Abstract
Rucaparib is a potent inhibitor of poly (ADP-ribose) polymerase (PARP) PARP1, PARP2 and PARP3, and to a lesser extent, PARP4, PARP10, PARP12, PARP15 and PARP16. Study 10 and ARIEL2 evaluated the use of rucaparib as treatment in patients with recurrent high-grade ovarian carcinoma and resulting in approval of rucaparib for patients with both germline and somatic BRCA mutation. Data from the Phase III trial ARIEL3 led to approval in platinum-sensitive disease as maintenance. This article reviews the efficacy, safety, pharmacokinetics and pharmacodynamics of rucaparib as well as future and ongoing trials.
Keywords: : BRCA mutated ovarian cancer, company tests, ovarian cancer, ovarian cancer maintenance treatment, PARP, platinum sensitive ovarian cancer, poly (ADP-ribose) polymerase inhibitors, rucaparib
Ovarian cancer is the leading cause of death among gynecological tumors [1]. Even though patients are typically sensitive to treatment with taxane and platinum-based chemotherapy in the upfront setting, most will relapse. Recurrent ovarian cancer remains a clinical challenge in the natural history of the disease due to drug resistance [2–4].
Poly (ADP-ribose) polymerase (PARP) inhibitors are a new class of drugs developed initially for the treatment of ovarian cancer patients with recurrent disease and BRCA gene mutation. Previous studies have indicated the effectiveness of PARP inhibitors in the setting of platinum-sensitive ovarian cancer [5,6]. Further trials incorporated the use of a biomarker as a predictive tool to the treatment with PARP inhibitors [7,8]. Nonetheless, the biomarker chosen has not yet been sufficiently precise to predict absence of benefit on an individual basis.
Biological basis of mechanism of action of PARP inhibitors
The past decade has witnessed impressive advances in our understanding of the various cellular components required for maintenance of the genome following DNA damage.
Data from The Cancer Genome Atlas estimates that approximately 50% of high-grade serous ovarian cancers have homologous recombination deficiency (HRD), indicating that homologous recombination (HR) is an important pathway in ovarian cancer. The HR pathway allows repair of double-stranded DNA breaks. Deficiency in HR DNA repair leads to genomic instability due to loss or duplication of chromosomal regions [9].
Genetically, synthetic lethality occurs when two lesions, which are individually not lethal, become lethal when combined in a single organism (or cell). The 17-member PARP superfamily of nuclear enzymes includes PARP1, PARP2 and PARP3, which are activated by and repair single stranded DNA damage [10].
The clinical development of PARP inhibitors was possible by in vitro findings of synthetic lethality of PARP inhibition in the setting of HRD. The inhibition of PARP leads to accumulation of DNA double-strand breaks that cannot be repaired due to HRD and subsequent cell death [11].
Furthermore, PARP inhibition can interfere with other DNA repair pathways, such as the alternative nonhomologous end-joining pathway that is upregulated in HR deficient cells [12,13]. PARP inhibitors can also result in trapping of PARP1 and PARP2 at the site of the DNA break, resulting in obstructed replication forks due to the accumulation of unrepaired single-strand breaks [12,14,15].
BRCA somatic mutations & epigenetic alterations in ovarian cancer
The HRD pathway in high-grade serous ovarian cancer patients can be assessed through different mechanisms, including germline mutations, somatic mutations, promoter methylation in BRCA genes and others involved in HR DNA repair [16]. BRCA germline mutations in the population occur in about 15% of women with high-grade epithelial ovarian cancer and somatic BRCA mutations are found in another 5–7%; however, the true prevalence remains unknown [9,17,18].
The stability of BRCA1 and BRCA2 somatic mutations is an important clinical consideration. Somatic BRCA mutations may change over time due to selection through treatment, cancer evolution and the development of resistance. Intratumor heterogeneity may be predictive for survival after chemotherapy treatment in high-grade serous ovarian cancer [19]. To date, the significance of tumor heterogeneity in relation to somatic BRCA mutation and HRD status and sensitivity to PARP inhibitors is not fully known.
An analysis of samples collected from patients in ARIEL2 Part 1, the Phase II trial of rucaparib in patients with platinum-sensitive, high-grade ovarian cancer patients described below was done for sequence of HR pathway genes, with 12 pairs of pretreatment and postprogression tumor biopsy. The primary mutations in six of 12 pretreatment biopsies were a truncation mutation in BRCA1, RAD51C or RAD51D. On the other hand, secondary mutations were seen in five of six patients in the postprogression biopsies, and most common were in RAD51C and RAD51D. These results show that secondary mutations restored the open reading frame and may be a mechanism of acquired resistance to PARP inhibitors [20].
In addition to mutations, epigenetic gene alterations, such as promoter methylation, can lead to silencing of HR genes [21]. Different studies have indicated that the clinical impact of BRCA methylation is complex. Existing data are conflicting, with some publications showing a decrease in survival for patients harboring BRCA methylation in contrast with others revealing no difference in survival with the methylation status [9,22–24].
The knowledge of PARP inhibitors activity beyond BRCA germline mutations is an important advance in the treatment of ovarian cancer, as can increase the number of patients likely to benefit from this type of treatment.
Loss of heterozygosity score as a molecular biomarker of efficacy of PARP inhibitors
Clinical data with PARP inhibitors indicate that there are ovarian cancer patients that benefit from treatment with a PARP inhibitor beyond those with germline BRCA mutations. These patients have no mutation in the BRCA gene but have a deficiency in the HR pathway, a profile called BRCAness phenotype [25]. The most common are the Fanconi anemia pathway genes (RAD51C, RAD51D, RAD50, BRIP1, BARD1, CHEK2, MRE11A, NBN, PALB2) [26].
A functional assessment of the DNA repair pathways is important to select the patients for the treatment with PARP inhibitors. Whole genome sequencing allows for identification of signatures of mutational and chromosomal alterations that correlate with specific DNA repair defects. Measures of HRD have been evaluated as a novel biomarker of PARP inhibitor efficacy with the use of next-generation sequencing assays. Structural variation signatures of HRD include copy number alterations, chromosomal rearrangements, loss of heterozygosity (LOH) scores and rearrangement signatures [27]. The ARIEL 2 and 3 trials referenced below utilized Foundation Medicine's T5 next-generation sequence assay (MA, USA). This test identifies genomic LOH segments inferred across 22 autosomal chromosomes using the genome-wide aneuploidy and copy number profile and minor allele frequencies of single-nucleotide polymorphisms [8].
The Phase III switch maintenance trial of niraparib in women with platinum-sensitive recurrent ovarian cancer response to induction platinum combination therapy (NOVA trial) validated a different measure of HRD. In that study, HRD was defined using a composite of factors associated with genomic instability, including LOH, telomeric allelic imbalance and large-scale state transitions (Myriad MyChoice, UT, USA) [7].
Rucaparib in the treatment setting
Rucaparib (formerly known as CO-338, AG-14699 and PF-01367338) is a potent PARP1, PARP2 and PARP3 inhibitor, and to a lesser extent PARP4, PARP10, PARP12, PARP15 and PARP16 [28]. Preclinical studies revealed that tumors with mutated or epigenetically silenced BRCA1/2 were sensitive to rucaparib [29].
In the clinical setting of rucaparib, the oral formulation of rucaparib was first evaluated in Study 10. This was a Phase I–II trial for rucaparib, including a Phase II portion which included patients with germline BRCA1/2-mutated ovarian carcinoma or other solid tumors. The Phase I part of Study 10 determined the maximum tolerated dose (600 mg twice daily) and the pharmacokinetics of rucaparib. The Phase II part included 42 patients with platinum-sensitive, high-grade ovarian carcinoma who received two to four prior regimens, progression-free interval of 6 months or more following their most recent platinum therapy and measurable disease. The investigator-assessed overall response rate (ORR) by RECIST criteria was 59.5% and by the RECIST/GCIG CA-125 was 83.3%. Median duration of response was 7.8 months (95% CI: 5.6–10.5) [30].
According to promising results, ARIEL2, a two-part Phase II trial was developed [8]. In Part 1, the primary end point was progression-free survival (PFS) and secondary end points were ORR, duration of response, safety and pharmacokinetics. Tumor samples were analyzed to identify HRD. The biomarker chosen for HRD was genomic LOH, with a cutoff to define LOH high of ≥14%. Based on HRD, patients were classified in three subgroups: BRCA mutant (deleterious germline or somatic), BRCA wild-type and LOH high group and BRCA wild-type and LOH low group.
In this trial, 206 patients were enrolled; however, only 204 patients received rucaparib and of this, 192 were classified into three groups based on HRD status: BRCA mutant (n = 40/20.8%), BRCA wild-type and LOH high (n = 82/42.7%) and BRCA wild-type and LOH low (n = 70/36.5%). Median PFS (months; 95% CI) was: BRCA mutant (12.8; 9.0–14.7), LOH high (5.7; 5.3–7.6) and LOH low (5.2; 3.6–5.5). PFS was significantly longer in the BRCA mutant subgroup (HR: 0.27; 95% CI: 0.16–0.44; p < 0.0001) and LOH high group (HR: 0.62; 0.42–0.90; p = 0.011) compared with the LOH low group. ORR by RECIST 1.1 was 80, 29 and 10% for BRCA mutant, LOH high and LOH low, respectively. Median duration of response (months; 95% CI) was also longer in the BRCA mutant (9.2; 6.4–12.9) and LOH high population (10.8; 5.7 – not reached) compared with the LOH low group (5.6; 4.6–8.5). Review of these data enabled optimization of the degree of LOH associated with clinical efficacy and was prospectively defined for ARIEL3 and Part 2 of ARIEL2 as ≥16%. Part 2 includes patients with at least three prior chemotherapy regimens and data are not yet available (Part 2; NCT01891344) [31].
The proportion of patients who achieved a response was similar irrespective of whether the BRCA mutation was germline or somatic or whether a patient had a BRCA1 or BRCA2 mutation. Non-BRCA HR genes were analyzed from the HR pathway (ATM, ATR, BRIP1, CHEK2, FANCA, FANCI, NBN, RAD51). In addition, methylation status was evaluated in 165 of 204 patients. Promoter hypermethylation in the BRCA1 gene was seen in 21 patients (13%) and in the RAD51C gene in four (2%) patients. Confirmed responses were detected in patients with tumors with both BRCA1 and RAD51C methylation. In ARIEL 2, genomic LOH had better sensitivity for response than mutation of HR pathway genes or methylation of BRCA1 or RAD51C [8].
An integrated analysis of data from Study 10 and ARIEL 2 with 106 patients demonstrated an ORR of 53.8% (95% CI: 43.8–63.5), with a median duration of response of 9.2 months (95% CI: 6.6–11.6). Complete and partial responses were achieved in 8.5 and 45.3% patients, respectively [32].
After the ARIEL 2 trial on 19 December 2016, the US FDA approved the use of rucaparib for advanced ovarian cancer patients with deleterious BRCA mutation (germline and/or somatic) identified by an approved companion diagnostic test who have been treated with at least two chemotherapies. The agency also approved the FoundationFocus CDxBRCA test to detect BRCA alterations [33].
Rucaparib in the maintenance setting
ARIEL 3 was a randomized, double-blind, placebo-controlled trial that included patients with platinum-sensitive high-grade serous or endometrioid ovarian, primary peritoneal or fallopian tube carcinoma. All patients received at least two previous platinum-based chemotherapy regimens and achieved complete or partial response to their last platinum based regimen [34]. This trial included 564 patients who were randomized 2:1 to receive oral rucaparib 600 mg twice daily or placebo in 28-day cycles. The ARIEL 3 trial prospectively validated the next-generation sequence HRD assay used in the ARIEL 2 trial using a cutoff for high genomic LOH of ≥16%. Patients were stratified in three cohorts: BRCA mutated (carcinoma associated with a deleterious germline or somatic BRCA mutation), HRD positive (BRCA-mutated carcinoma or BRCA wild-type and high-LOH carcinomas) and the intention to treat population (all randomly allocated patients).
The median investigator-assessed PFS (months; 95% CI) in the BRCA mutant group was 16.6 (13.4–22.9), compared with placebo with 5.4 months (3.4–6.7, [HR: 0.23; 95% CI: 0.16–0.34; p < 0.0001]). The patients with HRD-positive carcinoma had a PFS of 13.6 (10.9–16.2) versus 5.4 months in the placebo (5.1–5.6; 0.32 [0.24–0.42]; p < 0·0001) and in the intention-to-treat population was 10.8 (8.3–11.4) versus 5.4 in the placebo group (5.3–5.5; 0.36 [0.30–0.45]; p < 0.0001). All subgroups had a PFS benefit for rucaparib versus placebo, irrespective of volume of disease, response to chemotherapy, status of LOH or BRCA mutation. Increase in ORR was seen in all populations with measurable disease treated with rucaparib in this trial. The ORR by RECIST 1.1 for the BRCA mutant group with rucaparib was 38% (95% CI: 23–54) versus 9% in the placebo group (95% CI: 1–28), for the BRCA wild-type HRD positive was 27% (95% CI: 18–38) versus 7% with placebo (95% CI: 2–20) and for the intention to treat population was 18% (95% CI: 12–26) versus 8% with placebo (95% CI: 3–17). The overall survival data was not mature at the time of the publication.
With data from ARIEL 3 on 6 April 2018, the FDA approved the use of rucaparib as maintenance treatment for patients with recurrent epithelial ovarian, fallopian tube or primary peritoneal cancer who are in a complete or partial response to platinum-based chemotherapy [33].
Pharmacokinetics & pharmacodynamics of rucaparib
Studies of the pharmacokinetics and human metabolism of rucaparib showed that the cytochrome P450 enzymatic pathway metabolizes rucaparib. Co-administration of rucaparib can increase the systemic exposure of CYP1A2, CYP3A, CYP2C9 or CYP2C19 substrates, which may increase the risk of toxicities of these drugs and adjust dosage of these substrates may be necessary. Some examples include caffeine (CYP1A2), midazolam (CYP3A4), warfarin (CYP2C9) and omeprazole (CYP2C19). If co-administration of warfarin cannot be avoided, consider increasing the frequency of international normalized ratio monitoring. Rucaparib can be taken with or without food. Moderate food effect on pharmacokinetics was not considered to be clinically significant. On the other hand, a high-fat meal moderately increased rucaparib exposure which may be due to increased intestinal solubility following consumption of a high-fat meal [33].
Metabolism & safety of rucaparib
Rucaparib has a manageable toxicity profile. The most common treatment-emergent adverse events (AEs) of grades 3 or 4 in Study 10 were anemia (38.1%), asthenia/fatigue (26.2%) and alanine aminotransferase and/or aspartate transferase elevations (14.3%) [30]. In the ARIEL 2 trial, rucaparib displayed a safety profile with similar toxicity to Study 10. All patients had at least one treatment-emergent AE and the most frequent AEs, grade 3 or greater, were anemia or decreased hemoglobin in 22% of patients and elevations in alanine aminotransferase and/or aspartate aminotransferase in 12% of patients [8].
ARIEL 3 showed similar results in terms of safety and tolerability. In this trial, the most common AEs in the rucaparib group were: nausea (75%), asthenia/fatigue (69%), dysgeusia (39%), anemia/decreased hemoglobin (37%), constipation (37%) and vomiting (37%). Grade 3 or 4 AEs were seen in 56% of patients in the rucaparib group. AEs leading to dose reduction were observed in 55 and 4% of patients in the rucaparib and placebo group, respectively. The most common serious AEs in the rucaparib group were anemia (4% of patients), pyrexia (2%), vomiting (2%) and small intestinal obstruction (1%). Another AE observed in ARIEL 3 that is not seen often with other PARP inhibitors was an increase in alanine aminotransferase or aspartate aminotransferase concentration in 34% of patients in the rucaparib group, and in 10% was grade 3. These alterations were generally transient, selflimiting and not associated with other signs of liver toxicity [34].
Anemia is a common side effect of PARP inhibitors. Loss of PARP-2 reduces the life of erythrocytes and impairs the differentiation of erythroid progenitors. In vivo studies showed that the deletion of PARP-2 in mice leads to chronic anemia at steady state, despite increased erythropoietin plasma levels, which revels the role of PARP-2 in erythropoiesis [35]. In the ARIEL 3 trial, anemia of any grade occurred in 37% of patients and in 19% grade 3 or greater. These results were similar to other PARP inhibitors. Anemia grade 3 or greater was seen with olaparib in 19% of patients [36] and with niraparib in 25.3% of patients. A fatal but rare AE related with PARP inhibitors is secondary malignancies, such as acute myeloid leukemia and myelodysplasic syndrome. The incidence reported is between 0.4 and 1.5% and patients that developed these diseases used PARP inhibitors for a long time and received previous DNA damaging agents, as platinum chemotherapy [7].
Another laboratory alteration that occurs in the different PARP inhibitors is increase in creatinine. In ARIEL 3, creatinine increases grade 1 or 2 were observed within the first few weeks of rucaparib treatment and then stabilized with continued rucaparib treatment. Rucaparib inhibits MATE1 and MATE2-K transporters, which have a role in the renal secretion of creatinine. It is important to note that the elevation in creatinine is rarely associated with renal dysfunction. Other PARP inhibitors, including veliparib and olaparib, have a similar interaction with these transporters [37,38].
A summary of toxicities related with rucaparib 1 and recommended dose adjustments are reported in Tables 1 & 2, respectively.
Table 1. . Toxicities reported with rucaparib in the ARIEL 3 trial.
| Toxicities, percentage of patients | Grade | Rucaparib (n = 372) | Placebo (n = 189) |
|---|---|---|---|
| Hematologic toxicities | |||
| Anemia | All | 39 | 5 |
| Grade 3/4 | 21 | 0.5 | |
| Thrombocytopenia | All | 29 | 3 |
| Grade 3/4 | 5 | 0 | |
| Neutropenia | All | 20 | 5 |
| Grade 3/4 | 8 | 1 | |
| Gastrointestinal toxicities | |||
| Nausea | All | 76 | 36 |
| Grade 3/4 | 4 | 0.5 | |
| Constipation | All | 37 | 24 |
| Grade 3/4 | 2 | 1 | |
| Vomiting | All | 37 | 15 |
| Grade 3/4 | 4 | 1 | |
| Abdominal pain | All | 46 | 39 |
| Grade 3/4 | 3 | 0.5 | |
| Diarrhea | All | 32 | 22 |
| Grade 3/4 | 0.5 | 1 | |
| Dyspepsia | All | 15 | 5 |
| Grade 3/4 | <1 | 0 | |
| Dysgeusia | All | 40 | 7 |
| Grade 3/4 | 0 | 0 | |
| Respiratory toxicities | |||
| Nasopharyngitis/upper respiratory tract infection | All | 29 | 18 |
| Grade 3/4 | 0.3 | 1 | |
| Cough | All | 15 | 13 |
| Grade 3/4 | 0 | 0 | |
| General toxicities | |||
| Fatigue | All | 73 | 46 |
| Grade 3/4 | 7 | 3 | |
| Decreased appetite | All | 23 | 14 |
| Grade 3/4 | 1 | 0 | |
| Neurologic toxicities | |||
| Headache | All | 18 | 16 |
| Grade 3/4 | 1 | 1 | |
| Insomnia | All | 14 | 8 |
| Grade 3/4 | 0 | 0 | |
| Dermatologic toxicities | |||
| Photosensitivity reaction | All | 17 | 1 |
| Grade 3/4 | 1 | 1 | |
| Pruritus | All | 13 | 10 |
| Grade 3/4 | 0 | 0 | |
| Rash | All | 43 | 23 |
| Grade 3/4 | 1 | 0 | |
| Other nonhematologic toxicities | |||
| Increase in alanine aminotransferase or aspartate aminotransferase | All | 38 | 4 |
| Grade 3/4 | 11 | 0 | |
Table 2. . Recommended dose adjustments for rucaparib.
| Dose reduction | Dose |
|---|---|
| Initial dose | 600 mg twice daily (two 300 mg tablets) |
| First dose reduction | 500 mg twice daily (two 250 mg tablets) |
| Second dose reduction | 400 mg twice daily (two 200 mg tablets) |
| Third dose reduction | 300 mg twice daily (one 300 mg tablet) |
Rucaparib & others PARP inhibitors
Additional PARP inhibitors have also been approved for the treatment of ovarian cancer. Olaparib was the first PARP inhibitor approved in the USA, as monotherapy utilizing the capsule formulation for patients with high-grade ovarian carcinoma and germline BRCA1 or 2 mutation who have received three or more prior chemotherapies [5]. The SOLO-2 trial was a Phase III study that randomized patients for olaparib or placebo as maintenance treatment of patients with high-grade serous epithelial ovarian, fallopian tube or primary peritoneal cancer with platinum-sensitive, relapsed, germline BRCA mutations who had received at least two lines of previous chemotherapy and had an objective response to platinum-based chemotherapy. The PFS was more than three times longer in the olaparib arm (19.1 months [95% CI: 16.3–25.7] vs 5.5 months [5.2–5.8]; HR: 0.30 [95% CI: 0.22–0.41]) [36]. These results, in addition to results from a trial of olaparib maintenance in all comers ovarian cancer, allowed the approval of olaparib in USA for any patient with high-grade ovarian cancer after response to last platinum-based therapy.
Niraparib is another PARP inhibitor that was evaluated as monotherapy for maintenance treatment of patients with recurrent ovarian cancer in the NOVA trial. Niraparib showed an increase in PFS in the germline BRCA mutation group of 21 months with niraparib versus 5.5 months in the placebo group (HR: 0.27; 95% CI: 0.17–0.41). The non-gBRCA cohort with HRD had also a benefit in PFS of 12.9 months versus 3.8 (HR: 0.38; 95% CI: 0.24–0.59) as the overall non-gBRCA cohort of 9.3 versus 3.9 months (HR: 0.45; 95% CI: 0.34–0.6) [7]. This agent has been FDA-approved for maintenance in any high-grade ovarian cancer after response to platinum-based therapy.
Veliparib has been evaluated for the treatment of persistent or recurrent epithelial ovarian, fallopian tube or primary peritoneal cancer in patients who carry a germline BRCA1 or BRCA2 mutation. The Phase II trial showed an ORR in platinum-resistant and platinum-sensitive patients of 20% and 35%, respectively [39]. An ongoing placebo-controlled Phase III trial in newly diagnosed ovarian cancer patients, which is combining veliparib/placebo and chemotherapy, followed by veliparib/placebo maintenance has recently completed enrolment (NCT02470585). Veliparib is still not approved by FDA.
Talazoparib is a potent PARP1/2 inhibitor. The Phase I trial in patients with germline BRCA1/2 mutations showed a confirmed response in five of 12 patients (42%) with ovarian cancer [40]. The Phase II trial recruitment was completed and results have not yet been reported (NCT01286987).
Direct comparisons are not possible between all PARP inhibitors since there are several differences in the studies. First, the inclusion criteria in SOLO2 only included patients with germline BRCA mutation, differently from NOVA and ARIEL3. The exclusion criteria for the three trials was also slightly different. In the NOVA trial, there was a requirement that in patients who had had partial response to the prior platinum-based regimen, the size of the individual tumor nodule needed to be less than 2 cm with normal levels of CA-125, compared with ARIEL3 and SOLO-2 which had no restriction on tumor size. The definition of HRD in ARIEL 2 and 3 included only LOH, whereas the HRD score proposed for the NOVA trial included the three-marker assessment of HRD. In addition, assessment of response was done by investigator assessment in the SOLO2 and ARIEL3 trials, compared with central radiologic and clinical review in the NOVA trial [7,34,36].
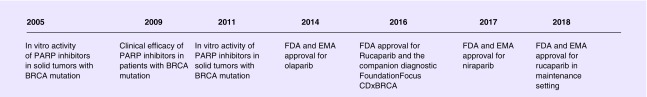
A timeline of PARP inhibitor development and approval is presented in Figure 1.
Figure 1. . Timeline of poly (ADP-ribose) polymerase inhibitor development and approval of poly (ADP-ribose) polymerase inhibitors.
EMA: European Medicines Agency; PARP: Poly (ADP-ribose) polymerase.
Future perspective & conclusion
There are unmet needs that highlight future areas of investigation of PARP inhibitors in ovarian cancer. Some questions remain regarding about the optimal duration and timing of administration of these drugs, long-term effects of PARP inhibition, mechanisms of resistance of PARP inhibitor and possible combinations that may overcome HR resistance or increase clinical efficacy. Further, the best evaluation of the dynamic changes in somatic mutations is unknown. Answers to these topics will have a profound impact on the broader clinical utility of PARP inhibitors across patients with all solid tumors.
ARIEL4 is an ongoing Phase III trial that will compare the efficacy and safety of rucaparib versus chemotherapy (monotherapy or doublet; investigator's choice) as treatment for relapsed ovarian, fallopian tube or primary peritoneal cancer with BRCA germline and/or somatic mutations who have received two or more prior lines of platinum-based chemotherapy. The physician's choice option allows for any platinum-based chemotherapy for patients with platinum-sensitive disease and weekly paclitaxel for patients with platinum-resistant or partially platinum-sensitive disease. The primary outcome is PFS and secondary outcomes include overall survival, safety and tolerability of rucaparib as compared with chemotherapy (NCT02855944). The comparison of results of ARIEL 3 and ARIEL 4 will help to further understand the ideal timing of use of rucaparib, as maintenance or treatment for patients with relapsed disease.
The combination of rucaparib and immunotherapy will also be evaluated. ATHENA is a first-line maintenance trial that will randomize patients in four arms (rucaparib in combination with nivolumab, rucaparib alone, nivolumab alone and placebo) in newly diagnosed patients with high-grade ovarian, fallopian tube or primary peritoneal cancer who have completed platinum-based chemotherapy [41]. Future areas of investigation include combination of rucaparib and other targeted therapies, like Wee1 kinase inhibitors, PI3K inhibitors; chemotherapy as DNA topoisomerase I inhibitors DNA methyltransferase inhibitors, immune checkpoint inhibitors and anti-angiogenics agents [42]. Addition studies in the platinum resistant scenario are warranted. Deeper efforts in the characterization of tumor biomarkers are ongoing, and a systemic approach will likely be necessary to better identify the patients that will better respond to therapy. The ongoing clinical trials of rucaparib in different solid tumors are presented in Table 3.
Table 3. . Select ongoing clinical trials of rucaparib in different solid tumors.
| Study | Drug | Setting | Phase |
|---|---|---|---|
| TRITON 2 NCT 02952534 |
Rucaparib | Metastatic castration-resistant prostate cancer and HRD | II |
| TRITON 3 NCT 02975934 |
Rucaparib | Metastatic castration-resistant prostate cancer and HRD | III |
| NCT03442556 | Docetaxel, carboplatin and rucaparib | Metastatic castration-resistant prostate cancer and HRD | II |
| CheckMate 9KD (NCT0333879) |
Nivolumab and rucaparib | Metastatic castration-resistant prostate cancer | II |
| NCT03413995 | Rucaparib | Metastatic castration-resistant sensitive cancer and HRD | II |
| ATLAS NCT03397394 |
Rucaparib | Metastatic urothelial carcinoma | II |
| NCT 02042378 | Rucaparib | Pancreatic cancer and a BRCA mutation | II |
| RUBY 2 NCT 02505048 |
Rucaparib | Metastatic breast cancer with a BRCAness genomic signature | II |
| NCT01074970 | Rucaparib | Triple negative breast cancer with BRCA1/2 mutations | II |
| NCT 01482715 | Rucaparib | Advanced solid tumors with BRCA mutation | I |
| NCT 03101280 | Rucaparib | Advanced gynecologic cancers and triple negative breast cancer | Ib |
| NCT 03101280 | Rucaparib and atezolizumab | Advanced gynecologic cancers and triple negative breast cancer | II |
| NCT 03476798 | Bevacizumab and rucaparib | Recurrent carcinoma of the cervix or endometrium | II |
| NCT 03337087 | Irinotecan, fluorouracil and rucaparib | Metastatic pancreatic, colorectal, gastroesophageal, or biliary cancer | I/II |
AE: Adverse event; DLT: Dose limiting toxicity; HRD: Homologous recombination deficiency; ORR: Objective response rate; PSA: Prostate specific antigen; PK: Pharmacokinetic.
In conclusion, the use of rucaparib as maintenance treatment showed increase in PFS compared with placebo in all patients with ovarian carcinoma who achieved response to platinum based chemotherapy, with manageable side effects. Further, the approval of rucaparib with a companion diagnostic test for BRCA mutation, represents an important new therapeutic option in the treatment of ovarian cancer.
Executive summary.
Overview of the drug
Rucaparib is a potent inhibitor of poly (ADP-ribose) polymerase (PARP) PARP1, PARP2 and PARP3 inhibitor, and to a lesser extent PARP4, PARP10, PARP12, PARP15 and PARP16 and is approved for patients patients with or without BRCA mutations.
The Phase II and III trials of rucaparib used as a biomarker for homologous recombination deficiency genomic loss of heterozygosity (LOH), which was quantified by the extent of LOH across the tumor genome using Foundation Medicine's T5 next-generation sequence assay (FoundationFocusC DxBRCA LOH, MA, USA).
Clinical efficacy & safety
The Phase II trial ARIEL2 Part 1 included 204 patients, and all subgroups (BRCA mutant, BRCA wild-type and LOH high and BRCA wild-type and LOH low) had an improve in overall response rate, duration of response and progression-free survival.
The Phase III trial ARIEL3 showed that the median progression-free survival in the BRCA mutant group, BRCA wild-type LOH high and in the intention to treat population was 16.6, 13.6 and 10.8 months compared with 5.4 months in the placebo group. The overall response rate was of 38, 27 and 18% in the same three cohorts, respectively, compared with placebo. The overall survival data were not mature at the time of the publication.
In the ARIEL3, the most common adverse events of any grade in the rucaparib group were: nausea (75%), asthenia/fatigue (69%), dysgeusia (39%), anemia/decreased hemoglobin (37%), constipation (37%) and vomiting (37%).
Pharmacokinetics & pharmacodynamics
Rucaparib is metabolized by cytochrome P450 enzymatic pathway and the co-administration of rucaparib can increase the systemic exposure of CYP1A2, CYP3A, CYP2C9 or CYP2C19 substrates, which may increase the risk of toxicities of these drugs.
Rucaparib can be taken with or without food although a high-fat meal moderately increased rucaparib exposure.
Acknowledgements
The authors want to thank P Morello for assistance in manuscript preparation.
Footnotes
Financial & competing interests disclosure
R Coleman is supported by CPRIT RP120214, the Ann Rife Cox Chair in Gynecology, Judy Reis/Albert Pisani and the MD Anderson ovarian cancer research fund. R Coleman has clinical research funding from Merck, AstraZeneca/Medimmune, Genentech/Roche, Novartis, Clovis Oncology, Abbvie and Janssen pharmaceuticals. Other parts of this work are supported by R35 CA209904, the Frank McGraw Memorial Chair in Cancer Research, the American Cancer Society Research Professor Award and the Blanton-Davis Ovarian Cancer Research Program. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as: •• of considerable interest
- 1.GLOBOCAN. Estimated cancer incidence, mortality and prevalence worldwide in 2012. 2012. www.globocan.iarc.fr
- 2.Pujade-Lauraine E, Wagner U, Aavall-Lundqvist E, et al. Pegylated liposomal doxorubicin and carboplatin compared with paclitaxel and carboplatin for patients with platinum-sensitive ovarian cancer in late relapse. J. Clin. Oncol. 2010;28(20):3323–3329. doi: 10.1200/JCO.2009.25.7519. [DOI] [PubMed] [Google Scholar]
- 3.Kemp Z, Ledermann J. Update on first-line treatment of advanced ovarian carcinoma. Int. J. Womens Health. 2013;5:45–51. doi: 10.2147/IJWH.S30231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ledermann JA, Raja FA, Fotopoulou C, Gonzalez-Martin A, Colombo N, Sessa C. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013;24(Suppl. 6):vi24–vi32. doi: 10.1093/annonc/mdt333. [DOI] [PubMed] [Google Scholar]
- 5.Ledermann J, Harter P, Gourley C, et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: a preplanned retrospective analysis of outcomes by BRCA status in a randomised Phase II trial. Lancet Oncol. 2014;15(8):852–861. doi: 10.1016/S1470-2045(14)70228-1. [DOI] [PubMed] [Google Scholar]
- 6.Ledermann J, Harter P, Gourley C, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N. Engl. J. Med. 2012;366(15):1382–1392. doi: 10.1056/NEJMoa1105535. [DOI] [PubMed] [Google Scholar]; •• First clinical trial that showed the relevance of poly (ADP-ribose) polymerase inhibitors in ovarian cancer.
- 7.Mirza MR, Monk BJ, Herrstedt J, et al. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. N. Engl. J. Med. 2016;375(22):2154–2164. doi: 10.1056/NEJMoa1611310. [DOI] [PubMed] [Google Scholar]; •• Publication that led approval of niraparib as maintenance treatment.
- 8.Swisher EM, Lin KK, Oza AM, et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, Phase II trial. Lancet Oncol. 2017;18(1):75–87. doi: 10.1016/S1470-2045(16)30559-9. [DOI] [PubMed] [Google Scholar]; •• Publication that led approval of rucaparib as treatment.
- 9.Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474(7353):609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott CL, Swisher EM, Kaufmann SH. Poly (ADP-ribose) polymerase inhibitors: recent advances and future development. J. Clin. Oncol. 2015;33(12):1397–1406. doi: 10.1200/JCO.2014.58.8848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bryant HE, Schultz N, Thomas HD, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature. 2005;434(7035):913–917. doi: 10.1038/nature03443. [DOI] [PubMed] [Google Scholar]; •• First manuscript that explains the relation of poly (ADP-ribose) polymerase inhibitor and synthetic lethality.
- 12.Helleday T. The underlying mechanism for the PARP and BRCA synthetic lethality: clearing up the misunderstandings. Mol. Oncol. 2011;5(4):387–393. doi: 10.1016/j.molonc.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Konstantinopoulos PA, Ceccaldi R, Shapiro GI, D'Andrea AD. Homologous recombination deficiency: exploiting the fundamental vulnerability of ovarian cancer. Cancer Discov. 2015;5(11):1137–1154. doi: 10.1158/2159-8290.CD-15-0714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murai J, Huang SY, Das BB, et al. Trapping of PARP1 and PARP2 by clinical PARP inhibitors. Cancer Res. 2012;72(21):5588–5599. doi: 10.1158/0008-5472.CAN-12-2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murai J, Huang SY, Renaud A, et al. Stereospecific PARP trapping by BMN 673 and comparison with olaparib and rucaparib. Mol. Cancer Ther. 2014;13(2):433–443. doi: 10.1158/1535-7163.MCT-13-0803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moschetta M, George A, Kaye SB, Banerjee S. BRCA somatic mutations and epigenetic BRCA modifications in serous ovarian cancer. Ann. Oncol. 2016;27(8):1449–1455. doi: 10.1093/annonc/mdw142. [DOI] [PubMed] [Google Scholar]; •• Intersting paper about other mechanisms of mutation in BRCA genes.
- 17.Pal T, Permuth-Wey J, Betts JA, et al. BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer. 2005;104(12):2807–2816. doi: 10.1002/cncr.21536. [DOI] [PubMed] [Google Scholar]
- 18.Risch HA, McLaughlin JR, Cole DE, et al. Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am. J. Hum. Genet. 2001;68(3):700–10. doi: 10.1086/318787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwarz RF, Ng CK, Cooke SL, et al. Spatial and temporal heterogeneity in high-grade serous ovarian cancer: a phylogenetic analysis. PLoS Med. 2015;12(2):e1001789. doi: 10.1371/journal.pmed.1001789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kondrashova O, Nguyen M, Shield-Artin K, et al. Secondary somatic mutations restoring RAD51C and RAD51D associated with acquired resistance to the PARP inhibitor rucaparib in high-grade ovarian carcinoma. Cancer Discov. 2017;7(9):984–998. doi: 10.1158/2159-8290.CD-17-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hennessy BT, Timms KM, Carey MS, et al. Somatic mutations in BRCA1 and BRCA2 could expand the number of patients that benefit from poly (ADP ribose) polymerase inhibitors in ovarian cancer. J. Clin. Oncol. 2010;28(22):3570–3576. doi: 10.1200/JCO.2009.27.2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunningham JM, Cicek MS, Larson NB, et al. Clinical characteristics of ovarian cancer classified by BRCA1, BRCA2, and RAD51C status. Sci. Rep. 2014;4:4026. doi: 10.1038/srep04026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chiang JW, Karlan BY, Cass L, Baldwin RL. BRCA1 promoter methylation predicts adverse ovarian cancer prognosis. Gynecol. Oncol. 2006;101(3):403–410. doi: 10.1016/j.ygyno.2005.10.034. [DOI] [PubMed] [Google Scholar]
- 24.Kalachand RD, Ruscito I, Dimitrova D, et al. Clinical characteristics and survival outcomes in BRCA1-methylated epithelial ovarian cancer (Bmeth-OC): a pooled analysis of data for 1,278 patients across five studies. J. Clin. Oncol. 2015;33(Suppl. 15):5526. [Google Scholar]
- 25.Konstantinopoulos PA, Spentzos D, Karlan BY, et al. Gene expression profile of BRCAness that correlates with responsiveness to chemotherapy and with outcome in patients with epithelial ovarian cancer. J. Clin. Oncol. 2010;28(22):3555–3561. doi: 10.1200/JCO.2009.27.5719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Randall LM, Pothuri B. The genetic prediction of risk for gynecologic cancers. Gynecol. Oncol. 2016;141(1):10–16. doi: 10.1016/j.ygyno.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 27.Vanderstichele A, Busschaert P, Olbrecht S, Lambrechts D, Vergote I. Genomic signatures as predictive biomarkers of homologous recombination deficiency in ovarian cancer. Eur. J. Cancer. 2017;86:5–14. doi: 10.1016/j.ejca.2017.08.029. [DOI] [PubMed] [Google Scholar]
- 28.Jenner ZB, Sood AK, Coleman RL. Evaluation of rucaparib and companion diagnostics in the PARP inhibitor landscape for recurrent ovarian cancer therapy. Future Oncol. 2016;12(12):1439–1456. doi: 10.2217/fon-2016-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Drew Y, Mulligan EA, Vong WT, et al. Therapeutic potential of poly(ADP-ribose) polymerase inhibitor AG014699 in human cancers with mutated or methylated BRCA1 or BRCA2. J. Natl Cancer Inst. 2011;103(4):334–346. doi: 10.1093/jnci/djq509. [DOI] [PubMed] [Google Scholar]
- 30.Kristeleit R, Shapiro GI, Burris HA, et al. A Phase I–II study of the oral PARP inhibitor rucaparib in patients with germline BRCA1/2-mutated ovarian carcinoma or other solid tumors. Clin. Cancer Res. 2017;23(15):4095–4106. doi: 10.1158/1078-0432.CCR-16-2796. [DOI] [PubMed] [Google Scholar]; •• Study Phase I/II with first clinical data about rucaparib.
- 31.A study of rucaparib in patients with platinum-sensitive, relapsed, high-grade epithelial ovarian, fallopian tube, or primary peritoneal cancer (ARIEL2) (ARIEL2) 2017. ClinicalTrials.govhttps://clinicaltrials.gov/ct2/show/NCT01891344
- 32.Oza AM, Tinker AV, Oaknin A, et al. Antitumor activity and safety of the PARP inhibitor rucaparib in patients with high-grade ovarian carcinoma and a germline or somatic BRCA1 or BRCA2 mutation: integrated analysis of data from Study 10 and ARIEL2. Gynecol. Oncol. 2017;147(2):267–275. doi: 10.1016/j.ygyno.2017.08.022. [DOI] [PubMed] [Google Scholar]
- 33.US FDA. www.accessdata.fda.gov/drugsatfda_docs/label/2018/209115s003lbl.pdf
- 34.Coleman RL, Oza AM, Lorusso D, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, Phase III trial. Lancet. 2017;390(10106):1949–1961. doi: 10.1016/S0140-6736(17)32440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Publication that led approval of rucaparib as maintenance treatment.
- 35.Farres J, Llacuna L, Martin-Caballero J, et al. PARP-2 sustains erythropoiesis in mice by limiting replicative stress in erythroid progenitors. Cell Death Differ. 2015;22(7):1144–1157. doi: 10.1038/cdd.2014.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pujade-Lauraine E, Ledermann JA, Selle F, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, Phase III trial. Lancet Oncol. 2017;18(9):1274–1284. doi: 10.1016/S1470-2045(17)30469-2. [DOI] [PubMed] [Google Scholar]; •• Publication that led approval of olaparib as maintenance treatment.
- 37.Kikuchi R, Lao Y, Bow DA, et al. Prediction of clinical drug–drug interactions of veliparib (ABT-888) with human renal transporters (OAT1, OAT3, OCT2, MATE1, and MATE2K) J. Pharm. Sci. 2013;102(12):4426–4432. doi: 10.1002/jps.23737. [DOI] [PubMed] [Google Scholar]
- 38.McCormick A, Swaisland H. In vitro assessment of the roles of drug transporters in the disposition and drug–drug interaction potential of olaparib. Xenobiotica. 2017;47(10):903–915. doi: 10.1080/00498254.2016.1241449. [DOI] [PubMed] [Google Scholar]
- 39.Coleman RL, Sill MW, Bell-McGuinn K, et al. A Phase II evaluation of the potent, highly selective PARP inhibitor veliparib in the treatment of persistent or recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer in patients who carry a germline BRCA1 or BRCA2 mutation – an NRG Oncology/Gynecologic Oncology Group study. Gynecol. Oncol. 2015;137(3):386–391. doi: 10.1016/j.ygyno.2015.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Bono J, Ramanathan RK, Mina L, et al. Phase I, dose-escalation, two-part trial of the PARP inhibitor talazoparib in patients with advanced germline BRCA1/2 mutations and selected sporadic cancers. Cancer Discov. 2017;7(6):620–629. doi: 10.1158/2159-8290.CD-16-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Clovis Oncology. 2017. http://clovisoncology.com/pipeline/rucaparib/
- 42.Gadducci A, Guerrieri ME. PARP inhibitors alone and in combination with other biological agents in homologous recombination deficient epithelial ovarian cancer: from the basic research to the clinic. Crit. Rev. Oncol. Hematol. 2017;114:153–165. doi: 10.1016/j.critrevonc.2017.04.006. [DOI] [PubMed] [Google Scholar]