of flat gallbladder wall thickening on MDCT to differentiate gallbladder cancer from cholecystitis. AJR. American journal of roentgenology September 2008;191(3):765–771. [DOI] [PubMed] [Google Scholar]
- 11.Yun EJ, Cho SG, Park S, et al. Gallbladder carcinoma and chronic cholecystitis: differentiation with two-phase spiral CT. Abdominal imaging Jan-Feb 2004;29(1):102–108. [DOI] [PubMed] [Google Scholar]
- 12.Kim BS, Oh JY, Nam KJ, et al. Focal thickening at the fundus of the gallbladder: computed tomography differentiation of fundal type adenomyomatosis and localized chronic cholecystitis. Gut and liver March 2014;8(2):219–223. [DOI] [PMC free article] [PubMed] [Google Scholar]


