Abstract
Radiation is a treatment for many gynecological malignancies, especially locally advanced cervical cancer. Development of sarcoma due to previous radiation occurs very rarely. They develop within the radiation field. We report a case of carcinosarcoma in our patient developed 8 years after the radiotherapy (RT) that she received in the form of external beam radiation and intracavitary RT along with concomitant chemotherapy consisting of cisplatin. Although the development of secondary primary cancer is rare, for every patient who receives radiation for treatment of cancer, close follow-up is recommended as they may have viable endometrium.
KEYWORDS: Radiation, sarcoma, second primary cancer, viable endometrium
INTRODUCTION
Cervical cancer is one of the most common cancers in women worldwide. Conventionally, radical hysterectomy or radiation therapy alone has been accepted as standard treatment for early-stage invasive cervical cancer and locally advanced cancers have been treated by radiotherapy (RT) alone consisting of a combination of high-dose intracavitary RT (ICRT) and external beam RT (EBRT). With the advances in the management of locally advanced cervical cancer, cisplatin-based chemotherapy has been concurrently used for the management of these tumors.
The risk of secondary malignancies associated with RT for cancer patients has become increasingly important since the mean age of patients at the onset of cancer has been decreasing and the survival rate has been increasing.[1]
CASE REPORT
A 42-year-old woman was diagnosed with squamous cell carcinoma of the cervix stage IIB. She was treated with external beam radiation 50.4 Gy/28 fractions by three-dimensional conformal radiation therapy (four-field box technique) along with concomitant chemotherapy weekly consisting of cisplatin 50 mg/m2 followed by three sittings of ICRT 8 Gy/fraction. She was on regular follow-up as per protocol and was disease free.
After 8 years of treatment, she complained of vaginal discharge and bleeding per vaginam; Her MRI [Figure 1] showing uterine cavity filled with heterogeneous mass lesion invading half of the myometrium suggestive of uterine corpus tumor The patient underwent total abdominal hysterectomy, bilateral salpingo-oophorectomy, and bilateral pelvic lymph node dissection. Intraoperatively, there was ileal stricture; therefore, ileoileal resection with anastomosis was also done. The surgery was optimal without any gross residual diseases.
Figure 1.
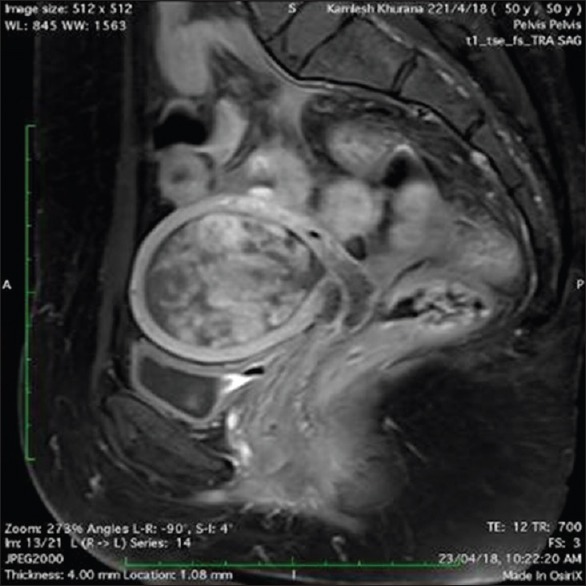
T1-weighted sagittal postcontrast image showing uterine cavity filled with heterogeneous mass lesion invading half of the myometrium. Cervix appearing normal
Histological examination [Figure 2] revealed uterine corpus carcinosarcoma.
Figure 2.
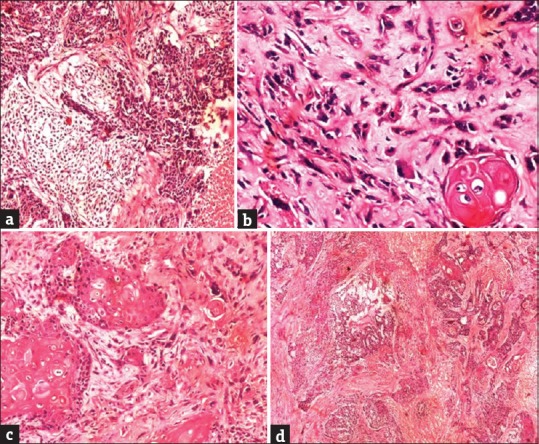
(a) Nests of tumor cells with intermingled stromal component (H and E, ×100), (b) sarcomatous component with a myxoid background (H and E, ×200), (c) squamous differentiation in the tumor (H and E, ×100), (d) nests of tumor cells with intermingled stromal component (H and E, ×40)
DISCUSSION
Radiation is a mainstay of the treatment for locally advanced cervical cancer, as the sole treatment in the past and concurrent with chemotherapy at present. Cervical cancer survivors have 80% increased risk to develop a second malignancy when compared to the general population. Treatment with RT was found to be important predictors that increased the risk for second cancer in cervical cancer survivors.[2] Uterine sarcoma was mostly reported in patients treated with RT for cervical cancer.[3]
Secondary uterine sarcomas occur in < 1% of patients treated with concurrent chemo-RT (CCRT). Secondary uterine sarcomas can occur more than 5 years from CCRT. The median survival period from the secondary tumor occurrence was only 4 months.
Wakayama et al. in a study of 313 patients with a prior history of CCRT for cervical cancer reported that three patients (0.96%) developed a primary second malignancy of the uterine corpus. The RT doses ranged from 58 to 64 Gy. The latency time from the CCRT to the development of the carcinosarcoma ranged from 68 to 118 months, with a median of 76 months.[4]
The mechanism of radiation-induced malignancies was not fully understood. Two mechanisms were proposed for the pathogenesis of radiation-induced malignancies. With low-dose radiation exposure, radiation single- and double-strand DNA breaks occur. The double-strand DNA breaks lead to gene mutation and malignant transformation of the radiated cell. On the other hand, the occurrence of cancer after high-dose radiation exposure is explained the bystander or abscopal effect. The release of soluble factors and charged particles from radiated cells crosses the gap junction into the normal cells. This induced inflammatory cytokines resulting in a release of reactive oxygen causing DNA damage.
There have been no standard criteria for a diagnosis of RT-associated cancer. Some proposed the following issues for diagnosis: (i) the development of sarcoma must be within a previously irradiated field; (ii) patients should have received a significant amount of radiation; (iii) a latency period of several years (at least 3–5 years) must elapse between the time of radiation and the development of the sarcoma; (iv) the diagnosis of the sarcoma must be histologically proven; and (v) the second sarcoma should have different histopathology from the primary neoplasm.[5,6] Our case satisfied the above-mentioned criteria although it cannot be completely ruled out that the occurrence of uterine carcinosarcoma in this patients might be de novo. There were no other well-recognized predisposing factors for uterine carcinosarcoma, such as obesity, diabetes mellitus, or metabolic syndrome, which may contribute to the cause of carcinosarcoma.[7]
CONCLUSION
Patients treated with definitive radiation therapy for invasive cervical cancer may still have viable endometrium at risk for neoplasia.
For those patients who received irradiation, a long-term follow-up with extreme caution is mandatory and Pap's smear should be the standard management.
For patients who present with any types of symptoms, post-RT should be aggressively investigated by imaging modalities and tissue biopsy and managed accordingly.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lee B, Ahn SH, Kim H, Son J, Sung J, Han Y, et al. Secondary cancer-incidence risk estimates for external radiotherapy and high-dose-rate brachytherapy in cervical cancer: Phantom study. J Appl Clin Med Phys. 2016;17:124–32. doi: 10.1120/jacmp.v17i5.6087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arnold M, Liu L, Kenter GG, Creutzberg CL, Coebergh JW, Soerjomataram I, et al. Second primary cancers in survivors of cervical cancer in the Netherlands: Implications for prevention and surveillance. Radiother Oncol. 2014;111:374–81. doi: 10.1016/j.radonc.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 3.Behtash N, Tehranian A, Ardalan FA, Hanjani P. Uterine papillary serous carcinoma after pelvic radiation therapy for cancer of the cervix J. Obst and Gynaecol. 2002;22:96–7. doi: 10.1080/01443610211114. [DOI] [PubMed] [Google Scholar]
- 4.Wakayama A, Kudaka W, Nakasone T, Taira Y, Aoki Y. Secondary uterine carcinosarcoma after concurrent chemoradiotherapy for cervical cancer: Case reports. Gynecol Oncol Rep. 2017;21:81–3. doi: 10.1016/j.gore.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsieh TC, Kao CH, Wu YC, Hsu CN, Wang CH, Lin YY, et al. Fulminant postirradiation soft tissue sarcoma. Clin Nucl Med. 2009;34:811–4. doi: 10.1097/RLU.0b013e3181b7d994. [DOI] [PubMed] [Google Scholar]
- 6.Cahan WG, Woodard HQ, Higinbotham NL, Stewart FW, Coley BL. Sarcoma arising in irradiated bone: Report of eleven cases 1948. Cancer. 1998;82:8–34. doi: 10.1002/(sici)1097-0142(19980101)82:1<8::aid-cncr3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 7.Menczer J. Review of recommended treatment of uterine carcinosarcoma. Curr Treat Options Oncol. 2015;16:53. doi: 10.1007/s11864-015-0370-4. [DOI] [PubMed] [Google Scholar]


