Abstract
Most of the plants used by herbalists amongst the various Kenyan communities have not been documented despite their widespread use. The purpose of this research was to document the medicinal plants used by the herbalists from the Maasai, a community that still relies on herbal medicine to a large extent for the provision of medical services. Semistructured interviews, direct observations, group discussions, and in-depth interviews were used to collect information from the traditional healers. A total of 47 plant species belonging to 31 families were identified. They were used in the treatment of 33 medical and 4 veterinary conditions.
1. Introduction
Medicinal plants still play an important role in primary healthcare in many sub-Saharan African countries due to variety of reasons including lack of health services, cultural norms, and traditional beliefs [1–3]. Many patients in these countries combine traditional medicine (TM) with conventional medicine, especially those with chronic diseases [4]. The use of TM is in most cases widespread and not only limited to the rural areas or low-income settings, but also in urban and well to do settings [3, 5, 6]. In addition, there is a growing global demand for traditional and complementary medicine [2]. The knowledge of these medicinal preparations is therefore important in order to enable health practitioners to be aware of the kind of TM their patients are on, so as to minimize potential adverse effects resulting from herb-drug interactions [7]. The documentation of the type of medicinal plants used by the traditional medical practitioners (TMPs) and the conditions treated is crucial to this endeavor [4]. In addition, databases containing this information would also be important for research and potential development of new drugs, as many of the drugs in current use have been developed from medicinal plants [8, 9]. Examples of these include paclitaxel, an antitumour drug developed from the bark of T. brevifolia [10], the antimalarial drug artemisinin from Artemisia annua [11], digoxin from Digitalis lanata, atropine from Atropa belladona, aspirin from Filipendula ulmaria, and several other drugs. However, despite the widespread use of medicinal plants in Kenya, several have not been documented [4, 12]. The main aim of this research was to document the medicinal plants used by the Maasai community in Narok County, one of the regions in Kenya whereby the practice of herbal medicine is still widespread for future research.
2. Materials and Methods
2.1. Study Area
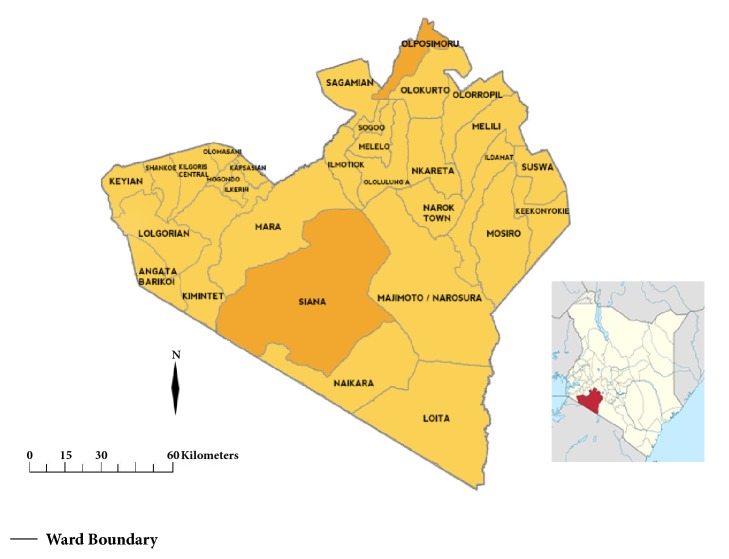
The study was conducted in two locations within Narok County, Olpusimoru (2°1′0′′S, 36°54′0′′E) a highland area located in the Northern part; and Sekenani (1°30′58.33′′S, 35°20′19.63′′E) a lowland area located in the South-Western region [Siana Ward] [Figure 1]. Olpusimoru is a mountainous forested terrain with an average altitude of 2478 metres and high rainfall, while Sekenani has an average altitude of 1820 m with comparatively low rainfall. It borders the globally famous Maasai Mara National Reserve on the East [13, 14].
Figure 1.
Map of Narok County showing Olpusimoru and Siana wards and its position within Kenyan map.
2.2. Data Collection
Ethnobotanical data was collected from TMPs between March and December 2016. The research team is comprised of professionals from the medical field and botany, including a physician (EN), two clinical pharmacologists (GK and ZK), a taxonomist (BW), and a plant specialist (WK). There were also two local lead persons, one from each site who accompanied the team at each visit in order to direct and introduce them to the TMPs. All TMPs that we met were willing to participate in the research. A total of 37 TMPs comprising 20 men and 17 women aged between 42 and 85 were interviewed. Semistructured interviews, direct observations, group discussions, and in-depth interviews were used to collect ethnopharmacological information [15–17]. The participant's biodata, conditions they treated, methods of treatment, medicinal plants used, methods of preparation and administration, and dosing forms were recorded. They were also asked to explain the manner in which they arrived at a diagnosis. At the end of each interview, the informants were requested to accompany the research team to sites where they collected the plants and assist in identification. Preliminary identification of the plants was then done by BW and WK, and the plants and their surrounding habitats photographed. The voucher specimens were then collected using standard botanical procedures, and further identification and confirmation were performed using the relevant taxonomic keys at University of Eldoret Herbarium where the specimens were subsequently deposited [18, 19]. The data was then compared to related research that has been carried out in the region.
2.3. Data Analysis
The medicinal importance of each plant species used was calculated as per the use-value index for each plant species (UVs) using the formula:
| (1) |
where U is the number of different uses mentioned by each TMP (informant) whereas N is the total number of TMPs interviewed during the survey [20, 21]. The UV index theoretically varies from 0, which implies that none of the informants mention any use of the plant, to 1 whereby the plant is most frequently mentioned as useful in treatment of the highest number of conditions.
3. Results and Discussion
A total of 47 plant species belonging to 31 families were identified, out of which 36 (77%) were from the lowland area (Sekenani), while 11 (23%) species were from the highlands (Olpusimoru) [Table 1]. The plant details including the voucher numbers are outlined in Table 2.
Table 1.
Classification of medicinal plants.
| Family | Species | ||
|---|---|---|---|
| No | Members | ||
|
| |||
| 1. | FABACEAE | 5 | Albizia gummifera, Dichrostachys cinerea, Erythrina senegalensis, Senegalia senegal, Vachellia nilotica |
|
| |||
| 2. | SOLANACEAE | 4 | Physalis peruviana, Solanum arundo, Solanum incanum, Solanum mauense |
|
| |||
| 3. | AMARANTHACEAE | 2 | Achyranthes aspera, Aerva javanica |
|
| |||
| 4. | APOCYNACEAE | 2 | Acokanthera schimperi, Carissa edulis |
|
| |||
| 5. | BURSERACEAE | 2 | Commiphora africana, Ficus sycomorus |
|
| |||
| 6. | CELASTRACEAE | 2 | Elaeodendron buchananii, Mystroxylon aethiopicum |
|
| |||
| 7. | EUPHORBIACEAE | 2 | Clutia abyssinica, Croton dichogamous |
|
| |||
| 8. | MALVACEAE | 2 | Grewia bicolor, Sida cuneifolia |
|
| |||
| 9. | RHAMNACEAE | 2 | Rhamnus prinoides, Ziziphus mucronata |
|
| |||
| 10. | RUBIACEAE | 2 | Galium aparinoides, Pavetta subcana |
|
| |||
| 11. | RUTACEAE | 2 | Teclea nobilis, Toddalia asiatica |
|
| |||
| 12. | APIACEAE | 1 | Anthriscus sylvestris |
|
| |||
| 13. | ASPARAGACEAE | 1 | Asparagus africanus |
|
| |||
| 14. | ASTERACEAE | 1 | Acmella calirhiza |
|
| |||
| 15. | BIGNONIACEAE | 1 | Kigelia africana |
|
| |||
| 16. | BORAGINACEAE | 1 | Cordia monoica |
|
| |||
| 17. | CANELACEAE | 1 | Warburgia ugandensis |
|
| |||
| 18. | CAPPARIDACEAE | 1 | Boscia angustifolia |
|
| |||
| 19. | COLCHICACEAE | 1 | Gloriosa superba |
|
| |||
| 20. | COMMELINACEAE | 1 | Aneilema equinoctiale |
|
| |||
| 21. | CRASSULACEAE | 1 | Kalanchoe crenata |
|
| |||
| 22. | CUCURBITACEAE | 1 | Momordica friesiorum |
|
| |||
| 23. | EBENACEAE | 1 | Diospyros abyssinica |
|
| |||
| 24. | FLACOURTIACEAE | 1 | Dovyalis abyssinica |
|
| |||
| 25. | LABIATAE | 1 | Leonotis mollissima |
|
| |||
| 26. | OLEACEAE | 1 | Olea europaea subsp. cuspidata |
|
| |||
| 27. | PRIMULACEAE | 1 | MyrsineaAfricana |
|
| |||
| 28. | ROSACEAE | 1 | Prunus africana |
|
| |||
| 29. | SANTALACEAE | 1 | Osyris lanceolata |
|
| |||
| 30. | SAPINDACEAE | 1 | Pappea capensis |
|
| |||
| 31. | VITACEAE | 1 | Cissus fischeri |
|
| |||
| Total | 47 | ||
Table 2.
Medicinal plant uses.
| No | Botanical Name | Family | Voucher No. | Maa name | Habitat | Parts used | Method of preparation | Medicinal uses |
|---|---|---|---|---|---|---|---|---|
| 1. | Achyranthes aspera L. | AMARANTHACEAE | OLP/08/15/007 | Olerubat | Highland | Roots | Boiled | Arthritis |
|
| ||||||||
| 2. | Acmella calirhiza Del | ASTERACEAE | OLP/08/15/009 | Ekum | Highland | Flowers | Crushed and mixed with water | Oral thrush in children |
|
| ||||||||
| 3. | Acokanthera schimperi (A.DC.) Schweinf | APOCYNACEAE | MAU/08/15/027 | Olmorijioi | Lowland | Roots | Boiled | Syphilis |
| Bark | Soaked in water | Arrow poison | ||||||
|
| ||||||||
| 4. | Aerva javanica (Burm.f.) Shult. | AMARANTHACEAE | MAU/08/15/032 | Eleleshwa-ekop | Lowland | Flowers | Ground into paste & mixed with water | East Coast Fever in cattle |
|
| ||||||||
| 5. | Albizia gummifera (J.F. Gmel.) C.A.Sm. | FABACEAE | MAU/08/15/018 | Osupakupe | Lowland | Pods | Crushed | Stomachache |
| Roots | Pounded | Skin disorders | ||||||
|
| ||||||||
| 6. | Aneilema aequinoctiale P. Beauv | COMMELINACEAE | MAU/08/15/020 | Enkaiteteyiai | Lowland | Leaves | Soaked in water | Malnutrition, colds |
| Flowers | Pressed to produce juice | Ocular disorders | ||||||
|
| ||||||||
| 7. | Anthriscus sylvestris (L.) Hoffm | APIACEAE | MAU/08/15/028 | Oldule | Lowland | Seeds | Mixed with honey and chewed | Chesty colds |
|
| ||||||||
| 8. | Asparagus africanus Lam | ASPARAGACEAE | MAU/08/15/006 | Empereempapa | Lowland | Leaves, stem & roots | Soaked in water | Mental illness |
| Leaves | Soaked in water | Wounds | ||||||
| Roots | Soaked in water | Venereal diseases | ||||||
| Chewed | Cough & sore throat | |||||||
|
| ||||||||
| 9. | Boscia angustifolia Harvey | CAPPARIDACEAE | MAU/08/15/001 | Oloireroi | Lowland | Leaves | Pounded | Cattle fever |
| Bark | Crushed & mixed with water | Gynaecological disorders | ||||||
|
| ||||||||
| 10. | Carissa edulis Harv | APOCYNACEAE | MAU/08/15/003 | Olamuriaki | Lowland | Roots | Boiled | Lower abdominal pains in pregnancy, gonorrhea, chest pains, polio symptoms |
|
| ||||||||
| 11. | Cissus fischeri Gilg | VITACEAE | MAU/08/15/011 | Osurkurtuti | Lowland | Leaves | Soaked in water | Respiratory disorders in cattle |
|
| ||||||||
| 12. | Clutia abyssinica Jaub. & Spach. | EUPHORBIACEAE | OLP/08/15/011 | Enkiparnyeny | Highland | Roots | Boiled | Appetizer |
|
| ||||||||
| 13. | Commiphora africana (A. Rich.) Endl | BURSERACEAE | MAU/08/15/034 | Osilalei | Lowland | Roots | Boiled | Swollen testicles, abdominal pains |
| Bark | Chewed | Snake bite | ||||||
| Fruits | Boiled | Typhoid | ||||||
|
| ||||||||
| 14. | Cordia monoica Roxb | BORAGINACEAE | MAU/08/15/031 | Oseki | Lowland | Leaves, bark | Leaves- boiled, bark - pounded | Leprosy |
| Roots | Boiled | Mental illness | ||||||
| Leaves | Pounded | Ocular disorders | ||||||
|
| ||||||||
| 15. | Croton dichogamous Pax | EUPHORBIACEAE | MAU/08/15/008 | Ollokirdangai | Lowland | Roots | Boiled | Polio-like symptoms, gonorrhea, chest pain |
|
| ||||||||
| 16. | Dichrostachys cinerea Wight et Arn | FABACEAE | MAU/08/15/009 | Emerrumori | Lowland | Leaves | Pounded | Local anaesthesia, ulcers, gonorrhea |
|
| ||||||||
| 17. | Diospyros abyssinica Hiern | EBENACEAE | MAU/08/15/025 | Olchartuyian | Lowland | Bark | Pounded & soaked in water | Malaria, ocular d/orders in livestock |
|
| ||||||||
| 18. | Dovyalis abyssinica (A. Rich.) Warb | FLACOURTIACEAE | OLP/08/15/006 | Olmorogi | Highland | Roots | Boiled | Gonorrhea |
| Leaves | Chewed | Toothache | ||||||
|
| ||||||||
| 19. | Elaeodendron buchananii (Loes) Loes. | CELASTRACEAE | MAU/08/15/004 | Osoket | Lowland | Roots | Dried and ground to powder | Wounds, syphilis |
| Roots | Boiled or dried and ground to powder | Respiratory d/orders | ||||||
| Leaves | Chewed | Diarrhoea | ||||||
|
| ||||||||
| 20. | Erythrina senegalensis DC. | FABACEAE | MAU/08/15/036 | Ol-oboni | Lowland | Roots | Boiled | Polio-like symptoms, gonorrhea, chest pain |
|
| ||||||||
| 21. | Ficus sycomorus L. | BURSERACEAE | MAU/08/15/024 | Olngaboli | Lowland | Roots | Boiled, chewed | Abortifacient |
|
| ||||||||
| 22. | Galium aparinoides Forssk | RUBIACEAE | MAU/08/15/026 | Olngeriantus | Lowland | Whole plant | Pounded & soaked in water or boiled | Throat cancer in cattle |
|
| ||||||||
| 23. | Gloriosa superba L. | COLCHICACEAE | MAU/08/15/022 | Sakutayei | Lowland | Roots | Chewed or soaked in water | Abortifacient |
|
| ||||||||
| 24. | Grewia bicolor | MALVACEAE | MAU/08/15/014 | Ositeti | Lowland | Roots | Soaked in water | Respiratory d/orders, snake bite |
|
| ||||||||
| 25. | Kalanchoe crenata (Andrews) Haw | CRASSULACEAE | OLP/08/15/008 | Ormasilig | Highland | Leaves | Warmed | Poultice |
|
| ||||||||
| 26. | Kigelia africana (Lam.) Benth. | BIGNONIACEAE | MAU/08/15/021 | Oldarpoi | Lowland | Fruits | Brewed | Measles in children |
| Roots | Boiled | Abortifacient | ||||||
| Bark | Boiled | Headache | ||||||
| Leaves | Boiled | Malaria | ||||||
|
| ||||||||
| 27. | Leonotis mollissima Guerke | LABIATAE | OLP/08/15/003 | Olbibi | Highland | Leaves | Soaked in water or boiled | Antiseptic, skin rashes, blood purifier |
|
| ||||||||
| 28. | Momordica friesiorum (Harms) C. Jeffrey | CUCURBITACEAE | OLP/08/15/001 | Esumeito | Highland | Roots | Pounded & mixed with water | Induce vomiting |
|
| ||||||||
| 29. | Myrsine Africana L. | PRIMULACEAE | OLP/08/15/004 | Seketet | Highland | Seeds | Ground | Antihelminthic, heartburn |
|
| ||||||||
| 30. | Mystroxylon aethiopicum (Thunb.) Loes. | CELASTRACEAE | MAU/08/15/035 | Olodonganayioi | Lowland | Bark | Boiled | Colic pain, especially in children |
|
| ||||||||
| 31. | Olea europaea subsp. cuspidata (Wall. ex G. Don) Cif. | OLEACEAE | MAU/08/15/023 | Oloirien | Lowland | Bark | Pounded and soaked in water | Antihelminthic |
| Leaves | Boiled | Liver disease | ||||||
| Roots | Boiled | Polio-like symptoms, gonorrhea, chest pain | ||||||
|
| ||||||||
| 32. | Osyris lanceolata Hochst. & Steud. ex A. DC. | SANTALACEAE | MAU/08/15/016 | Olosesiai | Lowland | Bark | Boiled | Abdominal pains in children |
| Leaves | Pounded | Diarrhoea | ||||||
| Roots | Boiled | Gonorrhea | ||||||
|
| ||||||||
| 33. | Pappea capensis Eckl. & Zeyh | SAPINDACEAE | MAU/08/15/029 | Olkisik-ongo | Lowland | Bark | Boiled | Abdominal disorders |
|
| ||||||||
| 34. | Pavetta subcana Hiern. | RUBIACEAE | MAU/08/15/002 | Olabai | Lowland | Roots | Boiled | Gonorrhea |
| Whole plant | Soaked in water | Cough in calves, fleas | ||||||
|
| ||||||||
| 35. | Physalis peruviana L. | SOLANACEAE | OLP/08/15/010 | Ormumai | Highland | Roots | Squeezed/chewed | Tonsillitis |
|
| ||||||||
| 36. | Prunus africana (Hook.f.) Kalkman | ROSACEAE | MAU/08/15/012 | Olkujuk | Lowland | Leaves | Pounded & soaked in water | Appetizer |
| Bark | Pounded & mixed with water | Stomachache | ||||||
|
| ||||||||
| 37. | Rhamnus prinoides L'Hér. | RHAMNACEAE | OLP/08/15/002 | Olkonyel | Highland | Roots | Boiled | Gonorrhea, arthritis |
| Stem | Pounded and mixed with water | Preservative | ||||||
|
| ||||||||
| 38. | Senegalia senegal (L.) Britton & P. Wilson | FABACEAE | MAU/08/15/010 | Oitioibor | Lowland | Roots | Boiled | Purgative, constipation & gonorrhea |
| Bark | Boiled | Diarrhoea & abdominal disorders | ||||||
|
| ||||||||
| 39. | Sida cuneifolia Roxb | MALVACEAE | MAU/08/15/005 | Olonini | Lowland | Roots | Chewed | Sore throat |
| Boiled | Reduce foetal movements in pregnancy | |||||||
|
| ||||||||
| 40. | Solanum arundo | SOLANACEAE | MAU/08/15/013 | Esokawai | Lowland | Roots | Chewed, pounded & soaked in water | Fever |
|
| ||||||||
| 41. | Solanum incanum L. | SOLANACEAE | MAU/08/15/015 | Entulelei | Lowland | Roots | Boiled | Abdominal pains, fever |
| Raw roots used | Toothache | |||||||
| Leaves | Chewed and applied | Snake bite | ||||||
| Fruits | Juice | Chest pain, wounds & skin disorders, Respiratory disorders in sheep | ||||||
|
| ||||||||
| 42. | Solanum mauense Bitter. | SOLANACEAE | MAU/08/15/007 | Olesayiet | Lowland | Berries | Cooked | Pneumonia |
| Roots | Boiled | Anthrax in both humans and animals | ||||||
|
| ||||||||
| 43. | Teclea nobilis Del. | RUTACEAE | MAU/08/15/019 | Olgilai | Lowland | Leaves, roots | Boiled | Pneumonia, arthritis |
|
| ||||||||
| 44. | Toddalia asiatica (L.) Lam | RUTACEAE | MAU/08/15/030 | Oleparmunyio | Lowland | Bark | Boiled or soaked in water | Respiratory disorders |
| Roots | Boiled | Malaria | ||||||
|
| ||||||||
| 45. | Vachellia nilotica (L.) P.J.H.Hurter & Mabb | FABACEAE | MAU/08/15/033 | Olkiloriti | Lowland | Bark | Pounded and mixed with water | Stomachache, indigestion |
|
| ||||||||
| 46. | Warburgia ugandensis Sprague. | CANELACEAE | OLP/08/15/005 | Osokonoi | Highland | Bark | Pound and mixed with water | Malaria, abdominal disorders |
| Boiled, ground to powder | Arthritis | |||||||
|
| ||||||||
| 47. | Zizyphus mucronata Willd. | RHAMNACEAE | MAU/08/15/017 | Oloilalei | Lowland | Roots | Soaked in water | Snake bite |
| Bark | Boiled | Arthritis, stomachache | ||||||
Medicinal Plant Uses. The plants were used in the treatment of 33 medical and 4 veterinary disorders. The detailed list of the plants and their respective medicinal uses are outlined in Table 2 and Supplementary Material section (available here). The most frequently used plant was Solanum incanum which had seven medical uses (UV = 0.19) followed by Olea europaea subsp. cuspidata which had five applications (UV = 0.14). Asparagus africanus, Carissa edulis, Commiphora africana, Elaeodendron buchananii, and Kigelia africana had four medicinal uses each (UV = 0.11).
Most of the plants used by traditional healers in Kenya have not documented despite the imminent risk of disappearance of this plants due to several factors including deforestation and overexploitation [4]. In addition, the practice is usually a guarded family secret, and some of the siblings may not be willing to inherit the art due to changing lifestyles [22]. The lack of adequate regulation of the practice in Kenya has also led to infiltration by several quacks. However, the Maasai is one community in Kenya which still practices TM to a large extent owing to several reasons including lack of adequate health facilities and traditional values [23]. Some of the reported plants have been evaluated in vitro and found to exhibit pharmacological activities related to the uses described by the TMPs [24]. These include Aerva javanica, Asparagus africanus, Carissa edulis, Sida cuneifolia, and Solanum incanum which have demonstrated to possess antibiotic/antifungal activities [25–28], while Gloriosa superba that is used as an abortifacient has oxytocic activity [29]. The plants used by the TMPs are largely similar to those used by their Kalenjin counterparts that we have reported before, although for different medicinal uses [3, 12, 30, 31]. Additionally, the methods of preparations are slightly different as the Maasai TMPs tend to use a lot of cold herbal infusions prepared by soaking the plant parts in water and hardly use the burnt leaves/barks as their counterparts
4. Conclusions
It is important to document traditional medicinal plants used by the various communities in Kenya in order to develop a database for future research. The risk of the rapid disappearance of the knowledge on traditional medicine calls for an urgent multidisciplinary approach towards conserving the information before it is lost forever. Some of these plants may contain undiscovered pharmacological properties which can serve as ingredients for the development of new drugs as has happened in Asia with the discovery of artemisinin. Additionally, medical personnel would also have an idea of the kind of herbal medicine that their patients may be taking and therefore minimize toxic effects through herb-drug interactions.
Acknowledgments
The authors are very grateful to John Ole Tira and Richard Ole Kuyo for their assistance in introduction to TMPs and identification of medicinal plants in Sekenani and Olpusimoru sites, respectively.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and/or its supplementary materials.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Supplementary Materials
Details of the medicinal plant uses.
References
- 1.Abdullahi A. A. Trends and challenges of traditional medicine in Africa. African Journal of Traditional, Complementary and Alternative Medicines. 2011;8:115–123. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. WHO Traditional Medicine Strategy 2014-2023. 2017. http://www.who.int/medicines/publications/traditional/trm_strategy14_23/en/ [Google Scholar]
- 3.Kipkore W., Wanjohi B., Rono H., Kigen G. A study of the medicinal plants used by the Marakwet Community in Kenya. Journal of Ethnobiology and Ethnomedicine. 2014;10, article 24 doi: 10.1186/1746-4269-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kigen G. K., Ronoh H. K., Kipkore W. K., JK R. Current trends of traditional herbal medicine practice in Kenya: a review. The African Journal of Pharmacology and Therapeutics. 2013;2(1):32–37. [Google Scholar]
- 5.Stanifer J. W., Patel U. D., Karia F., et al. The determinants of traditional medicine use in northern tanzania: a mixed-methods study. PLoS ONE. 2015;10(4):p. e0122638. doi: 10.1371/journal.pone.0122638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mhame P. P., Busia K., Kasilo O. M. Clinical Practices of African Traditional Medicine. Africa Health Monitor; 2010. [Google Scholar]
- 7.Fasinu P. S., Bouic P. J., Rosenkranz B. An overview of the evidence and mechanisms of herb–drug interactions. Frontiers in Pharmacology. 2012;3, article 69 doi: 10.3389/fphar.2012.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fabricant D. S., Farnsworth N. R. The value of plants used in traditional medicine for drug discovery. Environmental Health Perspectives. 2001;109(1):69–75. doi: 10.1289/ehp.01109s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sneader W. Drug Discovery: A History. Hoboken, New Jersey, NJ, USA: John Wiley and Sons, Ltd; 2005. [Google Scholar]
- 10.Wall M. E., Wani M. C. Camptothecin and taxol: discovery to clinic--thirteenth Bruce F. Cain Memorial Award Lecture. Cancer Research. 1995;55:753–760. [PubMed] [Google Scholar]
- 11.Miller L. H., Su X. Artemisinin: discovery from the Chinese herbal garden. Cell. 2011;146(6):855–858. doi: 10.1016/j.cell.2011.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kigen G., Kipkore W., Wanjohi B., Haruki B., Kemboi J. Medicinal plants used by traditional healers in Sangurur, Elgeyo Marakwet County, Kenya. Pharmacognosy Research. 2017;9(4):333–347. doi: 10.4103/pr.pr_42_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olpusimoru. Olpusimoru Forest; geoview.info. 2017, http://ke.geoview.info/olpusimoru_forest,181965.
- 14.Sekenani. Sekenani; geoview.info. 2017, http://ke.geoview.info/sekenani,1611716061n.
- 15.Stepp J. R. Advances in Ethnobiological Field Methods. Field Methods. 2016;17(3):211–218. doi: 10.1177/1525822X05277459. [DOI] [Google Scholar]
- 16.Alexiades M. N., Sheldon J. W. Selected Guidelines for Ethnobotanical Research: A Field Manual. Vol. 10. New York, NY, USA: New York Botanical Garden Bronx; 1996. (Advances in Economic Botany). [Google Scholar]
- 17.Martin G. Ethnobotany—A Manual of Methods. London, UK: Earthsacn Publishers Limited; 2004. [DOI] [Google Scholar]
- 18.Beentje H., Adamson J., Bhanderi D. National Museums of Kenya. 1994. Kenya trees, shrubs, and lianas. [Google Scholar]
- 19.Agnew A. D. Q. Upland Kenya Wild Flowers and Fern. 3rd. Nairobi, Kenya: Nature Kenya--The East Africa Natural History Society; 2013. [Google Scholar]
- 20.Albuquerque U. P., Lucena R. F., Monteiro J. M., Florentino A. T., et al. Evaluating two quantitative ethnobotanical techniques. Ethnobotany Research and Applications. 2006;4:51–60. [Google Scholar]
- 21.Tardío J., Pardo-De-Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain) Economic Botany. 2008;62(1):24–39. doi: 10.1007/s12231-007-9004-5. [DOI] [Google Scholar]
- 22.Bussmann R. W., Gilbreath G. G., Solio J., et al. Plant use of the Maasai of Sekenani Valley, Maasai Mara, Kenya. Journal of Ethnobiology and Ethnomedicine. 2006;2, article 22 doi: 10.1186/1746-4269-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiringe J. W. A survey of traditional health remedies used by the maasai of southern kaijiado district, Kenya. Ethnobotany Research and Applications. 2006:61–74. [Google Scholar]
- 24.Parker M. E., Chabot S., Ward B. J., Johns T. Traditional dietary additives of the Maasai are antiviral against the measles virus. Journal of Ethnopharmacology. 2007;114(2):146–152. doi: 10.1016/j.jep.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Maima A. O., Ndwigah S. N., Thoithi G. N., et al. Antimicrobial properties of some medicinal plants of the luo community of kenya. African Journal of Pharmacology and Therapeutics. 2014;3 [Google Scholar]
- 26.Teka A., Rondevaldova J., Asfaw Z., et al. In vitro antimicrobial activity of plants used in traditional medicine in Gurage and Silti Zones, south central Ethiopia. BMC Complementary and Alternative Medicine. 2015;15, article 286 doi: 10.1186/s12906-015-0822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taye B., Giday M., Animut A., Seid J. Antibacterial activities of selected medicinal plants in traditional treatment of human wounds in Ethiopia. Asian Pacific Journal of Tropical Biomedicine. 2011;1(5):370–375. doi: 10.1016/S2221-1691(11)60082-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mufti F. U., Ullah H., Bangash A., et al. Antimicrobial activities of Aerva javanica and Paeonia emodi plants. Pakistan Journal of Pharmaceutical Sciences. 2012:565–569. [PubMed] [Google Scholar]
- 29.Malpani A. A. Effect of the aqueous extract of Gloriosa superba Linn (Langli) roots on reproductive system and cardiovascular parameters in female rats. Tropical Journal of Pharmaceutical Research. 2011;10 [Google Scholar]
- 30.Kigen G., Some F., Kibosia J., et al. Ethnomedicinal plants traditionally used by the keiyo community in Elgeyo Marakwet County, Kenya. Journal of Biodiversity, Bioprospecting and Development. 2014;1:132–143. [Google Scholar]
- 31.Kigen G., Maritim A., Some F., et al. Ethnopharmacological survey of the medicinal plants used in Tindiret, Nandi County, Kenya. African Journal of Traditional, Complementary and Alternative Medicines. 2016;13:156–168. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details of the medicinal plant uses.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and/or its supplementary materials.