Abstract
Introduction:
Uterine-conservative surgery via laparoscopy is a challengeable and high risk because of heavy intra-operative bleeding events in reproductive women with highly vascular uterine benign disease. There are three reported cases of women with highly vascular uterine benign diseases and high risk of intra-operative heavy bleeding, but were treated successfully to control intra-operative heavy bleeding risk by transient occlusion of the uterine artery (TOUA) through laparoscopy and resulted in safe conservation of the uterus.
Case Presentation:
The cases of women with high risk of heavy bleeding during therapeutic procedure included cesarean scar pregnancy, hydatid form mole on cesarean scar, and cervical pregnancy. All these women had the strong desire to presere their fertility and uterus. In all the three cases, we used the method of TOUA and performed therapeutic surgeries successfully, with less bleeding and safe conservation of the uterus through laparoscopy.
Conclusion:
Laparoscopic TOUA could be a therapeutic option to manage heavy intra-operative bleeding during conservative uterine surgeries associated with the risk of heavy bleeding.
Keywords: Cervical pregnancy, Cesarean scar-hydatidiform mole pregnancy, Cesarean scar pregnancy, Laparoscopic surgery, Transient occlusion of uterine arteries (TOUA)
INTRODUCTION
Patients with gynecologic uterine diseases, where there are limitations to perform uterine-conservative surgery due to risks of intra-operative heavy bleeding and chances of complications in a surgical approach, occasionally received complicated interventions to manage intra-operative heavy bleeding or total hysterectomy finally. All of these uterine diseases have to be benign but not malignant, and most of them might be related to abnormal pregnancy, which includes abnormal implantation sites (previous operation scar and uterine endocervix) but not tubal and cornual pregnancy. Patients with uterine disease with high vascularity have blood supply by uterine artery majorly, unlike tubal pregnancy or cornual pregnancy where blood supply is by ovarian arterial flow. It is essentially important to control high vascularity of the disease so as to reduce intra-operative complication and keep a safe and stable operation field.
There were few data on how to control intra-operatively high vascular uterine disease, which was supplied majorly by the uterine artery for conserving fertility and the uterus. Also, there were few reports of other effective methods like vasopressin injection in such cases of abnormal pregnancy-related uterine disease.
To reduce the risk of intra-operative complications and heavy bleeding to obtain a stable operation field, it is essential that the uterine artery supply of the uterine abnormal vessels is controlled and uterine arterial blood flow is restored just after of the conservative surgery is completed, which could restore normally vascular architecture of the uterus and help further fertilization.
In these rare and unique conditions refractory to medical treatment, the expanding lesion with high vascularity disturbed surgical curettage through the uterine cervix using straight conventional instruments and could cause lesion site–heavy bleeding due to abnormal and high vascular architecture, which frequently results in failure of the curettage procedure and intra-operative complications.
To perform conservative surgical therapy effectively and safely, another approach, unlike transcervical approach, has to be considered, and to reduce intra-operative heavy bleeding, an effective controlling of uterine arterial flowing to the lesions is required.
There are several published reports to support conservative uterine surgeries with less intra-operative bleeding risk using technique of transient occlusion of uterine arteries (TOUAs).1–4 We considered an intra-abdominal approach incision and curettage of abnormal pregnancy where transcervical approach is not available. The benefits of laparoscopic surgery being compared to those of laparotomic operation, laparoscopic TOUA and then incision, curettage and suturing of the lesions (cervix and previous cesarean scar) were planned in these three cases. In all of the TOUA-performed operations, endovascular clips were removed and uterine arterial blood flow was restored.
The conservative TOUA laparoscopic surgery in all the three cases of rare gynecologic conditions with a risk of intra-operative heavy bleeding, which included cervical pregnancy and molar disease, and cesarean scar pregnancy was successful.
CASE PRESENTATION
Case 1
A 38-year-old woman, gravida 1 (P1 A2; P: para, A: abortus), with one previous cesarean section was referred to our center with amenorrhea lasting 8 weeks. She had no medical or surgical history except for the cesarean section. She complained of vaginal spotting without abdominal pain. Ultrasound showed a gestational sac on the cesarean scar. Dilatation and curettage was planned. However, continuous and heavy vaginal bleeding required conversion to laparoscopy under general anesthesia and red-cell transfusion (5 U of packed red blood cells). The peritoneum was incised with a cutting monopolar electrode through the triangular area (round, ovarian, and IP ligaments, and the psoas muscle) and along the infundibulopelvic (IP) ligament. The umbilical artery was isolated by blunt-tip suction, and the assistant moved the artery upward and in a lateral direction. It was possible to isolate the branching uterine artery along the umbilical artery using blunt-tip suction. The isolated uterine artery was occluded with an endoscopic vascular clip (Temporary Atraumatic Endo-Vessel-Clips; B. Braun Korea Co, Ltd, Seoul, Korea). Occlusion of the artery on the opposite side of the uterus was performed by the same method.4 Under TOUA, bladder dissection was carried out to treat adhesion of the bladder to the uterine serosa. After transverse incision of the pregnancy site, conceptual tissues were removed and finally the bed of conception was curetted by a laparoscopic forceps. The incised area, cesarean scar was sutured with two layers, including a continuous suture of inner myometrium, and a continuous interlocking suture of outer myometrium and serosa (Figure 1). Both endoscopic clips were removed after incision closure. A drainage tube was inserted through the suprapubic incision. The total volume of estimated blood loss was 1500 mL although the intra-operative estimated blood loss was 50 mL. The total operation time was 90 minutes and the time of laparoscopic surgery with TOUA was 45 minutes. The preoperative hemoglobin level was 12.4 g/dL. Her hemoglobin level was 13.7 g/dL on the day of the operation and 12.2 g/dL on the day after the operation. At 3 days postoperatively, the patient was discharged without any complications. Within 1 month after the surgery, serum beta-human chorionic gonadotropin (β-hCG) and uterine architecture proven by ultrasonography returned to be normal.
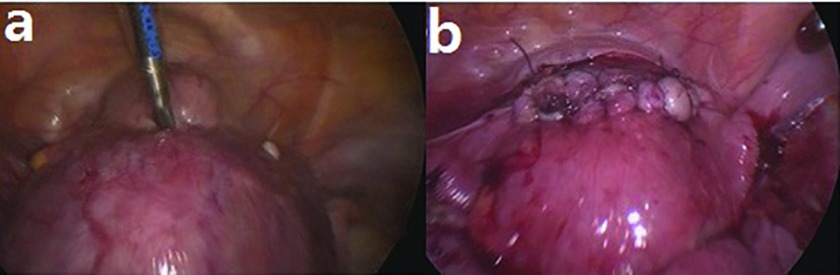
Figure 1.
Laparoscopic excision of cesarean scar pregnancy under TOUA. (A) Laparoscopy revealed a violet lesion in the lower segment of the uterus. (B) Postsutured uterus after removal of both vascular clips on the uterine arteries.
Case 2
A 44-year-old woman, gravida 1 (P1 A1; P: para, A: abortus) with one previous cesarean delivery visited our hospital with a 4-week amenorrhea and abnormal vaginal bleeding. She had no medical or surgical history except for the cesarean section. Her uterus was enlarged to 9 weeks' gestational age. Her initial β-hCG count was 450,945.9 mIU/mL. The sonogram showed a heterogeneous mass with multiple small cystic areas (Figure 2). Transcervical dilatation and curettage with laparoscopic TOUA under general anesthesia was performed. The volume of estimated blood loss was 130 mL. Two days after the operation, the patient was discharged without any complications. The pathology report showed a hydatidiform mole, suggesting a partial mole. The patient's β-hCG level decreased to 11,427.2 mIU/mL after 2 weeks. However, 1 week later, the β-hCG level increased to 16,180.9 mIU/mL. Ultrasound showed remnant molar tissue (2 × 2 cm) on the cesarean scar. Before reoperation, actinomycin (1.25 mg/m2) was injected twice and the patient's β-hCG level was 2422.7 mIU/mL. Laparoscopic excision of the hydatidiform mole on the cesarean scar and curettage of the excised bed was performed. There was a 3 × 2-cm remnant hydatidiform molar mass in the anterior lower segment (Figure 2). The volume of estimated blood loss was 400 mL. The operation time was 50 minutes and TOUA time 40 minutes. The patient's preoperative hemoglobin level was 11.6 g/dL and no blood transfusion was needed. Her hemoglobin level was 10.3 g/dL on the day after surgery. At 3 days after the operation, the patient was discharged without any complications. Her β-hCG level declined and normalized within 4 weeks of the operation. Two weeks later, her β-hCG level was undetectable.
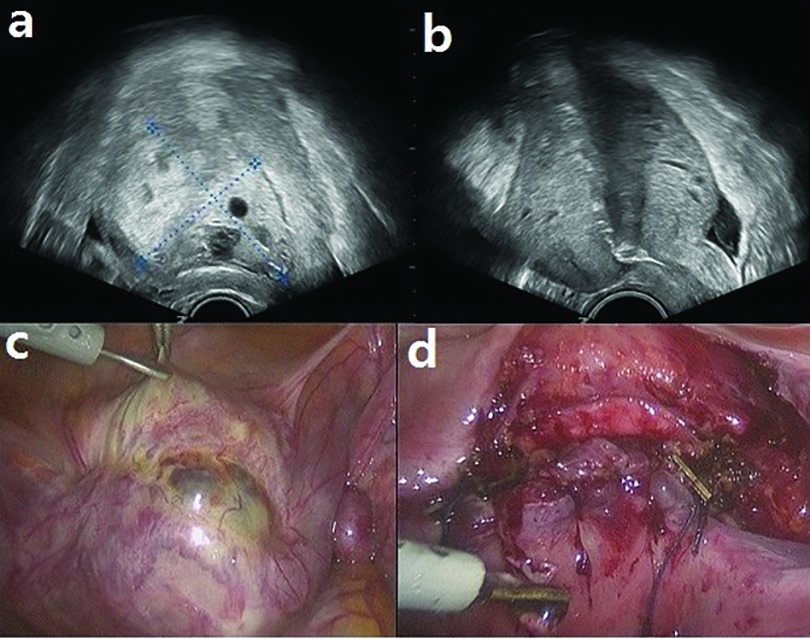
Figure 2.
Hydatidiform mole on a cesarean scar. (A) Initial ultrasonography showing enlarged uterus with a heterogenous mass containing multiple cystic lesions. (B) Ultrasonography after transcervical extirpation with laparoscopic TOUA. (C) Laparoscopy revealed a slight swelling in the lower segment. (D) Postsutured defect of the lower segment after vascular clip removal.
Case 3
A 40-year-old woman was referred to our hospital for a cervical pregnancy and amenorrhea lasting 6 weeks. She had a history of artificial abortion and open abdominal surgery owing to pelvic inflammatory disease about 20 years prior. She had scant vaginal bleeding. At the time of her visit, her β-hCG level was 2045.7 mIU/mL. An ultrasound examination showed a 5-cm mass-like lesion with an irregular margin and hyperechogenicity in her cervix. There was no definite gestational sac-like feature, and therefore, dilatation and curettage (D&C) biopsy was done for pathological confirmation; however, the procedure was incomplete because of profuse bleeding. Cervical cerclage was performed for bleeding control. The patient received 4 cycles of methotrexate (50 mg/m2) weekly, but the mass did not decrease in size and its vascularity did not diminish. Laparoscopic tissue extraction and curettage under TOUA was performed. After excision and curettage of the mass, the surgical defect was sutured with a continuous interlocking suture (Figure 3). Total operation time was 45 minutes. The volume of estimated blood loss was 200 mL. The patient's preoperative hemoglobin level was 13.2 g/dL and she was not given a blood transfusion. Her hemoglobin level was 11.5 g/dL on the day after surgery. On the fourth day after the operation, the patient was discharged without any complications. One week later, her β-hCG level entered the normal range. Two months later, on outpatient clinic, normal shape and vascularity was confirmed by ultrasonography.
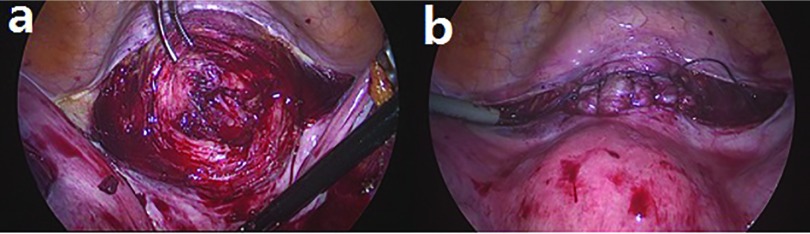
Figure 3.
Cervical pregnancy. (A) Laparoscopy, after incision into the cervix, revealed a gestational sac lesion. (B) Postsutured defect of the cervix, after removal of the vascular clips.
DISCUSSION
Noninvasive treatment as an option for the treatment of ectopic pregnancy and gestational disease such as cervix or cesarean scar sites include medical therapies such as multidose or intrafetal injection of local potassium chloride. However, there are high risks of methotrexate treatment failure in patients with a gestational age > 9 weeks, b-hCG > 10,000 mIU/mL, crown-rump length > 10 mm, and fetal cardiac activity. Furthermore, there is no effective medical treatment in patients who are hemodynamically unstable or have continuous vaginal bleeding. The use of methotrexate is limited to these case reports and other small case series.5–8 Dilation and evacuation is a conservative surgical option; however, its main complication is a high incidence of severe hemorrhage. Gestational trophoblastic disease in a cesarean scar is very rare and presents similar therapeutic challenges as the cesarean scar pregnancy.
When planning treatment for gynecologic diseases that carry substantial risks of massive bleeding, the bleeding makes it difficult to carry out the surgery, therefore laparoscopic surgery is converted to laparotomy or the patient undergoes another aggressive intervention.
In other words, if not for the bleeding risk, laparoscopic surgery could be a prioritized option as compared with other types of surgery. Accordingly, a method for prevention of intra-operative bleeding is important. Several reports describe methods to reduce intra-operative bleeding during elective gynecologic surgery. Topsoee et al9 reported a meta-analysis that showed that prophylactic intervention with tranexamic acid reduced intra-operative bleeding in cases of elective cesarean section or abdominal myomectomy. However, the ectopic pregnancy with abnormal high vascularity is different from the cases of elective cesarean section or abdominal myomectomy. Ugur et al10 reported a prospective randomized clinical study that showed that prophylactic vasopressin injection reduced operating time and the need for electrocoagulation for hemostasis during ectopic pregnancy. Techniques of vasopressin injection have been used worldwide. However, the above study was limited to salpingectomy due to tubal pregnancy. In the cases of high abnormal vascularity, vasopressin injection could directly flow into vessels and cause heart problems. Also, vasopressin is contraindicated in patients with vascular disease and impaired renal function.11 There was no definite effective method of conservative surgery with control of heavy intra-operative bleeding. Permanent ligation of the uterine arteries is another method of reducing intra-operative bleeding during elective gynecologic surgery. Helal et al12 reported that uterine artery ligation is associated with less blood loss. After uterine artery ligation, uterine biopsy reveals chronic hypovascularization. Performing a prophylactic uterine artery embolization before an operation is one option. Ko et al7 reported that prophylactic uterine artery embolization in patients with a high risk of bleeding might be a safe and effective way to prevent serious bleeding. However, uterine artery embolization and permanent ligation of the uterine arteries concerns fertility and ovarian insufficiency. According to current guidelines, uterine artery embolization and permanent ligation are contraindicated for patients who desire to preserve their fertility.
TOUA is an intra-operative technique for prevention of uterine bleeding that involves bilateral blockage of uterine arterial blood flow.1–4
Compared to other methods, TOUA has several additional benefits, which includes an effective uterine bleeding control during uterine operation and restoration of uterine blood flow at the end of an operation by removal of endovascular clips and immediately applying technique during a surgery with heavy uterine bleeding. Also, ovarian insufficiency in reproductive women received conservative uterine surgeries is clinically significant. Unlike permanent ligation or embolization of uterine arteries, conservative uterine surgery under TOUA could have no symptoms or aftereffects of ovarian insufficiency. In our published studies,1–4 there was no case of ovarian insufficiency or failure in patients who received TOUA through laparoscopy or laparotomy. However, the study of ovarian function and prospectively comparison was out of the scope of our study. To clarify effectiveness of TOUA in ovarian function reservation, we need large prospective randomized further study.
CONCLUSION
In rare, abnormal pregnancies such as cervical pregnancy or cesarean scar pregnancy with high risk of intra-operative bleeding, laparoscopic conservative surgery under TOUA could be a good option to perform a complete extirpation of abnormal conception with clean and stable operative condition.
Contributor Information
Yong-Soon Kwon, Department of Obstetrics and Gynecology, Nowon Eulji Medical Center, Eulji University, Seoul, Korea..
Yoo Mi Cho, Department of Obstetrics and Gynecology, College of Medicine, University of Ulsan, Ulsan University Hospital, Ulsan, Korea..
Kyong Shil Im, Department of Anesthesiology and Pain Medicine, Uijeongbu St Mary's Hospital, College of Medicine, Catholic University of Korea, Seoul, Korea..
Su Bin Yoo, Department of Anesthesiology and Pain Medicine, Uijeongbu St Mary's Hospital, College of Medicine, Catholic University of Korea, Seoul, Korea..
Sung Woo Hyung, Department of Anesthesiology and Pain Medicine, Uijeongbu St Mary's Hospital, College of Medicine, Catholic University of Korea, Seoul, Korea..
References:
- 1. Kwon YS, Jung DY, Lee SH, Ahn JW, Roh HJ, Im KS. Transient occlusion of uterine arteries with endoscopic vascular clip preceding laparoscopic myomectomy. J Laparoendosc Adv Surg Tech A. 2013;23(8):679–683. [DOI] [PubMed] [Google Scholar]
- 2. Kwon YS, Roh HJ, Ahn JW, Lee SH, Im KS. Laparoscopic adenomyomectomy under transient occlusion of uterine arteries with an endoscopic vascular clip. J Laparoendosc Adv Surg Tech A. 2013;23(10):866–870. [DOI] [PubMed] [Google Scholar]
- 3. Kwon YS, Roh HJ, Ahn JW, Lee SH, Im KS. Conservative adenomyomectomy with transient occlusion of uterine arteries for diffuse uterine adenomyosis. J Obstet Gynaecol Res. 2015;41(6):938–945. [DOI] [PubMed] [Google Scholar]
- 4. Kwon YS, Roh HJ, Ahn JW, Lee SH, Im KS. Transient occlusion of uterine arteries in laparoscopic uterine surgery. JSLS. 2015;19:e2014.00189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hung TH, Jeng CJ, Yang YC, Wang KG, Lan CC. Treatment of cervical pregnancy with methotrexate. Int J Gynaecol Obstet. 1996;53(3):243–247. [DOI] [PubMed] [Google Scholar]
- 6. Jeng CJ, Ko ML, Shen J. Transvaginal ultrasound-guided treatment of cervical pregnancy. Obstet Gynecol. 2007;109(5):1076–1082. [DOI] [PubMed] [Google Scholar]
- 7. Ko HK, Shin JH, Ko GY, Gwon DI, et al. Efficacy of Prophylactic Uterine Artery Embolization before Obstetrical Procedures with High Risk for Massive Bleeding. Korean J Radiol. 2017;18(2):355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mesogitis S, Pilalis A, Daskalakis G, Papantoniou N, Antsaklis A. Management of early viable cervical pregnancy. BJOG. 2005;112(4):409–411. [DOI] [PubMed] [Google Scholar]
- 9. Topsoee MF, Settnes A, Ottesen B, Bergholt T. A systematic review and meta-analysis of the effect of prophylactic tranexamic acid treatment in major benign uterine surgery. Int J Gynaecol Obstet. 2017;136(2):120–127. [DOI] [PubMed] [Google Scholar]
- 10. Ugur M, Yesilyurt H, Soysal S, Gokmen O. Prophylactic vasopressin during laparoscopic salpingotomy for ectopic pregnancy. J Am Assoc Gynecol Laparosc. 1996;3(3):365–368. [DOI] [PubMed] [Google Scholar]
- 11. Conforti A, Mollo A, Alviggi C, et al. Techniques to reduce blood loss during open myomectomy: a qualitative review of literature. Eur J Obstet Gynecol Reprod Biol. 2015;192:90–95. [DOI] [PubMed] [Google Scholar]
- 12. Helal AS, Abdel-Hady el-S, Refaie E, El Shamy M, El Fattah RA, Mashaly Ael M. Preliminary uterine artery ligation versus pericervical mechanical tourniquet in reducing hemorrhage during abdominal myomectomy. Int J Gynaecol Obstet. 2010;108(3):233–235. [DOI] [PubMed] [Google Scholar]