Abstract
The subscapularis tendon, at one point, was thought of as the forgotten tendon, with “hidden lesions” that referred to partial tears of this tendon. Better understanding of anatomy and biomechanics combined with improved imaging technology and the widespread use of arthroscopy has led to a higher rate of subscapularis tear diagnoses and repairs.
The bulk mass of the subscapularis muscle is more than that of all 3 other rotator cuff muscles combined. It functions as the internal rotator of the shoulder as the stout, rolled border of its tendon inserts onto the superior portion of the lesser tuberosity. A thorough history combined with specific physical examination maneuvers (including the bear hug, lift-off, and belly-press tests) is critical for accurate diagnosis. A systematic approach to advanced shoulder imaging also improves diagnostic capacity.
Once identified, most subscapularis tendon tears can be successfully repaired arthroscopically. The Lafosse classification is useful as part of a treatment algorithm. Type I and II tears may be addressed while viewing from the standard posterior glenohumeral portal; larger Lafosse type III and IV tears are best repaired with anterior visualization at the subacromial or subdeltoid space. Tendon mobilization for larger tears is critical for adequate repair.
In Lafosse type V tears, in which there is glenohumeral imbalance, tendon transfers and reverse replacement are commonly considered salvage options.
Keywords: Subscapularis tear, Irreparable subscapularis, Rotator cuff tear, Arthroscopic rotator cuff repair, Rotator cuff imaging, Subscapularis physical examination, Shoulder tendon transfer
Despite being the largest and strongest muscle in the rotator cuff, the subscapularis was once the “forgotten tendon,” with tears of this tendon described as “hidden lesions.”39, 63 Not uncommonly, detachment of the subscapularis fibers off the lesser tuberosity starts on the articular side and may have been missed in some patients when open cuff repair surgery was routinely performed. Increased awareness coupled with improved quality of imaging studies and the widespread adoption of arthroscopic techniques for the management of rotator cuff tears has led to a higher rate of subscapularis tear diagnoses and repairs.13, 55 In addition, new surgical procedures have been developed for patients with irreparable tears of the subscapularis.
This article provides a review of history, physical examination findings, and advanced imaging pearls for the diagnosis of subscapularis tendon tears. The classification, technique, and outcomes of arthroscopic repair techniques are discussed along with salvage options for irreparable tears.
Brief historical review
Subscapularis tendon tears were first described in cadavers by Smith in 1834, whereas the first description of subscapularis repair was published in 1954 by Hauser.31, 58 Interestingly, back then, Hauser already described the tear to be an undersurface tear, seen only with opening of the anterior fascial covering. Gerber refocused attention on the subscapularis in 1996 when he published the outcomes of open repair of isolated subscapularis tendon tears.26 Burkhart published the first series of arthroscopic subscapularis repairs in 2002.10 Once the forgotten tendon, advances in imaging and diagnostic awareness have brought recognition to the subscapularis tendon as we continue to understand its role in the shoulder biomechanics and rotator cuff repair outcomes. Although the description of isolated subscapularis tears is what brought attention to their importance, most subscapularis tears do occur in combination with tears of at least the anterior portion of the supraspinatus.9, 10, 43 The term anterosuperior tears was coined by Warner to recognize this pattern of cuff tearing.64
Anatomy
The subscapularis muscle originates in the subscapularis fossa along the anterior aspect of the scapula. Based on its muscle cross section, the subscapularis represents 53% of rotator cuff muscle mass, more than all 3 other muscles combined.35 Four to 6 tendon slips coalesce superiorly to form the rolled upper border of the subscapularis tendon as it inserts onto the lesser tuberosity.12 Several investigators have reported on the area of the subscapularis footprint. D'Addesi et al reported a 25 × 18-mm insertional footprint; Arai et al reported a 40.7 × 12.5-mm footprint; and Yoo et al described 4 facets of the subscapularis insertion totaling 51.5 × 10.7 mm, with the first facet representing 34% of the entire footprint.5, 14, 66 Differences in these measurements are based on incomplete representation of all 4 subscapularis tendon facets.66 The upper subscapularis attachment is through a robust tendon, whereas the lower third is largely muscular with very short tendon fibers.14
The biceps tendon and its sheath are intimately related to the subscapularis tendon. The superior border of the subscapularis tendon becomes the floor of the biceps groove and interdigitates with the supraspinatus fibers. Any evidence of instability or tearing of the long head of the biceps should prompt careful assessment of the subscapularis tendon because these conditions are commonly associated with each other.57 Concomitant biceps disease has been reported in at least 20% and as frequently as 90% of the time in patients with confirmed subscapularis tears, with increasing tear size correlating with more frequent biceps involvement.5, 18, 26, 30
The superior glenohumeral ligament and the coracohumeral ligament contribute to form the reflection pulley, or the superior-medial border of the biceps sheath.5, 63 Disruption of this pulley can also correspond to biceps tendon instability and tears of the superior portion of the subscapularis tendon. As the torn upper edge of the subscapularis tendon retracts medially, a bundle of fibers from the coracohumeral and superior glenohumeral ligaments that attach to the superior-lateral edge of the subscapularis become visible, adopting a bent configuration that corresponds to the “comma sign” in arthroscopic surgery.40, 62
Biomechanics
The subscapularis muscle functions as an internal rotator of the glenohumeral joint, working synergistically with the pectoralis major, latissimus dorsi, and teres major. In addition, it has a buttressing and stabilizing effect on the glenohumeral joint, especially in abduction and external rotation. This tenodesing effect is seen in throwers, in whom the muscle is electrically silent but the tendon itself stabilizes the joint during certain throwing motions.34 To evaluate its impact on glenohumeral stability, Marquardt et al evaluated the effects of arthroscopic release of the subscapularis tendon in cadavers and found that the subscapularis tendon inhibited anterior-inferior translation at the midrange of motion.44 Severe subscapularis tears may allow static anterior subluxation of the humeral head, a situation considered by most to require salvage procedures as opposed to primary repair.
The subscapularis is theorized to contribute anteriorly as a force couple with the infraspinatus and teres minor to transversely stabilize the glenohumeral joint. This is important for rotator cuff tensioning, as fixation of the subscapularis tendon restores the anterior portion of the cuff cable and balances the shoulder, decreasing the strain on posterosuperior rotator cuff repairs.60 The subscapularis muscle also opposes the upward pull of the deltoid with humerus abduction and elevation, thus maintaining proper glenohumeral joint mechanics with shoulder motion.
Diagnosis
History
A high index of suspicion for subscapularis disease should be held in evaluating patients older than 40 years with weakness after an anterior shoulder dislocation. Likewise, the subscapularis should be carefully assessed in patients with long head of the biceps disease or when pain is felt mostly anteriorly.12, 27, 37 Difficulty with activities that involve pushing inward, such as holding a box in front of the body with 2 hands, may also hint at subscapularis involvement.
Examination
As with any other shoulder condition, examination of the patient with possible subscapularis tearing should start with a general assessment of pain location, motion, and strength. Subscapularis tendon tears can translate into increased passive external rotation of the shoulder. This is best detected by assessing passive external rotation of both shoulders simultaneously to determine whether there is a substantial increase on the affected side. A number of physical examination maneuvers have been described to specifically assess the subscapularis. The 3 most commonly performed in our practice are the lift-off test, the belly-press test, and the bear hug test.
Lift-off test and internal rotation lag sign
First described by Gerber, this examination maneuver requires the shoulder to be placed in internal rotation so that the dorsum of the patient's hand is resting on the lower lumbar spine.26, 27 The patient is asked to lift the hand off the lower back (Fig. 1, A). Inability to do so is considered an indicator of subscapularis weakness. Some patients may “cheat” and extend the elbow to lift the hand, as opposed to further internally rotating the shoulder. The internal rotation lag sign is a similar test, but the examiner places the hand of the patient behind the trunk and off the body and asks the patient to maintain the hand in that position, not letting the hand drop to the lower back.
Figure 1.
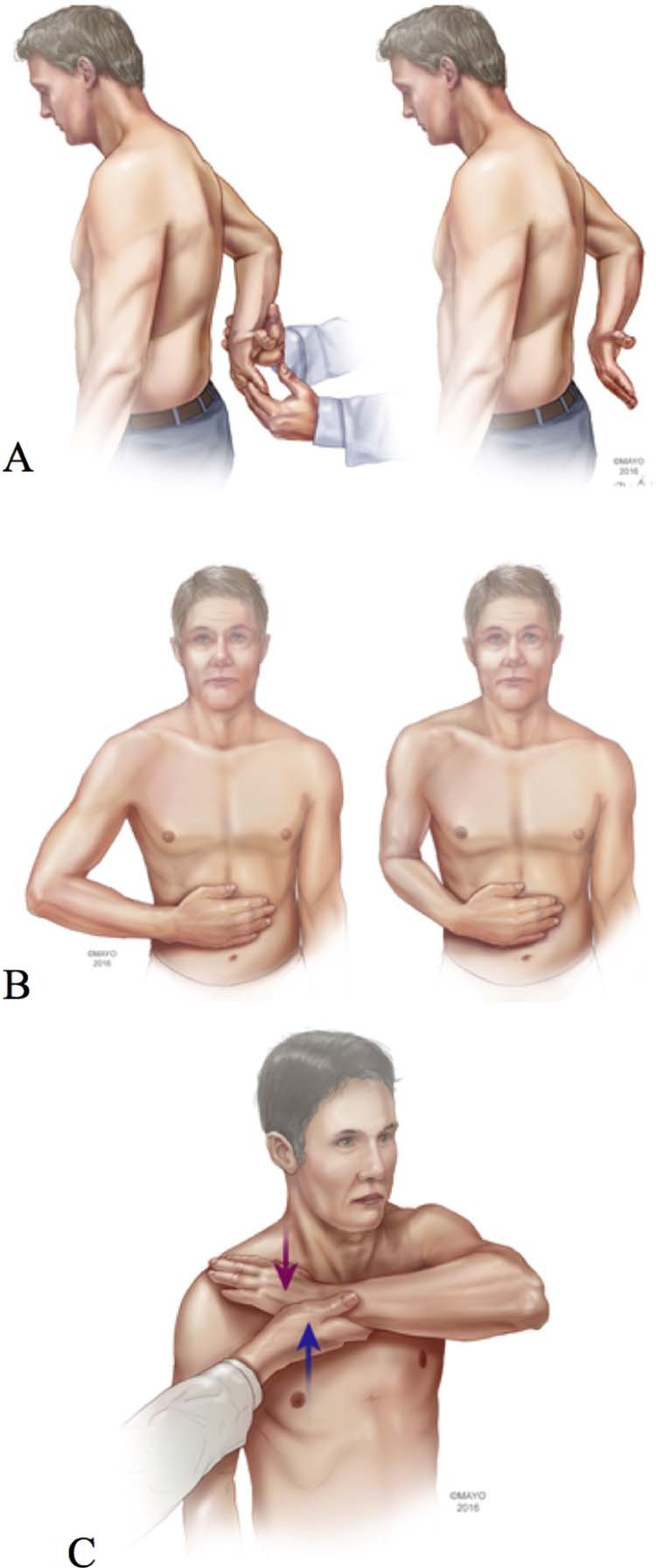
Subscapularis physical examination maneuvers. (A) Lift-off test. (B) Belly-press test. (C) Bear hug test.
Belly-press test
In the belly-press test, the patient is asked to rest the hand on the abdomen, to keep the elbow forward past the mid–coronal plane, and to press on the belly without letting the elbow move backward (Fig. 1, B). Subscapularis weakness makes it difficult or impossible to press into the abdomen without moving the elbow back because the patient compensates for lack of shoulder internal rotation with shoulder extension.26 The “Napoleon sign” was introduced to grade the severity of the belly-press test in reference to Napoleon Bonaparte's posture in paintings.10
Bear hug test
The bear hug test is performed with the hand of the affected extremity placed on top of the contralateral shoulder and the elbow pointing anteriorly (Fig. 1, C). The examiner tries to lift the hand off the patient's shoulder while the patient resists external rotation.6 This test is considered positive when the examiner can externally rotate the arm while the patient is trying to actively maintain internal rotation.
Comparative value of physical examination tests
Studies indicate that the combined sensitivity of these 3 diagnostic maneuvers to detect subscapularis tears is approximately 80%.21 The bear hug test is the most sensitive as it can detect isolated tears of the upper third of the subscapularis tendon. In an electromyography study, Tokish et al demonstrated that the lift-off test activated the lower subscapularis muscle more, whereas the belly-press test activated the upper subscapularis muscle more.61 A positive result of the lift-off test correlates with full-thickness tearing, higher grade fatty degeneration, and greater loss of internal rotation strength.67
Imaging
Plain radiographs
Anteroposterior views in internal rotation and external rotation allow visualization of rotator cuff calcifications and differential joint line narrowing. The lateral scapula or Y view assesses the supraspinatus outlet and may show areas of cystic formations in the tuberosities. Severe subscapularis tears may result in anterior subluxation, best seen on the axillary radiograph, and large anterosuperior cuff tears may lead to superior humeral head migration on the anteroposterior views.63 Cysts within the lesser tuberosity may also suggest subscapularis disease.59
Ultrasound
Ultrasound is a lower cost imaging modality that can be used dynamically to evaluate tendon disease. One study reported 39.5% sensitivity and 93.1% specificity values with use of ultrasound for the diagnosis of subscapularis tears.49 Sensitivity was lower for smaller tears and higher for larger tears. Bicipital peritendinous effusion >2 mm on ultrasound has been correlated with subscapularis tendon tears.11
Computed tomography
Computed tomography (CT), particularly computed arthrotomography with intra-articular injection of contrast material, may be used to evaluate subscapularis tearing and fatty infiltration. Although magnetic resonance imaging (MRI) has largely replaced CT in North America for rotator cuff imaging, CT should still be considered for patients with contraindications to MRI. In addition, for irreparable subscapularis tears requiring reverse shoulder arthroplasty (RSA), CT provides more accurate preoperative planning for arthroplasty, especially when dedicated planning software and patient-specific instrumentation are considered.
Magnetic resonance imaging
MRI and magnetic resonance arthrography (MRA) are the most common advanced imaging modalities used for evaluation of the rotator cuff. However, the diagnostic yield of MRI for patients with subscapularis tears is perceived to be inferior compared with posterosuperior tears. The overall sensitivity has been reported to be 37.5% for magnetic resonance evaluation of subscapularis tears, with 40% sensitivity for MRI and 36% sensitivity for MRA.22 In the study by Adams et al,3 the reported values for sensitivity and specificity were 36% and 100%, respectively. Sensitivity was better for larger tears involving >50% of the tendon in cephalad-caudal direction.
Some studies suggest that the diagnostic yield of MRI for subscapularis tearing may be improved with a dedicated, systematic reading approach. Pfirrmann et al reported a 95%-100% sensitivity and 55%-62% specificity for detecting subscapularis tears using MRA.54 In their study, a number of findings were particularly helpful in assessing the subscapularis, including (1) leakage of intra-articular contrast material under the subscapularis tendon insertion onto the lesser tuberosity on transverse and parasagittal images, (2) presence of fatty infiltration in the subscapularis muscle, and (3) abnormalities along the biceps course. Similarly, Furukawa et al reported on the diagnostic accuracy of radial, transverse, and oblique sagittal MRI for subscapularis tears. Radial-slice MRI images had a 95% sensitivity and 82% specificity, transverse images had a 58% sensitivity and 100% specificity, and oblique sagittal images had a 61% sensitivity and 100% specificity.25
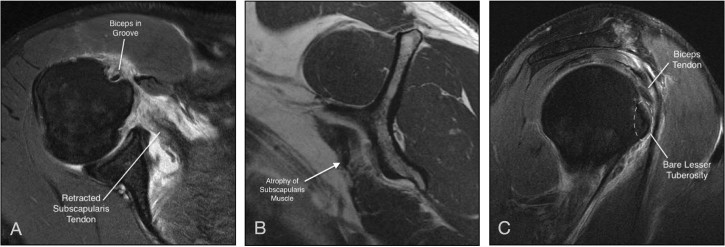
Adams et al also described a systematic approach of diagnosing subscapularis tears on preoperative MRI. Their 4-step evaluation consists of (1) the presence or absence of a subscapularis tear on axial cuts, (2) subluxation of the long head of the biceps tendon on axial cuts, (3) subscapularis atrophy on sagittal images, and (4) subscapularis tear off of the lesser tuberosity on sagittal images (Fig. 2). Subscapularis pathologic change on 2 of 4 images was considered to indicate subscapularis tearing. With this approach, they reported 73% sensitivity and 94% specificity for correct diagnosis of a subscapularis tear.1 There was an increase in diagnosis with larger tears that involved >50% of the tendon in the cephalad-caudal direction, which is in agreement with previously reported studies.3
Figure 2.
Applying the 4-step magnetic resonance imaging evaluation by Adams et al.1 (A) Axial image showing the biceps tendon in the groove with an obvious retracted tear of the subscapularis tendon. (B) Sagittal image showing grade 2 fatty infiltration of the subscapularis muscle. (C) Sagittal image showing a bare lesser tuberosity.
In addition to diagnosing a subscapularis tear on MRI, understanding the quality of tissue to be fixed is also extremely important. The Goutallier classification is used to measure fatty infiltration of the rotator cuff muscles on CT scans. Stage 0 corresponds to normal muscle; stage 1, some fatty streaks; stage 2, less fat than muscle; stage 3, equivalent fat and muscle; and stage 4, more fat than muscle.24, 29 MRI has also been used to stage fatty infiltration.24 Literature has shown correlation between the degree of fatty infiltration, severity and chronicity of rotator cuff tear, and outcomes of rotator cuff repair, with increased fatty infiltration associated with a more severe tear, a more chronic tear, and worse outcomes after repair.28, 45
Two additional studies have specifically analyzed the diagnostic value of biceps disease and perceived tendon length respectively. Meyer et al analyzed the relationship between tendon length and subscapularis tears, introducing the concept of tear in continuity.46 As the deeper fibers of the subscapularis are detached from the lesser tuberosity, retraction of the muscle unit will translate into a longer tendon on axial MRI cuts. In their study, the likelihood ratio of a partial subscapularis tear was 16 when the tendon measured 60 mm.
Shi et al challenged the concept of systematic involvement of the biceps tendon in subscapularis tears.57 In their study, biceps subluxation had a negative predictive value >90%, indicating that if the biceps is in the groove, chances are the subscapularis tendon is intact. However, the positive predictive value was only 35%, indicating that even if the biceps tendon is subluxed, the subscapularis may still be intact.67
Confirming subscapularis tears at the time of diagnostic arthroscopy
Because subscapularis tears commonly start on the articular side, direct visualization of the subscapularis tendon during arthroscopic surgery has the potential to provide better visualization of these lesions than open surgery.63 However, the existence of partial tears and tears in continuity, paired with the fact that the lesser tuberosity is difficult to fully visualize using a 30° arthroscope from the standard posterior portal, can make an accurate diagnosis challenging.
Specific intra-articular findings have been described to prompt the surgeon to evaluate the subscapularis tendon carefully. The most obvious is complete medial dislocation of the tendon of the long head of the biceps (Fig. 3). Partial tearing of the medial biceps as it exits the joint has been termed “sentinel sign” by Lafosse and colleagues, indicating a high-likelihood of partial-thickness subscapularis tearing.56 Medial retraction and adoption of a comma sign by the interval ligaments has also been described as an indicator of subscapularis tearing.40
Figure 3.
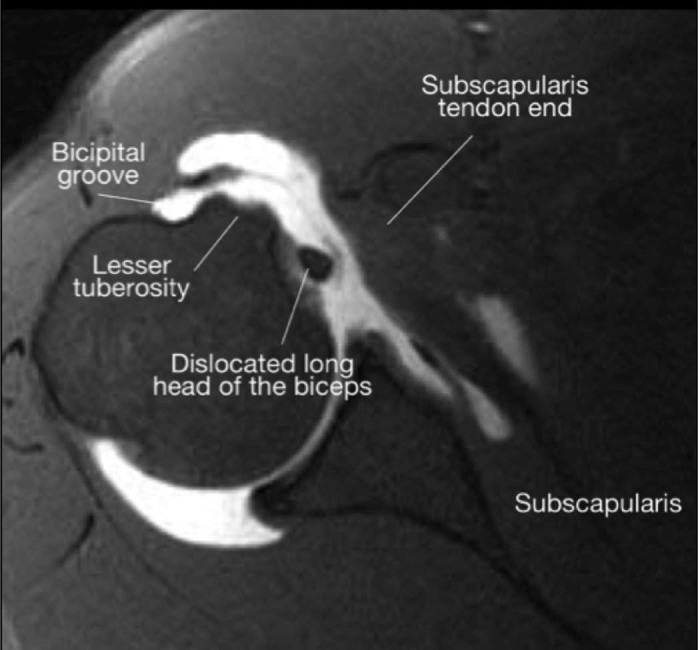
Medial dislocation of the long head of the biceps tendon.
A number of pearls may be considered at the time of arthroscopy to avoid missing tearing of the subscapularis. First, if the remaining cuff is intact and a subscapularis tear is suspected, removing the capsular tissue at the interval region may allow better visualization of the subscapularis tendon. Use of tissue graspers or traction sutures may unmask a partial tear in continuity as the normal upper rolled border of the subscapularis is visualized to be medially retracted.
With the camera in the posterior portal, visualization of the subscapularis tendon and its insertion into the lesser tuberosity is improved by placing the shoulder in flexion and internal rotation, translating the proximal humerus posteriorly (“posterior lever push”), or using a 70° arthroscope (Fig. 4).16 The standard 30° camera has previously been reported to show as little as 26% of the subscapularis when no humerus manipulation is used, but the posterior lever push can improve visualization.47, 65 Alternatively, visualization can be obtained by inserting the camera anteriorly.9 When associated disease of the labrum or biceps merits intervention, biceps tenotomy with or without tenodesis may facilitate visualization as well. Some authors state that detaching the biceps decreases tension on the subscapularis tendon and ensures that a dislocating or unstable biceps will not compromise subscapularis fixation.9
Figure 4.
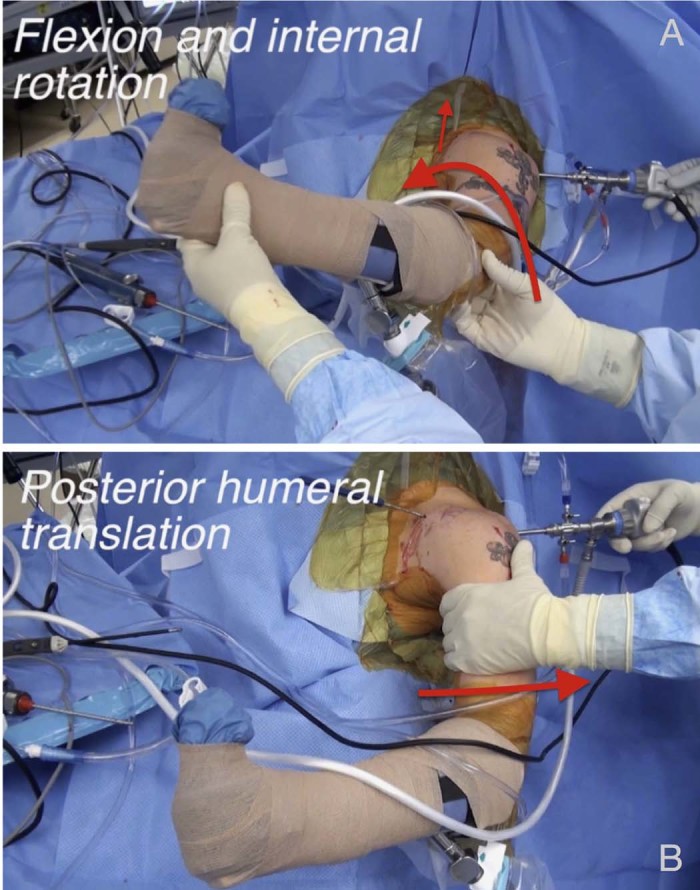
Manipulation methods for better arthroscopic subscapularis visualization. (A) Flexion and internal rotation of affected extremity. (B) “Posterior lever push,” whereby a posteriorly directed force is placed on the proximal humerus.
Tear classification
There are several classifications for subscapularis tendon tears. Pfirrmann et al used MRI to differentiate tears on the basis of their location in the subscapularis tendon.54 Grade 0 is a normal subscapularis tendon. Grade 1 is a lesion involving less than the upper quartile of the subscapularis tendon in a craniocaudal direction. Grade 2 is a lesion >25% of the craniocaudal diameter but no complete tendon detachment. Grade 3 is complete tendon detachment. Interobserver agreement using this grading scheme is substantial.
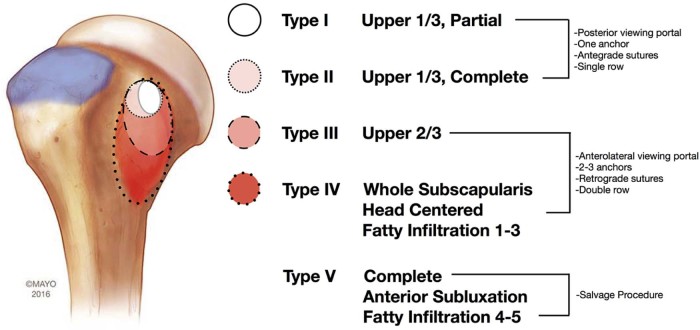
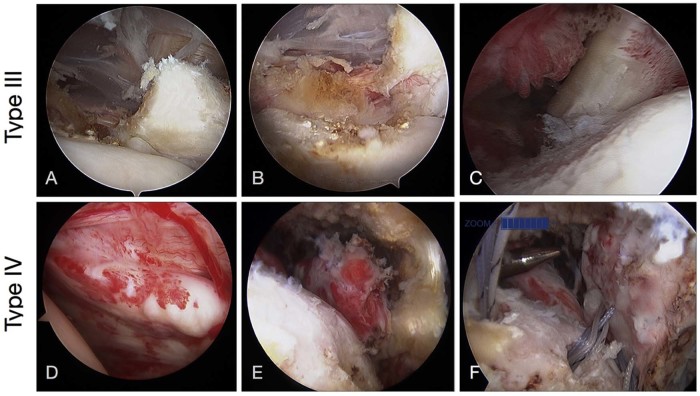
We find the Lafosse classification particularly useful to establish a treatment strategy (Fig. 5). A type I lesion is defined as a partial lesion of the superior third of the subscapularis tendon without complete detachment (undersurface tear of the upper third). Type II is a complete detachment of the superior third of the tendon. Type III is a complete tear of the superior two-thirds of the tendon without muscle detachment of the inferior third, thus limiting retraction of the tendon. Type IV is a complete tear off the lesser tuberosity with the tendon retracted closer to the glenoid but with the head centered and stage ≤3 fatty atrophy in the subscapularis muscle. Type V is a complete tear of the subscapularis tendon with eccentric positioning of the head or fatty degeneration stage >3 atrophy.36
Figure 5.
Lafosse classification of subscapularis tears and treatment algorithm.
Yoo and Rhee and colleagues introduced a classification system based on the facets of the lesser tuberosity.66 Type I is defined as fraying or a longitudinal split of the leading edge of the tendon. Type IIA is <50% subscapularis tendon detachment in the first facet. Type IIB is a >50% detachment in the first facet without complete disruption of the lateral band. Type III represents a subscapularis tear off the entire first facet with complete disruption of the lateral band. Type IV represents a tear involving the first 2 facets with medial retraction of the tendon, correlating to Lafosse type III as a tear of the upper two-thirds of the subscapularis tendon. Type V is defined as a complete subscapularis tendon tear.
Treatment
Overview
The general principles of rotator cuff tear management apply to subscapularis tears. Patients with partial or incomplete tears may improve with nonoperative treatment. On the contrary, acute traumatic tears are best treated with early surgical repair. The quality of the tendon, length of remaining tendon, atrophy, fatty infiltration, and retraction should be considered as well in the decision-making process.
Repair of the subscapularis tendon may be performed with open or arthroscopic techniques. Arthroscopic repair of the subscapularis tendon is our procedure of choice.9, 10 Open repair of the subscapularis provides a better opportunity for tendon augmentation with autograft, allograft, or commercially available patches. For the irreparable Lafosse type V tear, salvage options include reconstruction of the anterior capsule, tendon transfers, and RSA.
Arthroscopic repair
Mobilization and access to the subscapularis tendon are of paramount importance as this allows classification of tear morphology and anatomic reduction of the tendon back to the lesser tuberosity. Studies have shown, however, that medialization of the footprint by as much as 7 mm can be done without compromising muscle function.15 For mobilization and visualization, the rotator cuff interval may be surgically opened. Adhesions in the subcoracoid region anteriorly are resected to create adequate space between the coracoid bone and subscapularis tendon, performing a coracoidplasty if needed.9 Additional caution must be exercised in this region because of its proximity to the brachial plexus and axillary vasculature. Because the musculocutaneous nerve, the lateral cord of the brachial plexus, the axillary nerve, and the axillary artery are all >25 mm from the coracoid, staying adjacent and lateral to the coracoid during adhesion release can prevent neurovascular injury.41
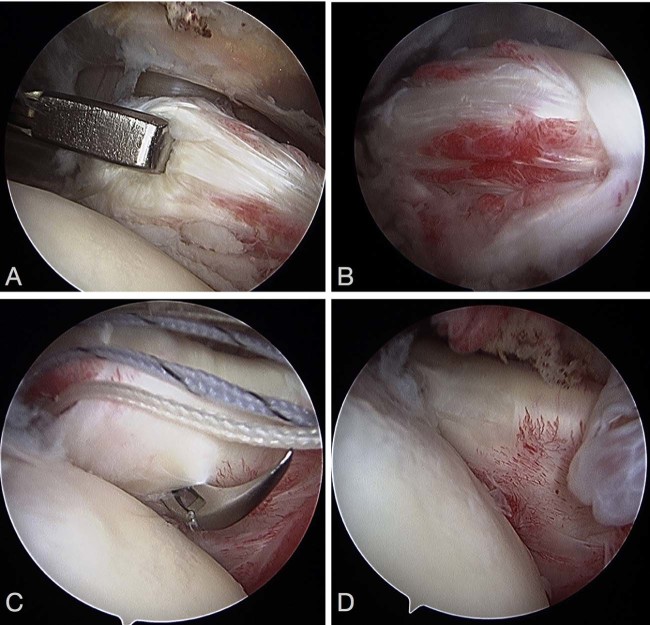
A tendon grasper or a traction suture is used to put lateral traction on the tendon when it is retracted medially (Fig. 6). Adhesions between the undersurface of the subscapularis and anterior neck to the glenoid are released to mobilize a retracted tendon. Sometimes there is an arc of tissue composed of the medial sling of the biceps sheath, the avulsed coracohumeral ligament, and the superior glenohumeral ligament that retracts with the subscapularis tendon, known as the “comma” tissue.40 This comma tissue is usually attached to the superolateral corner of the subscapularis tendon and serves as an anatomic marker for the leading edge of the tear.
Figure 6.
Intraoperative images of a subscapularis tear. (A) Traction on the subscapularis reveals the poor-quality tendon associated with a tear. (B) Tear in continuity seen in subscapularis tendon. (C) Intraoperative fixation of tendon with retrograde passing of sutures for horizontal mattress suture fixation. (D) Final picture of re-established rolled border.
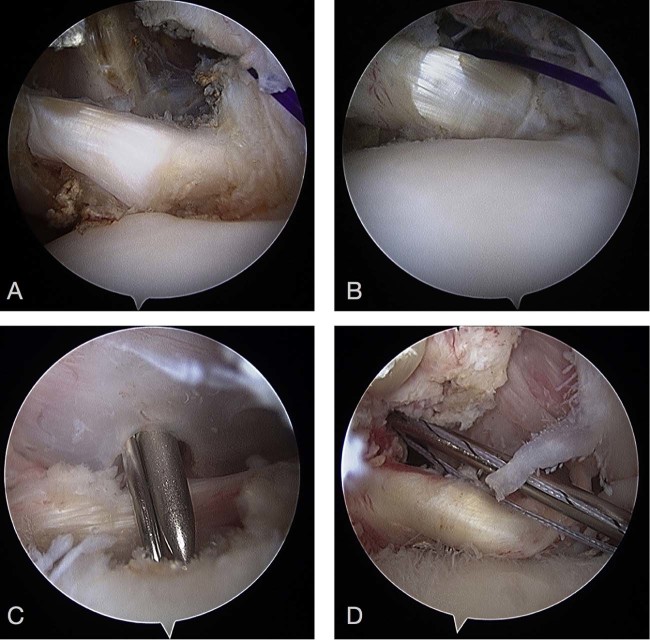
After mobilization of the tendon, our preference is to complete the repair to bone in a caudal-cranial direction. For optimal tendon-bone healing, the lesser tuberosity footprint is débrided but not fully decorticated. Lafosse type I and II tears can usually be repaired using 1 anchor loaded with multiple sutures (Fig. 7). Sutures are placed in a simple or mattress fashion to fix tendon to bone. The standard posterior glenohumeral portal provides adequate visualization of the footprint at this level.
Figure 7.
Arthroscopic fixation of type I and type II tears. (A) Type I tear. (B) Fixation of type I tear. (C) Type II tear. (D) Fixation of type II tear.
Lafosse type III and IV tears require more tendon mobilization and are best visualized subacromially through an anterolateral portal (Fig. 8). Two or 3 anchors and double-row techniques are preferred to re-create the footprint of the tendon. Given the thickness and location of the torn tendon, retrograde suture passing is typically best. One anchor is usually used for every square centimeter of exposed tendon.2 The comma tissue may be preserved or divided, depending on the tear configuration and the surgeon's preference.
Figure 8.
Arthroscopic fixation of type III and type IV tears. (A-C) Type III tear. Note the disruption of the superior tendinous portion in (A) and continuity of the muscle portion in (B). (C) Fixation of type III tear. (D-F) Type IV tear. (D) Before mobilization of tendon. (E) After mobilization of tendon; note how far back the tendon is retracted. (F) Suture fixation of the tendon with multiple anchors.
Open repair with or without augmentation
Truly isolated subscapularis tears and tears involving only the subscapularis and anterior supraspinatus tendons are best exposed through a deltopectoral approach. Large posterosuperior cuff tears that also extend into the subscapularis are better exposed through a superior deltoid-splitting approach.
Once the tear is exposed, traction sutures may be used to aid in tendon mobilization and release of bursal and articular adhesions. The lesser tuberosity is prepared to expose bleeding bone. Transosseous sutures passed at the margin of the articular cartilage and exiting at the bicipital groove will provide strong bone fixation and compress the tendon to the footprint. Anchors may be used as well, but they increase the cost of the procedure substantially.
If the subscapularis is markedly retracted or the quality of the tendon is compromised, consideration can be given to augmenting the repair. Our preference has been use of an Achilles tendon allograft, with the narrow portion of the allograft fixed on the lesser tuberosity and the wide aponeurosis draped and repaired to the subscapularis muscle belly.
Salvage procedures
For irreparable subscapularis tears, the presence of glenohumeral arthritis and the patient's activity level dictate treatment. For younger, active patients without arthritis, soft tissue reconstruction, allograft augmentation, or tendon transfers are viable options. Anterior capsule reconstruction with or without allograft augmentation has been reported in an effort to re-create the tenodesing effect of the subscapularis tendon and to balance the transverse force couple across the glenohumeral joint. Pectoralis major, pectoralis minor, and latissimus dorsi tendon transfers are additional methods of restoring shoulder mechanics with native rather than with cadaveric tissue. Preliminary data seem to indicate that anterior transfer of the latissimus dorsi is feasible, and it might end up becoming the tendon transfer of choice for irreparable subscapularis tears.20 For patients with glenohumeral arthritis and an irreparable subscapularis tear, RSA represents the best salvage option.
Outcomes
Good outcomes have been reported with both open and arthroscopic subscapularis tendon repairs in terms of pain relief and Constant, Simple Shoulder Test, American Shoulder and Elbow Surgeons (ASES), and University of California–Los Angeles (UCLA) scores.18, 42, 52
Subscapularis repair in the setting of other associated cuff tears
Burkhart et al reported on 25 shoulders treated with rotator cuff repair involving the subscapularis tendon; 8 of these were isolated subscapularis tendon tears, and 56% of shoulders also had biceps disease. After 11 months of follow-up, 92% had good to excellent results. This study also correlated the severity of the preoperative belly-press test result with the degree of subscapularis tear.10
Adams et al expanded on this study, reporting midterm results of 40 shoulders with rotator cuff tears involving the subscapularis tendon; 7 of these were isolated subscapularis tears, and 63% of shoulders had biceps disease. At 5 years, 88% of the patients were satisfied with their shoulder, with improved ASES and UCLA shoulder scores as well as range of motion (ROM). They confirmed, again, that the belly-press test result correlated with the extent of subscapularis tearing.2
Denard et al reported long-term results of 79 rotator cuff repairs, including 11 isolated subscapularis tears.17 Although results were not separated for isolated vs. combined subscapularis tears, the overall results showed improved UCLA, ASES, and visual analog scale pain scores along with increased forward flexion at 9 years of follow-up.
Lanz et al reported on 46 patients with rotator cuff tears involving a Lafosse type III or IV subscapularis tendon lesion; 6 were isolated subscapularis tendon tears. Three years after arthroscopic repair, patients had improved Constant and UCLA scores and satisfactory recovery of internal rotation strength, and 41 of 46 had intact tendons on MRI.38
Isolated subscapularis tears
Bennett reported on 8 isolated subscapularis tears repaired arthroscopically. All shoulders experienced improvement of ASES, Constant, and visual analog scale scores. No lift-off or belly-press tests were reported.8
Lafosse et al reported on arthroscopic repair of 17 isolated subscapularis tendons with a mean follow-up time of 29 months. Surgery led to improvements in the lift-off test, belly-press test, pain, strength, ROM, Constant score, and UCLA score. Of the 17 patients, 16 were very satisfied or satisfied with their results.36
Bartl et al reported on 21 isolated tears of the subscapularis with 27 months of follow-up. All patients had improved Constant scores, although strength measured by the belly-press and the lift-off tests was decreased. Those shoulders with a positive result of the belly-press test after surgery also had lower Constant scores. MRI performed at most recent follow-up showed an intact repair in 20 of 21 shoulders. However, atrophy of the subscapularis muscle was present in 25% of patients at most recent follow-up.7
Grueninger et al specifically reported on isolated Lafosse type III and IV subscapularis tears. Eleven patients underwent arthroscopic repair with improvement in strength postoperatively. Postoperative MRI showed tendon healing in all tendons with no change in fatty infiltration.30
Nové-Josserand et al reported on 47 shoulders with isolated subscapularis tears at 3.5 years after surgery; 25 of these underwent arthroscopic repair and 22 underwent open repair. In all cases, Constant score improved postoperatively. Postoperatively, the belly-press test result was normal more frequently in complete tears than in incomplete tears. Not surprisingly, incomplete tears were associated with minor retraction and complete tears with major retraction. Postoperative imaging revealed a 12.5% retear rate, with half of the tendons increasing fatty infiltration by 1 grade and 10% increasing by 2 grades. Neither preoperative tear size nor tendon retraction could be used in isolation for objective prognosis of repairs of isolated subscapularis tears. Subjective outcomes and strength were better after open repair.51, 52
Heikenfeld et al evaluated 19 isolated subscapularis tendon repairs with 24 months of follow-up. There were 2 retears on clinical examination and MRI but overall improved UCLA and Constant scores.32
Allograft augmentation and anterior capsular reconstruction
Alcid et al reported on 15 anterior capsular reconstructions using hamstring or tibialis allograft anchored to the humerus and anterior glenoid rim.4 Overall, pain and ASES scores improved, and reoperations were attributed to glenohumeral arthritis rather than to graft failure. Several other case reports describe resolution of glenohumeral instability but decreased ROM.33
Tendon transfer
Options for tendon transfer for irreparable subscapularis tendon tear include the pectoralis major, pectoralis minor, and latissimus dorsi tendons.20
Pectoralis major tendon transfer in the setting of irreparable subscapularis tendon tears revealed improved Constant scores and pain relief. Subcoracoid pectoralis transfer fared better than supracoracoid transfers, with no difference in the rates of musculocutaneous nerve injuries. Tendon transfers for shoulders with anterosuperior instability did poorly, whereas those without preoperative instability did better in terms of Constant scores, ROM, and strength.48, 50 Long-term outcomes after pectoralis major transfer show significant clinical improvement with pain relief and strength with a low-rate of progression to salvage using RSA.48
Paladini et al reported on pectoralis minor tendon transfers in 27 patients with anterosuperior rotator cuff tears involving an upper two-thirds irreparable subscapularis tendon tear, grade III fatty infiltration, and irreparable supraspinatus tear. All shoulders experienced improved Constant scores, ROM, and Simple Shoulder Test scores postoperatively, although strength testing did not reveal consistent improvements, likely indicating a tenodesis effect.53
Reverse total shoulder arthroplasty
The outcome of RSA for massive irreparable rotator cuff tears is well reported, but no study has specifically reported on RSA in the setting of isolated irreparable subscapularis tears. The constrained nature of RSA restores stable biomechanics for patients with static anterior subluxation. As such, the value of subscapularis function after RSA is debatable. Studies have found a higher dislocation rate with varying statistical significance but increased postoperative abduction and passive external rotation in RSA without subscapularis repair.19, 23 No differences in scapular notching were appreciated between those with and those without subscapularis repair. These differences in stability are likely dependent on the center of rotation, lateralization, and other implant-related features. These studies were also done on patients undergoing RSA for a variety of reasons, and their overall shoulder mechanics may differ from someone with a chronic subscapularis tear.
Summary
Tears of the subscapularis tendon are no longer forgotten or hidden lesions. Increased diagnostic awareness during history taking and physical examination are the first steps to diagnosis of subscapularis tendon tears. A systematic approach to advanced shoulder imaging improves diagnostic capacity. Once identified, most subscapularis tendon tears can be successfully fixed arthroscopically.
Lafosse type I and type II tears may be fixed with 1 or 2 anchors, most commonly while visualizing intra-articularly from the standard posterior portal; larger Lafosse type III and type IV tears are typically best addressed visualizing from an anterior subacromial portal and require placement of multiple anchors. Tendon mobilization for larger tears is of paramount importance. For Lafosse type V tendon tears, transfer of the pectoralis major has provided mixed results, RSA is commonly considered, and alternative tendon transfers are being developed.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- 1.Adams C.R., Brady P.C., Koo S.S., Narbona P., Arrigoni P., Karnes G.J. A systematic approach for diagnosing subscapularis tendon tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2012;28:1592–1600. doi: 10.1016/j.arthro.2012.04.142. [DOI] [PubMed] [Google Scholar]
- 2.Adams C.R., Schoolfield J.D., Burkhart S.S. The results of arthroscopic subscapularis tendon repairs. Arthroscopy. 2008;24:1381–1389. doi: 10.1016/j.arthro.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Adams C.R., Schoolfield J.D., Burkhart S.S. Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy. 2010;26:1427–1433. doi: 10.1016/j.arthro.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 4.Alcid J.G., Powell S.E., Tibone J.E. Revision anterior capsular shoulder stabilization using hamstring tendon autograft and tibialis tendon allograft reinforcement: minimum two-year follow-up. J Shoulder Elbow Surg. 2007;16:268–272. doi: 10.1016/j.jse.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Arai R., Sugaya H., Mochizuki T., Nimura A., Moriishi J., Akita K. Subscapularis tendon tear: an anatomic and clinical investigation. Arthroscopy. 2008;24:997–1004. doi: 10.1016/j.arthro.2008.04.076. [DOI] [PubMed] [Google Scholar]
- 6.Barth J.R., Burkhart S.S., De Beer J.F. The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006;22:1076–1084. doi: 10.1016/j.arthro.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Bartl C., Salzmann G.M., Seppel G., Eichhorn S., Holzapfel K., Wörtler K. Subscapularis function and structural integrity after arthroscopic repair of isolated subscapularis tears. Am J Sports Med. 2011;39:1255–1262. doi: 10.1177/0363546510396317. [DOI] [PubMed] [Google Scholar]
- 8.Bennett W.F. Arthroscopic repair of isolated subscapularis tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003;19:131–143. doi: 10.1053/jars.2003.50053. [DOI] [PubMed] [Google Scholar]
- 9.Burkhart S.S., Brady P.C. Arthroscopic subscapularis repair: surgical tips and pearls A to Z. Arthroscopy. 2006;22:1014–1027. doi: 10.1016/j.arthro.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 10.Burkhart S.S., Tehrany A.M. Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy. 2002;18:454–463. doi: 10.1053/jars.2002.30648. [DOI] [PubMed] [Google Scholar]
- 11.Chang K.V., Chen W.S., Wang T.G., Hung C.Y., Chien K.L. Associations of sonographic abnormalities of the shoulder with various grades of biceps peritendinous effusion (BPE) Ultrasound Med Biol. 2014;40:313–321. doi: 10.1016/j.ultrasmedbio.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Clark J.M., Harryman D.T., 2nd. Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713–725. [PubMed] [Google Scholar]
- 13.Codman E.A. Complete rupture of the supraspinatus tendon. Operative treatment with report of two successful cases. 1911. J Shoulder Elbow Surg. 2011;20:347–349. doi: 10.1016/j.jse.2010.10.031. [DOI] [PubMed] [Google Scholar]
- 14.D'Addesi L.L., Anbari A., Reish M.W., Brahmabhatt S., Kelly J.D. The subscapularis footprint: an anatomic study of the subscapularis tendon insertion. Arthroscopy. 2006;22:937–940. doi: 10.1016/j.arthro.2006.04.101. [DOI] [PubMed] [Google Scholar]
- 15.Denard P.J., Burkhart S.S. Medialization of the subscapularis footprint does not affect functional outcome of arthroscopic repair. Arthroscopy. 2012;28:1608–1614. doi: 10.1016/j.arthro.2012.02.030. [DOI] [PubMed] [Google Scholar]
- 16.Denard P.J., Burkhart S.S. Arthroscopic recognition and repair of the torn subscapularis tendon. Arthrosc Tech. 2013;2:e373–e379. doi: 10.1016/j.eats.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Denard P.J., Jiwani A.Z., Lädermann A., Burkhart S.S. Long-term outcome of a consecutive series of subscapularis tendon tears repaired arthroscopically. Arthroscopy. 2012;28:1587–1591. doi: 10.1016/j.arthro.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 18.Deutsch A., Altchek D.W., Veltri D.M., Potter H.G., Warren R.F. Traumatic tears of the subscapularis tendon. Clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med. 1997;25:13–22. doi: 10.1177/036354659702500104. [DOI] [PubMed] [Google Scholar]
- 19.Edwards T.B., Williams M.D., Labriola J.E., Elkousy H.A., Gartsman G.M., O'Connor D.P. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:892–896. doi: 10.1016/j.jse.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 20.Elhassan B., Christensen T.J., Wagner E.R. Feasibility of latissimus and teres major transfer to reconstruct irreparable subscapularis tendon tear: an anatomic study. J Shoulder Elbow Surg. 2014;23:492–499. doi: 10.1016/j.jse.2013.07.046. [DOI] [PubMed] [Google Scholar]
- 21.Faruqui S., Wijdicks C., Foad A. Sensitivity of physical examination versus arthroscopy in diagnosing subscapularis tendon injury. Orthopedics. 2014;37:e29–e33. doi: 10.3928/01477447-20131219-13. [DOI] [PubMed] [Google Scholar]
- 22.Foad A., Wijdicks C.A. The accuracy of magnetic resonance imaging and magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy. 2012;28:636–641. doi: 10.1016/j.arthro.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Friedman R.J., Flurin P.H., Wright T.W., Zuckerman J.D., Roche C.P. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg. 2017;26:662–668. doi: 10.1016/j.jse.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 24.Fuchs B., Weishaupt D., Zanetti M., Hodler J., Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. doi: 10.1016/s1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 25.Furukawa R., Morihara T., Arai Y., Ito H., Kida Y., Sukenari T. Diagnostic accuracy of magnetic resonance imaging for subscapularis tendon tears using radial-slice magnetic resonance images. J Shoulder Elbow Surg. 2014;23:e283–e290. doi: 10.1016/j.jse.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Gerber C., Hersche O., Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996;78:1015–1023. doi: 10.2106/00004623-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Gerber C., Krushell R.J. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991;73:389–394. doi: 10.1302/0301-620X.73B3.1670434. [DOI] [PubMed] [Google Scholar]
- 28.Gladstone J.N., Bishop J.Y., Lo I.K., Flatow E.L. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–728. doi: 10.1177/0363546506297539. [DOI] [PubMed] [Google Scholar]
- 29.Goutallier D., Postel J., Bernageau J., Lavau L., Voisin M. Fatty infiltration of disrupted rotator cuff muscles. Rev Rhum Engl Ed. 1995;62:415–422. [PubMed] [Google Scholar]
- 30.Grueninger P., Nikolic N., Schneider J., Lattmann T., Platz A., Chmiel C. Arthroscopic repair of traumatic isolated subscapularis tendon lesions (Lafosse type III or IV): a prospective magnetic resonance imaging–controlled case series with 1 year of follow-up. Arthroscopy. 2014;30:665–672. doi: 10.1016/j.arthro.2014.02.030. [DOI] [PubMed] [Google Scholar]
- 31.Hauser E.D. Avulsion of the tendon of the subscapularis muscle. J Bone Joint Surg Am. 1954;36-A:139–141. [PubMed] [Google Scholar]
- 32.Heikenfeld R., Gigis I., Chytas A., Listringhaus R., Godolias G. Arthroscopic reconstruction of isolated subscapularis tears: clinical results and structural integrity after 24 months. Arthroscopy. 2012;28:1805–1811. doi: 10.1016/j.arthro.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 33.Iannotti J.P., Antoniou J., Williams G.R., Ramsey M.L. Iliotibial band reconstruction for treatment of glenohumeral instability associated with irreparable capsular deficiency. J Shoulder Elbow Surg. 2002;11:618–623. doi: 10.1067/mse.2002.126763. [DOI] [PubMed] [Google Scholar]
- 34.Jobe F.W., Tibone J.E., Perry J., Moynes D. An EMG analysis of the shoulder in throwing and pitching. A preliminary report. Am J Sports Med. 1983;11:3–5. doi: 10.1177/036354658301100102. [DOI] [PubMed] [Google Scholar]
- 35.Keating J.F., Waterworth P., Shaw-Dunn J., Crossan J. The relative strengths of the rotator cuff muscles. A cadaver study. J Bone Joint Surg Br. 1993;75:137–140. doi: 10.1302/0301-620X.75B1.8421011. [DOI] [PubMed] [Google Scholar]
- 36.Lafosse L., Jost B., Reiland Y., Audebert S., Toussaint B., Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89:1184–1193. doi: 10.2106/JBJS.F.00007. [DOI] [PubMed] [Google Scholar]
- 37.Lafosse L., Lanz U., Saintmard B., Campens C. Arthroscopic repair of subscapularis tear: surgical technique and results. Orthop Traumatol Surg Res. 2010;96(Suppl 8):S99–108. doi: 10.1016/j.otsr.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Lanz U., Fullick R., Bongiorno V., Saintmard B., Campens C., Lafosse L. Arthroscopic repair of large subscapularis tendon tears: 2- to 4-year clinical and radiographic outcomes. Arthroscopy. 2013;29:1471–1478. doi: 10.1016/j.arthro.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 39.Lazarides A.L., Alentorn-Geli E., Choi J.H., Stuart J.J., Lo I.K., Garrigues G.E. Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg. 2015;24:1834–1843. doi: 10.1016/j.jse.2015.05.031. [DOI] [PubMed] [Google Scholar]
- 40.Lo I.K., Burkhart S.S. The comma sign: an arthroscopic guide to the torn subscapularis tendon. Arthroscopy. 2003;19:334–337. doi: 10.1053/jars.2003.50080. [DOI] [PubMed] [Google Scholar]
- 41.Lo I.K., Burkhart S.S. Transtendon arthroscopic repair of partial-thickness, articular surface tears of the rotator cuff. Arthroscopy. 2004;20:214–220. doi: 10.1016/j.arthro.2003.11.042. [DOI] [PubMed] [Google Scholar]
- 42.Mall N.A., Chahal J., Heard W.M., Bach B.R., Jr, Bush-Joseph C.A., Romeo A.A. Outcomes of arthroscopic and open surgical repair of isolated subscapularis tendon tears. Arthroscopy. 2012;28:1306–1314. doi: 10.1016/j.arthro.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 43.Mansat P., Frankle M.A., Cofield R.H. Tears in the subscapularis tendon: descriptive analysis and results of surgical repair. Joint Bone Spine. 2003;70:342–347. doi: 10.1016/s1297-319x(03)00044-7. [DOI] [PubMed] [Google Scholar]
- 44.Marquardt B., Garmann S., Hurschler C., Potzl W., Steens W., Witt K.A. The influence of arthroscopic subscapularis tendon and anterior capsular release on glenohumeral translation: a biomechanical model. J Shoulder Elbow Surg. 2006;15:502–508. doi: 10.1016/j.jse.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 45.Melis B., Nemoz C., Walch G. Muscle fatty infiltration in rotator cuff tears: descriptive analysis of 1688 cases. Orthop Traumatol Surg Res. 2009;95:319–324. doi: 10.1016/j.otsr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 46.Meyer D.C., Zimmermann S.M., Wieser K., Bensler S., Gerber C., Germann M. Lengthening of the subscapularis tendon as a sign of partial tearing in continuity. J Shoulder Elbow Surg. 2016;25:31–37. doi: 10.1016/j.jse.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 47.Miller M.D., Wiesel S.W. Lippincott Williams & Wilkins; Philadelphia: 2012. Operative techniques in sports medicine surgery. [Google Scholar]
- 48.Moroder P., Schulz E., Mitterer M., Plachel F., Resch H., Lederer S. Long-term outcome after pectoralis major transfer for irreparable anterosuperior rotator cuff tears. J Bone Joint Surg Am. 2017;99:239–245. doi: 10.2106/JBJS.16.00485. [DOI] [PubMed] [Google Scholar]
- 49.Narasimhan R., Shamse K., Nash C., Dhingra D., Kennedy S. Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop. 2016;40:975–979. doi: 10.1007/s00264-015-3043-9. [DOI] [PubMed] [Google Scholar]
- 50.Nelson G.N., Namdari S., Galatz L., Keener J.D. Pectoralis major tendon transfer for irreparable subscapularis tears. J Shoulder Elbow Surg. 2014;23:909–918. doi: 10.1016/j.jse.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 51.Nové-Josserand L., Hardy M.B., Leandro Nunes Ogassawara R., Carrillon Y., Godenèche A. Clinical and structural results of arthroscopic repair of isolated subscapularis tear. J Bone Joint Surg Am. 2012;94:e125. doi: 10.2106/JBJS.K.00008. [DOI] [PubMed] [Google Scholar]
- 52.Nové-Josserand L., Saffarini M., Hannink G., Carrillon Y. Influence of pre-operative tear size and tendon retraction on repair outcomes for isolated subscapularis tears. Int Orthop. 2016;40:2559–2566. doi: 10.1007/s00264-016-3299-8. [DOI] [PubMed] [Google Scholar]
- 53.Paladini P., Campi F., Merolla G., Pellegrini A., Porcellini G. Pectoralis minor tendon transfer for irreparable anterosuperior cuff tears. J Shoulder Elbow Surg. 2013;22:e1–e5. doi: 10.1016/j.jse.2012.12.030. [DOI] [PubMed] [Google Scholar]
- 54.Pfirrmann C.W., Zanetti M., Weishaupt D., Gerber C., Hodler J. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology. 1999;213:709–714. doi: 10.1148/radiology.213.3.r99dc03709. [DOI] [PubMed] [Google Scholar]
- 55.Richards D.P., Burkhart S.S., Lo I.K. Subscapularis tears: arthroscopic repair techniques. Orthop Clin North Am. 2003;34:485–498. doi: 10.1016/s0030-5898(03)00096-8. [DOI] [PubMed] [Google Scholar]
- 56.Sahu D., Fullick R., Giannakos A., Lafosse L. Sentinel sign: a sign of biceps tendon which indicates the presence of subscapularis tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2016;24:3745–3749. doi: 10.1007/s00167-014-3243-7. [DOI] [PubMed] [Google Scholar]
- 57.Shi L.L., Mullen M.G., Freehill M.T., Lin A., Warner J.J., Higgins L.D. Accuracy of long head of the biceps subluxation as a predictor for subscapularis tears. Arthroscopy. 2015;31:615–619. doi: 10.1016/j.arthro.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 58.Smith J.G. The classic: pathological appearances of seven cases of injury of the shoulder-joint: with remarks. 1834. Clin Orthop Relat Res. 2010;468:1471–1475. doi: 10.1007/s11999-010-1231-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Studler U., Pfirrmann C.W., Jost B., Rousson V., Hodler J., Zanetti M. Abnormalities of the lesser tuberosity on radiography and MRI: association with subscapularis tendon lesions. AJR Am J Roentgenol. 2008;191:100–106. doi: 10.2214/AJR.07.3056. [DOI] [PubMed] [Google Scholar]
- 60.Ticker J.B., Burkhart S.S. Why repair the subscapularis? A logical rationale. Arthroscopy. 2011;27:1123–1128. doi: 10.1016/j.arthro.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 61.Tokish J.M., Decker M.J., Ellis H.B., Torry M.R., Hawkins R.J. The belly-press test for the physical examination of the subscapularis muscle: electromyographic validation and comparison to the lift-off test. J Shoulder Elbow Surg. 2003;12:427–430. doi: 10.1016/S1058-2746(03)00047-8. [DOI] [PubMed] [Google Scholar]
- 62.Visona E., Cerciello S., Godeneche A., Neyton L., Fessy M.H., Nové-Josserand L. The “comma sign”: an anatomical investigation (dissection of the rotator interval in 14 cadaveric shoulders) Surg Radiol Anat. 2015;37:793–798. doi: 10.1007/s00276-015-1420-0. [DOI] [PubMed] [Google Scholar]
- 63.Walch G., Nové-Josserand L., Levigne C., Renaud E. Tears of the supraspinatus tendon associated with “hidden” lesions of the rotator interval. J Shoulder Elbow Surg. 1994;3:353–360. doi: 10.1016/S1058-2746(09)80020-7. [DOI] [PubMed] [Google Scholar]
- 64.Warner J.J., Higgins L., Parsons I.M., 4th, Dowdy P. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001;10:37–46. doi: 10.1067/mse.2001.112022. [DOI] [PubMed] [Google Scholar]
- 65.Wright J.M., Heavrin B., Hawkins R.J., Noonan T. Arthroscopic visualization of the subscapularis tendon. Arthroscopy. 2001;17:677–684. doi: 10.1053/jars.2001.25274. [DOI] [PubMed] [Google Scholar]
- 66.Yoo J.C., Rhee Y.G., Shin S.J., Park Y.B., McGarry M.H., Jun B.J. Subscapularis tendon tear classification based on 3-dimensional anatomic footprint: a cadaveric and prospective clinical observational study. Arthroscopy. 2015;31:19–28. doi: 10.1016/j.arthro.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 67.Yoon J.P., Chung S.W., Kim S.H., Oh J.H. Diagnostic value of four clinical tests for the evaluation of subscapularis integrity. J Shoulder Elbow Surg. 2013;22:1186–1192. doi: 10.1016/j.jse.2012.12.002. [DOI] [PubMed] [Google Scholar]