Abstract
Background
Armed conflicts affect more than one in 10 children globally. While there is a large literature on mental health, the effects of armed conflict on children’s physical health and development are not well understood. This systematic review summarizes the current and past knowledge on the effects of armed conflict on child health and development.
Methods
A systematic review was performed with searches in major and regional databases for papers published 1 January 1945 to 25 April 2017. Included studies provided data on physical and/or developmental outcomes associated with armed conflict in children under 18 years. Data were extracted on health outcomes, displacement, social isolation, experience of violence, orphan status, and access to basic needs. The review is registered with PROSPERO: CRD42017036425.
Findings
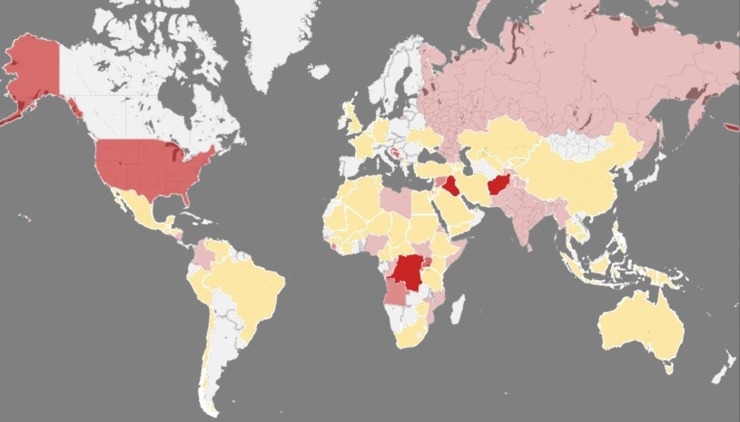
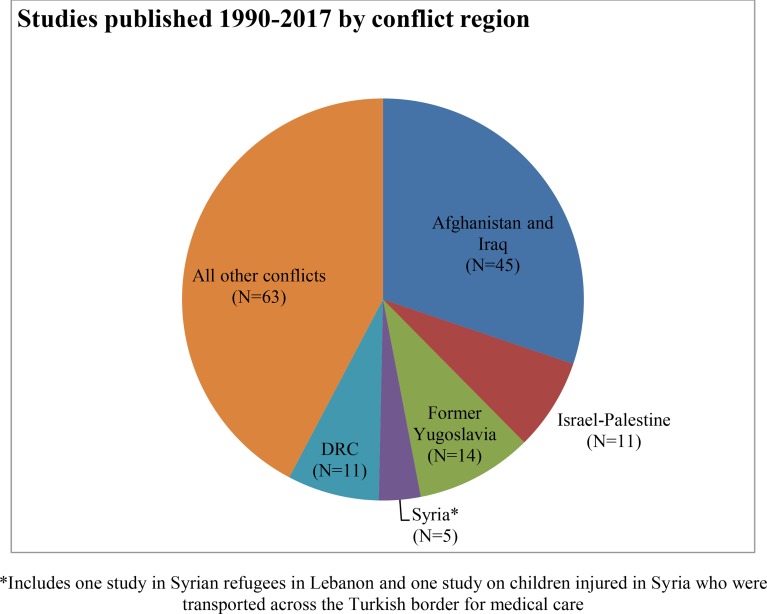
Among 17,679 publications screened, 155 were eligible for inclusion. Nearly half of the 131 quantitative studies were case reports, chart or registry reviews, and one-third were cross-sectional studies. Additionally, 18 qualitative and 6 mixed-methods studies were included. The papers describe mortality, injuries, illnesses, environmental exposures, limitations in access to health care and education, and the experience of violence, including torture and sexual violence. Studies also described conflict-related social changes affecting child health. The geographical coverage of the literature is limited. Data on the effects of conflict on child development are scarce.
Interpretation
The available data document the pervasive effect of conflict as a form of violence against children and a negative social determinant of child health. There is an urgent need for research on the mechanisms by which conflict affects child health and development and the relationship between physical health, mental health, and social conditions. Particular priority should be given to studies on child development, the long term effects of exposure to conflict, and protective and mitigating factors against the harmful effects of armed conflict on children.
Introduction
Millions of children are thought to be impacted by armed conflict worldwide, with estimates for the number of children living in areas affected by conflicts ranging as high as 246 million.[1] Over the past several decades schools, health facilities, and health workers have become direct targets, increasing the impact of war on children.[2, 3] Of the 49 armed conflicts that occurred in 2016, 12 were wars (Fig 1).[4, 5]
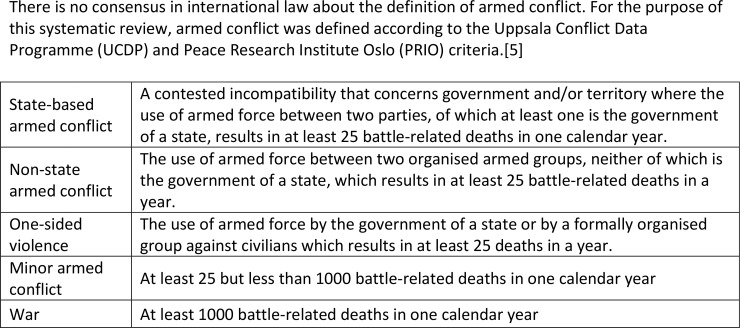
Fig 1. Definitions of armed conflict and conflict intensity.
Children who are exposed either directly or indirectly to armed conflict suffer harm that persists across their life course and beyond, to subsequent generations born after the conflict has ended. Although this impact has been anecdotally chronicled in news reports and literature, there is limited medical and public health research on how conflict affects on child physical health and development. Even the number of children directly or indirectly affected by conflict remains unclear.
The direct effects of combat on child health may include injury, illness, psychological trauma, and death. A complex set of political, social, economic, and environmental factors resulting from conflicts have indirect and lasting effects on children. Inadequate living conditions, environmental hazards, such as damaged buildings and unexploded ordnance, and lack of access to safe water and sanitation place children at risk for preventable and treatable diseases and injuries. The destruction of medical and public health infrastructure make it difficult to treat affected children by limiting both access and quality of available care.
Conflicts force children and families to leave their homes to seek safety within national borders (internal displacement) and across international borders—nearly two-thirds of the 28 million forcibly displaced children are internally displaced.[6] During flight, children may become separated from their families and are more vulnerable to infections, psychological trauma, and exploitation.[7, 8] Experiences of trauma affect children’s mental health, as well as that of their caregivers. Poor mental health of caregivers may negatively affect children’s physical and mental health, as well as their educational attainment and life opportunities.[8, 9] The destruction of educational and economic infrastructure creates conditions of poverty, which may last for generations. Economic and political sanctions deepen this poverty and have detrimental effects on child health and nutrition.[10]
Little is known about the impact of armed conflict on children’s physical health and development—even estimates of the number of children killed by conflict are lacking.[11–14] Research has focused primarily on the mental health effects of armed conflict on children and on downstream effects such as displacement.[9, 15–20] We undertook a systematic review of the evidence of the impact of armed conflict on children’s physical health and child development. Where available, risk factors, mitigating factors, and protective factors were abstracted.
Methods
Search strategy and selection criteria
Searches were undertaken in PubMed, Web of Science, CINAHL, EMBASE, Latin American and Caribbean Health Science (LILACS), IndMED, Africa-Wide Information, Open Grey and the New York Academy of Medicine Grey Literature Report from 1 January 1945 to the search date. The initial searches were performed 8–12 June 2015. The PubMed and EMBASE searches were updated on the 24 and 25 April 2017, respectively. The review is registered with PROSPERO: CRD42017036425.
Our intention was to perform a systematic review and meta-analysis of available data on the physical health and developmental effects of armed conflict on children. During the searches, it became clear that the varied focus, heterogeneous design, and variation in reporting of outcomes by published studies would not support this type of review. The aim of our review was therefore shifted to describe published studies on the effects of armed conflict on child health and development.
Search terms included multiple variants of “child” and “war.” Terms for physical health and child development were not used, as inclusion of these terms narrowed the search results and missed relevant papers known to the authors. The search terms used are provided in the web appendix. Medical Subject Headings terms were used when available, and snowball and hand searching was used to identify additional studies.
Screening and full text review was conducted by Ayesha Kadir (AK) and Sherry Shenoda (SS) for all publications using Covidence,[21] an electronic organisational tool for systematic reviews. Inclusion criteria included study population, setting of past or current armed conflict or a region where refugees/asylum-seekers are staying, and exposure of the study population to armed conflict. Armed conflict was defined according to the Uppsala Conflict Data Programme (UCDP)/Peace Research Institute Oslo (PRIO) criteria (Fig 1).[5] The UCDP database was used to identify conflicts meeting criteria for inclusion.[22] We included original research studies that provided data on children ages 0–18 years. Outcomes included physical or developmental morbidity associated with exposure to armed conflict, exposure to violence, and access to basic needs, including health care and education. Studies on mental and behavioural health were excluded unless they also provided data on physical health or child development. Additional exclusion criteria included review papers, studies published prior to 1945, and studies with a median date of data collection earlier than 1940. Studies on terrorism were excluded, as terrorist incidents are not universally associated with armed conflict. The Palestinian-Israeli conflict was considered to be an armed conflict. Studies providing data exclusively on nutrition, perinatal mortality, birth weight, breast and infant feeding, and immunization coverage were excluded; while the evidence remains limited on the scale and nature of the impact of armed conflict on these indicators, child nutrition and maternal and newborn health are broadly recognised as carrying high risk in conflict settings.[23, 24] However, if these data were presented together with other child health and development outcomes, then data for all reported child health and development outcomes were extracted. Studies on the effects of exposure to the atomic bomb were excluded, as there are existing reviews on this subject. Post war studies were included if they provided associations of the outcomes with armed conflict. No restrictions were made for sex, geographic location, language, or study design.
The risk of bias was assessed at the study ad outcome levels for each individual study based on the data source, study population, sampling strategy, data collection and analysis methods, and any special characteristics of the population. Studies that were deemed to have unsound or invalid methods were excluded. Given the challenges in obtaining data in conflict settings, studies from single facilities, studies using only facility-based data, and case reports were included. Data from studies meeting inclusion criteria were abstracted onto a data extraction form, including time period, study country and sub-region, identified conflict, study design, reference population, type of exposure, health outcomes, access to basic needs, mortality, and associations between exposures and outcomes. Where available, data were abstracted for protective and mitigating factors on child health outcomes. When possible, authors were contacted for missing data. In the case of queries or differences, an agreement was negotiated between the reviewers.
Role of the funding source
The University of Florida-Jacksonville provided partial funding for the study. There was no additional external funding received for this study. The study design, data collection, analysis, interpretation of data, and writing of the report were undertaken independently. All authors had full access to all the data in the study and they shared responsibility for the decision to submit for publication.
Results
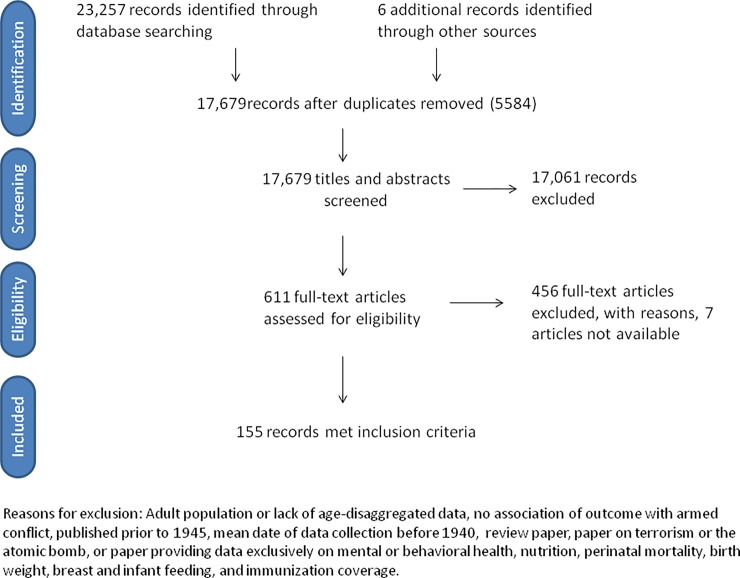
The searches retrieved 23,257 records, and six additional papers were retrieved through snowball and hand searching. After removal of duplicates, 17,679 titles and abstracts were screened. Of 618 papers eligible for full-text review, 7 were not available. 611 papers were reviewed in full text. 456 studies were excluded, with reasons (Fig 2). Our final sample consisted of 155 studies, including 18 published between July 2015 and April 2017.
Fig 2. Flow diagram.
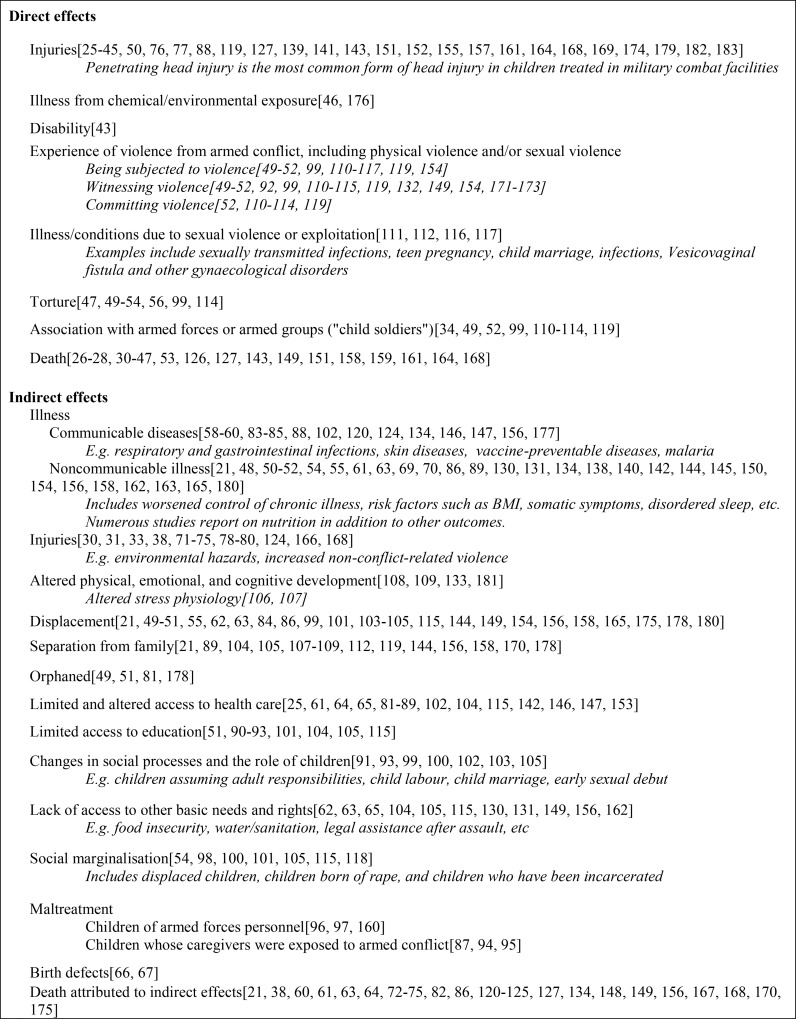
Among the included publications, 131 were quantitative studies, 18 qualitative, and six were mixed methods design. Included in the quantitative studies were 20 case reports, 44 chart or registry reviews, and 48 cross-sectional studies. The data from these studies is too heterogeneous to be pooled for meta-analysis. Collectively, they provide a body map of the child affected by armed conflict (Table 1 and Fig 3).
Table 1. Summary of included studies.
| Studies published 1 January 1945–12 June 2015 | |||||
| Autdor | Conflict zone | Population | Sample size | Summary of findings | |
| 1 | Aaby et al,[21] 1999 | Guinea Bissau | IDP and resident children | 422 | During the period of displacement, child mortality increased and nutritional status deteriorated for both IDP children from Bissau and resident children. Mortality for resident children was 4.5 times higher, decline in growth was significantly worse, and recovery later than for displaced children. |
| 2 | Abushaban et al,[66] 2004 | Kuwait | Kuwaiti infants with CHD | 2,256 | 2,256 babies with congenital heart disease (CDH). The mean annual incidence of CHD rose from 39.5 per 10 000 live births pre-war (1986–1989) to 103.4 per 10 000 live births post war (1992–2000) |
| 3 | Amitai et al,[138] 1992 | Israel-Palestine | Emergency department cases | 268 | Accidental atropine poisoning in children from atropine autoinjector provided to families in case of organophosphate nerve gas attacks. |
| 4 | Araneta et al,[67] 2003 | Iraq | Infants born to US military personnel who served in February 1991 | 45,013 | Increased prevalence of congenital disorders in infants conceived post-war to Gulf War veterans (GWV). Infants of GWV men had increased rate of tricuspid insufficiency or regurgitation, aortic stenosis, and renal agenesis or hypoplasia. Infants of female GWVs had higher prevalence of hypospadias. |
| 5 | Ascherio et al,[60] 1992 | Iraq | National | 16,076 | Three-fold increase in infant and child mortality after start of conflict. Four-fold and five-fold increases in age-adjusted mortality from injuries and diarrhoea, respectively. Regional differences in child mortality were maintained or exacerbated after onset of conflict. |
| 6 | Avogo and Agadjanian,[86] 2010 | Angola | Migrants to Luanda | 719 | Increased mortality among children whose families were displaced due to war. This effect was strongest during the first year after migration. |
| 7 | Barisić et al,[139] 1999 | Former Yugoslavia | Children with nerve injuries | 27 | Peripheral nerve injuries in children due to war involved multiple nerves, were located proximally on upper extremities, had complete or severe nerve damage, delayed reinnervation and poor spontaneous recovery outcomes. These patterns differed from children with peripheral nerve injury due to accidents, who primarily had single, partial peripheral nerve injuries that were located on distal extremities. |
| 8 | Barnes et al,[140] 2007 | Iraq | US high school students | 121 | Children of deployed military personnel had significantly higher BMI than non-deployed and civilian counterparts. Children of both deployed- and non-deployed military personnel had a higher mean HR than children of civilians. |
| 9 | Bertani et al,[141] 2015 | Afghanistan | Patients <16 years in a NATO military combat hospital | 89 | Injuries due to explosive device were more common in children than from firearms and were associated with a high rate of both traumatic and surgical amputation. All fractures were open fractures, with high rates of vessel and nerve injuries. |
| 10 | Betancourt et al,[111] 2008 | Sierra Leone | Former child soldiers | 260 | Child soldiers describe witnessing violence, becoming soldiers for survival, child labour, sexual violence, and unwanted pregnancy. |
| 11 | Betancourt et al,[110] 2010 | Sierra Leone | Former child soldiers | 156 | Average abduction age 10.5 years, nearly all were forced into conscription, nearly all reported witnessing violence, more than 1/4 had killed someone (including a loved one) and 1/3 of girls reported being raped |
| 12 | Bilukha and Brennan,[71] 2005 | Afghanistan | Injuries due to landmine or UXO | 6,114 | UN database, 1997–2002. 54% of UXO injuries were in children, the majority between ages 5–14 years. Of these, 42% were injured while playing with the device” |
| 13 | Bilukha et al,[73] 2003 | Afghanistan | Injuries due to landmine or UXO | 1,636 | ICRC database 2001–2002: 46% of UXO injuries were in children under 16 years. 49% of children injured were playing or tending animals. |
| 14 | Bilukha et al,[75] 2006 | Chechnya | Civilian injuries due to landmine or UXO | 3,021 | Region wide data, 1994–2005. 26% of UXO injuries were in children under 18 years, with 17% mortality rate in these children. 35% of children with upper body injuries, 20% with lower body injury, 24% with both upper and lower body injury, and 26% had limb amputations. |
| 15 | Bilukha et al,[72] 2008 | Afghanistan | Injuries due to landmine or UXO | 5,471 | ICRC database, 2002–2006. 47% of injuries and deaths were in children. 42% of child UXO injuries were upper body and 27% were both upper and lower body injuries. 2/3 of child injuries occurred during active hostilities. 2/3 were in children tending animals or tampering or playing with an explosive device |
| 16 | Bilukha et al,[74] 2011 | Nepal | Injuries due to landmine or UXO | 307 | National prospective surveillance 2006–2010. 55% of injuries were in children under 18 years, with 15% mortality rate in these children. Nearly two-thirds of child injuries occurred while playing or tampering with an explosive device, the greatest number in children aged 10–14 years old. 40% of explosions occurred in victim's homes. |
| 17 | Bodalal et al,[142] 2014 | Libya | Deliveries at a single health facility | 13,031 | Prevalence of preterm deliveries and LBW increased during the conflict when compared with pre-war. There was a higher rate of caesarean section delivery and episiotomy during the conflict. |
| 18 | Bogdanovich and Schevchenko,[25] 1946 | WWII | Paediatric eye injuries at a single tertiary facility | 220 | Incidence of ocular trauma increased 3.2 during armed conflict compared with peacetime. 84% of cases were in school-aged children.85% injuries were from weapons of war. Half of children presented 6 days or later after injury. |
| 19 | Borgman et al,[41] 2012 | Afghanistan and Iraq | Paediatric patients treated at US military combat facilities | 7,505 | Data from Patient Administration Systems and Biostatistics Activity Database (PASBA) and Joint Theatre Trauma Registry (JTTR). 79% of paediatric admissions were due to trauma. Paediatric trauma patients had higher mortality and longer hospital stays than adult comparison groups. Most common Injury mechanisms were blast, penetrating, blunt trauma, and burns. Children under <8 years had higher mortality than children >8 years. |
| 20 | Borgman et al,[143] 2015 | Afghanistan and Iraq | Isolated burn patients treated in US military combat facilities | 4,743 | Paediatric burns patients in conflict zones have higher mortality compared with patients in the United States. |
| 21 | Bosnjak et al,[89] 2002 | Former Yugoslavia | Children with seizures in two facilities | 111 | Displaced children from war-affected areas had worsened epilepsy control, with greater frequency of epileptic seizures and less regular follow up. These children were also more likely to be separated from their fathers or both parents than children from areas not directly affected by the war. Medication compliance was similar in both groups. |
| 22 | Bronstein and Montgomery,[144] 2013 | Afghanistan | Unaccompanied minors in state care in London | 222 | Nearly 2/3 of children reported sleep disturbance in the form of nightmares |
| 23 | Busby et al,[145] 2010 | Iraq | Households in Fallujah | 711 | Risk ratio 12.6 for childhood cancer in children in Fallujah 0–14 years compared with peers in Egypt and Jordan. |
| 24 | Celikel et al,[26] 2015 | Syria | Syrian children injured due to war in Syria who died in a single Turkish facility | 140 | 18% of in-hospital deaths were children, median age was 12. 70% of injuries were from bombing and shrapnel, 13.6% gunshot wounds, 13.6% blunt force and 2.8% motor vehicle crashes while trying to escape. 2/3 of paediatric deaths were due to head injuries, and 30% had isolated head and neck injuries |
| 25 | Chironna et al,[146] 2001 | Kosovo | Kosovar refugee children and youth in camps in Italy | 371 | 251 children ≤10 years, 119 were 11–20 years. Hyperendemic Hepatitis with exposure in early childhood. 61% of children aged 2–1 0 years were seropositive and 100% of children over 11 years were HAV seropositive. 11% of children 2–10 years were HBV positive and 39% of children and youth aged 11–20 were HBV positive. No children had been vaccinated against HBV. |
| 26 | Chironna et al,[147] 2003 | Iraq and Turkey | Kurdish refugee children and youth in camps in Italy | 269 | 98 children ≤10 years, 171 were 11–20 years. Hyperendemic Hepatitis A, High seroprevalence of Hepatitis E, with 89% of Hepatitis E exposed from Iraq. Hepatitis B was also endemic, and children from both Turkey and Iraq had low vaccination rates against Hepatitis B. |
| 27 | Cliff et al,[130] 1997 | Mozambique | Children in Mogincual district, Mozambique | 228 | High rates of malnutrition in war-affected areas, with a two-year outbreak of clinical Konzo. Konzo was attributed to shortened cassava processing due to war-related disruption |
| 28 | Cohn et al,[48] 1979 | Chile | Chilean refugee children in Denmark | 75 | All children were either tortured, had a parent who was tortured, or had a parent who was imprisoned in Chile. One third of children had sleep disturbances including nightmares and difficulty falling asleep. 1/4 reported nocturnal enuresis. Numerous somatic complaints, including anorexia, headaches, abdominal pain, difficulty concentrating, impaired memory, and constipation. |
| 29 | Coppola et al,[27] 2006 | Iraq | Paediatric cases treated at a US military combat facility | 85 | Data from surgical logs. Patterns of trauma included fragmentation wound (52%), penetrating trauma (23%), burn (19%), and blunt trauma (6%). The primary injury site was the lower extremities in 38%, followed by head injury (23%). |
| 30 | Cowan et al,[68] 1997 | Iraq | Live births to military service members | 75,461 | No elevated risk of birth defects, reduced fertility or differences in sex ratio was found among veterans of the first Gulf War. |
| 31 | Creamer et al,[28] 2009 | Afghanistan and Iraq | Paediatric patients treated in US military combat facilities | 2,060 | Data from PASBA database. Children accounted for a tenth of all combat support hospital admissions, the majority of which suffered penetrating trauma. Gunshot wounds were more common in Iraq, while burns and landmine injuries were more common in Afghanistan. Younger age was associated with higher mortality. |
| 32 | Curlin et al,[120] 1976 | Bangladesh | Population in Matlab Bazaar, Bangladesh | 120,000 | During the war, overall infant mortality rate rose 15% above baseline, of which the post-neonatal infant mortality rose 46%. Mortality in 1–4 year olds rose 43%. Mortality for all U5 subgroups returned to baseline during the year after the war. Among children 5–9 years olds, mortality rose 208% during the war and continued to rise during the year after, to 281% above baseline, attributed to smallpox and dysentery epidemics. |
| 33 | de Smedt,[103] 1998 | Rwanda | Rwandan refugees in Tanzania | 6 | Describes complex changes in social norms after the displacement due to conflict. Child marriage became common, with the median age of girls 15 years, and 15 years for boys. Marriages were reported in girls as young as 13 and boys as young as 14. |
| 34 | Deeb et al,[148] 1997 | Lebanon | Children in Beirut | 4101 | Muslim children had 1.6 times the risk of dying before 5 years compared to Christians. When controlling for the number of children ever born to the mothers, elevated risk of U5 mortality remained significant for lowest social class of Muslims only. |
| 35 | Denov,[112] 2010 | Sierra Leone | Former child soldiers | 80 | Describes children’s involvement with armed groups in detail. Children acted as front-line combatants, commanders of other child soldiers, spies, porters, cooks, domestic servants, and care-takers of younger children. The children described being subjected to extreme physical, psychological, and sexual violence, as well as injuries, chronic pain, loss of family and social and economic marginalisation. |
| 36 | Depoortere et al,[149] 2004 | Darfur, Sudan | IDPs in Darfur | 17,339 | In two villages affected by armed conflict, 5% and 34.5% of violent deaths were in children under 15. One refugee camp had markedly elevated non-violent mortality, of which 48% of deaths were in children under 5 years |
| 37 | Devanarayana and Rajindrajith,[150] 2010 | Sri Lanka | Children in two schools in war affected regions | 2,699 | Living in a war-affected area was independently associated with constipation (adjusted OR 1.48). |
| 38 | Di Maio and Nandi,[91] 2013 | Israel-Palestine | Palestinian boys 10–14 years in the West Bank | 45,419 | Closure of the border between Israel and the West Bank significantly increased the probability of child labour. A 10 day increase in the quarterly number of school closure days increased the probability of child labour by 11%. |
| 39 | Dickson-Gómez,[99] 2002 | El Salvador | Former child soldiers | 4 | Describes the experiences of child soldiers including witnessing and being subjected to torture, imprisonment, displacement, loss of family, being orphaned, assumption of adult roles and responsibilities, child marriage, teen pregnancy, and difficulty reintegrating into their communities. |
| 40 | Edwards et al,[151] 2012 | Afghanistan | Trauma patients in US military combat facilities | 1,205 | Data from JTTR. Children <15 years accounted for more than half of severe head and neck injuries. Children ≤7 years or younger were more likely injured by mortar fragments, while children 8–14 years were higher risk for land mine or UXO injury. |
| 41 | Edwards et al,[152] 2014 | Afghanistan and Iraq | Trauma patients in US military combat facilities | 1,205 | Data from JTTR. Children <15 years accounted for 25% of civilian admissions 2002–2010. Infants and young children ≤3 years most often required neurosurgical procedures. Extremity amputation and external fixation were more common in children >4 years |
| 42 | Eide et al,[153] 2010 | multiple | Children of US military personnel | 169,986 | During deployment, children of single parents had lower outpatient visit rates while children of married parents had increased visit rates. Parent age <24 years and single marital status were associated with lower visit rates. There was an overall increase in outpatient visits and well-child visits during deployment compared with periods when the parent was not deployed. |
| 43 | Elbert et al,[154] 2009 | Sri Lanka | 5th graders in north-eastern Sri Lanka | 420 | 77% of children had been displaced at least once. 92% had experienced violence from the war including combat, bombing, shelling, or witnessing the death of a loved one. |
| 44 | Erjavec and Volcic,[100] 2010 | Former Yugoslavia | Adolescent girls born of war-related rape | 11 | The adolescents describe social isolation from the mother's ethnic group, as well as being assaulted, shot at and threatened with rape. They also described taking on the role of carer for incapacitated mothers. |
| 45 | Feldman et al,[106] 2013 | Israel-Palestine | War-exposed and non-exposed children 1.5–5 years | 232 | War-exposed cohort had lower baseline cortisol levels and less reactivity to stress than the non-exposed cohort. Children’s baseline cortisol levels were independently related to maternal baseline cortisol lower maternal reciprocity, and greater maternal psychopathology. |
| 46 | Garfield and Leu,[121] 2000 | Iraq | Children U5 | 8,191 | Used MICS 1996 survey data. U5 mortality more than tripled during the war, then fell afterwards during post-war conflict and sanctions, but remained at least twice the pre-war level. |
| 47 | Gasparovic et al,[76] 2004 | Former Yugoslavia | Case report | 1 | 9 year old girl with injuries due to UXO, including intracranial shrapnel, intracardiac shrapnel, multiple intestinal perforations, multifragmentary fracture of the right distal humerus, and explosive injuries of the soft tissues of the right thigh and right foot. |
| 48 | Gataa and Muassa,[155] 2011 | Iraq | Patients at 2 facilities | 551 | One-fifth of patients with maxillofacial injuries were children <15 years |
| 49 | Geltman et al,[50] 2005 | Sudan | Sudanese unaccompanied minors in foster care in the US | 304 | One fifth of the youth reported being tortured and 29% sustained war-related physical injuries. They reported near-drowning, near-suffocation, head trauma, and loss of consciousness. The youths reported seeking health care for a variety of somatic symptoms including headaches, stomach aches, anorexia, and chest pains. Nearly 1/3 had sleep disturbances. |
| 50 | Gessner,[62] 1994 | Afghanistan | Displaced and resident families in Kabul | 612 | Displaced families lived with a mean of 15 people per room compared with residents, who had a mean of 2 people per room. The average number of people per toilet for displaced persons was 44, and two locations for displaced people had no working toilets. |
| 51 | Ghobarah et al,[57] 2004 | multiple | Populations in countries after civil war | Not specified | Significant reduction in DALYs for all disease categories in children <15 years, most commonly due to infectious diseases, and with the most severe reductions in children under 5. This effect was found for countries experiencing civil war as well as countries adjacent to them. |
| 52 | Goma Epidemiology Group,[156] 1995 | Rwanda | Children in three refugee camps | Not specified | Mortality estimates ranged 20-120/10,000/day for unaccompanied children and 100-800/10,000/day unaccompanied infants. High rate of death attributed to diarrhoea. . |
| 53 | Green,[51] 2007 | multiple | Case report | 3 | 3 child victims of torture, reported child labour, slow insertion of a knife into the child's thigh to extract information from the parents, and witnessing torture, including witnessing a parent tortured to death. The children reported recurrent nightmares and school absenteeism. |
| 54 | Greene et al,[157] 2014 | Iraq | Case report | 1 | 3 year old girl with blast injuries to the right arm and chest, who required highly specialised thoracic surgery and was hospitalised for 16 days. |
| 55 | Grein et al,[158] 2003 | Angola | Refugees in 4 camps | 6,599 | 18% of the population was U5. U5 mortality was four times above baseline. Main causes of child death were malnutrition, fever and malaria. Children accounted for one-fourth of deaths related to war violence, and 55% of disappearances. |
| 56 | Guha-Sapir and van Panhuis,[123] 2003 | multiple | Children in multiple conflict zones | Not specified | Analysed data from mortality surveys in 7 populations in Afghanistan, the Democratic Republic of Congo, Somalia, and Sudan. The relative risk of dying during conflict differed based on context and appeared to be associated with the fragility of the affected population. |
| 57 | Guha-Sapir and van Panhuis,[122] 2004 | multiple | Populations affected by armed conflict | Not specified | In pooled data from 37 datasets, children ≥5 years have a higher relative risk of dying during conflict compared to children U5. There were wide variations in mortality rates between conflicts. |
| 58 | Guy,[52] 2009 | DRC | Case report | 3 | The 3 children were subjected to physical and psychological torture and reported participation in violence. The three children had a combined total of 403 medical complaints. Clinical exam revealed 275 physical findings that were consistent with the torture mechanisms described by the children. |
| 59 | Hagopian et al,[69] 2010 | Iraq | Child cancer patients at a single facility | 698 | Leukaemia incidence in children aged <15 years presenting to the referral facility in Basra more than doubled over the period 1993–2007. |
| 60 | Halileh and Gordon,[131] 2006 | Israel-Palestine | Children 6–59 months in Gaza and the West Bank | 3,331 | 37% of children were anaemic, with linear decrease in prevalence of anaemia with increasing age. Independent risk factors included age <24 months, living in refugee camps, living in Gaza, and household income being affected by the conflict. |
| 61 | Hanevik and Kvåle,[77] 2000 | Eritrea | Landmine injury patients in 5 hospitals | 248 | Chart review of 248 patients with landmine injuries. 41% of patients were under 15 years, and 22% were 15–19 years old. |
| 62 | Helweg-Larsen et al,[29] 2004 | Israel-Palestine | Patients presenting to two emergency departments | 962 | Chart review of intentional injuries pre-conflict and during Intifada. Marked rise in intentional injuries during conflict. 3% of patients were <10 years old and 8% of patients were 10–14 years old. Head injuries were mostly caused by firearms and were more frequent among the very young children. |
| 63 | Henrich and Shahar,[132] 2013 | Israel-Palestine | 7th-10th graders in southern Israel | 362 | Greater rocket attack exposure predicted an increased aggression in boys, with increased odds of committing violence over the course of the study. |
| 64 | Hicks et al,[53] 2011 | Iraq | Iraqi civilians killed during the conflict | 92,614 | Data from Iraq Body Count database 2003–2008: 2,146 (3.5%) deaths were children under age 18. 36,900 (61.0%) civilian victims of unreported age. Children were killed by all measured methods, including execution, execution with torture, small arms gunfire, suicide bomb, vehicle bomb, roadside bomb, mortar fire, and air attacks both with and without ground fire |
| 65 | Hicks et al,[159] 2011 | Iraq | Death or injury due to suicide bomb | 42,928 | Data from Iraq Body Count database 2003–2010: Children accounted for 14% of deaths due to suicide bombs and for a higher proportion of deaths due to suicide bombs than from general armed violence. 16% of suicide bomb events resulted in the death of at least one child. |
| 66 | Hisle-Gorman et al,[160] 2015 | multiple | Children 3–8 years old of deployed US military personnel | 487,460 | Parental deployment was associated with increased rates of child maltreatment. For the children of injured veterans, there was a 24% increase in child maltreatment visit rates for each additional parent injury diagnosis. |
| 67 | Hoffer and Johnson,[161] 1992 | Iraq | Children with shrapnel wounds at US military combat facility | 19 | 19 of >100 children with shrapnel wounds had associated open fractures. Mechanism of injury included UXO, aerial bombardment, and bullet wounds from combat. Open fractures from shrapnel were most common in the tibia and fibula, and 9 children had bilateral fractures from shrapnel. |
| 68 | Inwald et al,[42] 2014 | Afghanistan | Intensive care patients at a British military combat facility | 811 | Data from Bastion intensive care unit database and JTTR. 14% of intensive care admissions were children, median age 8 years. 71% were trauma admissions, of which 65% had blast injuries, 20% gunshot wounds, and 15% blunt trauma. Body region of trauma: 45% extremities, 35% face/eyes, 26% head, 20% abdomen, 11% thorax, and 4% pelvis |
| 69 | Kandala et al,[59] 2009 | DRC | Children U5 in DRC | 9454 | Higher prevalence of childhood diarrhoea, acute respiratory infection and fever in provinces experiencing armed conflict |
| 70 | Kinra and Black,[78] 2003 | Former Yugoslavia | Landmine injury patients in Bosnia | 4,064 | ICRC database 1991–2000 (during and post-conflict). 14% of patients were children, the majority who were injured during recreational activities. Children were more likely to be injured during peacetime when compared with adults. |
| 71 | Klimo et al,[31] 2010 | Afghanistan | Neurosurgical patients at a US military combat facility | 43 | Data from surgeon’s personal records. 40% of paediatric patients (<18 years) were under 5 years of age The average age of paediatric patients was 7.5 years. Penetrating brain injuries were most common. IED most frequent source of projectile, followed by rocket, landmine, mortar and gunshot wound. |
| 72 | Kvaskoff et al,[162] 2013 | WWII | Cohort of French women born in 1925–1950 | 75,918 | There was a linear relationship between the level of World War II food deprivation before 20 years of age and endometriosis risk. |
| 73 | Lee et al,[124] 2006 | Myanmar | Households living in conflict zone | 1290 | Infant mortality rate in the conflict zone was nearly double and U5 mortality rate was nearly triple the level of the national rates. |
| 74 | Liu et al,[163] 2014 | multiple | Live births to war refugee women in Sweden | 20,723 | Significantly higher odds of preterm (OR 1.39, 95CI: 1.13–1.72) or very preterm birth (OR 2.15, 95CI: 1.37–3.38) during the 1st year of residency in Sweden. The risk continued beyond the first year, with increased risk of very preterm birth (OR = 1.54 95% CI 1.07–2.21) during the third to fifth year of residence. |
| 75 | Longombe et al,[116] 2008 | DRC | Child rape survivors | 7 | Case report of the gang rapes by armed forces of a 6 year old and a 12 year old, respectively. The children developed vesicovaginal fistulae. |
| 76 | Maclure and Denov,[113] 2006 | Sierra Leone | Former child soldiers | 36 | Description of the children's experiences, including physical abuse, psychological torture, witnessing of violence, drug use, child labour, and the use of children as human shields. |
| 77 | Mann,[101] 2010 | DRC | Congolese undocumented refugee children in Tanzania | >100 | Children describe social isolation, stigmatization, dehumanization, harassment and xenophobia, child labour, exploitation, and physical abuse. Fear of being reported to the police, imprisoned or deported. The children also describe lack of agency and barriers in access to education. |
| 78 | Manoncourt et al,[63] 1992 | Somalia | IDPs and residents in Mogadishu | 4169 | High child mortality rates (per 1000 live births), which varied by IDP status and residence. IDPs in camps with U5 mortality rate (MR) 240.6 (95CI: 206.0–275.2), and 5–14 MR 167.1 (95CI: 140.5–193.7). IDPs in towns with U5MR 86.2 (95CI: 50.1–122.3), and in 5–14 MR 89.7 (95CI 52.2–127.2). Residents with U5MR: 115.4 (95CI: 85.6–145.2), 5–14 MR 57.8 (95CI: 38.7–76.9). Markedly limited access to water for IDPs in camps. |
| 79 | Martin et al,[32] 2010 | Iraq | Paediatric neurosurgical patients at a US military combat facility | 42 | Prospective study. 15% of civilian patients were children <18 years, 62% of whom were ≤8 years. 52% had penetrating head injuries, 24% had closed head injuries, and 12% had penetrating spinal injuries. 22% overall mortality in children, and 32% mortality in children with penetrating head injuries. |
| 80 | Masterson et al,[87] 2014 | Syria | Syrian refugee women in Lebanon | 452 | Describes limited access to antenatal and delivery care, with high rates of complications and adverse birth outcomes, including low birth weight, preterm delivery, and infant mortality. Less than half reported any breastfeeding, citing inability to breastfeed, illness, and constant displacement as reasons. 75.8% reported beating their children more than usual. |
| 81 | Mathieu et al,[33] 2015 | Afghanistan | Combat facility paediatric patients with extremity trauma | 155 | Mean age of patients was 9 years. 46% were <8 years. Younger children more likely to have noncombat-related injuries (NCRI). Male to female ratio 3:1. 77 combat-related injuries (CRI) including 19% bullet wounds, 42% fragment wounds, 39% blast wounds. Motor vehicle crashes, falls and burns were the most common noncombat-related mechanism of injury. Injury severity score significantly higher for CRI. |
| 82 | Matos et al,[34] 2008 | Iraq | Paediatric trauma patients treated in a US combat facility | 1132 | Data from hospital records. 97% of patients were >8 years old. 63% of young children (≤8 years) and 83% of older children and adults had penetrating injuries. Young children had more severe injuries. Young age was independently associated with higher mortality. |
| 83 | McGuigan et al,[35] 2007 | Iraq | Paediatric trauma patients treated in a US combat facility | 99 | Data from hospital records. 55% of patients were <13 years old. 79% of injuries were due to battle or crossfire, the majority were blast wounds or penetrating trauma. None of the children had protective armour, and most had multiple injuries. Blast victims had a combination of blunt, penetrating, and thermal injuries. 9% mortality. |
| 84 | Metreveli and Vosk,[164] 1994 | Republic of Georgia | Child casualties in Georgian Civil War | 5 | Case report of five children injured or killed by hand grenades or firearms during the civil war. Treatment was hampered by a shortage of medical equipment and supplies. |
| 85 | Miller et al,[88] 1996 | Former Yugoslavia | Children treated in a referral facility, Sarajevo | 60 | Marked reduction in services, number of beds, number of staff, access to medications, barriers to care and length barriers to returning to family, for up to 18 months, due to the war. Of hospitalised children, 20% had experienced the death of a close relative in the war and 38% had one or more close family members injured. |
| 86 | Momeni and Aminjavaheri,[46] 1994 | Iran-Iraq | Children exposed to mustard gas | 14 | Compared with adults, the children had earlier onset of symptoms and a different clinical pattern. Children's first symptoms were cough and vomiting. Facial involvement was most common. Skin bullae appeared sooner, and the children developed more severe ophthalmic manifestations. |
| 87 | Montgomery and Foldspang,[165] 2001 | multiple | Child asylum seekers in Denmark | 311 | Predictors of sleep disturbance (frequent nightmares, delayed sleep onset, and night-time awakenings) included violent death of grandparents before the child's birth, torture of one or both parents, and being scolded more than previously. Being accompanied to Denmark by both parents reduced the risk of sleep disturbance (OR 0.3 and p<0.0005). |
| 88 | Mujkic et al,[166] 2008 | Former Yugoslavia | Child deaths due to injury 1986–2005 | 4,660 | During the war, the rates of child homicide and suicide using weapons more than tripled and unintentional child deaths with weapons increased more than 6-fold compared to pre-war period. After the war, these rates gradually returned to pre-war levels. |
| 89 | Nelson et al,[117] 2011 | DRC | Child survivors of sexual violence | 389 | Children <18 years were more likely than adults to have been gang raped, raped by a civilian, and raped during the day. Education was protective. The study found an increase in civilian-perpetrated rape during conflict. Nearly 1/4 of child rape survivors had physical sequelae and 19% reported pregnancy resulting from rape. 18% of the children reported efforts to bring the perpetrator to justice, most often with civilian perpetrators. |
| 90 | Nicaragua Health Study Initiative,[81] 1989 | Nicaragua | Households in two towns | 89 | Comparison of a town in a peaceful region with a town in a conflict zone. Children in town experiencing armed conflict had higher prevalence of stunting, lower odds of having an immunization card, lower rate of U5 vaccination completion, and twice the odds of being an orphan. |
| 91 | Nielsen et al,[126] 2006 | Guinea-Bissau | Children <5 years near Bissau | 8933 | U5 mortality doubled during the first six months of the war. In the later part of the war, U5 mortality began to return to baseline, but mortality for girls remained significantly higher than pre-war. Maternal education was protective against U5 mortality. |
| 92 | Novo et al,[85] 2009 | Former Yugoslavia | Rubella cases in Bosnia | 342 | Post-war rubella outbreak investigation revealed that MMR vaccination coverage dropped from 93.6% in Bosnia pre-war to 56.8% during the last two years of the war. Partially- and unvaccinated patients never received catch-up vaccinations. |
| 93 | O'Hare and Southall,[82] 2007 | multiple | Children in Sub-Saharan Africa | Not specified | Data from UNICEF SOWC 2006 report in 42 Sub-Saharan African countries. Median U5 mortality rate in countries with recent conflict was 197/1000 live births, significantly higher than countries without recent conflict (137/1000 live births, p = 0.009). Women in countries with recent conflict were less likely to deliver with a skilled birth attendant, 1 year olds had lower DTP vaccination rates, and primary school enrolment was lower. |
| 94 | Pannell et al,[36] 2015 | Afghanistan | Paediatric trauma patients in a NATO combat facility | 263 | Data from JTTR. 11.7% of trauma patients were children, median age 9 years (range 3 months—17 years), nearly 1/3 were under 6 years. 62% had battle injuries. Injury mechanism: 42% blast injuries, 17% GSW, 16% motor vehicle crash, 8% falls and 4% burns. More than half of children had penetrating injuries. ISS was higher for children <15 years. 8% inpatient mortality. |
| 95 | Patel et al,[104] 2012 | Uganda | IDPs in northern Uganda | >116 | 116 In-depth interviews and 16 focus group discussions. Displacement and low security led to disruption of community structure and social norms; this was associated with changes in sexual behaviour. Girls living in IDP camps were vulnerable to sexual exploitation, violence, economic and food insecurity, and had barriers in access to education and health care. |
| 96 | Pesonen et al,[108] 2008 | WWII | Helsinki birth cohort | 1,704 | Girls separated from their parents in early childhood were twice as more likely (OR 2.1, 95CI: 1.2–3.7) to have their menarche before or at the age of 12 than after the age of 13, compared with non-separated girls. |
| 97 | Pesonen et al,[107] 2010 | WWII | Helsinki birth cohort | 282 | Adults who had been separated from both parents during early childhood had higher salivary cortisol and plasma ACTH concentrations and greater salivary cortisol reactivity to during Trier Social Stress Test compared with non-separated. Gendered differences were found in baseline cortisol, ACTH, and cortisol reactivity. Age at separation from both parents predicted salivary cortisol, plasma cortisol, and plasma ACTH. |
| 98 | Pesonen et al,[109] 2011 | WWII | Helsinki birth cohort | 2,725 | Young men separated temporarily from both parents during early childhood had lower intelligence scores than non-separated men. Findings differed by length of separation and age at the time of separation. Verbal ability was particularly impacted in boys separated from their parents before school age. |
| 99 | Poirier,[90] 2012 | multiple | Children in Sub-Saharan Africa | Not specified | Data from 1950–2010 in 43 countries. Armed conflict and military expenditure increase the rate of children not attending school and have a negative effect on secondary school enrolment rate. |
| 100 | Qouta et al,[133] 2008 | Israel-Palestine | School children in Gaza | 865 | Witnessing severe military violence was associated with aggressive and antisocial behaviour in school children. Parenting practices appear to be a moderating factor. |
| 101 | Radoncic et al,[167] 2008 | Former Yugoslavia | Births at a tertiary facility in Bosnia | 101,712 | Perinatal mortality was decreasing before the war. There was a significant increase during the war and early post-war period and decline again to pre-war levels in 2001. The main causes of perinatal mortality were respiratory distress syndrome, birth asphyxia, congenital malformations, and intracranial haemorrhage. |
| 102 | Radonic et al,[79] 2004 | Former Yugoslavia | Patients with antipersonnel mine injuries | 422 | Data during the war 1991–1995 in southern Croatia. Children accounted for 7.8% of antipersonnel mine injuries and were most commonly injured while playing with the mines, on the way to school, or near their home. The mean age of injured children was 10.5 years. |
| 103 | Rashid,[54] 2012 | Kashmir, India/ Pakistan | Children who were detained and tortured in Kashmir | 43 | Data from personal accounts of children-in-conflict-with-law in Indian-held Kashmir. The children describe lengthy imprisonments in crowded facilities together with adults, forced labour, and inadequate food. Torture methods described included being stripped, blindfolded, having limbs stretched, electrocution of private parts and of limbs, hanging from ceiling by arms, beatings, rollers, breaking teeth, and threats to family. The children describe poor physical health and social isolation after release. |
| 104 | Rees et al,[94] 2013 | Timor-Leste | Women in an urban area and a rural village | 1513 | Victimization and war-related trauma increased the odds of Intermittent explosive disorder in women. Women with IED reported excessive and harmful punishment of their children. |
| 105 | Rentz et al,[97] 2007 | multiple | Children <18 years who experienced substantiated maltreatment in 2000–2003 | 147,982 | Texas child maltreatment data from 2000 to 2003: Substantiated child maltreatment in military families doubled after October 2002 (Rate ratio 2.15, 95CI: 1.85, 2.50), after controlling for child’s age, race/ethnicity, and gender. The rate of child maltreatment in military families increased by approximately 30% for each 1% increase in the percentage of active duty personnel departing to or returning from operation-related deployment. The majority of child maltreatment in military families was perpetrated by a parent. |
| 106 | Reyna,[168] 1993 | Iraq | Paediatric patients treated in a US combat facility | 50 | Data from hospital records. Description of 50 paediatric patients 0–19 years seen at an evacuation hospital in Kuwait. 80% were trauma patients, of which 65% had penetrating injuries. Injuries included shrapnel wounds, gunshot wounds, burns, motor vehicle accidents, crush injuries, and falls. There were no trauma-related deaths. |
| 107 | Roberts et al,[127] 2004 | Iraq | Households in Iraq | 6300 | Household survey found that crude infant mortality increased from 29 per 1000 live births pre-invasion to 57 deaths per 1000 live births post-invasion [95% CI 0–64]. Violence accounted for more than half of recorded child deaths in the post-invasion. |
| 108 | Rodríguez and Sánchez,[93] 2012 | Colombia | Children 6–17 years in Colombia | 20,642 | National survey found that violent attacks significantly increase the risk of school drop-out. An increase by one standard deviation of armed conflict exposure increased the joint probability of child labour and school drop-out by 13% in children 12–17 years. The effect appeared to be long-term, with adults in areas affected by conflict having lower educational outcomes. |
| 109 | Saile et al,[95] 2014 | Uganda | Households in Gulu and Nwoya districts | 283 | Traumatic war exposure in female guardian independently predicted child-reported experiences of abuse in the family. Partner violence between guardians and PTSD-symptoms in male guardians were the major proximal risk factors for child-reported victimization, suggesting that war exposure and subsequent trauma may be a mediating factor in violence against children. |
| 110 | Salignon and Legros,[134] 2002 | Republic of Congo | Residents of Mindouli | 10,026 | 83.5% of the population were displaced by the war and had returned to their homes in Mindouli during the 3 months preceding the survey. 195 U5 deaths were reported in the 6 months preceding the survey, accounting for 13% of the U5 population of Mindouli in November 1999. The U5 mortality rate exceeded 10 deaths/10,000/day November 1999-January 2000. Causes of U5 death were malnutrition (54,4%), fever (17.4%), diarrhoea (6.7%), and 21.5% other cause |
| 111 | Samms et al,[169] 2010 | Iraq | Case report | 1 | 16 year old with a gunshot wound to the pelvis and possible blast injury to the abdomen. The patient had an 83 day hospital course, required 30 operations, and was discharged to a local hospital. |
| 112 | Santavirta,[170] 2014 | WWII | People born in Finland 1933–1944 registered in the 1950 census | 66,053 | Men who were evacuated to foster care in Sweden at age <4 years had mortality risk 1.3 times higher than their counterparts who were not evacuated. There were no other significant mortality differences based on gender, age at time of evacuation, or between evacuation-status discordant siblings. |
| 113 | Schiff et al,[171] 2006 | Israel-Palestine | 7th-10th graders in Herzeliya, Israel | 1,150 | 1/3 respondents were in the proximity during an attack and 40% knew someone who was injured (psychological proximity). Physical and psychological proximity to attacks were significantly associated with alcohol consumption, when controlling for PTSD and depressive symptoms. |
| 114 | Schiff et al,[172] 2007 | Israel-Palestine | Jewish 10th and 11th graders in Haifa | 960 | Close physical exposure to armed conflict predicted higher levels of alcohol consumption, binge drinking among drinkers, and cannabis use. |
| 115 | Schiff et al,[173] 2012 | Israel-Palestine | Jewish and Arab Israeli 7th-11th graders | 4,151 | The youth reported high rates of exposure to war events. Cumulative exposure to war events was significantly associated with alcohol and drug consumption and involvement in school violence. |
| 116 | Schlecht et al,[105] 2013 | Uganda | Displaced Ugandan and Congolese refugee youth | 133 | Armed conflict resulted in breakdown of traditional community social structure and associated protective marriage practices. Displacement was also associated with social isolation and barriers in access to education. These social changes and challenges were associated with earlier sexual debut without involvement or knowledge of parents/caregivers, teen pregnancy, sexual exploitation of girls, transactional sex. |
| 117 | Shemyakina,[92] 2011 | Tajikistan | Households with school age children across Tajikistan | 6,160 | Based on 2 surveys (one representative at national level and one at regional and urban/rural level). Children 8–15 years old in conflict-affected area were less likely to attend school. Damage to household dwelling negatively associated with the enrolment of girls. Nationally, men and women of school age during the war were less likely to complete nine grades of schooling compared to their pre-war counterparts. |
| 118 | Shuker,[174] 1985 | not reported | Case report | 1 | 7 year old child with multiple high-velocity wounds sustained from artillery shelling, including avulsion of 6cm of the left mandible. The mandible was stabilised with a K-wire, resulting in spontaneous regeneration of the entire osseous defect. |
| 119 | Skokic et al,[61] 2006 | Former Yugoslavia | Newborns in Tuzla Canton 1992–2003 | 59,707 | During the war: 20% fewer live births than pre-war and higher prevalence of premature delivery compared with pre- and post-war. Average birth weight of term newborns was 200 and 300 grams lower than pre- and post-war, respectively. Barriers to care during conflict evidenced by significantly fewer births attended by trained health providers and fewer prenatal visits. |
| 120 | Slim et al,[37] 1990 | Lebanon | Patients with war-related abdominal injuries at a single facility | 270 | Children <16 years accounted for nearly 1/5 of abdominal trauma admissions. 70% of children had penetrating injuries from shrapnel, bullets, stab wounds, and blast explosions. The remaining 30% had blunt abdominal trauma. The children had 4.8% overall mortality; however patients transferred from other facilities had 55.6% mortality. |
| 121 | Soroush et al,[80] 2010 | Iran-Iraq | Patients with landmine or UXO injury | 3,713 | Data from hospital records of 3713 patients in western and south-western Iran. 41.8% of patients with landmine or UXO injuries were <18 years old. |
| 122 | Spiegel et al,[175] 2011 | Somalia | Refugee households in Dadaab camps | 753 | In a household survey of newly arrived refugees, 44 deaths reported, 29 (66%) were in children under 5. |
| 123 | Spinella et al,[40] 2008 | Afghanistan and Iraq | Paediatric patients treated in 7 US combat facilities | 1,305 | Data from PASBA database. Report on paediatric trauma admissions December 2001—May 2007, or 7.1% of all trauma admissions. Children were severely injured at admission, had longer hospital stays, and accounted for 13% of trauma deaths. Age <6 years was associated with higher mortality rate (10.7% compared with 3.8% in children 6–17 years). |
| 124 | Stern et al,[176] 1995 | Iraq | Case report | 1 | 8 year old with aplastic anaemia, only known exposure was that his home was situated near to burning oil wells |
| 125 | Terzic et al,[43] 2001 | Former Yugoslavia | Children treated at a tertiary care facility | 94 | Chart review of paediatric patients treated for war injuries. Most children were wounded by shelling and explosive devices, most commonly in the extremities. The most severe wounds were caused by shelling. 39.4% of children were permanently disabled and 3.3% died. |
| 126 | Trenholm et al,[114] 2013 | DRC | Male former child soldiers | 12 | Ethnographic study. Boys reported abduction, forced recruitment, and poverty as reasons for entering the military. They describe beatings, forced marches, sleep deprivation, starvation, substance use, witnessing rape, and being forced to rape. The boys describe normalization of sexual violence, with rape considered a bounty of war and also as means to release anger or reap revenge. |
| 127 | Valente et al,[84] 2000 | Angola | Polio cases in Angola | 1,093 | Description of a polio outbreak among displaced persons in Luanda. During a vaccination campaign in response to the outbreak, nearly 30% of districts could not be reached due to the conflict. |
| 128 | Van Herp et al,[64] 2003 | DRC | Households in 5 conflict-affected regions of DRC | 4,527 | Threshold and emergency level U5 mortality rates at the front line, primarily due to malnutrition and infections. Context-specific variations in direct and indirect exposure to combat and barriers in access to acute and preventive health care. |
| 129 | Van Leent and Hopkins,[177] 1951 | WWII | Refugee children in Australia | 4,721 | Sampled nearly 1/5 of refugee children, found low BCG vaccination rates. 36% were Mantoux positive, with a linear rise in Mantoux positivity with age: 3.9% positive at 1 year, up to 78% positive at 15 years. |
| 130 | Veale and Dona,[178] 2003 | Rwanda | Street Children in Rwanda | 290 | 87% came to the streets after the 1994 genocide. More than 3/4 had lost at least one parent, and 1/3 reported both parents were dead. 42% were homeless. The majority cited living on street due to changes in family structure, including loss of one or both parents, parent remarriage, becoming unaccompanied, being fostered in another family, or the closure of an unaccompanied children’s centre. |
| 131 | Verelst et al,[119] 2014 | DRC | 2nd and 3rd graders in Ituri district | 1305 | 499 children (38.2%) reported having been victims of sexual violence. The risk of sexual violence increased with exposure to war-related violence, separation from family, being injured during the war, imprisonment, and association with armed groups. |
| 132 | Villamaria et al,[44] 2014 | Afghanistan and Iraq | Paediatric vascular trauma patients treated in US combat facilities | 155 | Data from 2002–2011. The majority of vascular injuries in children were caused by blast injuries (58%), followed by bullets (37.4%) and falls (1.9%). Extremity injuries were more common while torso injuries were more lethal. |
| 133 | Vranković et al,[45] 1997 | Former Yugoslavia | Case report | 10 | In 10 paediatric penetrating head injury patients, 4 were injured by bullets and 6 by shrapnel. Patients with shrapnel wounds had associated cerebral oedema. All gunshot wound patients survived; half of patients with shrapnel wounds died. 4 patients had moderate neurological deficits. |
| 134 | Weile et al,[55] 1990 | Chile | Chilean refugee children in Denmark | 58 | Follow up of Cohn 1979. In child survivors of torture living as refugees in Denmark, there was an increase in the number of somatic symptoms and in the prevalence of symptoms over time. At follow up, 90% of children had one or more symptoms. Children who had continuous symptoms at the first study had significantly higher medication use. Number years lived in Denmark positively correlated to number of symptoms. |
| 135 | Wen et al,[70] 2000 | Vietnam and Cambodia | Children with leukaemia | 2,343 | Pooled data from three studies shows increase in the risk for AML of the children of veterans who served in Vietnam or Cambodia (OR 1.7; 95% Cl: 1.0, 2.9). This risk was increased in fathers who had two or more tours of duty (OR = 5.0; 95CI: 1.0, 24.5). |
| 136 | Wilson et al,[38] 2013 | Afghanistan | Paediatric trauma patients treated in a US combat facility | 41 | Data from facility trauma registry. 10% of trauma admissions were children, 71% were boys, and 59% were battle-related. More than 2/3 had penetrating injuries, most often from IEDs and landmines. 3/4 of injuries were severe, with AIS score ≥ 3, and 14.6% died. |
| 137 | Woods et al,[39] 2012 | Afghanistan and Iraq | Paediatric trauma patients treated in British combat facilities | 176 | Data from JTTR. Half of paediatric (<16) trauma cases were less than eight years old. The most common mechanism of injury was explosive injury (59%), followed by gunshot wound (20.5%), and motor vehicle crash (8.5%). The mortality rate was 11%. 70% of mortality was due to explosive injury and 15% due to motor vehicle crashes. Half of deaths were due to head injuries. |
| Search updates 25 April 2017 | |||||
| Author | Conflict zone | Population | Sample size | Summary of findings | |
| 1 | Bayarogullari et al,[179] 2016 | Syria | Case report | 2 | Two children with complex shrapnel wounds resulting in vertebral artery pseudoaneurysms. One patient lost to follow up due to displacement. |
| 2 | Ceri et al,[180] 2016 | Iraq | Yazidi refugee children in three camps | 42 | More than 2/3 of children reported sleep disturbances and >1/3 had somatic complaints |
| 3 | Charchuk et al,[58] 2016 | DRC | Children in Bilobilo IDP camp and Mubi village | 600 | IDP camp residence predicted falciparum malaria in children (OR 2.6, 95% CI: 1.2–5.7). Bed net ownership and use were significantly lower for the children from the IDP camp compared to the children from the village. |
| 4 | Chi et al,[102] 2015 | Burundi and Uganda | Health workers and women living in Burundi and Northern Uganda | 115 | Participants linked armed conflict with limited access to maternity and reproductive health services, poor quality of care, and increased neonatal morbidity and mortality. Conflict resulted in destruction and looting of facilities, targeted killing and abduction of health workers, and migration of health workers. Barriers in care resulted in increased use of traditional birth attendants. Girls 12–18 years from disadvantaged backgrounds were noted to be at high risk for sexual exploitation, unintended pregnancy, and subsequent health complications. |
| 5 | Cook et al,[49] 2015 | Myanmar | Karen refugees in Minnesota, USA | 179 | Children described witnessing and being subjected to war-related violence, including witnessing parents and community members being tortured and killed by soldiers, repeated and forced displacement, being beaten, child labour, and being forced to join the military. |
| 6 | Denov and Lakor,[115] 2017 | Uganda | Children born to mothers abducted by the Lord's Resistance Army | 60 | Children report witnessing combat and mass executions, seeing injured children and dead bodies. They reported being orphaned, being abandoned by parents, going without food or water, and lack of access to health care and education. Stigma and social exclusion from parents, families and communities led some children to describe life during war as preferable because they were loved, had a caring father present, and a sense of family. |
| 7 | Duque,[181] 2017 | Colombia | Children in Colombia | 13,344 | Violence exposure in first trimester of gestation and in early childhood was associated with decline in math reasoning, general knowledge, and Peabody Picture Vocabulary Test scores. |
| 8 | Guha-Sapir et al,[47] 2015 | Syria | Civilian violent deaths in Syria 2011–2015 | 78,769 | Children accounted for >16% of civilian deaths in non-state controlled areas and >23% of civilian deaths in government-controlled areas. The risk of death from different combat activities varied by location, however, children in all areas were more likely than men to die from air bombardments, shells, ground level explosives, and chemical weapons. 852 children were killed by execution, including execution after torture. |
| 9 | Hemat et al,[182] 2017 | Afghanistan | Trauma patients at single facility | 35,647 | Paediatric trauma patients at Kunduz Trauma Centre Jan 2014- June 2015: Children accounted for 50% of patients registered in the emergency department and 41% of operated patients. |
| 10 | Khamaysi et al,[183] 2015 | Syria | Case report | 5 | Report on 5 patients with traumatic bile leaks from war injuries, including two children. |
| 11 | Klimo et al,[30] 2015 | Iraq and Afghanistan | Paediatric neurosurgical patients at US military combat facilities | 647 | Data from JTTR. Review of neurosurgical cases 2004–2012. 76% of patients were boys, with a median age of 8 years. 60% of patients were under 9 years of age. 61% had penetrating head injuries. Most commonly mechanism of injury was IED explosion, blast, gunshot wound, and mortar. In-hospital mortality was 24%. |
| 12 | Lindskog,[125] 2016 | DRC | Infants born in DRC | 53,768 | Uses DHS data to analyse infant mortality among 15,103 mothers and 53,768 children. Infant mortality was higher during the war years compared with pre-war and post-war. There was a linear relationship between post-neonatal infant mortality and the number of conflict events |
| 13 | Nnadi et al,[83] 2017 | Nigeria | Polio cases in Borno | 4 | There were 4 reported cases of Polio in the region. Two infected children were unvaccinated, and two were partially vaccinated. In the two years preceding the case report, 50% of settlements in Borno were inaccessible to public health programmes. |
| 14 | Rabenhorst et al,[96] 2015 | Afghanistan and Iraq | US Air Force personnel deployed >30 days | 99,679 | There were no overall changes in substantiated child maltreatment (CM) rates post-deployment compared to pre-deployment, however rates of child injury increased post-deployment (RR1.6, 95% CI: 1.31, 2.01), as well as rates of moderate and severe maltreatment (RR 1.9, 95% CI: 1.34, 2.80) and CM involving alcohol use (RR 1.5, 95% CI: 1.11, 2.15). |
| 15 | Rouhani et al,[118] 2015 | DRC | Women raising children born from sexual violence | 757 | More than a third report stigma toward their child from the community and 2/3 reported often seeing their assailant and/or remembering the sexual assault when looking at the child. Stigma and maternal mental health disorder was associated with negative parenting attitudes. Family and community acceptance were associated with adaptive parenting attitudes. |
| 16 | Stark et al,[65] 2015 | Uganda | Congolese and Somali refugees in Kampala | >215 | 175 In-depth interviews, 40 key-informant interviews and 51 focus group discussions. Children reported discrimination in schools and teachers encouraging xenophobia Conversely, some reported reduced school fees and accommodations made for prayer. Children reported social marginalization in the community, barriers in access to sanitation, assault, and lack of access to health care and legal and protective services. |
| 17 | Sullivan et al,[98] 2015 | multiple | Californian children in public civilian schools, grades 7, 9, and 11 | 688,713 | Military-connected secondary school students reported higher levels of physical violence (OR 1.47, 95% CI: 1.43–1.50) and nonphysical harassment (OR 1.42, 95%CI: 1.38–1.45). They had twice the odds of carrying a gun to school (OR 2.2, 95% CI: 2.10–2.30), and nearly twice the odds of carrying a knife or other weapon to school (OR 1.81 (95% CI: 1.75–1.88). |
| 18 | Weishut,[56] 2015 | Israel-Palestine | Palestinian victims of sexual torture by Israeli authorities | 77 | Data on 77 cases from Public Committee Against Torture in Israel database. 15% of victims were minors. They describe beating of the genitals, forced confession, threats of rape, and threats of sexual violence against family members. |
Fig 3. Summary of principal findings reported in the literature.
Direct health effects
Children exposed to armed conflict suffer a broad range of injuries and illness that can be directly attributed to conflict (Fig 3). One third (N = 52) of included studies describe a range of physical injuries affecting all organ systems, broadly classified as penetrating injuries, blunt trauma, crush injuries and burns. Injuries were attributed to shelling, explosions, collapsing buildings, gunshots, and motor vehicle crashes.
Among injured children who reach health facilities, penetrating injuries are most common.[25–39] Penetrating head injury is the most frequent form of head injury among children treated in military combat facilities, accounting for 60–75% of all head injuries and carrying the highest mortality risk.[28, 30, 32] This pattern of head trauma differs markedly from that observed in peaceful settings, where blunt head trauma predominates. It is important to note that the admission criteria for combat support hospitals, access to military facility care, and care seeking behaviours of people living in combat zones are likely to influence the findings in military studies; Spinella et al documented that a child with a severe head injury had sought care at five other hospitals before presenting to a military facility.[40]
Reported mortality from trauma ranges from 2.6–18%,[33–44] and as high as 24% in neurosurgical patients.[30–32, 45] Younger trauma patients bear a significantly higher burden of mortality when compared with older children and adults.[40, 41] No studies provided data on mortality after transfer or discharge from health facilities.
While numerous case studies report children with traumatic amputations, only one study examined the prevalence of disability among war-injured children. This single facility retrospective chart review of 94 children with war-related injuries sustained during the wars in Croatia and Bosnian and Herzegovina found that nearly 40% of the children suffered permanent disability.[43] No studies describe the incidence or prevalence of childhood disability associated with armed conflict or its long term effects on health, development, or life opportunities.
Two studies document the effects of chemical or biological weapons on children. Momeni and colleagues describe the clinical manifestations of mustard gas exposure in a group of children during the Iran-Iraq war.[46] The paper highlights the difference in presentation when compared with adults, including earlier onset of symptoms, more frequent pulmonary and gastrointestinal symptoms, and predominant face and neck symptoms. Guha-Sapir and colleagues found that children in the ongoing conflict in Syria are twice as likely to die from chemical weapon attacks as adults (OR 2.11, 95% CI: 1.69–2.63).[47]
Studies documenting the torture of children report a variety of torture methods that children experienced and/or witnessed. These children suffer physical injuries, a variety of somatic complaints, enuresis, constipation, sleep disorders, and psychological disorders.[47–56] A follow-up study on children who were tortured or whose parents were tortured in Chile found that both the prevalence and frequency of somatic symptoms increased over time after resettlement in Denmark.[55]
Indirect health effects
Diseases
Exposure to armed conflict is associated with a higher burden of infectious, communicable, and noncommunicable diseases in children. A global study of disability-adjusted life years (DALYs) associated with civil war found significantly reduced DALYs in children under 14 years for all disease categories, with the most severe reductions in the under 5 (U5) age group.[57] Diseases such as malaria,[58] diarrhoea, acute respiratory infections, and fever[59] are more common and carry higher mortality.[60] A nationwide cross-sectional study in Iraq after the first Persian Gulf War found that age-adjusted mortality due to diarrhoea rose from 2.1 pre-war to 11.9 per 1000 person-years after onset of war.[60] Pregnancy and birth in conflict zones are also higher risk. A study in Tuzla Canton, Bosnia, found significantly fewer live births, increased preterm delivery, and low birth weight during wartime, which normalised again after the war.[61] Displacement due to conflict is associated with crowding, limited access to water and sanitation, and increased risk of infectious and communicable diseases.[62–65]
Environmental exposures
Studies on the effects of combat-related environmental exposures have identified an increased prevalence of birth defects and cancer, as well as ongoing risk of injury due to unexploded ordnance (UXO). The incidence of structural heart defects in Kuwaiti infants rose significantly after the first Persian Gulf War to levels exceeding the international incidence.[66] While the mechanism for this jump in prevalence cannot be identified by the study design, the authors suggest that war-related environmental pollution may play a role. This hypothesis is supported by a large study of birth defects in children of US Gulf War Veterans using active case ascertainment.[67] Conversely, an earlier review of military health records suggests no increased incidence of birth defects among the infants of US Gulf War Veterans.[68]
A study in Iraq found a significantly increased rate of leukaemia, particularly amongst younger children.[69] Similarly, Wen and colleagues found significantly increased risk of AML in children whose fathers reported having served in Vietnam or Cambodia.[70] AML risk was further elevated if fathers reported two or more tours.
Landmines and unexploded ordinance (UXO) remain a significant risk for children during conflict and long after combat has ended.[71–80] The burden of injury due to UXO varies by conflict, however children account for approximately half (42–55%) of injuries from UXO in Afghanistan, Nepal, Eritrea, and Iran.[71, 73, 74, 77, 80] The pattern of injuries in children is similar across settings; children more often suffer upper body injuries sustained while playing, going to school, or tending animals.[71–74, 78, 79]
Access to basic needs
Whilst the burden of disease increases due to conflict, access to health care becomes more difficult. Children in areas affected by conflict are less likely to receive vaccinations [81, 82] and conflicts may contribute to outbreaks of vaccine preventable diseases such as the polio outbreaks during the conflicts in Nigeria and Angola [83, 84] and a rubella outbreak in Bosnia and Herzegovina after hostilities had ended.[85] Combat may also hamper vaccination campaigns during disease outbreaks.[84] Several studies have reported that pregnant women displaced due to war were less likely to receive prenatal care or deliver with the assistance of a skilled birth attendant.[61, 82, 86, 87] Studies from the former Yugoslavia describe drastic reductions in the number of health personnel [88] and conditions where children with chronic conditions had less frequent access to medical care and experienced worsening of their condition.[89]
Conflict also prevents children from going to school and lowers their overall educational attainment. A large time-series cross-sectional study examining the impact of war in sub-Saharan Africa (1950–2010) found that armed conflict significantly reduced school attendance for both boys and girls, and with an inverse correlation between military expenditure and school attendance.[90] Similar findings have also been described in Palestine,[91] Tajikistan[92] and Colombia.[93] The Colombian study findings suggested this may have a long-term effect—adults in areas affected by conflict had lower educational outcomes.
Risk of abuse, neglect, and exposure to secondary violence
Children whose caregivers have been exposed to armed conflict are at increased risk for child abuse and neglect. Studies from Timor-l’Este, Uganda, and in Syrian refugees in Lebanon found that caregivers who suffer from stress or have a mental health disorder related to their exposure to armed conflict have higher rates of child-reported and caregiver-reported child abuse.[87, 94, 95] The Ugandan study findings suggest that war exposure and subsequent trauma are mediating factors for violence against children. Studies among U.S. military personnel have documented increased rates of physical abuse and neglect in the children of veterans, both during the period of deployment and after return.[96, 97] A large study of Californian children in civilian public schools found that the children of US military personnel have higher rates of experiencing violence in school and are more likely to carry a weapon.[98]
Social changes
Important changes in societal structure, norms, and roles take place in populations affected by conflict. Children may assume adult responsibilities, including providing for their families and caring for ill or disabled parents.[99–101] Several studies described changes in sexual behaviour, with earlier sexual debut and child marriage.[102–105] Displacement and separation from family may place children at increased risk for exploitation, high risk sexual behaviour, sexually-transmitted illness, and teen pregnancy.[104] Two studies from Uganda describe particular barriers in access to information and health care for adolescents that further compound their health risks.[104, 105]
Toxic stress and child development
While numerous studies document the multiple kinds of war-related violence that children witness, no studies examine the effect of these exposures on child motor and psychosocial development. Two studies examined the influence of war-related trauma on children’s stress physiology. Feldman et al. found that war-exposed children had altered cortisol and salivary amylase response to stress.[106] The same study also found that children’s baseline cortisol levels were independently related to maternal baseline cortisol, mother-child relationship, and maternal mental health. Similarly, the Helsinki Birth Cohort Study described altered stress physiology in children who were separated from their parents for a period during WWII.[107] Two other studies on the same birth cohort found that separated girls had significantly earlier onset of menarche than non-separated girls, and that children separated from their parents in early childhood had lower scores on intelligence testing, respectively.[108, 109]
Children associated with armed forces or armed groups (“child soldiers”)
Studies from Sierra Leone, the Democratic Republic of the Congo (DRC), and El Salvador document the extreme kinds of violence that children experience during association with armed forces or groups, including being forced to watch and take part in killing, cannibalism, rape, child marriage, and sexual slavery.[52, 99, 110–114] Three studies also describe the process of indoctrinating children and methods used to control and isolate them. The children in these studies describe regular physical and psychological abuse, torture, and the normalisation of violence.[52, 113, 115] In the words of one child: “After some time, [the violence] became part of me”.[113]
Several papers describe unwanted teenage pregnancies, gynaecological problems, and sexually transmitted illnesses among child soldiers.[99, 111, 112] A case report on three former child soldiers in the DRC describes a combined total of 403 medical complaints and 275 physical findings in multiple organ systems.[52] The sheer number and diversity of complaints and somatic findings in these three youth provides insight into the extensive harm wrought by association with armed groups.
Sexual violence
The witnessing, experience, and perpetration of sexual violence and sexual exploitation are documented by numerous papers in this review, nine of which dealt exclusively with these issues.[56, 100, 104, 105, 115–119] All included studies of children associated with armed groups document sexual violence of and by these children. However, the studies that focus exclusively on sexual violence and exploitation, suggest the problem is far more widespread. These studies describe children being: a) threatened with rape, b) raped, including gang rape, c) forced to watch rapes, including rapes of family members, and d) forced to rape others and engage in sexual slavery. They also document “survival-”, or transactional sex to obtain basic needs, and early marriage. Documented physical findings include traumatic genital injuries, vesicovaginal fistulae, and pregnancy. Two studies describe the experiences of children conceived through sexual violence, including social isolation and exposure to violence and threats from within their communities.[100, 118] A survey of women raising children conceived through conflict-associated rape reported that 66.1% often saw their assailant and/or remembered the sexual assault when they looked at their child.[118]
Mortality
More than one-third (n = 64) of studies included mortality as a main outcome. The heterogeneity of design and lack of denominators in much of the reported data preclude the pooling of data. However, numerous studies report significant increases in infant and child mortality during periods of armed conflict, in comparison to peacetime or when compared with peaceful parts of the same country.[21, 60, 82, 120–127] Most of these studies report on under 5 years (U5) mortality.
A pooled study of 37 datasets from 1985–2001 found that the relative risk of dying during periods of conflict was higher for older children (≥ 5 years) when compared to those U5.[122] In some countries, U5 mortality actually decreased during the period of conflict. The absolute U5 mortality remained higher than the ≥ 5 years mortality independent of the presence of conflict, suggesting that additional factors unrelated to conflict were contributing to U5 mortality in these populations.[122] This study suggests that there are nuanced and context-specific factors that lead to conflict-associated mortality during different periods of childhood.
Further examples in support of the importance of context on mortality outcomes is seen in studies by Ascherio and Nielsen that found maternal education is protective against child mortality in conflict settings.[60, 126] Avogo et al. found displacement of children due to war carries a higher mortality risk than displacement for other reasons, with the highest risk of death during the year after migration.[86] The study suggests that forced migration due to war exposes children to health risks after resettlement to which other migrant children are less vulnerable. Mortality studies by Hicks[53] and Guha-Sapir[47] document the direct deaths of children due to combat activities in Iraq and Syria, respectively. In addition to deaths from bombs and gunshot wounds, both studies document the torture and execution of children.
Geographic distribution of the literature
There is a notable trend in the geography of published studies. During the period 1946–2016, there were 280 distinct armed conflicts.[4] Papers providing data on child physical health and development are focused on a few specific conflicts and on particular regions of the world. There is a remarkable dearth of data on major past conflicts, such as the Korean War and the Chinese Civil War, and more recently the conflicts in Yemen, Myanmar, Guatemala, Mexico, the Central African Republic, and Pakistan. There is also a notable lack of data on protracted conflicts, such as those in Kashmir and in Xinjiang province, China.
Figs 4 and 5 illustrate the publication trend from 1990–2016. During this period, there were 165 armed conflicts across all regions of the globe.[22] Child health is studied in only 30 of these conflicts, and 60% of published studies focus on just six conflict zones. Closer examination of geographical reporting patterns reveals a conflict-specific focus on exposures and outcomes. For example, seven of the nine studies examining sexual violence against children were conducted in the DRC and Uganda.[104, 105, 115–119] All four studies from Sierra Leone focus on child soldiers. Of the 45 studies examining child health in Afghanistan and Iraq, half are case studies and chart reviews from military combat facilities.
Fig 4. The number of published studies on child health in countries with documented armed conflict 1990–2016.
Fig 5. Studies published 1990–2017 by conflict region (number of studies in parenthesis).
Discussion
This is the first systematic review of the global impact of armed conflict on child physical health and development. The review’s findings reveal the breadth of the problem, its pervasive and sustained impact on child health, and important nuances in the way conflict affects child health. Further, it describes how these effects differ based on the direct and indirect nature of the impact, characteristics of the individual conflict (e.g., types of combat, weapons, displacement, relief efforts), and contextual factors associated with the geographic location of the conflicts. The broad view given by the available evidence is quite disturbing and therefore warrants reporting in this first paper on our systematic review. Further analysis of subsets of the data will be presented in future publications.
It is important to reiterate that this review deliberately excluded papers reporting exclusively on child health outcomes that are known to carry high risk in conflict settings, including nutrition, perinatal mortality, infant feeding, and immunization coverage. Most papers that reported on perinatal mortality, birth weight, and infant feeding also reported on other child health outcomes, and were thus included in this review. However, the relative paucity of papers in our review providing data on these topics suggests that the evidence for the effect of armed conflict on maternal and newborn health is lacking. This finding is consistent with other recent reviews on the subject.[128, 129] Additionally, there is a large literature on the effects of forced displacement on child mental health,[19, 20] much of which was not identified by the searches. Finally, studies that were published as books were not included in the review; this is likely to have precluded the examination of a number studies, particularly those undertaken before 1990.
The grey literature database searches retrieved only 382 citations, none of which met inclusion criteria. This review is therefore limited to the peer-reviewed literature; this is an important limitation because traditional public health research in conflict settings is limited by security concerns, population movements, the destruction of public health infrastructure, and the disruption of routine data collection.[13] Furthermore, most of the studies rely on health facility data and are thus likely have selection bias, as they report on those patients who were able to access care in a facility where sufficiently complete records were maintained and were accessible to the researchers. Much of the available information about the health of populations living outside of refugee or IDP camps in areas of active conflict is not reported in the peer-reviewed literature and is therefore missing from this review. Among studies providing data from areas experiencing active conflict, the majority were retrospective chart reviews. Of the 11 population-based studies in settings with active conflict, 10 used a cross-sectional and/or qualitative design. [60, 64, 81, 106, 126, 130–134] While there were no marked differences in the findings from these studies compared with studies in refugees in neighbouring regions, the design of the studies make it difficult to draw further conclusions.
Through its pervasive harmful effects on children, armed conflict is a negative social determinant of child health. Numerous studies have documented that adversity during childhood can alter the architecture of the brain and neuroendocrine function, leading to alterations in learning, behaviour, and physiology, in turn predisposing the developing child to maladaptive behaviours and ill health throughout the life course.[135] The findings on stress physiology reported in this review are in keeping with previous studies on toxic stress and childhood adversity, and therefore have significant implications for generations of children growing up amid armed conflict.
For each individual child exposed to armed conflict, the way in which this exposure affects the child’s health is likely to be determined by a number of factors including genetic predisposition, physical health, mental health, development, behaviour, caregiver physical and mental health, forced displacement, and social arrangements. The influence of caregiver mental health on the physical and mental health of conflict-affected[9] and forcibly displaced children[8] is well-described. The findings of Feldman et al[106] suggest that in war-affected children, caregiver attachment and mental health may play a mediating role, and is therefore a potential area for intervention to mitigate the effects of armed conflict on children.
Numerous studies in this review report on physical health, mental health, and social conditions in the same population, suggesting they are interrelated. Other studies describe alterations in social arrangements due to conflict, such as disruption of communities and barriers in access to education, which affect child and adolescent health and wellbeing. The relationship between physical health, mental health, and social conditions in conflict-affected children is an area in need of further research, and that may provide insight into aggravating factors, mitigating factors, and ways to promote good health and resilience.
The overlap of different typologies of violence against children in the context of armed conflict is an important finding that merits further attention. In addition to risks for being injured, tortured, and/or a witness to or participant in combat, children with direct and indirect exposure to conflict are also at increased risk for other forms of violence, including abuse and neglect,[87, 94–97] community and school violence,[98] and domestic violence.[94, 95] Furthermore, Nelson et al describe an increase in civilian-perpetrated rape of children during a period of conflict in the DRC.[117] While these forms of violence against children are extensively described in grey literature reports, the association of these forms of violence with armed conflict points to an important need for child protection after the exposure to conflict has ended.
There is a compelling need for further research to improve our understanding of the medium and long term effects of the exposure to armed conflict as a form of violence against children. Areas in need of further study include global child development, children with chronic diseases, children with disabilities, and adolescent health. Of particular importance is the need to improve our understanding of the relationship between physical and mental health and social conditions in conflict-affected children and factors that protect and mitigate the harmful effects of armed conflict (Fig 6). In addition to informing the development of evidence-based interventions to treat and mitigate the harmful effects of conflict on children, such knowledge would improve our understanding of how to advance the health and well-being of adults who have experienced armed conflict and other adversities during childhood and adolescence. Such information would be of great use for peace research and conflict resolution.
Fig 6. Recommendations for future research.
The studies included in this review demonstrate that it is possible to study the ways that armed conflict affects child health and development using both quantitative and qualitative methods. However, the vast majority of the literature is descriptive because traditional epidemiological research is difficult to undertake in settings with insecurity and disrupted health systems. A study published after completion of this systematic review brings attention to a potential way to improve the study of conflict and child health and highlights an important role for humanitarian organizations working in settings where routine data is no longer available. Meiqari et al[136] describe paediatric data collected by Médecins Sans Frontières (MSF) in Tal-Abyad and Kobani, Syria. In spite of challenges, which included population movements and abrupt closing and opening of clinical services due to the shifting front lines of the conflict, the authors describe the epidemiology of a large cohort of children who received care in MSF facilities for periods between 2013–2016, including 27,742 children U5 seen in outpatient clinics, 4672 children under 18 years admitted for inpatient treatment, and a measles epidemic response. Meiqari and colleagues provide important data about child health epidemiology in the study region, as well as information on care-seeking behaviours in a conflict zone notorious for attacks on health care facilities.[137] By supporting colleagues working in conflict zones and developing epidemiological methods to better study health in low-security settings, we can improve the ability to conduct research that can meaningfully improve the care and outcomes of children affected by armed conflict.
Conclusion
This systematic review documents the pervasive effect of armed conflict as a form of violence against children and negative social determinant of child health. The studies serve as a record of the continuing occurrence of the six grave violations of children’s rights, which include the killing and maiming of children; recruitment or use of children as soldiers; sexual violence against children; abduction of children; attacks against schools or hospitals; and the denial of humanitarian access for children. There is an urgent need to improve our research on the mechanisms by which conflict affects child health and development and the relationship between physical health, mental health, and social conditions. Priority should be given to studies on child development, the long term effects of exposure to conflict, and protective and mitigating factors against the harmful effects of conflict on children. Collaboration with partners across sectors and incorporating a child rights perspective into research can improve both our understanding of the effect of conflict on child health as well as our response to their needs.
Supporting information
(DOC)
Acknowledgments
The University of Florida-Jacksonville provided partial funding for this work. The authors are indebted to Gretchen Kuntz for her assistance in developing and refining the searches, using Covidence, and obtaining full text papers. Several others also assisted in location of papers, including Jeremy Nagle (Science 2 Enquiry Desk, The British Library), Khalid Kadir, and Gonca Yilmaz, for which we are very grateful. Several individuals assisted in translation of papers to English, including Birte Kadir, Saadoon Kadir, Natalya Ustinova, Krzyzstof Karski, Raul Mercer, Vanya Petrovic, and Giuseppe Annunziata. Without their assistance, such a thorough review would not have been possible. Finally, we wish to thank Sham Lal and Michael Fahmi for support in the critical appraisal of two papers with complex methodological design.
Data Availability
All relevant data are within the manuscript and its Supporting Information files. The review is registered with PROSPERO, where the full search strategy is available: https://www.crd.york.ac.uk/PROSPEROFILES/36425_STRATEGY_20170427.pdf.
Funding Statement
The University of Florida-Jacksonville College of Medicine provided partial funding for the study. There was no additional external funding received for this study.
References
- 1.UNICEF. More than 1 in 10 Children Living in Countries and Areas Affected by Armed Conflict. New York: United States Fund for UNICEF; 2015. [Google Scholar]
- 2.Education Under Attack 2014. Global Coalition to Protect Education from Attack, 2014.
- 3.Report on Attacks on Health Care in Emergencies. Geneva: World Health Organization, 2016. [Google Scholar]
- 4.Dupuy K, Gates S, Nygård HM, Rudolfsen I, Rustad SA, Strand H, et al. Trends in Armed Conflict, 1946–2016. Oslo, Norway: Peace Research Institute Oslo (PRIO), 2017. [Google Scholar]
- 5.Uppsala Conflict Data Program. Definitions. Uppsala Universitet: Department of Peace and Conflict Research; 2018. [19 October 2018]. Available from: https://www.pcr.uu.se/research/ucdp/definitions. [Google Scholar]
- 6.UNICEF. Uprooted: The growing crisis for refugee and migrant children. 2016.
- 7.Marquardt L, Kramer A, Fischer F, Prufer-Kramer L. Health status and disease burden of unaccompanied asylum-seeking adolescents in Bielefeld, Germany: cross-sectional pilot study. Trop Med Int Health. 2016;21(2):210–8. 10.1111/tmi.12649 [DOI] [PubMed] [Google Scholar]
- 8.ISSOP Migration Working Group. ISSOP position statement on migrant child health. Child Care Health Dev. 2018;44(1):161–70. 10.1111/cch.12485 [DOI] [PubMed] [Google Scholar]
- 9.Slone M, Mann S. Effects of War, Terrorism and Armed Conflict on Young Children: A Systematic Review. Child Psychiatry Hum Dev. 2016. [DOI] [PubMed] [Google Scholar]
- 10.Choonara I. Economic sanctions and child health. Med Confl Surviv. 2013;29(2):93–8. [DOI] [PubMed] [Google Scholar]
- 11.Pearn J. Children and war. J Paediatr Child Health. 2003;39(3):166–72. [DOI] [PubMed] [Google Scholar]
- 12.Rieder M, Choonara I. Armed conflict and child health. Arch Dis Child. 2012;97(1):59–62. 10.1136/adc.2009.178186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray CJ, King G, Lopez AD, Tomijima N, Krug EG. Armed conflict as a public health problem. BMJ. 2002;324(7333):346–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wagner Z, Heft-Neal S, Bhutta ZA, Black RE, Burke M, Bendavid E. Armed conflict and child mortality in Africa: a geospatial analysis. Lancet. 2018;392(10150):857–65. 10.1016/S0140-6736(18)31437-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Attanayake V, McKay R, Joffres M, Singh S, Burkle F Jr., Mills E. Prevalence of mental disorders among children exposed to war: a systematic review of 7,920 children. Med Confl Surviv. 2009;25(1):4–19. 10.1080/13623690802568913 [DOI] [PubMed] [Google Scholar]
- 16.Barry MM, Clarke AM, Jenkins R, Patel V. A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC Public Health. 2013;13:835 10.1186/1471-2458-13-835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Betancourt TS, Borisova I, Williams TP, Meyers-Ohki SE, Rubin-Smith JE, Annan J, et al. Psychosocial adjustment and mental health in former child soldiers—systematic review of the literature and recommendations for future research. Journal of Child Psychology and Psychiatry. 2013;54(1):17–36. 10.1111/j.1469-7610.2012.02620.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bronstein I, Montgomery P. Psychological distress in refugee children: a systematic review. Clin Child Fam Psychol Rev. 2011;14(1):44–56. 10.1007/s10567-010-0081-0 [DOI] [PubMed] [Google Scholar]
- 19.Fazel M, Reed RV, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. Lancet. 2012;379(9812):266–82. 10.1016/S0140-6736(11)60051-2 [DOI] [PubMed] [Google Scholar]
- 20.Reed RV, Fazel M, Jones L, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in low-income and middle-income countries: risk and protective factors. Lancet. 2012;379(9812):250–65. 10.1016/S0140-6736(11)60050-0 [DOI] [PubMed] [Google Scholar]
- 21.Aaby P, Gomes J, Fernandes M, Djana Q, Lisse I, Jensen H. Nutritional status and mortality of refugee and resident children in a non-camp setting during conflict: follow up study in Guinea-Bissau. BMJ. 1999;319(7214):878–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uppsala Conflict Data Program: Uppsala University Department of Peace and Conflict Research; 2016 [20 September 2017]. Available from: http://ucdp.uu.se.
- 23.Salama P, Spiegel P, Talley L, Waldman R. Lessons learned from complex emergencies over past decade. Lancet. 2004;364(9447):1801–13. 10.1016/S0140-6736(04)17405-9 [DOI] [PubMed] [Google Scholar]
- 24.Sphere Project. Sphere Handbook: Humanitarian Charter and Minimum Standards in Disaster Response 2011. Available from: http://www.refworld.org/docid/4ed8ae592.html. [DOI] [PubMed] [Google Scholar]
- 25.Bogdanovich U, Schevchenko A. Eye injuries in children during wartime. Vrachebnoye Dielo. 1946;3–4:166–74. [Google Scholar]
- 26.Celikel A, Karbeyaz K, Kararslan B, Arslan MM, Zeren C. Childhood casualties during civil war: Syrian experience. Journal of Forensic and Legal Medicine. 2015;34:1–4. 10.1016/j.jflm.2015.04.021 [DOI] [PubMed] [Google Scholar]
- 27.Coppola CP, Leininger BE, Rasmussen TE, Smith DL. Children treated at an expeditionary military hospital in iraq. Archives of Pediatrics & Adolescent Medicine. 2006;160(9):972–6. [DOI] [PubMed] [Google Scholar]
- 28.Creamer KM, Edwards MJ, Shields CH, Thompson MW, Yu CE, Adelman W. Pediatric wartime admissions to US military combat support hospitals in Afghanistan and Iraq: learning from the first 2,000 admissions. J Trauma. 2009;67(4):762–8. 10.1097/TA.0b013e31818b1e15 [DOI] [PubMed] [Google Scholar]
- 29.Helweg-Larsen K, Abdel-Jabbar Al-Qadi AH, Al-Jabriri J, Bronnum-Hansen H. Systematic medical data collection of intentional injuries during armed conflicts: a pilot study conducted in West Bank, Palestine. Scand J Public Health. 2004;32(1):17–23. 10.1080/14034940310018048 [DOI] [PubMed] [Google Scholar]
- 30.Klimo P, Ragel BT, Jones GM, McCafferty R. Severe Pediatric Head Injury During the Iraq and Afghanistan Conflicts. Neurosurgery. 2015;77(1):1–7. 10.1227/NEU.0000000000000743 [DOI] [PubMed] [Google Scholar]
- 31.Klimo P, Ragel BT, Scott WH, McCafferty R. Pediatric neurosurgery during Operation Enduring Freedom. J Neurosurg Pediatr. 2010;6(2):107–14. 10.3171/2010.3.PEDS109 [DOI] [PubMed] [Google Scholar]
- 32.Martin JE, Teff RJ, Spinella PC. Care of pediatric neurosurgical patients in Iraq in 2007: clinical and ethical experience of a field hospital. J Neurosurg Pediatr. 2010;6(3):250–6. 10.3171/2010.6.PEDS1031 [DOI] [PubMed] [Google Scholar]
- 33.Mathieu L, Bertani A, Rongieras F, Chaudier P, Mary P, Versier G. Wartime paediatric extremity injuries: experience from the Kabul International Airport Combat support hospital. J Pediatr Orthop B. 2015;24(3):238–45. 10.1097/BPB.0000000000000166 [DOI] [PubMed] [Google Scholar]
- 34.Matos RI, Holcomb JB, Callahan C, Spinella PC. Increased mortality rates of young children with traumatic injuries at a US army combat support hospital in Baghdad, Iraq, 2004. Pediatrics. 2008;122(5):e959–66. 10.1542/peds.2008-1244 [DOI] [PubMed] [Google Scholar]
- 35.McGuigan R, Spinella PC, Beekley A, Sebesta J, Perkins J, Grathwohl K, et al. Pediatric trauma: experience of a combat support hospital in Iraq. J Pediatr Surg. 2007;42(1):207–10. 10.1016/j.jpedsurg.2006.09.020 [DOI] [PubMed] [Google Scholar]
- 36.Pannell D, Poynter J, Wales PW, Tien H, Nathens AB, Shellington D. Factors affecting mortality of pediatric trauma patients encountered in Kandahar, Afghanistan. Can J Surg. 2015;58(3 Suppl 3):S141–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Slim MS, Her C, Akel SR, Dajani OM, Hajj HA, Baraka A. Factors affecting survival of children after abdominal trauma in Lebanese civil war. Pediatric Surgery International. 1990;5(3):188–91. [Google Scholar]
- 38.Wilson KL, Schenarts PJ, Bacchetta MD, Rai PR, Nakayama DK. Pediatric trauma experience in a combat support hospital in eastern Afghanistan over 10 months, 2010 to 2011. Am Surg. 2013;79(3):257–60. [PubMed] [Google Scholar]
- 39.Woods KL, Russell RJ, Bree S, Mahoney PF, McNicholas J. The pattern of paediatric trauma on operations. J R Army Med Corps. 2012;158(1):34–7. [DOI] [PubMed] [Google Scholar]
- 40.Spinella PC, Borgman MA, Azarow KS. Pediatric trauma in an austere combat environment. Crit Care Med. 2008;36(7 Suppl):S293–6. [DOI] [PubMed] [Google Scholar]
- 41.Borgman M, Matos RI, Blackbourne LH, Spinella PC. Ten years of military pediatric care in Afghanistan and Iraq. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S509–13. [DOI] [PubMed] [Google Scholar]
- 42.Inwald DP, Arul GS, Montgomery M, Henning J, McNicholas J, Bree S. Management of children in the deployed intensive care unit at Camp Bastion, Afghanistan. J R Army Med Corps. 2014;160(3):236–40. 10.1136/jramc-2013-000177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Terzic J, Mestrovic J, Dogas Z, Furlan D, Biocic M. Children war casualties during the 1991–1995 wars in Croatia and Bosnia and Herzegovina. Croat Med J. 2001;42(2):156–60. [PubMed] [Google Scholar]
- 44.Villamaria CY, Morrison JJ, Fitzpatrick CM, Cannon JW, Rasmussen TE. Wartime vascular injuries in the pediatric population of Iraq and Afghanistan: 2002–2011. J Pediatr Surg. 2014;49(3):428–32. 10.1016/j.jpedsurg.2013.10.002 [DOI] [PubMed] [Google Scholar]
- 45.Vranković D, Kristek B, Muršić B, Takač I. [Therapeutic results in penetrating cranio-cerebral injuries of children: Our experiences under wartime conditions.]. Der Unfallchirurg. 1997;100(1):13–6. [DOI] [PubMed] [Google Scholar]
- 46.Momeni AZ, Aminjavaheri M. Skin manifestations of mustard gas in a group of 14 children and teenagers: a clinical study. Int J Dermatol. 1994;33(3):184–7. [PubMed] [Google Scholar]
- 47.Guha-Sapir D, Rodriguez-Llanes JM, Hicks MH, Donneau AF, Coutts A, Lillywhite L, et al. Civilian deaths from weapons used in the Syrian conflict. BMJ. 2015;351(h4736). [DOI] [PubMed] [Google Scholar]
- 48.Cohn J, Holzer KI, Koch L, Severin B. [Torture of children. A study of Chilean immigrant children in Denmark. A preliminary report]. Ugeskr Laeger. 1979;141(50):3431–3. [PubMed] [Google Scholar]
- 49.Cook TL, Shannon PJ, Vinson GA, Letts JP, Dwee E. War trauma and torture experiences reported during public health screening of newly resettled Karen refugees: A qualitative study. BMC International Health and Human Rights. 2015:1–13. 10.1186/s12914-015-0041-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Geltman PL, Grant-Knight W, Mehta SD, Lloyd-Travaglini C, Lustig S, Landgraf JM, et al. The "lost boys of Sudan": functional and behavioral health of unaccompanied refugee minors re-settled in the United States. Arch Pediatr Adolesc Med. 2005;159(6):585–91. 10.1001/archpedi.159.6.585 [DOI] [PubMed] [Google Scholar]
- 51.Green C. Politically-motivated torture and child survivors. Pediatr Nurs. 2007;33(3):267–70. [PubMed] [Google Scholar]
- 52.Guy KM. Child soldiers as zones of violence in The Democratic Republic of Congo: three cases of medico-legal evidence of torture. Torture. 2009;19(2):137–44. [PubMed] [Google Scholar]
- 53.Hicks MH, Dardagan H, Guerrero Serdan G, Bagnall PM, Sloboda JA, Spagat M. Violent deaths of Iraqi civilians, 2003–2008: analysis by perpetrator, weapon, time, and location. PLoS Med. 2011;8(2):e1000415 10.1371/journal.pmed.1000415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rashid J. An analysis of self-accounts of children-in-conflict- with-law in Kashmir concerning the impact of torture and detention on their lives. International Social Work. 2012;55(5):629–44. [Google Scholar]
- 55.Weile B, Wingender LB, Bach-Mortensen N, Busch P, Lukman B, Holzer KI. Behavioral problems in children of torture victims: a sequel to cultural maladaptation or to parental torture? J Dev Behav Pediatr. 1990;11(2):79–80. [PubMed] [Google Scholar]
- 56.Weishut DJ. Sexual torture of Palestinian men by Israeli authorities. Reprod Health Matters. 2015;23(46):71–84. 10.1016/j.rhm.2015.11.019 [DOI] [PubMed] [Google Scholar]
- 57.Ghobarah HA, Huth P, Russett B. The post-war public health effects of civil conflict. Soc Sci Med. 2004;59(4):869–84. 10.1016/j.socscimed.2003.11.043 [DOI] [PubMed] [Google Scholar]
- 58.Charchuk R, Paul MK, Claude KM, Houston S, Hawkes MT. Burden of malaria is higher among children in an internal displacement camp compared to a neighbouring village in the Democratic Republic of the Congo. Malaria J. 2016;15(1):431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kandala NB, Emina JB, Nzita PD, Cappuccio FP. Diarrhoea, acute respiratory infection, and fever among children in the Democratic Republic of Congo. Soc Sci Med. 2009;68(9):1728–36. 10.1016/j.socscimed.2009.02.004 [DOI] [PubMed] [Google Scholar]
- 60.Ascherio A, Chase R, Cote T, Dehaes G, Hoskins E, Laaouej J, et al. Effect of the Gulf War on infant and child mortality in Iraq. N Engl J Med. 1992;327(13):931–6. 10.1056/NEJM199209243271306 [DOI] [PubMed] [Google Scholar]
- 61.Skokic F, Muratovic S, Radoja G. Perinatal and maternal outcomes in Tuzla Canton during 1992–1995 war in Bosnia and Herzegovina. Croat Med J. 2006;47(5):714–21. [PMC free article] [PubMed] [Google Scholar]
- 62.Gessner BD. Mortality rates, causes of death, and health status among displaced and resident populations of Kabul, Afghanistan. JAMA. 1994;272(5):382–5. [PubMed] [Google Scholar]
- 63.Manoncourt S, Doppler B, Enten F, Nur AE, Mohamed AO, Vial P, et al. Public health consequences of the civil war in Somalia, April, 1992. Lancet. 1992;340(8812):176–7. [DOI] [PubMed] [Google Scholar]
- 64.Van Herp M, Parque V, Rackley E, Ford N. Mortality, violence and lack of access to healthcare in the Democratic Republic of Congo. Disasters. 2003;27(2):141–53. [DOI] [PubMed] [Google Scholar]
- 65.Stark L, DeCormier Plosky W, Horn R, Canavera M. 'He always thinks he is nothing': The psychosocial impact of discrimination on adolescent refugees in urban Uganda. Social Science and Medicine. 2015;146:173–81. 10.1016/j.socscimed.2015.10.045 [DOI] [PubMed] [Google Scholar]
- 66.Abushaban L, Al-Hay A, Uthaman B, Salama A, Selvan J. Impact of the Gulf war on congenital heart diseases in Kuwait. Int J Cardiol. 2004;93(2–3):157–62. 10.1016/S0167-5273(03)00193-1 [DOI] [PubMed] [Google Scholar]
- 67.Araneta MR, Schlangen KM, Edmonds LD, Destiche DA, Merz RD, Hobbs CA, et al. Prevalence of birth defects among infants of Gulf War veterans in Arkansas, Arizona, California, Georgia, Hawaii, and Iowa, 1989–1993. Birth Defects Res A Clin Mol Teratol. 2003;67(4):246–60. 10.1002/bdra.10033 [DOI] [PubMed] [Google Scholar]
- 68.Cowan DN, DeFraites RF, Gray GC, Goldenbaum MB, Wishik SM. The risk of birth defects among children of Persian Gulf War veterans. N Engl J Med. 1997;336(23):1650–6. 10.1056/NEJM199706053362306 [DOI] [PubMed] [Google Scholar]
- 69.Hagopian A, Lafta R, Hassan J, Davis S, Mirick D, Takaro T. Trends in Childhood Leukemia in Basrah, Iraq, 1993–2007. American Journal of Public Health. 2010;100(6):1081–7. 10.2105/AJPH.2009.164236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wen WQ, Shu XO, Steinbuch M, Severson RK, Reaman GH, Buckley JD, et al. Paternal military service and risk for childhood leukemia in offspring. Am J Epidemiol. 2000;151(3):231–40. [DOI] [PubMed] [Google Scholar]
- 71.Bilukha OO, Brennan M. Injuries and deaths caused by unexploded ordnance in Afghanistan: review of surveillance data, 1997–2002. BMJ. 2005;330(7483):127–8. 10.1136/bmj.38337.361782.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bilukha OO, Brennan M, Anderson M. The lasting legacy of war: epidemiology of injuries from landmines and unexploded ordnance in Afghanistan, 2002–2006. Prehosp Disaster Med. 2008;23(6):493–9. [DOI] [PubMed] [Google Scholar]
- 73.Bilukha OO, Brennan M, Woodruff BA. Death and injury from landmines and unexploded ordnance in Afghanistan. JAMA. 2003;290(5):650–3. 10.1001/jama.290.5.650 [DOI] [PubMed] [Google Scholar]
- 74.Bilukha OO, Laurenge H, Danee L, Subedi KP, Becknell K. Injuries and deaths due to victim-activated improvised explosive devices, landmines and other explosive remnants of war in Nepal. Inj Prev. 2011;17(5):326–31. 10.1136/ip.2010.030312 [DOI] [PubMed] [Google Scholar]
- 75.Bilukha OO, Tsitsaev Z, Ibragimov R, Anderson M, Brennan M, Murtazaeva E. Epidemiology of injuries and deaths from landmines and unexploded ordnance in Chechnya, 1994 through 2005. JAMA. 2006;296(5):516–8. 10.1001/jama.296.5.516-b [DOI] [PubMed] [Google Scholar]
- 76.Gasparovic H, Stern-Padovan R, Batinica S, Saric D, Jelic I. Intracardiac shrapnel in a polytraumatized child. Ann Thorac Surg. 2004;77(3):1083–5. 10.1016/S0003-4975(03)01221-9 [DOI] [PubMed] [Google Scholar]
- 77.Hanevik K, Kvåle G. Landmine injuries in Eritrea. BMJ. 2000;321(7270):1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kinra S, Black ME. Landmine related injuries in children of Bosnia and Herzegovina 1991–2000: comparisons with adults. J Epidemiol Community Health. 2003;57(4):264–5. 10.1136/jech.57.4.264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Radonic V, Giunio L, Boric T, Mimica Z, Furlan D, Definis-Gojanovic M. Antipersonnel mine injuries in Southern Croatia. Mil Med. 2004;169(4):313–9. [DOI] [PubMed] [Google Scholar]
- 80.Soroush A, Flahati F, Zargar M, Soroush M, Araghizadeh H, Khateri S, et al. Injuries Associated with Landmines and Unexploded Ordnances in Iran. Iran Red Crescent Med J. 2010;12(4):384–7. [Google Scholar]
- 81.Nicaragua Health Study Collaborative. Health effects of the war in two rural communities in Nicaragua. Nicaragua Health Study Collaborative at Harvard, CIES, and UNAN. Am J Public Health. 1989;79(4):424–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.O'Hare BA, Southall DP. First do no harm: the impact of recent armed conflict on maternal and child health in Sub-Saharan Africa. J R Soc Med. 2007;100(12):564–70. 10.1258/jrsm.100.12.564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nnadi C, Damisa E, Esapa L, Braka F, Waziri N, Siddique A, et al. Continued Endemic Wild Poliovirus Transmission in Security-Compromised Areas—Nigeria, 2016. Mmwr. 2017;Morbidity and mortality weekly report. 66(7):190–3. 10.15585/mmwr.mm6607a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Valente F, Otten M, Balbina F, Van de Weerdt R, Chezzi C, Eriki P, et al. Massive outbreak of poliomyelitis caused by type-3 wild poliovirus in Angola in 1999. Bull World Health Organ. 2000;78(3):339–46. [PMC free article] [PubMed] [Google Scholar]
- 85.Novo A, Huebschen JM, Muller CP, Tesanovic M, Bojanic J. Ongoing rubella outbreak in Bosnia and Herzegovina, March-July 2009—preliminary report. Euro Surveill. 2009;14(39). [DOI] [PubMed] [Google Scholar]
- 86.Avogo WA, Agadjanian V. Forced migration and child health and mortality in Angola. Soc Sci Med. 2010;70(1):53–60. 10.1016/j.socscimed.2009.09.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Masterson AR, Usta J, Gupta J, Ettinger AS. Assessment of reproductive health and violence against women among displaced Syrians in Lebanon. BMC Womens Health. 2014;14(1):25 10.1186/1472-6874-14-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Miller LC, Langhans N, Schaller JG, Zecevic E. Effects of war on the health care of Bosnian children. JAMA. 1996;276(5):370–1. [PubMed] [Google Scholar]
- 89.Bosnjak J, Vukovic-Bobic M, Mejaski-Bosnjak V. Effect of war on the occurrence of epileptic seizures in children. Epilepsy & Behavior. 2002;3(6):502–9. [DOI] [PubMed] [Google Scholar]
- 90.Poirier T. The effects of armed conflict on schooling in Sub-Saharan Africa. International Journal of Educational Development. 2012;32(2):341–51. [Google Scholar]
- 91.Di Maio M, Nandi TK. The effect of the Israeli–Palestinian conflict on child labor and school attendance in the West Bank. Journal of Development Economics. 2013;100(1):107–16. [Google Scholar]
- 92.Shemyakina O. The effect of armed conflict on accumulation of schooling: Results from Tajikistan. Journal of Development Economics. 2011;95(2):186–200. [Google Scholar]
- 93.Rodríguez C, Sánchez F. Armed Conflict Exposure, Human Capital Investments, And Child Labor: Evidence From Colombia. Defence and Peace Economics. 2012;23(2):161–84. [Google Scholar]
- 94.Rees S, Silove D, Verdial T, Tam N, Savio E, Fonseca Z, et al. Intermittent explosive disorder amongst women in conflict affected Timor-Leste: associations with human rights trauma, ongoing violence, poverty, and injustice. PLoS One. 2013;8(8):e69207 10.1371/journal.pone.0069207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Saile R, Ertl V, Neuner F, Catani C. Does war contribute to family violence against children? Findings from a two-generational multi-informant study in Northern Uganda. Child Abuse Negl. 2014;38(1):135–46. 10.1016/j.chiabu.2013.10.007 [DOI] [PubMed] [Google Scholar]
- 96.Rabenhorst MM, McCarthy RJ, Thomsen CJ, Milner JS, Travis WJ, Colasanti MP. Child maltreatment among U.S. Air Force parents deployed in support of Operation Iraqi Freedom/Operation Enduring Freedom. Child Maltreatment. 2015;20(1):61–71. 10.1177/1077559514560625 [DOI] [PubMed] [Google Scholar]
- 97.Rentz ED, Marshall SW, Loomis D, Casteel C, Martin SL, Gibbs DA. Effect of deployment on the occurrence of child maltreatment in military and nonmilitary families. Am J Epidemiol. 2007;165(10):1199–206. 10.1093/aje/kwm008 [DOI] [PubMed] [Google Scholar]
- 98.Sullivan K, Capp G, Gilreath TD, Benbenishty R, Roziner I, Astor RA. Substance abuse and other adverse outcomes for military-connected youth in California: Results from a large-scale normative population survey. JAMA Pediatrics. 2015;169(10):922–8. 10.1001/jamapediatrics.2015.1413 [DOI] [PubMed] [Google Scholar]
- 99.Dickson-Gómez J. Growing Up in Guerrilla Camp: The long-Term Impact of Being a Child Soldier in El Salvador's Civil War. Ethos. 2002;30(4):327–56. [Google Scholar]
- 100.Erjavec K, Volčič Z. Living With the Sins of Their Fathers: An Analysis of Self-Representation of Adolescents Born of War Rape. Journal of Adolescent Research. 2010;25(3):359–86. [Google Scholar]
- 101.Mann G. ‘Finding a Life’ Among Undocumented Congolese Refugee Children in Tanzania. Children & Society. 2010;24(4):261–70. [Google Scholar]
- 102.Chi PC, Bulage P, Urdal H, Sundby J. Perceptions of the effects of armed conflict on maternal and reproductive health services and outcomes in Burundi and Northern Uganda: A qualitative study. BMC International Health and Human Rights. 2015;15 (1)(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.de Smedt J. Child marriages in Rwandan refugee camps. Africa. 1998;68(2):211–37. [Google Scholar]
- 104.Patel SH, Muyinda H, Sewankambo NK, Oyat G, Atim S, Spittal PM. In the face of war: examining sexual vulnerabilities of Acholi adolescent girls living in displacement camps in conflict-affected Northern Uganda. BMC Int Health Hum Rights. 2012;12:38 10.1186/1472-698X-12-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schlecht J, Rowley E, Babirye J. Early relationships and marriage in conflict and post-conflict settings: vulnerability of youth in Uganda. Reprod Health Matters. 2013;21(41):234–42. 10.1016/S0968-8080(13)41710-X [DOI] [PubMed] [Google Scholar]
- 106.Feldman R, Vengrober A, Eidelman-Rothman M, Zagoory-Sharon O. Stress reactivity in war-exposed young children with and without posttraumatic stress disorder: relations to maternal stress hormones, parenting, and child emotionality and regulation. Dev Psychopathol. 2013;25(4 Pt 1):943–55. [DOI] [PubMed] [Google Scholar]
- 107.Pesonen AK, Raikkonen K, Feldt K, Heinonen K, Osmond C, Phillips DI, et al. Childhood separation experience predicts HPA axis hormonal responses in late adulthood: a natural experiment of World War II. Psychoneuroendocrinology. 2010;35(5):758–67. 10.1016/j.psyneuen.2009.10.017 [DOI] [PubMed] [Google Scholar]
- 108.Pesonen AK, Raikkonen K, Heinonen K, Kajantie E, Forsen T, Eriksson JG. Reproductive traits following a parent-child separation trauma during childhood: a natural experiment during World War II. Am J Hum Biol. 2008;20(3):345–51. 10.1002/ajhb.20735 [DOI] [PubMed] [Google Scholar]
- 109.Pesonen A-K, Räikkönen K, Kajantie E, Heinonen K, Henriksson M, Leskinen J, et al. Intellectual ability in young men separated temporarily from their parents in childhood. Intelligence. 2011;39(5):335–41. [Google Scholar]
- 110.Betancourt TS, Borisova II, Williams TP, Brennan RT, Whitfield TH, de la Soudiere M, et al. Sierra Leone's former child soldiers: a follow-up study of psychosocial adjustment and community reintegration. Child Dev. 2010;81(4):1077–95. 10.1111/j.1467-8624.2010.01455.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Betancourt TS, Simmons S, Borisova I, Brewer SE, Iweala U, Soudiere MD. High Hopes, Grim Reality: Reintegration and the Education of Former Child Soldiers in Sierra Leone. Comp Educ Rev. 2008;52(4):565–87. 10.1086/591298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Denov M. Coping with the trauma of war: Former child soldiers in post-conflict Sierra Leone. International Social Work. 2010;53(6):791–806. [Google Scholar]
- 113.Maclure R, Denov M. “I Didn't Want to Die So I Joined Them”: Structuration and the Process of Becoming Boy Soldiers in Sierra Leone. Terrorism and Political Violence. 2006;18(1):119–35. [Google Scholar]
- 114.Trenholm J, Olsson P, Blomqvist M, Ahlberg BM. Constructing Soldiers from Boys in Eastern Democratic Republic of Congo. Men and Masculinities. 2013;16(2):203–27. [Google Scholar]
- 115.Denov M, Lakor AA. When war is better than peace: The post-conflict realities of children born of wartime rape in northern Uganda. Child Abuse and Neglect. 2017;65:255–65. 10.1016/j.chiabu.2017.02.014 [DOI] [PubMed] [Google Scholar]
- 116.Longombe AO, Claude KM, Ruminjo J. Fistula and traumatic genital injury from sexual violence in a conflict setting in Eastern Congo: case studies. Reprod Health Matters. 2008;16(31):132–41. 10.1016/S0968-8080(08)31350-0 [DOI] [PubMed] [Google Scholar]
- 117.Nelson BD, Collins L, VanRooyen MJ, Joyce N, Mukwege D, Bartels S. Impact of sexual violence on children in the Eastern Democratic Republic of Congo. Med Confl Surviv. 2011;27(4):211–25. 10.1080/13623699.2011.645148 [DOI] [PubMed] [Google Scholar]
- 118.Rouhani SA, Scott J, Greiner A, Albutt K, Hacker MR, Kuwert P, et al. Stigma and parenting children conceived from sexual violence. Pediatrics. 2015;136(5):e1195–e203. 10.1542/peds.2014-3373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Verelst A, De Schryver M, De Haene L, Broekaert E, Derluyn I. The mediating role of stigmatization in the mental health of adolescent victims of sexual violence in Eastern Congo. Child Abuse Negl. 2014;38(7):1139–46. 10.1016/j.chiabu.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 120.Curlin GT, Chen LC, Hussain SB. Demographic crisis: The impact of the Bangladesh civil war (1971) on births and deaths in a rural area of Bangladesh. Popul Stud (Camb). 1976;30(1):87–105. [DOI] [PubMed] [Google Scholar]
- 121.Garfield R, Leu CS. A multivariate method for estimating mortality rates among children under 5 years from health and social indicators in Iraq. Int J Epidemiol. 2000;29(3):510–5. [PubMed] [Google Scholar]
- 122.Guha-Sapir D, van Panhuis WG. Conflict-related mortality: an analysis of 37 datasets. Disasters. 2004;28(4):418–28. 10.1111/j.0361-3666.2004.00267.x [DOI] [PubMed] [Google Scholar]
- 123.Guha-Sapir D, van Panhuis WG. The importance of conflict-related mortality in civilian populations. Lancet. 2003;361(9375):2126–8. 10.1016/S0140-6736(03)13691-4 [DOI] [PubMed] [Google Scholar]
- 124.Lee TJ, Mullany LC, Richards AK, Kuiper HK, Maung C, Beyrer C. Mortality rates in conflict zones in Karen, Karenni, and Mon states in eastern Burma. Trop Med Int Health. 2006;11(7):1119–27. 10.1111/j.1365-3156.2006.01651.x [DOI] [PubMed] [Google Scholar]
- 125.Lindskog EE. The effect of war on infant mortality in the Democratic Republic of Congo. BMC Public Health. 2016;16(1):1059 10.1186/s12889-016-3685-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Nielsen J, Jensen H, Andersen PK, Aaby P. Mortality patterns during a war in Guinea-Bissau 1998–99: changes in risk factors? Int J Epidemiol. 2006;35(2):438–46. 10.1093/ije/dyi246 [DOI] [PubMed] [Google Scholar]
- 127.Roberts L, Lafta R, Garfield R, Khudhairi J, Burnham G. Mortality before and after the 2003 invasion of Iraq: cluster sample survey. Lancet. 2004;364(9448):1857–64. 10.1016/S0140-6736(04)17441-2 [DOI] [PubMed] [Google Scholar]
- 128.Morof DF, Kerber K, Tomczyk B, Lawn J, Blanton C, Sami S, et al. Neonatal survival in complex humanitarian emergencies: setting an evidence-based research agenda. Conflict and Health. 2014;8(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lawn JE, Blencowe H, Kinney MV, Bianchi F, Graham WJ. Evidence to inform the future for maternal and newborn health. Best Practice & Research Clinical Obstetrics & Gynaecology. 2016;36:169–83. [DOI] [PubMed] [Google Scholar]
- 130.Cliff J, Nicala D, Saute F, Givragy R, Azambuja G, Taela A, et al. Konzo associated with war in Mozambique. Trop Med Int Health. 1997;2(11):1068–74. [DOI] [PubMed] [Google Scholar]
- 131.Halileh S, Gordon NH. Determinants of anemia in pre-school children in the occupied Palestinian territory. J Trop Pediatr. 2006;52(1):12–8. 10.1093/tropej/fmi045 [DOI] [PubMed] [Google Scholar]
- 132.Henrich CC, Shahar G. Effects of exposure to rocket attacks on adolescent distress and violence: a 4-year longitudinal study. J Am Acad Child Adolesc Psychiatry. 2013;52(6):619–27. 10.1016/j.jaac.2013.02.016 [DOI] [PubMed] [Google Scholar]
- 133.Qouta S, Punamaki RL, Miller T, El-Sarraj E. Does war beget child aggression? Military violence, gender, age and aggressive behavior in two Palestinian samples. Aggress Behav. 2008;34(3):231–44. 10.1002/ab.20236 [DOI] [PubMed] [Google Scholar]
- 134.Salignon P, Legros D. [Impact of war on civilian population health. Republic of the Congo, December 1998-February 2000]. Med Trop. 2002;62(4):433–7. [PubMed] [Google Scholar]
- 135.Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e46. 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 136.Meiqari L, Hoetjes M, Baxter L, Lenglet A. Impact of war on child health in northern Syria: the experience of Médecins Sans Frontières. European Journal of Pediatrics. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fouad FM, Sparrow A, Tarakji A, Alameddine M, El-Jardali F, Coutts AP, et al. Health workers and the weaponisation of health care in Syria: a preliminary inquiry for The Lancet-American University of Beirut Commission on Syria. Lancet. 390(10111):2516–26. 10.1016/S0140-6736(17)30741-9 [DOI] [PubMed] [Google Scholar]
- 138.Amitai Y, Almog S, Singer R, Hammer R, Bentur Y, Danon YL. Atropine poisoning in children during the Persian Gulf crisis. A national survey in Israel. JAMA. 1992;268(5):630–2. [PubMed] [Google Scholar]
- 139.Barisic N, Perovic D, Mitrovic Z, Jurenic D, Zagar M. Assessment of war and accidental nerve injuries in children. Pediatr Neurol. 1999;21(1):450–5. [DOI] [PubMed] [Google Scholar]
- 140.Barnes VA, Davis H, Treiber FA. Perceived stress, heart rate, and blood pressure among adolescents with family members deployed in Operation Iraqi Freedom. Mil Med. 2007;172(1):40–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Bertani A, Mathieu L, Dahan JL, Launay F, Rongiéras F, Rigal S. War-related extremity injuries in children: 89 cases managed in a combat support hospital in Afghanistan. Orthopaedics & Traumatology: Surgery & Research. 2015;101(3):365–8. [DOI] [PubMed] [Google Scholar]
- 142.Bodalal Z, Agnaeber K, Nagelkerke N, Stirling B, Temmerman M, Degomme O. Pregnancy outcomes in Benghazi, Libya, before and during the armed conflict in 2011. East Mediterr Health J. 2014;20(3):175–80. [PubMed] [Google Scholar]
- 143.Borgman MA, Matos RI, Spinella PC. Isolated pediatric burn injury in Iraq and Afghanistan. Pediatr Crit Care Med. 2015;16(2):e23–7. 10.1097/PCC.0000000000000307 [DOI] [PubMed] [Google Scholar]
- 144.Bronstein I, Montgomery P. Sleeping patterns of Afghan unaccompanied asylum-seeking adolescents: a large observational study. PLoS One. 2013;8(2):e56156 10.1371/journal.pone.0056156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Busby C, Hamdan M, Ariabi E. Cancer, Infant Mortality and Birth Sex-Ratio in Fallujah, Iraq 2005–2009. International Journal of Environmental Research and Public Health. 2010;7(7):2828–37. 10.3390/ijerph7072828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chironna M, Germinario C, Lopalco PL, Carrozzini F, Quarto M. Prevalence of hepatitis virus infections in Kosovar refugees. Int J Infect Dis. 2001;5(4):209–13. [DOI] [PubMed] [Google Scholar]
- 147.Chironna M, Germinario C, Lopalco PL, Carrozzini F, Barbuti S, Quarto M. Prevalence rates of viral hepatitis infections in refugee Kurds from Iraq and Turkey. Infection. 2003;31(2):70–4. 10.1007/s15010-002-3100-3 [DOI] [PubMed] [Google Scholar]
- 148.Deeb M, Khlat M, Courbage Y. Child survival in Beirut during wartime: time trends and socio-religious differentials. Int J Epidemiol. 1997;26(1):110–9. [DOI] [PubMed] [Google Scholar]
- 149.Depoortere E, Checchi F, Broillet F, Gerstl S, Minetti A, Gayraud O, et al. Violence and mortality in West Darfur, Sudan (2003–04): epidemiological evidence from four surveys. Lancet. 2004;364(9442):1315–20. 10.1016/S0140-6736(04)17187-0 [DOI] [PubMed] [Google Scholar]
- 150.Devanarayana NM, Rajindrajith S. Association between Constipation and Stressful Life Events in a Cohort of Sri Lankan Children and Adolescents. Journal of Tropical Pediatrics. 2010;56(3):144–8. 10.1093/tropej/fmp077 [DOI] [PubMed] [Google Scholar]
- 151.Edwards MJ, Lustik M, Eichelberger MR, Elster E, Azarow K, Coppola C. Blast injury in children: An analysis from Afghanistan and Iraq, 2002–2010. Journal of Trauma and Acute Care Surgery. 2012;73(5):1278–83. 10.1097/TA.0b013e318270d3ee [DOI] [PubMed] [Google Scholar]
- 152.Edwards MJ, Lustik M, Carlson T, Tabak B, Farmer D, Edwards K, et al. Surgical interventions for pediatric blast injury: An analysis from Afghanistan and Iraq 2002 to 2010. Journal of Trauma and Acute Care Surgery. 2014;76(3):854–8. 10.1097/TA.0b013e3182aa2e66 [DOI] [PubMed] [Google Scholar]
- 153.Eide M, Gorman G, Hisle-Gorman E. Effects of parental military deployment on pediatric outpatient and well-child visit rates. Pediatrics. 2010;126(1):22–7. 10.1542/peds.2009-2704 [DOI] [PubMed] [Google Scholar]
- 154.Elbert T, Schauer M, Schauer E, Huschka B, Hirth M, Neuner F. Trauma-related impairment in children—a survey in Sri Lankan provinces affected by armed conflict. Child Abuse Negl. 2009;33(4):238–46. 10.1016/j.chiabu.2008.02.008 [DOI] [PubMed] [Google Scholar]
- 155.Gataa IS, Muassa QH. Patterns of maxillofacial injuries caused by terrorist attacks in Iraq: retrospective study. Int J Oral Maxillofac Surg. 2011;40(1):65–70. 10.1016/j.ijom.2010.07.005 [DOI] [PubMed] [Google Scholar]
- 156.Goma Epidemiology Group. Public health impact of Rwandan refugee crisis: what happened in Goma, Zaire, in July, 1994? Goma Epidemiology Group. Lancet. 1995;345(8946):339–44. [PubMed] [Google Scholar]
- 157.Greene JM, Cannon JW, Clouse WD, Pratt JW. Fragmentation injury to the innominate artery in a three-year-old child. Ann Thorac Surg. 2014;97(5):1788–90. 10.1016/j.athoracsur.2013.07.115 [DOI] [PubMed] [Google Scholar]
- 158.Grein T, Checchi F, Escriba JM, Tamrat A, Karunakara U, Stokes C, et al. Mortality among displaced former UNITA members and their families in Angola: a retrospective cluster survey. BMJ. 2003;327(7416):650 10.1136/bmj.327.7416.650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hicks MH, Dardagan H, Bagnall PM, Spagat M, Sloboda JA. Casualties in civilians and coalition soldiers from suicide bombings in Iraq, 2003–10: a descriptive study. Lancet. 2011;378(9794):906–14. 10.1016/S0140-6736(11)61023-4 [DOI] [PubMed] [Google Scholar]
- 160.Hisle-Gorman E, Harrington D, Nylund CM, Tercyak KP, Anthony BJ, Gorman GH. Impact of Parents’ Wartime Military Deployment and Injury on Young Children’s Safety and Mental Health. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54(4):294–301. [DOI] [PubMed] [Google Scholar]
- 161.Hoffer MM, Johnson B. Shrapnel wounds in children. J Bone Joint Surg Am. 1992;74(5):766–9. [PubMed] [Google Scholar]
- 162.Kvaskoff M, Bijon A, Clavel-Chapelon F, Mesrine S, Boutron-Ruault M-C. Childhood and Adolescent Exposures and the Risk of Endometriosis. Epidemiology. 2013;24(2):261–9. 10.1097/EDE.0b013e3182806445 [DOI] [PubMed] [Google Scholar]
- 163.Liu C, Urquia M, Cnattingius S, Hjern A. Migration and preterm birth in war refugees: a Swedish cohort study. Eur J Epidemiol. 2014;29(2):141–3. 10.1007/s10654-013-9877-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Metreveli IT, Vosk A. Pediatric casualties during the civil conflict in the Republic of Georgia 22 November-5 December 1991. Prehosp Disaster Med. 1994;9(1):71–2. [DOI] [PubMed] [Google Scholar]
- 165.Montgomery E, Foldspang A. Traumatic experience and sleep disturbance in refugee children from the Middle East. Eur J Public Health. 2001;11(1):18–22. [DOI] [PubMed] [Google Scholar]
- 166.Mujkic A, Peek-Asa C, Young T, Rodin U. Effect of war on weapon-related deaths in Croatian children and youth. Arch Pediatr Adolesc Med. 2008;162(2):140–4. 10.1001/archpediatrics.2007.31 [DOI] [PubMed] [Google Scholar]
- 167.Radoncic F, Hudic I, Balic A, Fatusic Z. Perinatal outcomes during 1986–2005 in Tuzla Canton, Bosnia and Herzegovina. J Matern Fetal Neonatal Med. 2008;21(8):567–72. 10.1080/14767050802165935 [DOI] [PubMed] [Google Scholar]
- 168.Reyna TM. Observations of a pediatric surgeon in the Persian Gulf War. J Pediatr Surg. 1993;28(2):209–13. [DOI] [PubMed] [Google Scholar]
- 169.Samms S, Wittich A, Graf K. Extraordinary military medical care of a pediatric patient with penetrating pelvic trauma: a case report. Mil Med. 2010;175(11):926–8. [DOI] [PubMed] [Google Scholar]
- 170.Santavirta T. Unaccompanied evacuation and adult mortality: evaluating the finnish policy of evacuating children to foster care during World War II. Am J Public Health. 2014;104(9):1759–65. 10.2105/AJPH.2014.301939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Schiff M, Benbenishty R, McKay M, Devoe E, Liu X, Hasin D. Exposure to terrorism and Israeli youths' psychological distress and alcohol use: an exploratory study. Am J Addict. 2006;15(3):220–6. 10.1080/10550490600626200 [DOI] [PubMed] [Google Scholar]
- 172.Schiff M, Zweig HH, Benbenishty R, Hasin DS. Exposure to terrorism and Israeli youths' cigarette, alcohol, and cannabis use. Am J Public Health. 2007;97(10):1852–8. 10.2105/AJPH.2006.090514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Schiff M, Pat-Horenczyk R, Benbenishty R, Brom D, Baum N, Astor RA. High school students' posttraumatic symptoms, substance abuse and involvement in violence in the aftermath of war. Soc Sci Med. 2012;75(7):1321–8. 10.1016/j.socscimed.2012.05.010 [DOI] [PubMed] [Google Scholar]
- 174.Shuker S. Spontaneous regeneration of the mandible in a child. A sequel to partial avulsion as a result of a war injury. J Maxillofac Surg. 1985;13(2):70–3. [DOI] [PubMed] [Google Scholar]
- 175.Spiegel PB. Notes from the field: mortality among refugees fleeing Somalia—Dadaab refugee camps, Kenya, July-August 2011. MMWR Morb Mortal Wkly Rep. 2011;60(33):1133 [PubMed] [Google Scholar]
- 176.Stern SC, Kumar R, Roberts IA. Aplastic anaemia after exposure to burning oil. Lancet. 1995;346(8968):183. [DOI] [PubMed] [Google Scholar]
- 177.Van Leent JP, Hopkins PF. Report of a mantoux survey of "displaced persons" migrant children. Med J Aust. 1951;1(19):673–6. [DOI] [PubMed] [Google Scholar]
- 178.Veale A, Dona G. Street children and political violence: a socio-demographic analysis of street children in Rwanda. Child Abuse Negl. 2003;27(3):253–69. [DOI] [PubMed] [Google Scholar]
- 179.Bayarogullari H, Yanmaz R, Kartal I, Burakgazi G. Two cases with giant pseudo-aneurysm of vertebral artery secondary to shrapnel injury. Child's Nervous System. 2016;32(11):2233–7. 10.1007/s00381-016-3075-5 [DOI] [PubMed] [Google Scholar]
- 180.Ceri V, Ozlu-Erkilic Z, Ozer U, Yalcin M, Popow C, Akkaya-Kalayci T. [Psychiatric symptoms and disorders among Yazidi children and adolescents immediately after forced migration following ISIS attacks]. Neuropsychiatrie. 2016;30(3):145–50. 10.1007/s40211-016-0195-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Duque V. Early-life conditions and child development: Evidence from a violent conflict. SSM—Population Health. 2017;3:121–31. 10.1016/j.ssmph.2016.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Hemat H, Shah S, Isaakidis P, Das M, Kyaw NTT, Zaheer S, et al. Before the bombing: High burden of traumatic injuries in Kunduz Trauma Center, Kunduz, Afghanistan. PLoS ONE. 2017;12 (3)(e0165270). 10.1371/journal.pone.0165270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Khamaysi I, Suissa A, Yassin K, Gralnek IM. Traumatic bile leak in war-injured Syrians: Five patients treated by ERCP. Endoscopy. 2015;47:E426–E7. 10.1055/s-0034-1392656 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files. The review is registered with PROSPERO, where the full search strategy is available: https://www.crd.york.ac.uk/PROSPEROFILES/36425_STRATEGY_20170427.pdf.