Abstract
The Hawai‘i Patient Reward And Incentives to Support Empowerment (HI-PRAISE) project, part of the Medicaid Incentives for Prevention of Chronic Diseases program of the Affordable Care Act, examined the impact of financial incentives on Medicaid beneficiaries with diabetes. It included an observational pre-post study which was conducted at nine Federally Qualified Health Centers (FQHCs) between 2013 to 2015. The observational study enrolled 2,003 participants. Participants could earn up to $320/year in financial incentives. Primary outcomes were change in hemoglobin A1c, blood pressure, and cholesterol; secondary outcomes included compliance with American Diabetes Association (ADA) standards of diabetes care and cost effectiveness. Generalized estimating equation models were used to assess differences in clinical outcomes and general linear models were utilized to estimate the medical costs per patient/day. Changes in clinical outcomes in the observational study were statistically significant: mean hemoglobin A1c decreased from 8.56% to 8.24% (P < .0001); mean systolic blood pressure decreased from 125.16 to 124.18 mm Hg (P = .0137); mean diastolic blood pressure decreased from 75.54 to 74.78 mm Hg (P = .0005); total cholesterol decreased from 180.77 to 174.21 mg/dl (P < .0001); and low-density lipoprotein decreased from 106.17 to 98.55 mg/dl (P < .0001). Improved ADA compliance was also observed. A key limitation was a reduced sample size due to participant's fluctuating Medicaid eligibility status. HI-PRAISE showed no reduction in total health cost during the project period.
Keywords: Health incentives, behavioral economics, Medicaid, Diabetes, Financial Analysis, Pacific Islander
Introduction
Diabetes is a complex chronic disease, with worldwide prevalence approaching 400 million people. 1 Diabetes is the seventh leading cause of death in the United States (US). The National Diabetes Statistics Report estimated that 9.4% of the US adult population had diabetes in 2015; with 23.1 million diagnosed and 7.2 million undiagnosed.2 The total estimated cost of diagnosed diabetes in 2017 was $327 billion in the US.3 In Hawai‘i, the prevalence rate of diabetes increased from 8.4% in 2011 to 9.7% in 2014. In addition, people with pre-diabetes increased dramatically from 9.6% to 14.4% between 2011 and 2014 in Hawai‘i based on the Behavioral Risk Factor Surveillance System (BRFSS) reports.4
Research has shown that low-income populations are disproportionately affected by diabetes.5 A secondary data analysis of Hawai‘i BRFSS survey data from 2013 to 2015 indicated that the odds of diabetes is significantly higher among the Hawai‘i Medicaid population compared to their non-Medicaid counterparts (AOR = 1.75, 95% CI: 1.33 –2.31).6 Medicaid, as the largest payer of health insurance for low-income populations, and plays an important role in financial support for diabetes care. In 2014, the Patient Protection and Affordable Care Act (ACA) allowed states to expand Medicaid eligibility. Section 4108 of ACA authorized five-year grants to States to provide incentives to Medicaid beneficiaries of all ages who participate in prevention programs and demonstrate changes in health risk and outcomes, including the adoption of healthy behaviors.7
The overall objective of Hawaii's Medicaid Incentives for Prevention of Chronic Diseases (MIPCD) grant, Hawai‘i Patient Reward And Incentives to Support Empowerment (HI-PRAISE) project was to examine the impact of incentives on diabetes management among adult Medicaid beneficiaries diagnosed with diabetes. Evaluation measures included: (1) clinical outcomes; (2) compliance with American Diabetes Association (ADA) standards of medical care in diabetes;8 and (3) cost effectiveness.
Methods
Design
A pre-post, observational study with 2,003 participants was conducted at nine federally qualified health centers (FQHCs) in Hawai‘i from February 2013 to December 2015. A randomized controlled trial (RCT) with 320 participants was also conducted at Kaiser Permanente Hawai‘i from May 2014 to December 2015. For the cost analysis, a randomly selected comparison group (N=2,719) of Medicaid adults with diabetes was obtained through the Hawai‘i Department of Human Services (DHS). Institutional Review Board approval was obtained from the University of Hawai‘i, one FQHC, and Kaiser Permanente Hawai‘i.
Setting and Participants
Eligible participants for the observational study were established adult patients from the FQHCs who were Medicaid beneficiaries with a known diagnosis of Type 1 or Type 2 diabetes. Excluded were the pediatric population and women with gestational diabetes. Nine of 14 FQHCs in Hawai‘i participated in the HI-PRAISE project, with 2,003 participants recruited from a projected 2,848 eligible patients (Figure 1). Recruitment strategies included: informational flyers and posters, and direct invitation by FQHC clinicians and community health workers. Participants were required to sign an informed consent form. All participants were followed for at least 12 months.
Figure 1.
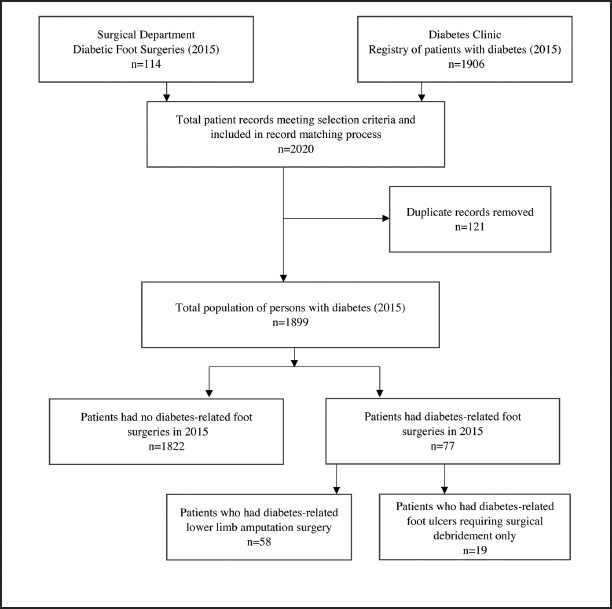
Observational Study Flow Diagram.
*FQHCs = Federally Qualified Health Centers. **COFA = The Compact of Free Association, which is an international agreement establishing and governing the relationships of free association between the United States and the three Pacific Island nations of the Federated States of Micronesia, the Marshall Islands, and Palau. The state of Hawai‘i terminated Medicaid and directed COFA migrants to the Connector, effective March 1, 2015.
The RCT target population were adults enrolled in Kaiser Permanente Quest Integration and receiving care coordination services or usual care for diabetes, from which 320 (159 intervention/161 control) participants were recruited. More details on the methodology and results of the RCT study have been published earlier,9 and are not reported in this article.
Supplemental service payments were provided to all participating sites for efforts in: recruitment, enrollment, goal setting, health coaching, incentive distribution, and data collection. Each participating site received $283 per participant/per year for the completion of these tasks. HI-PRAISE distributed a total of $1,305,599 in supplemental services to the nine FQHCs. Health coaches at the FQHCs comprised of a diverse group of staff ranging from medical assistants, community health workers, nutritionists, to pharmacists.
Intervention
Process and clinical outcome measures for diabetes were incentivized using a tiered approach. Table 1 lists the guidelines for incentives provided to improve diabetes self-management, compliance with ADA standards of diabetes care, clinical outcomes, and promotion of a healthy lifestyle. The financial levels of the incentives were based on Healthcare Effectiveness Data and Information Set (HEDIS) measures, with higher dollar amounts allocated to harder to achieve outcomes. Each site had the liberty to choose the type of incentive for their participants. However all sites were restricted to a total dollar amount for each behavior. Participants could earn up to a maximum of $320/year, if eligible, from enrollment through December 2015. The maximum amount that could be earned during the entire course of the study between 2013 and 2015 was $960. In determining what type of incentives work best with participants, HI-PRAISE considered the unique cultural, racial, and linguistic characteristics of the FQHCs' patients. Each FQHC determined the optimal types of incentives that would motivate and meet the needs of their patients through focus groups which allowed participants to choose their desired incentive. Preferences included gift cards/certificates to grocery stores, pharmacies, gas stations, or retail stores. Less common forms of incentives were vouchers for farmer's markets, massages, or healthy food. Participants would receive the earned incentives once incentivized outcomes were achieved. A satisfaction survey was administered annually during the study to ensure participants were receiving and appropriately utilizing the incentives distributed to them. Ninety-two percent of the survey respondents indicated they had used all the incentives, while 7% had used part of the incentives. Sixty-one percent used the incentives on themselves, 20% has used it for their families, and 17% used it for both themselves and their families, and 2% used it as presents. The health coaches at the FQHC described the incentivized outcomes achieved and distributed the earned incentives to the participants. In addition, the HI-PRAISE project tracked all incentives earned and paid, and notified sites monthly when a participant had earned an incentive.
Table 1.
HI-PRAISE Incentives Schedule.
| Variables | Incentive ($) |
| Improve Self-Management of Diabetes | |
| Blood glucose monitoring | ≤ $20 |
| Attend 1st session of diabetes education | ≤ $20 |
| Improve Compliance with ADA Recommended Preventative Measures | |
| Pneumococcal or Influenza vaccination | ≤ $10 |
| Improve Compliance with ADA Recommended Treatment and Management | |
| Retinal eye exam | ≤ $20 |
| Urine for Microalbumin test | ≤ $10 |
| LDL Cholesterol test | ≤ $20 |
| HbA1c test | ≤ $20 |
| Improvement in Clinical Outcomes of Diabetes | |
| HbA1c decrease of 1% | ≤ $20 |
| HbA1c goal of < 7% | ≤ $50 |
| Blood pressure goal of < 140/90 mm Hg | ≤ $20 |
| LDL Cholesterol goal of < 100 mg/dl | ≤ $20 |
| Eliminate Barriers to a Healthy Lifestyle (if applicable) | |
| Attend smoking cessation group or individual class | ≤ $20 |
| Attend counseling for behavioral health | ≤ $20 |
| Weight loss of 7% in one year | ≤ $50 |
| Maximum Total Direct Incentives | $320 |
ADA = American Diabetes Association, LDL = Low-density Lipoprotein, HbA1c = Glycated Hemoglobin.
HI-PRAISE project distributed $339,667 to participants from the FQHCs. The average amount of money earned in incentives was $180, and the average number of incentives earned over the course of the study was nine. The most commonly earned incentives included: completion of glycated hemoglobin (HbA1c) testing, cholesterol testing, and blood pressure at goal. The highest incentive amount distributed to a single participant over the course of the study was $785 and the lowest amount was $0, meaning that some participants (n = 135) did not receive a single incentive.
Measures
A Minimum Data Set (MDS) was developed for measuring and reporting outcomes across the MIPCD grantees that included five common domains: enrollment, demographics, services, incentives, and clinical outcomes. Demographic variables included: age, sex, education, race, ethnicity, Compact of Free Association (COFA) status, insurance, Medicare status, and housing arrangements; as well as history of hypertension, heart disease, and smoking. Additionally, participation in diabetes education sessions, and type and amount of incentives distributed were tracked. Clinical outcomes collected included: weight, height, body mass index, blood pressure, fasting blood glucose, HbA1c, fasting lipid profile, renal function, smoking cessation, retinopathy, and influenza/pneumococcal vaccination status.
Statistical Analysis
Data were analyzed using Statistical Analysis System (SAS) 9.4 (SAS Institute Inc., Cary, North Carolina). Summary statistics and frequency distributions were used to describe the characteristics of the study participants. Generalized estimating equation (GEE) models were used to assess the pre-post differences in FQHC participants. Likelihood ratio tests were used to choose the variance-covariance structure for the observational study. Linear contrasts were used to examine the longitudinal changes in clinical outcomes for all participants. Estimated coefficients and corresponding 95% confidence intervals from linear contrasts were used to quantify the differences in the GEE models. The estimated differences in clinical outcomes were adjusted for age, sex, and race.
For cost analysis, expenses related to outpatient, inpatient, emergency room, skilled nursing, hospice, prescription drugs, and dental care were included. The summarized costs per patient/day were first log transformed to meet the assumption of normality in general linear models (GLM). GLM models with group, time, and interaction between group and time were used to estimate the cost difference between groups after adjusting for age, gender, race, Medicare status, and COFA status. The estimated coefficients and standard errors for the interaction term (difference-in-differences) in the GLM were utilized to estimate the causal effect of the intervention on medical costs per patient/day and the cost effectiveness ratio was calculated.10
Results
The mean age of participants was 54.1 years with more females (59.8%) than males (40.2%) (Table 2). The largest racial group was Native Hawaiian and Other Pacific Islander (NH/OPI 44.1%) followed by Asian (17.9%). Participants with COFA status was 37.5%. Twenty-three percent received both Medicare and Medicaid benefits. Participants had other comorbidities in addition to diabetes such as hypertension (64.4%), heart disease (15.7%) and history of smoking or tobacco dependence (42.5%). A randomly selected unmatched comparison group (N=2,719) of Medicaid adults with diabetes was obtained through DHS to enable the cost effectiveness analysis. As indicated in Table 2, the comparison group differed from the FQHC group in race, for which the majority race was Asian (39.1% vs 17.9%, P < .001). The comparison group also had a greater number of dual eligible (37% vs 22.6%, P < .001) and fewer number of COFA migrants (8% vs 37.5%, P < .001). History of comorbidities were unavailable.
Table 2.
Characteristics of the Study Sample.
| Characteristic | Observational Study n = 2003 | Observational Study Comparison n = 2719 |
| Sex | ||
| Female | 1197 (59.8%) | 1479 (54.4%) |
| Male | 806 (40.2%) | 1240 (45.6%) |
| Race | ||
| White | 164 (8.2%) | 375 (13.8%) |
| Black | 10 (0.5%) | 44 (1.6%) |
| American Indian or Alaska Native | 3 (0.1%) | 7 (0.3%) |
| Asian | 359 (17.9%) | 1062 (39.1%) |
| Native Hawaiian and Other Pacific Islander | 884 (44.1%) | 792 (29.1%) |
| Other Race(s) | 167 (8.3%) | 245 (9.0%) |
| Multiple Races | N/A | N/A |
| Missing/Unknown | 416 (20.8%) | 194 (7.1%) |
| Ethnicity | ||
| Hispanic or Latino | 67 (3.3%) | N/A |
| Missing/Unknown | 39 (1.9%) | N/A |
| COFA Individuals | 752 (37.5%) | 209 (8.0%) |
| Dual-Eligible (Medicaid/Medicare) | 454 (22.6%) | 1071 (37%) |
| Mean Age in Years (SD) | 54.1 (12.4) | 58.3 (16.1) |
| Age | ||
| 18–19 | 3 (0.1%) | 0 (0%) |
| 20–29 | 68 (3.3%) | 119 (4.4%) |
| 30–39 | 201(10.0%) | 241 (8.9%) |
| 40–49 | 416 (20.8%) | 408 (15.0%) |
| 50–59 | 669 (33.4%) | 702 (25.8%) |
| 60–69 | 467 (23.3%) | 574 (21.1%) |
| 70+ | 182 (9.1%) | 675 (24.8%) |
| History of Hypertension | 1290 (64.4%) | N/A |
| History of Heart Disease | 314 (15.7%) | N/A |
| History of Smoking or Tobacco Dependence | 851 (42.5%) | N/A |
Participants showed small but statistically significant improvements in clinical measures from baseline to the end of the study (Table 3). The mean HbA1c decreased from 8.56% to 8.24% (P < .001). The mean systolic blood pressure decreased from 125.16 mm Hg to 124.18 mm Hg (P = .0137) and the mean diastolic blood pressure decreased from 75.54 mm Hg to 74.78 mm Hg (P < .001). Mean total cholesterol also decreased from 180.77 mg/dl to 174.21 mg/dl (P < .0001) and the LDL decreased from 106.17 mg/dl to 98.55 mg/dl (P < .0001). Additionally, sub-group analysis was conducted for each FQHC to assess the changes in key outcome measures. Five of the nine FQHCs showed significant improvements among their participants in the mean level of HbA1c from baseline to the end of the study, three FQHCs had no statistically significant changes and one FQHC had too few participants to conduct the analysis (Table 4). The mean HbA1c decreased from 8.51% to 7.84% (P < .0001) among participants at Health Center A; 8.49% to 7.90% (P < .001) at Health Center B; 8.87% to 8.36% (P < .0001) at Health Center C; 8.75% to 8.43% (P < .0001) at Health Center D, and 8.04% to 7.74% (P = .0046) at Health Center E.
Table 3.
Changes in Clinical Measures.
| Variables | Baseline | End of Study | Difference | 95% CI | P-value* | |
| HbA1c (%) | 8.56 | 8.24 | −0.32 | −0.41 | −0.25 | <.001 |
| SBP (mm Hg) | 125.16 | 124.18 | −0.98 | −1.76 | −0.20 | .0137 |
| DBP (mm Hg) | 75.54 | 74.78 | −0.76 | −1.20 | −0.33 | <.001 |
| Total Cholesterol (mg/dl) | 180.77 | 174.21 | −6.56 | −8.80 | −4.32 | <.001 |
| Triglycerides (mg/dl) | 179.73 | 176.31 | −3.42 | −12.47 | 5.63 | .4586 |
| LDL (mg/dl) | 106.17 | 98.55 | −7.62 | −9.34 | −5.89 | <.001 |
| HDL (mg/dl) | 43.50 | 43.59 | 0.09 | −0.52 | 0.71 | .7650 |
Analysis was adjusted for age, sex, and race
Table 4.
Glycemic Control by FQHC.
| n | Baseline | End of Study | Difference | 95% CI | P-value * | ||
| FQHC A | 157 | 8.51 | 7.84 | −0.67 | −1.00 | −0.34 | <.001 |
| FQHC B | 198 | 8.49 | 7.90 | −0.59 | −0.83 | −0.34 | <.001 |
| FQHC C | 230 | 8.87 | 8.36 | −0.51 | −0.75 | −0.27 | <.001 |
| FQHC D | 711 | 8.75 | 8.43 | −0.32 | −0.46 | −0.18 | <.001 |
| FQHC E | 142 | 8.04 | 7.74 | −0.30 | −0.52 | −0.09 | .0046 |
| FQHC F | 440 | 8.79 | 8.65 | −0.14 | −0.30 | 0.01 | .0700 |
| FQHC G | 37 | 8.81 | 9.25 | 0.45 | −0.24 | 1.13 | .2014 |
| FQHC H | 70 | 8.67 | 8.54 | −0.13 | −0.50 | 0.24 | .4915 |
| FQHC I | 5 | - | - | - | - | - | - |
Compliance with ADA standards of medical care in diabetes improved at the FQHCs over the study period from 2013 to 2015. Percentage of annual eye exams increased from 38.7% to 46.9%. Screening for diabetes nephropathy through urine testing for microalbumin increased from 38.6% to 50%. Attendance of diabetes education sessions increased from 16.8% to 41.6%. Testing for HbA1c and lipids increased from 54.3% to 77.1% and 45.6% to 62.6% respectively.
For the cost analysis, the outcomes reflected both the amount billed and paid. The coefficient for the interaction between group and time in Table 5 was the difference-in-differences estimate. Adjusting for Medicare eligibility, sex, and race, the amount billed and paid increased in the observational study by 60.0% and 61.9%, respectively. Using the baseline estimates of amounts billed and paid of $21.02 and $8.54, the intervention increased costs by $12.54 and $5.29, respectively. The total cost for the capital outlay was $1.41 per patient/day, which included variable costs of personnel, incentives, health coaches, diabetes education, transportation, air travel, training, and fixed costs of capital equipment.
Table 5.
Impact of Intervention on Mean Charges Billed and Amount Paid Per Day.
| Variable | Unadjusted | Adjusted for Gender/Age | Adjusted for Gender/Age/Medicare/COFA/Pacific Islanders | Adjusted for Gender only Males | Adjusted for Gender only Females |
| Mean Charges per day Billed Pre-Intervention at FQHC = $21.02 | |||||
| Diffs-in-Diffs Estimate in log scale (SE) |
0.636 (0.062) |
0.606 (0.060) |
0.600 (0.059) |
0.611 (0.095) |
0.606 (0.076) |
| Total Billed Increase ($)* | $13.37 | $12.74 | $12.61 | $12.84 | $12.74 |
| Mean Amount Paid per day Pre-Intervention at FQHC = $8.54 | |||||
| Diffs-in-Diffs Estimate in log scale (SE) |
0.630 (0.064) |
0.606 (0.062) |
0.619 (0.061) |
0.595 (0.097) |
0.617 (0.081) |
| Total Paid Increase ($)* | $5.38 | $5.18 | $5.29 | $5.08 | $5.27 |
The Total Billed (or Paid) Increase is the Diffs-in-Diffs estimate times the pre-intervention mean billed (or paid) per day.
Discussion
Prior to the ACA, several Medicaid programs implemented beneficiary incentive programs in an attempt to engage Americans in healthty behaviors and emphasize the importance of personal choices in determining health. Some of these programs such as Idaho's Preventative Health Assistance and Indiana's Healthy Indiana Plan are still operating. Pre-ACA Medicaid beneficiary incentives programs achieved mixed results, and some have faced skepticism from the health policy community.11 There are numerous studies in general populations evaluating the impact of financial incentives on preventive health behaviors such as smoking cessation and weight loss.12–18 These studies too have shown great variation in results of the effectiveness of incentives, however one common theme is that incentives that target processes (eg, going to the gym, getting a test, etc) have generally yielded better results than those incentives that target outcomes (eg, weight loss, drug adherence, etc).17–18 HI-PRAISE hypothesis was to employ an incentive strategy where process incentives would act as the mechanism to get patients into the clinic where health care providers and further outcome incentives would help patients improve their health outcomes. HI-PRAISE is the first study of its kind to conduct behavioral economic research in a community setting serving racial/ethnic minorities and medically underserved individuals, who were engaged through focus groups in determining the type of financial incentives which would most appeal to participants.12–18 The project showed statistical improvements in key clinical outcomes of HbA1c, blood pressure, and cholesterol along with increased patients' compliance with ADA standards of diabetes care in the observational study. Improvements in health outcomes varied by FQHCs with five of the eight facilities having achieved better outcomes in lowering A1c. However, these improvements in clinical outcomes were small and not clinically meaningful in the improvement of glycemic control or reduction of cardiovascular risk. HI-PRAISE was also strengthened by conducting cost analysis to assess the impact of incentives on health care cost. Successes and limitations in the designs and implementations of the project will be discussed.
The HI-PRAISE project did not show reduction in health cost at the end of the study. The observational study found that the intervention, contrary to expectations, raised costs. One limitation with a randomly selected comparison group (N=2,719) of Medicaid adults with diabetes obtained through DHS was the lack of access to baseline biometric outcomes to conduct matching. However, the DHS Medicaid beneficiary database is the only source that could provide a sufficiently large sample with a majority of adults who utilize the FQHCs and are thus comparable. Incentives by design increased contact with the medical system and physician induced demand.19 By increasing contact with medical professionals, this may have led to additional tests and procedures performed leading to improved ADA compliance and increased costs. However, over time there may be a decrease in the number of services necessary after initial contact and acute health concerns are resolved, or chronic disease management is improved. HI-PRAISE project included the cost effectiveness analysis component in the study but further analysis beyond the study period is necessary to demonstrate long-term effect.
The Oregon Health Study showed a similar increase in utilization of health care services in Medicaid populations with no significant improvements in physical health outcomes.20,21 The expansion of public health insurance, while improving access to care, did not improve clinical outcomes. Moral hazard in health insurance is the notion that medical insurance increases the demand for medical care.22 It is now known to specifically refer to the price sensitivity of demand for health care, conditional on underlying health status.23 According to the RAND Health Insurance Experiment, economists accept that traditional health insurance leads to moderate moral hazard in demand.24 In HI-PRAISE, the increases in utilization of health care services may be attributed to both a moral hazard on the part of the consumers and an enhanced awareness among the providers to incentivize diabetes care.
Bazerman, et al, refer to the common struggle between choosing what we desire in the heat of the moment versus choosing what would be best for us in the long run as “want/should conflict.”25 Potential behavioral economics solutions to consider pairing with financial incentives include prompting personal planning, commitment devices, and temptation bundling.26 Policy makers may be able to utilize behavioral interventions to “nudge” individuals towards should behaviors without restricting choices.27 The increases in the compliance rates of the ADA standards of care for diabetes along with lack of clinically meaningful improvements in outcomes in the observational study illustrate the challenge in defining optimal policy for chronic disease management. Paying low-income participants may incrementally improve compliance with standards of care when those rates are low, but financial incentives will also increase the costs for drugs and ambulatory visits, with an unclear long-term impact on health outcomes as well as hospitalizations and emergency room visits. Improving health requires reducing old unhealthy habits and building new healthy habits, which seems to be beyond the capacity of financial incentives alone.
A key limitation of HI-PRAISE was the eligibility status of Medicaid beneficiaries which impacted the sample size and led to smaller number of data points analyzed. COFA migrants lost Medicaid eligibility March 1, 2015 because of a policy change at the State level which reduced the FQHCs sample size by 38%. The HI-PRAISE project faced delays establishing fully executed contracts with the DHS and FQHCs which stalled the recruitment and enrollment process of the study. The FQHCs were not amenable to a study design that would exclude eligible participants from receiving incentives due to the community-based nature of health centers; hence the feasibility of a pre-post study design with the acceptance that it was not as robust as a RCT design.
The HI-PRAISE project considered the issue of sustainability by incorporating incentive distribution as part of staff's daily responsibilities. The project was conducted in the usual care setting, without study visits for data collection leading to a high number of missing orders and test results. Competing priorities such as Patient-Centered Medical Home (PCMH) certification and the roll out of electronic health records limited the ability of FQHC staff to fully engage in HI-PRAISE. High staff turnover at the FQHCs demanded ongoing training in project management including incentive distribution. Change and verification of Medicaid eligibility status, and safety and liability concerns at the FQHCs resulted in delays in the timely distribution of incentives. Thus, the pairing of incentives with positive behaviors may not have been as clear as intended. In addition, the variability among the incentives distributed at the FQHCs was also a limitation.
Diabetes education programs and PCMH model will continue at the FQHCs. Three FQHCs became ADA certified with support from HI-PRAISE. Further long-term studies with larger sample sizes are needed to better assess the impact of financial incentives on clinical outcomes of diabetes and associated costs.
Acknowledgements
The project described was supported by Grant Number 1B1CMS330884 from the Department of Health and Human Services (DHHS), Centers for Medicare & Medicaid Services (CMS). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of DHHS or any of its agencies. The research presented here was conducted by the awardee. Findings might or might not be consistent with or confirmed by the findings of the independent evaluation contractor. We are grateful to the patients of the FQHCs and Kaiser Permanente Hawai‘i for their participation. Many thanks to the executive team, management team, research team and health coaches and the HI-PRAISE team. We wish to acknowledge the support received from State of Hawai‘i Department of Human Services, IMPAQ, RTI, Econometrica, and CMS.
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Nathan DM. Diabetes: Advances in Diagnosis and Treatment. JAMA. 2015;314(10):1052–1062. doi: 10.1001/jama.2015.9536. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC), author National Diabetes Statistics Report: Estimates of diabetes and its burden in the United States, 2017. Atlanta, GA: US Department of Health and Human Services; 2017. [July 28, 2017]. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. [Google Scholar]
- 3.American Diabetes Association, author. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928. doi: 10.2337/dci18-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawaii Health Data Warehouse, author. Diabetes prevalence rate for the state of Hawaii for years 2011 to 2014. [March 1, 2018]. http://hhdw.org/health-reports-data/category/chronic-diseases/diabetes/#individual-year.
- 5.Volaco A, Cavalcanti AM, Filho RP, Precoma DB. Socioeconomic status: the missing link between obesity and diabetes mellitus? Curr Diabetes Rev. 2017 Jul 21; doi: 10.2174/1573399813666170621123227. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Li D, Chinn CC, Fernandes R, Wang CM, Smith MD, Ozaki RR. Risk of diabetes mellitus among Medicaid beneficiaries in Hawaii. Prev Chronic Dis. 2017;14:E116. doi: 10.5888/pcd14.170095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid Services (CMS), author Medicaid Incentives for the Prevention of Chronic Disease Model. [October 29, 2016]. https://innovation.cms.gov/initiatives/mipcd.
- 8.American Diabetes Association, author. Standards of medical care in diabetes - 2012. Diabetes Care. 2012;35 Suppl 1:S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernandes R, Chinn CC, Li D, Frankland TB, Wang CM, Smith MD, Ozaki RR. A Randomized Controlled Trial of Financial Incentives for Medicaid Beneficiaries with Diabetes. The Permanente Journal. 2018;22:17-080. doi: 10.7812/TPP/17-080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th edition. Publisher: Oxford University Press; 2015. [Google Scholar]
- 11.Blumenthal KJ, Saulsgiver SA, Norton L, et al. Medicaid incentive programs to encourage healthy behavior show mixed results to date and should be studied and improved. Health Aff. 2013;32(3):497–507. doi: 10.1377/hlthaff.2012.0431. [DOI] [PubMed] [Google Scholar]
- 12.Volpp KG, Troxel AB, Pauly MV, et al. A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360:699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 13.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss, a randomized controlled trial. JAMA. 2008;300(22):2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kullgren JT, Troxel AB, Loewenstein G, et al. Individual-versus group-based financial incentives for weight loss, a randomized, controlled trial. Ann Intern Med. 2013;158(7):505–514. doi: 10.7326/0003-4819-158-7-201304020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kendzor DE, Businelle MS, Poonawala IB, et al. Financial incentives for abstinence among socioeconomically disadvantaged individuals in smoking cessation treatment. Am J Public Health. 2015;105(6):1198–1205. doi: 10.2105/AJPH.2014.302102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeFulio A, Silverman K. The use of incentives to reinforce medication adherence. Prev Med. 2012;55(Suppl):S86–S94. doi: 10.1016/j.ypmed.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kane RL, Johnson PE, Town RJ, Butler M. A structured review of the effect of economic incentives on consumers' preventive behavior. Am J Prev Med. 2004;27(4):327–352. doi: 10.1016/j.amepre.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Strohacker K, Galarraga O, Williams DM. The Impact of Incentives on Exercise Behavior: A Systematic Review of Randomized Controlled Trials. Ann Behav Med. 2014;48(1):92–99. doi: 10.1007/s12160-013-9577-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fuchs VR. Physician-induced demand: A parable. J Health Econ. 1986;5(4):367–368. doi: 10.1016/0167-6296(86)90006-8. [DOI] [PubMed] [Google Scholar]
- 20.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment - effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finkelstein AN, Taubman SL, Allen HL, Wright BJ, Baicker K. Effects of Medicaid coverage on ED use - Further evidence from Oregon's experiment. N Engl J Med. 2016;375(16):1505–1507. doi: 10.1056/NEJMp1609533. [DOI] [PubMed] [Google Scholar]
- 22.Arrow K. Uncertainty and the welfare economics of medical care. Am Econ Rev. 1963;53(5):941–973. [Google Scholar]
- 23.Pauly MV. The economics of moral hazard: comment. Am Econ Rev. 1968;58(3):531–537. [Google Scholar]
- 24.Aron-Dine A, Einav L, Finkelstein A. The RAND health insurance experiment, three decades later. J Econ Perspect. 2013;27(1):197–222. doi: 10.1257/jep.27.1.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bazerman MH, Tenbrunsel AE, Wade-Benzoni K. Negotiating with yourself and losing: Making decisions with competing internal preferences. Acad Manage Rev. 1998;23(2):225–241. [Google Scholar]
- 26.Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth, and happiness. New Haven, CT: Yale University Press; 2008. [Google Scholar]
- 27.Bitterly B, Mislavsky R, Dai H, Milkman KL. The Psychology of Desire. New York, NY: Guilford Press; 2015. Want-Should Conflict: A Synthesis of Past Research. [Google Scholar]


