Keywords: nerve regeneration, absent sensory nerve action potential, cubital tunnel syndrome, disease severity, electrodiagnostic testing, in situ decompression, subcutaneous transposition, surgical outcomes, prognostic factors, peripheral nerve compression, neural regeneration
Abstract
For severe cubital tunnel syndrome, patients with absent sensory nerve action potential tend to have more severe nerve damage than those without. Thus, it is speculated that such patients generally have a poor prognosis. How absent sensory nerve action potential affects surgical outcomes remains uncertain owing to a scarcity of reports and conflicting results. This retrospective study recruited one hundred and fourteen cases (88 patients with absent sensory nerve action potential and 26 patients with present sensory nerve action potential) undergoing either subcutaneous transposition or in situ decompression. The minimum follow-up was set at 2 years. Primary outcome measures of overall hand function included their McGowan grade, modified Bishop score, and Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) score. For patients with absent sensory nerve action potential, 71 cases (80.7%) achieved at least one McGowan grade improvement, 76 hands (86.4%) got good or excellent results according to the Bishop score, and the average DASH score improved 49.5 points preoperatively to 13.1 points postoperatively. When compared with the present sensory nerve action potential group, they showed higher postoperative McGowan grades and DASH scores, but there was no statistical difference between the modified Bishop scores of the two groups. Following in situ decompression or subcutaneous transposition, great improvement in hand function was achieved for severe cubital tunnel syndrome patients with absent sensory nerve action potential. The functional outcomes after surgery for severe cubital tunnel syndrome are worse in patients with absent sensory nerve action potential than those without. This study was approved by the Ethical Committee of Huashan Hospital, Fudan University, China (approval No. 2017142).
Chinese Library Classification No. R459.9; R605; R741
Introduction
Electromyography has been widely used and plays an important role in diagnosing cubital tunnel syndrome. Electromyographic results facilitate the confirmation of the diagnosis and assessment of the severity of the disease (Lo et al., 2005; Logigian et al., 2014). Patients with absent sensory nerve action potential (SNAP) are believed to have more severe nerve damage than those who do not and it is reasonable to speculate that these patients would have inferior outcomes after surgery.
Two studies (Matsuzaki et al., 2004; Taha et al., 2004) have analyzed the outcomes of surgical treatment of cubital tunnel syndrome with absent SNAP but no clear trend was found. Taha et al. (2004) conducted a retrospective review of 38 limbs and found that 20 limbs (53%) experienced improved sensory symptoms and 2 limbs (13%) achieved improvement in muscle strength, whereas Matsuzaki et al. (2004) reviewed 15 patients and concluded that satisfactory functional recovery can be expected, with numbness relieved in 14 hands (93.3%) and intrinsic muscle strength reaching grade 4 or 5 in 11 hands (73.3%). Owing to the scarcity of reports and conflicting results, how absent SNAP affects surgical outcomes remains uncertain.
This study aims to evaluate the prognosis of severe cubital tunnel syndrome with absent SNAP and to compare surgical outcomes between patients with absent- or present-SNAP in severe cubital tunnel syndrome.
Subjects and Methods
Subjects
This retrospective study recruited 114 patients who had undergone surgical treatment for cubital tunnel syndrome in Huashan Hospital, China between May 2006 and September 2015. This study was approved by the Ethical Committee of Huashan Hospital, Fudan University, China (approval No. 2017142). All patients signed written informed consent.
Inclusion criteria were: (1) Cubital tunnel syndrome, confirmed by preoperative electromyography (American Association of Electrodiagnostic Medicine, 1999); (2) McGowan grade III (profound sensory disturbance and motor weakness with severe intrinsic atrophy and abnormal finger crossing or claw hand deformity) (McGowan et al., 1950; Goldberg et al., 1989); (3) minimum follow-up of 2 years.
Exclusion criteria were: (1) Revision patients; (2) cervical radiculopathy; (3) carpal tunnel syndrome or other peripheral neuropathies; (4) concomitant conditions such as tendon rupture, hemiplegia, hemodialysis or diabetes mellitus.
Upon searching our departmental electronic medical record system, 127 patients who had undergone surgical treatment for severe cubital tunnel syndrome in Huashan Hospital between August 2006 and December 2014 were identified as eligible. We made attempts to contact all eligible 127 cases, however, six patients could not be reached; 3 patients refused to participate; 2 experienced ruptured extensor tendons secondary to gouty arthritis; and 2 experienced hemiplegia secondary to cerebral infarction, leaving a final study cohort of 114 elbows out of the 127 eligible cases (89.8%). A total of 88 patients had absent SNAP and 26 patients had present SNAP.
Diagnosis of cubital tunnel syndrome
Cubital tunnel syndrome was diagnosed based on clinical findings, with subsequent confirmation using electrophysiological tests. All patients diagnosed with McGowan grade III cubital tunnel syndrome were recommended to have surgery immediately. Clinical findings included sensory disturbance in areas served by the ulnar nerve and motor dysfunction induced by intrinsic muscle atrophy. Electrophysiological tests included sensory and motor conduction velocity measurements and needle electromyography assessments of the muscles innervated by the ulnar nerve. Two senior neurologists performed all electrodiagnostic studies following the guidelines of American Association of Electrodiagnostic Medicine (American Association of Electrodiagnostic Medicine, 1999). Electrophysiological data analyzed in this study include: motor nerve conduction velocity (MNCV) across the elbow, MNCV in the forearm segment, percentage decrease of MNCV from the forearm segment to the elbow segment, compound motor action potential (CMAP) above the elbow, CMAP below the elbow, conduction block, absent SNAP, absent motor nerve action potentials, and spontaneous activity (positive sharp waves and fibrillation potentials) in the first dorsal interosseous, abductor digiti minimi, and flexor carpi ulnaris.
Preoperative baseline data
Preoperative data regarding demographic information and clinical characteristics were retrieved and extracted from the subjects’ electronic medical records. Age, sex, disease duration, surgical procedure, dominant hand, smoking and follow-up time were compared between the patients with absent SNAP and the patients with present SNAP. The Disabilities of the Arm, Shoulder, and Hand questionnaire (DASH) was used to evaluate preoperative overall functionality of the upper extremity.
Surgical procedures
In our institution, patients with elbow angular deformity (elbow osteoarthritis, cubitus valgus and posttraumatic elbows) underwent subcutaneous transposition (Huang et al., 2015). For idiopathic elbows, the choice of either in situ decompression (Gervasio et al., 2005) or subcutaneous transposition was decided between the surgeons and the patients. Three senior hand surgeons performed all procedures using uniform techniques at a single institution.
Postoperative data acquisition
Postoperative data of interest included sensory function (pain), motor function (interosseous muscle strength), and overall function, which was assessed by their McGowan grade, DASH score, and modified Bishop score (Kleinman and Bishop, 1989; Nouhan and Kleinert, 1997). Pain was evaluated using a visual analog scale (VAS) at rest (Watts, 2009), and present or absent residual pain were defined as the presence or absence of postoperative pain, respectively. Interosseous muscle strength was graded clinically using the British Medical Research Council Scale (MRC 0–5) (Seddon, 1954). A lower McGowan grade, lower DASH score, higher modified Bishop score, lower pain VAS, and higher interosseous muscle strength all indicate better hand function.
Statistical analysis
Statistical analysis was performed using SPSS 23.0 software (IBM, Armonk, NY, USA). Continuous data are expressed as the mean ± SD, and non-normally distributed data are expressed as Median (Q1–Q3). Grip strength and key-pinch strength are expressed as percentages of the contralateral hand. A comparison of normally distributed continuous data was performed using the independent samples t-test and paired t-test. For comparison of categorical data, the Pearson’s chi-square test was performed. The Mann-Whitney U test and Wilcoxon rank sum test were performed to compare non-normally distributed continuous data. Spearman’s rank correlation test was applied to assess the correlation between preoperative electrodiagnostic data and postoperative outcomes (McGowan grade, modified Bishop score, and DASH score). Differences were considered statistically significant if the P-value was less than 0.05.
Results
Number of participants
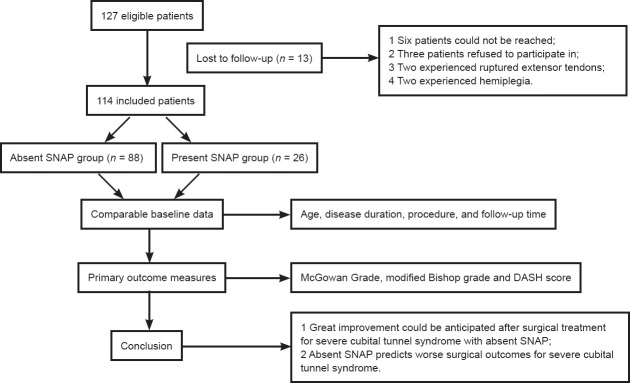
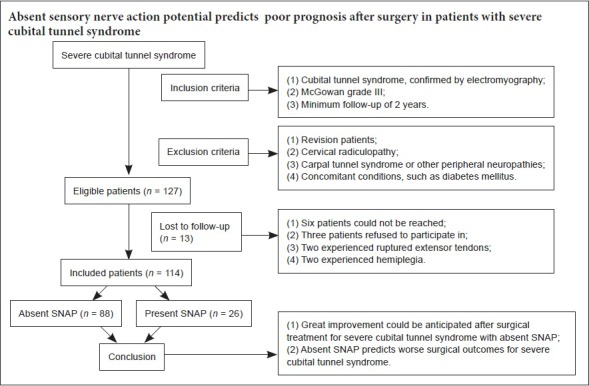
There were 127 eligible patients but we were unable to follow-up on 13 patients, leaving a final study cohort of 114 elbows out of the eligible 127 cases (89.8%). We followed 114 patients (88 with absent SNAP and 26 with present SNAP) for a mean of 51.4 months (50.0 months for absent SNAP group and 55.8 months for present SNAP group, P = 0.86) (Figure 1).
Figure 1.
Study flow chart.
SNAP: Sensory nerve action potential; DASH: Disabilities of the Arm, Shoulder, and Hand Questionnaire.
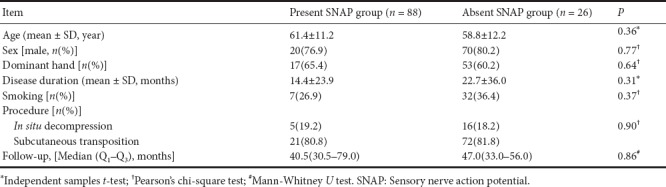
Preoperative baseline data of the participants
Demographic and clinical information on all participants are summarized in Table 1. No significant differences existed between the groups.
Table 1.
Demographics and clinical characteristics
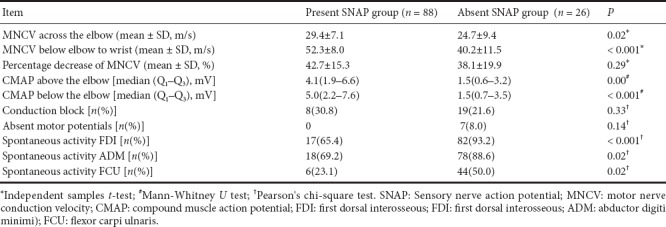
Preoperative electrodiagnostic results
Electrodiagnostic results for all patients are listed in Table 2. The distribution in diagnoses by two neurologists across the two groups showed no statistically significant difference existed (78.5% vs. 75.5%, P = 0.71, Pearson’s chi-square test). One neurologist identified 51 cases with absent SNAP out of 65 patients with severe cubital tunnel syndrome and the other neurologist identified 37 cases out of 49 severe syndrome patients.
Table 2.
Preoperative electrodiagnostic data
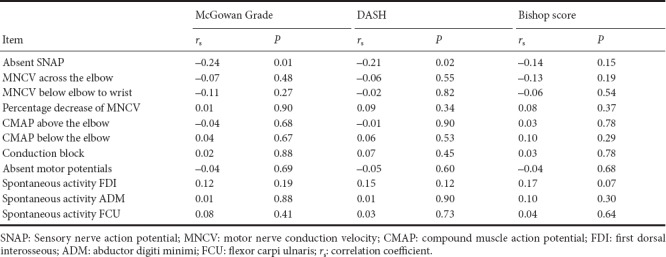
Association between preoperative electrodiagnostic data and postoperative surgical outcomes
The association between electrodiagnostic data and postoperative surgical outcomes is presented in Table 3. Absent SNAP was associated with higher postoperative McGowan grade (P = 0.01) and higher DASH score (P = 0.02). No other significant correlation existed between preoperative electrodiagnostic data and postoperative surgical outcomes.
Table 3.
Correlation between electrodiagnostic data and postoperative outcomes: Spearman's rank correlation test
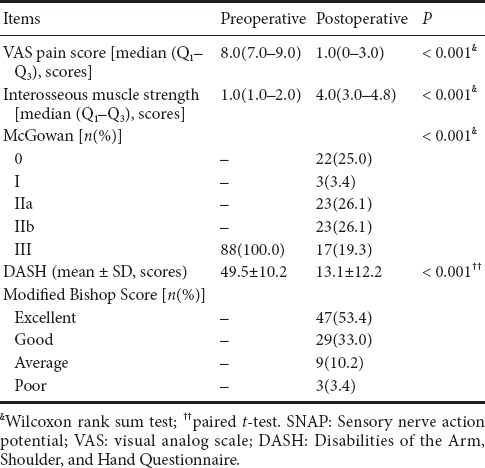
Surgical outcomes for patients with absent SNAP
Surgical outcomes for patients with absent SNAP are listed in Table 4. Eighty hands (90.9%) experienced improvement in their VAS score for pain, including 40 hands (45.5%) without pain. Seventy-one hands (80.7%) regained at least MRC grade 3 interosseous muscle strength. Improvement of at least one McGowan grade was achieved in 71 cases (80.7%), including 22 hands (25.0%) where the extremities recovered fully. The other 17 extremities (19.3%) remained on grade III. Tests using the modified Bishop scoring system showed that 76 hands (86.4%) achieved good or excellent outcomes. Significantly reduced DASH scores indicated greatly improved function of the affected hand.
Table 4.
Surgical outcomes for severe cubital tunnel syndrome with absent SNAP
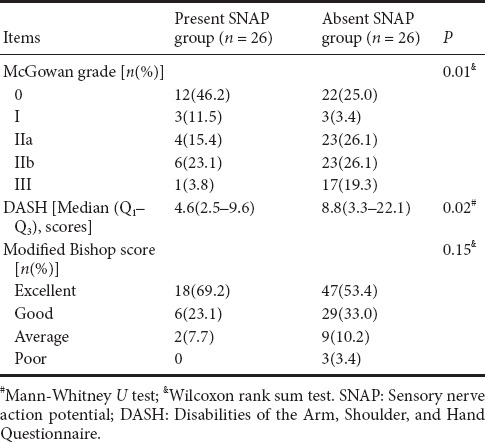
Comparison of surgical outcomes between patients with absent and present SNAP
The surgical outcomes are compared between patients with absent and present SNAP in Table 5. Patients with absent SNAP experienced more residual pain (54.5% vs. 30.8%, P = 0.03) and weaker interosseous muscle strength (3.7 vs. 4.4, P = 0.001) compared with present SNAP. They also had higher postoperative McGowan grade (P = 0.01) and higher DASH score (13.1 vs. 6.7, P = 0.02), but there was no statistical difference in the modified Bishop score (P = 0.15). Good or excellent outcomes according to the modified Bishop score were achieved in 86.4% of cases in the absent SNAP and 92.3% of the present SNAP group, but there was no statistically significant difference (P = 0.42).
Table 5.
Comparison of surgical outcomes between patients with absent and present SNAP
For patients with absent SNAP, 16 cases (18.2%) underwent in situ decompression, while 72 cases (81.8%) underwent subcutaneous transposition, and no statistically significant differences existed in terms of postoperative McGowan grade (P = 0.65), modified Bishop score (P = 0.46) or DASH score (P = 0.57).
Discussion
Currently, there is no consensus regarding the optimal surgical procedure for severe cubital tunnel syndrome. Many studies have advocated submuscular transposition to treat severe compression, on the other hand, in situ decompression and subcutaneous transposition have also been found to achieve satisfactory outcomes in severe cases (Pasque and Rayan, 1995; Nouhan and Kleinert, 1997; Dellon and Coert, 2003; Mortazavi et al., 2008; Karthik et al., 2012; Tong et al., 2017). In a randomized, prospective study on surgical treatment for severe ulnar nerve neuropathy, no difference was found between simple decompression and submuscular transposition regarding clinical or electrophysiological outcomes (Gervasio et al., 2005).
Currently available studies report controversial results regarding surgical treatment for severe cubital tunnel syndrome with absent SNAP. Some possible reasons for these divergent results could be the short-term follow-up and small number of patients. Taha et al. (2004) conducted a retrospective review of 38 limbs (27 McGowan grade II and 11 McGowan grade III), in situ decompression for 21 limbs and subcutaneous transposition for 17 limbs. They found that 20 limbs (53%) experienced improved sensory symptoms and 2 limbs (13%) achieved muscle strength improvement, however, some patients’ follow-up lasted as short as 3 months, which would greatly bias the outcome evaluation (Taha et al., 2004). Matsuzaki et al. (2004) reviewed 15 patients with absent SNAP and severe intrinsic muscle atrophy, submuscular anterior transposition, medial epicondylectomy and subcutaneous anterior transposition were used in 5 patients retrospectively, and they concluded that satisfactory functional recovery can be anticipated, with numbness relieved in 14 hands (93.3%) and intrinsic muscle strength reaching grade 4 or 5 in 11 hands (73.3%). Their study used only 15 patients, which would also bias the overall outcome evaluation (Matsuzaki et al., 2004). In the present study, following in situ decompression or subcutaneous transposition, great improvement was expected for patients suffering from severe cubital tunnel syndrome with absent SNAP, and no statistically significant difference existed between these two surgical procedures.
There has been no agreement on the prognostic value of preoperative electrodiagnostic results. Some researchers have proposed that MNCV, distal motor latency, conduction block and CMAP amplitude can be predictors of surgical outcome, while other reports indicated that preoperative electrophysiological findings had no association with surgical outcomes (Novak et al., 2002; Schreuders et al., 2004; Gervasio et al., 2005; Yamamoto et al., 2006; Friedrich and Robinson, 2011; Huang et al., 2015).
There had been no single study that compared surgical outcomes between patients with absent SNAP and present SNAP. In this study, we found that absent SNAP was associated with worse surgical outcomes in sensory function (pain), motor function (interosseous muscle strength), and overall recovery (postoperative McGowan grade and DASH score) than in present SNAP patients. Other electrodiagnostic data, including MNCV across the elbow, percentage decrease of MNCV in the cubital tunnel, absent motor action potentials, CMAP amplitude above the elbow, conduction block, and spontaneous activity (fibrillation potentials and positive sharp waves) were not associated with postoperative outcomes (McGowan grade, Modified Bishop score, and DASH score). We conclude that absent SNAP predicts inferior surgical outcomes for severe ulnar nerve compression.
Patients with McGowan grade III present profound sensory disturbance and severe intrinsic atrophy. Considering that all our patients were McGowan grade III with comparable baseline characteristics, a significant difference still exists between the absent and present SNAP groups in their surgical outcomes. This suggests that the broad McGowan grade III might be subdivided. It is reasonable to propose that absent SNAP indicates a more severe stage of the disease and could be used as a criterion for subdivision. At this stage we note that our study was retrospective and preoperative measurements such as grip strength, key-pinch strength and two-point discrimination were not routinely conducted. The objective data defining the exact loss of sensory and motor function to support this point would be the subject of a prospective study.
There are some limitations for this study. First, given the retrospective design, and 13 patients lost in follow-up, the potential for selection bias and recall bias were present. Second, the preoperative data were extracted from our hospital electronic medical record system, and not collected under controlled conditions, which could result in statistical error. Some preoperative measurements such as grip strength, key-pinch strength and two-point discrimination were not routinely conducted. This meant that the baseline data defining the exactly preoperative loss of sensory and motor function of these two groups was not completely comparable.
Additional file: Open peer review reports 1 (66.2KB, pdf) and 2 (66.2KB, pdf) .
Footnotes
Conflicts of interest: The authors declare they have no conflicts of interest.
Financial support: This study was supported by the National Natural Science Foundation of China, No. 81371374 (to DZ). The funding body played no role in the study design, in the collection, analysis and interpretation of data, in the writing of the paper, and in the decision to submit the paper for publication.
Institutional review board statement: The study was approved by the Ethical Committee of Huashan Hospital, Fudan University, China (approval No. 2017142). The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a prior approval by the institution’s human research committee.
Reporting statement: This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Biostatistics statement: The statistical methods of this study were reviewed by the biostatistician from Huashan Hospital, Fudan University, Shanghai, China.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Individual participant data that underlie the results reported in this article, after deidentification (text, tables, figures, and appendices) will be in particular shared. Study protocol form will be available. The data will be available immediately following publication without end date. Anonymized trial data will be available indefinitely at www.figshare.com.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewers: Mohammad Reza Farahpour, Islamic Azad University Urmia Branch, Iran; Vlad Bloanca, Universitatea de Medicina si Farmacie Victor Babes din Timisoara, Romania.
P-Reviewers: Farahpour MR, Bloanca V; C-Editor: Zhao M; S-Editors: Wang J, Li CH; L-Editors: Qiu Y, Song LP; T-Editor: Liu XL
Funding: This study was supported by the National Natural Science Foundation of China, No. 81371374 (to ZD).
References
- 1.American Association of Electrodiagnostic Medicine, American Academy of Neurology, American Academy of Physical Medicine and Rehabilitation. Practice parameter for electrodiagnostic studies in ulnar neuropathy at the elbow: summary statement. Muscle Nerve. 1999;22:408–411. doi: 10.1002/(sici)1097-4598(199903)22:3<408::aid-mus16>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 2.Dellon AL, Coert JH. Results of the musculofascial lengthening technique for submuscular transposition of the ulnar nerve at the elbow. J Bone Joint Surg. 2003;85A:1314–1320. doi: 10.2106/00004623-200307000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Friedrich JM, Robinson LR. Prognostic indicators from electrodiagnostic studies for ulnar neuropathy at the elbow. Muscle Nerve. 2011;43:596–600. doi: 10.1002/mus.21925. [DOI] [PubMed] [Google Scholar]
- 4.Gervasio O, Gambardella G, Zaccone C, Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56:108–117. doi: 10.1227/01.neu.0000145854.38234.81. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg BJ, Light TR, Blair SJ. Ulnar neuropathy at the elbow: results of medial epicondylectomy. J Hand Surg Am. 1989;14:182–188. doi: 10.1016/0363-5023(89)90003-8. [DOI] [PubMed] [Google Scholar]
- 6.Huang W, Zhang PX, Peng Z, Xue F, Wang TB, Jiang BG. Anterior subcutaneous transposition of the ulnar nerve improves neurological function in patients with cubital tunnel syndrome. Neural Regen Res. 2015;10:1690–1695. doi: 10.4103/1673-5374.167770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lo YL, Leoh TH, Xu LQ, Nurjannah S, Dan YF. Short-segment nerve conduction studies in the localization of ulnar neuropathy of the elbow: use of flexor carpi ulnaris recordings. Muscle Nerve. 2005;31:633–636. doi: 10.1002/mus.20250. [DOI] [PubMed] [Google Scholar]
- 8.Logigian EL, Villanueva R, Twydell PT, Myers B, Downs M, Preston DC, et al. Electrodiagnosis of ulnar neuropathy at the elbow (Une): a Bayesian approach. Muscle Nerve. 2014;49:337–344. doi: 10.1002/mus.23913. [DOI] [PubMed] [Google Scholar]
- 9.Karthik K, Nanda R, Storey S, Stothard J. Severe ulnar nerve entrapment at the elbow: functional outcome after minimally invasive in situ decompression. J Hand Surg Eur. 2012;37:115–122. doi: 10.1177/1753193411416426. [DOI] [PubMed] [Google Scholar]
- 10.Kleinman WB, Bishop AT. Anterior intramuscular transposition of the ulnar nerve. J Hand Surg Am. 1989;14:929–979. doi: 10.1016/s0363-5023(89)80046-2. [DOI] [PubMed] [Google Scholar]
- 11.Matsuzaki H, Yoshizu T, Maki Y, Naoto T, Yasuyuki Y, Satoshi T. Long-term clinical and neurologic recovery in the hand after surgery for severe cubital tunnel syndrome. J Hand Surg. 2004;29:373–378. doi: 10.1016/j.jhsa.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 12.McGowan A J. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. Bone Joint J. 1950;32-B:293–301. doi: 10.1302/0301-620X.32B3.293. [DOI] [PubMed] [Google Scholar]
- 13.Mortazavi SM, Heidari P, Asadollahi S, Farzan M. Severe tardy ulnar nerve palsy caused by traumatic cubitus valgus deformity: functional outcome of subcutaneous anterior transposition. J Hand Surg Eur. 2008;33:575–580. doi: 10.1177/1753193408092252. [DOI] [PubMed] [Google Scholar]
- 14.Nouhan R, Kleinert JM. Ulnar nerve decompression by transposing the nerve and Z-lengthening the flexor-pronator mass: clinical outcome. J Hand Surg Am. 1997;22:127–131. doi: 10.1016/S0363-5023(05)80192-3. [DOI] [PubMed] [Google Scholar]
- 15.Novak CB, Mackinnon SE, Stuebe AM. Patient self-reported outcome after ulnar nerve transposition. Ann Plast Surg. 2002;48:274–280. doi: 10.1097/00000637-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Pasque CB, Rayan GM. Anterior submuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg. 1995;20B:447–453. doi: 10.1016/s0266-7681(05)80151-2. [DOI] [PubMed] [Google Scholar]
- 17.Schreuders TA, Roebroeck ME, Jaquet JB, Hovius SE, Stam HJ. Long-term outcome of muscle strength in ulnar and median nerve injury: comparing manual muscle strength testing, grip and pinch strength dynamometers and a new intrinsic muscle strength dynamometer. J Rehab Med. 2004;36:273. doi: 10.1080/16501970410033677. [DOI] [PubMed] [Google Scholar]
- 18.Seddon HJ. London: HMSO; 1954. Peripheral Nerve Injuries. Medical Research Council Special Report Series, 282. [PubMed] [Google Scholar]
- 19.Taha A, Galarza M, Zuccarello M, Jamal T. Outcomes of cubital tunnel surgery among patients with absent sensory nerve conduction. Neurosurgery. 2004;54:891–895. doi: 10.1227/01.neu.0000115152.78918.61. [DOI] [PubMed] [Google Scholar]
- 20.Tong J, Xu B, Dong Z, Zhang C, Gu Y. Surgical outcomes for severe cubital tunnel syndrome in patients aged > 70 years: a mean follow-up of 4.5 years. Acta Neurochir. 2017;159:917–923. doi: 10.1007/s00701-017-3113-4. [DOI] [PubMed] [Google Scholar]
- 21.Watts AC, Bain GI. Patient-rated outcome of ulnar nerve decompression: a comparison of endoscopic and open in situ decompression. J Hand Surg. 2009;34:1492–1498. doi: 10.1016/j.jhsa.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto K, Shishido T, Masaoka T, Katori Y, Tanaka S. Postoperative clinical results in cubital tunnel syndrome. Orthopedics. 2006;29:347–353. doi: 10.3928/01477447-20060401-14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.