ABSTRACT
Widespread use of anticoagulant drugs for treatment and prevention of thromboembolic events means it is common to encounter patients requiring reversal of anticoagulation for management of bleeding or invasive procedures. While supportive and general measures apply for patients on all agents, recent diversification in the number of licensed agents makes an understanding of drug-specific reversal strategies essential. Recognising effects upon, and limitations of, laboratory measures of coagulation also plays an important role. An understanding of reversal strategies alone is insufficient to competently care for patients who may require anticoagulation reversal. It is also necessary to reduce the need for reversal through correct prescribing and by employing appropriate periprocedural bridging strategies for elective and semi-elective procedures. Finally, consideration of whether and when to reintroduce an anticoagulant drug following reversal is important not only to balance bleeding and thrombotic risks for individual patients but also for timely management of discharge.
KEYWORDS: anticoagulants, direct acting oral anticoagulants, reversal, haemorrhage, surgery
Key points
The type of anticoagulant, dose, timing of last dose and indication are significant points to establish when making decisions about anticoagulation reversal
For elective procedures and surgery, the need for anticoagulation reversal should be avoided by determining whether cessation of anticoagulant is required, and by following local bridging protocols
In patients bleeding while on anticoagulants, supportive treatment including blood components and local measures should be employed alongside the steps taken to reverse the anticoagulant effect
INR and APTT can be used to assess anticoagulant activity of vitamin K antagonists and unfractionated heparin respectively, but therapeutic ranges for these drugs cannot be used to interpret clotting tests in patients on other anticoagulants
Specific reversal agents exist for vitamin K antagonists (vitamin K and prothrombin complex concentrate), heparins (protamine sulphate) and dabigatran (Idarucizumab) but there is currently no specific reversal agent for fondaparinux or for the oral factor Xa inhibitors
Introduction
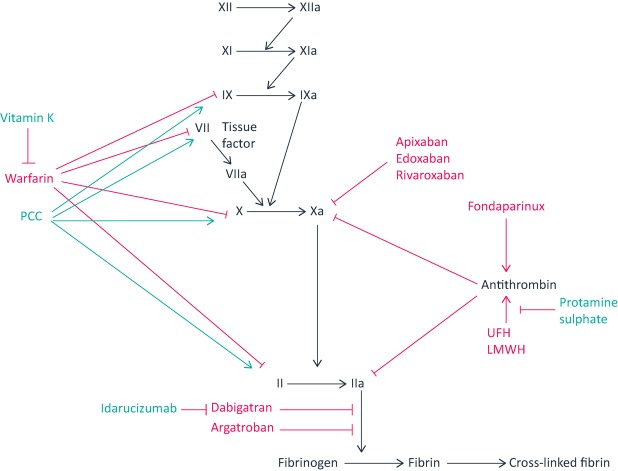
Since the earliest clinical investigation of heparin in the 1930s,1 the indications for anticoagulant drugs and the number of commonly encountered agents has increased (Table 1). These drugs act by inhibiting different stages of the coagulation cascade that culminates in the formation of cross-linked fibrin (Fig 1). It is common in clinical practice to encounter patients requiring anticoagulation reversal. Indications for anticoagulation reversal include:
bleeding
elective or emergency invasive procedures or surgery
over-anticoagulation, due to accidental or intentional overdose, drug interactions or reduced excretion.
Table 1.
Key pharmacokinetic features of common anticoagulant drugs
| Name | Excretion | Plasma half-life |
|---|---|---|
| Warfarin | Hepatic metabolism to inactive metabolites excreted in urine | Effective half-life 40 h |
| UFH | Rapid endothelial cell internalisation (saturateable), slower renal clearance | 45–90 min |
| LMWH | Predominantly renal | 4 h |
| Fondaparinux | 70% renal | 17–21 h |
| Argatroban | Hepatic | 45 min |
| Dabigatran | 80% renal | 13 h |
| Apixaban | 25% renal, 75% hepatic | 12 h |
| Edoxaban | 35% renal, 65% hepatic | 10–14 h |
| Rivaroxaban | 25% renal, 75% hepatic | 5–9 h |
LMWH = low-molecular-weight heparin; UFH = unfractionated heparin
Fig 1.
Representation of stage of action of anticoagulants and their reversal agents on a schematic clotting cascade. This diagram is intended to summarise drug actions but does not reflect the complexity of haemostasis believed to occur physiologically, where cell surface molecules regulate initiation, amplification and propagation of thrombus.31 Please see the main text for details on specific drug and reversal agent mechanisms. PCC = prothrombin complex concentrate; LMWH = low-molecular-weight heparin; UFH = unfractionated heparin; → = promotes; = suppresses
A decision to reverse anticoagulation must weigh the benefits of anticoagulation reversal in terms of stopping bleeding or reduction of bleeding risk against the risk of development or extension of thrombosis while anticoagulation is reversed. This can be particularly challenging in situations such as bleeding in patients with mechanical heart valves.
This article will focus on urgent reversal of anticoagulation. It is important that care of patients on anticoagulant drugs is optimised so that the need for urgent reversal is minimised. The benefits should be weighed against a patient's individual bleeding risk when deciding to anticoagulate and in choice of anticoagulant, and factors including potential drug–drug interactions and the need for dose reduction considered.2 Anti-platelet agents should be discontinued when an anticoagulant is used, except in certain circumstances.3 An anticoagulation plan should be prepared in advance of elective procedures so that urgent reversal is not required. Table 2 summarises the length of time for which different anticoagulants should be stopped prior to an invasive procedure. Some procedures (eg joint injections, endoscopic procedures with a low risk of bleeding and cataract surgery) can be performed without stopping anticoagulants. If anticoagulation is not lifelong, consideration should be given to deferring the procedure until treatment is completed. If anticoagulant treatment must be interrupted, bridging protocols should be employed that take into account drug pharmacokinetics and bleeding and the thrombotic risk.4
Table 2.
Approximate time prior to surgery or invasive procedure for which anticoagulant drug should be stopped. National4 and local guidelines and product literature should be consulted for specific details
| Drug | Duration between stopping and invasive procedure or surgery | Duration before stopping and invasive procedure or surgery in impaired renal function – creatinine clearance <30 | ||
|---|---|---|---|---|
| Low bleeding risk procedure | High bleeding risk procedure | Low bleeding risk procedure | High bleeding risk procedure | |
| Warfarin | 5 days | |||
| UFH | 4 hours | |||
| LMWH | Prophylactic dose, 12 hours | If used, discuss dose and timing with haematology | ||
| Treatment dose, 24 hours | ||||
| Fondaparinux | 24–42 hours | If used, discuss dose and timing with haematology | ||
| Argatroban | 4 hours | |||
| Dabigatran | 24 hours | 48 hours | Cr Cl > 50 to <80: 24–48 hours | Cr Cl > 50 to < 80: 48–72 hours |
| Cr Cl > 30 to <50: 48–72 hours | Cr Cl > 30 to <50: 72–96 hours | |||
| Apixaban | 24 hours | 48 hours | 48 hours | 72 hours |
| Edoxaban | 24 hours | 48 hours | 48 hours | 72 hours |
| Rivaroxaban | 24 hours | 48 hours | 48 hours | 72 hours |
LMWH = low-molecular-weight heparin; UFH = unfractionated heparin
In urgent situations where reversal is required a combination of general measures which apply regardless of which anticoagulant a patient is taking, and drug-specific management is used. Drug specific reversal strategies are summarised in Table 3. General measures include making an assessment of the dose and timing of the drug, considering its rate of elimination, and in the case of bleeding resuscitating the patient and identifying and treating the source of bleeding. The efficacy and evidence base for specific reversal strategies varies between anticoagulants, and an understanding of this, is important when making choices about reversal.
Table 3.
Current drug-specific reversal strategies and novel agents under development
| Drug | Drug-specific reversal strategy | Agents likely to be available in the future |
|---|---|---|
| Vitamin K antagonists | Vitamin K, four-factor PCC | |
| Unfractionated heparin | Protamine sulphate | Ciraparantag |
| Low molecular weight heparin | Protamine sulphate | Andexanet alfa, Ciraparantag |
| Fondaparinux | Consider recombinant activated factor VII | Andexanet alfa, Ciraparantag |
| Dabigatran | Idarucizumab | Ciraparantag |
| Factor Xa inhibitors | Four-factor PCC | Andexanet alfa, Ciraparantag |
PCC = prothrombin complex concentrate
General measures for anticoagulation reversal
Baseline information and investigations
It is important to establish what anticoagulant a patient is taking, the dose, frequency, timing of last dose and indication. The anticoagulant should be stopped. Other drugs that can affect bleeding (eg antiplatelet agents and non-steroidal anti-inflammatory drugs) should also be noted. Blood tests must include a full blood count and clotting screen (prothrombin time [PT], activated partial thromboplastin time [APTT], thrombin time [TT] and fibrinogen). Additional clotting samples for drug-specific tests may be requested, guided by discussion with haematology or the coagulation laboratory. Liver function tests and renal function tests are essential to provide information on drug elimination.
Supportive measures
Bleeding patients should receive appropriate resuscitation and blood-component support, which in the situation of major haemorrhage should follow national guidelines.5
Pharmacological measures
Tranexamic acid 1 g every 8 hours should be considered for patients requiring reversal of anticoagulation. Tranexamic acid is beneficial in patients bleeding following trauma, although these data do not relate specifically to those taking anticoagulants.6 It is reasonable to consider tranexamic acid for patients on anticoagulants with non-traumatic bleeding, provided there are not contraindications. Consideration of tranexamic acid is recommended prior to urgent surgery4 and in adults having surgery who are expected to have moderate blood loss.7
Local measures and intervention
Attempts should be made to identify the site of bleeding and where possible apply local measures to stop it eg pressure, endoscopy, surgery and interventional radiology.
Drug elimination
The extent to which an anticoagulant drug is contributing to bleeding or bleeding risk should be considered. If the timing, excretion route and elimination time (Table 1) suggest the drug has been cleared, specific reversal agents should not be employed. Haemodialysis and haemofiltration have little utility in anticoagulant reversal.
Specific management
Vitamin K antagonists
Vitamin K antagonists exert their anticoagulant effect by inhibiting the vitamin K dependent carboxylation of coagulation factors II, VII, IX and X (Fig 1). In the UK, warfarin is the most commonly prescribed vitamin K antagonist and we will focus on reversal of warfarin in this article. Acenocoumarol and phenindione may be encountered, and urgent reversal of all three agents follows similar principles.8 Where cessation or dose-reduction is insufficient, reversal can be achieved with oral or intravenous vitamin K or by replacement of the affected factors, a choice determined by the desired rapidity and depth of reversal.
In patients with a moderately elevated international normalised ratio (INR) (5–8) without bleeding, reversal is usually achieved by withholding one or two doses of warfarin, followed by dose reduction. INRs above 8 confer a substantially increased bleeding risk so anticoagulation should be reversed with oral vitamin K 1–5 mg. Oral vitamin K could also be considered in INRs of 5–8 when additional bleeding risk factors are present.9
Oral or intravenous vitamin K administration achieves a similar INR after 24 hours, but a more rapid initial effect occurs with the intravenous route, making it preferable in bleeding patients.10 For non-major bleeding, anticoagulation reversal can be managed with 1–3 mg intravenous vitamin K.9
In major bleeding or for emergency procedures which cannot be delayed until vitamin K has taken effect, rapid reversal of warfarin can be achieved using four-factor prothrombin complex concentrates (PCC) at a dose of 25–50 units/kg. These contain factors II, VII, IX and X and the vitamin K dependant anticoagulant proteins protein C and protein S. PCC containing lower levels of factor VII are termed three-factor PCC. They do not produce a good correction of the INR and are not recommended.9 PCC is superior to fresh-frozen plasma in achieving rapid correction of INR in patients with bleeding11 and those requiring urgent warfarin reversal for surgery or procedures.12 5 mg vitamin K should be given concurrently to maintain reversal when factor levels fall. PCCs should be avoided outside emergency situations; they carry risks associated with plasma-derived products (such as viral infection) and are associated with a risk of thrombosis. The limited data on thrombosis suggests the risk is relatively low and it is difficult to distinguish from other patient risk factors.13,14 Nonetheless, caution is advised in patients with recent thrombosis or surgery, cardiovascular disease, or liver disease.
Unfractionated heparin
Unfractionated heparin (UFH) enhances the activity of antithrombin, an endogenous negative regulator of the clotting cascade that inactivates thrombin and factor Xa (Fig 1) as well as factors IXa, XIa, XIIa. UFH has a short half-life (Table 1) so rapid reversal is achievable by stopping the infusion.15 Protamine sulphate is licensed for reversal of UFH, acting by preventing its interaction with antithrombin. Protamine sulphate is given as a slow intravenous bolus at a dose calculated from the number of units of UFH received in the last 2 hours, with 1 mg protamine sulphate neutralising approximately 80–100 units of UFH. In excess, protamine itself acts as an anticoagulant. Protamine is derived from fish sperm and there is a risk of allergic reactions, especially in individuals with previous protamine exposure, fish allergies and following vasectomy.
Low molecular weight heparin
Low-molecular-weight heparins (LMWH) contain shorter polymers than UFH, and their interaction with antithrombin affects Xa more than thrombin.1 Protamine sulphate is less effective at reversing anti-Xa activity than antithrombin activity but is recommended for LMWH reversal based on an absence of alternatives and evidence from animal studies and small retrospective studies.16 Up to 8 hours from LMW heparin administration protamine sulphate 1 mg/100 units can be considered, with a further dose of 0.5 mg/100 units if there is ongoing bleeding. If LMWH was given over 8 hours earlier, lower doses may be used.15
Fondaparinux
Fondaparinux is a synthetic pentasaccharide not a LMWH but is considered here as it is used in similar indications and has a similar mechanism of action, by promoting the interaction of antithrombin and factor Xa (Fig 1). Protamine sulphate has no activity against fondaparinux. Recombinant activated factor VII can be considered for critical bleeding,17 but this is an unlicensed indication.
Direct thrombin antagonists
Dabigatran and argatroban are direct thrombin antagonists. Dabigatran is given as an oral pro-drug dabigatran etexilate. Argatroban is given intravenously, its main use being in heparin-induced thrombocytopaenia. By inhibiting thrombin these drugs reduce the conversion of fibrinogen to fibrin (Fig 1). Argatroban has a short half-life of around 45 minutes – stopping the infusion and initiating general measures should achieve reversal.
There is a licensed antidote, idarucizumab, for rapid reversal of dabigatran for emergency surgery and procedures or in life-threatening or uncontrolled bleeding. It is an engineered antibody fragment that mimics structural features of thrombin to bind dabigatran with high affinity, without binding other thrombin substrates.18 In an open-label study, idarucizumab rapidly and completely reversed laboratory measures of anticoagulation in patients taking dabigatran.19
Factor Xa inhibitors
Rivaroxaban, apixaban and edoxaban act by inhibiting Xa (Fig 1). Minor bleeding should be managed using local measures and delaying the next dose or discontinuing the drug. For more severe bleeding, tranexamic acid and supportive measures should be used but there no licensed reversal agent. For life-threatening bleeding PCC may be considered;17 however, this is an unlicensed indication and should be discussed with a haematologist. The rationale is that elevation of factor levels above normal will promote haemostasis, but there is limited evidence to suggest an improvement in laboratory measures of clotting and in bleeding from studies in animals and healthy individuals.20 Prospective cohort studies have reported effective haemostasis using PCC, with rates of thromboembolic complications comparable to patients receiving PCC for warfarin reversal.21,22
What is the role of laboratory measurement?
Vitamin K antagonists and UFH are routinely monitored using the INR and APTT respectively. Anti Xa activity is a measure of LMWH anticoagulant effect, which may guide protamine doses.16
The effect of direct thrombin antagonists and factor Xa inhibitors on routine clotting tests, and the utility of these tests in guiding reversal of anticoagulation is more complex. Therapeutic ranges for vitamin K antagonists and UFH should not be used to interpret clotting results in the presence of other agents. Drug-specific assays may not be available in all laboratories or out of hours. It is important to inform the laboratory of the type of anticoagulant and the timing of the last dose. The effect on routine clotting tests can depend upon which laboratory reagents are used.23,24 Furthermore, the degree of intra-individual variation in drug levels (between peak and trough levels) and the degree of variation between individuals taking therapeutic doses must be taken into account when interpreting drug levels.25 Table 4 summarises possible interpretations of normal and prolonged PT, APTT and TT in the presence of thrombin antagonists and Xa inhibitors, and the commonest drug-specific assays for each agent.
Table 4.
Effect of direct thrombin antagonists and Xa inhibitors on clotting tests, and drug-specific assays
| Drug | PT | APTT | TT | Drug specific assay | |||
|---|---|---|---|---|---|---|---|
| Normal | Prolonged | Normal | Prolonged | Normal | prolonged | ||
| Dabigatran | Below or within therapeutic levels | Supra-therapeutic levels | Below or within therapeutic levels | Within or above therapeutic levels | Likely little or no drug present | Cannot interpret | Dilute thrombin time or ecarin clotting time |
| Rivaroxaban | Therapeutic levels unlikely but cannot be excluded | Therapeutic or supratherapeutic levels | Therapeutic or subtherapeutic levels | Therapeutic or supratherapeutic levels | Unaffected | Rivaroxaban-specific anti Xa activity | |
| Apixaban | Insensitive, cannot be assessed with these methods | Unaffected | Apixaban-specific anti Xa activity | ||||
| Edoxaban | Therapeutic levels cannot be excluded | Not useful | Unaffected | Edoxaban-specific anti Xa activity | |||
APTT = activated partial thromboplastin time; PT = prothrombin time; TT = thrombin time
Whether and when to restart anticoagulant drugs following reversal
The bleeding risk associated with restarting a drug must be balanced against the thrombotic risk while off anticoagulation. If haemostasis is secured following a procedure or an intervention for bleeding, a pragmatic approach is to restart anticoagulation following local bridging protocols and monitoring for further bleeding.4 Often a prophylactic dose of LMWH or a direct oral anticoagulant (DOAC) can be started 6–8 hours post procedure. Decisions are more challenging following reversal for bleeding when no procedure to achieve haemostasis is performed, for example in intracranial haemorrhage. For some patients, especially those with traumatic intracranial haemorrhage and a persistent risk of falls, consideration may be given to discontinuing anticoagulation. Data on the optimal time to reintroduce anticoagulation following intracranial haemorrhage is minimal and conflicting, with suggested times ranging from 4–7 days26 to 10–30 weeks.27
Future prospects
Two ‘universal’ reversal agents are under development. Andexanet alfa, recently licensed in America, is a recombinant Xa modified to lack catalytic and membrane-binding activity but retain affinity to Xa inhibitors, LMWH, fondaparinux and antithrombin.28 It corrects laboratory measures of coagulation in patients with major bleeding taking direct Xa inhibitors or the LMWH enoxaparin. Rates of thrombosis are higher than in studies examining PCC, but it is unclear to what extent this reflects interruption of anticoagulation and underlying pathology.29 Ciraparantag is a synthetic molecule that binds UFH, LMWH, fondaparinux, Xa inhibitors and dabigatran. It has been examined in healthy volunteers given edoxaban where it corrected laboratory measures of clot formation.30
References
- 1.Gray E. Mulloy B. Barrowcliffe TW. Heparin and low-molecular-weight heparin. Thromb Haemost. 2008;99:807–18. doi: 10.1160/TH08-01-0032. [DOI] [PubMed] [Google Scholar]
- 2.Czuprynska J. Patel JP. Arya R. Current challenges and future prospects in oral anticoagulant therapy. Br J Haematol. 2017;178:838–51. doi: 10.1111/bjh.14714. [DOI] [PubMed] [Google Scholar]
- 3.Floyd CN. Ferro A. Indications for anticoagulant and antiplatelet combined therapy. BMJ. 2017;359:j3782. doi: 10.1136/bmj.j3782. [DOI] [PubMed] [Google Scholar]
- 4.Keeling D. Tait RC, Watson H on behalf of the British Committee of Standards for Haematology. Perioperative management of anticoagulation and antiplatelet therapy. Br J Haematol. 2016;175:602–13. doi: 10.1111/bjh.14344. [DOI] [PubMed] [Google Scholar]
- 5.Hunt BJ. Allard S. Keeling D, et al. A practical guideline for the haematological management of major haemorrhage. Br J Haematol. 2015;170:788–803. doi: 10.1111/bjh.13580. [DOI] [PubMed] [Google Scholar]
- 6.CRASH-2 Trial Collaborators Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376:23–32. doi: 10.1016/S0140-6736(10)60835-5. [DOI] [PubMed] [Google Scholar]
- 7.National Institute for Health and Care Excellence . Blood transfusion Quality standard [QS138] London: NICE; 2016. [Google Scholar]
- 8.Hunt BJ. Levi M. Urgent reversal of vitamin K antagonists. BMJ. 2018;360:j5424. doi: 10.1136/bmj.j5424. [DOI] [PubMed] [Google Scholar]
- 9.Keeling D. Baglin T. Tait C, et al. Guidelines on oral anticoagulation with warfarin – fourth edition. Br J Haematol. 2011;154:311–24. doi: 10.1111/j.1365-2141.2011.08753.x. [DOI] [PubMed] [Google Scholar]
- 10.Watson HG. Baglin T. Laidlaw SL. Makris M. Preston FE. A comparison of the efficacy and rate of response to oral and intravenous vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol. 2001;115:145–9. doi: 10.1046/j.1365-2141.2001.03070.x. [DOI] [PubMed] [Google Scholar]
- 11.Sarode R. Jr Milling TJ. Refaai MA, et al. Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation. 2013;128:1234–43. doi: 10.1161/CIRCULATIONAHA.113.002283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldstein JN. Refaai MA. Milling TJ, Jr, et al. Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Lancet. 2015;385:2077–87. doi: 10.1016/S0140-6736(14)61685-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dentali F. Marchesi C. Giorgi Pierfranceschi M, et al. Safety of prothrombin complex concentrates for rapid anticoagulation reversal of vitamin K antagonists. A meta-analysis. Thromb Haemost. 2011;106:429–38. doi: 10.1160/TH11-01-0052. [DOI] [PubMed] [Google Scholar]
- 14.Brekelmans MPA. Ginkel KV. Daams JG, et al. Benefits and harms of 4-factor prothrombin complex concentrate for reversal of vitamin K antagonist associated bleeding: a systematic review and meta-analysis. J Thromb Thrombolysis. 2017;44:118–29. doi: 10.1007/s11239-017-1506-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hirsh J. Bauer KA. Donati MB, et al. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) CHEST. 2008;133(Suppl 6):141S–59S. doi: 10.1378/chest.08-0689. [DOI] [PubMed] [Google Scholar]
- 16.van Veen JJ Maclean RM. Hampton KK, et al. Protamine reversal of low molecular weight heparin: clinically effective? Blood Coagul Fibrinolysis. 2011;22:565–70. doi: 10.1097/MBC.0b013e3283494b3c. [DOI] [PubMed] [Google Scholar]
- 17.Makris M. Van Veen JJ Tait CR. Mumford AD. Laffan M. Guideline on the management of bleeding in patients on antithrombotic agents. Br J Haematol. 2013;160:35–46. doi: 10.1111/bjh.12107. [DOI] [PubMed] [Google Scholar]
- 18.Schiele F. van Ryn J. Canada K, et al. A specific antidote for dabigatran: functional and structural characterization. Blood. 2013;121:3554–62. doi: 10.1182/blood-2012-11-468207. [DOI] [PubMed] [Google Scholar]
- 19.Pollack CV., Jr Reilly PA. van Ryn J, et al. Idarucizumab for dabigatran reversal – full cohort analysis. N Engl J Med. 2017;377:431–41. doi: 10.1056/NEJMoa1707278. [DOI] [PubMed] [Google Scholar]
- 20.Dickneite G. Hoffman M. Reversing the new oral anticoagulants with prothrombin complex concentrates (PCCs): what is the evidence? Thromb Haemost. 2014;111:189–98. doi: 10.1160/TH13-05-0431. [DOI] [PubMed] [Google Scholar]
- 21.Majeed A. Agren A. Holmstrom M, et al. Management of rivaroxaban- or apixaban-associated major bleeding with prothrombin complex concentrates: a cohort study. Blood. 2017;130:1706–12. doi: 10.1182/blood-2017-05-782060. [DOI] [PubMed] [Google Scholar]
- 22.Albaladejo P. Samama CM. Sie P, et al. Management of severe bleeding in patients treated with direct oral anticoagulants: an observational registry analysis. Anesthesiology. 2017;127:111–20. doi: 10.1097/ALN.0000000000001631. [DOI] [PubMed] [Google Scholar]
- 23.Kitchen S. Gray E. Mackie I. Baglin T. Makris M. Measurement of non-coumarin anticoagulants and their effects on tests of haemostasis: Guidance from the British Committee for Standards in Haematology. Br J Haematol. 2014;166:830–41. doi: 10.1111/bjh.12975. [DOI] [PubMed] [Google Scholar]
- 24.Dale BJ. Chan NC. Eikelboom JW. Laboratory measurement of the direct oral anticoagulants. Br J Haematol. 2016;172:315–36. doi: 10.1111/bjh.13810. [DOI] [PubMed] [Google Scholar]
- 25.Samuelson BT. Cuker A. Measurement and reversal of the direct oral anticoagulants. Blood Rev. 2017;31:77–84. doi: 10.1016/j.blre.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.AlKherayf F. Xu Y. Gandara E, et al. Timing of vitamin K antagonist re-initiation following intracranial hemorrhage in mechanical heart valves: Systematic review and meta-analysis. Thromb Res. 2016;144:152–7. doi: 10.1016/j.thromres.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 27.Majeed A. Kim YK. Roberts RS. Holmstrom M. Schulman S. Optimal timing of resumption of warfarin after intracranial hemorrhage. Stroke. 2010;41:2860–6. doi: 10.1161/STROKEAHA.110.593087. [DOI] [PubMed] [Google Scholar]
- 28.Lu G. DeGuzman FR. Hollenbach SJ, et al. A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa. Nat Med. 2013;19:446–51. doi: 10.1038/nm.3102. [DOI] [PubMed] [Google Scholar]
- 29.Connolly SJ. Milling TJ., Jr Eikelboom JW, et al. Andexanet alfa for acute major bleeding associated with factor Xa inhibitors. N Engl J Med. 2016;375:1131–41. doi: 10.1056/NEJMoa1607887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ansell JE. Bakhru SH. Laulicht BE, et al. Single-dose ciraparantag safely and completely reverses anticoagulant effects of edoxaban. Thromb Haemost. 2017;117:238–45. doi: 10.1160/TH16-03-0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoffman M. Monroe DM., III A cell-based model of hemostasis. Thromb Haemost. 2001;85:958–65. [PubMed] [Google Scholar]