Key Clinical Message
Panniculitis is rarely seen in polymyositis. To the best of our knowledge, we report the first case of panniculitis which precedes the antisynthetase syndrome.
Keywords: antisynthetase syndrome, autoimmune disease, Panniculitis, polymyositis
1. INTRODUCTION
Panniculitis can occur in many conditions such as trauma, infection, neoplasm, enzymatic insufficiency, and connective tissue disease.1 Among connective tissue diseases, panniculitis is mostly associated with lupus erythematosus over the others2 and quite rare in dermatomyositis.3, 4 Panniculitis is even scarcer in polymyositis, with only two cases reported in PubMed Database.5, 6 To the best of our knowledge, panniculitis in antisynthetase syndrome has never been reported. Herein, we report the first case of a Thai male who presented with panniculitis and further investigation revealed he had polymyositis with antisynthetase syndrome.
2. OUR CASE
A 68‐year‐old Thai man with 1 year of ankylosing spondylitis suddenly developed tender erythematous skin eruptions on both thighs for two weeks (Figure 1A). His medication was prednisolone 10 mg per day, azathioprine 75 mg per day, and methotrexate 7.5 mg per week. He was initially diagnosed and treated as cellulitis with antibiotics. Hence, immunosuppressive agents except prednisolone were stop. Unfortunately, his lesions were not improved, so the skin biopsy was done. The result showed lobular panniculitis with sparse lymphocytic and histiocytic infiltrations with foci of lipomembranous changes (Figure 2). The tissue cultures for bacteria, fungus, and mycobacterium were all negative. Laboratory investigations showed strongly positive for Anti‐Jo1 and Anti‐R052 but negative for ANA, anti‐dsDNA, antiphospholipid antibodies, and Anti‐Scl70. He had neither cutaneous signs of lupus erythematosus nor dermatomyositis. His panniculitis was improved (Figure 1B) upon increasing the dosage of prednisolone to 30 mg per day. Two months later, he developed proximal muscle weakness with high serum creatine phosphokinase. The muscle biopsy was compatible with inflammatory myopathy. The screening investigations for malignancy showed all negative results. Only the CT chest revealed interstitial lung disease. Finally, he was diagnosed with polymyositis with antisynthetase syndrome.
Figure 1.
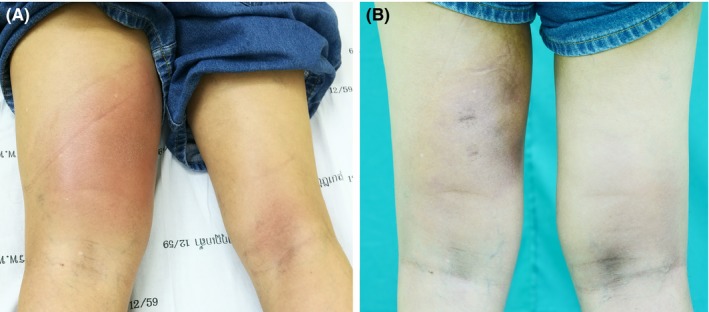
A, Tender ill‐defined erythematous indurated subcutaneous plaques on posterior left thigh and right popliteal fossa; B, After treatment, the lesions improved and became hyperpigmented 1859 × 821 mm (72 × 72 DPI)
Figure 2.
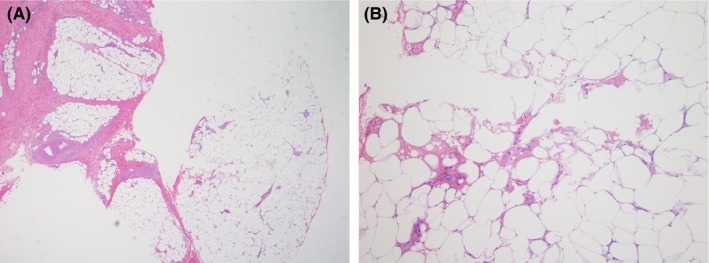
The histopathology from left thigh showed (A) lobular panniculitis with sparse cells infiltration (Hematoxylin‐eosin staining, ×4) (B) lymphocytic and histiocytic infiltrations with some foci of lipomembranous change (Hematoxylin‐eosin staining, ×40) 541 × 203 mm (150 × 150 DPI)
3. DISCUSSION
Antisynthetase syndrome is an autoimmune disease which is a separate entity from dermatomyositis or polymyositis. It is characterized by antibodies directed against an aminoacyl transfer RNA synthetase with clinical features of interstitial lung disease, myositis, Raynaud's phenomenon, and arthritis7 according to the diagnostic criteria proposed by Connors et al8 and Solomon et al.9 To our knowledge, there is no report of any patient with polymysitis and antisynthetase syndrome presenting with panniculitis.
Regarding the differential diagnosis of panniculitis, especially in immunocompromised host, the infectious etiologies should be ruled out first. In our case, all cultures were negative and histopathology excluded infections, instead suggesting connective tissue diseases that is lupus panniculitis and dermatomyositis. However, due to the similarities of clinical presentation and histopathology of both diseases, associated features and further investigations were required (Table 1). There were no specific rashes in this patient. However, the presence of myopathy, arthralgia, and interstitial lung disease favored the diagnosis of polymyositis and antisynthetase syndrome.
Table 1.
Comparative features between lupus panniculitis and dermatomyositis panniculitis
| Lupus panniculitis | Dermatomyositis/Polymyositis | |
|---|---|---|
| Presentation | Tender subcutaneous nodules and plaques; may have ulceration and lipoatrophy.14 | Painful, erythematous, indurated, nodules and plaques; may have ulceration and lipoatrophy.15 |
| Distribution | Face (esp. cheeks), upper arms, scalp, shoulders, hips, buttocks, breasts, trunk | Lower and upper extremities, usually spare face.16 |
| Associated features | Discoid rash or other lupus specific rashes | Typical cutaneous findings including heliotrope rash, Gottron's papules in dermatomyositis |
| Systemic features of lupus, such as arthralgia or Raynaud phenomenon.14, 17 | Symmetrical proximal muscle weakness.16 | |
| Investigations | ANA, anti‐dsDNA, anti‐RNP, leukopenia, hypocomplementemia and elevate ESR.14, 17 | Elevate serum CPK, Anti‐Jo1 |
| Electromyography (EMG) and muscle biopsy show evidence of myositis.6 | ||
| Histopathology | Lobular or mixed panniculitis composed of lymphocytes and plasma cells | Lobular or mixed pannicuitis composed of lymphocytes and plasma cells |
| Fat necrosis | ||
| Mucin deposition | Lipomembranous changes | |
| Lipomembranous change | Some lymphoid aggregations | |
| Nuclear dust and lymphoid aggregations in some cases.14 | May have calcification.16 |
Panniculitis in dermatomyositis and polymyositis is a rare finding and may precede, coexist, or appear after the onset of disease.4, 10 There were only two case‐reports of panniculitis in polymyositis. In the first case,6 a 58‐year‐old woman presented with panniculitis on her thigh, abdomen, and buttocks that preceded the development of polymyositis. The histopathological features showed lobular panniculus infiltrations with lymphocytes and plasma cells. This case was similar to our patient, which responded well to high dose prednisolone and had no evidence of malignancy. The second report5 was a 35‐year‐old woman who developed cutaneous ulcer and multiple panniculitic nodules on her abdomen and breasts after the onset of polymyositis. This case developed panniculitis while she was treated with immunosuppressive agents as in our patient.
At present, the treatment guideline of panniculitis in dermatomyositis and polymyositis has not been established yet. Most of the cases are treated with prednisolone with variable outcome. Other treatments are intravenous methyl prednisolone, azathioprine, methotrexate, intravenous immunoglobulin, hydroxychloroquine, or cyclosporine.3, 10, 11 It has been suggested that panniculitis may be a positive prognostic sign with a good response to treatment and rare underlying neoplasm.2, 4, 12, 13
In conclusion, we report the first case of polymyositis with antisynthetase syndrome, which has panniculitis preceding the onset of proximal muscle weakness. Although panniculitis is a very rare clinical finding in polymyositis and antisynthetase syndrome, this condition should be included in the differential diagnosis of patients presenting with idiopathic panniculitis.10
AUTHOR CONTRIBUTION
AR: conceived and designed the report, collected the data, analyzed the data, wrote and reviewed the manuscript. NS: conceived and designed the report, analyzed the data, wrote, reviewed the manuscript and approved the final draft. Both authors were involved in patient care.
Rungcharunthanakul A, Sampattavanich N. Polymyositis with antisynthetase syndrome presented with lobular panniculitis: A case report. Clin Case Rep. 2019;7:128–130. 10.1002/ccr3.1839
REFERENCES
- 1. Braunstein I, Werth VP. 2012. Update on management of connective tissue panniculitides. Dermatol Ther. 25(2):173‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carneiro S, Alvim G, Resende P, Auxiliadora Jeunon Sousa M, Cuzzi T, Ramos‐e‐Silva M. 2007. Dermatomyositis with panniculitis. Skinmed. 6(1):46‐47. [DOI] [PubMed] [Google Scholar]
- 3. Carroll M, Mellick N, Wagner G. 2015. Dermatomyositis panniculitis: a case report. Australas J Dermatol. 56(3):224‐226. [DOI] [PubMed] [Google Scholar]
- 4. Azevedo PO, Castellen NR, Salai AF, Barbosa FS, Alves C, Pinto C. 2018. Panniculitis associated with amyopathic dermatomyositis. An Bras Dermatol. 93(1):119‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mansur AT, Balaban D, Koc K, Goktay F, Aksu O, Gunes P. 2007. Polymyositis associated with vasculitic skin ulcers on flexural areas and panniculitis. Eur J Dermatol. 17(3):251‐252. [DOI] [PubMed] [Google Scholar]
- 6. Raimer SS, Solomon AR, Daniels JC. 1985. Polymyositis presenting with panniculitis. J Am Acad Dermatol. 13(2 Pt 2):366‐369. [DOI] [PubMed] [Google Scholar]
- 7. Witt LJ, Curran JJ, Strek ME. 2016. The diagnosis and treatment of antisynthetase syndrome. Clin Pulm Med. 23(5):218‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Connors GR, Christopher‐Stine L, Oddis CV, Danoff SK. 2010. Interstitial lung disease associated with the idiopathic inflammatory myopathies: what progress has been made in the past 35 years?. Chest. 138(6):1464‐1474. [DOI] [PubMed] [Google Scholar]
- 9. Solomon J, Swigris JJ, Brown KK. 2011. Myositis‐related interstitial lung disease and antisynthetase syndrome. J Bras Pneumol. 37(1):100‐109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Solans R, Cortes J, Selva A, et al. 2002. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 46(5 Suppl):S148‐S150. [DOI] [PubMed] [Google Scholar]
- 11. Sabroe RA, Wallington TB, Kennedy CT. 1995. Dermatomyositis treated with high‐dose intravenous immunoglobulins and associated with panniculitis. Clin Exp Dermatol. 20(2):164‐167. [DOI] [PubMed] [Google Scholar]
- 12. Molnar K, Kemeny L, Korom I, Dobozy A. 1998. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 139(1):161‐163. [DOI] [PubMed] [Google Scholar]
- 13. Chairatchaneeboon M, Kulthanan K, Manapajon A. 2015. Calcific panniculitis and nasopharyngeal cancer‐associated adult‐onset dermatomyositis: a case report and literature review. SpringerPlus. 4:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Winkelmann RK. 1983. Panniculitis in connective tissue disease. Arch Dermatol. 119(4):336‐344. [PubMed] [Google Scholar]
- 15. Lee MW, Lim YS, Choi JH, Sung KJ, Moon KC, Koh JK. 1999. Panniculitis showing membranocystic changes in the dermatomyositis. J Dermatol. 26(9):608‐610. [DOI] [PubMed] [Google Scholar]
- 16. Santos‐Briz A, Calle A, Linos K, et al. 2018. Dermatomyositis panniculitis: a clinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 32(8):1352‐1359. [DOI] [PubMed] [Google Scholar]
- 17. Peters MS, Su WP. 1989. Lupus erythematosus panniculitis. Med Clin North Am. 73(5):1113‐1126. [DOI] [PubMed] [Google Scholar]


