Abstract
Objective
To assess the long-term, health-related quality of life of intensive care unit survivors by systematic review.
Methods
The search for, and selection and analysis of, observational studies that assessed the health-related quality of life of intensive care unit survivors in the electronic databases LILACS and MEDLINE® (accessed through PubMed) was performed using the indexed MESH terms "quality of life [MeSH Terms]" AND "critically illness [MeSH Terms]". Studies on adult patients without specific prior diseases published in English in the last 5 years were included in this systematic review. The citations were independently selected by three reviewers. Data were standardly and independently retrieved by two reviewers, and the quality of the studies was assessed using the Newcastle-Ottawa scale.
Results
In total, 19 observational cohort and 2 case-control studies of 57,712 critically ill patients were included. The follow-up time of the studies ranged from 6 months to 6 years, and most studies had a 6-month or 1-year follow up. The health-related quality of life was assessed using two generic tools, the EuroQol and the Short Form Health Survey. The overall quality of the studies was low.
Conclusions
Long-term, health-related quality of life is compromised among intensive care unit survivors compared with the corresponding general population. However, it is not significantly affected by the occurrence of sepsis, delirium, and acute kidney injury during intensive care unit admission when compared with that of critically ill patient control groups. High-quality studies are necessary to quantify the health-related quality of life among intensive care unit survivors.
Keywords: Quality of life, Critical illness, Critical care, Intensive care units, Length of stay
INTRODUCTION
Technological advances in the intensive care have increasingly reduced intensive care unit (ICU) mortality.(1) However, the consequences of a critical illness can persist for a long time, affecting the physical, cognitive and mental health of ICU survivors.(2)The multiplicity of these consequences was recognized as "postintensive care syndrome" and may have a strong, negative impact on functioning and on health-related quality of life (HRQOL).(2)
Assessing outcomes related to physical and psychological factors, functional status, social interaction and HRQOL is as important as assessing the long-term mortality rate of ICU survivors.(3,4) Ideally, ICU survivors should reach their premorbidity and/ or admission HRQOL scores or even reach scores that are better than or similar to those of age-, sex- and comorbidity-matched individuals.(5)
Although HRQOL scores are increasingly included in studies and recognized as important outcome parameters in this population, such results generate inaccuracy in their interpretation for various reasons. First, the period during which HRQOL recovery should occur in not defined, and therefore, the optimal follow-up period for HRQOL evaluation remains undetermined. Frequently, postintensive care syndrome may clinically manifest as not only transient events,(6,7) occurring 5 years after hospital discharge,(8) but also permanent events, at least for some survivors. Second, baseline HRQOL evaluation is difficult, thus complicating critical illness burden investigations. In addition, the evaluation instruments used in the studies are different, thereby complicating the systematization and interpretation of HRQOL results. However, a better understanding of how much intensive care affects the long-term HRQOL of ICU survivors is necessary to help healthcare professionals in making decisions on future efforts to reduce the burden of critical illness.
The objective of this study was to perform a systematic review, evaluation and synthesis of observational studies published in the literature on the long-term HRQOL of ICU survivors in comparison with the corresponding general population and control groups.
METHODS
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Guidelines (PRISMA). (9) A systematic search strategy with the indices "quality of life [MeSH Terms]" AND "critically illness [MeSH Terms]" was used in the electronic databases, Latin American and Caribbean Health Sciences Literature (Literatura Latino-Americana e do caribe em Ciências da Saúde - LILACS) and Medical Literature Analysis and Retrieval System Online (MEDLINE®), which were accessed through PubMed from October 13, 2016, to November 7, 2016.
The titles and abstracts of the articles identified in the search strategy were evaluated based on eligibility criteria (Table 1) by three independent reviewers. Full-text articles were downloaded when the abstract lacked information on inclusion and exclusion criteria. The list of references of the selected articles and the personal files of the researchers were also searched for to identify possible studies that might also meet the eligibility criteria of the study and that might not have been found in the initial search. Any discrepancies between the reviewers were resolved by consensus, and a fourth reviewer assessed the publications in cases of persistent disagreement.
Table 1.
Eligibility criteria for article inclusion and exclusion
| Characteristics | Inclusion | Exclusion |
|---|---|---|
| Patients | Adult (> 18 years) intensive care unit survivors | Patients with specific diseases or undergoing investigation of certain therapies |
| Intervention | None | Any |
| Comparison | General population and/or control group | - |
| Outcome | Health-related quality of life | - |
| Study design | Observational study | Randomized, quasi-experimental, qualitative study, case report, review, thesis, editorial, comment |
| Publication | Language: English; period: last 5 years | - |
Data were independently retrieved from the selected articles by two reviewers. Discrepancies were resolved by consensus or by a third reviewer.
The methodological quality of the studies was evaluated using the Newcastle-Ottawa scale by two independent, previously trained and qualified reviewers. The methodological quality score of the cohort and case-control studies was calculated based on three components: study group selection (0 - 4 points), quality of adjustment for confounding factors (0 - 2 points) and evaluation of exposure or outcome of interest (0 - 3 points). The maximum score was 9 points, which expressed high methodological quality. Discrepancies between the reviewers were resolved by consensus, and another evaluation was performed by a third reviewer in case of persistent disagreement.
RESULTS
Study selection
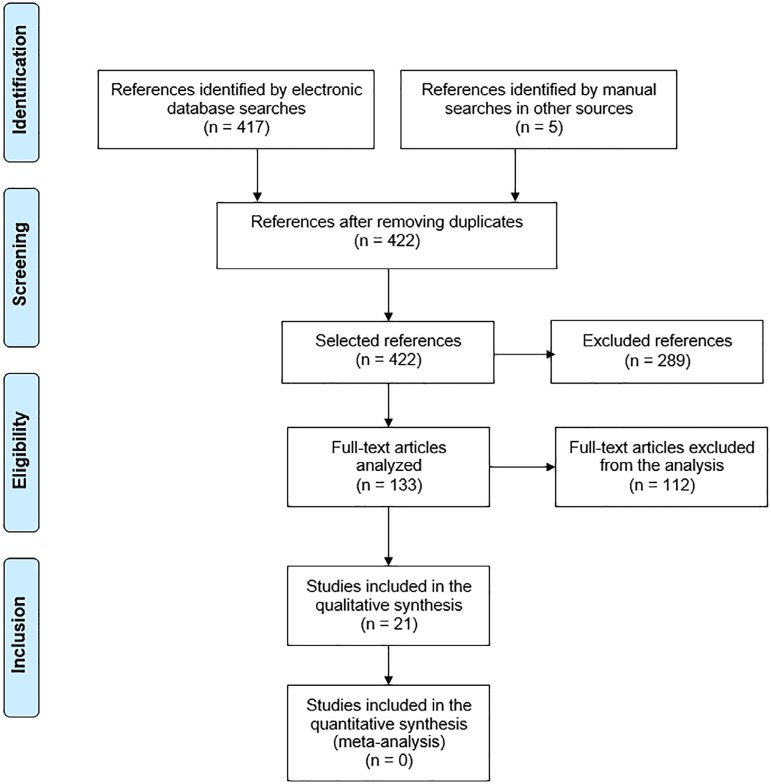
The database searches identified 417 references, and the consultation of other sources identified 5 references. Of these references, 289 were excluded because they were published outside of the 5-year period that was stipulated for this review. Of the other references, 112 were excluded after reading the title and the abstract, and eventually the full text, because they failed to meet the other inclusion criteria (Figure 1). There was no discrepancy in the number of articles selected by the three reviewers, and 21 articles were included.
Figure 1.
Flowchart of the selection of articles according to the inclusion and exclusion criteria.
Characteristics of the included studies
Most studies were conducted in Europe(10-21) and North America,(22-25) followed by Australia,(26,27) China(28) and Argentina.(29) Only one study was conducted in Brazil.(30)All studies were observational prospective cohorts, except four, namely, two retrospective cohorts(12,21)and two case-control studies.(28,30)
The 21 studies included a total of 57,712 critically ill patients, and the individuals were mostly adult, elderly males with varied severity scores on ICU admission. They were classified according to the ICU primary diagnostic groups, such as the following: cardiovascular, respiratory, renal, gastrointestinal, neurological, trauma, orthopedic, surgical, sepsis, hematological, gynecological and metabolic.
Follow-up time and assessment of health-related quality-of-life
The follow-up times of the studies ranged from 6 months to 6 years, and most studies had a 6-month(10,12,14,26,27) or a 1-year follow-up time.(13,15,17,21,23-25,29,30) HRQOL was assessed using two generic instruments, the EuroQol and the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36). The EuroQol version 5D was used in nine studies(12-14,16,19,21,24,29,30) and version 6D in two studies.(15,17) SF-36 was used in 11 studies(10,11,16,18,19,22,23,25-28) and version 12 of the 12-Item Short-Form Health Survey (SF-12) in two studies.(20,24) Long-term HRQOL was evaluated in 24,200 of the 57,712 critically ill patients included in the studies. The patient characteristics of the studies included in this review and the main findings on long-term HRQOL are outlined in table 2.
Table 2.
Patient characteristics for the included studies
| Reference | Country | Study design | Population | n | Age Mean (SD) | Males n (%) | Disease severity Mean (SD) | ICU diagnosis n (%) | Quality of life |
|---|---|---|---|---|---|---|---|---|---|
| Hofhuis et al.(10) | Holland | Prospective 6-month follow-up study | Patients admitted for longer than 48 hours | 749 | ≥ 80 years (n = 129) | 72 (56) | APACHE II: 20 (17 - 24) | Cardiovascular: 34 (26) versus 146
(24) Respiratory: 35 (27) versus 211 (34) Gastrointestinal: 55 (43) versus 207 (33) Neurological: 1 (1) versus 29 (5) Trauma: 2 (2) versus 21 (3) Others: 2 (2) versus 6 (1) |
Most SF-36 dimensions significantly improved over time. Among the octogenarians, the mean SF-36 dimensions 6 months after ICU discharge were similar to the basal and were not significantly lower than those of the normal population |
| < 80 years (n = 620) | 385 (62) | APACHE II: 18 (14 - 23) | |||||||
| van den Boogaard et al.(11) | Holland | Prospective 18-month follow-up study | Patients with and without delirium, ICU survivors | 915 | Patients with delirium: 65 (58 - 75) | 101 (60) | APACHE II: 17 (14 - 20) | Surgical: 77 (45) versus 589 (79)
Clinical: 54 (32) versus 77 (10) Trauma: 17 (10) versus 24 (3) Neurological: 23 (14) versus 54 (7) |
Patients with delirium during the ICU stay had a similar adjusted HRQOL evaluation, albeit with significantly more cognitive problems than patients without delirium |
| Patients without delirium: 65 (57 - 72) | 508 (68) | APACHE II: 13 (10 - 16) | |||||||
| Vaara et al.(12) | Finland | 6-month observational retrospective cohort study | ICU patients treated with RRT or not | 24,904 | Patients treated with RRT: 63 (52 - 72) | 1,143 (67.8) | SAPS II: 48 (37 - 62) | Cardiovascular: 330 (20) versus 6,058
(26) Gastrointestinal: 286 (17) versus 3,628 (16) Neurological: 103 (6) versus 4,483 (19) Renal: 269 (16) versus 383 (2) Respiratory: 159 (9) versus 3,135 (13) Trauma: 36 (2) versus 1,534 (7) Others: 467 (28) versus 3,431 (15) |
No clinically significant difference in EQ-5D score was found between patients treated with and without RRT after 6 months of follow up. In addition, a VAS of patients treated with RRT matched the score of patients treated without RRT and that of the general population |
| Patients treated without RRT: 62 (50 - 73) | 14,641 (63.1) | SOFA: 10 (7 - 13) | |||||||
| SAPS II: 33 (23 - 46) | |||||||||
| SOFA: 6 (3 - 8) | |||||||||
| Pavoni et al.(13) | Italy | 1-year observational prospective cohort study | Patients aged 80 years or older | 288 | Clinical: 87 (2) | 77 (27) | Clinical SAPS II: 52.3 (8.8) | Clinical: 54 (19) | The HRQOL of clinical and orthopedic elderly patients was worse than the HRQOL of surgical patients and of the normal population 1 year after ICU hospitalization |
| Planned abdominal surgery: 87 (1.5) | Planned abdominal surgery (AS): 30.2 (5.4) | Surgical: 74 (26) | |||||||
| Unplanned abdominal surgery: 88 (2.2) | Unplanned AS: 46.5 (6.2) | Orthopedic: 160 (55) | |||||||
| Orthopedic surgery: 85.9 (4.2) | Orthopedic surgery: 24.2 (7.2) | ||||||||
| Orwelius et al.(14) | Portugal | Prospective, multicenter, 6-month follow-up study | Adults ≥ 18 years with ICU stay > 48 hours | 313 | With community-acquired sepsis: 60 (50 - 70) | 59 (65) | SAPS II (IQR): 41 (34 - 51) | Noncoronary: 69 (76) versus 95 (43)
Coronary: 1 (1) versus 12 (5) Trauma: 3 (3) versus 46 (21) Elective surgery: 0 (0) versus 35 (16) Nonelective surgery: 18 (20) versus 34 (15) |
The long-term HRQOL of patients with community-acquired sepsis were not significantly different compared with ICU patients admitted for other diagnoses. However, when compared with the general population, the HRQOL of patients with sepsis showed a clinically significant decrease |
| Without community-acquired sepsis: 59 (43 - 71) | 124 (56) | SAPS II (IQR): 35 (27 - 44) | |||||||
| Wolters et al.(15) | Holland | 1-year prospective observational cohort study | Patients hospitalized at the ICU for longer than 24 hours | 1,101 | Patients with delirium: 60.5 (16.7) | 271 (66) | APACHE IV: 73.7 (28.3) | Clinical: 222 (54) versus 208 (30)
Elective surgery: 96 (23) versus 351 (51) Acute surgery: 94 (23) versus 130 (19) |
Delirium during ICU stay is not independently associated with the HRQOL of ICU survivors when adjusted for factors such as severity of illness during ICU stay |
| Patients without delirium: 59.4 (16.6) | 406 (59) | APACHE IV: 53.9 (22.4) | |||||||
| Oeyen et al.(16) | Belgium | 4-year prospective observational cohort study | Patients admitted to the ICU with AKI treated with RRT matched with patients without AKI-TRS | 141 | Patients with AKI-RRT: 57 (45 - 69) | 31 (66) | APACHE II: 26 (21 - 31) | Clinical: 32 (68) versus 67 (71)
Elective surgery: 1 (2) versus 4 (4) Emergency surgery: 10 (21) versus 18 (19) Trauma: 3 (6) versus 4 (4) Burn: 1 (2) versus 1 (1) |
The long-term QOL of survivors of critical illness with AKI-RRT was similar to that of patients without AKI-RRT, albeit lower than that of the general population |
| Patients without AKI-RRT: 57 (48 - 70) | 62 (66) | APACHE II: 24 (20 - 30) | |||||||
| Soliman et al.(17) | Holland | 1-year prospective cohort study | All ICU patients | 5,934 | 64 (52 - 73) | 3.710 (62) | APACHE IV: 49 (35 - 68) | Heart surgery: 2.162 (36) Sepsis: 556 (9) Subarachnoid hemorrhage: 359 (6) Traumatic brain injury: 327 (6) Others: 2.530 (43) |
The HRQOL 1 year after ICU hospitalization was significantly lower than that of the sex- and aged-matched general population. However, the 1-year HRQOL markedly varied by ICU survivor subgroup |
| Hofhius et al.(18) | Holland | 5-year prospective cohort study | ICU Patients for longer than 48 hours | 749 | 71 (62 - 77) | 457 (61) | APACHE II: 19 (14 - 23) | Cardiovascular: 184 (25) Respiratory: 244 (33) Gastrointestinal: 259 (35) Neurological: 30 (4) Trauma: 23 (3) Others: 9 (1) |
After correcting for natural decline, the HRQOL significantly decreased, and the physical functioning, social functioning and general health dimensions remained significantly lower than those of the age-matched general population, albeit with small effect sizes |
| Cuthbertson et al.(19) | Scotland | 5-year, multicenter, prospective cohort study | Patients with severe sepsis | 439 | 58 (45 - 67) | 234 (53) | APACHE II: 23 (17 - 28) | Respiratory: 138 (31)
Cardiovascular: 124 (28) Neurological: 44 (10) Gastrointestinal: 93 (21) Other: 26 (7) Unknown: 14 (3) |
Patients with severe sepsis have a significantly lower physical dimension of HRQOL than the normal population, although the mental dimension was slightly lower than the normative data up to 5 years after severe sepsis |
| SAPS II: 41 (30 - 54) | |||||||||
| Battle et al.(20) | United Kingdom | 2-year, observational, prospective cohort study | Patients with sepsis | 50 Group SIRS: (n = 19) | 58 (30) | 23 (46) | SOFA: 3 (4) | Respiratory: 18 (36)
Gastrointestinal: 9 (18) Neurological: 1 (2) Endocrine: 10 (20) Renal: 8 (16) Others: 4 (8) |
The HRQOL of patients with sepsis was significantly lower than local, normative data. More significant decreases in HRQOL were found in patients with septic shock than in patients with SIRS and sepsis |
| Group sepsis: (n = 16) | Charlson Comorbidity Index: 3 (4) | ||||||||
| Septic shock group: (n = 15) | |||||||||
| Honselmann et al.(21) | Germany | 1-year retrospective cohort study | Patients with pneumonia and/or sepsis | 217 | 71 (62 - 78) | 134 (62) | SAPS II: 36 (28 - 50) | Sepsis: 145 (67) Pneumonia: 72 (33) Sepsis and pneumonia: 99 (46) |
The HRQOL of patients with pneumonia and/or sepsis was significantly lower than that of the local reference group |
| Fan et al.(22) | United States | 2-year, multisite, prospective study with longitudinal follow-up | Patients under MV with ALI | 222 | 49 (40 - 58) | 123 (55) | APACHE II: 23 (19 - 28) | Pneumonia: 112 (50) Sepsis: 44 (20) Aspiration: 29 (13) Trauma: 7 (3) Others: 30 (14) |
The physical function was substantially impaired, when compared with the corresponding population in all time points (3, 6, 12 and 24 months), and remained markedly impaired in relation to baseline values estimated before ALI (72% baseline value at 24 months of follow-up), according to the SF-36 questionnaire |
| Heyland et al.(23) | Canada | 1-year multicenter, prospective, observational cohort study | Patients aged 80 years or older admitted to the ICU for less than 24 hours | 610 | 84 (80 - 99) | 338 (55) | APACHE II: 22 (7 - 49) | Cardiovascular: 94 (15) Respiratory: 94 (15) Sepsis: 135 (22) Gastrointestinal: 110 (18) CVA: 27 (4) Neurological: 20 (3) Trauma: 46 (8) Metabolic: 8 (1) Hematological: 18 (3) ABG/ valve replacement: 49 (8) Renal: 2 (0) Gynecological: 1 (0) Orthopedic: 6 (1) |
Octogenarian ICU survivors had significantly lower SF-36 scores in the physical functioning section than those of sex- and age-matched controls in all time points (3, 6, 9 and 12 months). A quarter of them returned to baseline levels of physical functioning at 12 months |
| Bagshaw et al.(24) | Canada | 1-year multicenter, prospective, observational cohort study | ICU patients aged 50 years or older for more than 24 hours | 421 | Frail: 69 (10.1) | 72 (52) | APACHE II 21.3 (6.5) | Surgery: 34 (26) versus 108 (38)
Cardiac arrest: 10 (7) versus 21 (7) Mechanical ventilation: 122 (88) versus 240 (85) Vasoactive drug therapy: 83 (60) versus 146 (52) Renal replacement therapy: 14 (10) versus 33 (12) |
12 months after critical illness, frail patients had a worse HRQOL, both in the EuroQol and in the SF-12 , than nonfrail survivors and the general population |
| Not frail: 66.2 (9.7) | 186 (66) | APACHE II 18.6 (7.1) | |||||||
| Feemster et al.(25) | United States | 1-year prospective, observational cohort study | All patients who visited their primary care unit at least once in the previous year | 11,243 | Outpatient: 64.8 (10.8) | 8.929 (97) | - | Hospital and ICU patients showed clinically significant decreases in SF-36 sections, albeit small and similar between both groups | |
| Hospital patient: 66.0 (10.7) | 1.297 (96) | ||||||||
| ICU patient: 66.8 (9.4) | 649 (97) | ||||||||
| McKinley et al.(26) | Australia | 6-month prospective, observational cohort study | Adult patients subjected to MV for longer than 24 hours and who stayed at the ICU for longer than 48 hours | 195 | 57 (16) | 116 (59) | APACHE II: 18.8 (6.9) | Cardiovascular: 38 (20) Respiratory: 46 (24) Gastrointestinal: 57 (30) Others: 50 (26) |
The mental health score of the SF-36 at 1 week was lower than the mean score of the age-matched population, although it improved within 8 to 26 weeks after hospital discharge |
| McKinley et al.(27) | Australia | 6-month prospective, observational cohort study | Adult ICU patients for longer than 48 hours | 222 | 57.2 (17.2) | 145 (65) | - | Cardiovascular: 81 (37) Respiratory: 13 (6) Gastrointestinal: 20 (9) Neurological: 57 (26) Trauma: 24 (11) Sepsis: 5 (2) Others: 22 (10) |
The mental health and physical functioning scores of the SF-36 were significantly lower in patients with poor sleep quality 6 months after ICU discharge |
| Zhang K et al.(28) | China | 6-year, multicenter, prospective case-control study | Adults, ≥ 18 years, who stayed at the ICU for longer than 24 hours | 224 | Sepsis group: 53 (17.3) | Sepsis group: 32 (76) | APACHE II: 18.3 (6.8) | Cardiovascular: 14 (33) versus 9 (27)
Respiratory: 22 (52) versus 12 (36) Renal: 12 (28) versus 9 (27) Hematological: 9 (21) versus 5 (15) Neurological: 23 (54) versus 16 (48) |
No difference in HRQOL was found between the sepsis and the control groups of critically ill patients. However, when compared the community control group, the patients with severe sepsis showed clinically significant impairment in 4 of the 8 domains of the SF-36 6 years after hospital discharge |
| Control group: 47 (18.1) | Control group: 23 (70) | APACHE II: 13.7 (6.5) | |||||||
| Das Neves et al.(29) | Argentina | 1-year, prospective, observational cohort study | Patients aged 15 years or older who remained under MV for longer than 48 hours | 112 | 33 (24 - 49) | 76 (68) | APACHE II: 15 (6) | Trauma: 56 (50) Traumatic brain injury: 46 (41) Medical: 32 (29) Emergency surgery: 15 (13) Elective Surgery: 9 (8) |
The patients showed high and persistent critical illness burden, severely affecting their HRQOL, which was adversely affected by events such as shock, MV duration and persistent weakness |
| Contrin et al.(30) | Brazil | 1-year, nested case-control study | Patients with severe sepsis | 100 | Control group: 52.2 (19.4) | 24 (48) | _ | Respiratory: 4 (8) versus 11 (22)
Urinary: 3 (6) versus 5 (10) Cardiovascular: 3 (6) versus 4 (8) Nervous: 9 (18) versus 5 (10) Trauma: 6 (12) versus 10 (20) Gastrointestinal: 12 (24) versus 4 (8) Neoplasia: 10 (20) versus 4 (8) Sepsis: 2 (4) versus 1 (2) Metabolic: 0 (0) versus 2 (4) Postoperative: 1 (2) versus 4 (8) |
Elderly patients with sepsis had more moderate and severe problems in all five dimensions of the HRQOL studied than critically ill patients without sepsis |
| Sepsis group: 51.3 (20.0) | 32 (64) | _ |
SD – standard deviation; ICU – intensive care unit; APACHE – Acute Physiology and Chronic Health Evaluation; SF-36 – Medical Outcomes Study 36 - Item Short - Form Health Survey; HRQOL – health-related quality of life; RRT – renal replacement therapy; SAPS – Acute Physiology Score; SOFA – Sequential Organ Failure Assessment; EQ-5D – EuroQol Health Questionnaire; VAS – visual analog scale; IQR – interquartile range; AKI – acute kidney injury; QOL – quality of life; SIRS – systemic inflammatory response syndrome; MV – mechanical ventilation; ALI – acute lung injury; CVA – cerebrovascular accident (stroke); SF-12 – 12-Item Short-Form Health Survey.
In 18 of the 21 studies included in this review, the long-term HRQOL of ICU survivors was compromised when compared with that of the corresponding general population. In studies with a 6-month follow-up time, the HRQOL of critically ill and elderly patients with low severity scores and critically ill patients with acute kidney injury was similar to that of the corresponding general population.(10,12,26)Most HRQOL dimensions improved in the long run.(10,16,18,19,22,24,26,29)The domains related to physical aspects were the most affected.(13,18,19,22,23,27)
Risk of bias in the included studies
The general methodological quality of the studies included in this review was low (Table 3). The Newcastle-Ottawa scores of the studies ranged from 2 to 5; a score lower than 4 indicated limited or low-quality evidence. Consensus was reached on all occasions, and no study was excluded from this review, based on the risk of bias assessed. Meta-analyses could not be performed because the studies included in this review had a predominantly observational cohort design.
Table 3.
Risk of bias for cohort and case-control studies using the Newcastle-Ottawa scale
| Reference | Design | Selection | Comparability | Outcome | Total |
|---|---|---|---|---|---|
| Hofhuis et al.(10) | Prospective cohort study | 2 | 0 | 3 | 5 |
| Van den Boogaard et al.(11) | Prospective cohort study | 2 | 0 | 2 | 4 |
| Vaara et al.(12) | Retrospective cohort study | 2 | 0 | 2 | 4 |
| Pavoni et al.(13) | Prospective cohort study | 2 | 0 | 2 | 4 |
| Orwelius et al.(14) | Prospective cohort study | 2 | 0 | 2 | 4 |
| Wolters et al.(15) | Prospective cohort study | 1 | 0 | 1 | 2 |
| Oeyen et al.(16) | Prospective cohort study | 2 | 1 | 2 | 5 |
| Soliman et al.(17) | Prospective cohort study | 1 | 0 | 1 | 2 |
| Hofhuis et al.(18) | Prospective cohort study | 2 | 0 | 2 | 4 |
| Cuthbertson et al.(19) | Prospective cohort study | 2 | 1 | 1 | 4 |
| Battle et al.(20) | Prospective cohort study | 1 | 0 | 1 | 2 |
| Honselmann et al.(21) | Retrospective cohort study | 1 | 1 | 2 | 4 |
| Fan et al.(22 | Prospective cohort study | 1 | 1 | 2 | 4 |
| Heyland et al.(23) | Prospective cohort study | 2 | 0 | 2 | 4 |
| Bagshaw et al.(24) | Prospective cohort study | 1 | 0 | 2 | 3 |
| Feemster et al.(25) | Prospective cohort study | 2 | 0 | 2 | 4 |
| McKinley et al.(26) | Prospective cohort study | 1 | 0 | 2 | 3 |
| McKinley et al.(27) | Prospective cohort study | 2 | 1 | 2 | 5 |
| Zhang K et al.(28) | Prospective case-control study | 2 | 1 | 1 | 4 |
| Das Neves et al.(29) | Prospective cohort study | 1 | 0 | 2 | 3 |
| Contrin et al.(30) | Nested case-control study | 2 | 0 | 2 | 4 |
Strong evidence – 6/9 consistent findings among several high-quality studies; moderately strong evidence – 4-5/9 consistent findings among several low- and/ or high-quality studies; Limited evidence – < 4 low-quality studies; conflicting evidence – inconsistent findings among multiple studies; no evidence – no evidence among studies.
DISCUSSION
This systematic review describes the long-term HRQOL of ICU survivors. In total, 21 studies were included in this review. The overall quality of the studies was low, according to the Newcastle-Ottawa scale, thus highlighting the need for studies with high methodological quality to determine the long-term HRQOL of ICU survivors. New studies with appropriate methodological designs may provide important data on the main factors that result in their change, as well as on possible therapeutic alternatives.
Critically ill patients
The long-term HRQOL of the critically ill patients differed among the studies analyzed, varying by population and follow-up time. In the short term, the mental component of the HRQOL in a population of critically ill patients with a low severity score was similar to that of the corresponding age-matched population at 8 and 26 weeks after hospital discharge.(26) In a 1-year follow-up, three studies, which were conducted in Holland,(17) Argentina(29) and the United States,(25) highlighted that HRQOL was significantly compromised and that it was even more affected among specific subgroups of ICU survivors, such as those diagnosed with shock who remained under mechanical ventilation for a long period and who showed persistent weakness.(17,29)Conversely, a study that compared the impact on HRQOL between hospital and ICU patients highlighted that HRQOL is clinically impaired in both groups 1 year after discharge, with no significant difference between hospital and ICU patients.(25)
In the 5-year period, after correcting for natural decline, the HRQOL of ICU survivors significantly decreased, and the physical and social functioning and overall health domains of ICU survivors remained significantly lower than those of the age-matched general population.(18) However, the size effect of the HRQOL reduction was weak on all domains of the evaluation instrument, thus suggesting that the ICU admission effect on the perception of HRQOL 5 years after discharge may not be clinically relevant.
Elderly critically ill patients
Among elderly ICU survivors, the HRQOL 1 year after ICU discharge was worse than that of the age-(13) and age- and sex-matched(23) general population. Conversely, in another study(10) with a shorter follow-up time, which was performed in an elderly population with lower severity scores, the HRQOL scores 6 months after ICU discharge were similar both to the scores before ICU admission, which were obtained by a patient representative, and to those of the age-matched general population. In both studies(13,23) that showed impaired HRQOL, physical functioning was the most affected domain. Understandably, elderly ICU survivors show impaired HRQOL given their likely increase in comorbidities, and this impairment was more visible in physical functioning.
Critically ill patients with sepsis
The HRQOL of critically ill patients with sepsis was not significantly different from that of nonelderly critically ill patients with sepsis,(30) of critically ill patients with community-acquired sepsis(14)or of age-, sex- and Charlson comorbidity index-matched critically ill patients without sepsis,(28) both in 6-month(14) and in 1-(30) and 6-year follow-up studies.(28) However, the HRQOL of these patients showed a clinically relevant impairment when compared with the general population.(14,19-21,28) Approximately 50 to 75% patients with sepsis(7) progressed with ICU-acquired muscle weakness, which is one of the main signs of physical function impairment of postintensive care syndrome, versus 25 to 50% patients subjected to mechanical ventilation.(7) However, the short-(14) and long-term(28,30) HRQOL of these patients was not significantly different in comparison with critically ill patients with other diagnoses, thus showing that ICU admission, regardless of diagnosis and patient clinical status, is the determinant of impaired HRQOL in these survivors.
Critically ill patients with delirium
The HRQOL of patients with delirium during their ICU stay was not significantly affected compared with patients without delirium after 12(15) and 18 months of follow-up,(11)although they showed significantly more cognitive problems.(11) Previous studies(31,32) have shown that delirium during an ICU stay is associated with long-term cognitive deficit and mortality, leading to speculation that delirium would also affect the long-term HRQOL, which has not been fully elucidated yet.
Critically ill patients with acute kidney injury treated with renal replacement therapy
Two studies(12,16)investigated the HRQOL of critically ill patients with acute kidney injury treated with renal replacement therapy. Both studies found no long-term HRQOL differences between critically ill patients with acute kidney injury and those without. However, the studies differed when comparing the HRQOL of critically ill patients with acute kidney injury with the HRQOL of the healthy population. Vaara et al.(12) found no differences at 6 months, whereas Oeyen et al.(16) found significant differences after 4 years of follow-up. Importantly, Vaara et al.(12) conducted a retrospective short-term study.
Critically ill patients with acute lung injury
Only one study(22) evaluated the HRQOL of critically ill patients with acute lung injury. In this population, which was evaluated in the United States, the baseline values of the physical functioning component of the HRQOL were substantially lower than those estimated at 2 years of follow-up. A previous and highly relevant study(8) on the subject demonstrated that ICU survivors who developed acute respiratory distress syndrome showed physical and psychological sequelae and a reduced physical function component of the HRQOL 5 years after ICU discharge, corroborating the finding of the study included in this review.
Critically ill patients with poor sleep quality
In individuals with poor sleep quality, the only study published on HRQOL in this population demonstrated that the physical and mental functioning components of the evaluation instrument were significantly lower in these individuals 6 months after ICU discharge.(27) Evidence indicates that low quality of ICU sleep and acute sleep deprivation lead to possible negative effects on recovery in critically ill patients,(33,34) including physical and psychological recovery.
CRITICALLY ILL PATIENTS WITH FRAILTY
Frailty is a multidimensional state characterized by physiological and cognitive loss in older patients, and it predicts adverse events and unfavorable outcomes.(35) Critically ill patients in a state of frailty classified with the Canadian Study of Health and Ageing Clinical Frailty Scale were evaluated in a multicenter cohort in Canada 1 year after ICU admission.(24) These individuals showed worse HRQOL scores than nonfrail individuals and the healthy population.(24) Another study included in this review, performed with elderly people aged 80 years or older, demonstrated that frailty was an independent predictor that was more significant than age, critical illness severity or comorbidities - which are commonly considered key determinants of long-term outcome.(23)
Postintensive care syndrome
A substantial, albeit unknown, proportion of ICU survivors is at risk of developing postintensive care syndrome. Increasing efforts have been made to use the term "postintensive care syndrome" to describe new or aggravated physical, cognitive or mental deficits, resulting from critical illness, that persist after hospitalization,(2,36) with the aim of understanding the epidemiology of this syndrome and its burden on the long-term HRQOL of ICU survivors. Approximately 25 to 50% of patients subjected to mechanical ventilation will develop ICU-acquired muscle weakness,(7) and approximately 85 to 95% of them persist with neuromuscular deficits for 2 to 5 years after hospital discharge.(7) Approximately 30 to 80% patients show cognitive impairment after their ICU stay,(37) and 10 to 50% patients show new depression, anxiety, posttraumatic stress and sleep disorder symptoms.(7) The high and persistent prevalence of changes related to postintensive care syndrome apparently justifies the long-term negative effects on the HRQOL of ICU survivors, and these consequences are more prominent in some specific situations found in the intensive care setting, as shown in this systematic review.
Importantly, the long-term HRQOL assessment presented by these studies clearly disregarded patients who dropped out or died, as only 42% (24,200 patients) of the total sample (57,712) was assessed. We believe that this finding compromises the HRQOL assessment of this population because sample loss may be related to worsened patient clinical status or death.
The search strategy used in electronic databases failed to identify some eligible studies. Previous systematic reviews(38,39) on the subject used broader search strategies such as the following: ("quality of life" OR "health status indicators") AND ("intensive care units" OR "critical care" OR "critical illness" OR "sepsis" OR "adult respiratory distress syndrome") and ("quality of life" OR "long-term outcome") AND ("intensive care" OR "critical care" OR "critically ill patients" OR "ICU patients" OR "critical care patients" OR "ICU stay" OR "ICU"). Dowdy et al.(38) included the terms "sepsis" and "acute respiratory distress syndrome" in the search strategy because an eligible study identified before conducting the search was not identified when using the initial terms. However, we complemented the search in the reference lists of other systematic reviews and relevant publications on the subject.
The scope of this review was comprehensive; therefore, the heterogeneity of the studies was a limitation, precluding their comparison. We chose to broaden our review to better describe the potential burden of ICU hospitalization on long-term HRQOL. Future, high-quality studies in specific populations are necessary to prepare meta-analyses for specific ICU groups.
FINAL CONSIDERATIONS
Long-term, health-related quality of life is compromised among intensive care unit survivors when compared with the corresponding general population. However, long-term, health-related quality of life is not significantly affected by the presence of sepsis, delirium or acute kidney injury during intensive care unit stay when compared with that of critically ill patient control groups. High-quality studies are necessary to quantify the health-related quality of life of intensive care unit survivors.
Footnotes
Conflicts of interest: None.
Responsible editor: Alexandre Biasi Cavalcanti
REFERENCES
- 1.Wunsch H, Guerra C, Barnato AE, Angus DC, Li G, Linde-Zwirble WT. Three-year outcomes for Medicare beneficiaries who survive intensive care. JAMA. 2010;303(9):849–856. doi: 10.1001/jama.2010.216. [DOI] [PubMed] [Google Scholar]
- 2.Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H. Improving long-term outcomes after discharge from intensive care unit report from a stakeholders' conference. Crit Care Med. 2012;40(2):502–509. doi: 10.1097/CCM.0b013e318232da75. [DOI] [PubMed] [Google Scholar]
- 3.Graf J, Koch M, Dujardin R, Kersten A, Janssens U. Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med. 2003;31(8):2163–2169. doi: 10.1097/01.CCM.0000079607.87009.3A. [DOI] [PubMed] [Google Scholar]
- 4.Wu A, Gao F. Long-term outcomes in survivors from critical illness. Anaesthesia. 2004;59(11):1049–1052. doi: 10.1111/j.1365-2044.2004.04011.x. [DOI] [PubMed] [Google Scholar]
- 5.Black NA, Jenkinson C, Hayes JA, Young D, Vella K, Rowan KM. Review of outcome measures used in adult critical care. Crit Care Med. 2001;29(11):2119–2124. doi: 10.1097/00003246-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness postintensive care syndrome-family. Crit Care Med. 2012;40(2):618–624. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 7.Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39(2):371–379. doi: 10.1097/CCM.0b013e3181fd66e5. [DOI] [PubMed] [Google Scholar]
- 8.Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM. Canadian Critical Care Trials Group Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hofhuis JG, van Stel HF, Schrijvers AJ, Rommes JH, Spronk PE. Changes of health-related quality of life in critically ill octogenarians a follow-up study. Chest. 2011;140(6):1473–1483. doi: 10.1378/chest.10-0803. [DOI] [PubMed] [Google Scholar]
- 11.van den Boogaard M., Schoonhoven L., Evers AW., van der Hoeven JG., van Achterberg T., Pickkers P. Delirium in critically ill patients impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. 2012;40(1):112–118. doi: 10.1097/CCM.0b013e31822e9fc9. [DOI] [PubMed] [Google Scholar]
- 12.Vaara ST, Pettilä V, Reinikainen M, Kaukonen KM. Finnish Intensive Care Consortium Population-based incidence, mortality and quality of life in critically ill patients treated with renal replacement therapy a nationwide retrospective cohort study in Finnish intensive care units. Crit Care. 2012;16(1):R13–R13. doi: 10.1186/cc11158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pavoni V, Gianesello L, Paparella L, Buoninsegni LT, Mori E, Gori G. Outcome and quality of life of elderly critically ill patients an Italian prospective observational study. Arch Gerontol Geriatr. 2012;54(2):e193–e198. doi: 10.1016/j.archger.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Orwelius L, Lobo C, Teixeira Pinto A, Carneiro A, Costa-Pereira A, Granja C. Sepsis patients do not differ in health-related quality of life compared with other ICU patients. Acta Anaesthesiol Scand. 2013;57(9):1201–1205. doi: 10.1111/aas.12164. [DOI] [PubMed] [Google Scholar]
- 15.Wolters AE, van Dijk D, Pasma W, Cremer OL, Looije MF, de Lange DW. Long-term outcome of delirium during intensive care unit stay in survivors of critical illness a prospective cohort study. Crit Care. 2014;18(3):R125–R125. doi: 10.1186/cc13929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oeyen S, De Corte W, Benoit D, Annemans L, Dhondt A, Vanholder R. Long-term quality of life in critically ill patients with acute kidney injury treated with renal replacement therapy a matched cohort study. Crit Care. 2015;19:289–289. doi: 10.1186/s13054-015-1004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soliman IW, de Lange DW, Peelen LM, Cremer OL, Slooter AJ, Pasma W. Single-center large-cohort study into quality of life in Dutch intensive care unit subgroups, 1 year after admission, using EuroQoL EQ-6D-3L. J Crit Care. 2015;30(1):181–186. doi: 10.1016/j.jcrc.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Hofhuis JG, van Stel HF, Schrijvers AJ, Rommes JH, Spronk PE. ICU survivors show no decline in health-related quality of life after 5 years. Intensive Care Med. 2015;41(3):495–504. doi: 10.1007/s00134-015-3669-5. [DOI] [PubMed] [Google Scholar]
- 19.Cuthbertson BH, Elders A, Hall S, Taylor J, MacLennan G, Mackirdy F, Mackenzie SJ, Scottish Critical Care Trials Group. Scottish Intensive Care Society Audit Group . Mortality and quality of life in the five years. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Battle CE, Davies G, Evans PA. Long term health-related quality of life in survivors of sepsis in South West Wales an epidemiological study. PLoS One. 2014;9(12):e116304. doi: 10.1371/journal.pone.0116304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Honselmann KC, Buthut F, Heuwer B, Karadag S, Sayk F, Kurowski V. Long-term mortality and quality of life in intensive care patients treated for pneumonia and/or sepsis Predictors of mortality and quality of life in patients with sepsis/pneumonia. J Crit Care. 2015;30(4):721–726. doi: 10.1016/j.jcrc.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Fan E, Dowdy DW, Colantuoni E, Mendez-Tellez PA, Sevransky JE, Shanholtz C. Physical complications in acute lung injury survivors a two-year longitudinal prospective study. Crit Care Med. 2014;42(4):849–859. doi: 10.1097/CCM.0000000000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heyland DK, Garland A, Bagshaw SM, Cook D, Rockwood K, Stelfox HT. Recovery after critical illness in patients aged 80 years or older a multi-center prospective observational cohort study. Intensive Care Med. 2015;41(11):1911–1920. doi: 10.1007/s00134-015-4028-2. [DOI] [PubMed] [Google Scholar]
- 24.Bagshaw SM, Stelfox HT, Johnson JA, McDermid RC, Rolfson DB, Tsuyuki RT. Long-term association between frailty and health-related quality of life among survivors of critical illness a prospective multicenter cohort study. Crit Care Med. 2015;43(5):973–982. doi: 10.1097/CCM.0000000000000860. [DOI] [PubMed] [Google Scholar]
- 25.Feemster LC, Cooke CR, Rubenfeld GD, Hough CL, Ehlenbach WJ, Au DH. The influence of hospitalization or intensive care unit admission on declines in health-related quality of life. Ann Am Thorac Soc. 2015;12(1):35–45. doi: 10.1513/AnnalsATS.201404-172OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKinley S, Aitken LM, Alison JA, King M, Leslie G, Burmeister E. Sleep and other factors associated with mental health and psychological distress after intensive care for critical illness. Intensive Care Med. 2012;38(4):627–633. doi: 10.1007/s00134-012-2477-4. [DOI] [PubMed] [Google Scholar]
- 27.McKinley S, Fien M, Elliott R, Elliott D. Sleep and psychological health during early recovery from critical illness an observational study. J Psychosom Res. 2013;75(6):539–545. doi: 10.1016/j.jpsychores.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 28.Zhang K, Mao X, Fang Q, Jin Y, Cheng B, Xie G. Impaired long-term quality of life in survivors of severe sepsis Chinese multicenter study over 6 years. Anaesthesist. 2013;62(12):995–1002. doi: 10.1007/s00101-013-2257-8. [DOI] [PubMed] [Google Scholar]
- 29.Das Neves AV, Vasquez DN, Loudet CI, Intile D, Sáenz MG, Marchena C. Symptom burden and health-related quality of life among intensive care unit survivors in Argentina A prospective cohort study. J Crit Care. 2015;30(5):1049–1054. doi: 10.1016/j.jcrc.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 30.Contrin LM, Paschoal VD, Beccaria LM, Cesarino CB, Lobo SM. Qualidade de vida de sobreviventes de sepse grave após alta hospitalar. Rev Latino Am Enfermagem. 2013;21(3) doi: 10.1590/S0104-11692013000300020. 8 telas. [DOI] [PubMed] [Google Scholar]
- 31.Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, Brummel NE, Hughes CG, Vasilevskis EE, Shintani AK, Moons KG, Geevarghese SK, Canonico AE, Hopkins RO, Bernard GR, Dittus RS, Ely EW, BRAIN-ICU Study Investigators Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell Jr FE. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 33.Pulak LM, Jensen L. Sleep in the intensive care unit a review. J Intensive Care Med. 2016;31(1):14–23. doi: 10.1177/0885066614538749. [DOI] [PubMed] [Google Scholar]
- 34.Kamdar BB, Needham DM, Collop NA. Sleep deprivation in critical illness its role in physical and psychological recovery. J Intensive Care Med. 2012;27(2):97–111. doi: 10.1177/0885066610394322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi: 10.1016/S0140-6736(12)62167-9. Erratum in Lancet. 2013;382(9901):1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elliott D, Davidson JE, Harvey MA, Bemis-Dougherty A, Hopkins RO, Iwashyna TJ. Exploring the scope of post-intensive care syndrome therapy and care engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med. 2014;42(12):2518–2526. doi: 10.1097/CCM.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 37.Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme Jr JF. Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005;171(4):340–347. doi: 10.1164/rccm.200406-763OC. [DOI] [PubMed] [Google Scholar]
- 38.Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, Herridge MS, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 2005;31(5):611–20. doi: 10.1007/s00134-005-2592-6. Erratum in Intensive Care Med. 2005;31(7):1007. [DOI] [PubMed] [Google Scholar]
- 39.Oeyen SG, Vandijck DM, Benoit DD, Annemans L, Decruyenaere JM. Quality of life after intensive care a systematic review of the literature. Crit Care Med. 2010;38(12):2386–2400. doi: 10.1097/CCM.0b013e3181f3dec5. [DOI] [PubMed] [Google Scholar]