Key Clinical Message
Respiratory rate is often measured manually and discontinuously by counting of chest wall movements in routine clinical practice. We introduce a novel approach to investigate respiration dynamics using a noncontact medical radar system for identifying patient at risk of infection. The system enables early detection of pneumonia in bedridden hospitalized patients.
Keywords: long‐term monitoring, medical radar, pneumonia, respiratory rate
1. INTRODUCTION
The use of continuous and long‐term monitoring of respiratory rate is vital for predicting pneumonia in symptomatic patients; however, it is often measured manually and discontinuously by counting of chest wall movements in routine practice.1 Hence, here we developed a point‐of‐care system for the early detection of pneumonia in symptomatic elderly bedridden hospitalized patients on the basis of 24‐hours continuous and noncontact monitoring of respiratory rate using a medical radar sensor.
We focused on designing a system that would improve hospitalized patient quality of life and reduce medical staff workload. To this end, we adopted a medical radar sensor for respiration monitoring that featured an extremely low burden on the patient and enabled unobtrusive measurements without the need to attach electrodes to the patient's body.2 To reduce medical staff workload, a prediction method, that is, return map,3 was implemented into the system to analyze the time series respiratory rates, thereby extracting the risk period of pneumonia and sending out an alarm. Infection is the most common cause of hospital‐acquired pneumonia, which is associated with prolonged hospital stay and increased mortality in elderly hospitalized patients.4 In this study, we evaluated the feasibility of this system for detecting the risk period of pneumonia on the basis of continuously monitored respiratory rates in elderly bedridden hospitalized patients.
2. MEDIAL RADAR SYSTEM AND PATIENT PRESENTATION
2.1. Remote monitoring of respiratory rate using a medical radar system
A diagram of the medical radar system is shown in Figure 1. The medical radar sensor remotely captures small chest wall displacements on the surface of the body caused by respirations. In brief, the transmitter of the medical radar sends a continuous electromagnetic wave (24 GHz) toward the chest and the wave is reflected and received by the receiver. The phase of the reflected wave is modulated by periodic movements on the surface of the body caused by respiration. Radar sensors have attracted much attention and are widely used in medical devices, such as sleep monitoring systems and infection screening systems.5, 6 In this study, we designed a compact radar system that can be attached under a standard hospital bed mattress to monitor a bedridden hospitalized patient's respiratory rate. The system provides respiratory rate measurements every minute throughout the day for a total of 1440 data points daily.
Figure 1.
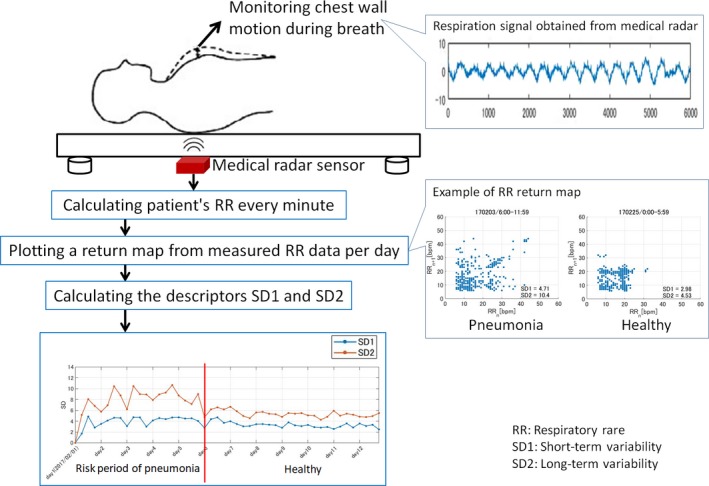
Diagram of the compact medical radar system that can be attached under the mattress of a standard hospital bed to monitor a bedridden hospitalized patient's respiratory rate
Moreover, the system included a nonlinear dynamics model, called a return map (also known as Poincaré plot), to predict the development of pneumonia using the measured time series respiratory rate equation: RR = (rr1, rr2, rr3, …, rrn, rrn+1). The time series respiratory rates were reconstructed with time‐delay embedding with simple plotting of each time respiratory rate y = (x 2, x 3, x 4, …, x n+1) against the respiratory rates taken earlier x = (x 1, x 2, x 3, …, x n). To extract the risk and severity period, an adaptive threshold was applied to the return map‐derived indices, that is, short‐term variability (SD1) and long‐term variability (SD2). SD1 indicates fast changes in respiratory rates, whereas SD2 corresponds to slow changes in long‐term measurements. SD1 and SD2 are defined as follows:
2.2. Clinical testing on two elderly bedridden hospitalized patients
A 79‐year‐old woman (patient A) was admitted to a long‐term care hospital for Alzheimer's dementia on October 24, 2016. On November 22, the patient suddenly became feverish (38.5°C), and chest radiography showed infiltrations at the right middle and lower lung, and she was diagnosed with pneumonia. A sputum culture grew Klebsiella pneumoniae.
A 92‐year‐old woman (patient B) was taken to a long‐term care hospital on January 19, 2017, for aftereffects of cerebral infarction and diabetes mellitus. On February 4, the patient complained of cough and sputum; 2 days later, she had a fever of 38.7°C. Chest radiography showed a new frosty glass shadow in the left lower lung, and she was diagnosed with pneumonia. A sputum culture grew Pseudomonas aeruginosa.
A comparison of SD1 and SD2 before confirming pneumonia and 1 week after starting treatment was conducted by Student's t test. The SD1 and SD2 values were significantly higher in the risk of pneumonia period than in the 1 week after starting treatment in both patients (patient A: SD1, 2.6 ± 0.6 vs 2.3 ± 0.5, P < 0.05, SD2, 3.9 ± 1.3 vs 3.2 ± 0.7, P < 0.05; patient B: SD1, 4.1 ± 0.9 vs 3.3 ± 0.5, P < 0.05, SD2, 8.2 ± 1.6 vs 5.3 ± 0.6, P < 0.05).
The patients were informed about the study procedure and provided written informed consent.
3. DISCUSSION
We intensively analyzed respiration datasets of patient A and patient B from the 2‐week measurement period, which includes the risk period of pneumonia confirmed by chest radiography. We focused on assessing the fluctuation of respiratory rate, SD1, and SD2 1 week before confirming pneumonia and 1 week after starting treatment. Figure 2 shows the trends of respiratory rate, SD1, SD2, body temperature, and pulse rate for both patients. The values of SD1 and SD2 were higher in the risk of pneumonia period and decreased after 1 week of treatment. Figure 2 shows a significant difference in SD1 and SD2 between the two periods (P < 0.05).
Figure 2.
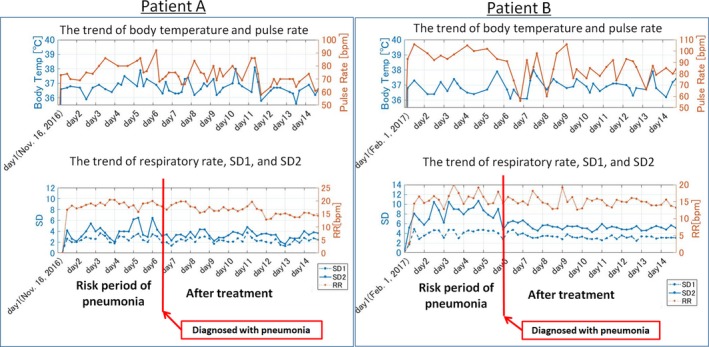
The trends of respiratory rate, SD1, SD2, body temperature, and pulse rate for patient A and patient B. SD, short‐term variability
Our results confirmed that continuous monitoring of respiratory rate enables the early detection of pneumonia and its severity. The extracted respiration features are based on the return map, which provides important information for detecting clinical deterioration in bedridden patients with pneumonia. It is important to note that the idea behind our medical radar system to detect pneumonia is to screen for symptoms of pneumonia, not to provide a medical diagnosis. The concept of using continuous and contactless monitored respiratory rates for predicting the development of non‐specific infectious disease stems from the fact that most infectious diseases are associated with inflammation when patients become symptomatic. For example, urinary tract infection (UTI) is common disease in bedridden hospitalized elderly patients; we will further investigate our system in UTI patients in a future study. In most hospitals, nurses routinely measure pulse rate and body temperature 2 or 3 times per day. In this sense, the dynamics of respiration features are more significant than changes in body temperature and pulse rate.
In conclusion, the novelty of the proposed system is that introduces a new approach to investigating respiration dynamics using a noncontact medical radar sensor for the early prediction of pneumonia that has the potential to serve as a helpful tool for improving patient quality of life and reduce medical staff workload to meet the needs of the aging society.
ETHICAL APPROVAL
This study was approved by the Ethics Committee of the Yokohama Hospital and The University of Electro‐Communications.
CONFLICT OF INTEREST
The authors declare no conflict of interests.
AUTHOR CONTRIBUTIONS
GS, MO, TK, YH, and TM: involved in study concept and design. YH: involved in acquisition of data. GS, MO, RN, TM, TK, YH, and TM: analyzed and interpreted the data. GS, YH, and TM: drafted the manuscript. All authors provided final approval of the version to be submitted.
Sun G, Okada M, Nakamura R, et al. Twenty‐four‐hour continuous and remote monitoring of respiratory rate using a medical radar system for the early detection of pneumonia in symptomatic elderly bedridden hospitalized patients. Clin Case Rep. 2019;7:83–86. 10.1002/ccr3.1922
REFERENCES
- 1. Strauß R, Ewig S, Richter K, König T, Heller G, Bauer T. The prognostic significance of respiratory rate in patients with pneumonia: a retrospective analysis of data from 705 928 hospitalized patients in Germany from 2010–2012. Dtsch Arztebl Int. 2014;111(29–30):503‐508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Loon K, Breteler M, Wolfwinkel L, et al. Wireless non‐invasive continuous respiratory monitoring with FMCW radar: a clinical validation study. J Clin Monit Comput. 2016;30(6):797‐805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moridani KM, Setarehdan SK, Motie NA, Hajinasrollah E. Non‐linear feature extraction from HRV signal for mortality prediction of ICU cardiovascular patient. J Med Eng Technol. 2016;40(3):87‐98. [DOI] [PubMed] [Google Scholar]
- 4. Leroy O, Meybeck A, d'Escrivan T, et al. Hospital‐acquired pneumonia in critically ill patients: mortality risk stratification upon onset. Treat Respir Med. 2004;3(2):123‐131. [DOI] [PubMed] [Google Scholar]
- 5. Sun G, Matsui T, Hakozaki Y, Abe S. An infectious disease/fever screening radar system which stratifies higher‐risk patients within ten seconds using a neural network and the fuzzy grouping method. J Infect. 2015;70(3):230‐236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Matsui T, Yoshida Y, Kagawa M, Kubota M, Kurita A. Development of a practicable non‐contact bedside autonomic activation monitoring system using microwave radars and its clinical application in elderly people. J Clin Monit Comput. 2013;27(3):351‐356. [DOI] [PubMed] [Google Scholar]


