Abstract
Background
Several types of psychotherapy have been proven successful in the treatment of personality disorders in younger age groups, however studies among older patients are lacking. We developed a group schema-focused therapy (SFT) enriched with psychomotor therapy (PMT) for older adults with cluster B and/or C personality disorders. This paper describes the design of a randomized controlled trial (RCT). We will evaluate the (cost-)effectiveness of this therapy protocol in specialized mental health care. We hypothesize that our treatment program is cost-effective and superior to treatment as usual (TAU) in reducing psychological distress and improving quality of life in older adults treated to specialized mental healthcare.
Methods
A multicenter RCT with a one-year follow-up comparing group schema-focused therapy enriched with psychomotor therapy (group SFT + PMT) and TAU for adults aged 60 years and older who suffer from either a cluster B and/or C personality disorder. The primary outcome is general psychological distress measured with the 53-item Brief Symptom Inventory. Secondary outcomes are the Schema Mode Inventory (118-item version) and the Young Schema Questionnaire. Cost-effectiveness analysis will be performed from a societal perspective with the EuroQol five dimensions questionnaire and structured cost-interviews.
Discussion
This study will add to the knowledge of psychotherapy in later life. The study specifically contributes to the evidence on (cost-) effectiveness of group SFT enriched with PMT adapted to the needs of for older adults with cluster b and/or c personality.
Trial registration
Netherlands Trial Register NTR 6621. Registered on 20 August 2017.
Keywords: Schema focused therapy, Psychomotor therapy, Older adults, Group therapy, Personality disorders, Multicenter RCT, Cognitive techniques, Experiential techniques, Design article
Background
The prevalence rate of personality disorders among community-dwelling older people is estimated at 8% [1] and varies between 33 and 58% among older people referred to specialized mental health care [2–4]. The disease burden due to personality disorders is high for patients (lowered quality of life, high levels of psychological distress and a high suicide risk) as well as for society (increased medical consumption and informal care) [5, 6]. For example, maladaptive personality traits are associated with a 16–30% increase in somatic healthcare consumption among older adults [7, 8]. Adequate detection and treatment is therefore warranted from both a patient and societal perspective. Even in specialized mental health care for older adults, personality disorders often remain undiagnosed and undertreated [9, 10]. Among younger patients several psychological therapies, among which schema focused therapy (SFT) have been developed that effectively reduce the burden of personality disorders [11, 12]. SFT addresses how early maladaptive schemas influence daily life and interpersonal relationships. Schemas pertain to one’s core conceptions of self, others and the world. They are formed in childhood and adolescence. In case of adverse circumstances, maladaptive schemas and associated coping styles will develop to survive (emotionally) which later on, in a healthier environment will lead to interpersonal dysfunctional coping and emotional instability. SFT helps patients to identify their most important maladaptive schemas and to respond in a more adaptive manner when these maladaptive schemas are triggered in daily life.
Review studies in adults (< 60 years) on the treatment for personality disorders concluded that SFT improves quality of life for the borderline personality disorder. They found a recovery from psychological symptoms and that it was less expensive compared to usual care [12]. The aforementioned studies focused on the borderline personality disorder [11] for which SFT was originally developed [13]. However, effectiveness of SFT has also been proven for the avoidant personality disorder [14], mixed group personality disorders [15], and more recently for the chronic mood- and anxiety disorders [16, 17]. Although SFT is generally delivered in an individual format, group SFT is considered to speed up and amplify the effects of individual SFT [18]. Even so-called short-term group SFT [19] is associated with improvements in affective symptoms as well as personality pathology. Studies in younger and middle aged patients which tested the association between the effect of SFT and age did not find a significant impact of age [18, 20]. Extrapolation of these findings to older samples may suggest that SFT also remains effective in later life. Of all psychotherapies focused on personality disorders, SFT is considered most relevant for geriatric practice due to its favorable effects on comorbid, often longstanding affective disorders [21–23]. To date, only three uncontrolled studies of SFT among older adults have been published [9]. These studies point to favorable effects of SFT in later life. First, among 51 depressed inpatients, SFT led to improvement of depressive symptoms, anxiety and five out of the seven maladaptive schemas [24]. Second, among 31 Dutch older outpatients, group SFT improved psychological distress with effect-sizes similar to those reported for younger patients. Moreover, changes in early maladaptive schemas mediated change in psychological distress in this latter study [21]. Third, in a multiple-baseline case series study among 8 older persons suffering from a cluster C personality disorder, psychopathology remained stable during an extended baseline period, while psychopathology significantly diminished during treatment and follow-up [25].
Although these studies among older patients are promising, some caution is needed since no randomized controlled studies evaluating SFT in later life have been conducted yet [9]. Therefore, we decided to perform such a randomized controlled trial and to present its study design here. SFT protocols examined among older patients up to now highly relied on cognitive techniques. Since cognitive techniques may become less effective with increasing age [26], we added several experiential techniques. These techniques are considered powerful methods to change early maladaptive schemas in older adults [21]. Not only did we add experiential techniques to the traditional, verbal SFT approach, we also enriched our treatment protocol with PMT. By offering PMT, patients will experience how their schemas influence their behavior and feelings. The ‘learning by doing’ approach offers opportunities to try out new behaviors [27]. Moreover, discovering the origin of feelings and physical sensations is an important therapeutic mechanism of SFT. PMT contributes to this important ingredient of SFT, by using bodily awareness and physical activities to let patients experience the way they tend to behave [28]. During the preparation phase of this trial, we ran five treatment groups to refine our protocol and test its feasibility. Participants of these pilot groups highly appreciated the psychomotor therapy, the experiential techniques and the adaptation of SFT to a geriatric population, in general.
Study objectives
The aim of this article is to describe the design of a RCT examining the (cost-)effectiveness of group SFT enriched with PMT compared to treatment as usual for older patients suffering from a cluster B and/or C personality disorder. We hypothesize that our treatment program is cost-effective and superior to treatment as usual (TAU) in reducing psychological distress and improving quality of life in older adults treated to specialized mental healthcare.
Methods
Design
We designed a multi-center randomized controlled trial with two parallel treatment groups: 20 sessions of group SFT enriched with PMT delivered over a 6-months period, versus treatment as usual (TAU) for older adults with cluster B and/or C personality disorders in specialized mental health care. Primary outcome is general psychological distress. In addition, cost-effectiveness of the intervention from a societal perspective is evaluated. Outcome measurements will be administered pre- and post-treatment as well as at 6 and 12 months post-treatment. Six mental health care organizations in the Northern Netherlands agreed to participate, one university department of geriatric psychiatry (University Medical Center Groningen) and five affiliated mental health organizations (GGZ Friesland van Andel department, GGZ Drenthe, Lentis, Dimence and Mediant). The study has been approved by the Medical Ethics Committee of the University Medical Center Groningen on May 12th, 2017 (M17.212189) and was registered in the Dutch Trial Register on August 20th, 2017 (NTR 6621).
Study population
Eligible are patients, 60 years or older with a cluster B and/or C personality disorder according to the DSM-5 who are referred to or are currently treated at an outpatient clinic for geriatric psychiatry of the participating centres in the Netherlands. According to DSM-criteria, the criterion threshold for diagnosing a personality disorder in older patients is too strict [29, 30]. For that reason we will also include older patients falling short one content criterion for a specific cluster B and/or C personality disorder, provided that they meet the general diagnostic criteria for a personality disorder (hereafter ‘subthreshold cluster B/C personality disorder’). Older patients generally endorse fewer specific personality disorder criteria than younger age groups (29% of the criteria contain measurement bias in older age groups), while the latent variable structure for each personality disorder suggests a similar severity level of personality pathology [30]. Specific inclusion criteria are: 1) age of 60 years or above; 2) cluster B or C personality disorder (or falling one content criterion short) as confirmed by the Structured Clinical Interview for DSM-5 for personality disorders (SCID-5-PD) [31] 3) mentally able to adhere to the group SFT treatment schedule and to fill out the schema (mode) questionnaires and 4) giving informed consent after having received oral and written information. Exclusion criteria are: 1) severe current mental illness, including bipolar I disorder, psychosis, or substance abuse disorders needing clinical detoxification; 2) an established neurodegenerative disorder; 3) cognitive impairment defined as a sum score below 23 points on the Montreal Cognitive Assessment (MoCA) battery [32]; 4) having received schema-focused therapy in the previous year or during the current illness episode; and 5) suicide risk interfering with adequate treatment delivery. Physical restraints or physical frailty are no exclusion criterion. Despite the group format, the PMT will be individually adapted so that even the frailest patients can participate.
Recruitment
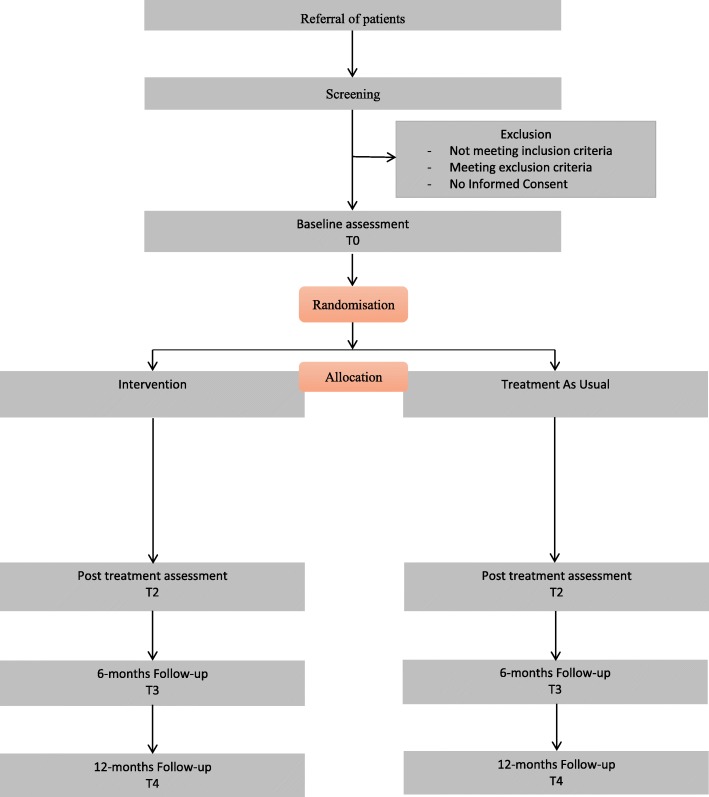
Mental health professionals working at the different sites can inform patients about the study when a cluster B or C personality disorder is suspected. After having received oral and written study information from their mental health professional interested potential eligible patients will get an appointment with the clinical psychologist at their clinic. During this screening session, the in- and exclusion criteria for the study are formally checked by administering amongst others the SCID-5-PD and MoCA and any remaining questions the patient has about the study are answered. For patients not meeting the in- and exclusion criteria the study ends after this screening session. Patients eligible for the study, will be given another 2 weeks to consider participation. Patients willing to participate in the study, will be asked to sign informed consent and are put on a waiting-list. Only the patients who gave written informed consent are included in the study. The data from the screening appointment, will be passed on – anonymously – for inclusion in the study database. When a minimum of 8 and maximum of 16 patients have given informed consent at a specific site, baseline measurements will be conducted, after which participants will be randomized (see flowchart) Fig. 1.
Fig. 1.
depicts the flowchart of the study
Sample size calculation
The only RCT comparing group SFT with TAU was conducted among younger adults with borderline personality disorder and found a between group Cohen’s d effect size (ES) of 2.0 on the Brief Symptom Inventory (BSI-53) [33]. For our power analysis, we tuned down the expected ES to 0.5 (medium effect) for two reasons. First, the ES of 2.0 was partly due to absence of an effect of TAU [34] while meta-analysis of psychotherapy in geriatric psychiatry shows an average pre-post ES of 0.4 for TAU [17]. Second, an open study on group SFT reported a pre-post Cohen’s d ES of 0.8 among older adults with mixed cluster B and C personality disorders [21]. Applying a 2-sided alpha of 0.05 and a power of 80% to detect an ES of 0.5, requires 63 patients per arm. Although compensation for dropout is not necessary according to the CONSORT criteria when performing intention to treat analyses (http://www.consort-statement.org/), we aim to include 140 patients in order to compensate for 10% early dropouts during the waiting-list period. Differences in the scores between the intervention and control group on the various outcome measures (BSI-53, EQ-5D-5 L, YSQ and SMI) will be analyzed using linear mixed-models accounting for missing data and relevant confounders.
Randomisation, blinding and treatment allocation
A stratified block randomisation will be performed aimed to assign participants evenly (1,1) over the two conditions [35]. Randomisation will be performed per study site and stratified by the presence of a full versus subthreshold cluster B/C personality disorder (PD – 1 criterion). Participants will be randomized in blocks when 8 to 16 consecutive patients have consented to participate at a specific study site. Randomisation will be performed centrally using online randomisation software QuickCalcs of GraphPad (http://www.graphapd.com/quickcalcs/randMenu).) by an independent investigator who will be blind to patient characteristics. Patients will be randomized in even patient numbers per stratum. In case of an uneven number of participants per stratum, the next even number of patients will be randomised and the last allocation will be forwarded to the next block randomisation with an uneven number of patients within that stratum. After randomisation, patients and their responsible geriatric psychiatrist or psychologist will be informed of their allocation. The therapists delivering the intervention will be informed which patients can be invited for group SFT + PMT.
Group Schema-focused therapy enriched with PMT
Two individual pre-treatment sessions without PMT take place before the group sessions. These are meant to make a personal treatment plan based on administering the Young Schema Questionnaire (YSQ) and Schema Mode Inventory (SMI) (see Mediators section below) and to explain the concept of group SFT enriched with PMT in more detail. The subsequent group interventions comprise 20 sessions over a period of 26 weeks. The first 18 sessions will be provided weekly after which two follow-up sessions are given at week 22 and 26. Each treatment session consists of a 2 h group session SFT and 1 h group session PMT, with a 15-min break in between. Treatment is provided according to a detailed protocol. This protocol is highly structured and based on the Dutch protocols short cognitive schema-focused group therapy [36] and experiential techniques [37, 38]. During the initial group sessions, patients will be further educated about the schema model, specifically in relation to their own three predominant schemas and coping styles (called ‘modes’ in schema focused therapy). In the second treatment phase the patients maladaptive schemas will be triggered and patients will be taught to respond in a more adaptive manner. In this treatment phase the ‘experiential imagery rescripting’ and ‘chair interventions’ will be conducted [37, 38]. All patients receive a personal schema-focussed therapy workbook for older adults. This workbook will be extended every session with a summary of the session information and homework assignments. The patients will write a weekly summary of their therapy process and fill in a ‘severity score form’. On this form patients rate the severity of their 3 predominant schemas and maladaptive modes. Based on clinical experience with older persons, geriatric themes like loss of a role in society, loss of loved-ones, comorbid somatic diseases and sociocultural beliefs in the treatment of elderly, are integrated in the treatment protocol [39, 40]. Furthermore, the protocol has been enriched with PMT to overcome the limitations of verbal therapy. During PMT, the psychomotor therapist sets up individual and group-based physical interventions to facilitate that patients experience their schemas and modes. Continuity between the verbal and psychomotor sessions is guaranteed by participation of the psychologist in the PMT as co-therapist. This way the observations pending PMT can be further analyzed in the verbal sessions.
Treatment as usual
Treatment as usual (TAU) will be unrestricted as long as no group SFT is provided. Usually this means that a multidisciplinary team will determine the best treatment for each patient. This can be either psychotherapeutic or drug treatment, individual or group treatment, outpatient-, day- or inpatient treatment or any combination deemed necessary. The treatment provided will be registered, to facilitate interpretation of results. From our clinical experience, we expect that TAU will mainly consist of structured and supportive case-management of personality problems or treatment restricted to (comorbid) axis I psychiatric disorders, ideally according to disorder specific guidelines.
Therapists, training and supervision
All interventions in the experimental group are provided by psychologists with a minimum of 2 years post graduate clinical training in combination with fully licensed and registered psychomotor therapists. During the verbal SFT sessions, a co-therapist will participate. Co-therapists are generally also psychologists but psychotherapeutic oriented nurse practitioners experienced in group treatment are also allowed. One of the psychologists providing verbal SFT will also participate as co-therapist in the PMT sessions. All psychologists and psychomotor therapists receive a two-day training led by the first author, a clinical psychologist who is also a licensed schema-focused therapist. The psychomotor therapists are trained by the third author. This training covers how to deliver a structured SFT program, training of the SFT adaptations to older adults and PMT techniques. The training is supported by video material of verbal SFT and PMT techniques. All therapists receive a manual with the treatment protocol, including a detailed description of all sessions divided in a SFT and a PMT section. Moreover, to improve protocol compliance, the SFT-interventions provided must be ticked off on standardized forms (part of the manual) per session. Session attendance of the individual patients will also be recorded by the therapists. During the study, all therapists will participate in a monthly supervision program provided by the first and third author. Furthermore, all SFT and PMT group sessions in the intervention arm will be audiotaped and saved for evaluation. Of each therapy group two audiotapes will be randomly selected and rated by independent psychologists on protocol compliance. All interventions listed in the treatment manual for the selected session will be evaluated on whether or not the intervention was delivered and the quality of that deliverance, as rated on a scale ranging from 0 (not delivered) to 10 (delivered excellently). A total of at least 10 tapes will be rated by two raters to assess the interrater reliability, as expressed the intra class correlation coefficient (ICC) [41].
Assessments
Data are collected at the following moments: at the screening, baseline (T1), at the end-of-treatment (T2, i.e. 6 months after baseline for the TAU group), and finally at 6- and 12-month follow-up (T3 and T4). Many outcomes consist of self-report measures. Some are assessed by structured telephone interviews conducted by research assistants who will be blind about the treatment allocation of the interviewed patient. These interviews include assessment of socio-demographic characteristics and psychiatric history (at baseline only) as well as medical consumption and costs in the past 3 months. Personal information about potential and enrolled participants will be stored confidentially. Table 1 shows the questionnaires used at each assessment.
Table 1.
.shows the questionnaires used at each assessment
| Time of assessment | |||||
|---|---|---|---|---|---|
| Screening | Baseline | Post treatment assessment | 6-month Follow-up | 12-month Follow- up |
|
| Primary outcomes | |||||
| Psychological distress: BSI-53 | X | X | X | X | |
| Health-related quality of life: EQ-5D-5 L | X | X | X | X | |
| Medical consumption & costs | X | X | X | X | |
| Secondary outcomes | |||||
| Life satisfaction: Cantril’s Ladder | X | X | X | X | |
| Mental wellbeing: WEMWBS | X | X | X | X | |
| Personality functioning: SIPP-SF | X | X | X | X | |
| Interoceptive body awareness: MAIA | X | X | X | X | |
| Psychotropic drug use & treatment received | |||||
| Mood variability: Mood-Zoom | X | X | X | X | |
| Characteristics | |||||
| Personality disorders: SCID-5-PD Cluster B & C | X | ||||
| Mental disorders: MINI-Plus | X | ||||
| Cognitive screening: MoCA | X | ||||
| Psychiatric treatment history: telephone interview | X | ||||
| Socio-demographics: telephone interview | X | ||||
| Chronic illnesses: LASA questionnaire | X | ||||
| Early life-events: NEMESIS questionnaire | X | ||||
| Alcohol use: AUDIT | X | ||||
| Current smoking: NEMESIS questions | X | ||||
| Physical activity: NEMESIS question | X | ||||
| Personality traits: PID-5-SF | X | ||||
Primary outcome parameter
Psychological distress in the past week, as indicated by the sum score of the Brief Symptom Inventory 53 item version (BSI-53), is the primary clinical outcome parameter. The BSI-53 is a self-report questionnaire and an abbreviated version of the Symptom Checklist-90 (SCL-90) [33, 42]. The BSI is validated for older adults and preferred over the SCL-90 since validation studies in older adults did not indicate any information loss compared to the SCL-90 [43]. We have chosen for psychological distress as the primary outcome parameter since 1) older patients with personality problems are rarely referred to geriatric mental healthcare for personality problems specifically, but nearly always for associated affective symptoms and 2) the study includes patients with a variety of personality disorders. Since the reliability of the Dutch BSI-53 subscales is rated as good and their convergent and divergent validity has been found to be satisfactory [42], subscale scores will be examined as secondary outcome parameters.
Economic evaluation
The EuroQol-5D-5 L (EQ-5D-5 L), a generic self-report instrument, will be administered to measure health-related quality of life at the time of assessment [44]. It consists of five questions, each related to a specific dimension of health status: mobility, self-care, usual activity, pain/discomfort and anxiety/depression. The utility score of the EQ-5D-5 L will be used to calculate Quality-Adjusted Life-Years (QALYs) [45]. Medical consumption and other cost data will be collected by means of structured telephone interviews, as previously done in a younger patient group [44]. Since a considerable amount of resource use is situated outside (mental) healthcare institutions, data of formal registries such as hospital information systems or insurer’s databases are incomplete [44]. Therefore, patient-reported prospective cost diaries [46] or retrospective cost interviews [47], are the preferred instruments covering all relevant events. We have chosen a 3-month recall interview [48, 49] since a prospective cost diary or a recall interview over a longer period are expected to lead to more missing items.
Secondary outcome parameters
A number of secondary outcome parameters have been chosen to specify the extent and nature of the effect of group schema focused therapy in later life.
Psychotropic drug use
Data on current psychotropic drug use and changes in between assessments will be collected as part of the telephone interviews, described above.
Life satisfaction
Life satisfaction will be assessed with Cantril’s ladder, a single self-report question to rate one’s current life situation on a scale (from 0 to 10) [50]. Life satisfaction is a conceptualization of subjective wellbeing which stresses the cognitive evaluation of one’s life situation, in contrast to for example feelings such as happiness. A score of 0 indicates ‘the worst possible life for you’ and 10 ‘the best possible life for you’.
Mental wellbeing
Mental wellbeing is assessed with the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) [51]. Mental health and mental illness have been shown to be related but distinct concepts [52]. Reduction or absence of mental illness does not necessarily imply good mental health and wellbeing. The WEMWBS focusses on mental wellbeing and consists of 14 items covering positive affect, satisfying interpersonal relationships and positive functioning. Items have to be rated on a 5-point Likert scales assessing the frequency of the positive feeling over the past 2 weeks. A higher sum score indicates a better mental wellbeing.
Personality functioning
Personality functioning is assessed with the Severity Indices of Personality Problems – Short Form (SIPP-SF) [53]. The SIPP-SF assesses five core domains of (mal)adaptive personality functioning defined in the DSM-5 alternative dimensional personality disorders model, namely: Identity Integration, Self-Control, Relational Functioning, Social Concordance and Responsibility. The 60-items of the questionnaire consists of propositions referring to the last three-months, which are answered on four-point Likert scales, ranging from fully agree to fully disagree. Higher scores imply more adaptive functioning. The SIPP-SF has been studied in an older sample and was suggested to be a useful clinical tool to assess effects of therapy on levels of personality functioning in this age group [54].
Interoceptive body awareness
Interoceptive body awareness is assessed with the Multidimensional Assessment of Interoceptive Awareness (MAIA) [55]. The MAIA is a 32-item self-report questionnaire, measuring eight dimensions covering both the ability to notice bodily sensations and to regulate their influence on behavior. Treatment responsiveness of the MAIA was recently shown in a study on bodily focused contemplative training [56] which found improvements on five of the eight MAIA scales.
Mood variability
Trying to measure emotion dysregulation in real life situations, we will assess mood variability with the self-report Mood Zoom, an experience sampling method for real-time mood assessment on a smartphone [57]. Participants are prompted by the phone to rate their current mood on a screen displaying six different moods which have to be scored on 7-point Likert scales. We will prompt participants three times a day, at random time points, over a one-week period per assessment.
Patient characteristics (and potential predictors of treatment outcome)
Patient characteristics will be assessed during the screening procedure in order to verify in- and exclusion criteria and the formal baseline assessment, to describe the study sample, and to test and control for baseline differences between the study groups. The screening procedure includes the formal assessment of cluster B or C personality disorders, 2) comorbid mental disorders, and 3) cognitive functioning. The formal baseline assessment includes 4) a psychiatric treatment history, 5) socio-demographics, 6) chronic somatic diseases, 7) early life events, 8) alcohol use, 9) current smoking, 10) physical activity and 11) personality traits.
Personality disorders
Personality disorders, according to the traditional categorical DSM-5 model, will be assessed with the Structured Clinical Interview for DSM-5 for personality disorders [31]. To minimize patient burden, the interview will be limited to the general diagnostic criteria for a personality disorder and the cluster B or C personality disorder criteria.
Mental disorders
Comorbid psychiatric disorders will be assessed with the aid of a DSM-5 checklist. This checklist summarizes all DSM-5 criteria for the following disorders: Major Depressive Disorder, Persistent Depressive Disorder, Manic and Hypomanic Episodes, Bipolar Disorders type I and II, Generalized Anxiety Disorder, Panic Disorder, Agoraphobia, Social Anxiety Disorder, Posttraumatic Stress Disorder, Obsessive Compulsive Disorder, Somatic Symptom Disorder, and Illness Anxiety Disorder. Based on the screening interview with the patient and all available information in the medical records, the psychologist checks which criteria have been present over the past 6 months and which psychiatric disorders are currently present.
Cognitive functioning
Global cognitive functioning will be assessed with the Montreal Cognitive Assessment (MoCA). The MoCA is a screening instrument to be administered by trained interviewers (psychologist in this study) for the detection of neurocognitive disorders and assesses a broad range of cognitive domains. We will exclude patients with a sum score below 23 points. A recent meta-analyses showed that a cutoff score of 23/30 shows overall better diagnostic accuracy and a lower false positive for the presence of neurocognitive disorders than the initially recommended score of 26/30 [32].
Psychiatric treatment history
Time of first treatment in mental healthcare will be assessed in the structured telephone interview at baseline.
Chronic somatic diseases
The presence of chronic somatic diseases is assessed by self-report questions as validated within the Longitudinal Aging Study Amsterdam (LASA) [58, 59]. The questions inquire about the presence of the following chronic diseases: chronic non-specific lung disease, cardiac diseases, atherosclerotic disease of the abdominal aorta or the arteries of the lower limb, diabetes mellitus, cerebrovascular disease, osteoarthritis, rheumatoid arthritis, malignant neoplasms, high blood pressure, stomach ulcers, bowel disorders, liver disease, epilepsy, allergies, thyroid disease, injuries, serious head trauma, and other chronic diseases. The LASA study shows that the accuracy of patients’ self-reports, as compared to general practitioners’ information regarding to the presence or absence of specific chronic diseases, is generally satisfactory [59].
Early life events
Childhood trauma will be assessed using a structured inventory previously used in the Mental Health Survey and Incidence Study (NEMESIS) [60]. In this inventory participants are asked whether they have experienced any kind of neglect or abuse before the age of 16. Covered are: emotional neglect, which includes the lack of parental attention or support and interest in one’s problems and experiences; psychological abuse, which includes verbal abuse, punishment without reason, subordination to siblings and being blackmailed; physical abuse, which includes being kicked, hit with or without an object and any other physical harm; and sexual abuse, which is defined as being sexually touched against one’s will, or being forced to touch someone sexually. After an affirmative answer, a question is asked about the frequency of these events, to be recorded as: never, once, sometimes, regularly, often or very often. A childhood abuse index can be constructed by recoding the frequency scores in (0) never, (1) once, sometimes and (2) regularly, often or very often. The scores of each of the four domains of abuse will be summed, resulting in a childhood abuse index which ranges from 0 to 8. Early life-events will be additionally measured and include divorce of parents, placement in children’s home, juvenile prison or foster care, and walking away from home.
Lifestyle characteristics
Alcohol use will be assessed with the Alcohol Use Disorder Identification Test (AUDIT) [61], a screening questionnaire for alcohol-related problems in the past year. Current smoking and physical activity will be assessed by two single questions from NEMESIS on current smoking and number of hours per week spent in physical exercise or sport lately, not counting sedentary pursuits such as chess or fishing [60].
Personality traits
Pathological personality traits are a second dimension of the DSM-5 alternative dimensional model for personality disorders and can be measured with the 220-item Personality Inventory for DSM-5 (PID-5) [62]. The PID-5 covers 25 pathological personality trait facets, which can be combined to obtain scores for five higher-order domains distinguished. These domains are related to the traditional big five personality traits and to concepts from schema-focused therapy [63]. Most items of the PID-5 are age neutral and thus can be used in older adults [64]. Recently, the PID-5-Short Form (PID-5-SF) has been validated, yielding nearly identical reliability and validity as the long form in scoring the DSM-5 domains and facets [63]. This version will be applied in the present study to minimize patient burden. All items are rated on four-point Likert scales from 0 (very false or often false) to 3 (very true or often true). The combination of pathological personality traits (PID-5-SF) and impaired personality functioning (SIPP-SF) results in the alternative DSM-5 model personality disorder diagnoses.
Mediators
We will examine whether any improvement on the primary and secondary outcome parameters in patients receiving the experimental schema therapy can be attributed to (i.e. is mediated by) improvements in the therapy specific targets. Mediators are early maladaptive schemes and schema modes, which will be assessed,in the experimental group only, pre-treatment (i.e. in the two initial, individual sessions of treatment) and 3, 6 and 12 months post-baseline, and schemas and modes severity scores, which will be assessed during treatment on a weekly basis.
Early maladaptive schemas
Early maladaptive schemas will be assessed with the self-report Young Schema Questionnaire second version (YSQ-2) [65–68]. The YSQ-2 is the most commonly used measure of early maladaptive schemas [65]. The YSQ-2 consists of 205 items, to be rated along a 6-point Likert scale, which measures the severity of 16 maladaptive schemas. The Dutch YSQ-2 has good reliability and convergent and discriminant validity [69].
Schema modes
Schema modes will be assessed with the Schema Mode Inventory (SMI), a 118-item, self-report questionnaire measuring 16 modes [65]. These modes can be divided into 4 types: healthy modes, parent modes, child modes and coping modes. All items are rated on a 6-point Likert scale. The Dutch SMI has an excellent test-retest reliability and the convergent and divergent validity of the subscales are satisfactory [70].
Schema and modes severity scores
Patients will rate the severity of their three most dominant schemas and modes on a scale from 0 (no burden at all) to 10 (a lot of burden) on a weekly basis.
Analyses
Analyses will be conducted according to the intention-to-treat principle. Differences between the intervention and control group on the various outcome measures (BSI-53, EQ-5D-5 L, secondary outcome parameters) will be analyzed using linear mixed-models, more specifically random coefficient analysis, which accounts for missing observations [71]. In these analyses, study site and patient will be included as random effects (with observations nested in patients and patients nested in study sites) and study arm and full versus subthreshold personality disorder as fixed effects. Interactions will be tested 1) between time of observation and study arm and 2) between this interaction and full versus subthreshold personality disorder, to check whether the intervention effect is different for patients with a full or subthreshold personality disorder. All analyses will be controlled for the baseline population characteristics described above.
Economic evaluation and budget impact analysis
The cost-effectiveness analysis will be performed alongside the clinical trial to assess the cost-effectiveness of group SFT + PMT versus TAU. The cost-effectiveness analysis will result in two separate incremental cost-effectiveness ratios (ICERs) for group SFT + PMT compared to TAU, i.e. incremental costs per additional point improvement on the BSI-53, and incremental costs per Quality Adjusted Life Year (QALY) gained. The analysis will be performed taking a societal perspective and with a time horizon of 18 months. Costs and effects will be discounted according to Dutch guidelines [45]. Univariate sensitivity analyses will investigate the impact of individual assumptions and parameters (e.g. costs of SFT + PMT and other elements). To quantify the uncertainty around the ICERs, bootstrap resampling will be performed. Results will be presented as tornado diagrams and cost-effectiveness acceptability curves, the latter representing the probability that group SFT + PMT is cost-effective given a certain value of ‘willingness to pay’ for a QALY (or one point improvement on the BSI). Included costs will be those of group SFT enriched with PMT, other forms of psychotherapy, hospital admissions, medication, outpatient visits, General practitioner visits, home care, and lost productivity from both paid and unpaid work. Unit prices will be determined according to Dutch guidelines [45].
A budget impact analysis will be performed to inform decision makers on the financial consequences of the adoption and diffusion of group STF + PMT in the Dutch health care system. The analysis will be performed according to the most recent principles of the ISPOR task force [72] and Dutch guidelines [45]. The trial results will be extrapolated to a time horizon of 5 years, and for the entire Dutch population concerned. Aging of the population will be taken into account. Sensitivity analysis will explore several scenarios, regarding speed of uptake of the therapy in clinical practice and patients’ willingness to participate.
Discussion
This paper presents the design of the first randomized controlled trial evaluating the effectiveness of group SFT enriched with PMT, for older adults with personality disorders. To date, only uncontrolled studies on the treatment of personality disorders have been conducted in this age-group [21, 25]. This RCT is especially relevant in the light of aforementioned underdetection and undertreatment of personality disorders in later life [10]. Nonetheless, we faced many choices when designing the protocol, since group SFT has rapidly evolved over the past decades and its applications have even broadened beyond personality disorders alone. Below the most important choices will be discussed.
Group versus individual format
Evaluation of group therapy within a randomized controlled design may result in some difficulties. First, sufficient patients have to provide informed consent before the therapy can start. This may lead to early dropouts when recruitment is slow at some study sites and waiting period becomes long. Secondly, some patients are reluctant towards group therapy. This may be especially so for older people, who easily feel they have to ‘hang themselves out to dry’ [73]. Nonetheless, we have taken the risk of non-participation as delivering SFT in a group format has many advantages. First, a group process may speed up the therapeutic process [74]. Secondly, group therapy may counterbalance loneliness, a frequently encountered problem in later life [75] especially among personality disordered persons. Thirdly, a group format is more efficient from an economic perspective [76] as well as in light of the scarcity of gerontopsychologists [77].
Choice of control group
The choice of an adequate control group is critical when designing a randomized controlled trial. Since personality disorders usually remain largely undetected in geriatric psychiatry and treatment is generally focused on the manifest affective symptoms, we considered comparison to usual care as most appropriate. Even if the mere provision of attention would explain a positive effect of our therapy, this may imply that treatment intensity in geriatric psychiatry in general is too low. Alternative options were disqualified for the following reasons. Firstly, an active control group to control for attention is generally desired in psychotherapeutic research [78]. Ideally, two effective therapies would be compared searching for the most effective treatment modality. However, for none of the available therapies for personality disorders, effectiveness is proven in geriatric psychiatry. When no differences are found then, this could easily lead to the wrong conclusion that both therapies are probably non-effective, and to withholding of effective treatment from older patients with personality disorders. Secondly, a waiting-list control group was dismissed for two reasons. First, the placebo-effect or spontaneous recovery may even be reduced by a waiting list [79]. Second, personality pathology is associated with a high disease burden and when referred to specialized mental health care, a waiting list of 18 months was not deemed acceptable. Finally, from an economic perspective, it is always more informative to assess cost-effectiveness of an intervention as compared to care as usual, since this best approaches the real-world situation if the intervention were to be implemented in routine clinical practice.
Enrichment with PMT.
Arguments for the addition of PMT have already been given in both the introduction and methods of this article. Nonetheless, this step is probably most debatable as even among younger patients no examples of this combination have been reported. However, pure cognitive interventions are generally less effective in later life [80] and older persons generally have more difficulties in expressing their emotions and feelings verbally than younger persons [81]. In our protocol we added PMT and experiential techniques and provided it to 5 pilot groups who reported a potential surplus value for the experiential techniques and PMT. The continuity of one of the group therapists who also attends the PMT sessions was highly appreciated.
Primary outcome parameter
Although group SFT focuses on personality change, we did not choose personality (dys)functioning as primary outcome parameter for several reasons. First, we did not restrict our study population to one personality disorder specifically. Many studies on SFT are restricted to borderline personality disorder. In those studies, it is rational to consider the severity of borderline personality pathology as the primary outcome parameter. In studies with mixed personality disorders, however, this becomes less suitable. Moreover, most personality pathology instruments are multidimensional and therefore difficult to consider as primary outcome parameter. And taking recovery, defined as not meeting the DSM-criteria for a personality disorder anymore, as the overarching outcome measure, would mean that a semi-structured diagnostic interview should be repeated at each follow-up assessment, which is time-consuming and could increase patient dropout. Second, in geriatric psychiatry most patients with a personality disorder are referred to specialized mental health care for disabling affective symptoms [30]. Specific treatment for personality disorders is often not available and rarely offered in old age psychiatric services. So the majority of older patients with personality disorders receive pharmacotherapy with or without nurse-led supportive care for an affective disorder, although psychotherapy is the preferred treatment for the underlying personality disorder according to clinical guidelines [45]. This is a situation which calls for a change, as meta-analyses among younger age groups have shown that comorbid personality disorders worsen the prognosis of affective disorders and predict relapse [82]. Moreover, previous studies on SFT in both younger and older patients have reported large effect-sizes for improvement of general distress [83]. Earlier research focused mainly on the cognitive variant of (group) SFT for treatment of personality disorders in younger and middle-aged adults (< 60 years). This cognitive variant may be somewhat less effective for older adults (> 60 years). This study will provide an answer to the question whether group SFT enriched with PMT adapted to the needs of for older adults with cluster b and/or c personality is effective and cost-effective. Acknowledging the numerous methodological choices that have to be made, we hope to motivate other researchers to conduct also RCT’s on the (cost-)effectiveness of the different psychotherapies in older adults with personality disorders.
Acknowledgements
We would like to thank the patients and therapists of the five pilot groups for their helpful feedback. We also thank the Rob Giel Centre of the University of Groningen, University Medical Center Groningen for facilitating the study.
Project members
Prof. dr. R.C. Oude Voshaar (Projectleader and secretary)
T: 050-3612367 | F: | E: r.c.oude.voshaar@umcg.nl
Universitair Medisch Centrum Groningen
Universitair Centrum Psychiatrie
Biologische Psychiatrie
Postbus 30001
9700 RB GRONINGEN
Prof. dr. R.A. Schoevers (Administrative responsibility)
T: 0503612065 | F: | E: r.a.schoevers@umcg.nl
Universitair Medisch Centrum Groningen
Universitair Centrum Psychiatrie
Postbus 30001
9700 RB GRONINGEN
Dr. M.L. Boshuisen (Project commission member)
Position: Psychiatrist
T: 050-5223292 | F: | E: m.l.boshuisen@lentis.nl
Lentis Ouderenpsychiatrie
Laan Corpus den Hoorn 102/2
9700 AB GRONINGEN
Prof. dr. S.P.J. van Alphen (Project advisor)
T: 0032-2-629 15 26 | F: | E: spj.vanalphen@planet.nl
Vrije Universiteit Brussel
Pleinlaan 2
1050 BRUSSEL
Dr. A.D.I. van Asselt (Project commission member)
Position: Senior onderzoeker, Health Economist|
T: 0503615296 | F: | E: a.d.i.van.asselt@umcg.nl
Universitair Medisch Centrum Groningen
Epidemiology
Health Technology Assessment
Hanzeplein 1
9713 GZ GRONINGEN
Dr. R.H.S. van den Brink (Project commission member)
Position: Senior researcher RGOc
T: 0503612089 | F: | E: r.h.s.van.den.brink@umcg.nl
Universitair Medisch Centrum Groningen
Universitair Centrum Psychiatrie
Rob Giel Onderzoekcentrum
Postbus 30001
9700 RB GRONINGEN
Drs. S.D.M. van Dijk (Project commission member)
Position: clinical psychologist
T: 0503612367 | F: | E: s.d.m.van.dijk@umcg.nl
Universitair Medisch Centrum Groningen
Universitair Centrum Psychiatrie
Postbus 30001
9700 RB GRONINGEN
Participating Organisations
Universitair Medisch Centrum Groningen
Universitair Centrum Psychiatrie
Postbus 30001
9700 RB GRONINGEN
Dimence
Postbus 5003
7400 GC DEVENTER
GGZ Drenthe
Postbus 30007
ASSEN
Funding
This study was supported by a grant of the Netherlands Organization for Health Research and Development (ZonMW); grant number 843001706.
Availability of data and materials
The proposed study will be using the data-management infrastructure of the University Center for Psychiatry (UMCG), which is a well-equipped, integrated system that meets current guidelines and regulations. After the main outcome and cost-effectiveness analysis have been published, all data will be freely available for other groups.
Authors ‘contributions
All authors have been involved in designing the study. SDMD and MSV have written the first draft of the manuscript in collaboration with RHSB and RCOV. R. Bouman, SPJA, PJD, DHV, JP, MLB and ADIA have critically commented on subsequent drafts. All authors read and approved the final manuscript.
Authors ‘information
S.D.M. van DIJK is a fully licensed clinical psychologist (FGzPt/VGCT/MSc.), behavioral therapist, and schema focused therapist. She is manager of the multiple day-treatment program for older patients with personality and affective disorders. She works as a teacher for the national postmaster psychology education (RINO and PPO). She has developed and executed the pilot study on group schema-focused therapy enriched with psychomotor therapy. She enrolled in a PhD program where she studies personality and personality disorders in older adults.
M.S. VEENSTRA is a graduated psychologist and is the PhD student of the current study at de Rob Giel Research Center of Mental Health Services Research of the University Medical Center Groningen. She carries out the daily tasks and is the contact for the participating institutions.
R. BOUMAN works as a psychomotor therapist at the University Medical Centre Groningen. She started this new treatment protocol with Silvia and treated the five pilot groups. She enrolled in a PhD program to study the effects of psychomotor therapy in older adults more closely.
P.J. VAN DALEN is a geriatric psychiatrist and trainer in geriatric psychiatry at Dimence, where he is manager care of the division Elderly Mental Health Care as well, participating in the management team. He is author of a chapter in the Guidebook intensive home treatment (2016) regarding the application of IHT in the elderly population with psychiatric problems.
J. PEEKEL is a health care psychologist and study coordinator at Mediant, Mental Health Organization. She works mainly with elderly patients.
D.H. VEENSTRA is a clinical psychologist (FGzPt) at Van Andel geriatric psychiatry, a division of GGZ Friesland. She works over 20 years in the mental health care for older adults and is experienced in diagnosis and treatment of a broad range of mental disorders. As manager she is responsible for the programs for in- and outpatient treatment and the multiple day-treatment programs.
S.P.J. VAN ALPHEN, PhD, is a psychologist and professor of clinical psychology at the Free University of Brussels (VUB). The main focus of his research field is screening, assessment and psychotherapy of personality pathology in later life. He is (co) author of many research articles and chapters of handbooks regarding personality disorders in older adults as well as the principal editor of the Dutch Handbook on Personality Disorders in later life.
A.D.I. VAN ASSELT, PhD, is a health economist/epidemiologist with over 15 years of experience in both trial-based and model-based economic evaluations, covering a wide range of clinical areas, among which SFT in patients with borderline personality disorder. She previously worked at the Maastricht UMC, where she was part of a team conducting assessments for the National Institute of Clinical Excellence (NICE) in the UK. She joined the departments of Epidemiology (UMCG) and PharmacoEpidemiology & Pharmacoeconomics (RuG) in March 2014.
R.H.S. VAN DEN BRINK, PhD, is a psychologist/epidemiologist working as senior researcher at the Rob Giel Research Center of Mental Health Services Research of the University Medical Center Groningen. He is coordinator of the Network for Geriatric Psychiatric Research of the collaborating mental health services in the Northern Netherlands and as such within the present proposal appointed as representative for the mental health care organizations participating in this trial.
M.L. BOSHUISEN is a geriatric psychiatrist and clinically specialized in the psychological treatment of older adults. She works as a program-director of the division of Old Age Psychiatry at Lentis/Dignis.
R.C. OUDE VOSHAAR is the principle investigator of the present study and professor of Old Age Psychiatry at the University of Groningen, University Medical Center Groningen. He is specialized in late-life affective disorders, encompassing mood, anxiety, and somatoform disorders. His research line focusses on the interaction between affective disorders and either cognitive dysfunctioning, physical frailty or personality pathology.
Name and contact information for the trial sponsor
ZonMw Postbus 93 245
2509 AE Den Haag
Phone +3170 349 51 11
E-mail info@zonmw.nl
Abbreviations
- AUDIT
Alcohol Use Disorder Identification Test
- BIA
Budget Impact Analysis
- BSI
Brief Symptom Inventory
- CEA
Cost-Effectiveness Analysis
- CERs
Incremental cost-effectiveness ratios
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- EMS
Early Maladaptive Schemes
- EQ-5D-5 L
EuroQoL assessment of health related quality of life
- ES
Effect Size
- GP
General Practitone
- LASA
Logitudinal Aging Study Amsterdam
- MAIA
Multidimensional Assessment of Interoceptive Awareness
- METC
Medical research ethics committee
- MoCA
Montreal Cognitive Assessment
- NEMESIS
Netherlands Mental Health Survey and Incidence Study
- PD
Personality Disorders
- PID-5-SF
Personality Inventory for DSM5 - Short Form
- PMT
Psycho-Motor Therapy
- QALYs
Quality-Adjusted Life-Years
- RCT
Randomized Clinical Trial
- RGOc
Rob Giel Research center of Mental Health Services
- ROMGPS
Routine Outcome Monitoring for Geriatric Psychiatry & Science
- SCID-5
Structured Clinical Interview for DSM-5 personality disorders
- SCL
Symptom Check List
- SFT
Schema Focussed Therapy
- SIPP-SF
Severity Indices of Personality Functioning – Short Form
- SMI
Schema Mode Inventory
- TAU
Treatment As Usual
- Wbp
Personal Data Protection Act (in Dutch: Wet Bescherming Persoonsgevens)
- WEMWBS
Warwick-Edinburgh Mental Well-being Scale
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of the University Medical center Groningen on the 12th of May 2017 (M17.212189). All participants have to sign inform consent after having received oral and written information about the study and procedures. Participants are informed that they can withdraw their consent at any time without disclosing reasons and without negative consequences for their future care. The researcher can decide to withdraw a subject from the study for urgent medical reasons.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
S. D. M. van Dijk, Phone: +31 50 3611312, Email: S.d.m.van.dijk@umcg.nl
M. S. Veenstra, Email: M.s.veenstra@umcg.nl
R. Bouman, Email: R.bouman@umcg.nl
J. Peekel, Email: J.Peekel@mediant.nl
D. H. Veenstra, Email: Dorothee.Veenstra@vanandel.nl
P. J. van Dalen, Email: P.van.dalen@dimence.nl
A. D. I. van Asselt, Email: A.d.i.van.asselt@umcg.nl
M. L. Boshuisen, Email: M.boshuisen@lentis.nl
S. P. J. van Alphen, Email: B.van.alphen@mondriaan.eu
R. H. S. van den Brink, Email: R.h.s.van.den.brink@umcg.nl
R. C. Oude Voshaar, Email: R.c.oude.voshaar@umcg.nl
References
- 1.Schuster JP, Hoertel N, Le Strat Y, Manetti A, Limosin F. Personality disorders in older adults: findings from NESARC. Am J Geriatr Psychiatry. 2013;21:757–768. doi: 10.1016/j.jagp.2013.01.055. [DOI] [PubMed] [Google Scholar]
- 2.Van Alphen SP, Engelen GJ, Kuin Y, Derksen JJ. The relevance of a geriatric sub-classification of personality disorders in the DSM-V. Int J Geriatr Psychiatry. 2006;21:205–209. doi: 10.1002/gps.1451. [DOI] [PubMed] [Google Scholar]
- 3.Thompson LW, Gallagher D, Czirr R. Personality disorder and outcome in the treatment of late-life depression. J Geriatr Psychiatry. 1988;21:133–153. [PubMed] [Google Scholar]
- 4.Molinari V, Marmion J. Personality disorders in geropsychiatric outpatients. Psychol Rep. 1993;73:256–258. doi: 10.2466/pr0.1993.73.1.256. [DOI] [PubMed] [Google Scholar]
- 5.Soeteman DI, Hakkaart-van Roijen L, Verheul R, Busschbach JJ. The economic burden of personality disorders in mental health care. J Clin Psychiatry. 2008;69:259–265. doi: 10.4088/JCP.v69n0212. [DOI] [PubMed] [Google Scholar]
- 6.Van Asselt ADI, Dirksen CD, Arntz A, Severens JL. The cost of borderline personality disorder: societal costs of illness in BPD patients. Eur Psychiatry. 2007;22:354–361. doi: 10.1016/j.eurpsy.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Friedman B, Veazie PJ, Chapman BP, Manning WG, Duberstein PR. Is personality associated with health care use by older adults? Milbank Quarterly. 2013;91:491–527. doi: 10.1111/1468-0009.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Powers A, Strube MJ, Oltmanns TF. Personality pathology and increased use of medical resources in later adulthood. Am J Geriatr Psychiatry. 2014;22:1478–1486. doi: 10.1016/j.jagp.2013.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Alphen SP, van Dijk SDM, Videler AC, Rossi G, Dierckx E, Bouckaert F, Voshaar RC. Personality disorders in older adults: emerging research issues. Curr Psychiatry Rep. 2015;17:538. doi: 10.1007/s11920-014-0538-9. [DOI] [PubMed] [Google Scholar]
- 10.Balsis S, Woods CM, Gleason ME, Oltmanns TF. Over and underdiagnosis of personality disorders in older adults. Am J Geriatr Psychiatry. 2007;15:742–753. doi: 10.1097/JGP.0b013e31813c6b4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stoffers JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Psychological therapies for people with borderline personality disorder (review) Cochrane Database Syst Rev. 2012;15:8. doi: 10.1002/14651858.CD005652.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brettschneider C, Riedel-Heller S, König HH. A systematic review of economic evaluations of treatments for borderline personality disorder. PLoS One. 2014;9:e107748. doi: 10.1371/journal.pone.0107748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Young JE, Klosko JS, Weishaar MA. Schema Therapy: A Practitioner’s Guide. Guilford Publications; 2014;9(9). https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0107748.
- 14.Bamelis LL, Evers SM, Spinhoven P, Arntz A. Results of a multicentre randomized controlled trial of the clinical effectiveness of schema therapy for personality disorders. Am J Psychiatry. 2014;171:305–322. doi: 10.1176/appi.ajp.2013.12040518. [DOI] [PubMed] [Google Scholar]
- 15.Masley SA, Gillanders DT, Simpson SG, Taylor MA. A systematic review of the evidence base for schema therapy. Cogn Behav Ther. 2012;41:185–202. doi: 10.1080/16506073.2011.614274. [DOI] [PubMed] [Google Scholar]
- 16.Kewes SA, Samson RA, Simpson SG, van Vreeswijk M. Short-term group schema therapy for mixed personality disorders: a pilot study. Front Psychol. 2015;5:1592. doi: 10.3389/fpsyg.2014.01592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang AX, Delucchi K, Dunn LB, Nelson JC. A review and meta-analysis of psychotherapy for late-life depression. Am J Geriatr Psychiatry. 2015;23:261. doi: 10.1016/j.jagp.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Van Vreeswijk MF, Spinhoven P, Eurelings-Bontekoe EH, Broersen J. Changes in symptom severity, schemas and modes in heterogeneous psychiatric patient groups following short-term schema cognitive-behavioural group therapy: a naturalistic pre-treatment and post-treatment design in an outpatient clinic. Clin Psychol Psychother. 2014;21:29–38. doi: 10.1002/cpp.1813. [DOI] [PubMed] [Google Scholar]
- 19.Broersen J, van Vreeswijk M. Schema therapy in groups: a short-term schema CBT protocol. In: Van Vreeswijk M, Broersen J, Nadort M, editors. The Wiley-Blackwell Handbook of Schema Therapy: Theory, Research and Practice. Chichester: Wiley-Blackwell; 2012. pp. 373–381. [Google Scholar]
- 20.Bamelis LL, Evers SM, Spinhoven P, Arntz A. Results of a multicenter randomized controlled trial of the clinical effectiveness of schema therapy for personality disorders. Am J Psychiatry. 2014;171(3):305–322. doi: 10.1176/appi.ajp.2013.12040518. [DOI] [PubMed] [Google Scholar]
- 21.Videler AC, Rossi G, Schoevaars M, van der Feltz-Cornelis CM, van Alphen SP. Effects of schema group therapy in older outpatients: a proof of concept study. Int Psychogeriatr. 2014;26:1709–1717. doi: 10.1017/S1041610214001264. [DOI] [PubMed] [Google Scholar]
- 22.Kindynis S, Burlacu S, Louville P, Limosin F. Effect of schema-focused therapy on depression, anxiety and maladaptive cognitive schemas in the elderly. Encéphale. 2013;39:393–400. doi: 10.1016/j.encep.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Newton-Howes G, Tyrer P, Johnson T, Mulder R, Kool S, Dekker J, Schoevers R. Influence of personality on the outcome of treatment of depression: systematic review and meta-analysis. J Personal Disord. 2014;28:577–593. doi: 10.1521/pedi_2013_27_070. [DOI] [PubMed] [Google Scholar]
- 24.Wetzelaer P, Farrell J, Evers SM, Jacob GA, Lee CW, Brand O, van Breukelen G, Fassbinder E, Fretwell H, Harper RP, Lavender A, Lockwood G, Malogiannis IA, Schweiger U, Startup H, Stevenson T, Zarbock G, Arntz A. Design of an international multicentre RCT on group schema therapy for borderline personality disorder. BMC Psychiatry. 2014;14:319. doi: 10.1186/s12888-014-0319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Videler AC, van Alphen SPJ, van Royen RJJ, van der Feltz-Cornelis CM, Rossi G, Arntz A. Schema therapy for personality disorders in older adults: a multiple-baseline study. Aging Ment Health. 2017;21:1–10. doi: 10.1080/13607863.2016.1262822. [DOI] [PubMed] [Google Scholar]
- 26.Renn BN, Areán PA. Psychosocial treatment options for major depressive disorder in older adults. Curr Treat Options Psychiatry. 2017;4(1):1–12. doi: 10.1007/s40501-017-0100-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knapp M, Patel A, Curran C, Latimer E, Catty J, Becker T, Drake RE, Fioritti A, Kilian R, Lauber C, Rössler W, Tomov T, van Busschbach J, Comas-Herrera A, White S, Wiersma D, Burns T. Supported employment: cost-effectiveness across six European sites. World Psychiatry. 2013;12(1):60–68. doi: 10.1002/wps.20017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blokland-Vos J, Günther G, Van Mook C. Je vak in schema’s. Deel 1: Vaktherapie binnen een kader van schematherapie 2008;2:17.
- 29.Balsis S, Gleason MEJ, Woods CM, Oltmanns TF. An item response theory analysis of DSM-IV personality disorder criteria across younger and older age groups. Psychol Aging. 2007;22:171–185. doi: 10.1037/0882-7974.22.1.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oltmanns TF, Balsis S. Personality disorders in later life: questions about the measurement, course, and impact of disorders. Annu Rev Clin Psychol. 2011;7:321–349. doi: 10.1146/annurev-clinpsy-090310-120435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.First MB, Williams JBW, Benjamin LS, Spitzer RL. User’s guide for the SCID-5-PD (structured clinical interview for DSM-5 personality disorder) Arlington: American Psychiatric Association; 2015. [Google Scholar]
- 32.Carson N, Leach L, Murphy KJ. A re-examination of Montreal cognitive Assessement (MoCA) cutoff scores. Int J Geriatr Psychiatry. 2018;33(2):379–388. doi: 10.1002/gps.4756. [DOI] [PubMed] [Google Scholar]
- 33.Derogatis LR. Brief symptom inventory. Baltimore: Clinical Psychometric Research; 1975. [Google Scholar]
- 34.Farrell JM, Shaw IA, Webber MA. A schema-focussed approach to group psychotherapy for outpatients with borderline personality disorder: a randomized controlled trial. J Behav Ther Exp Psychiatry. 2009;40:317–328. doi: 10.1016/j.jbtep.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Suresh KP. J Hum Reprod Sci. 2011;4:8–11. doi: 10.4103/0974-1208.82352. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Van Vreeswijk M, Broersen J. Kortdurende schemagroepstherapie; Cognitief gedragstherapeutische technieken. Houten: Bohn Stafleu van Loghum; 2012. [Google Scholar]
- 37.Van Vreeswijk M, Broersen J. Handboek Experientiele technieken. Houten: Bohn Stafleu van Loghum; 2017. [Google Scholar]
- 38.Van Vreeswijk M, Broersen J. Werkboek Experientiele technieken. Houten: Bohn Stafleu van Loghum; 2017. [Google Scholar]
- 39.Laidlaw K, Kishita N. Age appropriate augmented CBT for enhancing treatment outcome with older people. Geropsych J Gerontopsychol Geriatric Psychiatry. 2015;28(2):57–66. [Google Scholar]
- 40.Lynch TR, Cheavens JS, Cukrowicz KC, Thorp SR, Bronner L, Beyer J. Treatment of older adults with co-morbid personality disorder and depression: a dialectical behavior therapy approach. Int J Geriatr Psychiatry. 2007;22(2):131–143. doi: 10.1002/gps.1703. [DOI] [PubMed] [Google Scholar]
- 41.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 42.De Beurs E. Leiden: PITS. 2011. Brief symptom inventory: Dutch manual. [Google Scholar]
- 43.Van Alphen SPJ, Bolwerk N, Videler AC, Tummers JHA, van Royen RJJ, Barendse HPJ, Verheul R, Rosowsky E. Age related aspects and clinical implications of diagnosis and treatment of personality disorders in older adults. Clin Gerontol. 2012;35:27–41. doi: 10.1080/07317115.2011.628368. [DOI] [Google Scholar]
- 44.van Asselt AD, Dirksen CD, Arntz A, Giesen-Bloo JH, Severens JL. The EQ-5D: a useful quality of life measure in borderline personality disorder? Eur Psychiatry. 2009;24(2):79–85. doi: 10.1016/j.eurpsy.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 45.Zorginstituut. Richtlijn voor het uitvoeren van economische evaluaties in de gezondheidszorg, 17 november 2015.
- 46.Goossens ME, Rutten-van Mölken MP, Vlaeyen JW, van der Linden SM. The cost diary: a method to measure direct and indirect costs in cost-effectiveness reasearch. J Clin Epidemiol. 2000;53:688–695. doi: 10.1016/S0895-4356(99)00177-8. [DOI] [PubMed] [Google Scholar]
- 47.Van den Brink M, van den Hout WB, Stiggelbout AM, van de Velde CJ, Kievit J. Self-reports of health-care utilization: diary or questionnaire? Int J Technol Assess Health Care. 2005;21:298–304. doi: 10.1017/S0266462305050397. [DOI] [PubMed] [Google Scholar]
- 48.Severens JL, Mulder J, Laheij RJ, Verbeek AL. Precision and accuracy in measuring absence from work as a basis for calculating productivity costs in the Netherlands. Soc Sci Med. 2000;51:243–249. doi: 10.1016/S0277-9536(99)00452-9. [DOI] [PubMed] [Google Scholar]
- 49.Bouwmans C, Krol M, Severens H, Koopmanschap M, Brouwer W, Hakkaart-van Roijen L. The iMTA productivity cost questionnaire: A Standardized Instrument for Measuring and Valuing Health-Related Productivity Losses. Value Health. 2015;18(6):753–758. doi: 10.1016/j.jval.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 50.Cantril H. The pattern of human concerns. New Brunswick: Rutgers University Press; 1965. [Google Scholar]
- 51.Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, Parkinson J, Secker J, Sterward- Brown S. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Quality Life Outcomes. 2007;5:63. doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Keyes CLM. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consul Clin Psychol. 2005;73:539–548. doi: 10.1037/0022-006X.73.3.539. [DOI] [PubMed] [Google Scholar]
- 53.Verheul R, Andrea H, Berghout CC, Dolan C, Busschbach JJ, van der Kroft PJ, Bateman AW, Fonagy P. Severity indices of personality problems (SIPP-118): development, factor structure, reliability, and validity. Psychol Assess. 2008;20:23–34. doi: 10.1037/1040-3590.20.1.23. [DOI] [PubMed] [Google Scholar]
- 54.Rossi G, Debast I, van Alphen SPJ. Measuring personality functioning in older adults: construct validity of the severity indices of personality problems – short form (SIPP-SF) Aging Ment Health. 2017;21(7):703–711. doi: 10.1080/13607863.2016.1154012. [DOI] [PubMed] [Google Scholar]
- 55.Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, Stewart A. The multidimensional assessment of interoceptive awareness (MAIA). The multidimensional assessment of interoceptive awareness (MAIA) PLoS One. 2012;7:11. doi: 10.1371/journal.pone.0048230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bornemann B, Herbert BM, Mehling WE, Singer T. Differential changes in self-reported aspects of interoceptive awareness through 3 months of contemplative training. Front Psychol. 2015;6(5):1504. doi: 10.3389/fpsyg.2014.01504.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tsanas A, Saunders KE, Bilderbeck AC, Palmius N, Osipov M, Clifford GD, Goodwin GΜ, De Vos M. Daily longitudinal self-monitoring of mood variability in bipolar and borderline personality disorder. J Affect Dis. 2016;205:225–233. doi: 10.1016/j.jad.2016.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alders P, Comijs HC, Deeg DJH. Changes in admission to long-term care institutions in the Netherlands: comparing two cohorts over the period 1996-1999 and 2006-2009. Eur J Ageing. 2017;14:123–131. doi: 10.1007/s10433-016-0393-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kriegsman DM, Penninx BW, van Eijk JT, Boeke AJ, Deeg DJ. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients' self-reports and on determinants of inaccuracy. J Clin Epidemiol. 1996;49:1407–1417. doi: 10.1016/S0895-4356(96)00274-0. [DOI] [PubMed] [Google Scholar]
- 60.Vermeulen-Smit E, Ten Have M, Van Laar M, De Graaf R. Clustering of health risk behaviours and the relationship with mental disorders. J Affect Dis. 2015;171:111–119. doi: 10.1016/j.jad.2014.09.031. [DOI] [PubMed] [Google Scholar]
- 61.Conigliaro J, Lofgren RP, Hanusa BH. Screening for problem drinking. Impact on physician behavior and patient drinking habits. J Gen Intern Med. 1998;13(4):251–256. doi: 10.1046/j.1525-1497.1998.00075.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.De Young CG, Carey BE, Krueger RF, Ross SR. Ten aspects of the big five in the personality inventory for DSM-5. Personal Disord. 2016;7(2):113–123. doi: 10.1037/per0000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thimm JC, Jordan S, Bach B. The personality inventory for DSM-5 short form (PID-5-SF): psychometric properties and association with big five traits and pathological beliefs in a Norwegian population. BMC Psychol. 2016;4:61. doi: 10.1186/s40359-016-0169-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van den Broeck J, Bastiaansen L, Rossi G, Dierckx E, De Clercq B. Age- neutrality of the trait facets proposed for personality disorders in DSM-5: a DIFAS analysis of the PID-5. Jof Psychopathol Behav Assess. 2013;35:487–494. doi: 10.1007/s10862-013-9364-3. [DOI] [Google Scholar]
- 65.Young JE, Brown G. Young Schema-Questionnaire. In: ). In; Young JE, editor. Cognitive therapy for personality disorders: A schema-focused approach. 2. Sarasota: Professional Resource Press; 1994. [Google Scholar]
- 66.Sterk F, Rijkeboer M. Schema-Vragenlijst. Utrecht: Ambulatorium Universiteit Utrecht; 1997. [Google Scholar]
- 67.Young JE. Schema therapy: a practitioner’s guide. New York: The Guilford Press; 2003. [Google Scholar]
- 68.Rijkeboer MM, van den Bergh H, van den Bout J. Stability and discriminative power of the Young Schema questionnaire. J Behav Ther Exp Psychiat. 2005;36:129–144. doi: 10.1016/j.jbtep.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 69.Lobbestael J, van Vreeswijk MF, Arntz A, Spinhoven P, ‘t Hoen T. Dutch translation of the Young Atkinson mode inventory (YAMI) Maastricht: Maastricht University; 2005. [Google Scholar]
- 70.Lobbestael J, van Vreeswijk M, Spinhoven P, Schouten E, Arntz A. Reliability and validity of the short Schema mode inventory (SMI) Behav Cogn Psychother. 2010;38:437–458. doi: 10.1017/S1352465810000226. [DOI] [PubMed] [Google Scholar]
- 71.Twisk JWR. Applied longitudinal data analysis for epidemiology. A practical guide. Cambridge: Cambridge University Press; 2003. [Google Scholar]
- 72.Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, Orlewska E, Penna P, Rodriguez Barrios JM, Shau WY. Budget impact analysis principles of good practice: report ofthe ISPOR 2012 budget impact analysis good practice II task force. Value Health. 2014;17(1):5–14. doi: 10.1016/j.jval.2013.08.2291. [DOI] [PubMed] [Google Scholar]
- 73.Thompson LW, Powers DV, Coon DW, Takagi K, McKibbin C, Gallagher-Thompson D. In: Cognitive behavioural group therapy: for specific problems and populations. White JR, Freeman AS, editors. Washington DC: American Psychological Association; 2000. [Google Scholar]
- 74.Arrow H, Poole MS, Henry KB, Wheelan S, Moreland R. Time, change, and development: the temporal perspective on groups. Small Group Res. 2004;35:73–105. doi: 10.1177/1046496403259757. [DOI] [Google Scholar]
- 75.Haight B, Gibson F. Burnsides working with older adults: group process and techniques. 4. Boston: Jones and Bartlett; 2005. [Google Scholar]
- 76.Vos T, Haby MM, Magnus A, Mihalopoulos C, Andrews G, Carter R. Assessing cost-effectiveness in mental health: helping policy-makers prioritize and plan health services. Aust N Z J Psychiatry. 2005;39:701–712. doi: 10.1080/j.1440-1614.2005.01654.x. [DOI] [PubMed] [Google Scholar]
- 77.Zimmerman JA, Fiske A, Scogin F. Mentoring in clinical Geropsychology: across the stages of professional development. Educ Gerontol. 2011;37(5):355–369. doi: 10.1080/03601277.2011.553556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Moore M, Byng R, Stuart B, Harris T, Kendrick T. 'Watchful waiting' or 'active monitoring' in depression management in primary care: exploring the recalled content of general practitioner consultations. J Affect Disord. 2013;15(145(1)):120–125. doi: 10.1016/j.jad.2012.04.042. [DOI] [PubMed] [Google Scholar]
- 79.Zhipei ZLZ, Jiangling JWL, Xinyi C, Zhirui Z, Tiansong Z, Chunbo L. Comparison of psychological placebo and waiting list control conditions in the assessment of cognitive behavioral therapy for the treatment of generalized anxiety disorder: a meta-analysis. Shanghai Arch Psychiatry. 2014;26(6):319–331. doi: 10.11919/j.issn.1002-0829.214173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gould RL, Coulson MC, Howard RJ. Efficacy of cognitive behavioral therapy for anxiety disorders in older people: a meta-analysis and meta-regression of randomized controlled trials. J Am Geriatr Soc. 2012;60(2):218–229. doi: 10.1111/j.1532-5415.2011.03824.. [DOI] [PubMed] [Google Scholar]
- 81.Lenze EJ, Wetherel JL. A lifespan view of anxiety disorders. Dialogues Clin Neurosci. 2011;13(4):381–399. doi: 10.31887/DCNS.2011.13.4/elenze. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gunderson JG, Stout RL, Shea MT, Grilo CM, Markowitz JC, Morey LC, Sanislow C, Yen S, Zanarini MC, Keuroghlian AS, McGlashan TH, Skodol AE. Interactions of borderline personality disorder and mood disorders over 10 years. J Clin Psychiatry. 2014;75(8):829–834. doi: 10.4088/JCP.13m08972. [DOI] [PubMed] [Google Scholar]
- 83.Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, Kremers I, Nadort M, Arntz Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry. 2006;63:649–655. doi: 10.1001/archpsyc.63.6.649. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The proposed study will be using the data-management infrastructure of the University Center for Psychiatry (UMCG), which is a well-equipped, integrated system that meets current guidelines and regulations. After the main outcome and cost-effectiveness analysis have been published, all data will be freely available for other groups.