Abstract
Objective
The determinates of economic burden in lung cancer caregivers are poorly understood. Of particular interest is the role patient symptoms play in caregiver economic burden. Guided by a stress process conceptual framework, this study examined the predictors of economic burden reported by lung cancer spousal caregivers. Our study focused on the pathway of contextual and stressor variables leading to economic burden in lung cancer caregivers.
Method
Relying on survey data from 138 spouses, structural equation modeling was employed to examine the determinants of economic burden measured using the Family Impact Survey. Contextual variables included age, gender, education, and income; and stressor variables included patient physical and mental symptoms, as well as number of children in the home.
Results
A significant indirect path between age and economic distress through patient symptoms (p = 0.05) indicates younger spouses providing care for patients with more symptoms and reporting greater economic burden. Direct effects between contextual variables and economic burden revealed that caregivers with less education (p = 0.02) and those with more children at home (p = 0.01) reported more adverse economic outcomes.
Significance of Results
Numerous factors impact spousal caregivers’ economic burden, including the presence of children at home, being a younger caregiver, and lower educational attainment by caregivers. Moreover, the direct effects between age and economic burden were not significant, supporting the clear role patient symptoms play in the path to economic burden in spousal caregivers. These results underscore the need for healthcare providers to address psychosocial factors when dealing with patients and families with lung cancer. Specifically, the results highlight the importance of addressing patient symptoms early before they threaten the family’s economic well-being.
Keywords: Lung cancer, Spousal caregiver, Economic burden, Palliative care, Caregiver burden
INTRODUCTION
Lung cancer is the leading cause of cancer mortality in the United States, with over 221,130 new cases and 156,940 deaths in 2011 (American Cancer Society, 2011). Patients with lung cancer are typically diagnosed later and die earlier than patients with many other forms of cancer, putting survivors at risk for psychological and emotional distress (Braun et al., 2007; Pearman, 2008). Spouses in particular predominate in the caregiving role and experience the numerous burdens associated with care (Savage & Bailey, 2004).
A substantial body of literature documents the physical, emotional, personal, and financial costs of caring for elders with advanced chronic diseases; however, little attention has been paid to understanding the economic burden incurred by spouses of patients with lung cancer and the contextual and stressor variables that may influence such burden (Savage & Bailey, 2004; Schulz & Martire, 2004). Evidence suggests that serious life-threatening illness can have a substantial impact on family finances, and the cost-prohibitive treatment options associated with lung cancer pose potentially serious economic burdens for families (Kutikova et al., 2005; Pearman, 2008). Understanding the factors that contribute to economic burden is vital in identifying families at risk and for planning services and supportive interventions. Our study seeks to examine the predictors of economic burden of the spouses of persons recently deceased from lung cancer. Based on the “stress process model” (Pearlin et al., 1990), our study examines three domains: background and contextual factors; stressors, including the number of physical and psychological symptoms of the patient; and the latent outcome variable of economic distress. Figure 1 schematizes the components of the model investigated herein.
Fig. 1.
Conceptual model. This figure represents the conceptual framework, including three domains adapted from the stress process model of Pearlin et al. (1990).
Background and Context
Gender, caregiver age, income, and education influence the stressors individuals are exposed to and the outcomes they experience (Pearlin et al., 1990). Women represent a larger percentage of the caregiving population than males (Bakas et al., 2001; Gridelli et al., 2007). Numerous studies report that younger caregivers have more disruption in their schedule as a result of their caregiving duties, as opposed to older caregivers (Nijboer et al., 2000). Caregiving responsibilities negatively impact work performance and attendance, particularly for a younger spousal caregiver still employed outside the home (Sherwood et al., 2008). Limited attention has been given to understanding the relationship between socioeconomic status and economic burden. Two studies found that families with lower incomes report a greater economic burden associated with caring for persons with a serious illness (Covinsky et al., 1994; Yun et al., 2005). Finally, lower educational attainment has been found to negatively impact the mental health of the caregiver (Buckwalter et al., 1999), yet our understanding of the role educational attainment plays in the economic impact of caregiving is limited.
Primary Stressors
The primary stressors are the difficult circumstances experienced by family caregivers that stem from the patient’s care needs and typically include the illness-related symptoms that the caregiver helps to address (Pearlin et al., 1990).
Patient Symptoms
Patients with lung cancer experience a high prevalence of uncontrolled physical symptoms that commonly include pain, shortness of breath, nausea or vomiting, fatigue, and cough (Bakas et al., 2001; Griffin et al., 2007; Sarna, 1993), as well as the psychological symptoms of anxiety and depression. Substantial evidence supports a relationship between patient needs and symptoms and family caregiver secondary stressors and burden or psychological well-being (Gaugler et al., 2008; Grunfeld et al., 2004; Sherwood et al., 2006), yet little attention has been paid to the impact of symptoms on economic burden. One study of breast cancer caregivers found a decline in patient functioning to be associated with increased financial burden (Grunfeld et al., 2004). Pain symptoms and intensity of symptoms in cancer patients have been associated with higher medical expenses (Fortner et al., 2003), which would likely affect surviving spouses who shared the cost of care (Emanuel et al., 2000).
Number of Children in the Home
Family caregivers who care for a loved one while still taking care of a child at home have shown higher levels of depression and anxiety (Cannuscio et al., 2004; Ferrara et al., 2008). The financial demands associated with meeting the needs of children may compete with the financial demands of caring for an ill spouse. Additionally, splitting time between caregiving duties and taking care of children has been shown to negatively impact work performance and attendance, which may have a lasting economic impact (Sherwood et al., 2008). These impacts may be stronger in younger caregivers, as they are more likely than older caregivers to have young children at home.
Outcome
Outcomes refer to the varied effects and consequences of the caregiving stress process (Pearlin et al., 1990).
Economic Burden
Patients with lung cancer have higher healthcare costs and utilization than those with other forms of cancer (Kutikova et al., 2005). The few treatments available are often cost prohibitive (Pearman, 2008), and financial stress is of great concern for patients and their families (Hanratty et al., 2007). Although participating in clinical trials can improve survival and result in minimal cost to patient and caregiver (Du et al., 2003), there are few clinical trials for lung cancer patients and their family caregivers (Khullar & Colson, 2009). Providing care to a family member with lung cancer is expensive (Hayman et al., 2001). In 2010, the estimated cost of lung cancer care in the United States was more than 12 billion dollars (National Cancer Institute, 2010). Studies have noted that the cost of caregiving is particularly high for cancer patients who experience numerous and complicated symptoms, such as breathing difficulty, uncontrolled pain, nausea, and cough (Bakas et al., 2001). These symptoms may lead to a need for multiple medications, which have been found to be highly predictive of financial burden for breast cancer caregivers (Grunfeld et al., 2004).
Research addressing the economic impact of all cancers describes loss of employment, assets, and livelihood for both patient and caregiver (Brown et al., 2001). Family cancer caregivers report caregiving impacting their employment, including missing work due to caregiving duties, and most acutely at the end stage of the illness (Grunfeld et al., 2004). One multisite study of chronically ill individuals found that family caregivers were financially strained, forwent educational and employment opportunities, and had to delay their own medical needs as a result of the illness of the loved one (Covinsky et al., 1994). The majority of studies that have investigated financial strain associated with cancer or the financial impacts of caregiving (Covinsky et al., 1994; Hanratty et al., 2007; Yun et al., 2005) have focused on examination of the direct effects that lead to poor economic outcomes for the spousal caregiver. The use of a more detailed theoretically based analytical approach, structural equation modeling, as presented here, will allow for a more thorough understanding of both the direct and indirect effects that lead to financial burden in lung cancer caregivers.
Research Questions
Our study proposes several paths leading to economic burden in lung cancer spousal caregivers. Using structural equation modeling, we tested whether younger age of caregivers, lower income, and less education would be associated with greater caregiver economic burden. Additionally, we wanted to know if higher-order stressors (i.e., patient symptoms and number of children at home) were associated with greater economic burden. Finally, we tested whether higher-order stressors (i.e., patient symptoms and number of children at home) served as indirect pathways leading to higher economic burden in younger caregivers.
METHODS
Participant Identification and Recruitment
The results reported here are drawn from an ancillary mail survey of family members of patients who died with lung cancer drawn from the larger Assessment of Cancer Care and Satisfaction Study (ACCESS) conducted within the state of Wisconsin. The sampling and survey methods from ACCESS and the ancillary lung cancer family study have been previously described (Kramer et al., 2010; Trentham-Dietz & Walsh, 2008). In brief, of 358 primary family caregivers of persons who died with lung cancer who were identified in a statewide registry and who had contact information available, 205 (57%) agreed to receive the study questionnaire, and 169 returned surveys (82% of those who received the survey; 47% of the total contacted). The sample was limited to spouses (N = 138), as the majority of caregivers are spouses. Including the other small sample (N = 31) of caregivers (including siblings, parents, and other relatives) would represent a different caregiving process (Neal et al., 1997). The time between death and completion of the surveys averaged 19 months (SD = 7.37) and ranged from 9 to 34 months. Additionally, only three of the spouses reported not having insurance prior to diagnosis.
Measures
Dependent Variable: Economic Burden
The economic burden measure was created from several variables of interest addressing financial and economic burden to caregivers drawn from the Family Impact Survey (Covinsky et al., 1994). Caregivers were asked dichotomous questions (1 = yes, 0 = no) including:
“Did your family member’s illness result in the use of all or most of the family’s savings?”
“Did your family member’s illness result in the loss of a major source of income for your family?”
“Did the cost of care for your family member’s illness require putting off important medical care for anyone else in the family?”
“Did the cost of care for your family member require putting off plans for education or otherwise greatly change plans for anyone else in the family?”
“Did the cost of care for your family member’s illness make you go into debt?”
These variables were all initially included in the factoring model in order to create the latent variable economic burden.
Covariates
Age was measured as a continuous variable (0–99), while education (1 = grade 8 or less, 2 = grade 9– 11, 3 = grade 12, 4 = 1–3 years college, 5 = college degree,6 = advanced degree), income prior to patient diagnosis (1 = $0–14,999, 2 = $15,000–29,999, 3 = $30,000–49,999, 4 = $50,000–99,999 and 5 = more than), and gender (1 = female, 0 = male) were defined in categories.
Primary Stressors
An index of six common physical and psychological symptoms associated with lung cancer was assessed by asking the spouse (1 = yes, 0 = no) “Did your family member have during or after cancer treatment: (a) pain; (b) shortness of breath; (c) nausea or vomiting; (d) severe tiredness or fatigue; (e) loss of hope or depression; and/or (f) anxiety during or after any of his/her cancer treatments?” Children living in the home aged 17 or younger prior to patient diagnosis was a continuous variable.
Statistical Analysis
First, descriptive statistics were calculated using bivariate correlations among the contextual, stressor, and economic burden variables. Table 1 presents the results of these correlations.
Table 1.
Pearson Correlation of Major Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Caregiver Age | 1 | |||||||||
| 2 | Caregiver Education | .09 | .08 | ||||||||
| 3 | Family Income | −.26b | .21c | −.02 | |||||||
| 4 | Number Child in Home | −.28a | .08 | .01 | .12 | ||||||
| 5 | Patient Symptoms | −.39a | .10 | .32a | .19c | .09 | |||||
| 6 | Illness Resulted in Use of Savings | −.23b | −.19c | −.00 | .15 | .27a | .04 | ||||
| 7 | Illness Resulted in Loss of Income | −.32a | −.08 | .04 | .18d | .30a | .35a | .25b | |||
| 8 | Cost of Care Put off Medical Care | −.11 | −.01 | −.03 | .20c | .14d | .37a | .11 | .04 | ||
| 9 | Cost of Care Put off Education | −.19c | −.02 | .11 | .20c | .27b | .47a | .19c | .25b | .11 | |
| 10 | Duration Since Death | −.12 | .09 | −.09 | −.15 | .04 | .03 | .06 | .03 | .04 | 1 |
NOTE
p < .001
p < .01
p < .05
p < .10
Second, structural equation modeling (SEM) was employed to test the study’s hypotheses. Comprised of both factor and path analysis, SEM seeks to address hypotheses based on measurement and structured parameters within the proposed model (Pedhazur & Schmelkin, 1991). The software program MPLUS 5.2 (Muthen & Muthen, 2001) was utilized to estimate the parameters for the measurement model. The measurement model serves to define the latent construct from factored measures (Kaplan, 2009). Additionally, MPLUS was used to define the structural path model, describing the pathways within the proposed model. Model estimation is assessed using the significance of path coefficients and numerous goodness-of-fit statistics: chi square, RMSEA (root mean square of approximation) (Steiger & Lind, 1980), and CFI (comparative fit index) (Bentler, 1990). Models that are a better fit will have a nonsignificant chi square (p > 0.05), higher CFI (>0.9), and lower RMSEA (<0.8).
RESULTS
Sample Characteristics
Table 2 presents the demographic characteristics of the caregiving sample. Caregivers were predominantly female (n = 112, 81%), and the vast majority (93%, n = 128) had at minimum a high school education. The age of caregivers ranged from 43 to 85 (mean = 65, SD = 9 years), and 82% had annual incomes prior to diagnosis over $30,000. Table 1 presents the Pearson correlation coefficients between the contextual, stressor, and economic burden variables. Specifically, younger caregiver agewas correlated with several variables in the expected direction, describing more children present in the home, more patient symptoms, and higher economic burden, including loss of income and use of savings (r = –0.32 and –0.23, respectively). Of note, the variable “time since patient death” was not significantly correlated with any study variables. While not included in our model, this lack of correlation suggests that contextual variables play a larger role in economic burden than length of time since patient death. These correlations provide the basis for the following SEM model.
Table 2.
Descriptive Characteristics of Lung Cancer Caregivers
| N (%) | Mean | St D | |
|---|---|---|---|
| Caregiver Age | 65 | 9 | |
| 43–65 | 64 | ||
| 65 and up | 74 | ||
| Family Income | 2.87 | .971 | |
| Less than 15,000 | 12 (8.8) | ||
| 15,000 to 29,999 | 14 (11) | ||
| 30,000 to 49,999 | 63 (45) | ||
| 50,000 to 99,999 | 44 (32) | ||
| 100,000 and above | 5 (4) | ||
| Caregiver Gender | |||
| Female | 112 (81) | ||
| Male | 26 (19) | ||
| Caregiver Education | 5.43 | .869 | |
| Grade 1–11 | 10 (7) | ||
| Grade 12 | 80 (58) | ||
| 1–3 yrs college | 33 (24) | ||
| College degree | 11 (8) | ||
| Advanced degree | 4 (3) | ||
| Total Patient Symptoms | 2.95 | 1.986 | |
| 0 | 17 (12) | ||
| 1 | 20 (14.5) | ||
| 2 | 23 (16.5) | ||
| 3 | 22 (16) | ||
| 4 | 19 (14) | ||
| 5 | 23 (17) | ||
| 6 | 14 (10) | ||
| Number of Children in the Home | .14 | .629 | |
| 0 | 129 (93) | ||
| 1 | 4 (3) | ||
| 2 | 2 (1.4) | ||
| 3 | 2 (1.4) | ||
| 4 | 1 (.7) | ||
| Loss of Savings | .20 | .399 | |
| No | 111 (79) | ||
| Yes | 27 (20) | ||
| Lost Source of Income | .41 | .494 | |
| No | 81 (59) | ||
| Yes | 57 (41) | ||
| CG Had to Put off Own Medical Care | .07 | .248 | |
| No | 129 (93) | ||
| Yes | 9 (7) | ||
| Someone in Home had to Put Off Education | .05 | .223 | |
| No | 130 (94) | ||
| Yes | 8 (6) |
Measurement Model
The first exploratory step in the factor analysis was employed to determine the factor loadings on the latent variable (i.e., economic burden) for each of the five directly observed economic burden items taken from the Family Impact Survey (Covinsky et al., 1994). This step provided factor loads for these items, resulting in refinement of the model through removal of one item—family member debt—which had a nonsignificant relationship to the other variables in the measurement model. The second confirmatory step in the measurement model was employed to determine measurement fit for the four remaining items. One factor structure representing the latent variable was derived from four items with the highest factor loadings (Table 3). This final measurement model showed excellent fit, with each economic burden item adequately describing the latent construct (Table 4). (test of model fit included χ2 = 2.431, p > 0.296; RMSEA = 0.04; CFI = 0.99).
Table 3.
Confirmatory factor analysis for measurement model of economic burden variables
| Domains | Factor Loading |
R2 |
|---|---|---|
| Illness result in loss of savings | 0.924 | 0.68a |
| Family member illness results in major source of income | 0.387 | 0.17c |
| Had to put off medical care for other family members | 0.433 | 0.23b |
| Had to put off education plans for other family member | 0.512 | 0.34b |
Note.
p < 0.001
p < 0.01
p < 0.05.
Table 4.
Goodness of fit indices for measurement and structural models
| Model | χ2 | df | RMSEA | CI for RMSEA | CFI |
|---|---|---|---|---|---|
| Measurement model | 2.43 | 2 | 0.04 | 0.00–0.18 | 0.99 |
| Model 1 | 43.69 | 27 | 0.07 | 0.03–0.10 | 0.88 |
| Model 2 | 28.54 | 19 | 0.06 | 0.00–0.10 | 0.93 |
Note: CFI = comparative fit index; CI = 95% confidence interval; Model 1 = initial model including gender; Model 2 direct path from education to economic distress freed, gender removed; RMSEA = root mean square error of approximation.
Structural Model
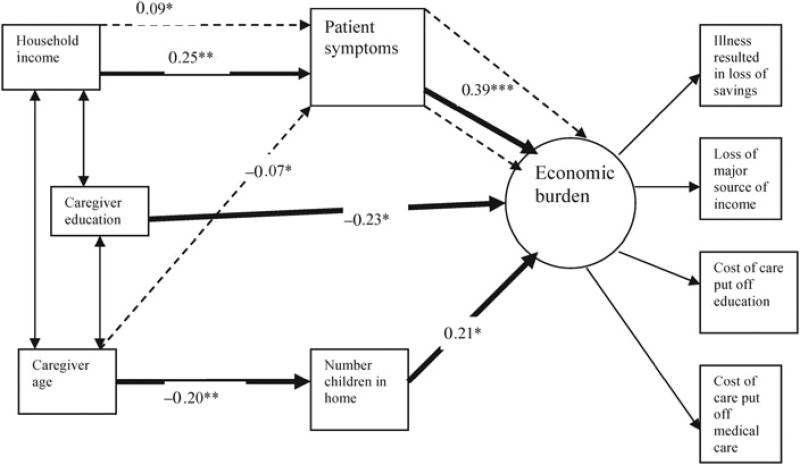
A structural model was specified that included the same contextual, stressor, and economic variables as in the measurement model, as well as the pathways between the variables. Through the use of modification indices, refinements were made to the initial structural model, specifically freeing the path from education to economic burden. While the use of modification indices is cautionary and should only be employed if it makes substantive sense (Kaplan, 2009), this path made conceptual sense given prior research showing a relationship between education level and caregiver burden (Buckwalter et al., 1999). All other paths were theoretically driven and remained in the final model, which had adequate fit (χ2 = 28.54, p > 0.05; CFI = 0.93; RMSEA = 0.06; see Figure 2 and Table 4). A detailed outline of the model effects are shown in Table 5.
Fig. 2.
Analytical model. Details the pathway of economic burden in lung cancer caregivers. Betas are shown above lines in the pathway. Dark lines = significant direct paths. Dotted lines = significant indirect paths. *p < 0.05, **p < 0.01, ***p < 0.001.
Table 5.
Final structural equation model estimates and standard errors
| Path | Estimate | SE |
|---|---|---|
| Direct effects | ||
| Economic burden on | ||
| Total symptoms | 0.39a | 3.93 |
| Income | 0.02 | 0.17 |
| Caregiver age | –0.05 | –0.52 |
| Child in home | 0.21c | 2.15 |
| Education | –0.23c | –2.28 |
| Total symptoms on | ||
| Age | –0.19c | –2.27 |
| Income | 0.25b | 2.93 |
| Education | 0.09 | 0.99 |
| Children in home | ||
| Age | –0.20b | –2.40 |
| Indirect effects | ||
| Economic distress on | ||
| Total symptoms Caregiver age | –0.07c | –1.96 |
| Child in home Caregiver age | –0.04 | –1.59 |
| Total symptoms Income | 0.09c | 2.31 |
| Total symptoms Education level | 0.03 | 0.96 |
Note.
p < 0.001
p < 0.01
p < 0.05.
Age and Economic Burden
Although Pearson bivariate correlations revealed significant relationships between younger age and higher economic burden as measured by three of the four economic burden items (see Table 1), in the final SEM analytic model, taking all other variables into consideration, there was no direct path between age and economic burden.
Socioeconomic Status and Economic Burden
As depicted in Figure 2, there was a significant path between caregiver education and economic burden in the expected direction (b = –0.23, p < 0. 05); caregivers with less education reported higher levels of economic burden. Alternatively, no direct relationship between income and economic burden was found. An indirect path between income and economic burden was found (b = 0.09, p < 0.05), showing that caregivers with higher income and higher-order patient symptoms had greater economic burden.
Stressors and Economic Burden
The results show a direct path between both increasing patient symptoms (b = 0.39, p < 0. 001) and greater number of children in the home (b = 0.21, p < 0.05) and increased economic burden.
Stressors and Age and Economic Burden
An indirect path from age through total symptoms leading to economic burdens was significant (b = –0.07, p < 0.05), suggesting that younger spouses caring for a husband or wife with more symptoms experienced higher economic burdens. No indirect path was found from age through number of children in the home and economic burden.
DISCUSSION
Support of family is a core function of hospice and palliative care (Hudson et al., 2008), yet the efforts to address spousal caregiver needs have been hampered by a lack of descriptive data on the correlates and predictors of economic burden. Guided by stress-process theory (Pearlin et al., 1990), our study sheds light on the salient contextual demographic and stressor variables that influence variability in economic burden experienced by spousal caregivers to husbands or wives with lung cancer. The results reveal that stressor variables such as patient symptoms and number of children in the home, and the demographic variable of education, were all directly associated with economic burden, whereas indirect paths of association were found between two other demographic variables (i.e., income and age) and economic burden through patient symptoms.
One of the most striking findings of our study is the variety of ways that patient symptoms influenced the variability found in economic burden. The number of symptoms in a patient was significantly and directly related to economic burden and simultaneously lay in the pathway between caregiver age and income and economic burden. Simply put, more symptoms were associated with greater financial cost. Given the low survival rates and the high incidence of physical and psychological symptoms associated with lung cancer and its treatments, many spouses were coping with their personal grief and emotional needs while witnessing the suffering of their husband or wife experiencing multiple symptoms (Pearman, 2008). Indeed, 75% of the caregivers in our study reported that their spouses experienced two or more of these symptoms. There is evidence to suggest that cancer caregivers commonly felt ill prepared to take up their caregiving role (Hinds, 1985), even when well educated (Hinds, 1985). Our results support the findings from a previous study of breast cancer caregivers which reported that higher-order patient symptoms, requiring multiple medications, were associated with economic burden among family caregivers (Grunfeld et al., 2004). While we have learned that symptoms are related to economic cost, future research is needed to examine the mechanisms that support or influence this relationship. Other evidence documents that certain symptoms such as pain are very expensive in terms of both direct and indirect costs (Grunfeld et al., 2004). The results of our study are preliminary in nature and do not include the potential role of symptom intensity, information about which the caregiver could only speculate. Thus, future research eliciting a lung cancer patient’s assessment of symptom severity would shed light on this aspect.
As expected, the number of children in the home was directly related to economic burden. These findings are not surprising given the high costs of child-rearing (Lino, 1998). It is not uncommon for family members enacting multiple caregiving roles to experience greater burden (Edwards et al., 2002). Interestingly, one study of caregivers of spouses with cancer reported that those with minor children in the home received more tangible support with household tasks and emotional support from other family members than those with none (Stommel & Kingry, 1991). These support patterns did not include financial support that would be more logically connected to economic burden. Not surprisingly, younger caregivers were more likely to have children in the home, although we did not find an indirect path between age and economic burden through the presence of minor children. Our findings indicate that caregivers with lower education levels were significantly more likely to experience economic burdens. This result is important given the relatively small amount of literature on the role that education plays in the economic burdens of caregivers. While education was significant in our model, one unexpected finding was that there was no direct relationship between income and burden, and, contrary to our hypothesis, caregivers with higher incomes who were caring for patients with more symptoms reported higher levels of economic burden. This is surprising in light of past research showing a correlation between low income and economic burden in studies of caregivers for patients with cancer and other chronic illnesses (Kim & Schulz, 2008; Schulz et al., 2006). It is possible that our primarily middle-class sample did not reflect sufficient variability of income to capture the potential effects of low income. An alternative explanation is that persons with higher incomes who were caring for patients with more severe symptoms had more resources available to expend in managing those symptoms, and they also may have had more income or savings to be lost than those with lower incomes.
While no direct path from age to economic burden was found, our results suggest that younger caregivers were significantly more likely to experience economic burdens, compared to older spousal caregivers, when providing for patients with a higher number of symptoms. These findings have been borne out in prior studies of cancer caregivers, which found that younger caregivers experience more demands than older ones (Grunfeld et al., 2004; Nijboer et al., 2000). As suggested in other work, younger caregivers are more likely to be in the workforce and have other pressures in addition to caregiving (Cannuscio et al., 2004). When symptoms are causing difficulties for their spouse, younger employed caregivers are more likely to perceive work-role disruptions caused by caring for a husband or wife.
Some 41% of the spouses surveyed reported a loss in source of income, and 20% reported a loss of savings due to illness. A smaller percentage of family caregivers reported that the costs of care for their husband or wife required putting off important medical care or educational plans for other family members. These findings suggest that some spouses were sacrificing their own medical needs and educational opportunities, which may subsequently have had other detrimental effects on health and well-being. Identifying these spouses who are at particular risk for economic burden and exploring alternative approaches for minimizing these risks would have important implications for service providers.
Implications
There are a number of implications that can be drawn from our study that need to be taken into consideration. First, routine assessment and follow-up of patient symptoms throughout the course of treatment and illness and ongoing support of caregivers in helping them to address these symptoms are essential. Timely assessment and treatment of physical and psychological symptoms associated with cancer and related treatment are considered critical to quality clinical care practice (NCPQPC, 2009). Service providers may consider interventions that provide additional education regarding symptom management, information on community resources, and financial counseling. Second, routine assessment of the resources of and demands on families, including the number of children in the home, and the financial strains they are experiencing, and potential community or financial resources to address their needs would be most useful. Finally, interventions and support are warranted for younger caregivers who have multiple demands and for caregivers who are less well educated, who might need additional support to ameliorate the economic burden of lung cancer on their families.
LIMITATIONS OF OUR STUDY
The results of our study provide additional insight into the costs of caregiving for spouses of patients with lung cancer. However, several limitations exist. First, the study is cross-sectional and relies on retrospective data. Over time, perceptions may change, hindering the specificity of a caregiver’s answers. While we asked caregivers to share their thoughts about the extent to which economic burdens resulted from the illness, without time-ordered data we must be cautious regarding any implications of causality. Another limitation that restricts the generalizability of study findings is the nature of the sample itself. Although ACCESS sought a representative statewide sample and over-sampled by race, the participants were primarily of European descent. Larger national studies are needed to offer population estimates regarding overall economic impacts for lung cancer caregivers. While the data do provide some information on the economic impact of caregiving, they lack specific information on caregiver employment status, the costs of care, and the assets of patients and caregivers. Additionally, the data do not provide information on caregiving supports (i.e., home health, financial assistance) or on other caregivers who might assist the primary caregiver. These variables are important, as they may provide further information as to specific caregiving experiences leading to economic burden in spousal caregivers. Moreover, the study lacks information about the exact costs of care associated with specific caregiving duties and the time spent in caregiving—important variables when attempting to understand the overall economic impact of lung cancer on a caregiving spouse. Finally, the data do not include information on symptom severity or intensity, important issues and difficult to assess when employing caregiver data.
Despite its limitations, our study provides important insight into the lives of the caregivers of spouses with lung cancer. The multifaceted hardships faced by these spouses are numerous, and the economic burden involved puts caregivers at risk for other detrimental outcomes (Aoun et al., 2005). The relationship between patient symptoms and economic burden has immediate practical implications for healthcare practitioners, underscoring the need to address patient symptoms early, before they affect a family’s economic well-being. The relationship between number of children in the home and economic burden suggests the potential value of identifying families at greater risk, and of considering a respite and family-based services to support them. Attention should be paid to documenting costs and expenditures, the effects of illness and contextual variables on caregiver employment, changes in social roles, perceptions of spouses regarding factors contributing to care costs, and the more distal effects of economic burden on caregiver and family outcomes. Given the stigma and isolation that lung cancer patients and families commonly experience, additional professional supports may be necessary to respond to their needs.
Acknowledgments
This study employed data from the Assessment of Cancer Care and Satisfaction Survey (ACCESS), a project of the Wisconsin Comprehensive Cancer Control Program. Funding for the Wisconsin CCC Program was provided by the Centers for Disease Control and Prevention, the Wisconsin Department of Health Services, the Wisconsin Partnership Fund for a Healthy Future, and the University of Wisconsin Paul P. Carbone Comprehensive Cancer Center. This manuscript was prepared with support from the National Institute of Mental Health (T32 MH65185 to Jan Greenberg).
The authors also gratefully acknowledge the bereaved family members for their participation in our study and the contributions of our colleagues who participated in the design of ACCESS.
Footnotes
The authors have no financial conflicts of interest to declare.
References
- American Cancer Society. Wisconsin cancer facts and figures. Waukesha, WI: American Cancer Society Midwest Division; 2011. [Google Scholar]
- Aoun SM, Kristjanson LJ, Currow DC, et al. Caregiving for the terminally ill: At what cost? Journal of Palliative Medicine. 2005;19(7):551–555. doi: 10.1191/0269216305pm1053oa. [DOI] [PubMed] [Google Scholar]
- Bakas T, Lewis RR, Parsons JE. Caregiving tasks among family caregivers of patients with lung cancer. Oncology Nursing Forum. 2001;28(5):847–854. [PubMed] [Google Scholar]
- Bentler P. Comparative fit indexes in structural equation modeling. Psychology Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Braun M, Mikulincer M, Rydall A, et al. Hidden morbidity in cancer: Spouse caregivers. Journal of Clinical Oncology. 2007;25(30):4829–4834. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- Brown ML, Lipscomb J, Snyder C. The burden of illness of cancer: Economic cost and quality of life. Annual Review of Public Health. 2001;22:91–113. doi: 10.1146/annurev.publhealth.22.1.91. [DOI] [PubMed] [Google Scholar]
- Buckwalter KC, Gerdner L, Kohout F, et al. A nursing intervention to decrease depression in family caregivers of persons with dementia. Archives of Psychiatric Nursing. 1999;13(2):80–88. doi: 10.1016/s0883-9417(99)80024-7. [DOI] [PubMed] [Google Scholar]
- Cannuscio CC, Colditz GA, Rimm EB, et al. Employment status, social ties, and caregivers’ mental health. Social Science & Medicine. 2004;58(7):1247–1256. doi: 10.1016/S0277-9536(03)00317-4. [DOI] [PubMed] [Google Scholar]
- Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients’ families: SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. The Journal of the American Medical Association. 1994;272(23):1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- Du W, Reeves JH, Gadgeel S, et al. Cost-effectiveness and lung cancer clinical trials. Cancer. 2003;98(7):1491–1496. doi: 10.1002/cncr.11659. [DOI] [PubMed] [Google Scholar]
- Edwards AB, Zarit SH, Stephens MA, et al. Employed family caregivers of cognitively impaired elderly: An examination of role strain and depressive symptoms. Aging & Mental Health. 2002;6(1):55–61. doi: 10.1080/13607860120101149. [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Fairclough DL, Slutsman J, et al. Understanding economic and other burdens of terminal illness: The experience of patients and their caregivers. Annals of Internal Medicine. 2000;132(6):451–459. doi: 10.7326/0003-4819-132-6-200003210-00005. [DOI] [PubMed] [Google Scholar]
- Ferrara M, Langiano E, di Brango T, et al. Prevalence of stress, anxiety and depression in with Alzheimer caregivers. Health and Quality of Life Outcomes. 2008;6:93. doi: 10.1186/1477-7525-6-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortner BV, Demarco G, Irving G, et al. Description and predictors of direct and indirect costs of pain reported by cancer patients. Journal of Pain and Symptom Management. 2003;25(1):9–18. doi: 10.1016/s0885-3924(02)00597-3. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Linder J, Given CW, et al. The proliferation of primary cancer caregiving stress to secondary stress. Cancer Nursing. 2008;31(2):116–123. doi: 10.1097/01.NCC.0000305700.05250.9d. quiz 124-115. [DOI] [PubMed] [Google Scholar]
- Gridelli C, Ferrara C, Guerriero C, et al. Informal caregiving burden in advanced non-small-cell lung cancer: The HABIT study. Journal of Thoracic Oncology. 2007;2(6):475–480. doi: 10.1097/01.JTO.0000275342.47584.f3. [DOI] [PubMed] [Google Scholar]
- Griffin JP, Koch KA, Nelson JE, et al. Palliative care consultation, quality-of-life measurements, and bereavement for end-of-life care in patients with lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition) Chest. 2007;132(Suppl. 3):404S–422S. doi: 10.1378/chest.07-1392. [DOI] [PubMed] [Google Scholar]
- Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Canadian Medical Association Journal. 2004;170(12):1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanratty B, Holland P, Jacoby A, et al. Financial stress and strain associated with terminal cancer: A review of the evidence. Journal of Palliative Medicine. 2007;21(7):595–607. doi: 10.1177/0269216307082476. [DOI] [PubMed] [Google Scholar]
- Hayman JA, Langa KM, Kabeto MU, et al. Estimating the cost of informal caregiving for elderly patients with cancer. Journal of Clinical Oncology. 2001;19(13):3219–3225. doi: 10.1200/JCO.2001.19.13.3219. [DOI] [PubMed] [Google Scholar]
- Hinds C. The needs of families who care for patients with cancer at home: Are we meeting them? Journal of Advanced Nursing. 1985;10(6):575–581. doi: 10.1111/j.1365-2648.1985.tb00550.x. [DOI] [PubMed] [Google Scholar]
- Hudson P, Quinn K, O’Hanlon B, et al. Family meetings in palliative care: Multidisciplinary clinical practice guidelines. BMC Palliative Care. 2008;7:12. doi: 10.1186/1472-684X-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan D. Structural equation modeling: Foundations and extensions. Los Angeles: Sage; 2009. [Google Scholar]
- Khullar O, Colson YL. The underfunding of lung cancer research. Journal of Thoracic Cardiovascular Surgery. 2009;138(2):275. doi: 10.1016/j.jtcvs.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Kim Y, Schulz R. Family caregiver strains: Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health. 2008;20(5):483–503. doi: 10.1177/0898264308317533. [DOI] [PubMed] [Google Scholar]
- Kramer BJ, Kavanaugh M, Trentham-Dietz A, et al. Predictors of family conflict at the end of life: The experience of spouses and adult children of persons with lung cancer. The Gerontologist. 2010;50(2):215–225. doi: 10.1093/geront/gnp121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutikova L, Bowman L, Chang S, et al. The economic burden of lung cancer and the associated costs of treatment failure in the United States. Lung Cancer. 2005;50(2):143–154. doi: 10.1016/j.lungcan.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Lino M. Do child support awards cover the cost of raising children? Family Economics & Nutrition Review. 1998;11(1/2):29. [Google Scholar]
- Muthen L, Muthen B. MPLUS user’s guide. 5. Los Angeles: Muthen & Muthen; 2001. [Google Scholar]
- National Cancer Institute. Cancer trends progress report, 2012. 2010 Available from http://progressreport.cancer.gov.
- National Consensus Project for Quality Palliative Care (NCPQPC) Clinical guidelines for quality palliative care. Pittsburgh: NCPQPC; 2009. [Google Scholar]
- Neal MB, Ingersoll-Dayton B, Starrels ME. Gender and relationship differences in caregiving patterns and consequences among employed caregivers. The Gerontologist. 1997;37(6):804–816. doi: 10.1093/geront/37.6.804. [DOI] [PubMed] [Google Scholar]
- Nijboer C, Triemstra M, Tempelaar R, et al. Patterns of caregiver experiences among partners of cancer patients. The Gerontologist. 2000;40(6):738–746. doi: 10.1093/geront/40.6.738. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, et al. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist. 1990;30(5):583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pearman T. Psychosocial factors in lung cancer: Quality of life, economic impact, and survivorship implications. Journal of Psychosocial Oncology. 2008;26(1):69–80. doi: 10.1300/j077v26n01_05. [DOI] [PubMed] [Google Scholar]
- Pedhazur E, Schmelkin L. Measurement, design and analysis: An integrated approach. Hillsdale, NJ: Lawrence Erlbaum; 1991. [Google Scholar]
- Sarna L. Women with lung cancer: Impact on quality of life. Quality of Life Research. 1993;2(1):13–22. doi: 10.1007/BF00642885. [DOI] [PubMed] [Google Scholar]
- Savage S, Bailey S. The impact of caring on caregivers’ mental health: A review of the literature. Australian Health Review. 2004;27(1):111–117. doi: 10.1071/ah042710111. [DOI] [PubMed] [Google Scholar]
- Schulz R, Martire LM. Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. American Journal of Geriatric Psychiatry. 2004;12(3):240–249. [PubMed] [Google Scholar]
- Schulz R, Boerner K, Shear K, et al. Predictors of complicated grief among dementia caregivers: A prospective study of bereavement. American Journal of Geriatric Psychiatry. 2006;14(8):650–658. doi: 10.1097/01.JGP.0000203178.44894.db. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Given BA, Given CW, et al. Predictors of distress in caregivers of persons with a primary malignant brain tumor. Research in Nursing and Health. 2006;29(2):105–120. doi: 10.1002/nur.20116. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Donovan HS, Given CW, et al. Predictors of employment and lost hours from work in cancer caregivers. Journal of Psychological Oncology. 2008;17(6):598–605. doi: 10.1002/pon.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger J, Lind J. Statistically based tests for the number of common factors; Paper presented at a meeting of the Psychometric Society; Iowa City, Iowa. 1980. [Google Scholar]
- Stommel M, Kingry M. Support patterns for spouse-caregivers of cancer patients: The effect of the presence of minor children. Journal of Cancer Nursing. 1991;14(4):200–205. [PubMed] [Google Scholar]
- Trentham-Dietz A, Walsh MC. ACCESS: Assessment of cancer care and satisfaction. Summary of results. Madison: University of Wisconsin, Paul P. Carbone Comprehensive Cancer Center; 2008. Available from http://www.wicancer.org/documents/ACCESS%20results%20doc.pdf. [Google Scholar]
- Yun YH, Rhee YS, Kang IO, et al. Economic burdens and quality of life of family caregivers of cancer patients. Oncology. 2005;68(2–3):107–114. doi: 10.1159/000085703. [DOI] [PubMed] [Google Scholar]