Abstract
Objective:
To describe the development and psychometric testing of items measuring connection to the cancer experience through a close friend or relative.
Methods:
Ten items assess four aspects of connection to cancer: emotional and cognitive involvement, kind and amount of shared experience, perceived similarity to the affected person, and negative change witnessed. Interviews were conducted with 2200 women close to someone with cancer. The sample was split into two samples for exploratory and confirmatory factor analysis. Sample 1 (n = 1342) was used to examine the underlying structure of the items. Sample 2 (n = 858) was used for CFA. Internal consistency and reliability analysis were also conducted.
Results:
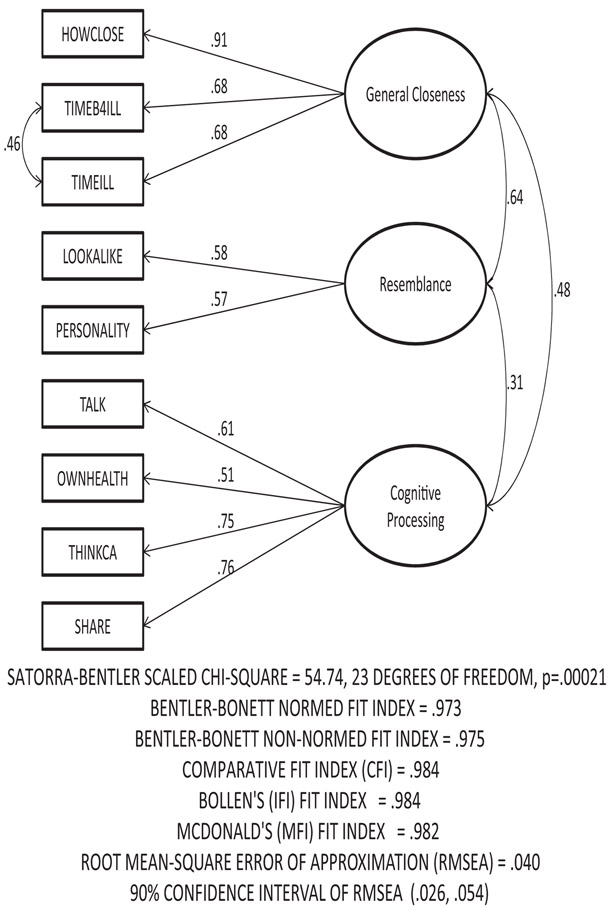
Three factors with moderate correlation were extracted: general closeness, resemblance, and cognitive processing. Results from the CFA analysis confirmed a good fit of the three-factor model (Bentler–Bonett NIF = 0.973, Bentler–Bonett NNFI = 0.975, RMSEA = 0.040 and CFI = 0.984) and all path coefficients were statistically significant.
Conclusion:
Findings provide preliminary evidence for the reliability and construct validity of the CONNECS scale in measuring individuals’ connection to the cancer experience through a close friend or relative.
Practice Implications:
CONNECS may be a useful tool for examining the impact of the cancer experience on risk perceptions, cancer worry, and medical decision making.
Keywords: Lived experience of cancer, Cancer connection, Scale development
1. Introduction
Being personally connected to someone with cancer and living through the experience alongside that person can have a profound impact in many areas of life [1–4]. As a result of watching a family member live with, or die from cancer, research finds that individuals may begin to view themselves as being more vulnerable to the disease [2,3,5–7] and they may experience strong negative emotions such as anxiety, fear, guilt, and cancer-specific worry [1,4,8,9]. Witnessing cancer in a family member has been found to affect consequential medical decision-making and health behaviors such as adhering to recommendations for cancer screenings, undergoing genetic testing, and undergoing prophylactic surgery [3,10–15]. While most of the work in this area has focused on familial relationships, especially those involving a mother or sister with breast cancer [2,3,8,16], there is evidence that witnessing cancer in an unrelated friend or acquaintance may have similar effects on one’s perception of personal cancer risk [5,17].
Many factors have been found to influence the intensity of experience related to seeing someone live with cancer. For instance, in their exploratory study of women who had a mother or sister with breast cancer, Chalmers and Thomson [8] found that women were more likely to have closely “lived the breast cancer experience” when they had a strong emotional attachment to the affected person, experienced open communication with her, and were able to spend more time and devote undivided attention to her experience. The illness trajectory also played a role, in that a more complex and variable illness resulted in greater emotional and psychological consequences for the unaffected person. In addition, they found that risk perceptions were often linked to how much a woman believed she resembled the affected relative, physically, behaviorally, psychologically, and emotionally. Other studies have also found that an individual’s connection to the cancer experience and perceptions of vulnerability to the disease are affected by the degree of emotional and cognitive involvement in another’s cancer history, exposure to a turbulent illness trajectory and physical suffering, emotional closeness, and perceived similarity to the person with cancer [2,3,18,19].
Despite the seemingly pervasive nature of indirect exposure to cancer on beliefs, feelings, and behavior, there is a lack of standardized measurement tools available to assess a person’s connection or degree of closeness to the cancer experience as witnessed through a family member or close friend. Most of the findings in this area come from qualitative research that relies upon open-ended reporting; however, a quantitative approach to measuring this type of cancer experience could be beneficial in survey research and in clinical settings.
The goal of the present study was to develop and psychometrically test a set of items intended to measure connection to the cancer experience through a close friend or relative with cancer. We aimed to develop a brief measure that would place relatively little burden on respondents and be practical for use in research and clinical settings, such as genetics counseling sessions. The items were developed within the larger context of a study on ovarian cancer risk factors and screening behavior. In developing the items, we relied upon the literature on the “lived experience” of cancer as well as a theoretical framework of judgment and decision-making [20] and heuristic processing [4,16,17,21,22]. Heuristic processing involves the use of mental short cuts or automatic judgments to make decisions when facing uncertain situations, in contrast to a more deliberative process of weighing the evidence. Affect, memory and similarity are among the constructs upon which heuristic reasoning is built. These empirically-based frameworks are consistent with findings from the qualitative literature in this area, suggesting that more salient or “mentally available” experiences with cancer, as determined by emotional strength and relationship closeness, are more likely to result in increased perceptions of vulnerability to cancer. These themes led us to focus on four key areas of assessment: emotional and cognitive involvement, kind and amount of shared experiences, perceived similarity or resemblance to the affected relative or friend, and degree of negative change observed.
2. Methods
2.1. Item development and cognitive testing
In order to develop the scale to measure connection to the cancer experience, we conducted a search for methods to assess closeness, or the strength of a person’s relationship with a relative or friend diagnosed with cancer. While no tested scale items or questions were found, our review provided insight into a number of factors that may be important in developing an assessment tool. The degree of closeness with a family member or friend with cancer, bereavement, perceived similarity of physical characteristics, intensity of the cancer experience, and the experience of talking openly about cancer in the family were among the critical themes in the qualitative literature [2,4,5,23,24]. Based on a combination of the themes noted in this literature, and the themes suggested by theoretical work in the judgment and decision-making literature, we developed a total of 10 items intended to assess connection to the experience of cancer, or what we refer to as CONNECS. The content of the items focused on the following general areas: how close the respondent was to the friend or relative with cancer, how much time had been spent with him or her, how closely she resembled him or her, the amount of negative change due to cancer that was witnessed, the extent of communication about the cancer experience with the relative or friend, and time spent thinking and talking with others about the experience. The specific items developed were intended to correspond with the general themes of emotional and cognitive involvement and shared experiences, tying into both concepts of affect- and availability-based heuristic processing. Questions on perceived physical and psychological similarity addressed the representativeness heuristic. Because the intensity of the cancer experience and witnessing the decline of a friend’s or relative’s quality of life was a key theme in the literature, we included an item that asked about witnessing negative change in the affected person’s quality of life. This is also in accord with the availability heuristic, which suggests that especially vivid or emotionally compelling events may strongly influence perception and judgment [25].
All scale items were tested for clarity of wording and appropriate response categories through cognitive testing. Cognitive testing was conducted with nine women between the ages of 38 and 77. Respondents were asked if the questions contained any terms that were unfamiliar or if they believed any response choices were inappropriate or insufficient. They were also asked if they liked or disliked the format of the questions and were invited to give suggestions on how they would improve them. Respondents reported experiencing little difficulty responding to the items, though one reported not understanding the relevance of the resemblance items and another reported being saddened by the emotions evoked by the questions. Participants reported that the questions and response options were straightforward and uncomplicated; however, several respondents indicated a preference for fewer response categories. Based on this feedback, the questions were revised by reducing the number of response categories from 5 to 3 and by developing response labels tailored specifically to each item. For example, the original response categories of “not at all,” “a little,” “somewhat,” “a lot,” and “very much” given in response to the item asking about the closeness of the relationship were revised to “not close,” “somewhat close,” and “very close.” See Table 2 for the items.
Table 2.
Descriptive statistics of individual CONNECS items by sample.
| Items | Sample | Mean | s | Median | Minimum | Maximum |
|---|---|---|---|---|---|---|
| How close was/is your relationship with the person? [HOWCLOSE] | 1a | 2.74 | 0.49 | 3.0 | 1.0 (Not close)b | 3.0 (Very close)b |
| 2a | 2.74 | 0.48 | 3.0 | |||
| How much time did you spend with the person before he/she became ill from cancer? [TIMEB4ILL] | 1 | 2.55 | 0.57 | 3.0 | 1.0 (No time) | 3.0 (A lot of time) |
| 2 | 2.51 | 0.61 | 3.0 | |||
| How much time did you spend/have you spent with the person during his/her illness? [TIMEILL] | 1 | 2.50 | 0.65 | 3.0 | 1.0 (No time) | 3.0 (A lot of time) |
| 2 | 2.46 | 0.65 | 3.0 | |||
| How much negative change did you witness/have you witnessed in the person’s quality of life or daily living after he/she became ill? [CHANGEQOL] | 1 | 2.15 | 0.80 | 2.0 | 1.0 (No negative change) | 3.0 (A lot of negative change) |
| 2 | 2.08 | .78 | 2.0 | |||
| How often did/do you talk with the person about the cancer? [TALK] | 1 | 2.02 | 0.68 | 2.0 | 1.0 (Never) | 3.0 (Very often) |
| 2 | 2.00 | 0.65 | 2.0 | |||
| How much do you believe you resemble the person physically? [LOOKALIKE] | 1 | 1.89 | 0.77 | 2.0 | 1.0 (Not at all) | 3.0 (A lot) |
| 2 | 1.87 | 0.76 | 2.0 | |||
| How much do you believe you resemble the person in terms of personality? [PERSONALITY] | 1 | 2.02 | 0.69 | 2.0 | 1.0 (Not at all) | 3.0 (A lot) |
| 2 | 2.06 | 0.69 | 2.0 | |||
| How much has the person’s experience with cancer affected how you think about your own health? [OWNHEALTH] | 1 | 2.20 | 0.73 | 2.0 | 1.0 (Not at all) | 3.0 (A lot) |
| 2 | 2.24 | 0.71 | 2.0 | |||
| How often do you think about the person’s experience with cancer? [THINKCA] | 1 | 2.10 | 0.63 | 2.0 | 1.0 (Not at all) | 3.0 (A lot) |
| 2 | 2.11 | 0.64 | 2.0 | |||
| How much time have you spent talking with friends or family members about any concerns you had about the person’s experience with cancer? [SHARE] | 1 | 1.93 | 0.59 | 2.0 | 1.0 (No time) | 3.0 (A lot of time) |
| 2 | 1.91 | 0.57 | 2.0 |
Sample 1: n = 1342; sample 2: n = 858.
For all items, the minimum and maximum values selected were the same for samples 1 and 2.
2.2. Design and sample
The data for this study was collected as part of a study focused on risk perception, worry and use of ovarian cancer screening among women at high, elevated and average risk of ovarian cancer. This study was conducted within the Henry Ford Health System (HFHS) in the Detroit, Michigan area. This large, integrated health system serves the primary and specialty health care needs of residents in southeastern Michigan, including Detroit and the surrounding metropolitan area. HFHS administrative staff identified 55,887 women enrolled in their system. We initially conducted a telephone eligibility screening of 20,483 women to identify 16,720 women eligible to participate. Those eligible to participate were women 30 years of age or older who had not been diagnosed with ovarian cancer and who reported not having had both of their ovaries removed.
2.3. Survey administration
From the women deemed eligible to participate, 3307 were randomly selected and invited to participate in a computer-assisted telephone interview (CATI) lasting approximately 35 min, of which 2524 agreed, consented, and completed the interview (overall response rate was 76.3%). Survey participants’ responses were entered directly into the CATI system, automatically creating a study data file. Interviewing for the study was conducted from January 16, 2008 to December 12, 2008. A follow-up telephone survey was conducted with consenting participants one year later; however, data from the follow-up survey were not used in the present analysis. At the completion of the interview, participants received a $15 gift card via mail.
2.4. Other measures
The baseline survey included instruments and scales not central to the current study that were used to assess personal history of cancer, family history of cancer, health behavior, cancer-related knowledge, anxiety, coping, perceptions of cancer risk, cancer screening behaviors, and demographic characteristics. Participants were asked whether they had friends and/or relatives who had been diagnosed with cancer and, if they had, to identify the one affected relative or friend with whom they felt the closest. Following these questions, the 10 items on connection to the cancer experience were administered.
2.5. Statistical analyses
To examine the characteristics of the CONNECS scale items, we first examined the distributional properties of the items including means, medians, standard deviations, and frequency of selection of each response category. This sample was randomly split into two samples with 61% (n = 1342) allocated to sample 1 (exploratory sample) and the remainder (n = 858) allocated to sample 2 (confirmatory sample). An approximate 60/40 split was used to provide a slightly larger sample for the exploratory analysis in order to increase stability of the factor coefficients.
To examine the structure of the scale, an exploratory factor analysis (EFA) was conducted using sample 1 responses to the 10 items. Given the ordinal nature of the response options, a polychoric correlation matrix was analyzed. Use of this type of matrix is also recommended when the response range is limited and the distribution of responses is skewed. The EFA was conducted using principal axis factoring (PAF) as implemented in SAS 9.2. Varimax rotation was used. The criteria for the number of factors to retain was based on the conceptual framework used to develop the scale, inspection of the scree plot, and results from a parallel analysis using the 95th percentile.
Based on the conceptual framework used to develop the items and the results of the EFA, a confirmatory factor analysis (CFA) was conducted using sample 2 responses. These analyses were conducted using EQS software version 6.1. Given the categorical nature of the response options, a polychoric correlation matrix was analyzed with estimation based on the maximum likelihood robust approach implemented by EQS. To provide a preliminary investigation of the factorial invariance of the CONNECS scale with respect to the relationship status of the close person, a multigroup analysis was conducted with relationship status as the grouping factor (relative vs. friend). From a measurement perspective, it is important to know whether an instrument of this nature would function similarly for relatives and friends. Again, sample 2 data was used for these analyses. Invariance of factor loadings, measurement error-covariances, and factor covariances were tested. First, separate models for respondents reporting on relatives and those reporting on friends were tested. Then a multigroup model was examined with constraints placed on the freely estimated factor loadings, error covariances, and the factor covariances.
2.6. Ethical considerations
Approval for this study was obtained from the Institutional Review Board (IRB) of the Centers for Disease Control and Prevention (CDC) with additional IRB and regulatory approval provided by the Henry Ford Health System. Because respondents were asked to provide potentially sensitive information about their family and personal history of cancer, we obtained a 301(d) Certificate of Confidentiality of the Public Health Service Act for this study. This certificate provides additional assurance that all responses provided by participants would be kept private and that information would not be shared with anyone outside the study staff, even under court order.
3. Results
3.1. Sample characteristics
Of the 2524 women who completed the survey, 2200 (87%) indicated having a close relative or friend previously diagnosed with cancer and completed all 10 items on the CONNECS scale. The mean age of women in the sample was 55 years with a range from 30 to 77 years. The majority of women were non-Hispanic white (67%), married (68%), fairly well educated (70% with at least some college), and had an income of at least $50,000 (62%) (Table 1). In the total sample, about 24% reported previously being diagnosed with cancer. When asked to identify the gender of the friend or relative with cancer to whom they felt closest, the vast majority (77.5%) indicated the person was female; 73% indicated he or she was a relative and 27% indicated a friend. The most frequently selected relative was a parent followed by a sibling.
Table 1.
Demographic and relationship characteristics for samples 1 and 2.
| Characteristic | Sample 1 (n = 1342) | Sample 2 (n = 858) | Total (N = 2200) | |
|---|---|---|---|---|
| Mean age (sd, min–max) | 55.1 (10.8, 30–77) | 55.3 (10.8, 30–77) | 55.2 (10.8, 30–77) | |
| Race/ethnicity (%) | NH, White | 67.7 | 66.4 | 67.2 |
| NH, Black | 26.0 | 27.4 | 26.5 | |
| Hispanic | 1.9 | 1.9 | 1.9 | |
| NH, Asian | 1.2 | 1.3 | 1.2 | |
| NH, Multi | 1.6 | 1.4 | 1.5 | |
| NH, AI/AN/NH/PI | 1.1 | 0.6 | 0.9 | |
| Not reported | 0.4 | 1.0 | 0.6 | |
| Education level (%) | <HS | 3.0 | 3.7 | 3.3 |
| HS/GED | 27.0 | 26.1 | 26.6 | |
| <4 Years of college | 34.0 | 33.0 | 33.6 | |
| 4+ Years of college | 18.6 | 19.8 | 19.2 | |
| Graduate degree | 17.2 | 17.4 | 17.3 | |
| Income (imputed) (%) | <$25k | 10.2 | 9.9 | 10.1 |
| $25k to <$35k | 10.4 | 11.8 | 11.0 | |
| $35k to <$50k | 16.2 | 18.3 | 17.0 | |
| $50k to <$75k | 24.1 | 22.1 | 23.4 | |
| $75k+ | 39.0 | 37.9 | 38.5 | |
| Marital status (%) | Married/partner | 69.1 | 65.5 | 67.7 |
| Separated/divorced | 13.7 | 17.5 | 15.2 | |
| Single/never married | 8.4 | 8.7 | 8.5 | |
| Widowed | 8.8 | 8.3 | 8.6 | |
| Description of close person with cancer (%) | Parent | 35.0 | 33.3 | 34.4 |
| Sibling | 15.7 | 14.1 | 15.1 | |
| Child | 2.2 | 2.3 | 2.3 | |
| Grandparent | 7.5 | 6.2 | 7.0 | |
| Aunt/uncle | 9.2 | 9.2 | 9.2 | |
| Other relative | 5.0 | 5.7 | 5.3 | |
| Friend | 25.8 | 29.1 | 26.8 | |
| Gender of close person with cancer (%) | Male | 22.3 | 20.9 | 21.7 |
| Female | 77.3 | 78.0 | 77.5 | |
| Not reported | 0.4 | 1.1 | 0.7 |
NH: non-hispanic; HS: high school.
The two samples created for exploratory and confirmatory factor analysis did not differ statistically on any of the demographic or relationship characteristics (Table 1).
3.2. Item analysis
Table 2 contains the item descriptive statistics by sample. The ratings for the question on emotional closeness (HOWCLOSE) and the amount of time spent with the friend or relative (TIMEB4ILL, TIMEILL) were high (means >2.4 and median of 3). On average, the ratings for the other items were somewhat lower with both mean and median ratings around 2 on the 3-point scale. The question with the highest average rating was the item on emotional closeness (HOWCLOSE) and the question with the lowest average rating was the one asking about physical resemblance (LOOKALIKE). In both samples, the item on closeness and the two items on the amount of time spent with the person showed evidence of negative skew with the majority of participants selecting the top response option for those items (76% & 76%, 59% & 57%, and 58% & 54% for HOWCLOSE, TIMEB4ILL, TIMEILL for samples 1 and 2, respectively) and only a small percent selecting the bottom response option for those items (2% & 2%, 4% & 6%, and 9% & 9% for HOWCLOSE, TIMEB4ILL, TIMEILL for samples 1 and 2, respectively). For the remaining items, the distribution across the three response categories was more symmetrical in nature among both samples 1 and 2.
3.3. EFA and reliability estimates
Sample 1 (n = 1342) was used to conduct an EFA to investigate the underlying structure of the CONNECS items. The scree plot indicated a break either after factor 2 or 3. The 2 factor solution was less conceptually clear and resulted in several items having factor loadings less than 0.40, a commonly used criterion for determining assignment of items to factors. In addition, the parallel analysis (based on using the 95th percentile value from 100 randomly generated data sets) suggested the inclusion of 3 factors. Since there is no clear consensus on the best method of selecting the number of factors, we elected to use several approaches. Given the conceptual framework used to develop the items, which supported the three-factor solution, the scree plot, and the results of the parallel analysis, the final solution was based on the extraction of 3 factors. As seen in Table 3, the three factors that emerged from the exploratory factor analysis were labeled general closeness, cognitive processing and resemblance. Items with loadings greater than 0.40 were considered to load on a particular factor. The items HOWCLOSE, TIMEILL, and TIMEB4ILL loaded highly on general closeness. The two items on resemblance composed a unique factor, while items on thinking and speaking about the cancer experience loaded highly on the cognitive processing factor. TALK or speaking with the friend or relative had moderate loadings on both the general closeness and cognitive processing factor, albeit more highly on cognitive processing. The item CHANGEQOL, or observation of negative change in the friend or relative, did not load strongly on any factor and was deleted from further analyses. Reliability estimates (Cronbach’s alpha) were computed for each factor based on inclusion of the items in bold text. As noted in Table 3, the internal consistency and reliability estimates of the subscales are fair given the brevity of each subscale. The reliability estimate for the total (all items together) was 0.73 for sample 1 and 0.71 for sample 2.
Table 3.
Results of the EFA of the CONNECS items based on principal factor analysis of the polychoric correlation matrix with varimax rotation (sample 1, n = 1342).
| Varimax rotated loadings |
|||
|---|---|---|---|
| Factor 1a | Factor 2b | Factor 3c | |
| How close was/is your relationship with the person? [HOWCLOSE] | 0.616 | 0.239 | 0.497 |
| How much time did you spend with the person before he/she became ill from cancer? [TIMEB4ILL] | 0.801 | 0.131 | 0.213 |
| How much time did you spend/have you spent with the person during his/her illness? [TIMEILL] | 0.778 | 0.193 | 0.198 |
| How much negative change did you witness/have you witnessed in the person’s quality of life or daily living after he/she became ill? [CHANGEQOL] | 0.092 | 0.361 | −0.024 |
| How often did/do you talk with the person about the cancer? [TALK] | 0.408 | 0.488 | 0.078 |
| How much do you believe you resemble the person physically? [LOOKALIKE] | 0.172 | 0.061 | 0.485 |
| How much do you believe you resemble the person in terms of personality? [PERSONALITY] | 0.133 | 0.147 | 0.535 |
| How much has the person’s experience with cancer affected how you think about your own health? [OWNHEALTH] | 0.096 | 0.531 | 0.301 |
| How often do you think about the person’s experience with cancer? [THINKCA] | 0.120 | 0.713 | 0.239 |
| How much time have you spent talking with friends or family members about any concerns you had about the person’s experience with cancer? [SHARE] | 0.101 | 0.635 | 0.129 |
| Eigenvalue for factor Cronbach’s alpha (bold items) | 3.254 | 0.924 | 0.427 |
| Sample 1 | 0.748 | 0.664 | 0.429 |
| Sample 2 | 0.731 | 0.662 | 0.422 |
General closeness.
Cognitive processing.
Resemblance.
3.4. CFA
Sample 2 (n = 858) was used to conduct confirmatory factor analysis (CFA) including a test of the factorial invariance of the instrument based on relationship status (friend vs. relative). The hypothesized model for the confirmatory analysis was based on the 3-factor structure found with EFA. Fig. 1 presents the results (standardized solution and fit indices) from the confirmatory analysis testing the 3-factor model. All fit indices, based on robust methods, are indicative of good model fit (Bentler–Bonett NFI [Normed Fit Index] = 0.973, Bentler–Bonett NNIF [Non-Normed Fit Index] = 0.975, CFI [Comparative Fit Index] = 0.984, RMSEA [Root Mean Square Error of Approximation] = 0.040). All coefficients from the items to the three factors were statistically significant. In addition, the correlation coefficients between the factors were moderate in size and statistically significant. Thus, the confirmatory analysis supported the 3-factor model.
Fig. 1.
Confirmatory factor analysis results for sample 2; standardized solution and goodness of fit statistics.
The results of the multigroup analysis with constraints indicated invariance of these parameters with respect to relative and friend groups. Again, the structure of these models was specified according to the EFA and combined CFA results. The fit statistics for the group reporting on a relative were indicative of a model with good fit. The Satorra–Bentler scaled Chi-square (SB χ2) was 42.15 with df = 22 and p = 0.006. The Bentler–Bonett NFI was 0.971, the Bentler–Bonnet NNFI was 0.977, the CFI was 0.986 and RMSEA was 0.039 (90% confidence interval of 0.020, 0.056). The fit statistics for the group reporting on a friend were also indicative of a model with good fit. The SB χ2 was 24.62 with df = 23 and p = 0.370. The NFI was 0.957, the NNFI was 0.995, the CFI was 0.997 and the RMSEA was 0.017 (90% confidence interval of 0.000, 0.056). After an examination of separate models, unconstrained and constrained multi-group models were examined. The fit statistics for the unconstrained multi-group model showed evidence of good fit. The SB χ2 was 78.12 with 46 degrees of freedom (p = 0.002). The CFI was 0.984 and the RMSEA was 0.04 (90% confidence interval of 0.024, 0.055). The fit statistics for the constrained model revealed virtually no decrement in overall fit compared with results for the constrained model with a SBχ2 of 87.11 and 56 degrees of freedom (p = 0.005). The RMSEA for this model was 0.036 (90% C.I. = 0.020, 0.050). The results of the Lagrange Multiplier Test (LMTest) for each of the constrained parameters revealed only one constraint to be untenable, the correlation between the general closeness factor and the resemblance factor. Although this finding should be interpreted with some caution due to the brevity of the resemblance factor, it is conceptually reasonable that the correlation between general closeness and resemblance would be different for relatives compared to friends. However, these results provide preliminary evidence of the measurement equivalence of the items with respect to reporting based on a relative versus a friend as the frame of reference.
4. Discussion and conclusion
4.1. Discussion
Over the past 20 years, researchers have described and attempted to capture various components of the lived experience of cancer. Without a consistent, quantifiable measurement approach, it has been difficult to assess this construct, investigate its sequelae, and compare results across studies so that it may be better understood. Our goal in developing CONNECS was to create an instrument that could be used to measure connection to the cancer experience in a way that was reliable and time-efficient. CONNECS could be a useful tool in future research aimed at investigating the sequelae of experiencing cancer in a friend or relative, with potentially important implications for understanding emotional response, cancer risk perception, and associated health behaviors, such as undergoing screening, genetic testing, and prophylactic medical procedures.
The results of our factor analysis seem to support the notion that general closeness, perceived resemblance, and cognitive processing of events are related but distinct aspects of connection to the cancer experience through a friend or relative. These themes were suggested by previous empirical and theoretical work as influencing an individual’s lived experience of cancer. In a practical sense, it may be helpful for therapists or genetic counselors to recognize the sub-components of a lived experience of cancer that might predict beliefs about cancer risk perceptions and health behaviors as well as an individual’s emotional response to witnessing a loved one with cancer. Despite the confirmation of these factors, there were indications that slight modifications to the measure could improve its sensitivity. Future modifications to the scale could entail expanding the response options on all items or changing the question wording or response labels of some items in order to differentiate levels of closeness at the upper end of this construct. While the items and response categories demonstrated adequate face validity and fared well in cognitive testing with respondents, expanding the scale for these items may be beneficial. In addition, the weakest factor within the scale, perceived resemblance, contains only two items and does not address other aspects of similarity, such as health behavior or shared interests and activities, which may be influential in the degree to which a person feels they resemble a close friend or relative with cancer.
The item that measured observation of negative change did not load onto any of the three factors. Our aim had been to address the extent to which a connection to the cancer experience may be greater from observing the worsening effects of cancer and its treatment over time. However, the item we used yielded little variability in responses as almost three-quarters of respondents endorsed observing negative change in quality of life in their relative or friend. This is not surprising inasmuch as cancer is a serious illness often requiring a number of treatments, each with its own symptoms and side effects. In order to better capture the experience of closeness to someone during the course of an illness, additional items that measure specific care-giving activities, which may assess the extent to which someone is close enough to observe a progression of worsening health, could be added and tested. In addition to expanding the measure to capture these components of closeness, future work could do more validation of the measure, perhaps by assessing the closeness of a relationship from the cancer patient’s perspective and by more closely assessing accounts of time spent together and time spent processing the cancer experiences over time. This could be achieved through more in-depth interviewing or by periodic self-assessments, as in a journaling study.
Several limitations of this study should be noted. By virtue of this study being conducted as part of a study assessing women’s perceptions of ovarian cancer, the current sample was restricted in ways that limit the generalizability of findings. First, the study included only women (no men) and excluded anyone who was younger than 30 years old. As we expand our knowledge of the effects of being connected to someone with cancer, it will be important to examine similarities and differences by the experiencer’s and cancer patient’s gender and the differences that occur from witnessing a close friend or relative with cancer at various life stages. It is likely that younger individuals may be more affected by cancer in someone close than would someone over 30 years of age. Our sample was also restricted to individuals who were enrolled in a particular managed health plan in one, Midwestern, region of the country. Future work should replicate findings within other regions and among more diverse, especially medically underserved, populations.
4.2. Conclusion
In conclusion, this new instrument characterizes a person’s degree of connection to the cancer experience in a close friend or relative with the disease. Based on previous qualitative work focused on the lived experience of cancer, along with theoretical work that structures our understanding of the impact of events around heuristic processing, the CONNECS scale characterizes three salient aspects of connection to the cancer experience: general closeness, perceived resemblance, and cognitive processing. Because the factor analysis and latent variable modeling were exploratory, our conclusions are tentative. Further research in other populations and settings is needed to confirm our findings on the efficacy of this instrument to examine the psychosocial and behavioral impact of experiencing cancer through a close friend or relative. Our results suggest that CONNECS provides a good starting point for examining that association consistently across studies.
4.3. Practice implications
CONNECS offers a fast and reliable account of a person’s connection to a close friend or relative with cancer. It may be a valuable tool in a clinical setting, including a genetic counseling context, wherein individuals may be seeking testing for genetic susceptibility to cancer in direct response to witnessing a cancer diagnosis or the progression of disease in an affected friend or relative. Additionally, it could be used as a tool to initiate discussions about the biological basis of inheritance versus the emotional impact of witnessing disease in close others. CONNECS may also be used in future research investigating the outcomes of a cancer connection when limiting participant burden and comparing with other findings is of importance to researchers.
Acknowledgements
We would like to thank the women from the Henry Ford Health System who were willing to respond to our detailed questionnaires. We thank Steven Leadbetter for statistical guidance throughout the study, and especially for contributions to the study design and sampling procedures. We recognize Sharon Alford-Hensley at Henry Ford Health Systems and Lawrence Scholl at ICI International for their excellent oversight and management of the data collection efforts. Finally, we thank Nicola Dawkins (ICI International) for assistance in questionnaire development.
Role of funding
Funding support was provided by the Centers for Disease Control and Prevention (Contract No. 200-2002-00574, Task order 0015).
Footnotes
Conflict of interest
All authors report no conflict of interest.
This manuscript was written in the course of employment by the United States Government and it is not subject to copyright in the United States.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- [1].Price MA, Butow PN, Lo SK, Wilson J, Kathleen Cuningham Consortium for Research into Familial Breast Cancer Psychosocial G. Predictors of cancer worry in unaffected women from high risk breast cancer families: risk perception is not the primary issue. J Genet Couns 2007;16:635–44. [DOI] [PubMed] [Google Scholar]
- [2].Foster C, Watson M, Moynihan C, Ardern-jones A, Eeles R. Genetic testing for breast and ovarian cancer predisposition: cancer burden and responsibility. J Health Psych 2002;7:469. [DOI] [PubMed] [Google Scholar]
- [3].d’Agincourt-Canning L, d’Agincourt-Canning L. The effect of experiential knowledge on construction of risk perception in hereditary breast/ovarian cancer. J Genet Couns 2005;14:55–69. [DOI] [PubMed] [Google Scholar]
- [4].Rees G, Fry A, Cull A. A family history of breast cancer: women’s experiences from a theoretical perspective. Soc Sci Med 2001;52:1433–40. [DOI] [PubMed] [Google Scholar]
- [5].Fiandt K, Pullen CH, Walker SN. Actual and perceived risk for chronic illness in rural older women. Clin Excell Nurse Pract 1999;3:105–15. [PubMed] [Google Scholar]
- [6].Aiken LS, Fenaughty AM, West SG, Johnson JJ, Luckett TL. Perceived determinants of risk for breast cancer and the relations among objective risk, perceived risk, and screening behavior over time. Womens Health 1995;1:27–50. [PubMed] [Google Scholar]
- [7].Vernon SW, Vogel VG, Halabi S, Bondy ML. Factors associated with perceived risk of breast cancer among women attending a screening program. Breast Cancer Res Treat 1993;28:137–44. [DOI] [PubMed] [Google Scholar]
- [8].Chalmers K, Thomson K. Coming to terms with the risk of breast cancer: perceptions of women with primary relatives with breast cancer. Qual Health Res 1996;6:256–82. [Google Scholar]
- [9].McAllister MF, Evans DG, Ormiston W, Daly P. Men in breast cancer families: a preliminary qualitative study of awareness and experience. J Med Genet 1998;35:739–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Andersen MR, Smith R, Meischke H, Bowen D, Urban N, Andersen MR, et al. Breast cancer worry and mammography use by women with and without a family history in a population-based sample. Cancer Epidemiol Biomarkers Prevent 2003;12:314–20. [PubMed] [Google Scholar]
- [11].Hurley KE, Miller SM, Costalas JW, Gillespie D, Daly MB. Anxiety/uncertainty reduction as a motivation for interest in prophylactic oophorectomy in women with a family history of ovarian cancer. J Womens Health Gend Based Med 2001;10:189–99. [DOI] [PubMed] [Google Scholar]
- [12].Schwartz MD, Taylor KL, Willard KS, Siegel JE, Lamdan RM, Moran K. Distress, personality, and mammography utilization among women with a family history of breast cancer. Health Psychol 1999;18:327–32. [DOI] [PubMed] [Google Scholar]
- [13].Schwartz MD, Peshkin BN, Tercyak KP, Taylor KL, Valdimarsdottir H. Decision making and decision support for hereditary breast-ovarian cancer susceptibility. Health Psychol 2005;24:S78–84. [DOI] [PubMed] [Google Scholar]
- [14].Stefanek ME, Helzlsouer KJ, Wilcox PM, Houn F. Predictors of and satisfaction with bilateral prophylactic mastectomy. Prev Med 1995;24:412–9. [DOI] [PubMed] [Google Scholar]
- [15].Meiser B, Butow P, Friedlander M, Schnieden V, Gattas M, Kirk J, et al. Intention to undergo prophylactic bilateral mastectomy in women at increased risk of developing hereditary breast cancer. J Clin Oncol 2000;18:2250–7. [DOI] [PubMed] [Google Scholar]
- [16].Katapodi MC, Facione NC, Humphreys JC, Dodd MJ, Katapodi MC, Facione NC, et al. Perceived breast cancer risk: heuristic reasoning and search for a dominance structure. Soc Sci Med 2005;60:421–32. [DOI] [PubMed] [Google Scholar]
- [17].Montgomery GH, Erblich J, DiLorenzo T, Bovbjerg DH, Montgomery GH, Erblich J, et al. Family and friends with disease: their impact on perceived risk. Prev Med 2003;37:242–9. [DOI] [PubMed] [Google Scholar]
- [18].Ormondroyd E, Moynihan C, Watson M, Foster C, Davolls S, Ardern-Jones A, et al. Disclosure of genetics research results after the death of the patient participant: a qualitative study of the impact on relatives. J Genet Couns 2007;16:527–38. [DOI] [PubMed] [Google Scholar]
- [19].Walter FM, Emery J, Braithwaite D, Marteau TM. Lay understanding of familial risk of common chronic diseases: a systematic review and synthesis of qualitative research. Ann Fam Med 2004;2:583–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Nisbett R, Ross L. Human Inferences: strategies and shortcomings of social judgement. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- [21].Tversky A, Kahneman D. Availability: a heuristic for judging frequency and probablity. Science 1973;185:1124–31. [Google Scholar]
- [22].Erblich J, Bovbjerg DH, Norman C, Valdimarsdottir HB, Montgomery GH. It won’t happen to me: lower perception of heart disease risk among women with family histories of breast cancer. Prev Med 2000;31:714–21. [DOI] [PubMed] [Google Scholar]
- [23].McAllister M Personal theories of inheritance, coping strategies, risk perception and engagement in hereditary non-polyposis colon cancer families offered genetic testing. Clin Genet 2003;64:179–89. [DOI] [PubMed] [Google Scholar]
- [24].Hopwood P Breast cancer risk perception: what do we know and understand? Breast Cancer Res 2000;2:387–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Peters E, McCaul KD, Stefanek M, Nelson W. A heuristics approach to understanding cancer risk perception: contributions from judgment and decision-making research. Ann Behav Med 2006;31:45–52. [DOI] [PubMed] [Google Scholar]