Abstract
INTRODUCTION:
Hospitals are one of the most important institutions in providing health-care services. Highly experienced specialists, advanced technology, and decisive decisions about patients’ deaths and lives are all gathered in a dynamic and unique organization called Hospital. A huge portion of human, financial, and equipment resources are allocated to teaching hospitals; however, these hospitals are always faced with a lack of funding. The purpose of this study was to investigate the financial challenges of teaching hospitals and providing solutions.
MATERIALS AND METHODS:
A qualitative study was conducted using face-to-face interviews with a purposeful sample of 37 top and middle managers in the level of the Ministry of Health, its universities, teaching hospitals, and its affiliated departments in Tehran. Thematic analysis approach was used to analyze the data by applying MAXQDA10 software.
RESULTS:
Six themes among the reasons for financial challenges in teaching hospitals were insufficient funding for the educational and research sections and paying more attention to treatment, increased financial burden due to presence of medical student, indigent patients, disability in budget managing due to their dependence on medical universities, relative autonomy of hospitals, and payment systems. Among other factors, there are also insurance problems arisen from increased deductions on bills due to insurance astringency and delayed payment.
CONCLUSION:
The findings of the present study indicated that the major financial challenges of teaching hospitals faced severe financial problems, which had a negative effect on their entire activities and led to weakness in the implementation of their missions. Considering budget division among three defined missions of teaching hospitals (treatment, research, and education), the largest share of budget was allocated to treatment. Therefore, an appropriate and definite budget division is suggested to improve the allocation of resources to all three missions and to enhance staff's and patients satisfaction.
Keywords: A qualitative study, financial and insurance challenges, providing solutions, stakeholders’ perspective, teaching hospitals
Introduction
Health-care services are provided by various providers in health-care networks.[1] Due to worldwide increasing trend of health services cost, funding for establishing a coherent health system is one of the main concerns of most governments in all countries with different income levels,[2] and patients are compelled to pay more for treatment. The service sector in each country is prominent in terms of economic, social development, and distribution of welfare services and facilities. Providing public health and ensuring that all citizens access primary and basic health services without bearing financial burden is the other important missions of governments and they are aware that a healthy society is the foundation for the development of a country, but despite this attention to the health, they faced a lot of challenges in providing primarily needs of a society.[3] In this regard, hospitals, as one of the most complex institutions in providing health services,[4] have a major role in the efficiency of the health system.[5] Hospital chief financial officer reported that hospitals and health systems are under constant pressure to reduce costs while also improving quality and maintaining a strong workforce. With this comes an array of financial challenges, as reimbursement levels continue to change and healthcare becomes more consumer centric.[6] Teaching hospitals are an important part of the health-care system comprising a paramount part of health education and research.[7,8] They in most countries are either affiliated with the medical school or are part of a national or regional health system.[9] Today, hospitals are important because they consume huge amounts of human, physical, financial, and equipment resources;[10] that is, the large proportion of health-care resources are absorbed into hospitals, and in particular teaching hospitals.[11] Considering the simultaneous and multifunctional role of teaching hospitals, the efficacy of these hospitals is a major challenge for decision makers in the health sector. The findings of related studies in different countries confirm that hospitals face financial challenges in achieving their missions since some of them receive their budget from the government or are self-regulated, on the one hand, and are responsible for providing health care to indigent people on the other hand. Accordingly, it seems necessary to take advantage of efficient management to overcome such complex issues, threatening the survival of teaching hospitals.[12,13] Some public and big hospitals, also face the same mismatch between revenues and expenses impacting the financial viability of nonprofit hospitals across the nation.
Other states whose nonprofit hospitals face persistent financial difficulties might find it helpful to consider whether structural impediments–rather than more traditional accounting measures like revenues and expenses–may also be undermining the operating performance of their own institutions. Absent mandatory financial support from private payers and consistent funding from Medicaid, teaching hospitals are undercompensated for the full costs of training physicians.[14] Also, reducing Medicare indirect medical education payments would threaten the stability and predictability that teaching hospitals need to invest in residency programs to train physicians for evolving health care needs. Failure to lift the limit on the number of Medicare-funded total residency slots could create significant access challenges, especially as the number of individuals with insurance increases.[8] The results of other studies conducted in some countries have shown the disparity between the number of beds in teaching hospitals and educational, research, and therapeutic needs.[8,15] Accordingly, it seems that financial problems and challenges against the teaching hospitals are raised even in developed countries. A large share of the teaching hospitals resources is devoted to the provision and delivery of health-care services to patients, and less has been allocated to training, provision of adequate equipment, and educational space for medical students and residents, and even a very small contribution has been considered for research. It can be argued that this unbalanced allocation of resources may prevent teaching hospitals from achieving all their organizational missions.[16] The results of some studies comparing teaching hospitals with nonteaching hospitals in developed countries showed that only 10% of the hospitals could effectively provide health-care services tailored to patients.[17] There are some problems such as the lack of therapeutic and educational spaces, which sometimes result in problems concerning provision of health-care services.[18,19] According to the preamble, there are a lot of issues related to the financial challenges faced by teaching hospitals. The present study sought to analyze the current financial challenges in teaching hospitals, to investigate the barriers using scientific evidence, and to identify possible solutions according experts’ viewpoints in order to contribute the policymakers and health system planners to improve the efficiency and effectiveness of the country's teaching hospitals.
Materials and Methods
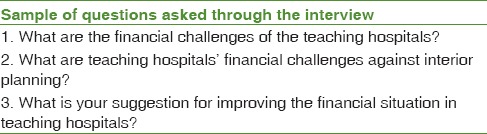
A qualitative research was employed to obtain a comprehensive understanding about financial challenges of teaching hospitals located in Tehran, Iran. The interviewees consisted of all key stakeholders, senior and middle managers in Tehran teaching hospitals, affiliated departments, and Ministry of Health headquarters. Selection of hospitals was done purposefully and based on their willingness to be included in the study. The sampling continued until reaching data saturation (n = 37). Before initiating the research, written consent was obtained from the relevant organizations. Data were collected by interviewing the participants. The interviewing texts were transcribed. Then, key concepts and themes were extracted and coded according to purpose of the research. In the first step, an interview topic guide was developed on the basis of findings of literature review and expert opinions [Table 1]. Most interviews last about 30 min and notes were taken from all interviews. Permission to record the interviews was obtained in all cases. The qualitative thematic analysis was used to analyze the data with the assistance of the MAXQDA software version NO10 produced for Persian language in Iran.
Table 1.
Summary of interview questions in topic guide
Results
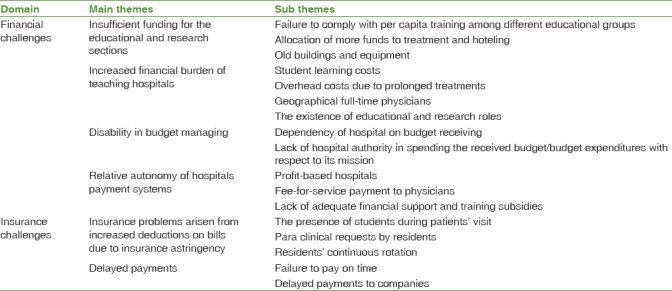
In regard to financial challenges of teaching hospitals that investigated in present study, six main themes categories were explored and presented according with their subthemes in Table 2.
Table 2.
Summary of main themes with their subthemes were explored
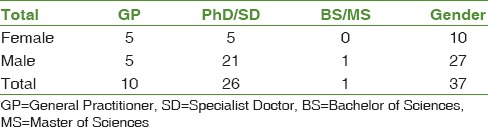
The frequency of interviewers based on education and sex is summarized in Table 3.
Table 3.
Frequency of interviewers based on education and sex
The frequency of interviewers based on work experienced and age is summarized in Table 4.
Table 4.
Frequency of interviewers based on work experience and age

Financial challenges
In accordance with stakeholders, the division of teaching hospital budget among its three missions is essential in order to achieve all the three goals; however, sometimes problems arise due to imbalance concerning budget division; that is, one mission is prioritized over two other missions. Most experts acknowledged that the main challenge of teaching hospitals is related to funding and budget, which can decelerate many of teaching hospital processes and procedures. In the following, you can see the view of one of hospital matrons concerning financial problem:
“Now, good suggestions are made in the hospital, but, unfortunately, they will be cut off because of the budget shortage and they will not be able to achieve the desired outcome.” P17-206.
The financial challenges faced by teaching hospitals comprise four sub-themes, including inadequate educational and research funding, increased financial burden on teaching hospitals, and disability of teaching hospitals concerning their budget expenditures, and the payment system along with the relative autonomy of the teaching hospitals.
Inadequate allocation of educational and research budgets
Most interviewees believed that teaching hospitals did not receive adequate educational funding from their affiliated universities; that is, hospitals still have difficulty with their educational curriculum. In other words, the educational per capita in these hospitals is not observed and hospitals are mostly responsible for treatment and education costs, of which a small share is allocated to education and research in hospitals. According to hospitals’ matrons, hospitals do not have enough education and research funding even for nursing groups; unfortunately, hospitals cannot go forward based on a training program for both staff and nursing students. Most senior hospital managers held that hospital's financial weakness is due to education budget cutoff, since they were forced to supply their funds through treatment at a certain time given the autonomy of the hospitals. Hospitals even did not have enough funding for the repair of their equipment. However, if a separate budget is allocated just to education and research by the departments, the problems can be solved. Indeed, because teaching hospitals are under the supervision of the medical universities, they must accommodate with university curricula, but there is no budget for spending on educational practices such as setting up pavilions, educational facilities, or paying professors. One of the hospitals; educational deputy said:
“In the teaching hospitals, a definite percentage of fee-for-services should be spent on medical education and training, but unfortunately, no education budget is provided” P33-42.
Some other interviewees also pointed out that currently so much of the budget, about 70%–80%, goes toward treatment, hoteling, and infrastructure creation, in fact, the focus of attention is on the treatment mission. On the other hand, due to lack of funding, even employee recruitment and provision of appropriate technology in the hospitals face challenges, interfering with treatment, research, and education goals. In addition, the lack of attention toward provision of educational and therapeutic equipment affect negatively all hospital activities and increase the incidence of medical errors due to shortage of medical education and training tools; and on the one hand, the old equipment for treatment. The financial affairs director of a hospital stated:
“Well, in the educational-therapeutic centers, the most important problem is related to financial and budget issues in comparison with private hospitals; however, their hoteling is appropriate” P13-50.
Some deputies also said that lack of funding even affects accreditation and assessment. For example, when fee-for-services are not paid on time, neither manager nor other staffs are expected to vigilantly follow accreditation and thus the assessments will face problems.
The increase of financial burden on teaching hospitals
A number of interviewees referred to self-regulation of teaching hospitals that converted them to profit-based hospitals as another challenge. On the other hand, some other experts pointed out that the increase of overhead costs in teaching hospitals due to waste of equipment for residents’ education and training is also another financial problem. In the past, patients were in charge of these overhead costs, but now it is covered by the educational system. In this regard, the number of patients hospitalized during a day rises due to additional par clinical requests made by residents at different years of residency, long treatment duration, and delayed counseling.
According to other interviewees, since patients who refer to governmental hospitals are often from middle class, the hospital financial burden increases. Based on financial affairs, directors of hospitals, staff, and faculty expenditures are higher in teaching hospitals as most physicians are geographical full time and there are educational and research roles that increase costs. A technical director of a hospital said:
“Because residents have to visit the patient, the patient's length of stay will be prolonged; on the other hand, more tests and par clinical measures are requested by the residents, resulting in increase of treatment cost.” P14-44.
The inability of teaching hospitals to decide on their budget
Most of the stakeholders mentioned that teaching hospitals cannot decide for their budget because these hospitals are under the supervision of the university and their budgets expenditures are decided at the Ministry of Health and at the medical university. Therefore, allocating a budget for conducting a research or setting up a research center is not in the priority. According to some of the interviewees’ viewpoint, the most important challenging factor is the lack of funding for implementation of hospital's interior plans; that is, they cannot spend on programs such as educational, research, and diagnostic programs with respect to their plans. Consequently, some other experts consider private hospitals ahead of teaching hospitals because although they have no medical education and training, they have more budget and can decide on budget expenditures; for example, to buy new equipment and provide facilities.
One of the hospital quality directors said,
”One of the main problems in the hospital is that it cannot decide on its own budget. The teaching hospital produce income but its budget is decided on in the university. This process affects many of the process and programs such as safety, research, diagnostic and therapeutic” P41-17.
The Payment system along with the relative autonomy of the teaching hospitals
Hospitals’ tendency toward being self-regulated has make them profit base in order to increase their incomes and provide some of their educational and therapeutic facilities such as conference halls, beds, equipment, and library through providing more health-care services. In the same vein, the kind of payment that is in form of fee-for-services creates problems. To help hospitals overcome financial challenges, allocation of financial support as well as training subsidies is suggested; therefore, the financial concerns of faculty members reduce.
Insurance challenges
Most scholars acknowledged that one of the reasons for the financial challenges of hospitals pertain to insurance, which had two sub-themes, including the increase of hospital deductions and delayed payment by insurance companies.
The increase of hospital deductions because of insurance companies’ astringency
Most hospital directors believed that since hospitals are contracting with insurance companies, they face a permanent challenge; that is the increase of hospital deductions due to insurance companies’ astringency. Given that in the first step residents visit the patients and seal the patients’ records at the teaching hospitals and the insurance companies do not accept the residents’ seals, deductions in hospital incomes increase. The other concern is related to residents’ rotation; that is, once they are trained about medical records filling by hospital discharge unit, they are replaced. Insurance companies are also about pharmaceutical and equipment bills; and with the smallest problem in patients’ medical records, deductions are made and the hospitals receive less than its own income.
Delayed payment by insurance agencies
According to many hospital and financial managers, another problem is related to delayed payments by insurance companies, which makes the hospital unable to do its tasks on time. Consequently, hospitals cannot pay the contractors. Ultimately, the qualities of hospitals as well as satisfaction of staff and patients reduce due to delayed payments.
Discussion
In the present study, participants and experts believed that the issue of funding is one of the most critical issues in teaching hospitals. Since these hospitals have three major missions of “treatment,” “education,” and “research” simultaneously, there must be a balance in terms of budget allocation.
Although many of the mentioned financial problems are related to each other, from the aspect of insufficient funding for the educational and research sections according to our study and in line with studies that have addressed the challenges of teaching hospitals, the lack of financial funds, especially in educational and research sections, is very evident. The simultaneous provision of education, research, and health-care services by these hospitals faces them with some financial problems. Regarding the financial challenges of teaching hospitals, most experts believed that teaching hospitals face a lot of financial challenges and are unable to afford their expenditures; on the other hand, they are treating indigent patients, which result in deterioration of the situation. Kane et al. also confirmed that the growth of hospital expenditures and the reduction of financial profit attracted special attention toward the costs of teaching hospitals. Teaching hospitals are often treat expensive and complex cases, and so far there has been a lot of research to cut off education-related costs, although estimating the routine costs of teaching hospitals for reasons such as low number of analytical studies remains vague in educational programs.[20]
From the aspect of increased financial burden of teaching hospitals similarly, according to statistics reported by the American Hospital Association in 2009, the expenditures of teaching hospitals are increasing; additionally, these hospitals are mainly giving services to low-income patients[18] which duplicate the financial strait of such organizations. In 2013, Shirvani confirmed these findings and pointed out that the health sector generally, along with the global health trend, faces major challenges in the treatment sector, including the high share of households from treatment costs, inadequate credits and inefficient use of available resources, the costs induced by the advancement of technology and medical equipment, the increase of the share of people's demands from the health sector, the lack of public access to health services, and people's dissatisfaction. Graskopof also stated in 2001 that overall costs are much higher in teaching hospitals than those in nonteaching hospitals due to additional responsibilities according to studies conducted in this regard.[16] A large number of interviewees also believed that the presence of students increase the expenditures of teaching hospitals; however, this is still a matter of doubt since according to Hosek et al., if students were to be substituted for physicians, production costs in teaching hospitals are expected to be lower than nonteaching hospitals at any level of production, but this claim requires more research.[21] Considering financial challenges, the majority of interviewees acknowledged that the burden of additional costs is more severe in teaching hospitals than private ones. Schwartz and Pogge in 2000 also showed that teaching hospitals and university centers are under intense organizational and financial pressures.[22]
From the aspect of disability in budget managing in general, the challenges of the general system and the health-care system comprise health financing problems, poor organizational structure of the health sector, and insufficiency of health financing management.[19] Nuss et al., in 2015 referred to the shortage of teaching hospitals and medical departments as another problem; however, medical education was reliant on hospitals and on old-age insurance in particular with respect to funding, which was stopped in 1997. Therefore, there is a need for new medical education models.[23] Huckman et al. argued that there is another problem in profit-based teaching hospitals, a phenomenon that occurs in relation to the occupational rotation of residents in July each year.[24] In 2014, their held that integration as an important strategy for heads of academic centers, including teaching hospitals to develop their health centers. There are many factors that affect the results of integration, such as management without certainty, different cultural differences in organizations, the need for dynamic organization management, concerns about profitability, and other related factors that need to be addressed.[25]
From the aspect of relative autonomy of hospitals’ payment systems also, Panch board association in 2015 announced that there are serious problems in many sections of teaching institutions across various countries considering the role of the teaching hospital, which offers the most advanced health-care services and has the responsibility of training. For instance, there are problems in accessing to government hospitals due to high population density and lack of teaching hospitals; in addition, private hospitals do not have enough equipment and facilities and they are mostly located in urban areas; these issues highlight the reconsideration of the number and structure of public and teaching hospitals.[26]
From the aspect of insurance problems arisen from increased deductions on bills due to insurance astringency and delayed payments In Brazil, the financial crisis in teaching hospitals began in the 1990s. The budget allocated to hospitals by the government is always lower than the amount required. Subsequently, the debt of hospitals increased (rising to about $100 million in late 2003) and 10% of hospital beds reduced. The reasons behind the crisis are still unclear. Hospital administrators held that hospitals cannot be effective and efficient without increasing patients’ reimbursement. The government is well aware that the budget for teaching hospitals should be increased.[27] According to the Association of American Medical Colleges in 1984, teaching hospitals faced at least ten challenges, including financial limitation risk by third-party payers, no new commitments for caring charitable patients, the tendency toward being profit-based hospital, and competition among doctors, hospitals due to increase of trained doctors, and competition in costs.[28]
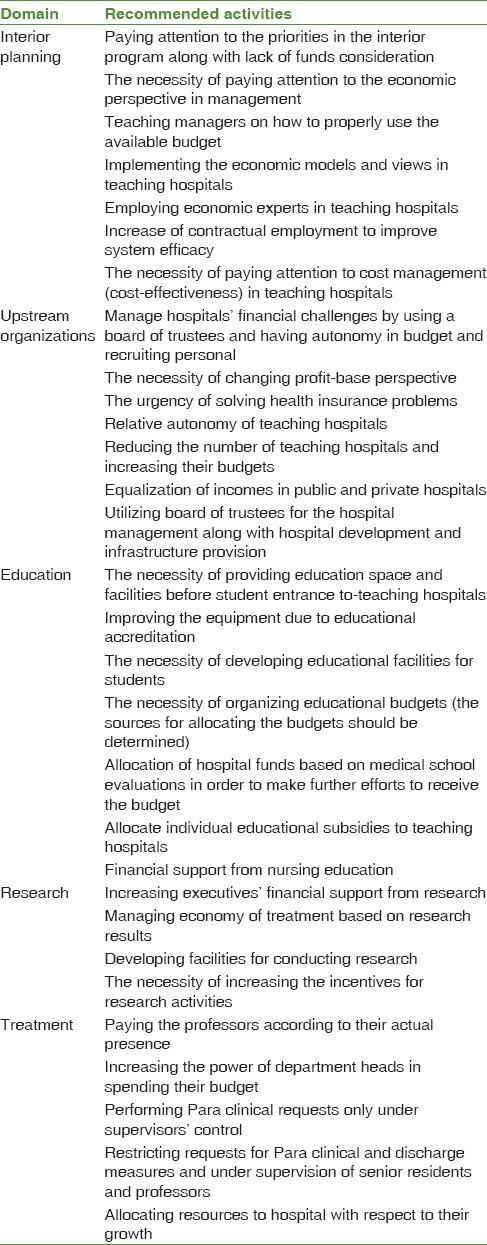
In this study, a number of experts have expressed their suggestion for solving such problems and limitations of teaching hospitals in five areas of interior planning, upstream organizations, education, research, and treatment in order to reduce the financial problems of teaching hospitals [Table 5].
Table 5.
Recommended strategies for managers
Limitation of the study
One of the limitations of this qualitative research is related to generalization of its findings; in other words, given the developing status of each country, its health system, and the position of teaching hospitals, these solutions may not be applicable and should be reconsidered.
Conclusion
The findings of studies suggest that issues such as poor responding status to educational and research indicators created due to lack of funding and integration of education with treatment in teaching hospitals can be considered as potential treat for achieving goals and mission is a main challenge influencing on the performance of health-care organizations and require further investigation. Hospital and medical costs, lack of financial resources, equipment, and training spaces, delayed payment by insurance companies and lack of payment to personnel, shifting more funds to treatment, and shortage of education funding are other issues that also need further study. The aforementioned issues have attracted the attention of health system decision makers and persuade them to develop facilities to help teaching hospitals deliver health services better, accommodate two other missions, education and research, and ultimately achieve patients’ satisfaction.
Financial support and sponsorship
This manuscript was supported and approved by the Faculty of Management and Medical Information, Iran University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This manuscript was a part of the PhD dissertation approved by the Faculty of Management and Medical Information, Iran University of Medical Sciences, with the ethics code of IUMS/SHMIS/1395/9321532002.
References
- 1.Sadaghiani E. Evaluation of Health Care Services and Hospital Standards. Iran, Tehran: Moein Publisher; 1997. p. 22. [Google Scholar]
- 2.Comparative Study of Health Indicators of the Eastern Mediterranean Region (EMRO) in 2001. Office of Financial and Budget Planning, Department of Management and Resources Development, Ministry of Health and Medical Education. 2004 [Google Scholar]
- 3.Ahangar A, Ahmadi AM, Mozayani AH, Dizaji SF. The role of risk-sharing mechanisms in finance health care and towards universal health coverage in low-and middle-income countries of World Health Organization regions. J Prev Med Public Health. 2018;51:59–61. doi: 10.3961/jpmph.17.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grifin D. What is hospital and how it works? In: Arab M, Valli L, Ravangard R, Kavusi Z, Ostovar R, Salami M, editors. Tehran: SID Publication; 2015. p. 33. [Google Scholar]
- 5.Sabermahani A, Goodarzi G, Barouni M, Khakian M. Estimation of technical efficiency of general hospitals of Kerman university of medical sciences by data envelopment analysis (DEA) method in 2007. J Kerman Univ Med Sci. 2010;17:59–67. [Google Scholar]
- 6.Gooch K. The Financial Challenges Facing Hospitals, Health Systems: 4 Takeaways. Hospital CFO Report; 17 April. 2018. [Last accessed on 2018 Oct 30]. Available from: https://www.beckershospitalreview.com/ finance/the-financial-challenges-facing-hospitals-health-systems- 4-takeaways.html .
- 7.Kupersmith J. Quality of care in teaching hospitals: A literature review. Acad Med. 2005;80:458–66. doi: 10.1097/00001888-200505000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Washington (USA): Association of American Medical Colleges; 2009. American Hospital Association. Teaching Hospitals: Their Impact on Patients and the Future Health Care Workforce. Report No.: 202.638.1100; p. 8. [Google Scholar]
- 9.Browne E. Teaching Hospitals. Islamic Medicine. 2002. [Last updated on 2017 Jan 17; Last accessed on 2016 Aug 29]. Available from: http://www.theinfolist.com/php/SummaryGet.php?Find Go=Listofuniversityhospitals .
- 10.Trotta A, Cardamone E, Cavallaro G, Mauro M. Applying the balanced scorecard approach in teaching hospitals: A literature review and conceptual framework. Int J Health Plann Manage. 2013;28:181–201. doi: 10.1002/hpm.2132. [DOI] [PubMed] [Google Scholar]
- 11.Najafi C. Designing the model of evaluation of hospital operation. Tehran. Management and Resources Development Department. Centre of Development Management and Administrative Reform. 2008 [Google Scholar]
- 12.Trotta A, Cardamone E, Cavallaro G, Mauro M. Applying the balanced scorecard approach in teaching hospitals: A literature review and conceptual framework. Int J Health Plann Manage. 2013;28:181–201. doi: 10.1002/hpm.2132. [DOI] [PubMed] [Google Scholar]
- 13.Padmore JS, Jaeger J, Riesenberg LA, Karpovich KP, Rosenfeld JC, Patow CA, et al. “Renters” or “owners”? Residents’ perceptions and behaviors regarding error reduction in teaching hospitals: A literature review. Acad Med. 2009;84:1765–74. doi: 10.1097/ACM.0b013e3181bf51c1. [DOI] [PubMed] [Google Scholar]
- 14.Hayden EW. Non-Profit Hospitals Face Structural as Well as Financial Challenges: Lessons from Massachusetts. Paper 24. Financial Services Forum Publications; March. 2005. [Last accessed on 2016 May 05]. pp. 13–4. Available from: http://www.scholarworks.umb.edu/ financialforum_pubs/24 . [DOI] [PubMed]
- 15.Najafpour ZH, Gudarzi Z, Keshmiri F, Pourreza A. Comparison of education and research indicators of patient safety status between selected hospitals of Tehran university of medical sciences based on WHO standards. Bimonthly Educ Strateg Med Sci. 2014;7:241–8. [Google Scholar]
- 16.Grosskopf S, Margaritis D, Valdmanis V. Effect of teaching on hospital productivity. Soc Econ Plan Sci. 2001;35:189–204. [Google Scholar]
- 17.Revision in Managing Teaching Hospitals; 8 April. 2016. [Last updated on 2016 May 11; Last accessed on 2016 Apr 05]. Available from: http://www.shahrekhabar.com .
- 18.Isna News. Lack of Education and Caring Space in Hospitals, a Major Problem in Teaching Hospitals; 25 April. 2016. [Last updated on 2016 Apr 30; Last accessed on 2016 May 02]. Available from: http://www.isna.ir/news/93120301158 .
- 19.Nasrollahpour Shirvani D, Mouodi S. Evidence-Based Policymaking in Health System and its Achievements and Challenges in Iran. Babol, Babol University of Medical Sciences and Health Care Services: Nooj Publishing; 2013. [Google Scholar]
- 20.Kane RL, Bershadsky B, Weinert C, Huntington S, Riley W, Bershadsky J, et al. Estimating the patient care costs of teaching in a teaching hospital. Am J Med. 2005;118:767–72. doi: 10.1016/j.amjmed.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 21.Hosek J, Palmer A. Teaching and hospital costs. [Last accessed on 2016 Jun 24];J Health Econ. 1983 2:29–46. doi: 10.1016/0167-6296(83)90010-3. Available from: http://www.sciencedirect.com/ science/article/pii/0167629683900103 . [DOI] [PubMed] [Google Scholar]
- 22.Schwartz RW, Pogge C. Physician leadership is essential to the survival of teaching hospitals. Am J Surg. 2000;179:462–8. doi: 10.1016/s0002-9610(00)00395-0. [DOI] [PubMed] [Google Scholar]
- 23.Nuss MA, Robinson B, Buckley PF. A statewide strategy for expanding graduate medical education by establishing new teaching hospitals and residency programs. Acad Med. 2015;90:1264–8. doi: 10.1097/ACM.0000000000000803. [DOI] [PubMed] [Google Scholar]
- 24.Huckman R, Song H, Barro J. Massachusetts: National Bureau of Economic Research; 2005. Cohort Turnover and Productivity: The July Phenomenon in Teaching Hospitals. Report No.: 11182; p. 45. [Google Scholar]
- 25.Thier SO, Kelley WN, Pardes H, Knight AW, Wietecha M. Success factors in merging teaching hospitals. Acad Med. 2014;89:219–23. doi: 10.1097/ACM.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 26.Punch Editorial Board. Teaching Hospitals and Healthcare Challenges. [Last updated on 2015 Sep 22; Last accessed on 2015 Aug 25]. Available from: http://www.punchng.com/topics/ editorial/
- 27.Castro Lobo MS, Ozcan Y, Sliva A, Estellita L, Fiszman R. Financing reform and productivity change in Brazilian teaching hospitals: Malmquist approach. CEJOR. 2010;18:141–52. [Google Scholar]
- 28.Association of American Medical Colleges. New Challenges for the Council of Teaching Hospitals and the Department of Teaching Hospitals. Discussion Paper; April. 1984. [Last accessed on 2017 May 10]. Available from: https://www.aamc.org/download/371974/data/0484_ new_ challenges_for_the_council_of_teaching_hospitals.pdf .


