Abstract
Once unimaginable, fertility management is now a nationally established part of cancer care in institutions, from academic centers to community hospitals to private practices. Over the last two decades, advances in medicine and reproductive science have made it possible for men, women and children to be connected with an oncofertility specialist or offered fertility preservation soon after a cancer diagnosis. The Oncofertility Consortium's National Physicians Cooperative is a large-scale effort to engage physicians across disciplines – oncology, urology, obstetrics and gynecology, reproductive endocrinology, and behavioral health – in clinical and research activities to enable significant progress in providing fertility preservation options to children and adults. Here, we review the structure and function of the National Physicians Cooperative and identify next steps.
Keywords: : fertility preservation, oncofertility, reproductive health
In 2007, the Oncofertility Consortium (OC) was established with the support of an NIH grant to address fertility concerns, including impact on quality of life, for children and patients of reproductive age diagnosed with cancer [1]. The original focus of the OC was female fertility preservation (FP) because at the time options were limited. To that end, initial clinical efforts were placed on offering ovarian tissue cryopreservation (OTC) to women and children. The OC has since expanded to become a global, interdisciplinary, and interprofessional network of specialists and scientists who explore the relationships between health, disease, survivorship and FP in children and patients of reproductive age [1–5]. To translate bench advances to clinical practice and to develop necessary interactions between practitioners, the OC developed the National Physicians Cooperative (NPC).
NPC administration
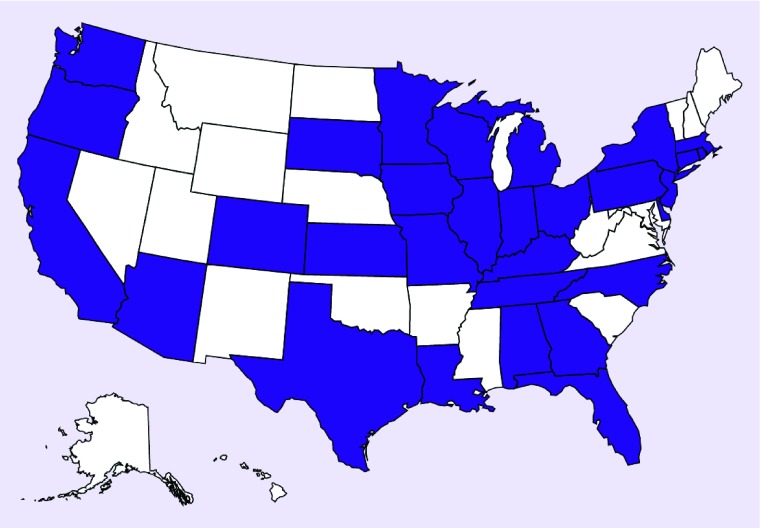
The NPC is a nationwide network of institutions dedicated to preserving the fertility of patients with cancer and other conditions whose progression or treatment may impair fertility. The NPC was originally comprised of four core centers: Northwestern University, University of Pennsylvania, Oregon National Primate Research Center and University of California, San Diego [6], but has since expanded to include 83 institutions within the USA (Figure 1). In addition to the NPC, the OC has expanded to include the Oncofertility Global Partners Network, with 91 institutions in 37 countries [7]. The NPC is managed by an administrative team that provides guidance on developing a successful FP program and facilitates review of OTC and testicular tissue cryopreservation (TTC) protocols by the site's institutional review board (IRB) (Table 1). NPC membership is open to any institution with providers who care for children, adolescents and/or adults of childbearing age whose disease or its treatment may impair fertility. Participants at NPC member institutions include oncologists, surgeons, endocrinologists, urologists, gynecologists, rheumatologists, mental health professionals, geneticists, embryologists, patient navigators, research coordinators, social workers, nurses, nurse practitioners, physician assistants and trainees in both adult and pediatric populations. Due to the diverse nature of the oncofertility community, specialized subcommittees were formed at the urging of our members. All NPC participants are invited to join subcommittees focused on specific interest areas, including basic science, male oncofertility, pediatrics, education, and gender and sex diversity. These subcommittees facilitate interactions between individuals at NPC member institutions, provide participants with a forum to discuss challenges, develop research collaborations, identify best practices with highly engaged peers and have developed numerous products that expand the reach of the OC to improve patient and provider education, ultimately leading to improved patient care and outcomes (Table 1). These materials are available for patient and provider education through Reprotopia (a K-gray reproductive health education website); SaveMyFertility (an informational website providing education and guidance to patients, parents and providers); and the patient navigator website (a site where patients and providers can walk through available FP options) (Table 2). To supplement online written materials, the OC maintains a library of video content on the OC website and YouTube channel including archived Oncofertility Conference presentations, Virtual Grand Rounds and laboratory training materials.
Figure 1. . States with National Physicians Cooperative member institutions are shown in purple, demonstrating the geographical reach of the Oncofertility Consortium.
Table 1. . Oncofertility Consortium-National Physicians Cooperative products created from 2007 to 2017 to address the unmet needs of Oncofertility Consortium stakeholders.
| Year | Product | Source | Type |
|---|---|---|---|
| 2007 | Ovarian tissue slow-freeze media and holding media | Sage/Origio | Laboratory media |
| 2007 | Ovarian tissue cryopreservation protocol and consent documents | Oncofertility Consortium | IRB document |
| 2007 | Ovarian tissue cryopreservation users manual | Oncofertility Consortium | Training resource |
| 2007 | Oncofertility: fertility preservation for cancer survivors | Springer | Textbook |
| 2009 | Save My Fertility iPhone App | Apple | Educational material |
| 2009 | Preservation of fertility in patients with cancer | New England Journal of Medicine | Publication |
| 2010 | Oncofertility: ethical, legal, social and medical perspectives | Springer | Textbook |
| 2012 | Oncofertility medical practice | Springer | Textbook |
| 2012 | Adolescent fertility values clarification tool | Oncofertility Consortium and Moffitt Cancer Center | Training resource |
| 2013 | Testicular tissue cryopreservation protocol | Oncofertility Consortium and University of Pittsburgh | IRB document |
| 2013 | Fertility preservation | Yen and Jaffe's Reproductive Endocrinology, 7th Edition | Book chapter |
| 2014 | Ovarian tissue dissection video | Oncofertility Consortium | Training resource |
| 2014 | Fertility preservation preferences and perspectives among adult male survivors of pediatric cancer and their parents | Journal of Adolescent and Young Adult Oncology | Publication |
| 2014 | Oncofertility communication | Springer | Textbook |
| 2014 | Prospective study of depression and anxiety in female fertility preservation and infertility patients | Fertility and Sterility | Publication |
| 2015 | OC-SHARES | Oncofertility Consortium | Training resource |
| 2015 | Understanding fertility in young female cancer patients | Journal of Women's Health | Publication |
| 2015 | Pediatric and teen ovarian tissue removed for cryopreservation contains follicles irrespective of age, disease diagnosis, treatment history and specimen-processing methods | Journal of Adolescent Young Adult Oncology | Publication |
| 2015 | Impact of fertility concerns on tamoxifen initiation and persistence | Journal of the National Cancer Institute | Publication |
| 2015 | Oncofertility: a grand collaboration between reproductive medicine and oncology | Reproduction | Publication |
| 2015 | In vitro follicle growth supports human oocyte meiotic maturation | Scientific Reports – Nature | Publication |
| 2016 | Good manufacturing practice requirements for the production of tissue vitrification and warming and recovery kits for clinical research | Journal of Assisted Reproductive Genetics | Publication |
| 2016 | Proceedings of the working group session on fertility preservation with gender and sex diversity | Transgender Health | Publication |
| 2016 | Oncologists’ role in patient fertility care: a call to action | JAMA Oncology | Publication |
| 2016 | Fellow education day curriculum | Oncofertility Consortium | Training resource |
| 2017 | Updated provider and patient pocket guides | SaveMyFertility.org | Educational material |
| 2017 | Pediatric and adolescent oncofertility | Springer | Textbook |
| 2017 | Fertility preservation and restoration for patients with complex medical conditions | Springer | Textbook |
| 2017 | New you, that's who: puberty | Oncofertility Consortium | Educational material |
| 2017 | New you, that's who: menstruation | Oncofertility Consortium | Educational material |
| 2017 | New you, that's who: anatomy | Oncofertility Consortium | Educational material |
| 2017 | The ethics of fertility preservation for pediatric patients with differences (disorders) of sex development | Journal of the Endocrine Society | Publication |
| 2017 | Retrospective OTC protocol | NPC-PIN | IRB document |
| 2017 | ASRM e-learning training modules | ASRM and Oncofertility Consortium | Educational material |
| 2017 | Fertility preservation training for obstetrics and gynecology fellows: a highly desired but non-standardized experience | Fertility Research and Practice | Publication |
| 2017 | Practices and attitudes regarding women undergoing fertility preservation: a survey of the National Physicians Cooperative | Journal of Adolescent Young Adult Oncology | Publication |
| 2017 | ‘Tissue papers’ from organ-specific decellularized extracellular matrices | Advanced Functional Materials | Publication |
| 2017 | Fertility lost-fertility found: narratives from the leading edge of oncofertility | Narrative Inquiry in Bioethics | Publication |
| 2017 | ‘When you're a baby you don't have puberty’: understanding of puberty and human reproduction in late childhood and early adolescence | Journal of Early Adolescence | Publication |
| 2017 | Oncofertility program implementation increases access to fertility preservation options and assisted reproductive procedures for breast cancer patients | Journal of Surgical Oncology | Publication |
| 2018 | Ovarian tissue cryopreservation in young females through the Oncofertility Consortium's National Physicians Cooperative | Future Oncology | Publication |
| 2018 | Fertility preservation | Yen and Jaffe's Reproductive Endocrinology, 8th Edition | Book chapter |
ASRM: American Society for Reproductive Medicine; IRB: Institutional review board; OC-SHARES: Oncofertility Consortium-Scientific Help Agreement for Research Endeavors; OTC: Ovarian tissue cryopreservation.
Table 2. . Enduring educational resources developed through the Oncofertility Consortium and National Physicians Cooperative for ongoing use and reference throughout the Oncofertility Consortium community.
| Educational resource | Summary |
|---|---|
| Oncofertility Consortium website www.oncofertility.northwestern.edu |
Authoritative resource for professionals in reproductive medicine, reproductive health research, oncology, biomechanics, material science, social sciences, bioethics, religion, policy research and educational sciences. This site provides continually updated content to expand current knowledge research, clinical practice and training in a wide spectrum of topics and issues |
| Oncofertility conference presentations and virtual grand rounds https://oncofertility.northwestern.edu/media |
The OC maintains video archives of all lectures at the Annual Oncofertility Conference and Virtual Grand Rounds. These presentations, given by domestic and international leaders in the field are hosted on the OC website with accompanying slides for easy review |
| Introduction to reproduction www.coursera.org/learn/reproductive-health |
The objective of this MOOC is to ensure an understanding of reproductive health and not confuse reproduction with sex. This course examines reproduction through a biological and scientific lens in an interactive format |
| ASRM principles of fertility preservation for reproductive healthcare providers certificate course https://store.asrm.org/Default.aspx?TabID=1356&productId=2777391 |
Developed in collaboration with OC leaders, this e-learning module is free to both ASRM members and nonmembers and covers the topics of:
|
| Oncofertility books www.woodrufflab.org/oncofertility-books |
The OC, with substantial input from the NPC, has published six books on oncofertility covering the overall scope of reproductive health and considerations for cancer patients and those with non-malignant conditions whose disease or treatment may affect fertility. Titles include:
|
| SaveMyFertility www.savemyfertility.org |
A resource for adult cancer patients and the parents of children with cancer who want to learn more about fertility preservation before and during cancer treatment and protecting their hormonal health after cancer treatment. This website also provides guidance to clinicians and other healthcare providers on how to discuss fertility and hormonal health with patients, survivors and families |
| Reprotopia www.reprotopia.northwestern.edu/ |
This website is dedicated to providing authoritative reproductive health education to individuals of all ages – ‘From K to Gray’. The OC and its partners have created a variety of useful websites, courses and other education tools to educate the public about the importance of reproduction and science. Reprotopia packages all of these web materials into one easy-to-navigate website |
| Repropedia www.repropedia.org |
This reproductive dictionary was created by an international team of scientists and clinicians and includes an API, allowing it to be built into other websites to supplement information and clarify unclear terms. Repropedia contains more than 500 reproductive health terms and biology information |
| Patient navigator for fertility preservation http://preservefertility.northwestern.edu/ | This website provides patients with a concise, easy to understand summary of available fertility preservation options at various stages of diagnosis, treatment and survivorship |
| New you, that's who www.reprotopia.northwestern.edu/projects/new-you-that's-who | This video project is targeted toward children 10–14 years of age to teach the basics of reproductive health. It uses proper, anatomically correct terms to cover the topics of puberty, anatomy and the menstrual cycle along with songs and animations to provide easy-to-understand information. It helps parents, guardians and teachers teach children about the fundamental characteristics of the human body and reproductive health |
API: Application programming interface; ASRM: American Society for Reproductive Medicine; MOOC: Massive open online course; NPC: National Physicians Cooperative; OC: Oncofertility Consortium.
All NPC member institutions participate in a robust exchange of research initiatives, best practices and exemplary patient care and are advised to follow American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network (NCCN) guidelines for informing patients of fertility risk and the range of FP options available to them based on age, time-to-treatment, medical condition and personal preferences. Standard FP options include pelvic shielding, egg and embryo banking, and ovarian transposition for adult females; sperm banking, testicular sperm extraction, and testis shielding for adult males; ovarian shielding and transposition for adolescent females; and testis shielding for adolescent males. Experimental procedures must be submitted to the institution's IRB for review and research determination, including any FP procedure deemed experimental by the American Society for Reproductive Medicine (ASRM), such as OTC and TTC [8,9]. Some NPC member institutions are not in a position to offer OTC or TTC to patients due to administrative constraints, lack of infrastructure or tissue expertise, or patient volume, and instead elect to participate in other ways such as survey studies and product development [10]. Institutions without OTC or TTC protocols on-site are able to quickly obtain referrals for their patients at nearby institutions with expanded FP services by contacting the OC's national FP hotline, the FERTline.
Strategies to improve reproductive outcomes for patients
While the NPC administrative team facilitates development of educational materials and dissemination of research achievements, the individual participants at NPC member institutions are direct points of contact with patients and many are leaders in translational research. NPC investigators can access rare human reproductive tissues for further research to explore and expand the reproductive options of patients. Leaders from the four core NPC sites established a comprehensive framework for a national OTC protocol. The initial framework included a letter of agreement for membership, IRB templates, creation of a slow-freeze media for OTC and a business partnership with a company (Origio) to provide high-quality manufacturing facilities for the specialized OTC media. This framework enabled distribution of OTC media to approved sites, agreements with ReproTech (a US company that provides long-term storage of reproductive tissue) to store OTC or TTC tissue, partnership with Memorial Blood Centers (a US FDA-licensed and compliant scientific laboratory) to perform infectious disease testing, and a pathway for cataloging research tissue and clinical data. Each process is outlined in detail within the OTC User Manual on the OC website (Table 1). OTC- and TTC-specific materials are publicly available to ensure that any institution interested in performing OTC or TTC, regardless of affiliation with the NPC, can utilize OC-developed protocols.
Between 2007 and 2017, 420 participants underwent OTC at an NPC member institution under an IRB-approved protocol. Patients could elect to freeze 100% of their ovarian tissue for their own future use or keep 80% of the removed ovarian tissue for future use and donate 20% of the remaining tissue to the OC-NPC Repository. Ten percent of the research tissue was formalin fixed and paraffin embedded to generate a fixed research tissue archive, and the remaining research tissue was either used fresh or cryopreserved for future study. The actual amount of tissue removed from each patient ranged from a small biopsy to a whole ovary, depending on site- and patient-specific variables and patient-provider decisioning. The OC-NPC Repository is accessible to NPC researchers through a formal tissue access request as part of the Oncofertility Consortium-Scientific Help Agreement for Research Endeavors (OC-SHARES; Table 1).
Scientific objectives
Research using the OC-NPC Repository has led to new knowledge and breakthrough technologies that have the potential to provide new FP and restoration options for young cancer patients [11]. On the basic science side, OC researchers are developing new ways to grow and mature follicles ex vivo and engineer novel biomaterials for ovarian tissue transplantation to restore reproductive and/or endocrine function [11–14]. Research using human tissue has led to our understanding of how best to transport ovarian tissue and how to cryopreserve tissue and individual follicles [12,13]. Moreover, histological assessment of ovarian tissue has led to a better understanding of follicle distribution and architecture [11] and an understanding that primordial follicles survive and grow better in vitro when maintained in an environment that mimics the ovarian cortex [13]. Perhaps most strikingly, we now know that human follicles can grow in vitro to the large antral stage, can produce hormones and can complete ‘ovulation’ resulting in the generation of MII oocytes in vitro [15–17]. Additionally, a first-ever assessment of oocyte changes with advanced maternal age showed that chromosome cohesion decreases and predates other indicators of physiologic aging, similar to what has been demonstrated in studies in model organisms (mouse) [18]. These are significant advances providing a prismatic view on human follicle maturation that could not have been done in any other setting, and are providing the urgently needed fundamental new knowledge necessary to ensure that advances are being made that will meet the needs of both current and future patients.
Clinical advancements
The NPC has undertaken various projects that reach across several diverse clinical disciplines with the ultimate goal of better understanding the intricacies of the patient populations being served. We have highlighted important clinical activities below that are most relevant to the oncology community.
Tamoxifen adherence
Tamoxifen initiation and persistence in reproductive-age estrogen receptor-positive breast cancer survivors is low, with patients younger than 40 years at greatest risk for either discontinuing or being nonadherent to antiestrogen treatment [19]. The underlying reasons for the poor utilization of this life-preserving treatment had not been well investigated. An OC-supported study tested the hypothesis that fertility concerns may contribute to poor tamoxifen use among premenopausal patients and found that, in a large young breast cancer patient cohort, fertility concerns were statistically associated with both a failure to initiate tamoxifen treatment and with early discontinuation of the drug [20]. In addition, expanded access to FP education prior to initial cancer therapy was important to help increase long-term tamoxifen use as recommended by ASCO [21,22]. An international study is currently underway to determine if temporary interruption of endocrine therapy to achieve a pregnancy will negatively impact breast cancer outcomes [23]. The study also includes a psychooncological supplementary assessment of fertility concerns, psychological well-being and decision-making. Importantly, a recent multicenter case–control study showed that pregnancy after treatment for breast cancer, regardless of hormone receptor status, did not impact disease-free survival when compared with nonpregnant patients. These findings were based on a median follow-up of 7.2 years postpregnancy [24]. To this end, young breast cancer patients who have completed treatment, who are clinically stable and express interest in becoming pregnant should be supported to reach this survivorship goal [25].
Good manufacturing practice
Globally, there is lack of standardization of freezing methodologies with centers performing both slow-freeze or vitrification of reproductive tissues. Within the USA, there is growing interest in vitrification for OTC as there are numerous reports of live births as a result of transplantation of vitrified ovarian tissue in Asia [26–28]. Domestically, products that are manufactured with the intent of receiving FDA approval for clinical use must be produced under an FDA-approved investigational new drug application. Thus, the OC began generating a reliable methodology and material list for an ovarian tissue vitrification kit and a supplementary warming and thawing kit [29]. Kits were based on careful development of protocols with the expertise of cryobiologists, and manufactured using good manufacturing practice requirements and good laboratory practice techniques and validated using nonhuman primate ovarian tissue [30]. Discussion with industry partners is ongoing to move toward manufacture and distribution of these kits for clinical use.
Provider knowledge & attitudes
To better understand clinician perspectives on FP and challenges in patient communication, a number of studies were developed and implemented through the OC. A 2011 survey of pediatric oncology specialists found that fertility threats are a major concern and found that specialists agreed that patients should be offered fertility consultation [31]. However, only 46% of survey respondents indicated that they refer male pubertal patients over 50% of the time, and only 12% of survey respondents reported referring female pubertal patients over 50% of the time, indicating further education of providers is necessary [32]. A 2016 survey was distributed to physicians, advanced practice nurses (APNs) and nurses within the field of pediatric oncology with special focus on adolescent males. This study found that 93.6% of physicians, 74.6% of APNs and 48.2% of nurses discussed the impact on fertility 76–100% of the time with their adolescent male patients. Physicians and APNs reported high levels of comfort discussing fertility issues with their patients, with nurses feeling less comfortable. This study indicated progress from the 2011 survey study, but supported the need of further education for providers, especially nurses, to discuss fertility and FP with their patients and families [31].
Patient & family perspectives
To understand additional barriers that may impact fertility discussions, the OC completed multiple studies to examine the decision-making process of parenthood goals among younger adolescents diagnosed with cancer. A focus group was hosted of adult survivors of adolescent and young adult (AYA) cancer, ages 15–39 years at time of diagnosis and their parents and found that while fertility was not recognized as a priority at the time of diagnosis, it is a significant concern later in life [33]. A narrative review of adolescent decision-making in the oncology setting was conducted to examine decisions related to cancer treatment, fertility concerns and capacity for decision-making regarding life-threatening health issues. This review concluded adolescents had a strong desire to participate in decisions about their cancer treatment and had significant fertility-related concerns [34]. A subsequent ethical examination of a case of a parent who made a decision to preserve a very young child's fertility on behalf of that child concluded that parents should feel empowered to make such decisions on behalf of a child who is too young to provide consent to maintain an open reproductive future for the child [35]. ASCO, ASRM and the American Academy of Pediatrics and Children's Oncology Group also support this endorsement [9,36,37].
Development of values clarification tools to address adolescent fertility knowledge
Consortium members adapted a version of the Wenzel reproductive concerns instrument to pilot test the Adolescent Fertility Values Clarification Tool to better understand how adolescent girls felt about FP and future parenthood. Results showed most parents did not accurately predict their daughter's response and underestimated their daughter's level of concern about potential infertility [38]. The final tool contains an introduction to use, types of responses typically seen among teen girls as fertility is discussed and how to address them, and frequently asked questions [31]. The development of this tool provided evidence that loss of fertility is a significant quality-of-life issue for female teens and provides a rubric for discussions around this issue.
Adoption
The OC has addressed family-building challenges for patients who are diagnosed with infertility due to their disease or treatment. Cancer survivors often face challenges when adopting as a result of real or perceived discrimination by adoption agencies. Through an IRB-approved study, questionnaires were developed and distributed to 27 adoption agencies in 21 states to examine perspectives on parenting postcancer [39]. The study found that agency perspectives vary widely on whether cancer survivors should be allowed to adopt, with limited federal and state regulations pertaining to adoption. Cancer survivors are encouraged to research a number of adoption agencies as they may find the variation in policies to work in their favor on their journey to parenthood. The OC has developed a ‘Cancer Friendly Adoption Agencies’ page on the OC website to assist cancer survivors.
Expansion of the OC & NPC mission
In 2012 and 2013, the European Society of Human Reproduction and Embryology and ASRM, respectively, determined that egg banking was no longer experimental and was a safe and effective FP option for postpubertal women [40]. At that time, the OC expanded its attention to providing FP options to additional patient populations: pediatric girls, pediatric boys, patients with nonmalignant conditions, disorders of sex development (DSD) and transgender individuals.
Pediatric girls
OTC remains the only FP option for prepubertal girls [41–43]. Using the adult protocol as a template, NPC member institutions obtained IRB approval for OTC in pediatric patients. Pediatric oncologists partner with their institutional reproductive endocrinology and infertility clinic or local fertility center for ovarian tissue freezing per the OTC procedure. As OTC began expanding to pediatric centers, the median age of patients enrolling in OTC protocols through the NPC has dropped from 30.6 years of age in 2007 to 12.4 years in 2017. Experimental options that may be available in the future include heterotopic or orthotopic transplantation of ovarian tissue back into the patient for restoration of reproductive or endocrine function, in vitro maturation of immature follicles to obtain mature eggs for use in IVF, or use of ovarian bioprosthesis [15,17,44–46]. Each of these exciting options highlight active areas of basic science research within the OC and NPC.
Pediatric boys & adult males
For adult males, the most common method of FP is sperm banking. For prepubertal boys, or AYA males unable to provide a sperm sample, TTC may offer an option for restoring future fertility, similar to the use of OTC in the female population. The TTC protocol and framework is available through the OC at the University of Pittsburgh and serves as the coordinating center for other institutions interested in offering TTC to their patients. TTC has not been used for spermatogenic recovery or pregnancy, but experimental options that may be available in the future include transplantation of spermatogonial stem cells back into the patient's testes, maturation of spermatozoa in testicular tissue organ culture and testicular tissue autografting or xenografting [47–49]. Given this potential, seven NPC member institutions have obtained IRB approval and enrolled a collective 108 patients.
Nonmalignant conditions, disorders of sex development, and gender dysphoria
NPC member institutions have the ability to expand their OTC eligibility to allow enrollment of patients with nonmalignant conditions whose disease or treatment may cause infertility and between 2007 and October 2017, 70 such patients were enrolled (Table 3). DSD patients also face infertility due to various degrees of abnormal gonadal development, while transgender patients potentially face infertility as a result of the treatments needed to fully transition to another gender [42,50,51]. The Gender and Sex Diversity subcommittee of the NPC has mapped issues faced by transgender and sex diverse patients to identify appropriate FP interventions, and address psychological concerns and ethical considerations [52]. At the time of this publication, no NPC institutions offer OTC and TTC to transgender patients; however, many sites are working with their institution to identify appropriate consent and education strategies for this patient population, and involve the patient's mental health provider during their recommended assessment for medical intervention, as detailed by the World Professional Association for Transgender Health and Endocrine Society clinical practice guidelines [53–56].
Table 3. . Number of patients with nonmalignant conditions enrolled in National Physicians Cooperative ovarian tissue cryopreservation protocols from January 2007 to October 2017.
| Diagnosis | NPC OTC patients |
|---|---|
| Sickle cell anemia | 17 |
| Aplastic anemia | 11 |
| Beta thalassemia | 9 |
| Fanconi anemia | 9 |
| Turner syndrome | 5 |
| HLH | 5 |
| Myelodysplastic syndrome | 4 |
| Diamond–Blackfan anemia | 2 |
| Catamenial migraine | 1 |
| Combined immunity deficiency | 1 |
| Hurler's syndrome | 1 |
| Interferon gamma deficiency | 1 |
| Systemic-onset juvenile idiopathic arthritis | 1 |
| Trisomy 8 myelodysplastic syndrome | 1 |
| Idiopathic hypereosinophilic syndrome | 1 |
| XO/XY mosaicism | 1 |
HLH: Hemophagocytic lymphohistiocytosis; NPC OTC: National Physicians Cooperative ovarian tissue cryopreservation.
Conclusion
The Oncofertility Consortium has created an infrastructure for sharing scientific and medical advances in a way that enables patients access to the most up-to-date medical treatment plans and emerging reproductive technologies. The NPC has effectively worked in a coordinated and strategic manner enabling better science, education and medical applications to reach men, women and children to preserve their reproductive potential. Moving forward, there is a need for long-term monitoring of technical advancements, including success rates, lab variability and tissue utilization, however, there is currently no systematic data collection process in place within the USA. Data collection is institution-specific and patient volumes at individual centers vary greatly. Additionally, due to the experimental nature of OTC, there is currently no consensus on the best method to freeze and thaw ovarian tissue. Further research is needed to develop best practices and streamlined protocols for mass utilization within the USA.
Future perspective
Cancer survivorship rates have steadily increased due to advances in early diagnosis and treatment. Unfortunately, many AYA cancer survivors face reproductive dysfunction, including infertility, caused by the disease process or cancer treatment and the potential for significant psychological distress due to infertility, which often leads to adverse health outcomes and a poorer quality of life. The NPC has been involved in a number of OC-led clinical studies investigating patient experiences, methods of service delivery and financial, ethical, legal or religious considerations affecting the access of patients or providers to oncofertility services. Over the last decade, the NPC has grown exponentially by geographic location, membership and in the number and types of patients served. The original four core NPC member institutions were large academic hospital systems and treated adult female cancer patients. Today, NPC member institutions include private IVF centers, community hospitals, pediatric hospitals and standalone cancer centers, with participants from various clinical disciplines treating diverse populations of pediatric and adult patients. Beyond the continental USA, Oncofertility Global Partner membership has rapidly increased and OC materials have been translated into seven different languages. As the OC's global reach has expanded, relationships between Global Partner and NPC member institutions have developed organically through collaborative research protocols, subcommittee participation and joint publications. In an effort to promote an inclusive network and to further catalyze these connections, the OC will launch the Oncofertility Professional Engagement Network (OPEN). OPEN will merge the NPC with the Global Partners Network and build upon the solid foundation of each group by supporting a strong global network where members share resources, methodologies and experiences, and foster significant collaboration among members. OPEN will continue the work of the valuable NPC subcommittees, where highly engaged colleagues will meet, in person and virtually, to develop new research protocols, identify best practices, and discuss challenges and pathways to success in specific focus areas. By merging these powerful groups together, the OC will turn novel science into accessible end points for clinicians and patients alike and provide a platform where concerns are raised, consensus is developed and patterns are identified at the intersection of technology and application.
The field of Oncofertility is ever-evolving with new stakeholders and changing challenges. In an ideal world, we would eliminate the need for our field. We can imagine this in a setting: where advances in cancer detection, diagnosis and treatments eliminate cancer all together; where mitigation strategies exist to protect full fertility or where interventional options exist to preserve full fertility; where FP is considered by all stakeholders (patients, partners, providers, the public); and where FP is fully accessible to all. With the strength and determination of such a field, we will ultimately achieve this ambitious vision.
However, in the immediate future there is still a critical need to advance patient needs in FP through the work of integrated clinical and basic research teams. In the next few years, we will be seeking solutions to the oncofertility problems of a diverse population of stakeholders – from the younger and younger pediatric population to the older and older adult ones, to sex diverse individuals, to those with various types of infertility (iatrogenic, genetic, trauma) and to those across a broad access grid with respect to education, geography, economic status, etc. We will consider FP in contexts wider than we ever have. We will think about fertility needs across the anatomical spectrum from the gonad to the reproductive tract to the nipple; we will expand endocrine support across the lifespan from puberty and menstrual cyclicity to menopause and contraception; we will apply what we learn in humans to endangered and threatened species to ensure a world of terrestrial diversity; we will meet transgenerational expectations; and we will imagine ways to reproduce in new territories beyond earth and ways that transcend our bodies with reproductive bioprosthetics. All the while, we will do so in a manner that enables autonomous and error-free reproduction and will be cognizant of whose interest, under what auspices and for what purposes we do so.
Executive summary.
Adolescents have a strong desire to participate in their cancer treatment and have significant fertility-related concerns.
The Oncofertility Consortium (OC) has created an infrastructure for sharing scientific and medical advances in a way that enables patients to access to the most up-to-date medical treatment plans and emerging reproductive technologies.
The National Physicians Cooperative (NPC) is a nationwide network of member institutions dedicated to preserving the fertility of their patients.
The NPC has worked in a coordinated and strategic manner enabling better science, education and medical applications to reach men, women and children to preserve their reproductive potential.
Individual participants at NPC member institutions are the direct points of contact with patients and many are leaders in translational research.
Physicians and advanced practice nurses have a high comfort level in discussing fertility issues with patients while further education is needed for providers, especially nurses, to assist with fertility and FP discussions with patients and their families.
Acknowledgements
Special acknowledgement to the patients who generously donated reproductive tissue to the OC-NPC Repository to advance oncofertility research and the National Physicians Cooperative.
Footnotes
Author's contributions
The authors, BM Smith, F Duncan, L Ataman, K Smith, G Quinn, ME Pavone, TK Woodruff, provided substantial contributions to the conception and design of the manuscript and interpretation of data for publication, drafted and revised the manuscript for intellectual content, gave final approval of the version to be published and agrees to be accountable for all aspects of the work ensuring that questions related to the accuracy or integrity of any part of the work are investigated and resolved. The authors, RJ Chang, C Finlayson, K Orwig, H Valli-Pulaski, MB Moravek, MB Zelinski, HI Su, W Vitek, JF Smith, JS Jeruss, C Gracia, C Coutifaris, D Shah, L Nahata, V Gomez-Lobo, LC Appiah, RR Brannigan, V Gillis, W Gradishar, A Javed, AS Rhoton-Vlasak, LA Kondapalli, E Neuber, JP Ginsberg, CH Muller, J Hirshfeld-Cytron, WH Kutteh, SR Lindheim, B Cherven, LR Meacham, P Rao, L Torno, LS Sender, ST Vadaparampil, JL Skiles, T Schafer-Kalkhoff, OJ Frias, J Byrne, LM Westphal, DJ Schust, JL Klosky, KA McCracken, A Ting, Z Khan, C Granberg, B Lockart, B Scoccia, MM Laronda, JE Mersereau, C Marsh, provided significant contributions to the design of the manuscript and interpretation of data for publication, revised the manuscript at length for intellectual content, gave final approval of the version to be published and agrees to be accountable for all aspects of the work ensuring that questions related to the accuracy or integrity of any part of the work are investigated and resolved.
Financial & competing interests disclosure
This work was supported by the Center for Reproductive Health After Disease (P50HD076188) from the NIH National Center for Translational Research in Reproduction and Infertility (NCTRI). The below authors acknowledge relationships with the following: J Hirschfeld-Cytron is a consultant in the Natera Genetics Company; ME Pavone is an advisory board member in Ferring Pharmaceuticals; SR Lindheim is a consultant and speaker in Bayer; a medical advisor in Crossbay; a speaker in Abbvie and Cooper Surgical; LA Kondapalli is a memeber of Speakers’ Bureau in Ferring Pharmaceuticals. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Open access
This work is licensed under the Attribution-NonCommercial-NoDerivatives 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Woodruff TK. From the bench to bedside to babies: translational medicine made possible by funding multidisciplinary team science. J. Assist. Reprod. Genet. 2013;30(10):1249–1253. doi: 10.1007/s10815-013-0082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woodruff TK. The Oncofertility Consortium – addressing fertility in young people with cancer. Nat. Rev. Clin. Oncol. 2010;7(8):466–475. doi: 10.1038/nrclinonc.2010.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woodruff TK. Oncofertility: a grand collaboration between reproductive medicine and oncology. Reproduction. 2015;150(3):S1–S10. doi: 10.1530/REP-15-0163. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Describes the interaction between fundamental and clinical science leading to the field of oncofertility.
- 4.Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N. Engl. J. Med. 2009;360(9):902–911. doi: 10.1056/NEJMra0801454. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Clinical basis for fertility management in the cancer setting.
- 5.Woodruff TK. The emergence of a new interdiscipline: oncofertility. Cancer Treat. Res. 2007;138:3–11. doi: 10.1007/978-0-387-72293-1_1. [DOI] [PubMed] [Google Scholar]
- 6.Waimey KE, Duncan FE, Su HI, et al. Future directions in oncofertility and fertility preservation: a report from the 2011 Oncofertility Consortium Conference. J. Adolesc. Young Adult Oncol. 2013;2(1):25–30. doi: 10.1089/jayao.2012.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ataman LM, Rodrigues JK, Marinho RM, et al. Creating a global community of practice for oncofertility. J. Glob. Oncol. 2016;2(2):83–96. doi: 10.1200/JGO.2015.000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ethics Committee of American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil. Steril. 2013;100(5):1224–1231. doi: 10.1016/j.fertnstert.2013.08.041. [DOI] [PubMed] [Google Scholar]; • Important committee opinion on the ethics of fertility management in the cancer setting.
- 9.Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J. Clin. Oncol. 2013;31(19):2500–2510. doi: 10.1200/JCO.2013.49.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bortolleto P, Confino R, Smith BM, Woodruff TK, Pavone ME. Practices and attitudes regarding women undergoing fertility preservation: a survey of the National Physicians Cooperative. J. Adolesc. Young Adult Oncol. 2017;6(3):444–449. doi: 10.1089/jayao.2017.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duncan FE, Pavone ME, Gunn AH, et al. Pediatric and teen ovarian tissue removed for cryopreservation contains follicles irrespective of age, disease diagnosis, treatment history, and specimen processing methods. J. Adolesc. Young Adult Oncol. 2015;4(4):174–183. doi: 10.1089/jayao.2015.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan FE, Zelinski M, Gunn AH, et al. Ovarian tissue transport to expand access to fertility preservation: from animals to clinical practice. Reproduction. 2016;152(6):R201–R210. doi: 10.1530/REP-15-0598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laronda MM, Duncan FE, Hornick JE, et al. Alginate encapsulation supports the growth and differentiation of human primordial follicles within ovarian cortical tissue. J. Assist. Reprod. Genet. 2014;31(8):1013–1028. doi: 10.1007/s10815-014-0252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jakus AE, Laronda MM, Rashedi AS, et al. “Tissue papers” from organ-specific decellularized extracellular matrices. Adv. Funct. Mater. 2017;27(3) doi: 10.1002/adfm.201700992. pii:1700992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiao S, Zhang J, Romero MM, Smith KN, Shea LD, Woodruff TK. In vitro follicle growth supports human oocyte meiotic maturation. Sci. Rep. 2015;5:17323. doi: 10.1038/srep17323. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Describes the first human MII egg from in vitro follicle growth methodology.
- 16.Skory RM, Xu Y, Shea LD, Woodruff TK. Engineering the ovarian cycle using in vitro follicle culture. Hum. Reprod. 2015;30(6):1386–1395. doi: 10.1093/humrep/dev052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu M, Barrett SL, West-Farrell E, et al. In vitro grown human ovarian follicles from cancer patients support oocyte growth. Hum. Reprod. 2009;24(10):2531–2540. doi: 10.1093/humrep/dep228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duncan FE, Hornick JE, Lampson MA, Schultz RM, Shea LD, Woodruff TK. Chromosome cohesion decreases in human eggs with advanced maternal age. Aging Cell. 2012;11(6):1121–1124. doi: 10.1111/j.1474-9726.2012.00866.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hershman DL, Shao T, Kushi LH, et al. Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res. Treat. 2011;126(2):529–537. doi: 10.1007/s10549-010-1132-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Llarena NC, Estevez SL, Tucker SL, Jeruss JS. Impact of fertility concerns on tamoxifen initiation and persistence. J. Natl Cancer Inst. 2015;107(10) doi: 10.1093/jnci/djv202. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Illuminates the value of fertility management as part of maintaining patient compliance with life-preserving cancer treatments.
- 21.American Society of Clinical Oncology. Tamoxifen guideline update 2014. www.asco.org/about-asco/press-center/news-releases/asco-guideline-update-recommends-tamoxifen-10-years-women-non
- 22.Vu JV, Llarena NC, Estevez SL, Moravek MB, Jeruss JS. Oncofertility program implementation increases access to fertility preservation options and assisted reproductive procedures for breast cancer patients. J. Surg. Oncol. 2017;115(2):116–121. doi: 10.1002/jso.24418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pagani O, Ruggeri M, Manunta S, et al. Pregnancy after breast cancer: are young patients willing to participate in clinical studies? Breast. 2015;24(3):201–207. doi: 10.1016/j.breast.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 24.Lambertini M, Kroman N, Ameye L, et al. Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J. Natl Cancer Inst. 2018;110(4):426–429. doi: 10.1093/jnci/djx206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lambertini M, Del Mastro L, Pescio MC, et al. Cancer and fertility preservation: international recommendations from an expert meeting. BMC Med. 2016;14:1. doi: 10.1186/s12916-015-0545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Demeestere I, Simon P, Dedeken L, et al. Live birth after autograft of ovarian tissue cryopreserved during childhood. Hum. Reprod. 2015;30(9):2107–2109. doi: 10.1093/humrep/dev128. [DOI] [PubMed] [Google Scholar]
- 27.Donnez J, Dolmans MM, Pellicer A, et al. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: a review of 60 cases of reimplantation. Fertil. Steril. 2013;99(6):1503–1513. doi: 10.1016/j.fertnstert.2013.03.030. [DOI] [PubMed] [Google Scholar]; • Compendium of outcomes following tissue transplant to restore fertility in cancer survivors.
- 28.Kawamura K, Cheng Y, Suzuki N, et al. Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proc. Natl Acad. Sci. USA. 2013;110(43):17474–17479. doi: 10.1073/pnas.1312830110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Laronda MM, McKinnon KE, Ting AY, Le Fever AV, Zelinski MB, Woodruff TK. Good manufacturing practice requirements for the production of tissue vitrification and warming and recovery kits for clinical research. J. Assist. Reprod. Genet. 2017;34(2):291–300. doi: 10.1007/s10815-016-0846-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ting AY, Yeoman RR, Campos JR, et al. Morphological and functional preservation of pre-antral follicles after vitrification of macaque ovarian tissue in a closed system. Hum. Reprod. 2013;28(5):1267–1279. doi: 10.1093/humrep/det032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fuchs A, Kashanian JA, Clayman ML, et al. Pediatric oncology providers’ attitudes and practice patterns regarding fertility preservation in adolescent male cancer patients. J. Pediatr. Hematol. Oncol. 2016;38(2):118–122. doi: 10.1097/MPH.0000000000000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kohler TS, Kondapalli LA, Shah A, Chan S, Woodruff TK, Brannigan RE. Results from the survey for preservation of adolescent reproduction (SPARE) study: gender disparity in delivery of fertility preservation message to adolescents with cancer. J. Assist. Reprod. Genet. 2011;28(3):269–277. doi: 10.1007/s10815-010-9504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stein DM, Victorson DE, Choy JT, et al. Fertility preservation preferences and perspectives among adult male survivors of pediatric cancer and their parents. J. Adolesc. Young Adult Oncol. 2014;3(2):75–82. doi: 10.1089/jayao.2014.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Quinn GP, Murphy D, Knapp C, et al. Who decides? Decision making and fertility preservation in teens with cancer: a review of the literature. J. Adolesc. Health. 2011;49(4):337–346. doi: 10.1016/j.jadohealth.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Important paper on fertility preservation decisioning in the cancer setting.
- 35.Quinn GP, Stearsman DK, Campo-Engelstein L, Murphy D. Preserving the right to future children: an ethical case analysis. Am. J. Bioeth. 2012;12(6):38–43. doi: 10.1080/15265161.2012.673688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fallat ME, Hutter J. Preservation of fertility in pediatric and adolescent patients with cancer. Pediatrics. 2008;121(5):e1461–e1469. doi: 10.1542/peds.2008-0593. [DOI] [PubMed] [Google Scholar]
- 37.Oktay K, Harvey BE, Partridge AH, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J. Clin. Oncol. 2018;36(19):1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]
- 38.Quinn GP, Knapp C, Murphy D, Sawczyn K, Sender L. Congruence of reproductive concerns among adolescents with cancer and parents: pilot testing an adapted instrument. Pediatrics. 2012;129(4):e930–e936. doi: 10.1542/peds.2011-2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gardino SL, Russell AE, Woodruff TK. Adoption after cancer: adoption agency attitudes and perspectives on the potential to parent post-cancer. Cancer Treat. Res. 2010;156:153–170. doi: 10.1007/978-1-4419-6518-9_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Practice Committee of American Society for Reproductive Medicine. Ovarian tissue cryopreservation: a committee opinion. Fertil. Steril. 2014;101(5):1237–1243. doi: 10.1016/j.fertnstert.2014.02.052. [DOI] [PubMed] [Google Scholar]
- 41.Chambon F, Brugnon F, Greze V, et al. Cryopreservation of ovarian tissue in pediatric patients undergoing sterilizing chemotherapy. Hum. Fertil. (Camb.) 2016;19(1):23–31. doi: 10.3109/14647273.2016.1151561. [DOI] [PubMed] [Google Scholar]
- 42.Johnson EK, Finlayson C, Rowell EE, et al. Fertility preservation for pediatric patients: current state and future possibilities. J. Urol. 2017;198(1):186–194. doi: 10.1016/j.juro.2016.09.159. [DOI] [PubMed] [Google Scholar]
- 43.Wallace WH, Smith AG, Kelsey TW, Edgar AE, Anderson RA. Fertility preservation for girls and young women with cancer: population-based validation of criteria for ovarian tissue cryopreservation. Lancet Oncol. 2014;15(10):1129–1136. doi: 10.1016/S1470-2045(14)70334-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Laronda MM, Jakus AE, Whelan KA, Wertheim JA, Shah RN, Woodruff TK. Initiation of puberty in mice following decellularized ovary transplant. Biomaterials. 2015;50:20–29. doi: 10.1016/j.biomaterials.2015.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Skory RM, Xu Y, Shea LD, Woodruff TK. Engineering the ovarian cycle using in vitro follicle culture. Hum. Reprod. 2015;30(6):1386–1395. doi: 10.1093/humrep/dev052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pacheco F, Oktay K. Current success and efficiency of autologous ovarian transplantation: a meta-analysis. Reprod. Sci. 2017;24(8):1111–1120. doi: 10.1177/1933719117702251. [DOI] [PubMed] [Google Scholar]
- 47.Gassei K, Orwig KE. Experimental methods to preserve male fertility and treat male factor infertility. Fertil. Steril. 2016;105(2):256–266. doi: 10.1016/j.fertnstert.2015.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hermann BP, Sukhwani M, Winkler F, et al. Spermatogonial stem cell transplantation into rhesus testes regenerates spermatogenesis producing functional sperm. Cell Stem Cell. 2012;11(5):715–726. doi: 10.1016/j.stem.2012.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Orwig KE, Schlatt S. Cryopreservation and transplantation of spermatogonia and testicular tissue for preservation of male fertility. J. Natl Cancer Inst. Monogr. 2005;(34):51–56. doi: 10.1093/jncimonographs/lgi029. [DOI] [PubMed] [Google Scholar]
- 50.Campo-Engelstein L, Chen D, Baratz AB, Johnson EK, Finlayson C. The ethics of fertility preservation for pediatric patients with differences (disorders) of sex development. J. Endocr. Soc. 2017;1(6):638–645. doi: 10.1210/js.2017-00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hirshfeld-Cytron J, Gracia C, Woodruff TK. Nonmalignant diseases and treatments associated with primary ovarian failure: an expanded role for fertility preservation. J. Womens Health (Larchmt) 2011;20(10):1467–1477. doi: 10.1089/jwh.2010.2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ethics Committee of the American Society for Reproductive Medicine. Access to fertility services by transgender persons: an ethics committee opinion. Fertil. Steril. 2015;104(5):1111–1115. doi: 10.1016/j.fertnstert.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 53.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int. J. Transgend. 2012;13(4):165–232. [Google Scholar]
- 54.Hembree WC, Cohen-Kettenis P, Delemarre-Van De Waal HA, et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2009;94(9):3132–3154. doi: 10.1210/jc.2009-0345. [DOI] [PubMed] [Google Scholar]
- 55.Finlayson C, Johnson EK, Chen D, et al. Proceedings of the working group session on fertility preservation for individuals with gender and sex diversity. Transgend. Health. 2016;1(1):99–107. doi: 10.1089/trgh.2016.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2017;102(11):3869–3903. doi: 10.1210/jc.2017-01658. [DOI] [PubMed] [Google Scholar]
- 57.De Roo SF, Rashedi AS, Beerendonk CCM, et al. Global oncofertility index-data gap slows progress. Biol. Reprod. 2017;96(6):1124–1128. doi: 10.1093/biolre/iox051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Anazodo A, Ataman-Millhouse L, Jayasinghe Y, Woodruff TK. Oncofertility – an emerging discipline rather than a special consideration. Pediatr. Blood Cancer. 2018;65(11):e27297. doi: 10.1002/pbc.27297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kong BY, Skory RM, Woodruff TK. Creating a continuum of care: integrating obstetricians and gynecologists in the care of young cancer patients. Clin. Obstet. Gynecol. 2011;54(4):619–632. doi: 10.1097/GRF.0b013e318236ea2c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miller EJN, Cookingham LM, Woodruff TK, et al. Fertility preservation training for obstetrics and gynecology fellows: a highly desired but non-standardized experience. Fertil. Res. Pract. 2017;3:9. doi: 10.1186/s40738-017-0036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Woodruff TK, Smith K, Gradishar W. Oncologists’ role in patient fertility care: a call to action. JAMA Oncol. 2016;2(2):171–172. doi: 10.1001/jamaoncol.2015.5609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Finlayson C, Johnson EK, Chen D, et al. Proceedings of the working group session on fertility preservation for individuals with gender and sex diversity. Transgend. Health. 2016;1(1):99–107. doi: 10.1089/trgh.2016.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Basco D, Campo-Engelstein L, Rodriguez S. Insuring against infertility: expanding state infertility mandates to include fertility preservation technology for cancer patients. J. Law Med. Ethics. 2010;38(4):832–839. doi: 10.1111/j.1748-720X.2010.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Walter JR, Xu S, Woodruff TK. A call for fertility preservation coverage for breast cancer patients: the cost of consistency. J. Natl Cancer Inst. 2017;109(5) doi: 10.1093/jnci/djx006. [DOI] [PubMed] [Google Scholar]
- 65.Armstrong AG, Kimler BF, Smith BM, Woodruff TK, Pavone ME, Duncan FE. Ovarian tissue cryopreservation in young females through the Oncofertility Consortium's National Physicians Cooperative. Future Oncol. 2018;14(4):363–378. doi: 10.2217/fon-2017-0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Giwa S, Lewis JK, Alvarez L, et al. The promise of organ and tissue preservation to transform medicine. Nat. Biotechnol. 2017;35(6):530–542. doi: 10.1038/nbt.3889. [DOI] [PMC free article] [PubMed] [Google Scholar]