Abstract
Evidence suggests that affective problems, such as depression and anxiety, increase risk for late-life dementia. However, the extent to which affective problems influence cognitive decline, even many years prior to clinical diagnosis of dementia, is not clear. The present study systematically reviews and synthesises the evidence for the association between affective problems and decline in cognitive state (i.e., decline in non-specific cognitive function) in older adults. An electronic search of PubMed, PsycInfo, Cochrane, and ScienceDirect was conducted to identify studies of the association between depression and anxiety separately and decline in cognitive state. Key inclusion criteria were prospective, longitudinal designs with a minimum follow-up period of 1 year. Data extraction and methodological quality assessment using the STROBE checklist were conducted independently by two raters. A total of 34 studies (n = 71 244) met eligibility criteria, with 32 studies measuring depression (n = 68 793), and five measuring anxiety (n = 4698). A multi-level meta-analysis revealed that depression assessed as a binary predictor (OR 1.36, 95% CI 1.05–1.76, p = 0.02) or a continuous predictor (B = −0.008, 95% CI −0.015 to −0.002, p = 0.012; OR 0.992, 95% CI 0.985–0.998) was significantly associated with decline in cognitive state. The number of anxiety studies was insufficient for meta-analysis, and they are described in a narrative review. Results of the present study improve current understanding of the temporal nature of the association between affective problems and decline in cognitive state. They also suggest that cognitive function may need to be monitored closely in individuals with affective disorders, as these individuals may be at particular risk of greater cognitive decline.
Key words: Affective problems, ageing, anxiety, cognitive decline, depression, meta-analysis, systematic review
Introduction
Decline in cognitive state is a central feature of ageing, and severe deterioration in cognitive function has frequently been associated with poorer quality of life and worse performance on physical tasks (Tabbarah et al., 2002). Accelerated decline in cognitive state also has an influential and adverse impact upon the psychological, social, emotional and financial status of the individual, which can subsequently contribute to heightened levels of burden and distress (Wilson et al., 2007). Cognitive symptoms are common in affective disorders, particularly impairments in memory, executive control, feedback sensitivity and affective processing (Clark et al., 2009). These cognitive symptoms are associated with pathophysiology across a distributed neural circuit, which is made up of various regions across the prefrontal cortex, as well as subcortical regions and also temporal lobe structures (Clark et al., 2009). Both affective disorders, such as depression and anxiety, and poor cognitive function are common in older adulthood (Rovner et al., 1989; Alexopoulos and Abrams, 1991). It is estimated that after age 70, the combination of low mood and poor cognition doubles with every 5 years. By age 85, around one in four of individual experience both these comorbid conditions (Arve et al., 1999). Due to the high prevalence of these conditions in older adulthood, this is a research area of clinical relevance and importance.
Previous research has proposed that affective problems, such as depression and anxiety, may be associated with accelerated cognitive ageing (da Silva et al., 2013; Gulpers et al., 2016). However, there are significant gaps in our understanding of this link. For instance, the precise temporal order of the association between affective problems and decline in cognitive state is currently unclear. It is possible that affective problems may act as an early risk factor for decline in cognitive state, or alternatively that affective problems may be a prodromal symptom of oncoming cognitive impairment. Additionally, previous studies, including several meta-analyses, have been largely diagnosis driven, with a primary focus on dementia as an outcome (Jorm, 2001; Ownby et al., 2006; Byers and Yaffe, 2011; da Silva et al., 2013; Bennett and Thomas, 2014; Cherbuin et al., 2015). Less is known about the impact of affective problems on decline in cognitive state across the entire population spectrum. The focus on the transition to dementia as an outcome may be problematic, as it is now believed that there is a long pre-clinical period of several decades before cognitive impairment becomes evident (Morris, 2005). It is possible that participants who transition to dementia at follow-up assessment may have already developed substantial cerebral pathology by the time of baseline assessment, even if they were not yet presented with any cognitive symptoms. In this case, associations between affective disorders and development of dementia may be the result of reverse causality. The present study focuses on the association between affective disorders and decline in cognitive state in healthy older adults in order to minimise effects of possible reverse causality.
Cognitive state refers to a composite measure of overall cognitive function. It has been studied extensively in previous research (Nordin et al., 2006; Kavé et al., 2008; Sohrabi et al., 2008; Esslinger et al., 2011), using assessments of overall cognitive status, such as the Mini-Mental State Examination (MMSE) or composite assessments of multiple cognitive domains (e.g. memory, information processing speed, executive function). Therefore, decline in cognitive state is defined in the present review as a decline in overall cognitive function, rather than decline in specific cognitive domains. There is evidence from longitudinal research that low scores on cognitive state tests may predict onset of functional impairment (Moritz et al., 1995; Gill et al., 1996), and functional dependence over time (Agüero-Torres et al., 2002; Gill et al., 2002; Wang et al., 2002). For this reason, it is important to investigate how affective problems influence decline in cognitive state over time.
There are large individual differences in the extent of cognitive decline experienced by healthy older adults; however, the decline in cognitive state occurs at a steady and gradual rate over time. On average there is a decline of around 1–2 standard deviations in fluid cognition from age 20 to 70, after which average decline increases to around 0.5 s.d. every 10 years (Anstey and Low, 2004). This stable decline is often maintained over time until symptoms of dementia begin to manifest, at which point a sharper decline in cognitive state may be observed (Rubin et al., 1998). As such, studies in which substantial cognitive decline is apparent within a short time frame of under 1 year may be more indicative of pathological ageing (e.g. oncoming dementia), rather than healthy ageing. Since the present study aims to examine the longitudinal association between affective disorders and decline in cognitive state in cognitively healthy individuals, it includes only longitudinal studies with sufficient time between baseline and follow-up assessments (i.e., minimum 1 year) for a substantial decline to occur within these populations. There are several studies that have investigated the association between affective problems and decline in cognitive state (Bassuk et al., 1998; Geerlings et al., 2000; Paterniti et al., 2002; Ganguli et al., 2006; Reyes-Ortiz et al., 2008; Köhler et al., 2010; Bunce et al., 2012; Gale et al., 2012; Johnson et al., 2013; Neubauer et al., 2013; Royall and Palmer, 2013; Rajan et al., 2014; Chang and Tsai, 2015, Chen and Chang, 2016; Brailean et al., 2017). However, it is difficult to draw a straightforward conclusion from this work due to conflicting findings. Specifically, some studies report a significant association between affective problems and decline in cognitive state (Geerlings et al., 2000; Paterniti et al., 2002; Reyes-Ortiz et al., 2008; Köhler et al., 2010; Johnson et al., 2013; Royall and Palmer, 2013; Rajan et al., 2014; Chang and Tsai, 2015, Chen and Chang, 2016), while conversely others report that affective problems do not predict decline (Bassuk et al., 1998; Ganguli et al., 2006; Bunce et al., 2012; Gale et al., 2012; Neubauer et al., 2013; Brailean et al., 2017). These contradictory results are likely attributable to inconsistencies in methodologies and study design, such as length of follow-up, sampling, definitions used, differences in assessment tools and also the primary aim of each study (Bennett and Thomas, 2014). To date, however, there have been no systematic reviews or meta-analyses addressing associations between affective problems and subsequent decline in cognitive state, prior to the onset of dementia. Due to inconsistencies in findings, as well as the lack of attempts to synthesise these data, it is still unclear whether affective problems across the life course are associated with a decline in cognitive state, prior to the onset of dementia and cognitive impairment. The primary aim of the present study therefore was to systematically review and synthesise current evidence regarding the longitudinal association between affective problems (depression and anxiety separately) and subsequent decline in cognitive state, with consideration of several potential moderators, including mean age of sample at baseline, length of follow-up, quality of study and publication year.
Method
Search strategy
This review was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). A systematic literature search was conducted using PubMed, PsycInfo, Cochrane, and ScienceDirect databases for studies investigating the association between affective problems and decline in cognitive state. All studies published up to November 2016 were included in the search. There was no restriction on the start date. Our search terms comprised three search blocks (Table 1). The first search block included keywords relating to affective problems. The second search block contained keywords describing the decline in cognitive state. To reduce the number of irrelevant hits, a third search block was added, which contained keywords related to methodology, to ensure all studies with cross-sectional designs were excluded from search results. In addition, reference lists of relevant papers were scanned for articles of interest.
Table 1.
Key terms used for systematic search
| Search block 1 (Affective problems) | Search block 2 (Cognitive decline) | Search block 3 (Study design) |
|---|---|---|
| Depress* OR MDD OR Dysthymi* OR Anxi* OR GAD OR worr* OR Phobia OR Panic OR Agoraphobia OR ‘Obsessive compulsive’ OR OCD OR PTSD OR ‘Post traumatic stress’ OR ‘Post-traumatic stress’ OR mood OR affective OR psychiatric OR neuropsychiatric | ‘Cognitive function’ OR ‘Cognitive impairment’ OR ‘Cognitive decline’ OR ‘Cognitive deficit’ OR ‘Cognitive loss’ OR ‘Cognition loss’ OR ‘Cognitive ability’ OR ‘Cognitive abilities’ OR ‘Cognitive status’ OR ‘Cognitive change’ OR ‘Cognition change’ OR ‘Cognitive performance’ OR ‘Cognitive dysfunction’ OR ‘Cognitive complaints’ OR ‘Cognitive capability’ OR ‘Cognitive ageing’ OR ‘Cognitive aging’ OR Memory OR Attention OR ‘Reaction time’ OR ‘Speed of processing’ OR ‘Processing speed’ OR Intelligence OR ‘General mental ability’ OR GMA OR ‘Executive function’ OR ‘Neuropsychological testing’ OR ‘Mini mental state exam’ OR MMSE OR ‘Mental status’ | Longitudinal OR prospective OR follow-up OR cohort OR ‘life course’ OR lifespan OR ‘life span’ OR lifelong OR ‘lifelong’ |
Inclusion/exclusion criteria
Stringent inclusion/exclusion criteria were applied to articles identified through the initial search.
Design criteria
Original studies written in English up to November 2016 were included. Only studies using longitudinal, prospective designs with human participants were included in order to test for the association between affective disorders and decline in cognitive state over time. Cross-sectional, case-control, experimental, including intervention and treatment, studies were excluded. Studies with a follow-up period of 1 year or greater were included, as it is possible that substantial decline in cognitive state may not be observed over very short follow-up periods in a general population. Included studies used samples drawn from a general population, whereas studies using specific clinical populations only, for example, a sample of stroke patients, were excluded. This criterion was used because inclusion of clinical samples may increase the heterogeneity of data synthesis and reduce the comparability of studies. Studies with a sample size of 100 or less were also considered ineligible, due to insufficient statistical power.
Outcome-related criteria
Samples with cognitive impairment or dementia present at baseline were excluded. In addition to this, studies with any measure of change in cognitive state from baseline to follow-up were selected for inclusion. Other outcomes, such as the transition to dementia or cognitive performance at follow-up without consideration of change from a baseline measure were omitted. This was because the present study aimed to look at the association between affective disorders and cognitive decline within healthy ageing populations, rather than samples with dementia. Additionally, studies assessing specific cognitive domains, such as attention or visuospatial ability exclusively, rather than cognitive state, were also excluded to reduce heterogeneity.
Predictor-related criteria
Both diagnostic and dimensional measures of depression and anxiety at baseline assessment were judged as eligible. Studies with retrospective assessments of affective problems were excluded, as such assessments may be less reliable. Both binary indicators of affective problems, defined as either a diagnosis or as a score above a threshold level, or continuous symptoms scores, as assessed by a validated scale of affective problems were included in this review.
Screening procedure
All articles identified through our search strategy were screened for eligibility using a three-step process. All references were first reviewed by title. Next, the remaining references were screened by abstract. Finally, all remaining articles were read in full and final eligibility determinations were made on this basis. All articles were reviewed for inclusion by one rater, and 10% of all articles were additionally screened by an independent rater, in order to assess the consistency of screening. Any disagreements were resolved during consensus meetings.
Data extraction
Data from the relevant articles were extracted using a detailed coding form. Information extracted included: Study information (Authors, publication year, DOI); Sample information (Country, mean age at baseline, gender composition, ethnicity, year of data collection, number of follow-ups, time between lags, total length of follow-up, sample size at baseline, sample size at final follow-up); Instrument information (Type of affective problem, measure used to assess affective problem, measure used to assess decline in cognitive state); Statistical information (Statistical test used, effect sizes, covariates adjusted for in statistical model). Where results for more than one follow-up were reported, the longest follow-up was selected for our analysis, as longer follow-up times allow a greater period for the decline in cognitive state to occur. Similarly, where multiple models were reported with various adjustments made, the most conservative model (with the greatest amount of adjustments) was selected. In cases where insufficient statistical information was available, original authors were contacted directly via email. All studies were evaluated for methodological quality using STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines (Elm et al., 2007).
Statistical analysis and data synthesis
All analyses were conducted in R Studio (Studio, 2012), using the metafor package. Separate meta-analyses were run for studies in which affective problems were assessed as a binary predictor (using a defined threshold), and studies where affective problems were assessed as a continuous predictor (using a symptom score). In addition, separate analyses were conducted for studies that used depression or anxiety as predictors of decline in cognitive state.
Odds ratios (ORs) were used as a common effect size across studies with a binary measure of affective problems. When ORs were not reported in original studies, these were estimated from available data using standard computational techniques (Lipsey and Wilson, 2000; Borenstein et al., 2009; Field and Gillett, 2010). Log ORs were then computed for subsequent analysis. Standardised regression coefficients were used as a common effect size across studies with a continuous measure of affective problems. If unstandardised effect sizes were reported, or measures were not standardised to a z score before analysis, coefficients were converted to standardised coefficients using standard computational methods (Kim and Ferree, 1981; Duncan, 2014). In cases where insufficient information was reported in the study to calculate the standardised coefficients, authors were contacted directly via email. We also converted the estimated regression coefficients into ORs to facilitate the comparison with the analyses using a binary predictor of depression.
Multi-level meta-analyses were conducted to account for multiple effect sizes within studies (Van Den Noortgate and Onghena, 2003). Heterogeneity across studies was assessed using the Q statistic, with p < 0.1 suggesting significant heterogeneity between studies, and the I2 statistic, in which 25, 50 and 75% represent low, medium and high heterogeneity (Higgins et al., 2003).
Additional meta-regression analyses were also conducted to assess the effects of potential moderators, including the length of follow-up, age of sample at baseline, publication year, method of affective problem assessment (diagnosis or self-report) and quality of studies. All moderators were entered initially as continuous variables, except for the assessment method of affective problems which was coded as a binary variable. For significant moderators, binary variables were created using the average values and sub-group analyses were run using these variables.
Publication bias was assessed using Begg's funnel plot and Begg's rank correlation test (Richard and Pillemer, 1984; Song et al., 2000; Egger et al., 2008).
Results
Literature search
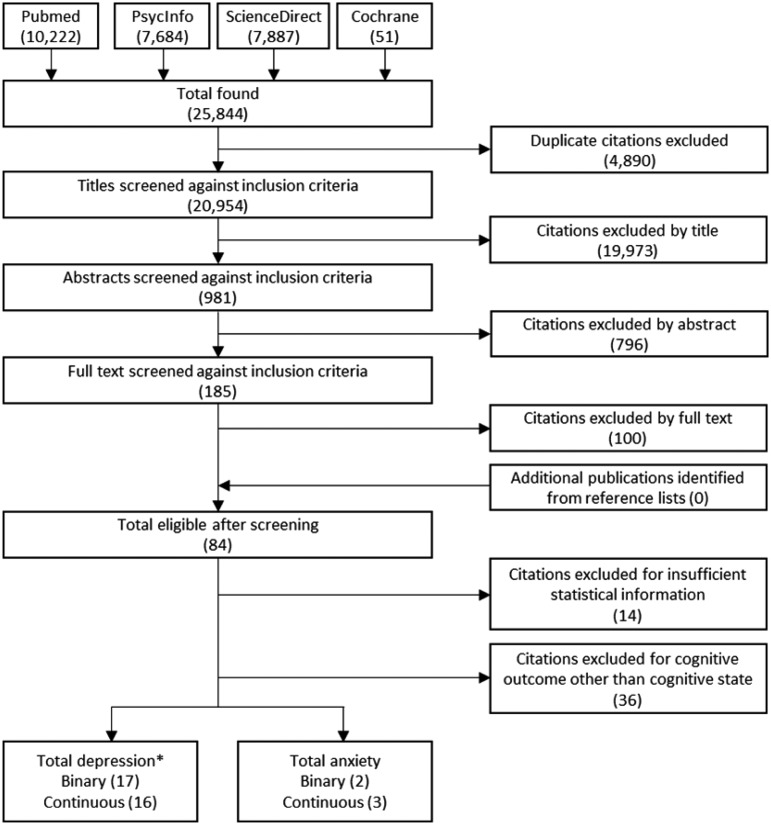
Our search identified 25 844 references. After exclusion of duplicates, 20 954 unique citations remained. At stage 1, citations were screened by title and 981 were determined to be eligible (inter-rater reliability = 96%). In stage 2, remaining citations were screened by abstract and 185 were judged as relevant (inter-rater reliability = 91%). Finally, all 185 citations were selected for full-text screening, after which 84 references remained (inter-rater reliability = 94%). At this stage, a further 36 studies were excluded, as they were addressing the decline in specific cognitive outcomes, rather than cognitive state. Of the 48 studies remaining, initially there were 18 with insufficient information for calculation of effect sizes. Authors were contacted directly by email about this and four (22%) responded to provide the relevant information. This left a total of 34 studies with sufficient information to calculate effect sizes, with 32 studies investigating the link between depression and a decline in cognitive state (n = 68 793), and five studies investigating anxiety and decline in cognitive state (n = 4698; Fig. 1 and Table 2).
Fig. 1.
Flowchart of selection.
Note: *One study assessed both binary and continuous assessments of depression, meaning that although there are 17 studies using binary measures of depression and 16 studies using continuous measures of depression, in total there are only 32 studies reporting on depression and cognitive decline.
Table 2.
Studies included in the systematic literature review and meta-analyses
| Study ID | Author | Year | Country | % Female | Mean age at baseline | Mean length of follow-up | Measure of cognition | Type of affective problem | Measure of affective problem |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Bassuk | 1998 | USA | 63 | 73.72 | 12 | Short Portable Mental Status Questionnaire (SPMSQ) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 2 | Brodaty | 2012 | Australia | 59 | 78.41 | 2 | Mean of other cognitive domain scores | Depression | Neuropsychiatric Inventory |
| 2 | Brodaty | 2012 | Australia | 59 | 78.41 | 2 | Mean of other cognitive domain scores | Anxiety | Neuropsychiatric Inventory |
| 3 | Chang | 2015 | Taiwan | 49 | 63.34 | 4 | Short Portable Mental Status Questionnaire (SPMSQ) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 4 | Downer | 2016 | USA | 58 | 73.18 | 14 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 5 | Dufouil | 1996 | France | 60 | 74.78 | 3 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 6 | Ganguli | 2006 | USA | 61 | 74.60 | 12 | Mini Mental state Examination (MMSE) | Depression | Modified Center for Epidemiologic Studies Depression Scale (CES-D) |
| 7 | Geerlings | 2000 | The Netherlands | 51 | 69.39 | 3 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) (>16 vs. <16) |
| 8 | Han | 2008 | Canada | 66 | 79.11 | 1 | Mini Mental state Examination (MMSE) | Depression | Hamilton Depression Rating Scale (HDRS) |
| 9 | Kohler | 2010 | The Netherlands | 48 | 69.40 | 6 | Mini Mental state Examination (MMSE) | Depression | Revised 90-item version of the Symptom Checklist (SCL-90) |
| 10 | Niti | 2009 | Singapore | 64 | 65.40 | 1.5 | Mini Mental state Examination (MMSE) | Depression | Chinese version of the 15 item Geriatric Depression Scale (GDS) |
| 11 | Paterniti | 2002 | France | 43 | 64.96 | 4 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 12 | Raji | 2007 | USA | 59 | 72.70 | 7 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 13 | Reyes-Ortiz | 2008 | USA | 57 | 72.70 | 11 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 14 | Rosenblatt | 2003 | USA | 63 | 40.30 | 11.5 | Mini Mental state Examination (MMSE) | Depression | Diagnostic Interview Schedule (DIS) |
| 15 | Sawyer | 2012 | USA | 69 | 70.18 | 4 | Mini Mental state Examination (MMSE) | Depression | Duke Depression Evaluation Schedule (DDES) |
| 16 | Sinoff | 2003 | Israel | 63 | 77.64 | 3.1 | Mini Mental state Examination (MMSE) | Anxiety | Sinoff's Short Anxiety Screening Test (SAST) |
| 17 | Wilson | 2016 | USA | 74 | 76.30 | 8 | Battery of 19 cognitive performance tests | Depression | Subset of questions from the Diagnostic Interview Schedule |
| 18 | Yaffe | 1999 | USA | 100 | 72.94 | 4 | Mini Mental state Examination (MMSE) | Depression | Geriatric Depression Scale (GDS) |
| 19 | Bierman | 2008 | The Netherlands | 53 | 69.49 | 9 | Mini Mental state Examination (MMSE) | Anxiety | Hospital Anxiety and Depression Scale-Anxiety (HADS-A) |
| 20 | Bunce | 2012 | Australia | 49 | 76.55 | 12 | Mini Mental state Examination (MMSE) | Depression | Goldberg Depression Scale |
| 20 | Bunce | 2012 | Australia | 49 | 76.55 | 12 | Mini Mental state Examination (MMSE) | Anxiety | Goldberg Anxiety Scale |
| 21 | Chen | 2016 | Taiwan | 45 | 70.95 | 14 | Short Portable Mental Status Questionnaire (SPMSQ) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 22 | Chiao | 2016 | Taiwan | 57 | 71.04 | 14 | Short Portable Mental Status Questionnaire (SPMSQ) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 23 | Dotson | 2008 | USA | 40 | 75.38 | 4.4 | Mini Mental State Exam (MMSE), and Blessed Information Memory and Concentration Scale (BIMCS) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 24 | Gale | 2012 | England | 55 | 64.07 | 6 | Principal components analyses of 5 cognitive outcomes | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 25 | Geerlings | 2000 | The Netherlands | 51 | 69.39 | 3 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) score (per point increase) |
| 26 | Han | 2006 | Canada | 66 | 79.11 | 1 | Mini Mental state Examination (MMSE) | Depression | HDRS |
| 27 | Johnson | 2013 | USA | 69 | 73.50 | 2 | Mini Mental state Examination (MMSE) & Clinical Dementia Rating (CDR-SB) | Depression | Geriatric Depression Scale (GDS30) |
| 28 | Neubauer | 2013 | Germany | 60 | 75.70 | 1 | Mini Mental state Examination (MMSE) and Syndrome Short Test (SKT) | Depression | Geriatric Depression Scale (GDS30) |
| 29 | Panza | 2009 | Italy | 36 | 71.90 | 3.5 | Mini Mental state Examination (MMSE) | Depression | Italian version of the Geriatric Depression Scale (GDS) |
| 30 | Rajan | 2014 | USA | 63 | 72.41 | 9 | Cognitive battery of four tests | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 31 | Royall | 2013 | Japan, Hawaii, and the mainland-US | 77.80 | 10 | Cognitive Abilities Screening Instrument (CASI) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) | |
| 32 | Turner | 2015 | USA | 70 | 73.90 | 5 | Measure derived from 19 cognitive tests | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) & Geriatric Depression Scale (GDS) |
| 33 | Van den Kommer | 2013 | The Netherlands | 53 | 69.25 | 13 | Mini Mental state Examination (MMSE) | Depression | Center for Epidemiologic Studies Depression Scale (CES-D) |
| 34 | Vinkers | 2004 | The Netherlands | 63 | 85.00 | 4 | Mini Mental state Examination (MMSE) | Depression | Geriatric Depression Scale (GDS) |
| 35 | Wilson | 2011 | USA | 76 | 80.70 | 3.4 | Derived from 19 cognitive tests | Depression | 48-item Neuroticism scale from the NEO Personality Inventory-Revised. Depression sub-scale |
| 35 | Wilson | 2011 | USA | 76 | 80.70 | 3.4 | Derived from 19 cognitive tests | Anxiety | 48-item Neuroticism scale from the NEO Personality Inventory-Revised. Anxiety sub-scale |
Depression studies
Of the depression studies, 17 used a binary measure of depression (k = 34) and 16 measured depression as a continuous variable (k = 36). Depression studies had a mean follow-up length of approximately 6.61 years (s.d. = 4.41). The mean age of participants was 72.15 at baseline (s.d. = 7.56) and the gender composition of the sample was approximately 59.48% female. The majority of studies took place in the USA (n = 14), followed by the Netherlands (n = 4) and Taiwan (n = 3). Studies also took place in Australia, Canada, France (n = 2 for each), Germany, England, Italy, Singapore and Japan, Hawaii and the mainland-USA (n = 1 for each). Overall, the majority of studies used the Center for Epidemiologic Studies Depression Scale (CES-D) to assess depression present at baseline (n = 16), followed by the Geriatric Depression Scale (GDS) (n = 7), the Diagnostic Interview Schedule (DIS) (n = 3), the Neuroticism scale from the NEO Personality Inventory, the Duke Depression Evaluation Schedule (DDES), the Goldberg Depression Scale, Neuropsychiatric Inventory, Hamilton Rating Scale for Depression (HDRS), the Symptom Checklist (n = 1 for each). Only one study reported separate effect sizes for more than one follow-up period (Bassuk et al., 1998). This study reported effect sizes at 3 years after baseline (n = 2030), 6 years after baseline (n = 1447) and 12 years after baseline (n = 756). The effect size with the longest follow-up (12 years) was selected for inclusion in the meta-analysis.
Anxiety studies
Of the five anxiety studies, two used a binary indicator of anxiety (k = 2) and three used a continuous measure of anxiety (k = 3). Anxiety studies had a mean follow-up time of 5.9 years (s.d. = 4.36). On average, participants were 76.56 years old at baseline (s.d. = 4.23) and were predominantly female (60.14% female). The majority of studies took place in Australia (n = 2), followed by the USA, the Netherlands and Israel (n = 1 for each). Anxiety was assessed using Sinoff's Short Anxiety Screening Test (SAST), Hospital Anxiety and Depression Scale-Anxiety (HADS-A), Neuropsychiatric Inventory, Goldberg Anxiety Scale and the Neuroticism scale from the NEO Personality Inventory (n = 1 for each). All anxiety studies had a score of 60% or greater on the STROBE checklist (maximum score = 81%, median score = 78%).
Depression and decline in cognitive state
Meta-analysis of studies with depression as a binary predictor
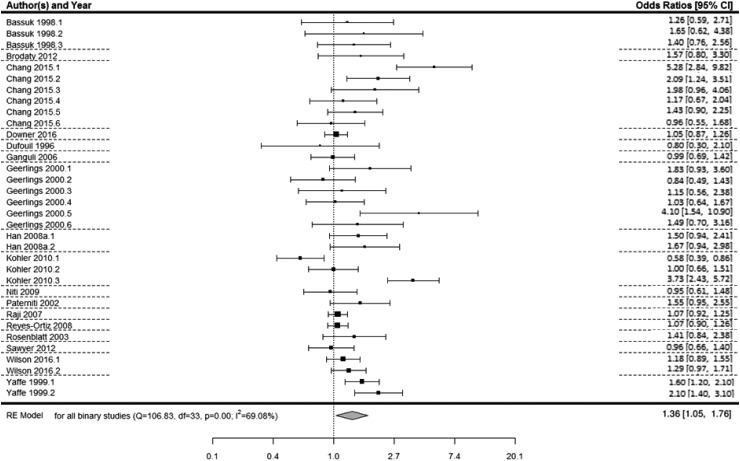
There were 34 relevant effect sizes across 17 studies with a binary measure of depression (Dufouil et al., 1996; Bassuk et al., 1998; Yaffe et al., 1999; Geerlings et al., 2000; Paterniti et al., 2002; Rosenblatt et al., 2003; Ganguli et al., 2006; Raji et al., 2007; Han et al., 2008; Reyes-Ortiz et al., 2008; Niti et al., 2009; Köhler et al., 2010; Brodaty et al., 2012; Sawyer et al., 2012; Chang and Tsai, 2015; Downer et al., 2016; Wilson et al., 2016). A multi-level meta-analysis of 34 effect sizes revealed that depression was associated with an increased risk of subsequent decline in cognitive state (OR 1.36, 95% CI 1.05–1.76, p = .02; Fig. 2).
Fig. 2.
Forest plot of the association between binary depression and decline in cognitive state*. Notes for multiple effect sizes within studies: Bassuk* (1: High SPMSQ at baseline; 2: Medium SPMSQ at baseline; 3: High or medium SPMSQ at baseline), Chang (1: Males with persistent depressive symptoms; 2: Males with increasing depressive symptoms; 3: Males with decreasing depressive symptoms; 4. Females with persistent depressive symptoms; 5: Females with increasing depressive symptoms; 6: Females with decreasing depressive symptoms), Geerlings* (1: CES-D threshold in high education sample; 2: CES-D threshold in low education sample; 3: Felt depressed some of the time v. never in high education sample; 4: Felt depressed some of the time v. never in low education sample; 5: Felt depressed most of the time v. never in high education sample; 6: Felt depressed most of the time v. never in low education sample), Han (1: Major depression v. no depression; 2: Minor depression v. no depression), Kohler (1: Low depression v. no depression; 2: Middle depression v. no depression; 3: High depression v. no depression), Wilson* (1: Major depression v. no depression; 2: Elevated depression symptoms v. no depression), Yaffe (1: 3–5 depressive symptoms v. 0–2 depressive symptoms; 2: >6 depressive symptoms v. 0–2 depressive symptoms).
* Represents effect sizes within studies where there may be some overlap in the sample.
Assessment of heterogeneity, meta-regression and sub-group analyses
Significant heterogeneity was observed across the studies with depression as a binary predictor (Q = 106.83, df = 33, p < 0.0001, I2 = 69.08%). An omnibus meta-regression analysis including publication year, mean age at baseline, length of follow-up, method of depression assessment (diagnosis or self-report) and quality of study revealed that these variables together were able to explain a significant amount of heterogeneity in the model (QM = 13.32, df = 5, p = 0.02). However, even after accounting for these factors, significant heterogeneity remained in the model (QE = 93.51, df = 28, p < 0.0001). To further explore the effect of publication year, age at baseline, length of follow-up, depression assessment and quality on heterogeneity, individual meta-regressions were conducted for each of these potential modifiers. These analyses revealed that mean age at baseline (p = 0.13), publication year (p = 0.19), quality of the study (p = 0.09) and depression assessment (p = 0.91) did not significantly explain the between-study variability.
Meta-regression analyses including the length of follow-up showed significant between-study variability, whereby studies with shorter follow-up periods had significantly greater effect sizes than studies with longer follow-up periods (B = −0.03, s.e. = 0.009, p = 0.002). Additionally, meta-regression analyses including the method of cognitive assessment (MMSE v. neuropsychiatric batteries) showed significant between-study variability (B = −0.2, s.e. = 0.08, p = 0.01). To further explore precisely how these significant factors were involved in this association sub-group meta-analyses were conducted.
To explore how length of follow-up affected the association, effect sizes were divided by the mean follow-up length in years (M = 6.35 (s.d. = 4.25) years), resulting in two groups of longer (k = 7, M = 10.79 (s.d. = 2.45) years) and shorter follow-up periods (k = 10, M = 3.25 (s.d. = 1.48) years). Multi-level sub-group meta-analyses revealed that depression was significantly associated with decline in cognitive state in studies with shorter follow-up periods (OR 1.43, 95% CI 1.03–2.00, p = 0.03) and was approaching significance in studies with longer follow-up periods (OR 1.15, 95% CI 0.98–1.36, p = 0.08). However, the overall effect size was larger for studies with shorter follow-up periods than those with longer follow-up periods. Studies with longer follow-up periods did not differ significantly from studies with shorter follow-up periods on quality (t(14.29) = 1.08, p = 0.3), publication year (t(15.38) = 0.1, p = 0.92), mean age at baseline (t(10.67) = −0.41, p = 0.69), or depression assessment (t(14.07) = −0.5, p = 0.63).
The meta-regression analysis including the method of cognitive assessment suggested that effect sizes were significantly smaller for studies using the MMSE than studies using neuropsychiatric batteries (B = −0.2, s.e. = 0.08, p = 0.01). However, there were only four studies using neuropsychiatric battery assessments of cognitive state, so results need to be treated with caution.
Meta-analysis of studies with depression as a continuous predictor
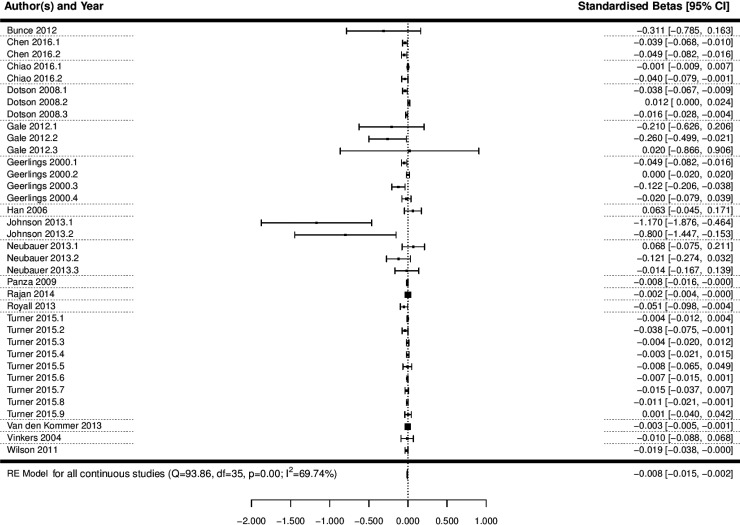
A multi-level meta-analysis of the 36 effect sizes across 16 studies with a continuous measure of depression was conducted (Geerlings et al., 2000; Vinkers et al., 2004; Han et al., 2006; Dotson et al., 2008; Panza et al., 2009; Wilson et al., 2011; Bunce et al., 2012; Gale et al., 2012; Johnson et al., 2013; Neubauer et al., 2013; Royall and Palmer, 2013; Van den Kommer et al., 2013; Rajan et al., 2014; Turner et al., 2015; Chen and Chang, 2016; Chiao and Weng, 2016). This analysis revealed that depression was significantly associated with a decline in cognitive state (B = −0.008, 95% CI −0.015 to −0.002, p = 0.012; Fig. 3; OR 0.992, 95% CI 0.985–0.998).
Fig. 3.
Forest plot of the association between continuous depression and a decline in cognitive state. Notes for multiple effect sizes within studies: Chen 2016 (1: Cognition starting high and declining; 2: Cognition starting low and declining), Chiao 2016* (1: Negative affect; 2: Lack of positive affect), Dotson 2008* (1: Baseline CES-D on MMSE; 2: Average CES-D on BIMCS; 3: Average CES-D on MMSE); Gale 2012 (1: Age 50–60; 2: Age 60–80; 3: Age 80–90), Geerlings 2000* (1: CES-D Score per point increase, education >8 years; 2: CES-D Score per point increase, education < 8 years; 3: Negative affect score per point increase, education >8 years; 4: Negative affect score per point increase, education <8 years), Johnson 2013* (1: MMSE; 2: CDR-SB), Neubauer 2013* (1: Depression at T1 predicting cognition change from T1 to T2; 2: Depression at T2 predicting cognition change from T2 to T3; 3: Depression at T3 predicting cognition change from T3 to T4), Turner 2015* (1: CES-D; 2: CES-D Positive affect; 3: CES-D Negative affect; 4: CES-D Somatic complaints; 5: CES-D Interpersonal problems; 6: GDS; 7: GDS Positive affect; 8: GDS Negative affect; 9: GDS Positive and negative affect).
* Represents effect sizes within studies where there may be some overlap in the sample.
Assessment of heterogeneity and meta-regression analyses
Significant heterogeneity was observed across studies with depression as a continuous predictor (Q = 93.86, df = 35, p < 0.0001, I2 = 69.74%). In order to try and explain some of this heterogeneity, an omnibus meta-regression analysis was conducted, including mean age at baseline, length of follow-up, quality and publication year as potential moderators. This analysis revealed that together these variables were not able to explain a significant amount of the heterogeneity in the model (QM = 8.97, df = 4, p = 0.06), but even after accounting for these factors, significant heterogeneity remained within the model (QE = 84.9, df = 31, p < 0.0001). In order to explore the influence of age at baseline, follow-up length, quality and publication year in more depth, individual meta-regressions were conducted for each potential modifier. These analyses revealed that mean age at baseline (p = 0.27), length of follow-up (p = 0.1), publication year (p = 0.18), method of cognitive assessment (p = 0.47) and quality (p = 0.11) could not significantly explain between-study variability individually.
Publication bias
Publication bias is unlikely for meta-analyses of depression studies measured as a continuous variable, as Begg's rank correlation test was non-significant (p = 0.07). Begg's funnel plot also appears relatively symmetrical (online Supplementary Fig. S1). There may have been some publication bias present in the meta-analysis of studies with depression as a binary predictor, as although Begg's funnel plot appears symmetrical (online Supplementary Fig. S1), Begg's rank correlation test was significant (p = 0.02). Results should, therefore, be interpreted with caution.
Anxiety and decline in cognitive state
Due to the limited number of studies with anxiety which met our inclusion criteria, meta-analyses for these studies were not possible. Instead, these studies are described in the form of a narrative review. Of the five relevant anxiety studies, two used a binary indicator of anxiety (Sinoff and Werner, 2003; Brodaty et al., 2012) and three used a continuous measure of anxiety (Bierman et al., 2008; Wilson et al., 2011; Bunce et al., 2012).
Two of these studies reported that anxiety was a significant predictor of decline in cognitive state (Sinoff and Werner, 2003; Wilson et al., 2011). Specifically, Sinoff and Werner, 2003 reported that in a sample of 100 people, anxiety (assessed using Sinoff's Short Anxiety Screening Test – SAST) had a strong direct and indirect effect on predicting future decline in cognitive state over 3.2 years (B = 0.23, 95% CI −0.03 to –3.95, p < 0.05). Similarly, Wilson et al. (2011) found that in 785 older adults, higher levels of anxiety symptoms (assessed using the anxiety sub-scale from the 48-item Neuroticism scale) were significantly associated with more rapid decline in cognitive state over a 3.4-year period (B = −0.003, s.e. = 0.001, p = 0.01).
Conversely, three of the eligible studies found no association between anxiety symptoms and a decline in cognitive state (Bierman et al., 2008; Brodaty et al., 2012; Bunce et al., 2012). Bierman et al. (2008) found no evidence that anxiety (assessed using the anxiety sub-scale from the Hospital Anxiety and Depression Scale – HADS-A) predicted a linear decline in cognitive state in a sample of 2351 people over a period of 9 years. Instead, a significant negative quadratic trend for cognition was reported. The authors state that this is suggestive of a curvilinear association between anxiety levels and cognitive performance. Specifically, milder anxiety symptoms may be associated with an improvement on the MMSE until it reaches an optimal level, beyond which the beneficial influence reduces, so more severe anxiety is related to poorer cognitive function. The authors posit that the Yerkes and Dodson law regarding the association between arousal and cognitive performance (Yerkes and Dodson, 1908; Mendl, 1999) may also apply to anxiety symptoms. Brodaty et al. (2012) found that in a sample of 480 non-impaired people, the odds of decline in global cognitive state over a period of 2 years were not significantly higher for participants with anxiety (assessed using Neuropsychiatric Inventory) at baseline than those without (OR 1.63, 95% CI 0.5–5.8, p = 0.45). They did, however, find a significant effect of anxiety at baseline on the decline in executive function (OR 3.54, 95% CI 1.3–9.9, p = 0.016). Finally, Bunce et al. (2012) found no evidence that anxiety (assessed using the Goldberg Anxiety Scale) affected change in cognitive state over a period of 12 years in a sample of 836 community-dwelling individuals over the age of 70 (B = −0.14, s.e. = 0.19, p = 0.46).
Discussion
The aim of the current study was to systematically investigate associations between affective problems (depression and anxiety) present at baseline and subsequent decline in cognitive state. Our findings revealed that individuals with depression (measured as a binary or continuous predictor) were at an increased risk of a greater decline in cognitive state. These findings are consistent with previous reviews which have indicated an association between affective problems and development of dementia (Jorm, 2001; Ownby et al., 2006; Byers and Yaffe, 2011; da Silva et al., 2013; Bennett and Thomas, 2014; Cherbuin et al., 2015; Gulpers et al., 2016). Our results extend these findings by linking affective problems to a greater decline in cognitive state in samples without dementia at baseline.
Strengths and limitations
Several limitations of the current study must be acknowledged. They are subject to the limitations of the included studies. Our analyses suggest that there are several key methodological differences between studies which significantly affect the results produced. For example, our results suggest that effects may differ based on length of follow-up. As shown, this is unrelated to differences in publication year, age at baseline, or method of depression assessment (self-report or diagnosis). It is possible that this is more likely attributable to additional unobserved heterogeneity.
This review only included studies of decline in cognitive state as an outcome. For this reason, it is not clear whether affective problems may differentially influence decline in different cognitive domains. Additionally, the majority of included studies assessed cognitive state using the MMSE. This measure has been criticised for lacking sensitivity to subtle changes in cognition and for ceiling and floor effects (Tombaugh and McIntyre, 1992). Consistent with this, the meta-analysis of studies using depression as a binary predictor revealed that effect sizes are significantly smaller for studies using the MMSE than studies using neuropsychiatric batteries. It is therefore possible that the widespread use of the MMSE may have resulted in an underestimation of the association between affective disorders and decline in cognitive state in healthy older adults over time. One further limitation is that excluding cognitive impairment and dementia at baseline does not completely rule out the possibility of reverse causality.
Beyond this, included studies used different approaches and instruments to assess affective problems. Research suggests that there is low overlap among different scales of depression and anxiety, with content analysis suggesting that different types of assessments may capture different symptoms (Fried, 2017). It is therefore possible that studies included in this review are not entirely comparable on the basis that the methods of assessing depression are heterogeneous and may each be capturing different kinds of symptoms. Beyond this, there were also very few studies which met our inclusion criteria which examined the association between anxiety and decline in cognitive state, meaning that a quantitative meta-analysis was not possible. Moreover, an additional limitation is that as there were no studies investigating comorbidity between anxiety and depression. Finally, many of the studies did not report separate effect sizes for different types of symptoms of affective problems (e.g. negative affect symptoms, somatic symptoms, etc.), meaning we could not look at how different symptoms of affective problems may influence decline in cognitive state in the current study.
Plausible mechanisms
Three major hypotheses have been proposed to explain this observed association. The first states that affective problems may act as an aetiological risk factor for the subsequent decline in cognitive state, perhaps by lowering the threshold for manifesting decline (Butters et al., 2008; Bennett and Thomas, 2014). The second hypothesis proposes that affective problems may act as a prodromal feature of dementia. Specifically, affective problems may manifest as an early clinical presentation of this disorder. Affective problems and decline in cognitive state may therefore be different symptoms of the same underlying condition (Panza et al., 2010; Bennett and Thomas, 2014). The third hypothesis posits that affective problems and decline in cognitive state are separate processes but may share common risk factors and underlying neurobiological substrates (Djernes, 2006; Enache et al., 2011; Bennett and Thomas, 2014). These hypotheses are not necessarily mutually exclusive and it is likely that multiple pathways and mechanisms underlie this relationship.
There are several biological and behavioural pathways which may be involved in the association between affective problems and decline in cognitive state. These include vascular disease, increased cortisol production leading to atrophy of the hippocampus (Geerlings and Gerritsen, 2017), increased deposition of β-amyloid plaques (Byers and Yaffe, 2011), inflammatory changes (Byers and Yaffe, 2011) and a decline in the levels and activities of neurotrophic factors (Royall et al., 2017). A multiple pathways model has also been proposed by Butters et al. (2008), which posits that depression-associated cerebrovascular disease and glucocorticoid neurotoxicity may operate to decrease levels of brain and cognitive reserve, as well as interact with pathology of Alzheimer's disease, giving rise to the clinical manifestation of Alzheimer's disease and accelerated cognitive decline. Additional potential lifestyle and behavioural pathways associated with affective problems include educational attainment, social support, early life adversity and health behaviours such as exercise regime, alcohol consumption, smoking status and medication status. It is more likely that a complex interaction of biological and sociobehavioural mechanisms are involved in linking affective problems with cognitive decline, rather than one single aetiological determinant (da Silva et al., 2013).
Implications and future directions
Future research should focus on investigating whether effective treatment and management of affective problems may reduce risk of decline in cognitive state. Additionally, future reviews could focus on how affective problems are associated with decline in specific cognitive domains, such as memory, executive function and information processing speed. This information can help to elucidate the pattern of decline characteristic of individuals with a history of affective problems. The present review could not address the issue of comorbidity between depression and anxiety and how comorbidity is associated with subsequent decline in the mental state. Indeed, comorbidity of depression and anxiety disorders is common. It is estimated that around 50–60% of individuals who have experienced depression also have a history of anxiety disorder (Kessler et al., 1996; Fava et al., 2000). Additionally, it is believed that comorbidity of anxiety and depression may be related to higher symptom severity and persistence, as well as poorer functional outcomes (Angst et al., 1999; Roy-Byrne et al., 2000). For this reason, it is important for future research to address how comorbid depression and anxiety is associated with future cognitive decline, and whether comorbidity of these conditions may result in poorer cognitive outcomes than depression or anxiety in isolation. One additional question which remains unresolved is whether affective problems act as a risk factor for the accelerated decline in cognitive state or whether they are an early biomarker representing prodromal dementia. While we excluded studies where cognitive impairment was present at baseline, it is also known that dementia has a preclinical period of many decades (Sperling et al., 2011). It is therefore possible that participants in included studies may have already built up substantial dementia pathology at baseline, even if cognitive symptoms were not yet apparent. Associations could therefore be due to reverse causality from subtle cognitive changes short of dementia. Future research should focus on distinguishing more clearly between these possibilities.
As average life expectancy lengthens and rapid demographic ageing occurs in populations worldwide, there is a dramatic predicted increase in the number of older adults living in our society (Oeppen and Vaupel, 2002; Lutz et al., 2008). By 2030, it is estimated that approximately one in five people in England will be over the age of 65 (House of Lords, 2013). Given the predicted increase in population size of adults over the age of 65, as well as the poor outcomes and economic costs associated with a decline in cognitive state and impairment, it is important to identify life course risk factors for poorer late-life cognitive outcomes, for potential early intervention. These findings may have value in identifying individuals who may be at a greater risk of deterioration in cognitive function over time. It is possible that effective management and treatment of depression may reduce risk and improve cognitive outcomes within these individuals. However, there has also been some evidence to suggest there may be persisting neurocognitive disturbances even after remission of depression (Frasch et al., 2000; Weiland-Fiedler et al., 2004; Paelecke-Habermann et al., 2005). Additionally, cognition may be an important treatment target for depression (Kaser et al., 2017). Due to the high prevalence of depression in the population, these results are of great public health importance.
In conclusion, demographic ageing is occurring rapidly worldwide and the number of people living with dementia is expected to grow substantially in prevalence over the next thirty years. As such, focussing research on potentially modifiable life-course risk factors, such as affective problems, is of increasing importance. This review highlights the importance of affective problems, particularly depression, in this context.
Acknowledgements
We would like to thank all the authors of the work included in the current review, and all the participants who took part in these studies.
Financial support
This project was supported by the Economic and Social Research Council (ESRC). Grant Number: ES/J500173/1
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291718001137.
click here to view supplementary material
References
- Agüero-Torres H et al. (2002) The impact of somatic and cognitive disorders on the functional status of the elderly. Journal of Clinical Epidemiology 55(10), 1007–1012. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS and Abrams RC (1991) Depression in Alzheimer's disease. Psychiatric Clinics of North America. [PubMed]
- Arve S et al. (1999) Coexistence of lowered mood and cognitive impairment of elderly people in five birth cohorts. Aging (Milan, Italy) 11(2), 90–95. [PubMed] [Google Scholar]
- Anstey KJ and Low LF (2004) Normal cognitive changes in aging. Australian Family Physician 33(10), 783. [PubMed] [Google Scholar]
- Bassuk SS, Berkman LF and Wypij D (1998) Depressive symptomatology and incident cognitive decline in an elderly community sample. Archives of General Psychiatry 55(12), 1073–1081. [DOI] [PubMed] [Google Scholar]
- Bennett S and Thomas AJ (2014) Depression and dementia: cause, consequence or coincidence? Maturitas 79(2), 184–190. [DOI] [PubMed] [Google Scholar]
- Bierman EJ et al. (2008) Anxiety symptoms and cognitive performance in later life: results from the longitudinal aging study Amsterdam. Aging and Mental Health 12(4), 517–523. [DOI] [PubMed] [Google Scholar]
- Borenstein M et al. (2009) Introduction to Meta-Analysis. Chichester, UK: John Wiley & Sons, Ltd. [Google Scholar]
- Brailean A et al. (2017) Longitudinal associations between late-life depression dimensions and cognitive functioning: a cross-domain latent growth curve analysis. Psychological Medicine 47(4), 690–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodaty H et al. (2012) Neuropsychiatric symptoms in older people with and without cognitive impairment. Journal of Alzheimer's Disease 31(2), 411–420. [DOI] [PubMed] [Google Scholar]
- Bunce D et al. (2012) Depression, anxiety and cognition in community-dwelling adults aged 70 years and over. Journal of Psychiatric Research 46(12), 1662–1666. [DOI] [PubMed] [Google Scholar]
- Butters MA et al. (2008) Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues in Clinical Neuroscience 10(3), 345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL and Yaffe K (2011) Depression and risk of developing dementia. Nature Reviews Neurology 7(6), 323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang SL and Tsai AC (2015) Gender differences in the longitudinal associations of depressive symptoms and leisure-time physical activity with cognitive decline in ⩾ 57year-old Taiwanese. Preventive Medicine 77, 68–73. [DOI] [PubMed] [Google Scholar]
- Chen TY and Chang HY (2016) Developmental patterns of cognitive function and associated factors among the elderly in Taiwan. Scientific Reports 6, 33486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherbuin N, Kim S and Anstey KJ (2015) Dementia risk estimates associated with measures of depression: a systematic review and meta-analysis. BMJ Open 5(12), e008853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiao C and Weng LJ (2016) Mid-life socioeconomic status, depressive symptomatology and general cognitive status among older adults: inter-relationships and temporal effects. BMC Geriatrics 16(1), 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark L, Chamberlain SR and Sahakian BJ (2009) Neurocognitive mechanisms in depression: implications for treatment. Annual Review of Neuroscience 32, 57–74. [DOI] [PubMed] [Google Scholar]
- Da Silva J et al. (2013) Affective disorders and risk of developing dementia: systematic review. The British Journal of Psychiatry 202(3), 177–186. [DOI] [PubMed] [Google Scholar]
- Djernes JK (2006) Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatrica Scandinavica 113(5), 372–387. [DOI] [PubMed] [Google Scholar]
- Dotson VM, Resnick SM and Zonderman AB (2008) Differential association of concurrent, baseline, and average depressive symptoms with cognitive decline in older adults. The American Journal of Geriatric Psychiatry 16(4), 318–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downer B et al. (2016) Effects of comorbid depression and diabetes mellitus on cognitive decline in older Mexican Americans. Journal of the American Geriatrics Society 64(1), 109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dufouil C et al. (1996) Longitudinal analysis of the association between depressive symptomatology and cognitive deterioration. American Journal of Epidemiology 144(7), 634–641. [DOI] [PubMed] [Google Scholar]
- Duncan OD (2014) Introduction to Structural Equation Models. Elsevier, New York. [Google Scholar]
- Egger M, Davey-Smith G and Altman D (eds). (2008) Systematic Reviews in Health Care: Meta-Analysis in Context. John Wiley & Sons, London. [Google Scholar]
- Elm EV et al. (2007) Policy and practice-The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bulletin of the World Health Organization 85(11), 867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enache D, Winblad B and Aarsland D (2011) Depression in dementia: epidemiology, mechanisms, and treatment. Current Opinion in Psychiatry 24(6), 461–472. [DOI] [PubMed] [Google Scholar]
- Esslinger C et al. (2011) Cognitive state and connectivity effects of the genome-wide significant psychosis variant in ZNF804A. Neuroimage 54(3), 2514–2523. [DOI] [PubMed] [Google Scholar]
- Fava M et al. (2000) Anxiety disorders in major depression. Comprehensive Psychiatry 41(2), 97–102. [DOI] [PubMed] [Google Scholar]
- Field AP and Gillett R (2010) How to do a meta-analysis. British Journal of Mathematical and Statistical Psychology 63(3), 665–694. [DOI] [PubMed] [Google Scholar]
- Frasch K et al. (2000) Do cognitive deficits in depressive disorders remit? Psychiatrische Praxis 27(6), 291–295. [PubMed] [Google Scholar]
- Fried EI (2017) The 52 symptoms of major depression: lack of content overlap among seven common depression scales. Journal of Affective Disorders 208, 191–197. [DOI] [PubMed] [Google Scholar]
- Gale CR, Allerhand M and Deary IJ (2012) Is there a bidirectional relationship between depressive symptoms and cognitive ability in older people? A prospective study using the English longitudinal study of ageing. Psychological Medicine 42(10), 2057–2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguli M et al. (2006) Depressive symptoms and cognitive decline in late life: a prospective epidemiological study. Archives of General Psychiatry 63(2), 153–160. [DOI] [PubMed] [Google Scholar]
- Geerlings MI and Gerritsen L (2017) Late-life depression, hippocampal volumes, and HPA-axis regulation. A systematic review and meta-analysis. Biological Psychiatry 82, 339–350. [DOI] [PubMed] [Google Scholar]
- Geerlings MI et al. (2000) Depression and risk of cognitive decline and Alzheimer's disease. The British Journal of Psychiatry 176(6), 568–575. [DOI] [PubMed] [Google Scholar]
- Gill TM, Hardy SE and Williams CS (2002) Underestimation of disability in community-living older persons. Journal of the American Geriatrics Society 50(9), 1492–1497. [DOI] [PubMed] [Google Scholar]
- Gill TM et al. (1996) Impairments in physical performance and cognitive status as predisposing factors for functional dependence among nondisabled older persons. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 51(6), M283–M288. [DOI] [PubMed] [Google Scholar]
- Gulpers B et al. (2016) Anxiety as a predictor for cognitive decline and dementia: a systematic review and meta-analysis. The American Journal of Geriatric Psychiatry 24(10), 823–842. [DOI] [PubMed] [Google Scholar]
- Han L et al. (2006) The temporal relationship between depression symptoms and cognitive functioning in older medical patients—prospective or concurrent? The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 61(12), 1319–1323. [DOI] [PubMed] [Google Scholar]
- Han L et al. (2008) 12-month cognitive outcomes of major and minor depression in older medical patients. The American Journal of Geriatric Psychiatry 16(9), 742–751. [DOI] [PubMed] [Google Scholar]
- Higgins JP et al. (2003) Measuring inconsistency in meta-analyses. BMJ: British Medical Journal 327(7414), 557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House of Lords (2013) ‘Ready for Ageing?’ Select Committee on Public Service and Demographic Change. Report of Session 2012–13. HL Paper 140. London: The Stationery Office Limited. [Google Scholar]
- Johnson LA, Hall JR and O'Bryant SE (2013) A depressive endophenotype of mild cognitive impairment and Alzheimer's disease. PLoS ONE 8(7), e68848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF (2001) History of depression as a risk factor for dementia: an updated review. Australian & New Zealand Journal of Psychiatry 35(6), 776–781. [DOI] [PubMed] [Google Scholar]
- Kaser M, Zaman R and Sahakian BJ (2017) Cognition as a treatment target in depression. Psychological Medicine 47(6), 987–989. [DOI] [PubMed] [Google Scholar]
- Kavé G et al. (2008) Multilingualism and cognitive state in the oldest old. Psychology and Aging 23(1), 70. [DOI] [PubMed] [Google Scholar]
- Kessler RC et al. (1996) Comorbidity of DSM-III—R major depressive disorder in the general population: Results from the US National Comorbidity Survey. The British journal of psychiatry. [PubMed] [Google Scholar]
- Kim JO and Ferree GD Jr (1981) Standardization in causal analysis. Sociological Methods & Research 10(2), 187–210. [Google Scholar]
- Köhler S et al. (2010) Depressive symptoms and cognitive decline in community-dwelling older adults. Journal of the American Geriatrics Society 58(5), 873–879. [DOI] [PubMed] [Google Scholar]
- Light RJ and Pillemer DB (1984) Summing up: The science of reviewing research. Cambridge, MA: Harvard University Press [Google Scholar]
- Lipsey MW and Wilson D (2000) Practical Meta-Analysis (applied social research methods). Sage publications, Thousand Oaks California. [Google Scholar]
- Lutz W, Sanderson W and Scherbov S (2008) The coming acceleration of global population ageing. Nature 451(7179), 716–719. [DOI] [PubMed] [Google Scholar]
- Mendl M (1999) Performing under pressure: stress and cognitive function. Applied Animal Behaviour Science 65(3), 221–244. [Google Scholar]
- Moher D et al. and Prisma Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6(7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moritz DJ, Kasl SV and Berkman LF (1995) Cognitive functioning and the incidence of limitations in activities of daily living in an elderly community sample. American Journal of Epidemiology 141(1), 41–49. [DOI] [PubMed] [Google Scholar]
- Morris JC (2005) Early-stage and preclinical Alzheimer disease. Alzheimer Disease and Associated Disorders 19(3), 163. [DOI] [PubMed] [Google Scholar]
- Neubauer AB, Wahl HW and Bickel H (2013) Depressive symptoms as predictor of dementia versus continuous cognitive decline: a 3-year prospective study. European Journal of Ageing 10, 37–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niti M et al. (2009) APOE-ϵ4, depressive symptoms, and cognitive decline in Chinese older adults: Singapore longitudinal aging studies. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 64(2), 306–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordin E, Rosendahl E and Lundin-Olsson L (2006) Timed “Up & Go” test: reliability in older people dependent in activities of daily living—focus on cognitive state. Physical Therapy 86(5), 646–655. [PubMed] [Google Scholar]
- Oeppen J and Vaupel JW (2002) Broken limits to life expectancy. Science 296(5570), 1029–1031. [DOI] [PubMed] [Google Scholar]
- Ownby RL et al. (2006) Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Archives of General Psychiatry 63(5), 530–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paelecke-Habermann Y, Pohl J and Leplow B (2005) Attention and executive functions in remitted major depression patients. Journal of Affective Disorders 89(1), 125–135. [DOI] [PubMed] [Google Scholar]
- Panza F et al. (2009) Temporal relationship between depressive symptoms and cognitive impairment: the Italian longitudinal study on aging. Journal of Alzheimer's Disease 17(4), 899–911. [DOI] [PubMed] [Google Scholar]
- Panza F et al. (2010) Late-life depression, mild cognitive impairment, and dementia: possible continuum? The American Journal of Geriatric Psychiatry 18(2), 98–116. [DOI] [PubMed] [Google Scholar]
- Paterniti S et al. (2002) Depressive symptoms and cognitive decline in elderly people. The British Journal of Psychiatry 181(5), 406–410. [DOI] [PubMed] [Google Scholar]
- Rajan KB et al. (2014) Gene behavior interaction of depressive symptoms and the apolipoprotein E ε4 allele on cognitive decline. Psychosomatic Medicine 76(2), 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raji MA et al. (2007) Depressive symptoms and cognitive change in older Mexican Americans. Journal of Geriatric Psychiatry and Neurology 20(3), 145–152. [DOI] [PubMed] [Google Scholar]
- Reyes-Ortiz CA et al. (2008) Church attendance mediates the association between depressive symptoms and cognitive functioning among older Mexican Americans. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 63(5), 480–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt A et al. (2003) Major depression and cognitive decline after 11.5 years: findings from the ECA study. The Journal of Nervous and Mental Disease 191(12), 827–830. [DOI] [PubMed] [Google Scholar]
- Rovner BW et al. (1989) Depression and Alzheimer's disease. The American journal of psychiatry 146(3), 350. [DOI] [PubMed] [Google Scholar]
- Royall DR and Palmer RF (2013) Alzheimer's disease pathology does not mediate the association between depressive symptoms and subsequent cognitive decline. Alzheimer's & Dementia 9(3), 318–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royall DR et al. (2017) Serum proteins mediate depression's association with dementia. PLoS ONE 12(6), e0175790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin EH et al. (1998) A prospective study of cognitive function and onset of dementia in cognitively healthy elders. Archives of Neurology 55(3), 395–401. [DOI] [PubMed] [Google Scholar]
- Sawyer K et al. (2012) Depression, hippocampal volume changes, and cognitive decline in a clinical sample of older depressed outpatients and non-depressed controls. Aging & Mental Health 16(6), 753–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinoff G and Werner P (2003) Anxiety disorder and accompanying subjective memory loss in the elderly as a predictor of future cognitive decline. International Journal of Geriatric Psychiatry 18(10), 951–959. [DOI] [PubMed] [Google Scholar]
- Sohrabi MB et al. (2008) Evaluation and comparison of cognitive state and depression in elderly admitted in sanitarium with elderly sited in personal home. Knowledge & Health 3(2), 27–31. [Google Scholar]
- Song F et al. (2000) Publication and related biases: a review. Health Technology Assessment 4(10), 1–115. [PubMed] [Google Scholar]
- Sperling RA et al. (2011) Toward defining the preclinical stages of Alzheimer's disease: recommendations from the national institute on aging-Alzheimer's association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's & Dementia 7(3), 280–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studio R (2012) RStudio: Integrated Development Environment for R. Boston, Massachusetts: RStudio Inc. [Google Scholar]
- Tabbarah M, Crimmins EM and Seeman TE (2002) The relationship between cognitive and physical performance: MacArthur studies of successful aging. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 57(4), M228–M235. [DOI] [PubMed] [Google Scholar]
- Tombaugh TN and McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. Journal of the American Geriatrics Society 40(9), 922–935. [DOI] [PubMed] [Google Scholar]
- Turner AD et al. (2015) Depressive symptoms and cognitive decline in older African Americans: two scales and their factors. The American Journal of Geriatric Psychiatry 23(6), 568–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Kommer TN et al. (2013) Depression and cognition: how do they interrelate in old age? The American Journal of Geriatric Psychiatry 21(4), 398–410. [DOI] [PubMed] [Google Scholar]
- Van Den Noortgate W and Onghena P (2003) Multilevel meta-analysis: a comparison with traditional meta-analytical procedures. Educational and Psychological Measurement 63(5), 765–790. [Google Scholar]
- Vinkers DJ et al. (2004) Temporal relation between depression and cognitive impairment in old age: prospective population based study. BMJ 329(7471), 881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L et al. (2002) Predictors of functional change: a longitudinal study of nondemented people aged 65 and older. Journal of the American Geriatrics Society 50(9), 1525–1534. [DOI] [PubMed] [Google Scholar]
- Weiland-Fiedler P et al. (2004) Evidence for continuing neuropsychological impairments in depression. Journal of Affective Disorders 82(2), 253–258. [DOI] [PubMed] [Google Scholar]
- Wilson RS et al. (2007) Chronic distress and incidence of mild cognitive impairment. Neurology 68(24), 2085–2092. [DOI] [PubMed] [Google Scholar]
- Wilson RS et al. (2011) Vulnerability to stress, anxiety, and development of dementia in old age. The American Journal of Geriatric Psychiatry 19(4), 327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS et al. (2016) Late-life depression is not associated with dementia-related pathology. Neuropsychology 30(2), 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K et al. (1999) Depressive symptoms and cognitive decline in nondemented elderly women: a prospective study. Archives of General Psychiatry 56(5), 425–430. [DOI] [PubMed] [Google Scholar]
- Yerkes RM and Dodson JD (1908) The relation of strength of stimulus to rapidity of habit-formation. Journal of Comparative Neurology 18(5), 459–482. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291718001137.
click here to view supplementary material