Abstract
Objectives
To identify emergency department (ED) heart rate (HR) values that identify children at elevated risk of ED revisit with admission.
Methods
We performed a retrospective cohort study of patients 0 to 18 years discharged from a tertiary-care pediatric ED from January 2013 to December 2014. We created percentile curves for the last-recorded HR-for-age using data from calendar year 2013 and used receiver operating characteristic curves to characterize the performance of the percentiles for predicting ED revisit with admission within 72 hours. In a held-out validation dataset (calendar year 2014 data), we evaluated test characteristics of last-recorded HR-for-age cutpoints identified as promising on the ROC curves, as well as those identifying the highest 5% and 1% of last-recorded HRs-for-age.
Results
We evaluated 183,433 eligible ED visits. Last-recorded HR-for-age had poor discrimination for predicting revisit with admission (area under the curve 0.61, 95% confidence interval 0.58, 0.63). No promising cutpoints were identified on the receiver operative characteristic curves. Cutpoints identifying the highest 5% and 1% of last-recorded HRs-for-age showed low sensitivity (10.1% and 2.5%) with numbers needed to evaluate of 62 and 50, respectively, to potentially prevent one revisit with admission.
Conclusions
Last-recorded ED HR discriminates poorly between children who are and are not at risk for revisit with admission in a pediatric emergency department. The use of single-parameter HR in isolation as an automated trigger for mandatory reevaluation prior to discharge may not improve revisit outcomes.
Keywords: Discharge, readmissions, vital signs, quality improvement
Introduction
Rapidly distinguishing between children who are dangerously ill and children who are ill but will recover with minimal or no intervention is one of the key challenges of pediatric emergency care. In order to avoid discharging children with dangerous illnesses (including, notably, sepsis),1 some emergency departments (EDs) have sought to use discharge vital signs as an adjunct to clinical judgment, often by mandating reevaluation of patients with an elevated HR.2 Such policies may prompt therapy to reduce HR, such as fluid boluses or antipyretics, and may delay or prevent discharge.
The clinical utility of discharge HR-based reevaluation strategies has not been demonstrated. If these strategies are effective at identifying children in need of additional care, they should be more widely implemented. However, even interventions with strong face validity may be ineffective. Implementation of ineffective strategies may reduce time and resources available for more high-yield activities or may lead to unintended negative consequences. The choice of HR cutpoints may impact the effectiveness of discharge-HR based interventions. In practice, most HR cutpoints for children are based on expert opinion and are not empirically derived.3–8 One recent publication identified an association between a pre-specified measure of elevated HR for age (above the 99th percentile for healthy outpatients) and a small increased risk of revisit (risk ratio 1.3) but no increased risk in a composite outcome of revisit with clinically important intervention or admission.9
We sought to empirically identify cutpoints for discharge heart rate (HR) that would identify children at high risk of revisit with admission after ED discharge using a large electronic health record dataset. We also aimed to identify alternate measures of HR that may be more effective and subsets of patients for whom evaluation of discharge HR may be particularly useful.
Materials and Methods
Study design and setting
We performed a retrospective study of children visiting the Children’s Hospital of Philadelphia emergency department (ED) in calendar years 2013 and 2014. This ED is a large, urban, academic, tertiary-care pediatric ED with approximately 90,000 visits per year.
Selection of participants
We extracted demographic and clinical data from the electronic (Epic™) health record. We evaluated all children less than 18 years of age during the study time period with at least one index ED visit. An index visit was defined as any ED visit with at least one HR that ended in a disposition of discharge and was not preceded by another ED visit within 7 days. We included all eligible visits for patients with multiple visits.
Measurements
Revisits were defined as any visit to the ED within 72 hours of discharge from an index visit. Revisit with admission was defined as any revisit within 72 hours of discharge that ended in a disposition of admission to the hospital, admission to the observation unit, or death. We evaluated the last-recorded HR prior to ED discharge, even when only one HR was recorded. Triage HR, maximum HR, body temperature at the time of triage HR and last-recorded HR, medications given during the visit, and ED disposition were also extracted.
Outcome
Our primary outcome was the proportion of index ED visits followed by an ED revisit with admission within 72 hours. Revisit with admission was chosen as the primary outcome because it was considered more likely to identify children with serious unrecognized illness at the initial visit. Alternate outcomes were evaluated, including any revisit, as described further in the sensitivity analysis section below.
Analysis overview
Our primary analysis was performed in three steps. First, we developed percentile curves for last-recorded HR-for-age which would allow us to evaluate the relationship between vital signs and outcomes across ages. Second, we used data from 2013 to create receiver operating characteristic (ROC) curves to identify candidate cutpoints for last-recorded HR using an outcome of ED revisit with admission within 72 hours. Finally, we used data from 2014 to evaluate the performance of candidate HR-for-age cutpoints. Details of these steps are presented below.
Percentile creation
We used HR data from visits in 2013 ending in discharge, admission, or observation to create the percentiles. A random subset (40%) of the data was used to generate the curves and the remaining 60% was used to evaluate the fit of the percentiles overall and within 5 age groups: less than 1 year, 1 to less than 3 years, 3 to less than 6 years, 6 to less than 12 years, and 12 years and older. We initially used the GAMLSS package in R software to create a last-recorded HR-for-age percentile reference that would allow conversion of HRs to z-scores.10 However, the distribution of last-recorded HRs differed from a normal distribution in a manner that could not be modeled well using the GAMLSS framework, and the fit of the upper centiles in the validation dataset was poor. Therefore, we created a last-recorded HR-for-age percentile reference using quantile regression with cubic splines, a method that does not require any assumptions about the underlying distribution of data.11 We created multiple upper centile curves (12 levels ≥90th percentile) to allow identification of the level best associated with the outcomes of interest.
Cutpoint identification
For the primary analysis presented here, we generated ROC curves examining the relationship between last-recorded HR percentile and our primary outcome in discharged patients in 2013. We considered 5% and 1% to be the upper and lower bounds of the proportion of ED visits for which it may be feasible to delay discharge in order to perform some degree of further observation, evaluation or treatment, ranging from a single set of repeat vital signs to admission. Therefore, we chose to examine cutpoints for the highest 5% and 1% of discharge HR among discharged patients using 2014 data, in addition to any promising cutpoints identified from the ROC curves.
Performance of candidate cutpoints
We calculated standard test characteristics for candidate HR percentile cutpoints.
Sensitivity Analyses
The primary analysis included all index visits. After the primary analysis, we performed sensitivity analyses using 2014 data to evaluate alternate HR measures, restricted inclusion criteria, and alternate outcomes. For each sensitivity analysis only the parameter(s) indicated were changed, otherwise the inclusion criteria (all discharged visits in 2014), HR cutpoint (last-recorded HR-for-age percentiles), and outcome (revisit with admission within 72 hours) of the primary analysis were used. The sensitivity analyses are detailed below:
Additional HR types and temperature-adjusted HR: We created percentiles for triage-for-age and maximum HR-for-age (the maximum HR observed during the ED visit) using 2013 data. We also created and evaluated HR-for-age percentiles adjusted for body temperature for last HR and triage HR by subtracting 10 beats per minute for each degree Celsius above 37 and adding 10 beats per minute for each degree Celsius below 37.12–14 When a simultaneously recorded temperature was not available, we used the HR without adjustment. For each set of percentiles, we evaluated discrimination with ROC curves and determined the cutpoints that identify the highest 5% and 1% of HRs-for-age.
Restricted inclusion criteria: Last-recorded HR may be related to outcomes differently in visits with certain characteristics, either because of true physiologic differences or altered clinician behavior related to HR. Therefore, we evaluated the test characteristics of candidate last-recorded HR-for-age cutpoints in three restricted groups. First, we restricted the sample to visits in which albuterol had not been given, because of the effect of beta-agonist medications on HR. Second, we restricted the sample to visits in which one or more boluses of intravenous fluid had been given, because HR is often a factor considered when determining the need for an intravenous bolus and assessing the adequacy of the response to a bolus. We used logistic regression to compare the risk of revisit for visits with and without albuterol administration and with and without bolus administration. Finally, we restricted the sample to visits in which the last HR was recorded 30 minutes or fewer before discharge, as these HRs are more likely to be representative of the HR at the time of discharge.
Varied outcomes: We evaluated the predictive value and test characteristics of selected cutpoints above for the following alternate outcomes: any ED revisit, ED revisit with intensive care unit (ICU) admission, and ED revisit with admission within 1 or 7 days.
Resolution of tachycardia: We identified visits in which any HR, starting at triage, was above the highest 5% cutpoint for last-recorded HR-for-age. Among those visits, we considered visits in which the last-recorded HR was less than this cutpoint to have resolved tachycardia, and used logistic regression to evaluate whether resolved tachycardia was associated with a change in risk of ED revisit, with or without admission, within 72 hours.
Statistical analyses were done using Stata 14.2 [College Station, Texas]. The study was designated not human subjects research by the Institutional Review Board (IRB) at Penn State College of Medicine and met criteria for not human subjects research set by the Children’s Hospital of Philadelphia IRB.
Results
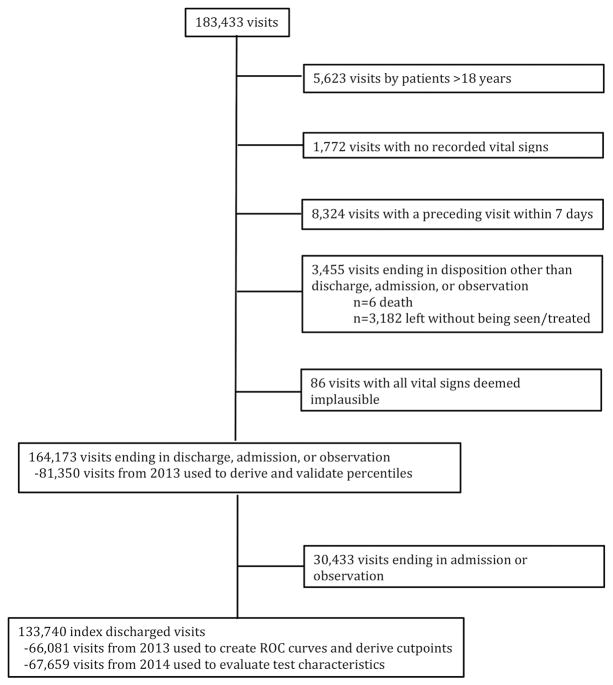
There were 183,433 visits by 104,159 patients in 2013 and 2014 (Figure 1). Visit data from 2013 and 2014 showed generally similar demographic and visit characteristics, including a similar prevalence of ED revisits with admission (0.8%, Table 1). The proportion of visits with a HR within 30 minutes of discharge was higher in 2014 than 2013 (p<0.001).
Figure 1.
Flowchart of visit exclusions and included data
Table 1.
Demographic and clinical information, by visit
| 2013 | 2014 | |||
|---|---|---|---|---|
| N | % | N | % | |
| Total included visits | 81,350 | 82,823 | ||
| Distinct patients | 61,949 | 59,367 | ||
| Age | ||||
| 0 to <1 year | 13,058 | 16% | 12,958 | 16% |
| 1 to <4 years | 24,882 | 31% | 24,954 | 30% |
| 4 to <12 years | 28,437 | 35% | 29,345 | 35% |
| 12 to <18 years | 14,973 | 18% | 15,566 | 19% |
| Race | ||||
| American Indian or Alaska Native | 51 | 0.06% | 57 | 0.07% |
| Asian | 2,523 | 3% | 2,466 | 3% |
| Black or African American | 50,308 | 62% | 50,630 | 61% |
| Native Hawaiian or other Pacific Islander | 70 | 0.09% | 86 | 0.1% |
| White | 19,511 | 24% | 20,088 | 24% |
| Multiple Races | 1,225 | 2% | 1,367 | 2% |
| Other | 7,629 | 9% | 8,083 | 10% |
| Unknown | 33 | 0.04% | 46 | 0.06% |
| Ethnicity | ||||
| Hispanic or Latino | 6,118 | 8% | 6,337 | 8% |
| Not Hispanic or Latino | 75,191 | 92% | 76,409 | 92% |
| Unknown | 41 | 0.05% | 77 | 0.09% |
| Chief complainta | ||||
| Fever | 13,501 | 17% | 13,091 | 16% |
| Respiratory distress | 16,315 | 20% | 17,238 | 21% |
| Trauma | 13,251 | 16% | 13,395 | 16% |
| Discharged visits | 66,081 | 81% | 67,659 | 82% |
| Distinct patients for discharged visits | 49,366 | 50,533 | ||
| Of discharged visits | ||||
| Any revisit (3 days) | 1,821 | 2.8% | 1,873 | 2.8% |
| Revisit with admission (3 day) | 557 | 0.8% | 552 | 0.8% |
| Revisit with ICU admission (3 days) | 32 | 0.05% | 22 | 0.03% |
| Revisit with admission (1 day) | 166 | 0.3% | 180 | 0.3% |
| Revisit with admission (7 days) | 860 | 1.4% | 833 | 1.3% |
| Received albuterol | 6,025 | 9% | 6,371 | 9% |
| Received one or more boluses | 2,317 | 4% | 2,127 | 3% |
| Last HR ≤ 30 minutes before discharge | 12,278 | 19% | 17,394 | 26% |
Most common chief complaints presented, visits may have more than one chief complaint
The median number of HRs recorded for discharged visits was 2 (interquartile range 1, 3), with 33% of discharged visits having only one recorded HR.
HR-for-age percentiles
The last-recorded HR-for-age percentiles (Supplemental File 1) demonstrated good fit in the validation subset. Among five age groups the proportions of HRs above the 95th percentile ranged from 4.8% to 5.5% and the proportions above the 99th percentile ranged from 0.7% to 1.4%.
Primary Analysis
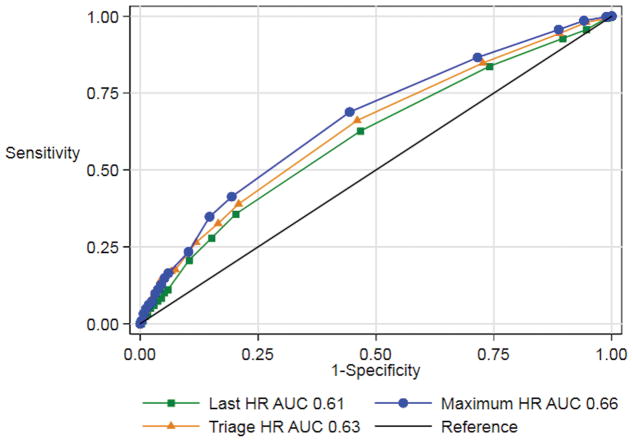
The area under the curve (AUC) for predicting revisit with admission using last-recorded HR was 0.61 (95% confidence interval [CI]: 0.58, 0.63) (Figure 2). Because no promising cutpoints were identified on the ROC curves, only cutpoints for the highest 5% and 1% of HR-for-age were evaluated further. These cutpoints corresponded to the 91st and 97th percentiles of last-recorded HR among all ED patients, because higher last-recorded HRs were more prevalent among visits ending in admission. These cutpoints had low sensitivity and positive predictive value (PPV), with likelihood ratios (positive) of 2.0 and 2.4, respectively, and likelihood ratios (negative) of 0.95 and 0.99 (Table 2). Between 50 and 62 children with high last-recorded HRs would need to be evaluated to potentially prevent one revisit with admission.
Figure 2.
Receiver operating characteristic curves for discharge, triage, and maximum HR-for-age percentiles identifying discharged visits with a return admission within 72 hours
Table 2.
Test characteristics for identifying discharged visits followed by revisit and admission within 3 days using cutpoints selecting visits with the highest 5% and 1% of last-recorded HRs for age
| Highest 5% | Highest 1% | |||
|---|---|---|---|---|
| Point estimates | 95% Confidence intervals | Point estimates | 95% Confidence intervals | |
| % Test + | 5.2% | 5.0%, 5.3% | 1.0% | 1.0%, 1.1% |
| Sensitivity | 10.1% | 7.8%, 13.0% | 2.5% | 1.4%, 4.2% |
| Specificity | 94.9% | 94.7%, 95.1% | 99.0% | 98.9%, 99.0% |
| Positive predictive value | 1.6% | 1.2%, 2.1% | 2.0% | 1.1%, 3.3% |
| Negative predictive value | 99.2% | 99.2%, 99.3% | 99.2% | 99.1%, 99.3% |
| Likelihood ratio (+) | 2.0 | 1.5, 2.6 | 2.4 | 1.4, 4.2 |
| Likelihood ratio (−) | 0.95 | 0.7, 1.3 | 0.99 | 0.6, 1.7 |
| Number needed to evaluate | 62 | 48, 82 | 50 | 30, 91 |
Sensitivity Analyses
Maximum HR had a higher AUC than last-recorded HR (0.66, 95% CI 0.64, 0.68). The AUC for triage HR (0.63, 95% CI 0.61, 0.66) and the sensitivity, PPV, and positive likelihood ratios all had overlapping confidence intervals with those for last-recorded HR (Table 3).
Table 3.
Selected test characteristics for sensitivity analyses of alternate HR cutpoints, restricted inclusion criteria, and alternate outcomes.
| Analysis | Highest 5% | Highest 1% | ||||
|---|---|---|---|---|---|---|
| Sensitivity | PPVa | LR (+)b | Sensitivity | PPVa | LR (+)b | |
| Primary | 10.1% | 1.6% | 2.0 | 2.5% | 2.0% | 2.5 |
| Alternate HR types | ||||||
| Triage HR | 15.9% | 2.2% | 2.7 | 4.3% | 2.7% | 3.4 |
| Maximum HR | 14.9% | 2.3% | 2.9 | 4.9% | 3.2% | 3.9 |
| Temperature-adjusted HR | ||||||
| Adjusted last-recorded HR | 9.2% | 1.5% | 1.8 | 1.6% | 1.3% | 1.6 |
| Adjusted triage HR | 13.5% | 1.9% | 2.5 | 3.4% | 2.8% | 3.4 |
| Restricted inclusion criteria | ||||||
| No albuterol | 4.9% | 1.2% | 1.6 | 1.1% | 1.9% | 2.6 |
| Bolus | 10.5% | 4.3% | 2.4 | - | 0 | - |
| Last HR ≤ 30 minutes before discharge | 10.6% | 2.1% | 2.0 | 2.2% | 2.7% | 2.6 |
| Alternate outcomes | ||||||
| Any return (3 days) | 7.1% | 3.8% | 1.4 | 1.5% | 4.0% | 1.4 |
| Return with ICU admission (3 days) | 13.6% | 0.1% | 2.7 | - | 0 | - |
| Return admission (1 day) | 10.6% | 0.5% | 2.0 | 1.7% | 0.4% | 2.1 |
| Return admission (7 days) | 11.1% | 2.8% | 2.2 | 3.2% | 4.0% | 3.2 |
PPV: positive predictive value.
LR (+): likelihood ratio positive.
No other modifications, including using temperature-adjusted HR, restricting the type of analyzed visits, and using alternate outcomes, resulted in improved test characteristics. The risk of revisit with admission was higher for visits in which albuterol was given (odds ratio [OR] 2.2, 95% CI 1.7, 2.7) compared to when it was not given, and higher for visits in which intravenous boluses were given (OR 2.3, 95% CI 1.7, 3.2) compared to visits in which no bolus was given. Test characteristics in these restricted visit groups were not improved compared to the primary analysis including all index visits (Table 3).
Visits in which tachycardia resolved were more likely to end in discharge (OR 2.4, 95% CI 2.3, 2.6) compared to visits in which tachycardia was present and was not resolved at the last-recorded HR. Among visits that ended in discharge, resolution of tachycardia was not associated with a significant change in risk of revisit with admission (OR 1.4, 95% CI 0.97, 1.9) and was associated with an increased, rather than a decreased, risk of any revisit (OR 1.3, 95% CI 1.1, 1.6).
Conclusions
Multiple prior studies in children and adults have shown associations between abnormal vital signs and more serious illness or poorer outcomes,15–24 and clinicians already consider HR in decisions regarding therapy and admission. Our study design did not directly measure the association between HR and outcomes because, in many cases, HR would have already been incorporated into therapy decisions and the decision to admit or discharge. Our study evaluated the potential additional benefit of a focused look at the last-recorded HR to avoid poor outcomes after discharge. While we found a weak association between the last-recorded HR and subsequent ED revisit with admission, a detailed analysis and sensitivity analyses did not identify HR cutpoints that discriminated well between children at high and low risk of revisit with admission. For example, if re-evaluation were triggered for a HR in the highest 5% of all discharged ED patients, 62 patients would require reevaluation to potentially prevent one revisit with admission, and the vast majority (90%) of revisits with admission would be preceded by a discharge HR that would not have triggered any re-evaluation. This estimation presumes that re-evaluation would be able to prevent subsequent revisit with admission; however, it is likely that some of these revisits with admission were not preventable, and the true number needed to evaluate would actually be higher.
Clinicians are often advised to follow changes in vital signs, or of scores derived from vital signs.6,25 However, evidence for whether and how changes in vital signs or vital sign scores are associated with outcomes is lacking. Among discharged visits with an elevated HR at any time during the ED visit, resolution of tachycardia was associated with an increase in risk of revisit, rather than a decrease in risk. One possible explanation for this unexpected finding is ascertainment bias; the decision to wait for resolution of tachycardia, or to repeat measurements of heart rate, may reflect increased concern on the part of the clinician that is associated with more serious illness. Additionally, the documentation of a single HR in the typical range just prior to discharge may sometimes reflect variability in HR or a transient decrease in HR rather than a true resolution of the process causing tachycardia, and may therefore be inappropriately reassuring in certain patients. The finding that resolution of tachycardia is associated with increased risk of revisit counters the clinical practice of observing and watching for normalization of vital signs at the end of a visit to determine suitability for discharge. We also found that maximum HR had the largest AUC for predicting revisit with admission. If these findings are confirmed in other ED populations, it may be advisable for clinicians to consider maximum HR more heavily in their decision-making than a final HR. This finding is supported by research in adult patients admitted to the hospital, for whom vital sign abnormalities in the 24 hours preceding discharge, but not necessarily occurring just prior to discharge, were associated with an increased likelihood of death or readmission within 30 days.26
Test characteristics were not improved when we adjusted HR for body temperature. Although many children with a very high fever do not have a dangerous illness, the lack of improved test characteristics when adjusting for body temperature may reflect some association between increased body temperature and more severe illness.
Strengths of this study included the large population and several novel sensitivity analyses that, to our knowledge, have not been explored in prior research. We developed validated HR-for-age percentiles specific to the ED setting, which may be of use to researchers or those developing clinical tools. We used these percentiles and ROC curves to identify cutpoints with the best discrimination, rather than determining HR cutpoints a priori.
Ensuring that clinicians are aware of tachycardia prior to discharge is an intervention with strong face validity. Our findings and those of Wilson et al.9 do not support the use of the last-recorded HR as a trigger to prevent or delay discharge, but our work is not definitive. Given the uncertain benefit, it is especially important to consider the risks of HR-based triggers. The biggest risk may be that clinicians could be inappropriately reassured by a non-elevated HR. The negative likelihood ratios of last-recorded HR-for-age were extremely weakly informative (0.95–0.99). Therefore, when clinicians have other reasons to be concerned about a patient, a non-elevated HR should not be used in isolation as justification for being less concerned. The diversion of time and resources from more high-yield activities and the risks from unnecessary testing or admission in tachycardic patients are two other important potential risks that should be balanced against uncertain benefit.
The most important limitation of this study is our inability to directly measure the outcome of interest: harm due to inadequate care or inappropriate discharge at the index visit. We used ED revisit with admission as a proxy for this outcome, but the relationship between revisit with admission and both harm and appropriateness of care is unclear.27–30 Despite their limitations, revisits, with or without admission, are often used as quality indicators by hospitals and other groups. Therefore, in the absence of other options that are measurable on a large scale, we believe that revisit with admission is an appropriate outcome for an initial evaluation of the clinical value of last-recorded HR-based reevaluation strategies. Revisit with admission likely overestimates the frequency of harm due to inadequate care; therefore, its use as an outcome measure would likely result in falsely decreased sensitivity and falsely elevated PPV. Because the sensitivity and PPV in this study were so low, it seems unlikely that desirable test characteristics would be achieved even with a relatively large increase in sensitivity and a small decrease in PPV.
The study was retrospective, and the frequency and timing of HR measurement and recording were likely impacted by disease severity, patient characteristics, and provider characteristics. Some elevated HR observations would not have been included in our evaluation because they caused the clinical team to admit the child or recheck the HR, which would bias toward the null. The similar results of our evaluation limited to HRs done 30 minutes or less before discharge provide some reassurance that confounding by factors that influence the timing of the discharge HR did not fundamentally alter the results. HR measurements were done for clinical rather than research purposes and were not measured using standard protocols. This increases the likelihood of measurement error, but is representative of how HR measurements are performed when HR-based discharge safety programs are implemented.
Evaluation of a single pediatric ED is another limitation. Our findings were similar to those in another recent retrospective study of two pediatric EDs and four pediatric urgent care centers within a health care system.9 However, we are not aware of any studies of discharge HR and outcomes in general EDs or urgent care centers. In general EDs, particularly those with a low volume of pediatric patients, it is possible that HR-based triggers for pediatric patients may be more beneficial.31 Additionally, we were only able to identify revisits to the single studied ED; some children who revisited a different ED or who accessed outpatient care may have been misclassified as non-revisits. As described by Wilson et al., we do not believe that any misclassification is likely to be differential between children with and without elevated HR.9 We were also unable to assess death at home, which we would expect to be exceedingly rare in a pediatric population.
The most important area for future research may be the development of validated outcome measures that more directly assess harm and appropriateness of initial care and discharge. The use of the last-recorded HR in general EDs and the incorporation of HR and other clinical characteristics into a multi-component clinical decision rule also require further evaluation.
In summary, most discharged patients with an elevated heart rate in a pediatric ED do not subsequently require admission, and most patients who require admission after ED discharge did not have an elevated HR at the end of the initial visit. Our findings support the need for careful consideration of the impact of HR-based discharge safety tools before implementation. Clinicians should also be cautious when considering resolution of tachycardia in discharge decisions.
Supplementary Material
Selected percentiles for discharge, triage, and maximum HR
Footnotes
Conflicts of interest and source of funding: The study was unfunded. The authors have no potential conflicts of interest.
References
- 1.Roohan PJ, Schettine A, Gesten F, et al. New York State Report on Sepsis Care Improvement Initiative: Hospital Quality Performance 2015. New York, NY: Office of the Medical Director Office of Quality and Patient Safety; 2017. [Google Scholar]
- 2.Domagala SE. Discharge Vital Signs: An Enhancement to ED Quality and Patient Outcomes. Journal of Emergency Nursing. 2009;35(2):138–140. doi: 10.1016/j.jen.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Warren DG, Jarvis A, LeBlanc L, Gravel J the CTAS National Working Group. Revisions to the Canadian Triage and Acuity Scale Paediatric Guidelines (PaedCTAS) Canadian Journal of Emergency Medicine. 2008;10(3):224–232. [PubMed] [Google Scholar]
- 4.Gilboy N, Tanabe P, Travers D, Rosenau AM. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 5.Goldstein B, Giroir B, Randolph A International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. [DOI] [PubMed] [Google Scholar]
- 6.Parshuram CS, Hutchison J, Middaugh K. Development and initial validation of the Bedside Paediatric Early Warning System score. Crit Care. 2009;13(4):R135. doi: 10.1186/cc7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akre M, Finkelstein M, Erickson M, Liu M, Vanderbilt L, Billman G. Sensitivity of the pediatric early warning score to identify patient deterioration. Pediatrics. 2010;125(4):e763–769. doi: 10.1542/peds.2009-0338. [DOI] [PubMed] [Google Scholar]
- 8.Pediatric Advanced Life Support. Provider Manual. Dallas, TX: American Heart Association; 2011. [Google Scholar]
- 9.Wilson PM, Florin TA, Huang G, Fenchel M, Mittiga MR. Is Tachycardia at Discharge From the Pediatric Emergency Department a Cause for Concern? A Nonconcurrent Cohort Study. Annals of Emergency Medicine. 2017 Feb; doi: 10.1016/j.annemergmed.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Rigby R, Stasinopolous D. Generalized additive models for location, scale and shape (with discussion) Journal of the Royal Statistical Society, Series C. 2005;54:507–554. [Google Scholar]
- 11.Borghi E, de Onis M, Garza C, et al. Construction of the World Health Organization child growth standards: selection of methods for attained growth curves. Stat Med. 2006;25(2):247–265. doi: 10.1002/sim.2227. [DOI] [PubMed] [Google Scholar]
- 12.Daymont C, Bonafide CP, Brady, Patrick W. Heart rates in hospitalized children by age and body temperature. Pediatrics. doi: 10.1542/peds.2014-3738. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson M, Harnden A, Perera R, et al. Deriving temperature and age appropriate heart rate centiles for children with acute infections. Arch Dis Child. 2009;94(5):361–365. doi: 10.1136/adc.2008.145011. [DOI] [PubMed] [Google Scholar]
- 14.Davies P, Maconochie I. The relationship between body temperature, heart rate and respiratory rate in children. Emerg Med J. 2009;26(9):641–643. doi: 10.1136/emj.2008.061598. [DOI] [PubMed] [Google Scholar]
- 15.Cruz AT, Perry AM, Williams EA, Graf JM, Wuestner ER, Patel B. Implementation of goal-directed therapy for children with suspected sepsis in the emergency department. Pediatrics. 2011;127(3):e758–766. doi: 10.1542/peds.2010-2895. [DOI] [PubMed] [Google Scholar]
- 16.Barfod C, Lauritzen MMP, Danker JK, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department - a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2012;20:28. doi: 10.1186/1757-7241-20-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berger T, Green J, Horeczko T, et al. Shock index and early recognition of sepsis in the emergency department: pilot study. West J Emerg Med. 2013;14(2):168–174. doi: 10.5811/westjem.2012.8.11546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Considine J, Thomas S, Potter R. Predictors of critical care admission in emergency department patients triaged as low to moderate urgency. J Adv Nurs. 2009;65(4):818–827. doi: 10.1111/j.1365-2648.2008.04938.x. [DOI] [PubMed] [Google Scholar]
- 19.Hong W, Earnest A, Sultana P, Koh Z, Shahidah N, Ong MEH. How accurate are vital signs in predicting clinical outcomes in critically ill emergency department patients. Eur J Emerg Med. 2013;20(1):27–32. doi: 10.1097/MEJ.0b013e32834fdcf3. [DOI] [PubMed] [Google Scholar]
- 20.Horeczko T, Wintemute GJ. Asthma vital signs at triage: home or admission (ASTHmA) Pediatr Emerg Care. 2013;29(2):175–182. doi: 10.1097/PEC.0b013e3182809a45. [DOI] [PubMed] [Google Scholar]
- 21.Ley EJ, Singer MB, Clond MA, et al. Admission heart rate is a predictor of mortality. J Trauma Acute Care Surg. 2012;72(4):943–947. doi: 10.1097/TA.0b013e3182465527. [DOI] [PubMed] [Google Scholar]
- 22.Olsson T, Terent A, Lind L. Rapid Emergency Medicine score: a new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. J Intern Med. 2004;255(5):579–587. doi: 10.1111/j.1365-2796.2004.01321.x. [DOI] [PubMed] [Google Scholar]
- 23.Subbe CP, Slater A, Menon D, Gemmell L. Validation of physiological scoring systems in the accident and emergency department. Emerg Med J. 2006;23(11):841–845. doi: 10.1136/emj.2006.035816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu J-H, Weng Y-M, Chen K-F, Chen S-Y, Lin C-C. Triage vital signs predict in-hospital mortality among emergency department patients with acute poisoning: a case control study. BMC Health Serv Res. 2012;12:262–269. doi: 10.1186/1472-6963-12-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rothman MJ, Tepas JJ, Nowalk AJ, et al. Development and Validation of a Continuously Age-Adjusted Measure of Patient Condition for Hospitalized Children Using the Electronic Medical Record. J Biomed Inform. 2017 Jan; doi: 10.1016/j.jbi.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen OK, Makam AN, Clark C, et al. Vital Signs Are Still Vital: Instability on Discharge and the Risk of Post-Discharge Adverse Outcomes. J Gen Intern Med. 2017;32(1):42–48. doi: 10.1007/s11606-016-3826-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sabbatini AK, Kocher KE, Basu A, Hsia RY. In-Hospital Outcomes and Costs Among Patients Hospitalized During a Return Visit to the Emergency Department. JAMA. 2016;315(7):663–671. doi: 10.1001/jama.2016.0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pham JC, Kirsch TD, Hill PM, DeRuggerio K, Hoffmann B. Seventy-two-hour Returns May Not be a Good Indicator of Safety in the Emergency Department: A National Study: 72-HOUR RETURNS ARE NOT A GOOD ED SAFETY INDICATOR. Academic Emergency Medicine. 2011;18(4):390–397. doi: 10.1111/j.1553-2712.2011.01042.x. [DOI] [PubMed] [Google Scholar]
- 29.Abualenain J, Frohna WJ, Smith M, et al. The Prevalence of Quality Issues and Adverse Outcomes among 72-Hour Return Admissions in the Emergency Department. The Journal of Emergency Medicine. 2013;45(2):281–288. doi: 10.1016/j.jemermed.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 30.Hsia RY, Asch SM, Weiss RE, et al. Is emergency department crowding associated with increased “bounceback” admissions? Med Care. 2013;51(11):1008–1014. doi: 10.1097/MLR.0b013e3182a98310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bourgeois FT, Shannon MW. Emergency care for children in pediatric and general emergency departments. Pediatr Emerg Care. 2007;23(2):94–102. doi: 10.1097/PEC.0b013e3180302c22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Selected percentiles for discharge, triage, and maximum HR