Abstract
Background
Offering consumers the opportunity to swap to lower-salt foods while shopping has potential to reduce salt intake. Offering a wider range of alternatives which are much lower in salt could increase the magnitude of salt reduction gained but may interfere with consumers’ engagement and willingness to accept swaps.
Objectives
To compare the salt reduction from offering swaps to a similar product but with minimally less salt to offering swaps with a substantial salt reduction including a range of alternative foods.
Methods
In an experimental, randomised trial conducted in a virtual online supermarket, participants with high blood pressure were asked to buy 12 items of food. One group was offered similar alternatives with 5–20% less salt (LS swaps); and the other group was offered these LS swaps and alternatives with >20% less salt (MLS swaps). The primary outcome was the change in salt density of the shopping basket (g/100g) from initially selected items, to the final items chosen.
Results
947 participants completed the task and were included in the analysis. There was a significant reduction in salt content of the final selected shopping basket in both groups; with a significantly greater reduction in the group offered LS + MLS swaps (−0.09g/100g, 95% C.I. −0.10, −0.07; p < 0.001). The proportion of swaps accepted was the same in both groups and the mean salt reduction per swap accepted in the group offered LS + MLS swaps was more than double that of the group offered LS swaps alone. 30% of MLS swaps accepted were from a different food subcategory.
Conclusions
Offering alternative products with a large reduction in salt, including potentially dissimilar products, does not decrease acceptability and leads to significantly greater reductions in the salt content of the shopping basket.
Trial registration
ISRCTN, ISRCTN91306993. Registered 5th February 2018 – retrospectively registered. https://www.isrctn.com/ISRCTN91306993.
Keywords: Salt reduction, Swaps, Grocery shopping, Supermarket, Food purchasing behaviour change
1. Introduction
High dietary salt intake is associated with high blood pressure (hypertension) and increased risk of cardiovascular disease and chronic kidney disease (Arcand et al., 2017; Strazzullo, D’Elia, Kandala, & Cappuccio, 2009). Salt reduction initiatives, both population and individual level, form an integral part of national strategies to combat hypertension, currently ranked as the 2nd biggest risk factor for premature mortality in the United Kingdom (UK) behind smoking (GBD 2015 Risk Factors collaborators, 2016; Public Health England, 2014). Guidelines for the prevention and management of hypertension, both in the UK and internationally, recommend salt reduction (NICE, 2011; WHO, 2016). In high-income countries such as the UK, the majority of salt in the diet comes from processed foods rather than salt added at the table or in cooking (Anderson et al., 2010; Sanchez-Castillo, Warrender, Whitehead, & James, 1987). As well as prevailing on manufacturers to reduce the salt content of foods, we need to encourage individuals to purchase foods with lower salt content. For many high-salt foods there are similar, lower-salt alternatives and this offers the potential to encourage consumers to swap their usual products for lower-salt foods.
Several studies have evaluated swap interventions to encourage healthier food purchases, either alone or as part of a multicomponent intervention in real or virtual supermarket settings (Eyles et al., 2017; Forwood, Ahern, Marteau, & Jebb, 2015; Huang et al., 2006; Ni Mhurchu et al., 2010; Winett et al., 1991a, 1991b), including one study that showed significant reductions in salt using a smartphone app to suggest lower-salt alternatives (Eyles et al., 2017). However, there is little evidence available on how the nature of the food swaps offered, particularly the magnitude of change and the similarity of the alternative choices, influences acceptability and hence the overall intervention effect. In previous swap studies, where reported, the alternatives offered were either within the same brand (Ni Mhurchu et al., 2010) or the same narrow product category (Eyles et al., 2017; Forwood et al., 2015). This approach constrains the variety of swaps offered and the potential reduction in salt as there is often less variation in salt content among very similar products than across a wider range of products; for example, between different types of cheddar cheese compared to across all types of cheese.
We hypothesised that offering alternatives with a greater reduction in salt (>20% less salt), sometimes involving a slightly different type of food (“out-of-category”) could have a greater impact on the total amount of salt purchased than confining swap options to very similar (“within-category”) products.
However, the success of this strategy depends on the acceptability of the swaps offered. Rational choice theory, and the economic concept of ‘utility’, would suggest that offering lower-salt alternatives that are most similar to the original product would be more acceptable to consumers (Dominick Salvatore, 2008). Offering an out-of-category product could potentially reduce utility, prompting the purchaser to offset the loss of utility against the expected health gain, potentially reducing the acceptability of such swaps and limiting salt reduction. Furthermore, consumers often use heuristics to simplify decision-making, relying on experience, cues and ‘rules of thumb’ to make judgement decisions, rather than more systematic and reflective processes which require more cognitive effort (Chaiken, Liberman, & Eagly, 1989). Offering consumers an out-of-category swap may invoke this more effortful decision-making process (Mandrik et al., 1996) causing consumers to disengage with the intervention thus limiting its impact. Accordingly, there is a need to better understand the acceptability of offering consumers substantially lower salt alternatives within a wider range of products.
In this study we aimed to inform the development of a ‘swap-based’ intervention. We used a virtual online supermarket to test the impact on the salt content of the shopping basket, of offering very similar products with minimally less salt compared to offering much lower salt alternatives, including ‘out of category’ products and to investigate specific participant characteristics associated with the acceptance of swaps.
2. Methods
2.1. Study design
This 2-arm randomised experiment used a virtual online supermarket which emulates a real online supermarket (www.woodssupermarket.co.uk). It contains a food database downloaded from a UK grocery retailer (Tesco.com API. February 2012) with ∼11,000 products. Products are categorised into food categories and subcategories similar to real-world online supermarkets, for example the category ‘dressings’ contains subcategories ‘salad dressing’ and ‘mayonnaise & salad cream’ (see Supplementary Table 1 for full list of categories and subcategories). The database includes detailed nutrient information, downloaded from the retailer and supplemented with nutrient data provided by Kantar WorldPanel and the MRC Human Nutrition Research food and nutrient database. Salt content of foods was based on the sodium content x 2.5g. The website looks and functions like a real online supermarket website except that participants do not pay for the groceries and no goods are delivered. The development and testing of this online supermarket platform are detailed elsewhere (Forwood et al., 2015).
The study was conducted online between June and September 2017.
2.2. Participant and recruitment
Participants were recruited via two channels: a database of volunteers with diabetes, a respiratory condition or heart disease, from across England but predominantly from Greater Manchester (www.researchforthefuture.org); and a UK-wide panel from a market research agency (www.researchnow.co.uk). Participants were eligible if they were aged 18 or over with self-reported high blood pressure, spoke English, were responsible for at least some of their household grocery shopping and regularly shopped in a supermarket spending at least £25 per shop. People following a medically prescribed diet or restricted diet such as a vegetarian, vegan or gluten free diet were not eligible. Individuals were invited to participate in the study via email and directed to an online eligibility screening questionnaire and consent form.
2.3. Randomisation and blinding
Eligible participants who consented were randomised to one of the two intervention arms and automatically directed to the online supermarket website. Randomisation was on a 1:1 basis, in blocks of two, using computerised random number generation. Intervention allocation was concealed from researchers until after completion of the study and data collection. It was not possible to blind participants to the intervention.
2.4. Procedure
The experiment was delivered online, immediately following participant randomisation. Outcome data were collected automatically through the online supermarket website and exported for analysis. The website introduced the shopping task, provided instructions and a pre-determined shopping list of 12 items for the task. The shopping list focused on foods which contribute substantially to household salt purchased (NiMhurchu et al., 2011), foods which individuals with high blood pressure would typically be advised to reduce consumption of (BHF, 2013), and foods with potential for swaps to a reduced salt alternative. Participants completed the task once.
The list included:
-
•
Bacon or sausages for a cooked breakfast
-
•
Cold meat (e.g. for a sandwich or to go with a salad)
-
•
Bread or rolls for lunch
-
•
Cheese or cheese spread for a sandwich
-
•
A pizza
-
•
Soup for a light meal
-
•
A ′ready meal' e.g. a prepared meal
-
•
A savoury snack e.g. a pack of crisps or nuts
-
•
Butter or spread (to use on toast or sandwiches)
-
•
Dressing or mayonnaise for a salad
-
•
A box or bag of breakfast cereal
-
•
A packet of biscuits
Participants were asked to ‘buy’ all the items on the list, but not to buy additional items. They were not limited to a set budget and were reminded that this was not a real supermarket and they would not be asked to spend their own money. For full instructions see Supplementary Fig. 1.
On completing the shopping task participants were asked to complete a short survey including questions on participant demographics; online shopping experience; blood pressure history; efforts to reduce salt; and their shopping habits (Supplementary Table 2).
2.5. Experimental conditions
Participants selected items from the list, added them to their online shopping basket and, where a lower-salt alternative existed, they were offered a swap. The percentage reduction in salt content and the price were displayed for each alternative offered.
In the lower salt intervention (LS), alternative products offered were: from the same food category and subcategory; contained between 5 and 20% less salt (g/100g) than the originally selected product and the product weight and price was constrained to be between half and double the pack weight and price originally chosen. Only one alternative product was displayed at a time, chosen at random from all available alternative products matching the criteria. If there was more than one alternative product, participants had the option to be shown another alternative, until they had exhausted all alternatives. If no alternatives meeting the criteria were available, no swap was offered. The product initially selected served as the control choice for each purchased item for each participant.
In the much lower salt intervention (LS + MLS) participants were offered one alternative fulfilling the LS criteria (described above) and also one alternative product which was from the same food category, but not limited to the same subcategory, with at least 21% less salt than the originally selected product, and with the same constraints on price and product weight as for LS swaps only. An example swap (and corresponding salt content) would be: for an initial choice of ‘Brand A’ Mature Cheddar 400G (1.9g/100g), a LS alternative of ‘Brand B’ Vintage Cheddar Cheese 350g (1.75g/100g) or MLS alternative of ‘Brand C’ Double Gloucester 250g (1.25g/100g).
2.6. Outcome measures
Primary and secondary outcomes: The primary outcome was the mean difference in salt density (g/100g) between the initial basket of items (i.e. the products chosen before any swaps were offered) and the final selected basket of items (those in the basket at ‘checkout’), weighted by the total weight (g) of food in the basket. The difference was also calculated as salt in g/MJ. Secondary outcomes were the number of items for which swaps were offered, and the number accepted; the proportion of offered swaps which were accepted per participant; the average salt reduction per accepted swap; and proportion of accepted swaps which were not within the same subcategory (for the MLS intervention only).
Sugar content, saturated fat content and cost of the initial and final shopping baskets (weighted for total purchased energy) were also calculated to measure any spill-over effects.
Other outcomes included: participant shopping behaviours including use of nutrition labels and factors influencing their shopping decisions; online shopping experience; history of advice on salt reduction; and intervention acceptability.
2.7. Sample size
Nine hundred participants (450 per group) were required to detect an absolute treatment difference of 0.04 g/MJ (change of ∼5%) of salt and a common SD of 0.2 g/MJ to achieve 80% power at 5% significance level; based on the mean salt content of a shopping basket from a previous shopping intervention (mean 0.70 g/MJ (SD) 0.22) (Ni Mhurchu et al., 2010).
2.8. Analysis
Statistical analysis was conducted using STATA version 14.1 (StataCorp. Stata Statisti, 2015) and conducted according to the pre-specified protocol. Difference in the primary outcome was estimated using linear regression analysis with significance evaluated at p-value<0.05. Assumptions of linear regression were tested and met. Among secondary outcomes, Poisson regression was used to estimate differences in the number of swaps offered and accepted, reporting the Incidence Rate Ratio (IRR); and linear regression to estimate the difference in average proportion of swaps accepted per participant and the average salt reduction per accepted swap.
We present both the unadjusted effect and after taking into account hypothesised explanatory covariates including: participants' rating of price, health, habits, and family food preferences as important factors influencing grocery shopping decisions; and baseline salt content of the shopping basket. Exploratory observational analyses were conducted to investigate associations between participants’ use of nutrition labels, history of dietary salt advice, and the importance of price and health in their purchasing decisions. Observational analyses were conducted using linear regression adjusted for intervention group only.
3. Results
3.1. Participants
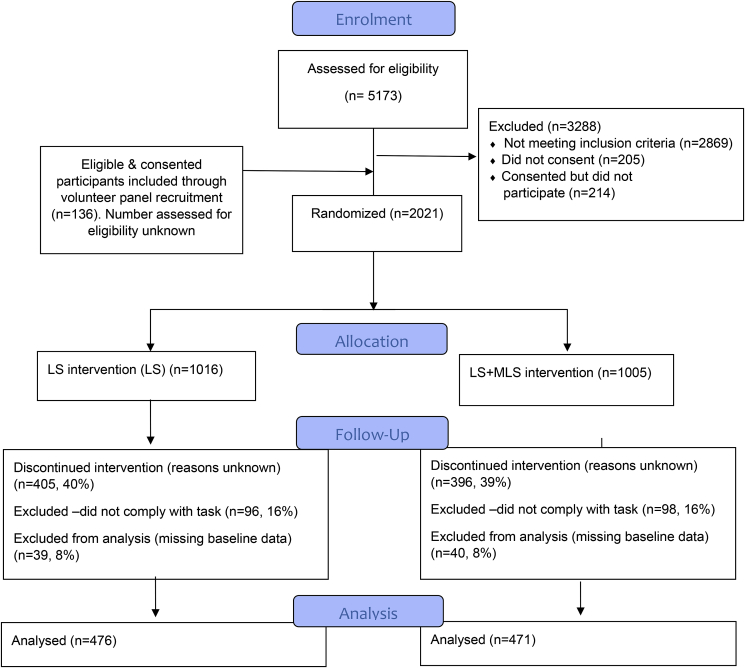
Of the 5309 participants screened for eligibility, 2021 were randomised. Of these, 79 participants (4%) did not provide baseline data, 801 (40%) did not complete the shopping task and a further 194 (9.5%) did not adhere to the task instructions (defined as selecting fewer than three items from the list provided) and were excluded from the analysis. Numbers who were excluded were similar across intervention groups (see Consort diagram Fig. 1).
Fig. 1.
Consort diagram.
947 participants completed the task and were included in the analysis. Most participants (96%) had used online shopping and 44% had used online grocery shopping in the past year. Family likes/dislikes (84%), price (74%) and health (44%) were reported as the strongest drivers of food choices. Baseline characteristics are shown in Table 1.
Table 1.
Participant characteristics.
| Characteristics |
LS group N (%) |
LS + MLS group N (%) |
Total N (%) |
|---|---|---|---|
| Total | 476 | 471 | 947 |
| Age | |||
| 18-24 | 2 (1) | 3 (1) | 5 (1) |
| 25-34 | 19 (4) | 9 (2) | 28 (3) |
| 35-44 | 26 (5) | 25 (5) | 51 (5) |
| 45-54 | 73 (15) | 88 (19) | 161 (17) |
| 55-64 | 169 (36) | 150 (32) | 319 (34) |
| 65 or older | 187 (39) | 196 (42) | 383 (40) |
| Sex (n,%) | |||
| Male | 274 (58) | 276 (59) | 550 (58) |
| Female | 202 (42) | 195 (41) | 397 (42) |
| Household income (total household income before tax) | |||
| Below £15, 500 | 84 (18) | 88 (19) | 172 (18) |
| Between £15, 600 and £25,000 | 106 (22) | 118 (25) | 224 (24) |
| Between £26,000 and £35,000 | 102 (21) | 98 (21) | 200 (21) |
| Between £36,000 and £50,000 | 106 (22) | 81 (17) | 187 (20) |
| £51,000 or above | 78 (16) | 86 (18) | 164 (17) |
| Highest educational level | |||
| None | 24 (5) | 35 (7) | 59 (6) |
| Up to 4 GCSE's | 70 (15) | 79 (17) | 149 (16) |
| 5 or more GCSE's or 1 A-level | 66 (14) | 66 (14) | 132 (14) |
| 2 or more A-levels | 94 (20) | 95 (20) | 189 (20) |
| Bachelor's degree | 144 (30) | 129 (27) | 273 (29) |
| Post-Graduate degree or qualification | 78 (16) | 67 (14) | 145 (15) |
| Online shopping experience (groceries) | |||
| Never or not in the last year | 274 (58) | 258 (55) | 532 (56) |
| 1–3 times in the last year | 69 (15) | 74 (16) | 143 (15) |
| 4–11 times in the last year | 66 (14) | 67 (14) | 133 (14) |
| 1–3 per month | 43 (9) | 44 (9) | 87 (9) |
| Once per week or more often | 24 (5) | 28 (6) | 52 (5) |
| Online shopping experience (non-food items) | |||
| Never or not in the last year | 15 (3) | 25 (5) | 40 (4) |
| 1–3 times in the last year | 73 (15) | 71 (15) | 144 (15) |
| 4–11 times in the last year | 221 (46) | 194 (41) | 415 (44) |
| 1–3 per month | 138 (29) | 133 (28) | 271 (29) |
| Once per week or more often | 29 (6) | 48 (10) | 77 (8) |
| Participant has a household member who has been diagnosed with high blood pressure | 124 (30) | 130 (31) | 254 (31) |
| Participant has ever been advised by their doctor or health professional to cut down their salt intake | 190 (40) | 195 (41) | 385 (41) |
| Participant has a household member who has been advised to cut down their salt intake | 57 (14) | 76 (18) | 133 (16) |
| Participant ever tried to cut down their salt intake | 322 (68) | 327 (69) | 649 (69) |
| Participant has a household member who has ever tried to cut down their salt intake | 167 (42) | 177 (43) | 344 (42) |
| How often participants look at nutrition labels for salt | |||
| At least sometimes | 329 (69) | 298 (63) | 627 (66) |
| Never or rarely | 147 (31) | 173 (37) | 320 (34) |
| Drivers of shopping choices (n, % Yes) | |||
| Family likes/dislikes | 392 (85) | 386 (84) | 778 (84) |
| Price | 338 (73) | 350 (76) | 688 (74) |
| Health | 206 (44) | 185 (40) | 391 (42) |
| Special/offers | 145 (30) | 175 (38) | 320 (35) |
| Habits | 70 (15) | 54 (11) | 124 (13) |
| Convenience | 51 (11) | 62 (13) | 113 (12) |
| Appearance (of products) | 54 (12) | 54 (12) | 108 (12) |
| Animal welfare | 50 (11) | 54 (12) | 104 (11) |
| Organic | 20 (4) | 9 (2) | 29 (3) |
| Special Diet | 17 (4) | 8 (2) | 25 (3) |
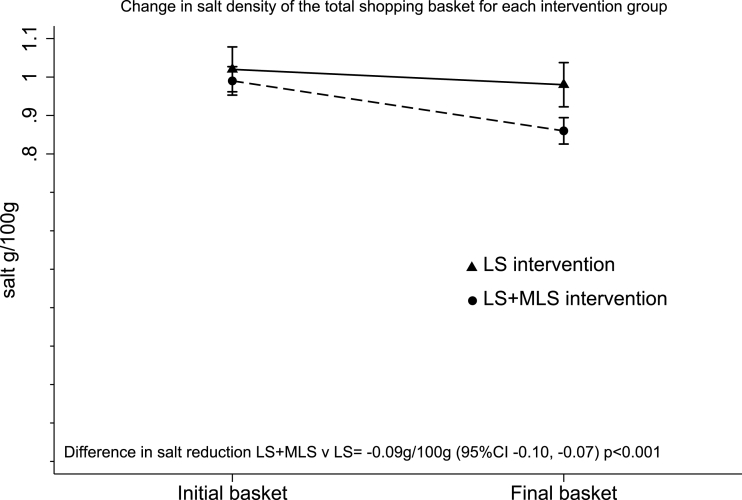
3.2. Primary outcome
The mean number of products selected in the final basket was 17 (SD 12), weighing 7.1 kg (SD 6.5) in total, with 54.4g salt (SD 48.5) and a salt density of 0.92g/100g (SD 0.53).
There was a significant reduction in the salt density of the final shopping basket in both intervention groups: LS -0.04g/100g (95% C.I. −0.04, −0.03 P < 0.001); MLS -0.13g/100g (95% C.I. −0.14, −0.11 p < 0.001); with a significantly greater reduction in the LS + MLS group compared to the LS group (−0.09g/100g 95% C.I. −0.10, −0.07 p < 0.001) (Fig. 2). This equates to a reduction in salt between the final and initial baskets of −4% for the LS group, −13% for the LS + MLS group and a between group difference of −9% (Table 2).
Fig. 2.
Change in salt density (g/100g) of the total shopping basket after swaps for each intervention group.
Table 2.
Change in salt density, total salt and total food weight between the initial and final shopping baskets for each intervention group (using independent t-tests) and the effect of the intervention groups on these changes.
| LS (n = 476) |
LS + MLS (n = 471) |
Difference between intervention groups LS + MLS v LS |
P = value | Difference between intervention groups LS + MLS v LS |
P = value | |
|---|---|---|---|---|---|---|
| Difference Final-initial (95% C.I) |
Difference Final-initial (95% C.I) |
Unadjusted (95% C.I) | adjusted b (95% C.I) | |||
| Total basket salt density (g/100g) (weighted) | −0.04 (−0.04, −0.03)a | −0.13 (−0.14, −0.11)a | −0.09 (−0.10, −0.07) | <0.001 | −0.09 (−0.11, −0.08) | <0.001 |
| % difference | −3.76 (-4.19, -3.32)a | −12.65 (-13.90, -11.39)a | −8.89 (-10.22, -7.56) | <0.001 | −8.94 (-10.27, -7.62) | <0.001 |
| Total basket salt content (g/MJ) (weighted) | −0.04 (−0.05, −0.04)a | −0.11 (−0.13, −.10)a | −0.07 (−0.09, −0.05) | <0.001 | −0.07 (−0.09, −0.06) | <0.001 |
| % difference | −4.45 (-5.17, -3.73)a | −12.25 (-13.58, -10.92)a | −7.80 (-9.30, -6.29) | <0.001 | −8.04 (-9.53, -6.55) | <0.001 |
| Total salt (g) | −2.93 (−3.43, −2.43)a | −7.97 (−8.78, −7.17)a | −5.04 (−5.99, −4.10) | <0.001 | −5.17 (−6.10, −4.23) | <0.001 |
| Total food weight (kg) | −0.07 (−0.10, −0.04)a | −0.21 (−0.27, −0.16)a | −0.15 (−0.20, −0.08) | <0.001 | −0.15 (−0.21, −0.09) | <0.001 |
Significant at p < 0.05.
Calculated using linear regression adjusted for: health considered important; price considered important; shopping habits considered important; family likes/dislikes considered important; and baseline shopping basket salt content.
There was also a significant reduction in both groups in salt content relative to the total energy of the final basket (g/MJ) with a significant between group difference of −0.07 g/MJ (95% C.I. −0.09, −0.06; p < 0.001), equivalent to an −8% between-group difference (Table 2).
3.3. Secondary outcomes
There was no difference between groups in the total number of items bought and no difference between groups in the salt density (g/100g) in the initial shopping basket. There was a significant reduction in both total salt content (g) and total product weight (kg) in the final shopping basket within each intervention group; and a significant between-group difference for both total salt (−5.2g 95% C.I. −6.1, −4.2 p < 0.001) and total weight (−0.15 kg 95% C.I. −0.21, −0.09 p < 0.001) (Table 2).
There were very small changes in saturated fat and sugar in the final basket, with a significant between-group difference of −0.08 g/MJ (95% C.I. −0.16, −0.01 p = 0.023) for saturated fat; and 0.12 g/MJ (95% C.I. 0.00, 0.25 p = 0.043) for sugar (Supplementary Table 3). There was a small decrease in cost of the basket after swaps in both groups, but no between-group difference (Supplementary Table 3). There was a significantly larger decrease in total energy in the shopping basket post-swaps in the LS + MLS group (−1.71 MJ 95% C.I. −2.54, −0.89 p < 0.001).
3.3.1. Acceptance of swaps
The proportion of swaps accepted out of those offered was the same in both groups. However, the LS + MLS group were offered almost twice as many swaps with 15.7 swaps compared with 8.4 in the LS group (IRR 1.86, 95% C.I. 1.79, 1.93, p < 0.001) and accepted a significantly higher number of offered swaps, 4.39 compared to 2.69 in the LS group (IRR 1.64, 95% C.I. 1.53, 1.76 p < 0.001). In the LS + MLS group 68% of accepted swaps were MLS swaps. Of the swaps accepted, 30% in the LS + MLS group were from a different subcategory and 70% from the same subcategory. The mean salt reduction per swap accepted in the LS + MLS group was more than double that of the LS group (Table 3).
Table 3.
Impact of the intervention (LS + MLS compared to LS) on the acceptance of swaps.
| All, Mean (SD) (N = 947) |
LS, Mean (SD) (N = 476) |
LS + MLS, Mean (SD) (n = 471) |
Difference LS + MLS compared to LS (95% C.I) | p-value | Difference LS + MLS compared to LS (adjb) (95% C.I) | p-value | |
|---|---|---|---|---|---|---|---|
| Average proportion of swaps accepted per participanta | 0.33 (0.27) | 0.34 (0.28) | 0.33 (0.26) | −0.01 (−0.04, 0.03) | 0.6221 | −0.00 (−0.04, 0.03) | 0.785 |
| Salt difference per swap (g/100g) | −0.34 (0.29) | −0.21 (0.10) | −0.46 (0.35) | −0.25 (−0.29, −0.21) | <0.001 | −0.25 (−0.29, −0.21) | <0.001 |
Calculated as the number of swaps accepted out of those offered per participant.
Calculated using linear regression adjusted for: health considered important; price considered important; shopping habits considered important; family likes/dislikes considered important; and baseline shopping basket salt content.
In an exploratory observational analysis among all participants, those who rated health as an important consideration when grocery shopping accepted 13% more swaps than participants who did not view this as a priority (95% C.I. 10%, 17%; p < 0.001) and reduced the salt in their final basket by an additional −0.03g/100g (95% C.I. −0.05, −0.02; p < 0.001), equivalent to 3% greater reduction in salt (Table 4). There was no difference in average salt reduction per swap. Similarly, participants who reported previously being advised to reduce their salt intake (or who had a household member who had been so advised) and those who reported they regularly used nutrition labels for salt content accepted more swaps and reduced the salt in their final basket more than those who had not (Table 4). There was no significant association between the importance attached to price and any of the outcomes.
Table 4.
The impact of health or price being considered important, use of nutrition labels, and salt reduction advice, with salt reduction and swap outcomesa.
| Beta (95% C.I) |
Price important | p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| Health important | p-value | Advised to reduce salt | p-value | Use of nutrition labels | p-value | |||
| Salt reduction (g/100g) (n = 924) | −0.03 (−0.05, −0.02) | <0.001 | −0.03 (−0.04, −0.01) | <0.001 | −0.02 (−0.04, −0.01) | 0.004 | 0.00 (−0.02, 0.02) | 0.872 |
| Proportion of swaps accepted (n = 923) | 0.13 (0.10, 0.17) | <0.001 | 0.06 (0.03, 0.10) | <0.001 | 0.10 (0.06, 0.13) | <0.001 | 0.01 (−0.03, 0.05) | 0.662 |
| Average salt reduction per swap (g/100g) (n = 811) | 0.01 (−0.03, 0.05) | 0.579 | −0.03 (−0.07, 0.00) | 0.062 | −0.01 (−0.05, 0.03) | 0.628 | 0.00 (−0.04, 0.04) | 0.883 |
Beta (95% CI) from linear regression models adjusted for intervention group. Each covariate (e.g. Health important) are modelled as dummy variables (yes vs no) in separate models with “no” being the comparator.
658 (70%) of all participants ‘strongly’ or ‘somewhat’ agreed that this type of swap intervention is something they would like to see when they do their usual shopping and 7% somewhat or strongly disagreed. Increasing acceptability of the intervention was associated with a greater reduction in salt in the total shopping basket; −0.04 g/100g greater reduction in salt with each increasing category of acceptance (95% C.I. −0.05, −0.03; p < 0.001).
4. Discussion
Offering shoppers with hypertension alternatives with substantially less salt, including out-of-category items, lowered the salt content of their total shopping basket by 9% more than offering within-category swaps with minimal salt reduction alone. The proportion of swaps accepted in each group was similar but in the group offered both LS and MLS swaps, two-thirds of the accepted swaps were much lower in salt than the original product; leading to a two-fold greater reduction in salt per swap accepted. In this group, 30% of accepted swaps were from a different subcategory. This suggests that despite the potentially higher cognitive effort required in making purchasing decisions when offered out-of-category swaps this did not adversely affect the acceptability of swaps and resulted in greater salt reduction overall.
This study used a randomised experimental design and was planned to detect a difference of at least 5% in salt between groups. The virtual online supermarket provided a well-controlled environment in which swaps could be offered across a large, representative selection of products. Variability in the shopping basket between participants was limited by the use of a shopping list, focused on high-salt foods which also provided sufficient opportunity for swaps. The outcome measure was objectively recorded and not reliant on self-report. Although this was a virtual supermarket experiment, it closely mimicked real-life online shopping, using a database of products from the largest UK grocery retailer, ensuring participants were presented with an array of familiar products, to increase the likelihood that users engage with the task in a realistic way.
This study has some limitations. The study completion rate of 47% of all randomised participants is low which could introduce a degree of non-response bias and impact generalisability. Participant characteristics were collected at the end of the experiment and no data is therefore available on non-completers. However, the completion rate is comparable to a previous study (Forwood et al., 2015) and to ‘success rates’ more generally for online shopping tasks (Sterne, 2002). A review of reviews of online behaviour change interventions also found the average completion rate for internet delivered interventions is approximately 50% (Kohl et al., 2013). Participants in this study all had hypertension, which potentially increases their motivation to reduce their salt intake, and their capacity to benefit. Hypertension affects more than one in four adults in England (Public Health England, 2014) so reductions in salt intake among this group will contribute to salt reduction at a population level. The benefit of salt reduction for individuals without existing hypertension is also well documented, (He, Li, & Macgregor, 2013) however the effectiveness of this swap-based approach in those without hypertension is unknown.
While this virtual environment allows efficient testing of interventions the external validity is unknown. Shoppers do not pay for their goods nor take delivery of them and their choices may represent their intentions or stated preferences rather than their true purchasing behaviour. The alternatives offered were chosen automatically and at random from all items matching the swap criteria, and in some cases may not have provided sufficiently appropriate or desirable swaps. However, there is no reason to imagine that these factors would influence the relative impact of the LS + MLS versus LS swaps. Field trials might therefore want to test the more varied LS + MLS strategy in intervention to encourage swaps in real supermarket environments, rather than limiting choices to swaps within a narrower product range.
Only one other study has reported offering swaps for salt reduction. The store-based study utilised a smartphone application (app) to identify and present lower salt alternatives to shoppers, finding an average reduction in the shopping basket salt content of over 20% (0.9 g/MJ to 0.7 g/MJ) (Eyles et al., 2017). Previous studies of swap interventions have focused on other nutrients. A study of tailored swaps conducted in a commercial online supermarket found a 10% reduction in the saturated fat content of the shopping basket after swaps (Huang et al., 2006). Two previous randomised controlled trials in supermarket settings combined tailored swaps with nutrition education with varying results. One found no significant effect on saturated fat content of purchased items (Ni Mhurchu et al., 2010), though the study authors recognised that the effects may have been attenuated by the high baseline level of knowledge about healthy eating among participants; and the other found significant reductions in the purchase of high-fat meat and dairy products (Winett et al., 1991b). These studies did not report on the acceptance of swaps or the per-swap change in nutrients. One virtual online supermarket study focused on achieving a reduction in energy density, reported that participants accepted only one in four lower-energy swaps compared to one in three swaps in this study (Forwood et al., 2015).
The current study is unique in reporting the effect of health-related behaviours, such as use of nutrition labels or advice to reduce salt, on acceptance of swaps and impact on salt reduction. Participants who had been advised to reduce their salt intake, who reported that health was an important consideration when purchasing food or who used nutrition labels, were significantly more likely to accept swaps and achieved a greater reduction in salt, suggesting that the benefits of swap-based interventions could be enhanced by complementary interventions that boost intrinsic motivation to reduce salt.
This study adds to the evidence base on offering healthier food alternatives as a mechanism to improve the nutritional composition of peoples’ grocery shopping baskets, in particular, filling a gap in the evidence around lower salt swaps (Hartmann-boyce et al., 2018). We hypothesised that offering swaps with a substantial reduction in salt, even if they may be out-of-category products, would result in a greater overall reduction in salt content despite the potential loss of effectiveness due to increased cognitive effort. The proportion of swaps accepted in each group was the same and nearly 70% of the accepted swaps in the LS + MLS group were for products with more than 20% less salt; indicating that alternatives with a greater salt reduction are no less acceptable. Furthermore, in 30% of LS + MLS swaps, the accepted alternative was from a different product subcategory to the original item, suggesting that out-of-category swaps are acceptable. Overall, the LS + MLS intervention resulted in a 13% reduction in salt content of the shopping basket from the initially selected items. If this percentage reduction was carried through to individual level daily salt intake, it would result in a decrease of 1g per day based on the average adult salt intake in the UK of 8.1g; this would be sufficient for individuals with hypertension to make a meaningful step towards achieving the recommended salt intake of less than 6 g per day. To put this reduction in context, average daily salt intake among adults in the UK decreased 1.4g over a 10 year period from 2001 to 2011 (Sadler et al., 2011).
Some retailers in the UK have already implemented similar swap functions in commercial online grocery shopping sites (Coresight Research, 2017; Denny, 2015). This suggests that there is commercial willingness to implement this behavioural strategy. In addition, technologies now exist to enable consumers to scan food products and identify lower salt or healthier alternatives while shopping in store (Edo. 2018. http://www.edo, 2018; Dunford et al., 2014). The results of experimental interventions such as this study can inform future developments in these digital tools.
5. Conclusions
Offering alternatives with greater reductions in salt is acceptable to shoppers and leads to significantly greater reductions in the salt content of their shopping basket than offering only swaps to very similar products with only small reductions in salt. Offering lower-salt alternatives which are from a wider range of products, rather than limited to the same brand or food subcategory provides greater opportunity for larger reductions in salt per swap and does not negatively impact acceptability. This research could inform the development of new tools and interventions to support healthier food choices while grocery shopping.
Ethics and consent
Approval for the study was given by the University of Oxford, reference R42142/RE001, on the 20th January 2017. All participants were shown a detailed participant information sheet and subsequently confirmed their consent.
Availability of data
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request but are not publicly available. Restrictions apply to the availability of these data, which were used under license for the current study.
Conflicts of interest
The authors declare that they have no competing interests.
Funding
SPR is funded by a British Heart Foundation fellowship and the Medical Research Council.
SJ and PA are NIHR senior investigators and are funded by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC) Obesity, Diet and Lifestyle Theme and National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care Oxford at Oxford Health NHS Foundation Trust.
CP's time on this project was funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care Oxford at Oxford Health NHS Foundation Trust.
MR is funded by the British Heart Foundation (grant number: 006/PSS/CORE/2016/OXFORD).
The project costs were funded by the British Heart Foundation and the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care Oxford.
Authors’ contributions
All authors contributed to the study design, edited the paper and critically revised, and approved the final manuscript. SJ, CP, PA and SPR interpreted the data. SPR analysed the data and led the writing of the paper.
Study reporting
The study was reported in accordance with the Consort 2010 reporting guidance.
Acknowledgements
The authors thank David Judge for providing technical support to deliver the intervention website to participants and Constantinos Koshiaris for advice on statistical methods.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.appet.2018.11.028.
Contributor Information
Sarah Payne Riches, Email: sarah.payneriches@phc.ox.ac.uk.
Paul Aveyard, Email: paul.aveyard@phc.ox.ac.uk.
Carmen Piernas, Email: carmen.piernas-sanchez@phc.ox.ac.uk.
Mike Rayner, Email: mike.rayner@dph.ox.ac.uk.
Susan A. Jebb, Email: susan.jebb@phc.ox.ac.uk.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplementary figure 1. OLS instructions. An image of the virtual online supermarket instruction page, which includes the shopping list for the task.
Supplementary table 1. Product categorisation. The categorisation framework used to define products as ‘within category’ if they were from both the same high-level category and subcategory; or from a different category if they were only within the same high-level category but a different subcategory.
Supplementary table 2. Participant Survey Questions. The content of the survey participants were asked to complete when they had completed the online shopping task.
Supplementary Table 3. Change in nutritional composition and cost between the control and purchased baskets.
References
- Anderson C.A.M., Appel L.J., Okuda N., Brown I.J., Chan Q., Zhao L. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 Years: The INTERMAP study. Journal of the American Dietetic Association. 2010;110(5):736–745. doi: 10.1016/j.jada.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcand J.A., Wong M.M.Y., Santos J.A., Leung A.A., Trieu K., Thout S.R. More evidence that salt increases blood pressure and risk of kidney disease from the science of salt: A regularly updated systematic review of salt and health outcomes (April–July 2016) 2017;19(8):813–823. doi: 10.1111/jch.13049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BHF Cut down on salt. 2013. https://www.bhf.org.uk/publications/healthy-eating-and-drinking/cut-down-on-salt Available from:
- Chaiken S., Liberman A., Eagly A. Unintended thought. In: Uleman J.S., Bargh J.A., editors. Unintended thought. Guilford; New York: 1989. pp. 212–252. [Google Scholar]
- Coresight Research (@Coresight News) "@Ocado launched a calorie saver at checkout; it got 10x the uptake of its comparable money-saver option - tim Steiner at #WRC2017. 4 Apr 2017. https://twitter.com/search?q=ocado_calorie_saver&src=typd Tweet.
- Denny A. Case Study: Sainsbury's response to the sugars challenge. http://www.fdin.org.uk/wp-content/uploads/2015/10/Response-To-The-Sugars-Challenge-Annie-Denny-Sainsburys.pdf. Accessed 06 01 2018.
- Dominick Salvatore . Microeconomics: Theory and applications. 5th ed. Oxford University Press; Oxford: 2008. Microeconomics: Theory and applications; pp. 57–86. [Google Scholar]
- Dunford E., Trevena H., Goodsell C., Ng K.H., Webster J., Millis A. FoodSwitch: A mobile phone app to enable consumers to make healthier food choices and crowdsourcing of national food composition data. JMIR mHealth uHealth. 2014 doi: 10.2196/mhealth.3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edo. 2018. http://www.edoapp.co.uk/. Accessed 06 January 2018.
- Eyles H., McLean R., Neal B., Jiang Y., Doughty R.N., McLean R. A salt-reduction smartphone app supports lower-salt food purchases for people with cardiovascular disease: Findings from the SaltSwitch randomised controlled trial. European Journal of Preventive Cardiology. 2017;24(13):1435–1444. doi: 10.1177/2047487317715713. [DOI] [PubMed] [Google Scholar]
- Forwood S.E., Ahern A.L., Marteau T.M., Jebb S.A. Offering within-category food swaps to reduce energy density of food purchases : A study using an experimental online supermarket. International Journal of Behavioral Nutrition and Physical Activity. 2015;12(85) doi: 10.1186/s12966-015-0241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 risk factors collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann-Boyce J., Bianchi F., Piernas C., Payne Riches S., Frie K., Nourse R. Grocery store interventions to change food purchasing behaviours: A systematic review of randomized controlled trials. American Journal of Clinical Nutrition. 2018;107(6):1004–1016. doi: 10.1093/ajcn/nqy045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He F.J., Li J., Macgregor G.A. Vol 1325. 2013. pp. 1–15. (Effect of longer term modest salt reduction on blood pressure : Cochrane systematic review and meta-analysis of randomised trials). April. [DOI] [PubMed] [Google Scholar]
- Huang A., Barzi F., Huxley R., Denyer G., Rohrlach B., Jayne K. The effects on saturated fat purchases of providing internet shoppers with purchase- specific dietary advice: A randomised trial. PLoS for Clinical Trials. 2006;1(5):e22. doi: 10.1371/journal.pctr.0010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohl L.F.M., Crutzen R., De Vries N.K. Online prevention aimed at lifestyle behaviors: A systematic review of reviews. Journal of Medical Internet Research. 2013;15(7) doi: 10.2196/jmir.2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandrik C.A. Consumer heuristics: The tradeoff between processing effort and value in brand choice. In: Corfman Kim P., John G., Lynch, editors. Vol 23. Association for Consumer Research; Provo, UT: 1996. pp. 301–307. (NA - advances in consumer research). [Google Scholar]
- Ni Mhurchu C., Blakely T., Jiang Y., Eyles H.C., Rodgers A., Ni Mhurchu C. Effects of price discounts and tailored nutrition education on supermarket purchases: A randomized controlled trial. American Journal of Clinical Nutrition. 2010;91(3):736–747. doi: 10.3945/ajcn.2009.28742. [DOI] [PubMed] [Google Scholar]
- NICE Hypertension - clinical management of primary hypertension in adults. NICE Clinical Guideline. 2011;127 [Google Scholar]
- NiMhurchu C., Capelin C., Dunford E.K., Webster J.L., Neal B.C., Jebb S.A. Sodium content of processed foods in the United Kingdom : Analysis of 44,000 foods purchased by 21,000 households. American Journal of Clinical Nutrition. 2011;93(10):594–600. doi: 10.3945/ajcn.110.004481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health England . 2014. Tackling high blood pressure from evidence into action. London. [Google Scholar]
- Sadler K., Nicholson S., Steer T., Gill V., Bates B., Cox L. Department of Health; England: 2011. National diet and nutrition survey - assessment of dietary sodium in adults ( aged 19 to 64 years ) in England. 2012. [Google Scholar]
- Sanchez-Castillo C.P., Warrender S., Whitehead T.P., James W.P. An assessment of the sources of dietary salt in a British population. Clinical Science. 1987;72(1):95–102. doi: 10.1042/cs0720095. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release. Vol 14. StataCorp LP; College Station, TX: 2015. [Google Scholar]
- Sterne J. Web metrics: Proven methods for measuring web site success. Wiley; 2002. Well-marked trails: Measuring web site navigation. (Chapter 10) page 208-209. [Google Scholar]
- Strazzullo P., D'Elia L., Kandala N.-B., Cappuccio F.P. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2016. SHAKE the salt habit the SHAKE technical package for salt reduction. [Google Scholar]
- Winett R.A., Moore J.F., Wagner J.L., Hite L.A., Leahy M., Neubauer T.E. Altering shoppers' supermarket purchases to fit nutritional guidelines: An interactive information system. Journal of Applied Behavior Analysis. 1991 Jan;24(1):95–105. doi: 10.1901/jaba.1991.24-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winett R.A., Wagner J.L., Moore J.F., Walker W.B., Hite L.A., Leahy M. An experimental evaluation of a prototype public access nutrition information system for supermarkets. Health Psychology. 1991;10(1):75–78. doi: 10.1037//0278-6133.10.1.75. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figure 1. OLS instructions. An image of the virtual online supermarket instruction page, which includes the shopping list for the task.
Supplementary table 1. Product categorisation. The categorisation framework used to define products as ‘within category’ if they were from both the same high-level category and subcategory; or from a different category if they were only within the same high-level category but a different subcategory.
Supplementary table 2. Participant Survey Questions. The content of the survey participants were asked to complete when they had completed the online shopping task.
Supplementary Table 3. Change in nutritional composition and cost between the control and purchased baskets.
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request but are not publicly available. Restrictions apply to the availability of these data, which were used under license for the current study.