Abstract
Purpose
This study aimed to evaluate the current status of reproductive disorders as long‐term complications in adolescent and young adult (AYA) cancer patients by comparing survivors of childhood‐onset with those of AYA‐onset cancer in Japan.
Methods
We conducted a national survey of AYA cancer survivors and healthy AYAs and analyzed the results from survivors who underwent chemotherapy and reported fertility problems as their current concern.
Results
Among all of the childhood‐onset survivors, 27 (35.5%; nine males [28.1%] and 18 females [40.9%]) listed reproduction fertility problems as their current concern. Among all AYA‐onset survivors, 25 (69.5%; 1/4 males [25.0%] and 24/32 females [75.0%]) listed these problems as a current concern. In contrast, 96.3% (26/27) of all childhood‐onset cancer survivors and 68.0% (17/25) of all AYA‐onset cancer survivors who received chemotherapy listed these problems as a current concern.
Conclusions
A considerable number of both childhood‐onset and AYA‐onset cancer survivors, and especially those who had undergone chemotherapy, reported reproductive dysfunction as a delayed complication. It is vitally important to establish a supportive care system both for the patients whose fertility was abolished after the completion of cancer treatment and prophylactically for patients before they begin treatment.
Keywords: adolescent, cancer survivors, fertility preservation, reproduction, young adults
1. INTRODUCTION
Total‐body irradiation, irradiation of the gonads, and chemotherapy regimens containing high doses of alkylators can place adolescent and young adult (AYA) patients with cancer at risk of subfertility after the successful completion of cancer treatment. Multiple studies have shown that cancer survivors have decreased measures of ovarian reserve compared with unexposed women of similar age.1 Depletion of the follicular pool may manifest clinically as menstrual cycle irregularity, subfertility, and primary ovarian insufficiency. Even among those who resume regular menses after treatment, the risks of infertility and primary ovarian insufficiency are increased.2, 3 Accelerated reproductive aging in cancer survivors of mid‐reproductive age parallels observations during natural reproductive aging in women of late‐reproductive age.4
We carried out a large‐scale national survey of AYA cancer survivors that included investigation of reproductive issues to reveal the current problems and needs of these survivors in Japan. This report, which analyzes the reproductive function and fertility of AYAs gained through this national survey, is the first in Japan to reveal the frequency of problems related to the reproductive function of AYA cancer survivors with childhood and AYA onset of cancer and its relationship with chemotherapy.
2. MATERIALS AND METHODS
2.1. Definitions
We defined “child(ren)” as individual(s) of ≤15 years of age, “adolescents and young adults (AYAs)” as individuals of 16‐39 years of age, “survivors” as individuals who had completed their cancer therapy at least 12 months previously, and “healthy AYAs” as AYAs who never been diagnosed as having cancer.
2.2. Surveys
We distributed questionnaires in this national survey to AYA cancer survivors via their doctors and a patient advocacy group from June 2016 to November 2016. The selection of survivors was made with the help of staff cooperating with the survey researchers in facilities participating in this study, the secretariats of most of the cancer‐related associations and societies in Japan, and the community through cancer clinics and patient organizations.
Two hundred healthy AYAs registered with a research company were also recruited to answer a web‐based questionnaire. The healthy AYAs were divided into four age‐groups with 50 people (25 men and 25 women) in each age‐group (Table 1).
Table 1.
Respondents’ characteristics
| Respondents | Sex | N | Age in years | |||
|---|---|---|---|---|---|---|
| 15‐19 | 20‐24 | 25‐29 | 30‐39 | |||
| Healthy AYA | All | 200 | 50 | 50 | 50 | 50 |
| Male | 100 | 25 | 25 | 25 | 25 | |
| Female | 100 | 25 | 25 | 25 | 25 | |
| AYA cancer survivors | 118 | Onset | Current | Gynecologic/Breast | ||
| Childhood onset | All | 76 | 7.57 ± 4.54 | 24.0 ± 5.98 | ||
| Male | 32 | 7.69 ± 4.21 | 23.0 ± 5.57 | |||
| Female | 44 | 7.48 ± 4.81 | 24.7 ± 6.23 | |||
| AYA onset | All | 36 | 27.5 ± 5.78 | 33.2 ± 4.83* | 7/9 | |
| Male | 4 | 21.3 ± 6.18 | 31.8 ± 2.63** | |||
| Female | 32 | 28.3 ± 5.32 | 33.4 ± 5.03*** | 7/9 | ||
| Female excluding gynecologic tumors | 26 | 29.1 ± 4.97 | 33.6 ± 5.01*** | 0/9 | ||
AYA, adolescent and young adult.
Age: mean ± SD. Responders who did not record their sex, age of onset, and current age were excluded.
P < 0.001 vs overall with childhood onset, Student's t test.
P < 0.005 vs males with childhood onset, Student's t test.
P < 0.001 vs females with childhood onset, Student's t test.
2.3. Questionnaire
The questionnaire included questions on the topics of disease, influence and support, decision making and communication, health and mental status, reproductive function and fertility, education, work, economic status, self‐management, and background of the respondents (Figure 1).
Figure 1.
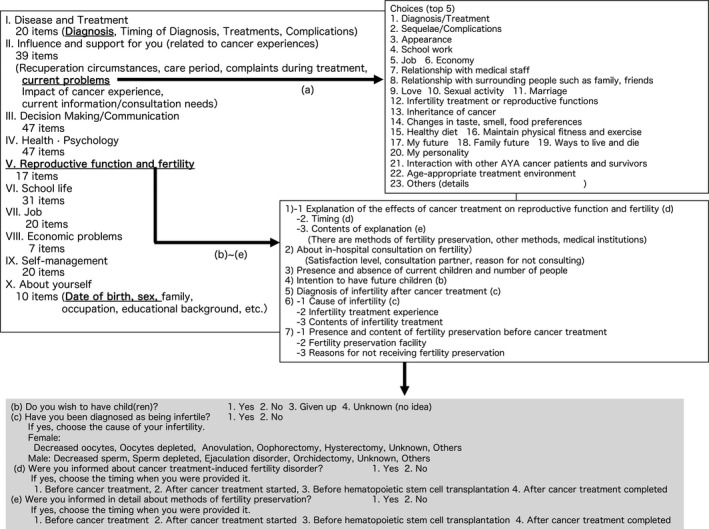
Outline of the questionnaire contents. The specific questions and answers related to reproductive function are shown in the gray‐colored box
2.4. Statistical analysis
In this study, only responders who completed the questions related to reproductive function in the questionnaire were analyzed. A Student's t test and Pearson's chi‐square test were used for comparisons of age of the responders and responses related to the problems of cancer survivors and healthy AYAs, respectively. Differences were considered significant when P < 0.01.
2.5. Human/Animal rights
This article does not contain any studies with human and animal subjects performed by any of the authors.
2.6. Approval by Ethics Committee
This study was approved by the ethics review board of Gifu University Hospital (approval no. 28‐126). The work was conducted as a joint study by a working group tasked with the “Study on the ideal way of comprehensive care for adolescents and young adults (AYA) with cancer” (Principal Investigator: Keizo Horibe).
3. RESULTS
We distributed 752 copies of the survivor survey form, and 261 forms (34.7%) were collected from the respondents. Among them, 112 people completed the questions on reproductive function.
3.1. Demographic information of the participants
These 112 respondents included 76 with childhood onset and 36 with AYA onset of cancer. The age of onset and current age of the 32 males and 44 females with childhood onset were 7.69 ± 4.21 and 23.0 ± 5.57 years in the males and 7.48 ± 4.81 and 24.7 ± 6.23 years in the females, respectively. All of the responders with a primary disease of gynecologic and breast cancer were females with onset as young adults.
The age of onset and current age of the four males and 32 females with AYA onset were 21.3 ± 6.18 and 31.8 ± 2.63 years in the males, 28.3 ± 5.32 and 33.4 ± 5.03 years in the females, and 29.1 ± 4.97 and 33.6 ± 5.01 years in the female cancer survivors with nongynecologic disease, respectively. The current mean age of the cancer survivors with AYA onset was significantly higher than that of the pediatric cancer survivors among the males, females, and females with nongynecologic cancer (Table 1).
The primary diseases of the respondents were leukemia in 15 males and 12 females, malignant lymphoma in three males and four females, brain tumor in six male and three female survivors of childhood‐onset cancer, breast cancer in nine and gynecologic cancer in seven females, brain tumor in two males, and leukemia and rhabdomyosarcoma in one male each among the survivors of AYA‐onset cancer (Table 2).
Table 2.
Primary diseases of the respondents
| Female | Male | |
|---|---|---|
| Childhood onset | ||
| Leukemia | 15 | 12 |
| Malignant lymphoma | 3 | 4 |
| Brain tumor | 6 | 3 |
| Rhabdomyosarcoma | 2 | 3 |
| Osteosarcoma | 3 | 1 |
| Hepatoblastoma | 0 | 1 |
| Neuroblastoma | 0 | 1 |
| Retinoblastoma | 0 | 1 |
| Others | 4 | 1 |
| Not recorded | 11 | 5 |
| AYA onset | ||
| Breast cancer | 9 | 0 |
| Brain tumor | 1 | 2 |
| Leukemia | 2 | 1 |
| Uterine cervical cancer | 3 | 0 |
| Ovarian cancer | 3 | 0 |
| Uterine corpus cancer | 1 | 0 |
| Thyroid cancer | 1 | 0 |
| Rhabdomyosarcoma | 0 | 1 |
| Others | 1 | 0 |
| Not recorded | 11 | 0 |
3.2. Reproductive problems of AYA cancer survivors as a current concern
Table 3 summarizes the survivors of childhood‐onset and AYA‐onset cancer who listed reproductive function in their top 5 “current problems” compared with healthy AYA controls. Five of the 200 healthy AYAs (two males and three females) and 52 of the 112 (46.4%) AYA survivors in total, including 10 of 36 (27.8%) males and 42 of 76 (55.3%) females, were concerned about their reproductive problems.
Table 3.
Healthy AYA and cancer survivors who listed reproduction and fertility problems as current concerns
| Respondents | Sex | n | Reproduction and fertility problems listed as current concerns (%) |
|---|---|---|---|
| Healthy AYA | All | 200 | 5 (2.5) |
| Male | 100 | 2 (2.0) | |
| Female | 100 | 3 (3.0) | |
| AYA cancer survivorsa | 118 | 52 (44.1)* | |
| Childhood onset | All | 76 | 27 (35.5)* |
| Male | 32 | 9 (28.1)* | |
| Female | 44 | 18 (40.9)* | |
| AYA onset | All | 36 | 25 (69.5)* , † |
| Male | 4 | 1 (25.0)ns,ns | |
| Female | 32 | 24 (75.0)* , † | |
| Female excluding gynecologic tumors | 26 | 22 (84.6)* , † |
AYA, adolescent and young adult; ns, not significant.
Including those with no recorded sex and/or onset.
P < 0.01 vs healthy AYA, Pearson's chi‐square test
P < 0.01 vs AYA onset, Pearson's chi‐square test
According to the time of onset, nine of 32 males (28.1%) and 18 of 44 females (40.9%) surviving childhood‐onset cancer and one of four males (25.0%), 24 of 32 females (75.0%), and 22 of 26 females (84.6%) with nongynecologic cancer surviving AYA‐onset cancer listed reproduction and fertility problems as current concerns. Reproductive concerns were significantly higher in the female survivors than in the healthy AYAs (Table 3).
3.3. Chemotherapy experience in the cancer survivors with reproductive problems
Of the 27 survivors of childhood‐onset cancer reporting current problems with reproduction, 26 (96.3%) had received anticancer drug treatment. Among them, nine of nine (100%) were male and 17 of 18 (94.4%) were female. Of the 17 survivors of AYA‐onset cancer with current problems of reproduction, 17 (68.0%) had received chemotherapy. Among them, one of one (100%) was male, 16 of 24 (66.7%) were female, and 18 of 22 (81.8%) were female with nongynecologic diseases (Table 4).
Table 4.
Reproduction and fertility problems of AYA cancer survivors who had received chemotherapy
| Respondents | Sex | n | Reproduction and fertility problems listed as current concerns (%) |
|---|---|---|---|
| AYA cancer survivorsa | 52 | 43 (82.7) | |
| Childhood onset | All | 27 | 26 (96.3) |
| Male | 9 | 9 (100) | |
| Female | 18 | 17 (94.4) | |
| AYA onset | All | 25 | 17 (68.0) |
| Male | 1 | 1 (100) | |
| Female | 24 | 16 (66.7) | |
| Female excluding gynecologic tumors | 22 | 18 (81.8) | |
AYA, adolescent and young adult.
Including those with no recorded sex and/or onset.
4. DISCUSSION
As a result of this survey, the proportion of cancer survivors among the AYAs who had a problem with reproductive function and infertility was higher than that of the AYA healthy controls regardless of whether cancer onset occurred in childhood or AYA except for the males with AYA‐onset cancer of whom there were few respondents. This tendency was more pronounced in the survivors of AYA‐onset cancer (69.5%) than in those of childhood‐onset cancer (35.5%).
This might be why the present mean age of the survivors with childhood‐onset cancer (24.0 years old) was significantly lower than that of the survivors of AYA‐onset cancer (33.2 years old). The present age of the survivors of AYA‐onset cancer is almost the same as the average age of first marriage in Japan in 2015, which was 33.3 years old in men and 31.1 years old in women. This might be a major reason why more AYA‐onset survivors had reproductive concerns than did childhood‐onset survivors. However, it is strikingly important that 28.1% of the males and 40.9% of the females reported some problems in reproductive functions and fertility even among the survivors of childhood‐onset cancer.
In addition, among the survivors reporting troubles with reproductive function and infertility, 82.7% overall, 96.3% surviving childhood‐onset, and 68.0% surviving AYA‐onset cancer had received anticancer drug therapy. Even though many of the survivors of childhood‐onset cancer are relatively young, they still had troubles with reproductive function.
The present study showed that many survivors of childhood‐onset cancer whose primary diseases were mainly hematological disease or sarcoma might have received high‐dose chemotherapy including alkylators. Some of them could have recovered their regular menstrual cycle such that they would not notice that their ovarian reserve had been severely decreasing until they reached the AYA stage.
Based on the results of this survey, it is necessary to further improve the medical care system to provide information prior to anticancer drug treatment,5 preserve fertility, and manage mental and medical care related to reproductive function after cancer treatment for those with both AYA‐onset and childhood‐onset cancer. Other data from this same survey also revealed that there might be a huge number of AYA cancer survivors who were never informed about potential harm to their reproductive function and the possibility of fertility preservation before and/or during their cancer treatment (T. Furui, Y. Takai, F. Kimura, M. Kitajima, M. Nakatsuka, K. Morishige, A. Higuchi, C. Shimizu, M. Ozawa, A. Ohara, R. Tatara, T. Nakamura,K. Horibe, & N. Suzuki, unpublished data). It is vitally important to establish a supportive care system both for the patients whose fertility was abolished after the completion of cancer treatment and prophylactically for patients before they begin treatment. Because this study analyzed only questions related to the preservation of reproductive function from a very wide range of questions posed to the AYA cancer survivors, further information on the reproductive function of these survivors and their actual status regarding fertility preservation could not be examined in great detail. As a next step, we would like to focus on the points that could not be clearly elucidated in the present study through specialized research on fertility and reproductive function.
DISCLOSURES
This study was approved by the ethics review board of Gifu University Hospital (approval no. 28‐126).
Conflict of interest: Tatsuro Furui, Yasushi Takai, Fuminori Kimura, Michio Kitajima, Mikiya Nakatsuka, Ken‐ichiro Morishige, Akiko Higuchi, Chikako Shimizu, Miwa Ozawa, Akira Ohara, Ryohei Tatara, Terukazu Nakamura, and Nao Suzuki declare that they have no conflict of interest. Keizo Horibe received research funding from Pfizer Inc
Furui T, Takai Y, Kimura F, et al. Problems of reproductive function in survivors of childhood‐ and adolescent and young adult‐onset cancer revealed in a part of a national survey of Japan. Reprod Med Biol. 2019;18:105–110. 10.1002/rmb2.12255
REFERENCES
- 1. Dillon KE, Sammel MD, Prewitt M, et al. Pretreatment antimullerian hormone levels determine rate of posttherapy ovarian reserve recovery: acute changes in ovarian reserve during and after chemotherapy. Fertil Steril. 2013;99:477‐483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chiarelli AM, Marrett LD, Darlington G. Early menopause and infertility in females after treatment for childhood cancer diagnosed in 1964‐1988 in Ontario, Canada. Am J Epidemiol. 1999;150:245‐254. [DOI] [PubMed] [Google Scholar]
- 3. Sklar CA, Mertens AC, Mitby P, et al. Premature menopause in survivors of childhood cancer: a report from the childhood cancer survivor study. J Natl Cancer Inst. 2006;98:890‐896. [DOI] [PubMed] [Google Scholar]
- 4. Gracia CR, Sammel MD, Freeman E, et al. Impact of cancer therapies on ovarian reserve. Fertil Steril. 2012;97:134‐140.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31:2500‐2510. [DOI] [PMC free article] [PubMed] [Google Scholar]


