Abstract
BACKGROUND AND AIM:
Mental health issues including depression and anxiety are common in pregnancy worldwide. This study aimed to identify factors associated with mental disorders in a sample of Iranian pregnant women.
MATERIALS AND METHODS:
A cross-sectional study was conducted among pregnant women referred to a prenatal-care clinic in an urban area, Isfahan, Iran. The questionnaires in this study included the General Health Questionnaire and additional structured questionnaires exploring sociodemographic, obstetric, and economic risk factors and empowerment for decision-making regarding pregnancy, parenting, financial authority, trust, and confidence in health-care staff. Regression analysis was performed to assess the impact of the number of variables on the likelihood of the presence of mental health problems.
RESULTS:
Overall, 54.2% and 11.7% of the women had anxiety and depression, respectively. No statistically significant associations were reported between anxiety and depression and obstetric characteristics such as gestational age, parity, abortion, previous infertility, unwanted pregnancy, and the screening test results. According to the logistic regression analysis, the predictors of depression and anxiety were acknowledging psychological changes in pregnancy and empowerment for decision-making regarding pregnancy and parenting and financial authority (P < 0.05).
CONCLUSIONS:
probably, women's empowerment on becoming aware of psychological changes during pregnancy and making decisions on pregnancy, parenting, and financial authority is the factor affecting the mental health of pregnant women.
Keywords: Anxiety, depression, Iran, mental health, pregnancy
Introduction
Depression and anxiety are common mental disorders during pregnancy and after childbirth worldwide. It has been reported that 25% of women in developing countries and 10% in developed countries suffer from a significant mental health problem during pregnancy and after childbirth.[1] A meta-analysis showed that the average prevalence of antenatal mental disorders was 15.6% in low- and low-to-middle-income countries. It is at least 50% higher than that of high-income countries.[2] Studies in Iran showed that the rate of depression and anxiety symptoms during pregnancy ranged at 25%–55%.[3,4] Antenatal anxiety and depression were found to be associated with poor obstetric, neonatal outcomes[5] and postpartum depression,[6] suicidal attempts,[7] and adverse infant outcomes such as preterm birth and low birth weight.[8]
The related mental health factors reflected the impact of multiple socioeconomic and biological factors on mental health during pregnancy.[9] Furthermore, it is believed that factors associated with mental health in pregnancy are related to specific cultural norms.[10] Moreover, each culture influences the way people understand mental health and their regard for it. Therefore, an understanding of and sensitivity to factors valued by different cultures will increase the relevance and success of potential interventions. In addition, it is necessary to understand a particular community's concepts of mental health before engaging in mental health promotion.[11] A mental health promotion framework that represents a public health approach to mental illness prevention identifies the following as key social and economic determinants of community and individual mental health.[12] Therefore, this study aimed to identify associated factors in a sample of Iranian pregnant women.
Materials and Methods
This was a cross-sectional study conducted in an urban area of Isfahan, Iran. The study research protocol was approved by the Ethics Committee affiliated with Isfahan University of Medical Sciences.
Participants
This cross-sectional study was performed from September to January 2015 on 300 Iranian pregnant women referred to prenatal care centers in Isfahan. Sampling was conducted randomly among the health centers of Isfahan, Iran. Given the number of samples in the study of Forouzandeh et al., using the Gigi chart and the Pokok statistical formula, the number of samples was estimated to be 300 women.[13] The study inclusion criteria were being married and having the ability to read and write. The women were informed of the study aim and process. Those women who expressed an interest to participation in this study signed the written informed consent form and filled out questionnaires.
The questionnaires in this study included the General Health Questionnaire (GHQ) and additional structured questionnaires exploring sociodemographic, obstetric, and economic risk factors. Some questions were derived from worldwide findings regarding major risk factors for perinatal anxiety and depressive symptoms, whereas others were created in an attempt to study the effects of sociodemographic determinants specific to Iran.
The GHQ was a 28-item self-report questionnaire designed by Goldberg (1972). The questions of anxiety and depression subscales of valid GHQ were used to measure mental health. Each of the subscales of depression and anxiety are composed of 7 items. This tool is designed in a 4-point Likert scale (0–3) as follows: never: 0; usual: 1; more than usual: 2; and much more than usual: 3. The cutoff point in each subscale is the score of 6, and higher scores indicate pathologic symptoms. The validity of the questionnaire has been confirmed in Iran.[14] The Cronbach's α for the present study was 0.93.
Risk factors examined included demographic, obstetric, and psychosocial risk factors. Information on maternal age and education, partner's education, women and partner's occupation, economic status, housing, gestational age, parity, abortion, previous infertility, previous dead children, pregnancy plan, result of screening test, and preparation for parenting was sought.
Knowledge of pregnant women about changes in mood during pregnancy was assessed using a researcher-made questionnaire. The scientific validity of this instrument was measured with a survey of six experts. Knowledge of pregnant women about changes in mood during pregnancy recording sheet consisted of five questions; for example: question 1: are pregnant women more irritable and sensitive than ever before. The internal consistency of the questionnaire was confirmed with Cronbach's alpha of 0.79, while its reliability was approved with dividing the women and with a correlation coefficient of 90% in a pilot study.
Perceived confidence to health-care center staff among pregnant woman was assessed using a researcher-made questionnaire. The scientific validity of this instrument was measured with a survey of six experts. The confidence in health-care center staff recording sheet consisted of five questions; for example: questions 1: how confident are you that in case of occurring a problem for you and your fetus, healthcare staff and physicians can control the situation? The questionnaire was designed in a 5-point Likert scale (0–4) from never (0) to very much (4). The internal consistency of the questionnaire was confirmed with Cronbach's alpha of 0.82, while its reliability was approved with dividing the women and with a correlation coefficient of 90% in a pilot study.
Furthermore, the questionnaire of empowerment for decision-making and financial authority contained ten questions and was based on a valid questionnaire from the Ministry of Health and Medical Education. Examples of questions asked in this questionnaire were “how much your opinion is considered for making decisions that you make for your children?” “Can you make any suggestion for allowance or spending the family's income?” It had a 5-point Likert scale with an appropriate internal consistency using the calculation of Cronbach's alpha coefficients of 0.79–0.93. Furthermore, its appropriate reliability based on the split-half method was reported using the calculation of correlation coefficients of 80%–90%.
Statistical analysis was performed using the SPSS version 19.0 software (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to summarize the demographic, obstetric, and psychosocial characteristics of the sample. The correlations between binary categorical variables were analyzed by Chi-square tests. In addition, multiple logistic regression analysis was applied to assess demographic, obstetric, and psychosocial characteristics of probable anxiety and depression during pregnancy. The 95% confidence interval and adjusted odds ratios were presented for the final models. P < 0.05 was considered statistically significant.
Results
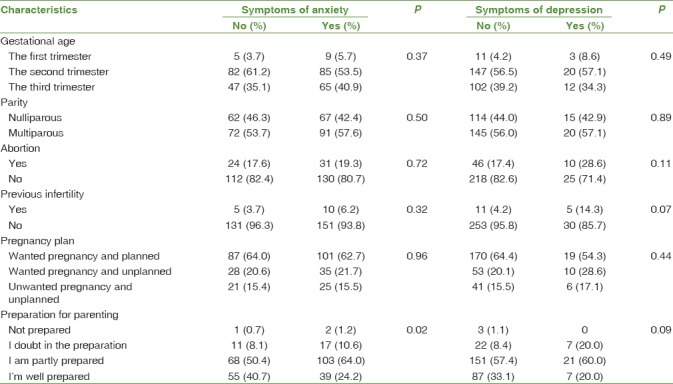
Three hundred women agreed to participate and completed the questionnaires and 98.8% (n = 296) of the women answered the questions on the GHQ. The maternal mean (standard deviation [SD]) age of the women was 29.2 (4.8) years. According to the subscales of depression and anxiety in the GHQ, 161 (54.2%) women had the symptoms of anxiety, 35 (11.7%) women had the symptoms of depression, and 126 (42.6%) women had mental problems. There was a statistically significant association between the scores of depression and anxiety (P < 0.000). No statistically significant association was found between the demographic and obstetric characteristics and depression and anxiety. However, the partner's occupation and education had statistically significant association with depression (P < 0.05) [Tables 1 and 2].
Table 1.
Relationships between demographic variables and anxiety and depression
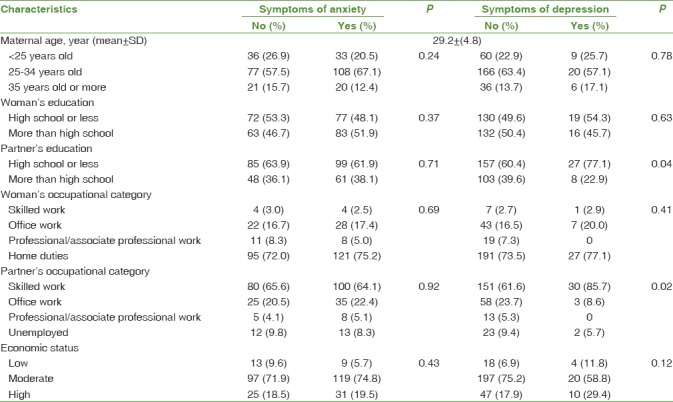
Table 2.
Relationships between obstetric variables and anxiety and depression
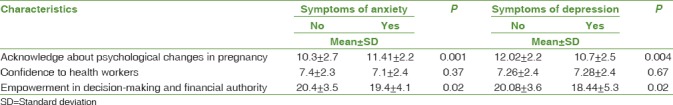
Furthermore, the results of this study showed that the knowledge about changes in mood during pregnancy and empowerment for decision-making and financial authority was associated with the symptoms of anxiety and depression [Table 3].
Table 3.
Relationships between social variables and anxiety and depression
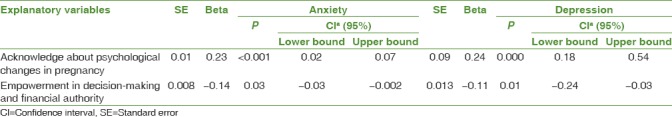
Multiple logistic regression test revealed that the knowledge of changes in mood during pregnancy and empowerment for decision-making and financial authority (P < 0.05) was the predictor of anxiety and depression during pregnancy. In addition, partner's job and education failed to independently and significantly predict anxiety and depression during pregnancy and therefore, were excluded from the model [Table 4].
Table 4.
Results of multiple linear regression, including factors related to anxiety and depression
Discussion
In this study, anxiety was observed in more than half of the pregnant women, which had a higher prevalence than depression. In fact, 54.2% of women showed symptoms of anxiety, while 11.7% of them showed symptoms of depression. Unlike the present study, many studies have reported a higher prevalence of depression in pregnancy,[15,16] while other studies have reported similar prevalence rate,[17] including a systematic review where a prevalence rate of 11.3% has been reported, with the results almost similar to the current study.[18] Furthermore, in a study conducted by Lee et al., the prevalence of anxiety in pregnancy was reported as 54%, which is similar to the present study.[19] The outcome selection is likely to have much impact on the incidence.[9] Differences in methodology, the time of study during pregnancy, and different measurement tools among the studies may lead to differences in the prevalence of depression in countries. Moreover, individual, social, and economic differences of people might be another reason for the difference in the prevalence rates of depression and anxiety during pregnancy between different studies.[20]
In this study, no significant relationship was observed between maternal age and mental health. Although some studies suggest that the rate of mental health problems is higher among younger women,[2,21] a number of studies have reported no relationship between mental health and age,[22,23,24] and the results of this research are consistent with these studies. Analyses indicate that the young age of parents is not associated with low mental health by itself; but more likely, the young parents are living in poor socioeconomic conditions.[25,26]
In the present study, no statistically significant relationship was observed between the education level and occupation of pregnant women, their socioeconomic status, and anxiety and depression during pregnancy. In many studies, no statistically significant associations were reported between depression during pregnancy with the education level, occupation,[26] and economic status.[24] In the present study, the partner's employment status had a statistically significant association with depression in pregnancy. In addition, it was consistent with the results of Karmaliani et al.'s study.[27] In the present study, 73.6% of women were homemakers and mostly relied on the income of their spouses. Therefore, depression in pregnant women appeared to be related to their partner's job status, which appears to be logical.
No statistically significant relationship was reported between anxiety and depression with obstetric factors including the age of pregnancy, unwanted pregnancies, and number of pregnancies, abortions, and infertility. Similarly, in other studies, no statistically significant association was reported between anxiety and depression and unwanted pregnancy,[16,28] results of which are in line with the current study. Furthermore, two studies reported that unwanted pregnancies were risk factors for depression in the first trimester of pregnancy.[19,29] It is likely that stress and shock due to unintended pregnancies is reduced with the progression of pregnancy.[30] It was noted that the majority of the women in this study were in the second (56.4%) and third (38.6%) trimesters of pregnancy.
In addition, no statistically significant relationship was reported between the history of abortion and mental health problems including anxiety and depression. This study was consistent with other studies.[4,31] Meanwhile, a statistically significant correlation was reported in some studies between abortion and depression and anxiety.[32,33] The probable reason for such conflictions can be variations in risk factors such as tendency to get pregnant, social support at the time of abortion, and self-blame for pregnancy and abortion. In addition, the time gap between abortion and the current pregnancy plays an important role in developing depression and anxiety during pregnancy.[34] The World Health Organization also recommends the minimum temporal distance between abortion and new pregnancy to be 6 months so that the woman can regain her physical and mental health.[34] According to existing evidence and expansion of family planning services coverage in Iran, the interval between pregnancies is often more than 6 months, and most women in this study were in the second and third quarter, and thus, these results are not unexpected.
In this study, a statistically significant correlation was found between the empowerment of women in pregnancy and anxiety and depression. According to the findings of this study, empowered women will have higher mental health. On the other hand, some researches demonstrate that mothers with higher skills and competency pass their pregnancy period with fewer problems.[35,36] Moreover, the outcomes of women's empowerment include the individual's independence, better decision-making,[37] and improvement of well-being during pregnancy.[38] The empowerment of pregnant women improves their health and reduces maternal mortality.[39] And also, the International Conference on Population and Development in Beijing (1995) considered the fact that the empowerment of women improves gestational health.[40]
In the present study, a statistically significant relationship was found between the women's readiness for childbirth and child-rearing as a factor affecting their anxiety. More prepared women reported lower levels of anxiety. Preparation for childbirth during pregnancy can reduce negative experiences regarding childbirth and is seen as a protective factor against anxiety.[41] Furthermore, some studies showed that women needed to raise their awareness for developing their inner strength, improving their independence and abilities, overcoming pregnancy's changes, and for better physical and mental performance.[20,42]
Limitation
Some limitations of this study that need to be considered in interpreting the results are as follows: this was a cross-sectional study; thus, interpreting the cause and effect relationship between the variables studied is limited and, according to the results, only the factors associated with anxiety and depression in pregnant women can be identified. Diagnostic tools and clinical interviews were not used in the diagnosis of depression and anxiety. In this study, the screening instrument of GHQ was used; although it is a valid tool in Iran, such kinds of tools cannot exactly diagnose and identify anxiety and depression. Despite these limitations, the strength of our study is that, we tried that the studied population would be selected from all pregnant women referred to public and private health centers and offices of obstetricians and gynecologists practicing in the city of Isfahan with sufficient generalization capability. In addition, the present study provides fundamental and important information on the prevalence of and factors associated with mental health for measures and programs of promoting mental health.
Conclusions
Given its broad factors, knowledge of the risk factors of mental disorder during pregnancy in sociocultural context might identify the development of effective strategies within the limited resources of health-care systems to target populations with greater needs for integrated population-level interventions targeted at improving the mental well-being of pregnant women. In general, it may be the most effective approach for reducing anxiety and depression such as programs that promote women's empowerment may offer additional mental health benefits.[43]
Financial support and sponsorship
Funding for this study was provided by Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to thank Isfahan University of Medical Sciences, Isfahan, Iran, and all women who participated in this research.
References
- 1.World Health Organization. Maternal Mental Health and Child Health and Development in Low and Middle Income Countries: Report of the Meeting, Geneva, Switzerland, 30 January-01 February, 2008. 2008 [Google Scholar]
- 2.Fisher J, Tran T, Duc Tran T, Dwyer T, Nguyen T, Casey GJ, et al. Prevalence and risk factors for symptoms of common mental disorders in early and late pregnancy in vietnamese women: A prospective population-based study. J Affect Disord. 2013;146:213–9. doi: 10.1016/j.jad.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Rezaee R, Framarzi M. Predictors of mental health during pregnancy. Iran J Nurs Midwifery Res. 2014;19:S45–50. [PMC free article] [PubMed] [Google Scholar]
- 4.Sadeghi N, Azizi S, Molaeinezhad M. Anxiety status in pregnant mothers at third trimester of pregnancy and its related factors in referrals to Bandar Abbas Hospitals in 2012. Iran J Obstet Gynecol Infert. 2014;17:8–15. [Google Scholar]
- 5.Alderdice F, McNeill J, Lynn F. A systematic review of systematic reviews of interventions to improve maternal mental health and well-being. Midwifery. 2013;29:389–99. doi: 10.1016/j.midw.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Hartmann JM, Mendoza-Sassi RA, Cesar JA. Postpartum depression: Prevalence and associated factors. Cad Saude Publica. 2017;33:e00094016. doi: 10.1590/0102-311X00094016. [DOI] [PubMed] [Google Scholar]
- 7.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–8. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 8.Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: A review. Arch Womens Ment Health. 2012;15:1–4. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- 9.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bull World Health Organ. 2012;90:139G–49. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roomruangwong C, Epperson CN. Perinatal depression in Asian women: Prevalence, associated factors, and cultural aspects. Asian Biomed. 2011;5:179–93. [Google Scholar]
- 11.Herrman H, Saxena S, Moodie R. World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice: A Report of the World Health Organization, Department of Mental Health and Substance Abuse in Collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. 2005 [Google Scholar]
- 12.Walker L, Verins I, Moodie R, Webster K. Responding to the Social and Economic Determinants of Mental Health: A Conceptual Framework for Action. Promot Mental Health. 2005:89–108. [Google Scholar]
- 13.Forouzandeh N, Delaram M, Deris F. The quality of mental health status in pregnancy and it's contributing factors on women visiting the health care centers of Shahrekord, (2001-2002) J Reprod Infert. 2003;4:146–56. [Google Scholar]
- 14.Noorbala A, Mohammad K. The validation of general health questionnaire-28 as a psychiatric screening tool. Hakim Res J. 2009;11:47–53. [Google Scholar]
- 15.Faisal-Cury A, Menezes P, Araya R, Zugaib M. Common mental disorders during pregnancy: Prevalence and associated factors among low-income women in São Paulo, Brazil: Depression and anxiety during pregnancy. Arch Womens Ment Health. 2009;12:335–43. doi: 10.1007/s00737-009-0081-6. [DOI] [PubMed] [Google Scholar]
- 16.Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, le Roux I, et al. Depressed mood in pregnancy: Prevalence and correlates in two cape town peri-urban settlements. Reprod Health. 2011;8:9. doi: 10.1186/1742-4755-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Felice E, Saliba J, Grech V, Cox J. Prevalence rates and psychosocial characteristics associated with depression in pregnancy and postpartum in Maltese women. J Affect Disord. 2004;82:297–301. doi: 10.1016/j.jad.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: A systematic review. J Affect Disord. 2010;123:17–29. doi: 10.1016/j.jad.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 19.Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, Fong DY, et al. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. 2007;110:1102–12. doi: 10.1097/01.AOG.0000287065.59491.70. [DOI] [PubMed] [Google Scholar]
- 20.Biratu A, Haile D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: A cross-sectional study. Reprod Health. 2015;12:99. doi: 10.1186/s12978-015-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shahmiry H, Momtazi S. The prevalence of depression and its relationship with personal characteristics in pregnant women. Med J Tabriz Univ Med Sci. 2006;28:83–6. [Google Scholar]
- 22.Abuidhail J, Abujilban S. Characteristics of Jordanian depressed pregnant women: A comparison study. J Psychiatr Ment Health Nurs. 2014;21:573–9. doi: 10.1111/jpm.12125. [DOI] [PubMed] [Google Scholar]
- 23.Ratcliff BG, Sharapova A, Suardi F, Borel F. Factors associated with antenatal depression and obstetric complications in immigrant women in Geneva. Midwifery. 2015;31:871–8. doi: 10.1016/j.midw.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 24.Srinivasan N, Murthy S, Singh AK, Upadhyay V, Mohan SK, Joshi A, et al. Assessment of burden of depression during pregnancy among pregnant women residing in rural setting of Chennai. J Clin Diagn Res. 2015;9:LC08–12. doi: 10.7860/JCDR/2015/12380.5850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmied V, Johnson M, Naidoo N, Austin MP, Matthey S, Kemp L, et al. Maternal mental health in Australia and New Zealand: A review of longitudinal studies. Women Birth. 2013;26:167–78. doi: 10.1016/j.wombi.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Agostini F, Neri E, Salvatori P, Dellabartola S, Bozicevic L, Monti F, et al. Antenatal depressive symptoms associated with specific life events and sources of social support among Italian women. Matern Child Health J. 2015;19:1131–41. doi: 10.1007/s10995-014-1613-x. [DOI] [PubMed] [Google Scholar]
- 27.Karmaliani R, Asad N, Bann CM, Moss N, Mcclure EM, Pasha O, et al. Prevalence of anxiety, depression and associated factors among pregnant women of Hyderabad, Pakistan. Int J Soc Psychiatry. 2009;55:414–24. doi: 10.1177/0020764008094645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Groves AK, Kagee A, Maman S, Moodley D, Rouse P. Associations between intimate partner violence and emotional distress among pregnant women in Durban, South Africa. J Interpers Violence. 2012;27:1341–56. doi: 10.1177/0886260511425247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marchesi C, Bertoni S, Maggini C. Major and minor depression in pregnancy. Obstet Gynecol. 2009;113:1292–8. doi: 10.1097/AOG.0b013e3181a45e90. [DOI] [PubMed] [Google Scholar]
- 30.Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord. 2016;191:62–77. doi: 10.1016/j.jad.2015.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM, et al. Risk factors for depressive symptoms during pregnancy: A systematic review. Am J Obstet Gynecol. 2010;202:5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bergner A, Beyer R, Klapp BF, Rauchfuss M. Pregnancy after early pregnancy loss: A prospective study of anxiety, depressive symptomatology and coping. J Psychosom Obstet Gynaecol. 2008;29:105–13. doi: 10.1080/01674820701687521. [DOI] [PubMed] [Google Scholar]
- 33.Gong X, Hao J, Tao F, Zhang J, Wang H, Xu R, et al. Pregnancy loss and anxiety and depression during subsequent pregnancies: Data from the C-ABC study. Eur J Obstet Gynecol Reprod Biol. 2013;166:30–6. doi: 10.1016/j.ejogrb.2012.09.024. [DOI] [PubMed] [Google Scholar]
- 34.Marston C. Report of a WHO Technical Consultation on Birth Spacing Geneva Switzerland, 13-15 June 2005. 2007 [Google Scholar]
- 35.Froozanfar S, Majlessi F, Rahimi FA, Pourreza A. Assessment of the relationship between empowerment and reproductive behavior. J Daneshvar Med. 2012;18:1–9. [Google Scholar]
- 36.Jahdi F, Montazeri A, Balouchi M, Behboodi MZ. The impact of group prenatal care on pregnant women empowerment. Payesh. 2014;13:229–34. [Google Scholar]
- 37.Malhotra A, Schuler SR. Women's empowerment as a variable in international development. Measuring Empowerment: Cross-Disciplinary Perspectives.edited by Deepa Narayan : The world bank. 2005:71–88. [Google Scholar]
- 38.Abada T, Tenkorang EY. Women's autonomy and unintended pregnancies in the Philippines. J Biosoc Sci. 2012;44:703–18. doi: 10.1017/S0021932012000120. [DOI] [PubMed] [Google Scholar]
- 39.Borghei NS, Taghipour A, Roudsari RL, Keramat A. Development and validation of a new tool to measure Iranian pregnant women's empowerment. East Mediterr Health J. 2016;21:897–905. doi: 10.26719/2015.21.12.897. [DOI] [PubMed] [Google Scholar]
- 40.McIntosh CA, Finkle JL. The Cairo conference on population and development: A new paradigm? Population and Development Review 21. 1995;2:223–60. [Google Scholar]
- 41.Abbott MW, Williams MM. Postnatal depressive symptoms among pacific mothers in Auckland: Prevalence and risk factors. Aust NZJ Psychiatry. 2006;40:230–8. doi: 10.1080/j.1440-1614.2006.01779.x. [DOI] [PubMed] [Google Scholar]
- 42.Cunningham K, Ruel M, Ferguson E, Uauy R. Women's empowerment and child nutritional status in South Asia: A synthesis of the literature. Matern Child Nutr. 2015;11:1–9. doi: 10.1111/mcn.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cohen A, Raja S, Underhill C, Yaro BP, Dokurugu AY, De Silva M, et al. Sitting with others: Mental health self-help groups in Northern Ghana. Int J Ment Health Syst. 2012;6:1. doi: 10.1186/1752-4458-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


