For the majority of patients with chronic heart failure (HF), there are periods of stability punctuated by episodes of clinical worsening leading to hospitalization. Although generally regarded as necessary for short-term symptomatic relief, these hospitalizations are traditionally viewed as an ominous inflection point in the natural history of HF. Indeed, observational studies suggest post-hospitalization mortality risk 3-fold higher than patients never hospitalized, with stepwise increases in risk with each subsequent hospitalization.1, 2 These findings, in combination with biomarker data collected from hospitalized patients, led to a hypothesis that HF hospitalization represented a distinct pathophysiologic event that directly mediated poor post-discharge outcomes.3, 4 Comparisons were drawn to acute myocardial infarction as a transient period of irreversible end-organ injury that left patients with a permanently heightened risk of adverse outcomes. This theory sparked a generation of neutral/negative phase III hospitalized HF trials designed to test effects of investigational therapies initiated soon after hospital presentation (e.g., within 24–48 hours) on post-discharge mortality and re-hospitalization endpoints, with the belief that rapid introduction of therapy may attenuate or abort organ injury.4 Likewise, the concept of “door-to-diuretic” time has recently emerged, again extrapolating from acute myocardial infarction that rapid therapy and symptomatic relief soon after hospital presentation may directly lead to improved longer-term outcomes.5, 6
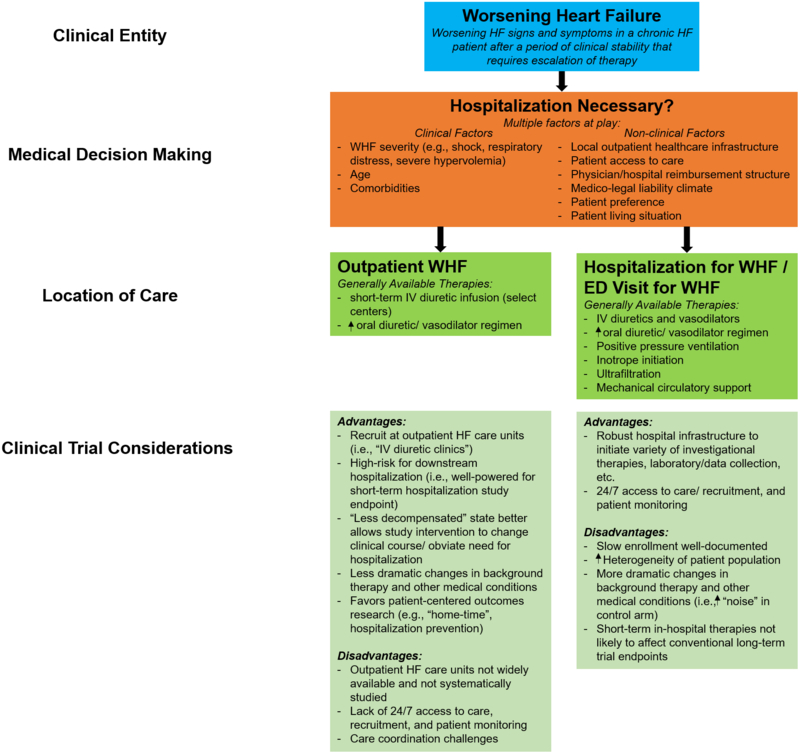
However, in contrast to the traditional teaching regarding HF hospitalization, emerging data strongly suggests that WHF and location of care should be disentangled (Figure).7 Multiple analyses from clinical trial cohorts have found WHF patients treated in the outpatient setting to have subsequent mortality similar to hospitalized populations.8–10 Importantly, these studies suggest that clinical characteristics, rather than location of care or recentness of hospitalization, are the dominant determinants of risk.10 As such, patients hospitalized for HF are not universally at highest risk.10 A proportion of both clinically stable and clinically worsening patients treated in the outpatient setting may carry comparable or even higher risk than many hospitalized patients. Although this newer framework may appear intuitive, it represents a paradigm shift in terms of how we recognize and study WHF, how we view the risks and benefits of HF hospitalization, and how we design future clinical trials.4
Figure. Conceptual Framework for Worsening Heart Failure.
Worsening heart failure may be managed in both the outpatient and inpatient settings, as determined by many factors. Studying the inpatient versus outpatient WHF populations in randomized clinical trials presents specific advantages and disadvantages for successful clinical trial execution. ED indicates emergency/department; HF, heart failure; IV, intravenous.Reproduced with permission from Greene SJ et al.7 Copyright © 2018 American Medical Association. All rights reserved.
In this issue of the Journal, Ferreira and colleagues provide further insight into the interplay between HF risk and location of care.11 The authors present a post-hoc analysis from the BIOlogy Study to TAilored Treatment in Chronic Heart Failure (BIOSTAT-CHF), a prospective observational study of 2,516 HF patients with worsening signs and symptoms across 11 European countries with median follow-up 21 months.12 Patients treated in either the inpatient (N=1,694) or outpatient setting (N=822) were eligible. In comparing patients across these 2 care locations, the authors found inpatients to generally carry a higher risk profile, with tendency for higher natriuretic peptide level, lower blood pressure, higher heart rate, greater comorbidity burden, and less background use of guideline-directed medical therapy. Likewise, as compared to outpatients, inpatient status was independently associated with higher risk of the primary composite endpoint of mortality or HF hospitalization. However, this association was driven exclusively by excess HF hospitalization with no independent association between location of care and mortality after adjustment. Next, the authors derived an integer risk score comprised of objective clinical characteristics to stratify the cohort into tertiles of risk and performed further comparisons by inpatient versus outpatient status. The distribution of risk profile varied by care setting, with the inpatient group having substantially more “high-risk” and substantially fewer “low-risk” patients. Nonetheless, there was sizeable overlap in the incidence of the primary endpoint across inpatient and outpatient groups, such that all but the low-risk outpatients carried risk similar to the overall inpatient group.
The authors should be congratulated for a timely study that further supports biology and clinical risk as independent from location of HF care. Importantly, this study elegantly demonstrates that while a hospitalized cohort may contain a greater percentage of “high-risk” patients, “high-risk” is not specific to the hospital setting and a large proportion of outpatients carry a similar prognosis. Nonetheless, limitations of this work should be acknowledged. First, the definition of WHF and the inclusion criteria for BIOSTAT-CHF warrant attention. The protocol language specified inclusion of patients with worsening signs and symptoms, but worsening was apparently defined per investigator discretion.12 Although population risk was enriched via certain criteria (e.g., reduced ejection fraction and/or elevated natriuretic peptide level, <50% of target dose of either ACEI/ARB or beta-blocker therapy), these factors cannot distinguish between stable or worsening clinical status since they reflect only a single time point. Rather, documentation of an escalated loop diuretic regimen (as used in most prior and ongoing WHF trials) or worsening clinical signs/symptoms over ≥2 time points would have provided a more robust and generalizable WHF definition. The uncertainty regarding the degree of worsening versus stability is particularly relevant to the outpatient cohort, where lack of hospitalization coupled with relatively modest rates of clinical congestion on exam (e.g., edema 36%, rales 26%, jugular venous distention 22%) questions the presence or degree of clinical deterioration in this group. Nonetheless, this feature should not diminish the importance of the present findings, as demonstration of overlapping degrees of risk between hospitalized and stable outpatients would still convey the importance of objective clinical variables, rather than location of care, in driving patient risk. Second, further uncertainly regarding the WHF definition lies with inclusion of new-onset HF in BIOSTAT-CHF. Previous work has outlined significant differences between de novo or recently diagnosed HF and worsening of chronic HF.13 This feature should be recognized when generalizing findings to other HF populations. Third, BIOSTAT-CHF was an exclusively European cohort. Characteristics of enrolled cohorts and the relative associations with clinical events may not be generalizable to other global regions. This limitation may be particularly important in the context of the observed independent association with the primary endpoint driven exclusively by rehospitalization, an endpoint much more vulnerable to global differences in practice patterns as compared to mortality.
REASSESSING THE IMPACT OF HEART FAILURE HOSPITALIZATION: A MARKER, NOT MEDIATOR, OF RISK
Unlike acute myocardial infarction where sudden onset of a clinical symptom (i.e., chest pain) correlates strongly with timing of a biologic event (i.e., plaque rupture) and prompt presentation to a hospital, “acute” HF is usually not “acute”. Only a minority of WHF patients experience rapid and severe deterioration leading to an immediate emergency department (ED) presentation.7 By contrast, most experience gradual worsening of signs and symptoms over a more extended period, an observation further supported by invasive monitoring showing gradual increases in filling pressures days to weeks before onset of worsening symptoms and hospital presentation.14 Likewise, markers of organ injury are not specific to the hospital stay. Persistent or new-onset troponin elevation can be seen before, during, or after a hospitalization, as well as in times of clinical stability.15 Thus, it is increasingly important to recognize that while hospitalization for many WHF patients is undoubtedly necessary (e.g., cardiogenic shock, respiratory failure) and certainly a marker of risk, the decision to hospitalize a patient is 1) inherently subjective; 2) influenced by many non-clinical factors, including patient preference, level of caregiver support, global and regional healthcare infrastructure and practice patterns, and financial and liability incentives; and 3) not in and of itself representative of a sudden change in biology.7 Just as subjective is the timing of actual hospital presentation, as the decision of if/when to initiate, continue, or abort an escalated outpatient regimen in favor of hospitalization may be highly variable. For these reasons, it is not surprising that despite numerous attempts with sophisticated statistical models and machine learning, the ability to predict hospitalization in HF populations remains poor, whereas several robust and validated models exist for biologic endpoints like mortality.16, 17 The current data from BIOSTAT-CHF adds to the mounting evidence strongly suggesting hospitalization for HF be best viewed as a care strategy and location of care, rather than a distinct biologic entity.8–11
CLINICAL TRIAL CONSIDERATIONS
Future research must determine the degree to which WHF is an inevitable consequence of progressive HF versus a result of poor healthcare delivery and suboptimal use of guideline-directed therapy. Nonetheless, effective study of WHF must start with a robust and thoughtful definition. Although the most appropriate and practical definition of WHF can be debated and current approaches center on escalation of diuretic therapy, it is increasingly clear that WHF should not be defined strictly by HF hospitalization. Rather, we advocate for a definition based on patient characteristics and/or therapy received, irrespective of the care setting. Although clinical trial considerations may vary by location of patient enrollment (Figure), a select number of recent and ongoing trials have already incorporated outpatient WHF within trial eligibility criteria and endpoint definitions.18 Advantages of such strategies include the potential to improve the generalizability of findings to the broader WHF population, mitigate the issue of variable thresholds of hospitalization across countries in a global trial, and increase statistical power for purposes of reduced sample size and duration of follow-up.
In conclusion, as the public health and economic burden of HF continues to grow, recognizing the existence and prognostic significance of outpatient WHF is critical. Outpatient status is not an effective surrogate for clinical stability or low-risk. Although hospitalization is certainly a marker of a high-risk population, a substantial proportion of the outpatient HF population has a comparable prognosis and an urgent need for improved therapy.
Acknowledgments
CONFLICT OF INTEREST
S.J.G. is supported by the National Heart Lung and Blood Institute T32 postdoctoral training grant (T32HL069749–14), a Heart Failure Society of America/ Emergency Medicine Foundation Acute Heart Failure Young Investigator Award funded by Novartis, and has received research support from Amgen and Novartis. G.M.F. has received research funding from Otsuka, Novartis, Roche Diagnostics, Amgen, Merck, American Heart Association, and the National Heart, Lung, and Blood Institute; and has served as a consultant for Novartis, Roche Diagnostics, Amgen, Trevena, Cytokinetics, Madeliene, Myokardia, Bristol-Myers Squibb, Stealth Biotherapeutics, and GlaxoSmithKline. J.B. has received research support from the National Institutes of Health, PCORI and the European Union; and serves as a consultant for Amgen, Array, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squib, CVRx, G3 Pharmacautical, Innolife, Janssen, Luitpold, Medtronic, Merck, Novartis, Relypsa, StealthPeptide, SC Pharma, Vifor, and ZS Pharma.
Funding: None
REFERENCES
- 1.Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB, Yusuf S, Swedberg K, Young JB, Michelson EL, Pfeffer MA. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation 2007;116:1482–1487. [DOI] [PubMed] [Google Scholar]
- 2.Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J 2007;154:260–266. [DOI] [PubMed] [Google Scholar]
- 3.Metra M, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Ponikowski P, Unemori E, Voors AA, Adams KF Jr., Dorobantu MI, Grinfeld L, Jondeau G, Marmor A, Masip J, Pang PS, Werdan K, Prescott MF, Edwards C, Teichman SL, Trapani A, Bush CA, Saini R, Schumacher C, Severin T, Teerlink JR. Effect of serelaxin on cardiac, renal, and hepatic biomarkers in the Relaxin in Acute Heart Failure (RELAX-AHF) development program: correlation with outcomes. J Am Coll Cardiol 2013;61:196–206. [DOI] [PubMed] [Google Scholar]
- 4.Ambrosy AP, Butler J, Gheorghiade M. Clinical trials in acute heart failure: beginning of the end or end of the beginning? Eur J Heart Fail 2017;19:1358–1360. [DOI] [PubMed] [Google Scholar]
- 5.Matsue Y, Damman K, Voors AA, Kagiyama N, Yamaguchi T, Kuroda S, Okumura T, Kida K, Mizuno A, Oishi S, Inuzuka Y, Akiyama E, Matsukawa R, Kato K, Suzuki S, Naruke T, Yoshioka K, Miyoshi T, Baba Y, Yamamoto M, Murai K, Mizutani K, Yoshida K, Kitai T. Time-to-Furosemide Treatment and Mortality in Patients Hospitalized With Acute Heart Failure. J Am Coll Cardiol 2017;69:3042–3051. [DOI] [PubMed] [Google Scholar]
- 6.Felker GM, Januzzi JL Jr. “Time Is Muscle” in Acute Heart Failure: Critical Concept or Fake News? J Am Coll Cardiol HF 2018;6:295–297. [DOI] [PubMed] [Google Scholar]
- 7.Greene SJ, Mentz RJ, Felker GM. Outpatient Worsening Heart Failure as a Target for Therapy: A Review. JAMA Cardiol 2018;3:252–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skali H, Dwyer EM, Goldstein R, Haigney M, Krone R, Kukin M, Lichstein E, McNitt S, Moss AJ, Pfeffer MA, Solomon SD. Prognosis and response to therapy of first inpatient and outpatient heart failure event in a heart failure clinical trial: MADIT-CRT. Eur J Heart Fail 2014;16:560–565. [DOI] [PubMed] [Google Scholar]
- 9.Okumura N, Jhund PS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Swedberg K, Zile MR, Solomon SD, Packer M, McMurray JJ. Importance of Clinical Worsening of Heart Failure Treated in the Outpatient Setting: Evidence From the Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure Trial (PARADIGM-HF). Circulation 2016;133:2254–2262. [DOI] [PubMed] [Google Scholar]
- 10.Cook TD, Greene SJ, Kalogeropoulos AP, Fonarow GC, Zea R, Swedberg K, Zannad F, Maggioni AP, Konstam MA, Gheorghiade M, Butler J. Temporal Changes in Postdischarge Mortality Risk After Hospitalization for Heart Failure (from the EVEREST Trial). Am J Cardiol. 2016;117:611–616. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira JP, Metra M, Mordi I, Gregson J, Ter Maaten J, Tromp J, Anker S, Dickstein K, Hillege HL, Ng L, Van Veldhuisen DJ, Lang CC, Voors A, Zannad F. Heart failure in the outpatient versus inpatient setting: findings from the BIOSTAT-CHF study. Eur J Heart Fail 2018. [DOI] [PubMed] [Google Scholar]
- 12.Voors AA, Anker SD, Cleland JG, Dickstein K, Filippatos G, van der Harst P, Hillege HL, Lang CC, Ter Maaten JM, Ng L, Ponikowski P, Samani NJ, van Veldhuisen DJ, Zannad F, Zwinderman AH, Metra M. A systems BIOlogy Study to TAilored Treatment in Chronic Heart Failure: rationale, design, and baseline characteristics of BIOSTAT-CHF. Eur J Heart Fail. 2016;18:716–726. [DOI] [PubMed] [Google Scholar]
- 13.Greene SJ, Hernandez AF, Dunning A, Ambrosy AP, Armstrong PW, Butler J, Cerbin LP, Coles A, Ezekowitz JA, Metra M, Starling RC, Teerlink JR, Voors AA, O’Connor CM and Mentz RJ. Hospitalization for Recently Diagnosed Versus Worsening Chronic Heart Failure: From the ASCEND-HF Trial. J Am Coll Cardiol 2017;69:3029–3039. [DOI] [PubMed] [Google Scholar]
- 14.Zile MR, Bennett TD, St John Sutton M, Cho YK, Adamson PB, Aaron MF, Aranda JM Jr., Abraham WT, Smart FW, Stevenson LW, Kueffer FJ, Bourge RC. Transition from chronic compensated to acute decompensated heart failure: pathophysiological insights obtained from continuous monitoring of intracardiac pressures. Circulation 2008;118:1433–1441. [DOI] [PubMed] [Google Scholar]
- 15.Greene SJ, Butler J, Fonarow GC, Subacius HP, Ambrosy AP, Vaduganathan M, Triggiani M, Solomon SD, Lewis EF, Maggioni AP, Bohm M, Chioncel O, Nodari S, Senni M, Zannad F, Gheorghiade M. Pre-discharge and early post-discharge troponin elevation among patients hospitalized for heart failure with reduced ejection fraction: findings from the ASTRONAUT trial. Eur J Heart Fail 2017;20:281–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mortazavi BJ, Downing NS, Bucholz EM, Dharmarajan K, Manhapra A, Li SX, Negahban SN, Krumholz HM. Analysis of Machine Learning Techniques for Heart Failure Readmissions. Circ Cardiovasc Qual Outcomes. 2016;9:629–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frizzell JD, Liang L, Schulte PJ, Yancy CW, Heidenreich PA, Hernandez AF, Bhatt DL, Fonarow GC, Laskey WK. Prediction of 30-Day All-Cause Readmissions in Patients Hospitalized for Heart Failure: Comparison of Machine Learning and Other Statistical Approaches. JAMA Cardiol 2017;2:204–209. [DOI] [PubMed] [Google Scholar]
- 18.Gheorghiade M, Greene SJ, Butler J, Filippatos G, Lam CS, Maggioni AP, Ponikowski P, Shah SJ, Solomon SD, Kraigher-Krainer E, Samano ET, Muller K, Roessig L, Pieske B. Effect of Vericiguat, a Soluble Guanylate Cyclase Stimulator, on Natriuretic Peptide Levels in Patients With Worsening Chronic Heart Failure and Reduced Ejection Fraction: The SOCRATES-REDUCED Randomized Trial. JAMA. 2015;314:2251–2262. [DOI] [PubMed] [Google Scholar]