Abstract
Background
This study assessed the therapeutic effect of adjunctive bifrontal transcranial direct current stimulation (tDCS) in patients with tinnitus.
Methods
Forty-four patients who visited our university hospital with a complaint of non-pulsatile subjective tinnitus in January through December 2016 were enrolled. All patients received directive counseling and sound therapy, such as a sound generator or hearing aids, and/or oral clonazepam. Patients who agreed to undergo additional bifrontal tDCS were classified as the study group (n = 26). For tDCS, 1.5 mA of direct current was applied to the prefrontal cortex with a 10–20 EEG system for 20 minutes per session.
Results
The Tinnitus Handicap Inventory (THI), Beck Depression Inventory, and Visual Analog Scale (VAS) scores decreased significantly after treatment (P < 0.001). Patients who had a moderate or catastrophic handicap were significantly more likely to respond favorably to bifrontal tDCS (P = 0.026). There was no correlation of number of tDCS sessions with change in the THI or VAS score (P > 0.05). Logistic regression analysis revealed that the initial THI score was independently associated with improvement in the THI. However, tDCS was not a significant determinant of recovery.
Conclusion
tDCS can be used as an adjunctive treatment in patients with severe tinnitus. Although tDCS did not decrease the loudness of tinnitus, it could alleviate the distress associated with the condition in some patients with a moderate or catastrophic handicap.
Keywords: Adjunctive Bifrontal Transcranial Direct Current Stimulation, Distress, Tinnitus
Graphical Abstract
INTRODUCTION
Tinnitus is a troublesome symptom involving perception of sounds without a source. Individuals with tinnitus have frequent symptoms that negatively affect quality of life. The epidemiologic characteristics of tinnitus differ widely from population to population and from country to country. In Korea, the prevalence of tinnitus was reported to be 19.7% in individuals aged 12 years or older, with a women predominance.1 In the UK, the prevalence was reported to be 16.9% in the 40–69-year age group.2 A study based on the 1999–2004 National Health and Nutrition Examination Survey in the US reported that the risk of tinnitus increased with advancing age and that the majority of individuals with the disorder were in their sixties.3
Auditory deafferentation is caused by various conditions, including ageing, exposure to noise, and diseases affecting the middle ear, that may lead to reorganization of the auditory cortex.4 Altered tinnitus-related functional connectivity between different regions of the brain, involvement of non-auditory brain networks, such as perception, salience, and distress networks, as well as the memory area also play a role in the maintenance of tinnitus.5 Consequently, tinnitus is related to pathologic changes in the brain and is not confined to peripheral hearing loss.
Various neuromodulation techniques, such as transcranial direct current stimulation (tDCS) and repetitive transcranial magnetic stimulation (rTMS), have been introduced for treatment of diverse neurologic disorders, including chronic pain, Parkinson's disease, stroke, aphasia, multiple sclerosis, epilepsy, Alzheimer's disease, depression, and tinnitus.6,7 The stimulation targets most frequently used for tinnitus include not only the auditory cortex but also the prefrontal cortex and the anterior cingulate cortex. It is thought that reversal of pathologic neural activity is modulated directly or indirectly in the functionally connected brain networks.
Bifrontal tDCS uses a weak current of 0.2–2.0 mA and alters the excitability of the cortex; anodal tDCS increases cortical excitability and cathodal tDCS decreases excitability by hyperpolarization.6 In a previous study, we demonstrated that about 80% of patients showed a 50% or greater decrease in the Tinnitus Handicap Inventory (THI) score when treated with tDCS combined with tailor-made notched music training (TMNMT).6 However, not all patients like TMNMT, which relies on ready availability of preferred music and involves a very long treatment period. In addition, the small sample size in our previous study limited our ability to interpret its results.
The aims of the present study were to evaluate the therapeutic effect of bifrontal tDCS for tinnitus in a large sample size and to determine whether this treatment modality has a role adjunctive to that of conventional treatment.
METHODS
Patients
Patients who visited the tinnitus clinic at our university hospital between January and December 2016 complaining of non-pulsatile subjective tinnitus that had persisted for at least 3 months and followed up for longer than one month were screened. The exclusion criteria were as follows: THI, Beck Depression Inventory (BDI), and Visual Analog Scale (VAS) scores not obtained or obtained only once; previous tDCS; a history of treatment with other types of neuromodulation, such as vagus nerve stimulation, transcranial random noise stimulation (tRNS), or rTMS; and presence of patient factors precluding evaluation of tinnitus, such as mental retardation, schizophrenia, or low compliance.
Treatment protocols
The patients were divided into a tDCS group and a conventional treatment group. The conventional treatment group received 2–8 weeks of directive counselling based on the Jastreboff neurophysiologic model, sound therapy that included a sound generator or hearing aids, and clonazepam for patients who wished to take medication.
The tDCS group underwent tDCS in addition to conventional treatment. tDCS was delivered using a DC-Stimulator Plus (neuroConn GmbH, Ilmenau, Germany). Saline-soaked cathodal and anodal electrodes (each with an area of 35 cm2) were placed over the F3 and F4 areas, respectively, in accordance with the 10–20 system, in order to stimulate the dorsolateral prefrontal cortex (DLPFC) bilaterally. The intensity and duration of stimulation were set to 1.5 mA and 20 minutes (a 10-seconds fade-in/fade-out time), respectively.
Follow-up and evaluation of response to treatment
All patients were instructed to visit the hospital at monthly intervals. Responses on the THI, BDI, and VAS were checked at each visit until the end of treatment. The initial severity of tinnitus-related distress was classified as slight (THI score 0–16), mild (18–36), moderate (38–56), severe (58–76), or catastrophic (78–100). Patients with a final improvement in THI score of ≥ 20 were defined as treatment responders and those with a final improvement of < 20 were considered non-responders.
Statistical analysis
The χ2 and Fisher's exact tests were used to compare the data between groups and to analyze trends. The nominal data are presented as the mean, standard deviation, and range unless otherwise stated. The Shapiro-Wilk test was performed to test the data for normality. The paired t-test was used to compare the pretreatment and post-treatment THI, BDI, and VAS scores. Pearson correlation analysis was used to assess the relationship between number of tDCS sessions and the change in THI Score. All statistical analyses were performed using SPSS version 25.0 software (IBM Corp., Armonk, NY, USA). A P value < 0.05 was considered statistically significant.
Ethics statement
This study was performed in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Eulji University (EMC IRB 2018-06-010). IRB granted a waiver of written informed consent for this study.
RESULTS
Patient characteristics
Seventy patients (37 men, 33 women; mean age, 47.81 ± 14.1 [range, 18–82] years) were recruited (Table 1). Forty-four patients had unilateral tinnitus and 26 had bilateral tinnitus. The mean interval between symptom onset and treatment was 23.94 ± 53.93 (range, 3–360) months; the mean hearing level on the right was 21.97 ± 22.00 dB and that on the left was 20.57 ± 20.03 dB. The initial THI and BDI scores were 47.29 ± 24.474 (range, 12–100) and 12.03 ± 9.92 (range, 0–44), respectively. When the mean interval was classified according to THI score, it was longest in patients with severe handicap (Table 2). The mean initial VAS tinnitus loudness score was 4.87 ± 2.47. The mean follow-up duration was 8.29 ± 9.26 months.
Table 1. Patient characteristics.
| Variables | Total patients (n = 70) | Bifrontal tDCS treatment group (n = 26) | Conventional treatment group (n = 44) | P value | |
|---|---|---|---|---|---|
| Age, yr | 45 ± 16.4 | 44 ± 9.6 | 50 ± 15.9 | 0.072 | |
| Gender | 0.899 | ||||
| Men | 37 (52.9) | 14 (53.8) | 23 (52.3) | ||
| Women | 33 (47.1) | 12 (46.2) | 21 (47.7) | ||
| Onset of tinnitus, mon | 23.94 ± 53.93 | 26.23 ± 45.56 | 22.59 ± 58.77 | 0.787 | |
| Laterality | 0.076 | ||||
| Uniltaeral | 44 (62.9) | 20 (76.9) | 24 (54.5) | ||
| Bilateral | 26 (37.1) | 6 (23.1) | 20 (45.5) | ||
| History of trauma | 6 (8.6) | 3 (11.5) | 3 (6.8) | 0.664 | |
| Hearing thresholds, dB | |||||
| Right | 21.97 ± 22.00 | 26.19 ± 25.44 | 19.48 ± 19.57 | 0.220 | |
| Left | 20.57 ± 20.03 | 18.04 ± 19.57 | 22.07 ± 22.33 | 0.420 | |
| Follow-up periods, mon | 8.29 ± 9.26 | 10.36 ± 11.77 | 6.77 ± 7.23 | 0.118 | |
| Initial assessment | |||||
| THI | 47.29 ± 24.47 | 57.92 ± 22.16 | 41.00 ± 23.81 | 0.004 | |
| BDI | 12.03 ± 9.92 | 14.48 ± 11.43 | 10.64 ± 8.79 | 0.123 | |
| Final assessment | |||||
| THI | 28.06 ± 19.24 | 29.23 ± 17.99 | 27.36 ± 20.11 | 0.698 | |
| BDI | 9.59 ± 8.85 | 9.73 ± 10.03 | 9.46 ± 7.84 | 0.919 | |
| VAS for loudness | 3.7 ± 2.46 | 4.15 ± 2.15 | 3.43 ± 2.61 | 0.238 | |
Data are presented as mean ± standard deviation for numerical variables and number (%) for nominal variables.
tDCS = transcranial direct current stimulation, THI = Tinnitus Handicap Inventory, BDI = Beck Depression Inventory, VAS = Visual Analog Scale (0–10).
Table 2. Mean intervals between symptom and treatment according to score for initial THI.
| Score for THI | Total group, mon | Bifrontal tDCS treatment group, mon | Conventional treatment group, mon |
|---|---|---|---|
| Slight (THI 0–16) | 21.71 ± 16.44 | - | 25.17 ± 19.02 |
| Mild (THI 18–36) | 12.52 ± 5.37 | 34.25 ± 28.68 | 7.95 ± 2.67 |
| Moderate (THI 38–56) | 17.79 ± 8.39 | 14.86 ± 5.08 | 20.71 ± 16.62 |
| Severe (THI 58–76) | 44.36 ± 25.18 | 39.67 ± 12.86 | 59.13 ± 43.59 |
| Catastrophic (THI 78–100) | 30.50 ± 16.64 | 36.50 ± 24.40 | 18.50 ± 14.07 |
Data are presented as mean ± standard deviation for numerical variables.
THI = Tinnitus Handicap Inventory, tDCS = transcranial direct current stimulation.
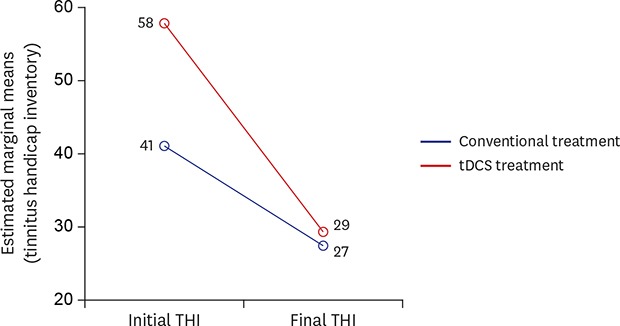
Twenty-six (37.1%) of the 70 patients received 1–6 sessions of tDCS (mean, 1.04 ± 1.89) and the remaining 44 received conventional treatment. There was no significant difference in age, gender, side affected by tinnitus, history of trauma, onset, or hearing level on either side between the two study groups. The mean follow-up duration was 10.36 ± 11.77 months in the tDCS group and 6.77 ± 7.23 months in the conventional treatment group. The mean initial THI score was higher in the tDCS group than in the conventional treatment group (57.92 ± 22.16 vs. 41 ± 23.81; P = 0.004). There was no significant between-group difference in the BDI score (P > 0.05). The VAS score for tinnitus loudness was significantly higher in the tDCS group than in the conventional treatment group (5.73 ± 2.52 vs. 4.36 ± 2.314; P = 0.024).
Outcomes according to treatment method
Initially, we analyzed all of the enrolled patients' data together, irrespective of study group. The post-treatment THI and VAS scores indicated a significant reduction in patient distress and tinnitus loudness (P < 0.001). In total, the final THI score was 28.06 ± 19.24 and the final VAS score was 3.70 ± 2.46 (Table 1). The BDI score decreased to 9.59 ± 8.85 after treatment (P = 0.006). The χ2 test for trend demonstrated that patients with an initial THI score indicating more severe tinnitus-related distress tended to be treatment responders (P < 0.001). The percentages of patients with mild to catastrophic handicap who responded to treatment were 0% (0/7) for slight handicap, 26.1% (6/23) for mild handicap, 50% (7/14) for moderate handicap, 78.6% (11/14) for severe handicap, and 75% (9/12) for catastrophic handicap.
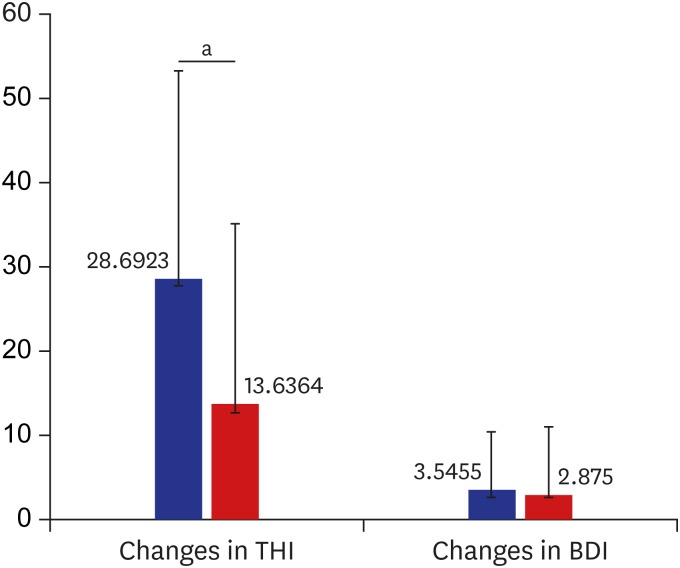
The final THI scores were then analyzed separately according to treatment group. The change in the mean THI score was greater in the tDCS group than in the conventional treatment group (28.69 ± 24.81 vs. 13.63 ± 21.59; P = 0.010) (Fig. 1). However, there was no significant between-group difference in the mean BDI score or VAS score after treatment (P > 0.05).
Fig. 1. Changes in questionnaire scores after treatment. The blue color indicates patients treated with bifrontal tDCS. The red color indicates patients treated conventionally. The error bars indicate the standard deviation in each group.
tDCS = transcranial direct current stimulation, BDI = Beck Depression Inventory, THI = Tinnitus Handicap Inventory.
aP < 0.05.
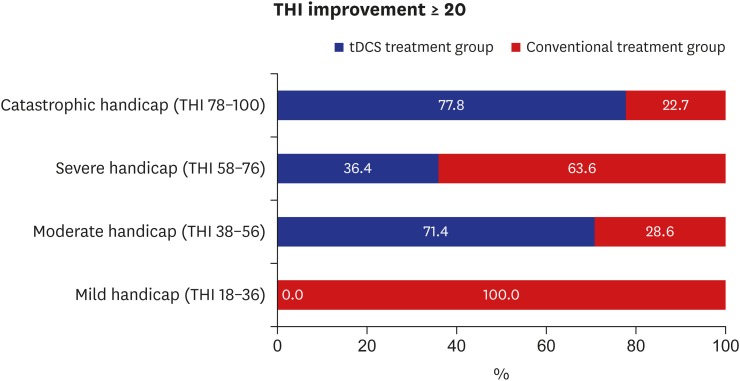
In patients whose final improvement in THI score was ≥ 20, differences were observed according to the initial degree of tinnitus severity and type of treatment received (P = 0.011; χ2). Treatment responders with initially moderate or catastrophic handicap were more likely to have received tDCS (Fig. 2); however, treatment responders with initially severe handicap were more likely to have received conventional treatment. None of the patients in the tDCS group with initially mild symptoms showed an improvement in THI of ≥ 20. However, there was no significant difference in the initial severity of tinnitus or type of treatment received in patients whose final THI score improvement was < 20 (P > 0.05).
Fig. 2. Proportion of treatment responders in each group according to initial degree of tinnitus handicap.
tDCS = transcranial direct current stimulation, THI = Tinnitus Handicap Inventory.
Pearson correlation analysis revealed no correlation between change in THI score and number of tDCS sessions (r = 0.068; P = 0.692). Similarly, there was no correlation between the number of tDCS sessions and the BDI or VAS score for tinnitus loudness (P > 0.05).
Prognostic factors
Conditional logistic regression analysis revealed a positive association of the initial THI score with an improvement in THI of ≥ 20 (odds ratio [OR], 1.060; 95% confidence interval [CI], 1.031–1.091; P < 0.001) and a negative association with a final THI score < 18 (OR, 0.969; CI, 0.945–0.993; P = 0.013). Thus, patients with more severe tinnitus-related distress initially were classified as responders after treatment but those with lower initial levels of distress showed better final recovery. Unexpectedly, the regression model did not identify application of tDCS as an independent prognostic factor for improvement in the THI score.
DISCUSSION
In this study, we found that tinnitus-related distress was alleviated in some patients who were treated with additional bifrontal tDCS targeting the DLPFC but that application of tDCS was not in itself an independent prognostic factor. These findings suggest that the therapeutic effect of bifrontal tDCS may be weak and that the severity of tinnitus-related distress may vary according to involvement of the DLPFC. It has been reported that the DLPFC plays a role in tinnitus by facilitating auditory memory and modulating input to the primary auditory cortex, leading to top-down inhibitory modulation of auditory processing.8,9 The number of tDCS sessions was not correlated with the THI, BDI, or VAS scores, suggesting the dose-dependent relationship may be limited in bifrontal tDCS.
Previous studies have shown that the results of application of rTMS to both the prefrontal cortex and the auditory cortex are better than stimulation of the prefrontal cortex or auditory cortex alone.10,11 Similarly, applying tRNS to the auditory cortex after bifrontal tDCS resulted in a significant decrease in both tinnitus loudness and tinnitus-related distress.12 A single session of tRNS applied to the auditory cortex was reported to achieve a significant decrease in tinnitus loudness and tinnitus-related distress, and multiple tRNS sessions seemed to be more effective than a single session or use of an alternative method of current stimulation.13 In view of the evidence thus far, a further study is needed to investigate the effects of multi-site stimulation in conjunction with combined tDCS-tRNS beyond bifrontal tDCS.
In contrast, there was no statistically significant treatment-related difference in the changes in and final scores for the BDI and VAS. This suggests that bifrontal tDCS may be less able to control depressive symptoms or reduce the loudness of tinnitus than expected. One research group has compared the efficacy of tDCS with that of escitalopram, which is one of the most commonly used serotonin reuptake inhibitors, in patients with major depressive disorder.14 Although results of 22 sessions of tDCS were superior to those of placebo, some patients developed new-onset mania as well as itching and skin redness; further, escitalopram was more effective than tDCS in that study. Therefore, medical treatment should be considered before tDCS in patients with tinnitus and severe depression even though a recent guideline cautions against routine prescription of antidepressants, anticonvulsants, or anxiolytics.15
Interestingly, all treatment responders who had initially mild tinnitus received conventional treatment alone. This suggests that bifrontal tDCS has no additional effect in patients with mild tinnitus-related distress. Moreover, patients who responded to bifrontal tDCS were more likely to have moderate or catastrophic handicap than severe handicap. We assume that this finding, although not statistically significant, might reflect the longer duration of severe handicap than that in the other subgroups. A factor analysis study of rTMS reported that tinnitus was suppressed in patients with a shorter duration of tinnitus, normal hearing, and no sleep disturbance, and suggested that the central auditory network becomes less plastic over time,16 which supports our assumption. Patients with severe tinnitus-related distress of short duration may be ideal candidates for neuromodulation.
The location of the surface electrodes is another issue. In order to stimulate the bifrontal cortex, the electrodes have been traditionally placed in one of two ways, i.e., “left-anode-right-cathode montage” or “right-anode-left-cathode montage.”7 The former montage has been reported to achieve greater improvement of the depressive symptoms of tinnitus while the latter montage alleviates anxiety.6,17 However, we could not find evidence to support this concept. High-definition tDCS using a 4 × 1 ring electrode targeting the right DLPFC has been developed for more precise current delivery.18 A recent study also suggested the possibility of stimulating the anterior cingulate cortex with high-definition tDCS; this structure is located deeply and its function is related to emotional experience and tinnitus-related distress.19,20 A previous study of rTMS demonstrated that preceding mediofrontal stimulation of the anterior cingulate cortex with a double cone-coil before rTMS to the auditory cortex achieved better results than conventional rTMS targeting the left DLPFC and auditory cortex.20 Therefore, future tDCS studies should concentrate on using high-definition tDCS to stimulate various brain regions more precisely.
This study has several limitations. First, our analysis was based on data derived from a retrospective medical chart review. Second, not all patients complied with conventional treatment; for example, some patients refused to accept the sound generator or hearing aids because of the additional cost involved or because they felt self-conscious when wearing these devices. Third, more objective tools for assessment of tinnitus, such as radiologic evaluation or electroencephalography, were not used in this study. Nevertheless, we were able to assess the clinical importance of bifrontal tDCS by observing the natural course of tinnitus in patients in this retrospective cohort study. Finally, the number of sessions performed was relatively small. Nevertheless, some patients who had a higher tinnitus handicap showed a favorable treatment outcome. Given that tinnitus tends to wax and wane, adjunctive application of bifrontal tDCS at times when tinnitus is severe would help to alleviate the tinnitus-related distress.
In summary, patients with tinnitus who received conventional treatment plus bifrontal tDCS showed a significant reduction in THI score but not in VAS tinnitus loudness or BDI scores. In particular, patients treated with tDCS who initially had moderate or catastrophic handicap were more likely to show improvement in their THI score. However, application of additional bifrontal tDCS was not identified as a significant prognostic factor for improvement of the THI score. Bifrontal tDCS can be used as an adjunctive treatment for severe tinnitus. Although this treatment modality does not reduce tinnitus loudness, addition of bifrontal tDCS to conventional treatment alleviates the distress associated with tinnitus in some patients with moderate or catastrophic handicap.
Footnotes
Funding: This research was funded by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2017R1C1B5017839).
Disclosure: The author has no potential conflicts of interest to disclose.
References
- 1.Park KH, Lee SH, Koo JW, Park HY, Lee KY, Choi YS, et al. Prevalence and associated factors of tinnitus: data from the Korean National Health and Nutrition Examination Survey 2009–2011. J Epidemiol. 2014;24(5):417–426. doi: 10.2188/jea.JE20140024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dawes P, Fortnum H, Moore DR, Emsley R, Norman P, Cruickshanks K, et al. Hearing in middle age: a population snapshot of 40- to 69-year olds in the United Kingdom. Ear Hear. 2014;35(3):e44–e51. doi: 10.1097/AUD.0000000000000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shargorodsky J, Curhan GC, Farwell WR. Prevalence and characteristics of tinnitus among US adults. Am J Med. 2010;123(8):711–718. doi: 10.1016/j.amjmed.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Hoare DJ, Adjamian P, Sereda M. Electrical stimulation of the ear, head, cranial nerve, or cortex for the treatment of tinnitus: a scoping review. Neural Plast. 2016;2016:5130503. doi: 10.1155/2016/5130503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peter N, Kleinjung T. Neuromodulation for tinnitus treatment: an overview of invasive and non-invasive techniques. J Zhejiang Univ Sci B. 2018 doi: 10.1631/jzus.B1700117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee HY, Choi MS, Chang DS, Cho CS. Combined bifrontal transcranial direct current stimulation and tailor-made notched music training in chronic tinnitus. J Audiol Otol. 2017;21(1):22–27. doi: 10.7874/jao.2017.21.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lefaucheur JP, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, et al. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS) Clin Neurophysiol. 2017;128(1):56–92. doi: 10.1016/j.clinph.2016.10.087. [DOI] [PubMed] [Google Scholar]
- 8.Taira T. Tinnitus: from traditional concept to challenges to loosen the gordian knot. World Neurosurg. 2012;77(5-6):651–653. doi: 10.1016/j.wneu.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Engineer ND, Riley JR, Seale JD, Vrana WA, Shetake JA, Sudanagunta SP, et al. Reversing pathological neural activity using targeted plasticity. Nature. 2011;470(7332):101–104. doi: 10.1038/nature09656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noh TS, Kyong JS, Chang MY, Park MK, Lee JH, Oh SH, et al. Comparison of treatment outcomes following either prefrontal cortical-only or dual-site repetitive transcranial magnetic stimulation in chronic tinnitus patients: a double-blind randomized study. Otol Neurotol. 2017;38(2):296–303. doi: 10.1097/MAO.0000000000001266. [DOI] [PubMed] [Google Scholar]
- 11.Park S, Park HJ, Kyeong SH, Moon IS, Kim M, Kim HN, et al. Combined rTMS to the auditory cortex and prefrontal cortex for tinnitus control in patients with depression: a pilot study. Acta Otolaryngol. 2013;133(6):600–606. doi: 10.3109/00016489.2012.763181. [DOI] [PubMed] [Google Scholar]
- 12.To WT, Ost J, Hart J, Jr, De Ridder D, Vanneste S. The added value of auditory cortex transcranial random noise stimulation (tRNS) after bifrontal transcranial direct current stimulation (tDCS) for tinnitus. J Neural Transm (Vienna) 2017;124(1):79–88. doi: 10.1007/s00702-016-1634-2. [DOI] [PubMed] [Google Scholar]
- 13.Claes L, Stamberger H, Van de Heyning P, De Ridder D, Vanneste S. Auditory cortex tACS and tRNS for tinnitus: single versus multiple sessions. Neural Plast. 2014;2014:436713. doi: 10.1155/2014/436713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brunoni AR, Moffa AH, Sampaio-Junior B, Borrione L, Moreno ML, Fernandes RA, et al. Trial of electrical direct-current therapy versus escitalopram for depression. N Engl J Med. 2017;376(26):2523–2533. doi: 10.1056/NEJMoa1612999. [DOI] [PubMed] [Google Scholar]
- 15.Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER, Jr, et al. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg. 2014;151(2) Suppl:S1–S40. doi: 10.1177/0194599814545325. [DOI] [PubMed] [Google Scholar]
- 16.Wang H, Li B, Wang M, Li M, Yu D, Shi H, et al. Factor analysis of low-frequency repetitive transcranial magnetic stimulation to the temporoparietal junction for tinnitus. Neural Plast. 2016;2016:2814056. doi: 10.1155/2016/2814056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faber M, Vanneste S, Fregni F, De Ridder D. Top down prefrontal affective modulation of tinnitus with multiple sessions of tDCS of dorsolateral prefrontal cortex. Brain Stimulat. 2012;5(4):492–498. doi: 10.1016/j.brs.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Shekhawat GS, Vanneste S. High-definition transcranial direct current stimulation of the dorsolateral prefrontal cortex for tinnitus modulation: a preliminary trial. J Neural Transm (Vienna) 2018;125(2):163–171. doi: 10.1007/s00702-017-1808-6. [DOI] [PubMed] [Google Scholar]
- 19.Kreuzer PM, Lehner A, Schlee W, Vielsmeier V, Schecklmann M, Poeppl TB, et al. Combined rTMS treatment targeting the anterior cingulate and the temporal cortex for the treatment of chronic tinnitus. Sci Rep. 2015;5:18028. doi: 10.1038/srep18028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.To WT, Eroh J, Hart J, Jr, Vanneste S. Exploring the effects of anodal and cathodal high definition transcranial direct current stimulation targeting the dorsal anterior cingulate cortex. Sci Rep. 2018;8(1):4454. doi: 10.1038/s41598-018-22730-x. [DOI] [PMC free article] [PubMed] [Google Scholar]