Abstract
Background
This study compared the biomechanical properties of a new lesser tuberosity (LTO) repair with a tensionable construct with suture tape and preplaced racking hitches vs. a traditional LTO repair using 4 high-strength sutures. The hypothesis was that there would be no difference between the 2 constructs.
Methods
LTO repairs were performed on 6 matched, paired cadaveric shoulders after placement of an uncemented humeral stem. The LTO in group 1 was repaired with 4 high-strength #2 sutures, each passed individually through the subscapularis tendon. The LTO in group 2 was repaired with 2 suture tape loops with a preplaced racking hitch knot and 2 passes through the subscapularis tendon. All sutures were passed around the humeral stem before passing through the subscapularis tendon. The specimens then underwent cyclic displacement and load-to-failure testing.
Results
Load to failure was 209.6 ± 71.2 N in group 1 compared with 502.8 ± 168.6 N in group 2 (P = .018). There was no difference in displacement between the 2 groups. All failures in group 1 occurred by knot slippage. The mode of failure in group 2 was tendon tearing in 5 of 6 cases.
Conclusion
A simplified LTO repair with suture tape and compression bridge and a preplaced half racking knot achieves favorable biomechanical properties in a technically efficient manner that may be useful clinically.
Level of evidence: Basic Science Study, Biomechanics
Keywords: Shoulder arthroplasty, lesser tuberosity osteotomy, subscapularis management, glenohumeral arthritis, racking hitch knot, biomechanical, technical efficiency
Subscapularis healing after total shoulder arthroplasty (TSA) is critical for maintenance of glenohumeral joint stability and optimization of functional outcome.2, 14 Poor healing rates with tenotomy has led many surgeons to adopt a peel technique or lesser tuberosity osteotomy (LTO).5, 7,13
From a biomechanical perspective, the goal of subscapularis repair after TSA is to optimize strength at time 0 and minimize displacement to facilitate healing. These properties are optimized by passing sutures around the humeral stem or by using a stem-based repair to avoid reliance on weak metaphyseal bone.8, 12 The downside of these repairs, however, is the complexity. In the former technique, as reported by Ponce et al,12 4 sutures are passed around the stem through up to 8 holes in the proximal humerus, and then each limb is passed through the subscapularis tendon, followed by the creation of 4 knots. In the latter described by Lederman et al,8 6 sutures are preplaced on the stem with 8 passes through the tendon, 2 passes through the bicipital groove, and the creation of 6 knots. An additional consideration of the latter is that it is implant specific.
A simplified subscapularis repair technique for TSA has recently been developed that uses suture tape with only 3 holes in the proximal humerus, 2 passes through the subscapularis tendon, and 2 knots. This technique uses suture tape and prefashioned racking hitches to create a transosseous equivalent repair that can be tensioned to remove slack in the construct (Tendon Compression Bridge [TCB]; Arthrex, Inc., Naples, FL, USA). Although the technique is appealing from an efficiency standpoint, further study is needed to compare it with a traditional technique. The purpose of this study was therefore to compare the biomechanical properties of the TCB repair vs. a traditional LTO repair using 4 high-strength sutures. The hypothesis was that there would be no difference between the 2 constructs.
Materials and methods
Six fresh frozen cadaveric matched pairs of shoulder specimens without evidence of previous surgery were used to evaluate 2 types of LTO repairs. The mean age of the specimens was 58.3 ± 8.2 years. All cadavers were male. Cadavers were randomized to receive 2 repairs with equal distribution (3 left and 3 right for each repair).
The overlying skin and deltoid were removed. The rotator cuff was inspected and confirmed to be intact in all specimens. The rotator interval was opened, and the biceps was tenotomized at the level of the glenoid. The entire rotator cuff was elevated off the scapula from medial to lateral, preserving the muscle. The scapula was removed. The humeral shaft was osteotomized 15 cm distal to the articular surface just above the elbow and then potted in standard epoxy for subsequent testing.
A fleck LTO was performed with the use of a 2-mm oscillating saw blade and a curved osteotome. The goal was to create an osteotomy that was approximately 2.5 cm2 in the coronal plane and 5 mm thick.4, 12 The humeral head was osteotomized with an anatomic cut made to match native inclination and retroversion. The humeral canal was then broached for placement of an uncemented short stem humeral prosthesis (Univers Apex; Arthrex, Inc.) according to the manufacture's recommendations. The size of the humeral stem was kept consistent between the respective matched pairs. The humerus was then prepared for repair of the LTO as subsequently described. The final stem was implanted after suture placement.
Traditional #2 suture repair
Before placement of the humeral stem, 4 holes were created with a 2-mm drill bit in the bicipital groove spanning from the superior to inferior aspects of the LTO. Two holes were created in the metaphysis just medial to the LTO. Four high-strength #2 FiberWire sutures (Arthrex, Inc.) were passed from lateral to medial by entering the bicipital groove, creating loops within which the humeral stem would be placed, and exiting medially. The inferior 2 sutures exited through the medial metaphyseal holes, and the 2 superior sutures exited below the collar of the humeral stem.
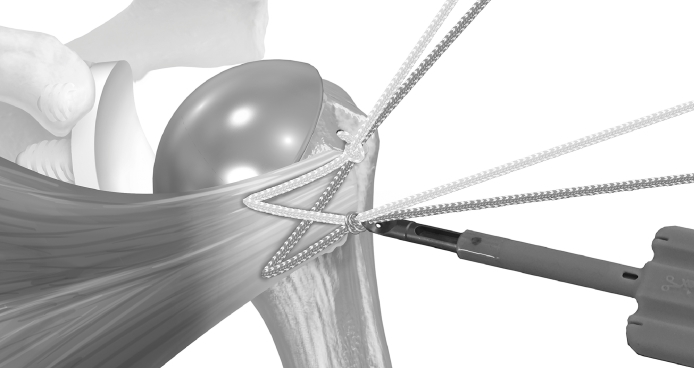
The 4 suture limbs were then passed through the subscapularis just medial to the LTO, evenly spaced, using 1 pass for each construct. The LTO was reduced to its anatomic position by placing a simple #2 suture between the superior subscapularis and anterior supraspinatus tendon at the lateral aspect of the rotator interval. Slack was manually removed from the construct, and each suture was then tied to its corresponding limb with a 6-throw surgeon's knot (Fig. 1).
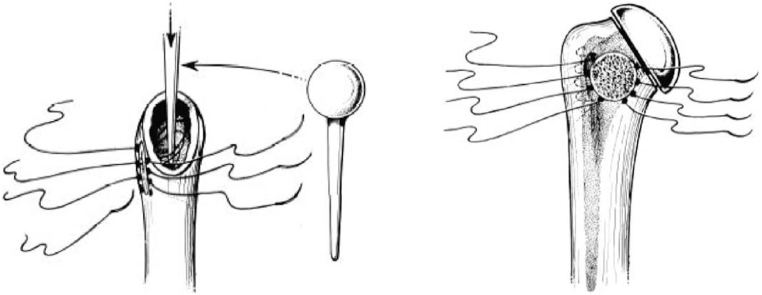
Figure 1.
Schematic of the traditional lesser tuberosity repair with 4 sutures passed around a humeral stem.
Suture tape racking hitch repair
Before placement of the humeral stem, 2 holes were created with a 2-mm drill bit in the bicipital groove at the superior and inferior aspects of the LTO. One hole was created in the metaphysis just medial to the LTO. The TCB suture tape constructs were then passed from lateral to medial by entering the bicipital groove, passing around the humeral stem, and exiting medially (Fig. 2). The inferior suture tape construct exited the medial metaphyseal hole, and the superior suture tape construct exited below the collar of the humeral stem. Each suture tape construct has a prefashioned racking hitch that was positioned to rest in the bicipital groove. The 2 medial ends of the suture are wedged together on a needle to facilitate suture passage.
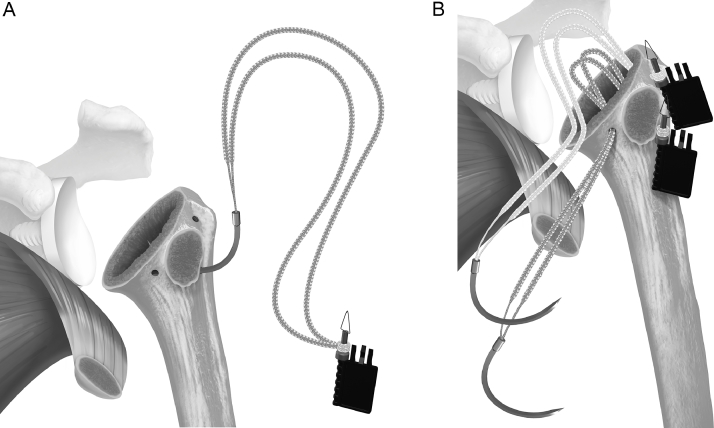
Figure 2.
(A) A suture tape prefashioned with a half racking suture on the end is passed from lateral to medial through the inferior 2 holes, and (B) a separate suture is passed through the superior hole.
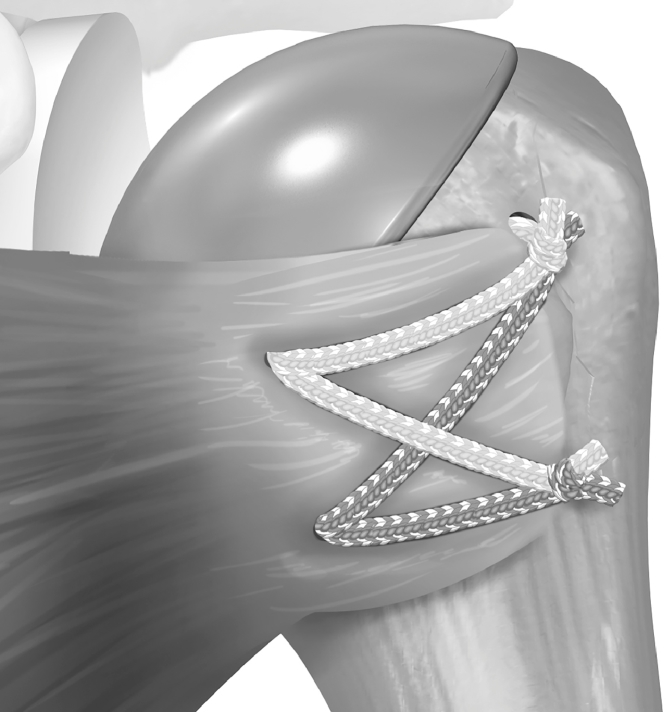
The 2 suture tapes constructs were then passed through the subscapularis just medial to the LTO, evenly spaced, using 1 pass for each construct. The needle was removed from each construct to leave 2 superior and 2 inferior limbs (Fig. 3). The LTO was reduced to its anatomic position by placing a simple #2 suture between the superior subscapularis and anterior supraspinatus tendon at the lateral aspect of the rotator interval. Then, 1 of the superior limbs and 1 of the inferior limbs were shuttled through the superior racking hitch knot (Fig. 4). The suture limbs were passed through a tensioner to remove slack and to tension the repair (Fig. 5). Tensioning was done under visual inspection. The repair was locked with 2 half hitches. The process was then repeated for the inferior racking half hitch using the remaining 2 suture limbs (Fig. 6).
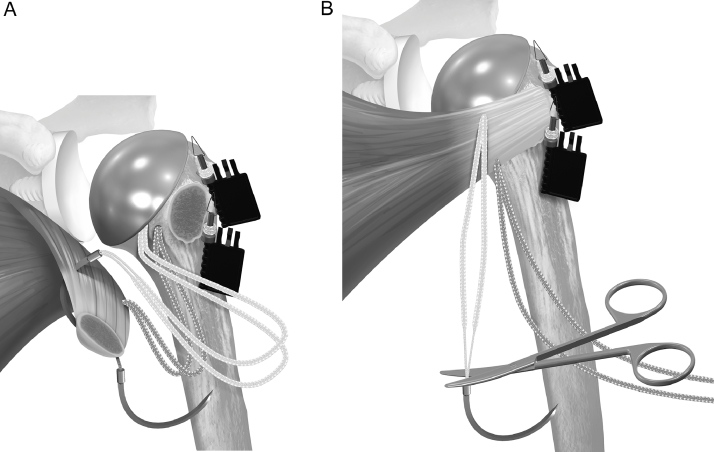
Figure 3.
The stem is placed so that the sutures pass around the prosthesis. (A) The sutures are passed through the subscapularis tendon, and (B) the wedged ends are cut to provide access to 4 free limbs.
Figure 4.
(A) One suture limb from each pair is selected and (B) passed through the prefashioned half racking suture.
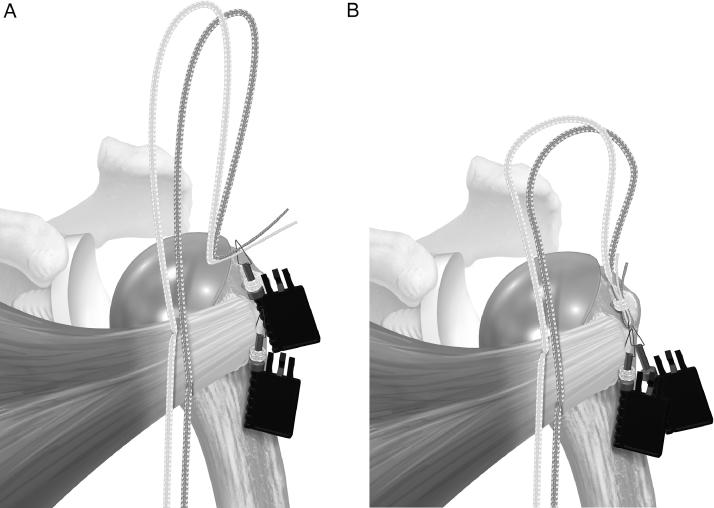
Figure 5.
The suture limbs passed through the half racking suture are tensioned. Tensioning was done under visual inspection.
Figure 6.
Final repair.
Biomechanical testing
The potted humeral shafts were mounted on a hydraulic testing system (Instron, Canton, MA, USA). The shoulders for testing were at 45° of glenohumeral abduction in neutral rotation with the line of pull 135° to the axis of the humerus to allow the subscapularis repair to be stressed in line with its axis.4, 12 The free subscapularis muscle was clamped with a cyro-jaw. Carbon dioxide was applied to the subscapularis muscle to freeze the muscle in position.
Each specimen was cycled at a rate of 1 Hz from 10 to 100 N for 500 cycles and then pulled to failure at 33 mm/s. We chose 500 cycles based on previous biomechanical studies examining the subscapularis in TSA.3, 8 Displacement was recorded using video tracking. Markers were placed on each side of the repair, cycling was video recorded, and then displacement was digitally calculated. Displacement of the LTO was measured at time 0 and after 500 cycles. Ultimate load to failure and the mechanism of failure was recorded for each construct. Displacement was recorded with video tracking. The stiffness of each construct at the LTO-bone junction was calculated as the slope of the linear region of the each sample's load vs. displacement.
Statistical analysis
Descriptive statistics are reported as mean ± standard deviation for each group. A Student t test was used to compare values, with significance set at 0.05.
Results
The results of each specimen are summarized in Tables I and II. The difference in mean cyclic displacement between group 1 (1.2 ± 1.0 mm) and group 2 (1.1 ± 1.2 mm) was not significant (P = .804). Stiffness in group 2 (70.8 ± 19.8 N/mm) trended toward being higher compared with group 1 (48.4 ± 18.9 N/mm, P = .072; Table III).
Table I.
Results for each specimen repaired with #2 suture
| Specimen | Load to failure | Stiffness | Displacement | Mode of failure |
|---|---|---|---|---|
| (N) | (N/mm) | (mm) | ||
| 1 | 406.9 | 0.11 | Suture slippage | |
| 2 | 226.6 | 0.88 | Suture slippage | |
| 3 | 344.1 | 2.39 | Suture slippage | |
| 4 | 227.8 | 2.19 | Suture slippage | |
| 5 | 267.9 | 1.64 | Suture slippage | |
| 6 | 270.5 | 0.10 | Suture slippage | |
| Mean | 290.6 | 70.8 | 1.2 | |
| Standard deviation | 71.2 | 19.8 | 1.0 |
Table II.
Results for each specimen repaired with tendon compression bridge repair
| Specimen | Load to failure | Stiffness | Displacement | Mode of failure |
|---|---|---|---|---|
| (N) | (N/mm) | (mm) | ||
| 1 | 613.8 | 0.22 | Tendon tearing | |
| 2 | 297.2 | 3.50 | Tendon tearing | |
| 3 | 333.2 | 0.79 | Tendon tearing | |
| 4 | 566.8 | 0.14 | Tendon tearing | |
| 5 | 471.4 | 0.77 | Tendon tearing | |
| 6 | 734.5 | 0.91 | Suture slippage | |
| Mean | 502.8 | 48.4 | 1.1 | |
| Standard deviation | 168.6 | 18.9 | 1.2 |
Table III.
Comparison of lesser tuberosity osteotomy repair with the traditional #2 sutures to the tendon compression bridge repair
| Variable | #2 sutures | TCB | P value |
|---|---|---|---|
| Load to failure, N | 209.6 ± 71.2 | 502.8 ± 168.6 | .018 |
| Stiffness, N/mm | 70.8 ± 19.8 | 48.4 ± 18.9 | .072 |
| Cyclic displacement, mm | 1.2 ± 1.0 | 1.1 ± 1.2 | .804 |
TCB, tendon compression bridge.
Data are presented as mean ± standard deviation.
Load to failure was 209.6 ± 71.2 N in group 1 compared with 502.8 ± 168.6 N in group 2 (P = .018). All failures in group 1 occurred by knot slippage. The mode of failure in group 2 was tendon tearing in 5 of 6 cases and suture slippage in 1.
Discussion
This study evaluated a new subscapularis repair for TSA. The results confirm the study hypothesis that a suture tape repair with a preplaced racking hitch is at least equivalent to a traditional repair. This suture tape repair may be useful given its simplification compared with traditional repairs.
Multiple reports have documented poor healing after subscapularis tenotomy during TSA.5, 10 More recent reports have noted improved healing and function with an LTO or subscapularis peel approach.1, 7,13 Based on these studies, tendon-to-bone (eg, peel) or bone-to-bone (eg, LTO) healing have become a popular technique for subscapularis management after TSA.
In the current study, load to failure was higher with the new suture tape repair compared with four #2 sutures passed around the stem. In addition, it is important to note the mode of failure was different between the repair techniques. In the #2 suture group, all failures occurred by suture slippage. In contrast, the mode of failure with the suture tape repair was tendon tearing in 5 of 6 cases. Thus, the weak link in the latter repair was transferred to the tendon. This is likely due to the unique mode of fixation with the racking hitch knot. Kelly et al6 previously demonstrated that a racking hitch knot has lower suture slippage (elongation) than a conventional knot, and the findings from our study support that conclusion.
Several previous biomechanical studies have evaluated subscapularis repair in TSA. Ponce et al12 compared a LTO with sutures passed around the stem vs. a peel repaired with transosseous sutures or a tenotomy repaired with side-to-side sutures. Cyclic displacement was significantly lower and load to failure (738 N) was significantly higher with the LTO technique compared with the transosseous peel or soft tissue tenotomy repairs. Our load to failure for this type of repair was only 291 N. This lower value may be because we used #2 suture, whereas Ponce et al used #5 suture, which has higher strength. Our results for the 4 suture repair are more similar to Giuseffi et al,4 who also used #2 suture and reported mean a load to failure of 447 N for an LTO repair with sutures passed around the humeral stem. Similarly, Fishman et al3 reported a load to failure of 375 N using 4 #2 sutures passed around the stem as well as an additional titanium cable.
Lederman et al9 compared an LTO repair with #5 sutures passed around the stem vs. a stem-based peel repair using the same humeral stem and protocol used in the current study. They reported a mean load to failure of 612 N, with a mean displacement of 2.2 mm after 500 cycles in the LTO group and 683 N and 2.9 mm in the peel group. Our load to failure with the suture tape repair was comparable at 503 N. It is likely that there is little clinical difference in these load-to-failure values given the normal forces experienced by the subscapularis, which are estimated to be 100 N.12 In addition, our mean displacement was lower at 1.1 mm after 500 cycles. This value may be more clinically relevant than load to failure for achieving healing and highlights one of the benefits of the suture tape repair in the current study. This low displacement is likely a result of the tensioning device, which allows slack to be removed from the system, and the racking hitch knot, which minimizes suture slippage.
In addition to biomechanical strength, one of the factors that should be considered in subscapularis repair after TSA is the technical efficiency of the procedure. In an interesting study, Park et al11 performed a biomechanical study comparing a double-row rotator cuff repair with 2 medial suture passes vs. 4 medial suture passes. They noted that the 2 suture pass technique was equivalent biomechanically but more efficient and described a technical efficiency ratio (TER) as follows:
Such analysis may provide a way to compare the variety of different subscapularis repair techniques that have been proposed for TSA. In the Park et al11 model, the pilot holes equated to the number of anchors, and the formula was designed for a double-row rotator cuff repair. In arthroplasty, however, the technique is different because the sutures are typically passed around or through 1 implant (eg, as opposed to 4 anchors in the denominator above). Therefore, for subscapularis repair after TSA, we proposed that the TER formula should reflect the work required to achieve a given number of suture limbs crossing the subscapularis and therefore is more accurately represented as:
Extrapolating this model, the TER of the TCB repair is 1.75 ([2 knots + 2 tendon passes + 3 drill holes]/4 suture limbs). By comparison the control technique has a TER of 3.5 ([4 + 4 + 6]/4). The latter may increase if more drill holes are used or more suture passes are performed (ie, Mason-Allen configuration), as have been described previously. In the stem-based repair described by Lederman et al,8 there are 2 drill holes in the bone and 4 holes in the stem through which suture limbs are passed, and 6 sutures cross the subscapularis to produce a TER of 3.3 ([6 + 8 + 6]/6). The suture tape repair technique in the current study thus appears to be a highly efficient technique for achieving a load to failure and displacement that is comparable with other techniques.
This study has several limitations. First, this was a biomechanical study with a small number of cadavers and may not reflect clinical healing. Further study is needed to examine the clinical results.
Second, we did not evaluate bone density and only used male cadavers. However, the effect of bone density is likely minimized by passing the sutures around the stem.
Third, we did not evaluate pressurized contact area of the constructs or suture elongation, both of which may vary between the constructs.
Finally, the control in the current study used #2 suture. As noted previously, other studies have used #5 suture. However, the #2 suture technique has been reported clinically with a healing rate of 81% to 96%.2 Furthermore, the control technique does not take away from the findings of the new repair, which demonstrated acceptable biomechanical properties.
Conclusion
A simplified LTO repair with suture tape and a preplaced half racking knot achieves favorable biomechanical properties in a technically efficient manner which may be useful clinically.
Disclaimer
This study was supported by a grant from Arthrex, Inc.
Acknowledgments
Patrick J. Denard is a consultant for Arthrex, Inc. The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- 1.Buckley T, Miller R, Nicandri G, Lewis R, Voloshin I. Analysis of subscapularis integrity and function after lesser tuberosity osteotomy versus subscapularis tenotomy in total shoulder arthroplasty using ultrasound and validated clinical outcome measures. J Shoulder Elbow Surg. 2014;23:1309–1317. doi: 10.1016/j.jse.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 2.Denard PJ, Lederman E, Gobezie R, Hanypsiak BT. Stem-Based Repair of the Subscapularis in Total Shoulder Arthroplasty. Am J Orthop (Belle Mead NJ) 2016;45:228–230. [PubMed] [Google Scholar]
- 3.Fishman MP, Budge MD, Moravek JE, Jr, Mayer M, Kurdziel MD, Baker KC. Biomechanical testing of small versus large lesser tuberosity osteotomies: effect on gap formation and ultimate failure load. J Shoulder Elbow Surg. 2014;23:470–476. doi: 10.1016/j.jse.2013.06.024. [DOI] [PubMed] [Google Scholar]
- 4.Giuseffi SA, Wongtriratanachai P, Omae H, Cil A, Zobitz ME, An KN. Biomechanical comparison of lesser tuberosity osteotomy versus subscapularis tenotomy in total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:1087–1095. doi: 10.1016/j.jse.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Jackson JD, Cil A, Smith J, Steinmann SP. Integrity and function of the subscapularis after total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:1085–1090. doi: 10.1016/j.jse.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Kelly JD, 2nd, Vaishnav S, Saunders BM, Schrumpf MA. Optimization of the racking hitch knot: how many half hitches and which suture material provide the greatest security. Clin Orthop Relat Res. 2014;472:1930–1935. doi: 10.1007/s11999-014-3478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lapner PL, Sabri E, Rakhra K, Bell K, Athwal GS. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94:2239–2246. doi: 10.2106/JBJS.K.01365. [DOI] [PubMed] [Google Scholar]
- 8.Lederman E, Streit J, Idoine J, Shishani Y, Gobezie R. Biomechanical study of a subscapularis repair technique for total shoulder arthroplasty. Orthopedics. 2016;39:e937–e943. doi: 10.3928/01477447-20160623-09. [DOI] [PubMed] [Google Scholar]
- 9.Lederman E, Streit J, Idoine J, Shishani Y, Gobezie R. Biomechanical study of a subscapularis repair technique for total shoulder arthroplasty. Orthopedics. 2016;39:e937–e943. doi: 10.3928/01477447-20160623-09. [DOI] [PubMed] [Google Scholar]
- 10.Miller SL, Hazrati Y, Klepps S, Chiang A, Flatow EL. Loss of subscapularis function after total shoulder replacement: a seldom recognized problem. J Shoulder Elbow Surg. 2003;12:29–34. doi: 10.1067/mse.2003.128195. [DOI] [PubMed] [Google Scholar]
- 11.Park MC, Peterson A, Patton J, McGarry MH, Park CJ, Lee TQ. Biomechanical effects of a 2 suture-pass medial inter-implant mattress on transosseous-equivalent rotator cuff repair and considerations for a "technical efficiency ratio". J Shoulder Elbow Surg. 2014;23:361–368. doi: 10.1016/j.jse.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 12.Ponce BA, Ahluwalia RS, Mazzocca AD, Gobezie RG, Warner JJ, Millett PJ. Biomechanical and clinical evaluation of a novel lesser tuberosity repair technique in total shoulder arthroplasty. J Bone Joint Surg Am. 2005;87(Suppl 2):1–8. doi: 10.2106/JBJS.E.00441. [DOI] [PubMed] [Google Scholar]
- 13.Scalise JJ, Ciccone J, Iannotti JP. Clinical, radiographic, and ultrasonographic comparison of subscapularis tenotomy and lesser tuberosity osteotomy for total shoulder arthroplasty. J Bone Joint Surg Am. 2010;92:1627–1634. doi: 10.2106/JBJS.G.01461. [DOI] [PubMed] [Google Scholar]
- 14.Utz CJ, Bauer TW, Iannotti JP. Glenoid component loosening due to deficient subscapularis: a case study of eccentric loading. J Shoulder Elbow Surg. 2011;20:e16–e21. doi: 10.1016/j.jse.2011.03.024. [DOI] [PubMed] [Google Scholar]