Abstract
For multifactorial reasons an estimated 20% of patients remain unsatisfied after total knee arthroplasty (TKA).
Appropriate tension of the soft tissue envelope encompassing the knee is important in total knee arthroplasty and soft tissue imbalance contributes to several of the foremost reasons for revision TKA, including instability, stiffness and aseptic loosening.
There is debate in the literature surrounding the optimum way to achieve balancing of a total knee arthroplasty and there is also a lack of an accepted definition of what a balanced knee replacement is.
It may be intuitive to use the native knee as a model for balancing; however, there are many difficulties with translating this into a successful prosthesis.
One of the foundations of TKA, as described by Insall, was that although the native knee has more weight transmitted through the medial compartment this was to be avoided in a TKA as it would lead to uneven wear and early failure. There is a focus on achieving symmetrical tension and pressure and subsequent ‘balance’ in TKA, but the evidence from cadaveric studies is that the native knee is not symmetrically balanced.
As we are currently trying to design an implant that is not based on its anatomical counterpart, is it possible to create a truly balanced prosthesis or to even to define what that balance is? The authors have reviewed the current evidence surrounding TKA balancing and its relationship with the native knee.
Cite this article: EFORT Open Rev 2018;3:614-619. DOI: 10.1302/2058-5241.3.180008.
Keywords: measured resection, patient outcomes, soft tissue balancing, total knee arthroplasty (TKA)
Introduction
Total knee arthroplasty (TKA) is an effective intervention for managing end-stage degenerative joint disease of the knee.1 The clinical outcome relies upon surgical factors such as implant alignment, sizing, and rotation as well as adequate soft-tissue balancing.1 Implant alignment has been shown to relate to post-operative TKA function and patient quality of life.2 Appropriate tension of the soft tissue envelope encompassing the knee is important during TKA; incorrect tensioning can potentially lead to joint stiffness or instability.3 Soft-tissue imbalance contributes to several of the foremost reasons for revision following primary TKA, including instability, stiffness, and aseptic loosening.4
There is much debate surrounding the optimum way to achieve a balanced total knee arthroplasty. However, there is no agreed consensus on the definition of a balanced total knee replacement. Babazadeh et al5 defined a balanced knee as one which has:
A full range of movement.
Symmetrical medial-lateral balance at full extension and 90 degrees of flexion resulting in a rectangular tibiofemoral gap.
Correct valgus/varus alignment in both flexion and extension.
Balanced flexion-extension gap without medial-lateral tightness or laxity.
A well-tracking patella during full motion.
Maximal flexion occurring with the patella reduced and without excessive rollback of the femur on the tibia.
Correct rotational balance between the tibial and femoral components.
However, this definition is not in keeping with soft-tissue balancing of the native knee as demonstrated through cadaveric studies.6,7 The native knee has an intrinsically lax lateral collateral ligament relative to the medial collateral ligament,6,7 which differs from the proposed symmetrical medial–lateral balance in a total knee replacement. There is also more rollback of the lateral femoral condyle compared with the medial, with internal rotation of the tibia in flexion6,7 as opposed to the rectangular tibiofemoral flexion gap in a TKA.
The term a ‘balanced knee replacement’ is commonly used throughout the orthopaedic literature. However, proposed concepts of TKA balancing have inconsistencies with how a native knee is balanced. This results in a lack of clarity regarding what a balanced TKA is and how it should be achieved. The authors conducted a review of the literature with the aim of determining what defines a ‘balanced knee replacement’ and how this relates to the native knee. The article addresses the mechanical alignment and rotation of the knee joint, before then reviewing the issues of soft-tissue tensioning. These aspects have influence over how the knee joint functions and therefore may be related to overall patient outcome following total knee arthroplasty.
Joint alignment and rotation
Native knee
Alignment
The average normal distal femoral alignment is 9° of the anatomical valgus, and the normal proximal tibial alignment is 3° of anatomical varus.8 Therefore, in the native knee there is an increase in the load transmitted through the medial compartment.
Rotation
The tibia internally rotates relative to the femur with increasing flexion due to a greater posterior translation of the lateral femoral condyle relative to the medial femoral condyle.9 Multi-centre ex vivo cadaver studies and in vivo studies demonstrate a significant inter-individual and activity-dependent variability.9 It appears that rotational patterns are variable and under control of the forces imposed on the joint by foot position, body inertia and muscular action.9
Total knee arthroplasty
Mechanical alignment
One of the foundations of TKA, as described by Insall et al,10 was that although the native knee has more load transmitted through the medial compartment, this was to be avoided in a TKA as it would lead to uneven wear and early failure. To overcome this issue the classic technique described by Insall et al10 has been generally adopted, which creates mechanical alignment rather than anatomical alignment. In an effort to equalize the pressures in the medial and lateral compartments the tibia is aligned in neutral varus/valgus, and hence the 3° of anatomic tibial varus is lost and 3° of external rotation of the femoral component is required to compensate and thus balance the flexion gap. However, there have been advances in polyethylene technology so the earlier concerns regarding uneven wear may no longer be relevant.
In the native knee the mechanical axis and therefore joint reaction force tends to lie more medial to the centre of the knee joint. In TKA, to avoid overloading the medial compartment the tibia is cut at 0°. This results in ‘valgizing’ the knee to produce a mechanical axis that goes through the centre of the knee joint and is thought to equalize the pressure in medial and lateral compartments. The annotated radiographs (Fig. 1) illustrate this point with the block arrows demonstrating pressure across medial and lateral compartments. The diagram in the bottom left shows Insall et al’s10 technique for creating a rectangular flexion gap by externally rotating the femoral component 3° from the posterior condylar axis.
Fig. 1.
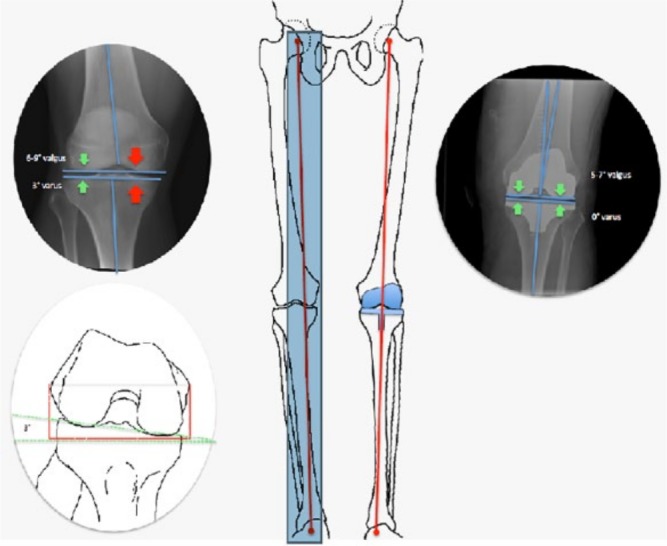
Limb alignments in native vs. traditional total knee arthroplasty (as described by Insall).10
Rotation
In TKA mechanical alignment, where the joint line becomes orthogonal, stability is dependent on correct and precise rotation of the femoral component to compensate for the 3° loss of joint line obliquity due to the tibia cut.11 Controversy exists regarding the most favourable method of determining accurate femoral rotation.11 Two surgical techniques are commonly used to address this: measured resection and gap-balancing.1
Surgical techniques
The two most commonly utilized approaches to achieving joint alignment and rotation are measured resection and gap-balancing. These techniques have different approaches to determining alignment and rotation. There is a body of literature reviewing comparisons between the two that has identified advantages and disadvantages of both approaches.1,11–13
Measured resection
The main principles of measured resection are to replace bony resection with a prosthesis of matched thickness and to determine femoral implant rotation using anatomical landmarks.1 Bony landmarks (femoral epicondyles, posterior femoral condyles, of the anteroposterior axis) are the primary determinants of femoral component rotation.11 It is recommended that the femoral component is placed either parallel to the transepicondylar axis,14–16 perpendicular to the anteroposterior axis,17 or approximately 3° to 4° externally rotated relative to the posterior condylar axis.18 Measured resection maintains anatomical alignment but alters true tibial and femoral alignment of a native knee.11 Critics of measured resection argue that the use of anatomical landmarks can be unreliable, particularly the use of the posterior condylar axis to determine femoral rotation19 due to anatomical variation between patients and its dependence on the surgeon’s ability to correctly identify landmarks.12,20
This highlights a potential issue in the overall concept of defining a balanced knee as, due to variation across the population, it may be that a ‘one theory for all’ may not be ideal for all patients. This is also an issue for gap-balancing, which is discussed below, as pre-existing ligament stiffness varies throughout the population and can then have implications for how a specific knee is naturally balanced by the surrounding native soft tissues.
Gap-balancing
The gap-balancing technique differs in that the tibial bone cut is made first.5 A precise proximal tibial resection is critical as a varus or valgus tibial resection will result in increased internal or external rotation of the femur respectively.21 Following this, symmetrical tension is applied to the joint line in extension using a ligament tensor, knee balancer, or laminar spreaders.5 Then the knee is placed in 90° flexion and the same tensioning device is used to distract the joint, or vice versa with flexion gap assessed first and then the extension gap.5 (Purists would suggest that no soft tissue releases should be performed, using bone cuts only to balance extension and flexion gaps.) The femoral component rotation is thus dictated by tension of the balanced ligaments and not by the anatomical landmarks.22–24
The limitations of gap-balancing are that the level of the joint line or anatomical femoral rotation can be sacrificed in order to achieve perfect balance in flexion and extension.13 Kaipel et al25 found that 36 out of 40 knees which had undergone TKA with gap-balancing had altered femoral rotation post-operatively compared to pre-operatively. Furthermore, all osteophytes need to be removed at first, to avoid unnecessary soft-tissue release, and this may have consequences for the stability of the knee. Gap-balancing does not take into account the natural increased laxity on the lateral side of the knee.26,27 Applying equal tension to the medial and lateral collateral ligaments will cause more joint space opening on the lateral side, thereby creating a balance due to a more externally rotated flexion gap.18 Elevation of the joint line can lead to mid-flexion instability.28 Another criticism is that the tension is assessed and balanced at 0° and 90° but not throughout the whole range of movement. This means that this approach can be associated with mid-flexion (45°) instability.
Overall, gap-balancing is thought to create superior soft-tissue knee balancing compared to measured resection. However, balancing a knee in extension does not mean it is balanced in flexion and vice versa.1 Therefore, some critics argue the measured resection in fact gives a more consistently balanced knee throughout the whole range of movement rather than just at static positions of flexion and extension (Figs. 2 and 3).29
Fig. 2.
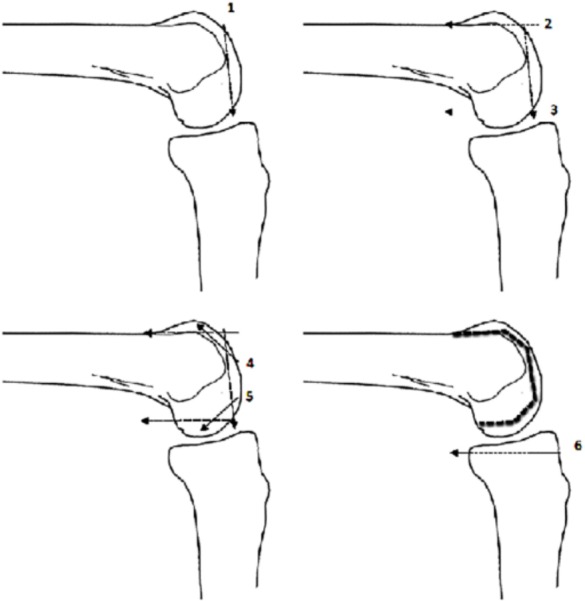
Measured resection. Femoral and tibial cuts are made independently of each other. Soft tissue releases are then made as necessary.
Fig. 3.
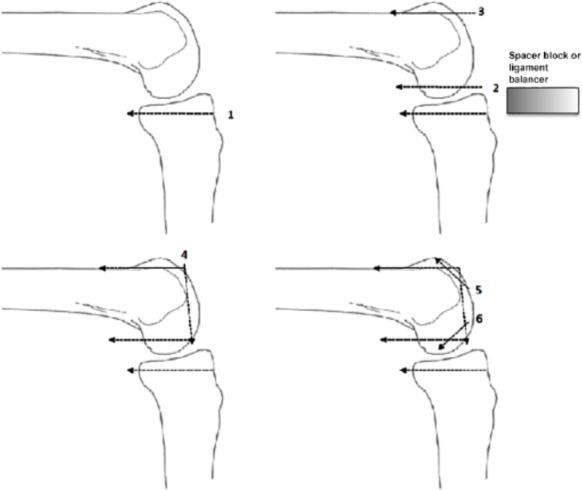
Gap-balancing. The tibial bone cut is made first, then femoral bone cuts are made to produce rectangular extension and flexion gaps based on equally tensioned ligaments.
Ligament balancing and tension
The balancing and tensioning of ligaments determines the joint gap throughout the knee’s range of movement, from full extension to full flexion.
Native knee
Nowakowski et al6 identified that there is general agreement that flexion and extension gaps with TKA should be equal and symmetrical. However, to date there are no available comparisons with physiologically normal knee joints that had not undergone bone resection.6 There are also no standards specifying what degree of force should be used for gap distraction.6 Therefore Nowakowski et al6 measured the flexion and extension gaps in ten cadaveric knees. They concluded that the extension and flexion gaps are physiologically asymmetrical and unequal, and the kinematics are markedly altered after resection of the posterior cruciate ligament (PCL) and/or anterior cruciate ligament (ACL).6 Tanaka et al7 found that both medial and lateral joint gaps at 0° of flexion were significantly smaller than those at other flexion angles,8 therefore further demonstrating that the flexion and extension gaps in a native knee are not equal.
Total knee arthroplasty
Ligament balancing
The basis of the flexion-extension balancing in TKA is an attempt to obtain equal-sized, rectangular gaps in both flexion and extension.30,31 Both the flexion and extension gap should be equal as the femoral prosthesis has a uniform thickness in flexion and extension,5 requiring the TKA model to deviate from the flexion-extension gaps of the native knee. An unequal flexion-extension gap in a TKA can result in overstuffing of the joint where the gap is smallest and/or laxity of the knee where the gap is largest.32 However, in contradistinction to this approach, Roth et al33 showed that there is little evidence that achieving equal ligamentous laxities prevents either overly tight or overly loose soft-tissue restraints after TKA.
Roth et al33 highlighted the issue of inserting a prosthetic joint but retaining native ligaments in situ, producing varying degrees of stiffness and therefore impacting on that individual joint’s balancing and tension. Smith et al34 found that the superficial medial collateral ligament (MCL), deep MCL, PCL, and iliotibial band forces were particularly sensitive in stance phase.34 For all the ligaments, the total contact force was positively correlated with ligament stiffness and reference strain.34
Tension
Estimating the soft-tissue balancing can be achieved with spacer blocks, laminar spreaders, tensioning devices and trial components.35 Manual spreaders or tensioners utilize the surgeon’s manual distraction force,35 whereas some spreaders/tensioning devices incorporate a torque meter which indicates the angular deviation, as well as the distraction distance.36,37 Heesterbeek et al38 aimed to assess how much force was needed to pre-tension the ligaments during a TKA. The force at the stiffness transition point was significantly different between extension and flexion, and both compartments and all values varied considerably between patients.38
A further issue with the use of tension to determine ligament balancing is that there is a paucity of literature evaluating how much tension should be put through the knee and that this value may vary on an individual basis as demonstrated by Heesterbeek et al.38 Kamat et al39 suggested that there may be superior surgical approaches depending on the individual’s pre-operative knee biomechanics. For example, they found that a gap-balancing technique demonstrated better results in a smaller subgroup of knees with greater pre-operative tissue imbalance.39
Whilst there is a body of research surrounding the most accurate way of determining soft-tissue tension within a knee, Nagai et al40 found no significant difference in joint-centre gap or varus ligament balance at flexion or extension between the different joint distraction forces. Ten Ham et al41 compared the use of manual spacers and tensioners. They found that the tensioner-guided system resulted in significantly more valgus laxity in flexion compared with the spacer-guided system.41 In extension, the situation was reversed. However, they found no clinical difference in outcome between the use of spacers or a tensioner.41
The amount of tensioning on a knee joint, both medially and laterally, relates to the amount of pressure that is transmitted through the medial and lateral joint compartments. Kinetic sensors are being utilized to aid the surgeon to achieve equal intracompartmental pressure within the knee joint. There have been several studies showing improved patient outcomes in those with balanced intracompartmental pressures4,42 and demonstrating that this is more consistently achieved with the use of kinetic sensors.43,44 However, Meneghini et al45 found that post-operative patient scores were unrelated to mediolateral balance of the knee. Verstraete et al3 tried to determine an optimum amount of pressure to be transmitted through the knee compartments. However, as their study was performed on native knee cadavers they found that the intracompartmental pressures were not equal. They also performed their study on non-arthritic knees. As the majority of TKAs are performed for arthritis the measurements may not be a true representation of the TKA patient cohort.
Conclusions
A definition of a balanced TKA is difficult if not impossible to produce. When Insall10 described his classical alignment theory this was in part an effort to avoid the error of increasing the natural 3 degrees of varus of the tibia to 6 degrees (error +/–3 degrees) where early failure was observed. To continue to use this classical alignment technique may, however, condemn the TKA to never being truly balanced. To remove a wedge of bone from the tibia and then balance the knee around this, by using gap-balancing or measured resection, is not possible as the ligaments within the knee no longer have the same biomechanical properties.
Whilst this review focusses on the balancing of a TKA, variation in balancing does not consistently translate to variation in patient outcome. The issue of patient outcome and satisfaction is highly complex, multifactorial and too extensive to be adequately assessed in this report. This review has addressed the current surgical approaches to balancing a TKA and how this varies from the biomechanics of a native knee.
There are issues surrounding all of the modes and methods utilized to define and achieve a balanced knee prosthesis. Across the body of research there is little consistency between what surgeons are trying to achieve in arthroplasty (i.e. symmetrical ligament balancing and intracompartmental pressures), and what we observe in the native knee. There is also little consideration for the anatomical and physiological variation across the population, so it may be that a unifying prosthesis and surgical approach to realizing a balanced knee is not achievable.
Therefore, the main obstacle to defining ‘balance’ in the context of knee arthroplasty is that by the nature of this procedure the surgeon is altering the anatomy and subsequent forces transmitted through the joint. Consequently, there is no reference point or ‘gold standard’ with regards to achieving perfect balance. The introduction of modern technologies to orthopaedics may allow the surgeon to implant the TKA within +/– one degree. The refinement of robotic technology, for example, may allow this to occur and also allow for a prosthesis to be designed to the specifications of a patient’s individual biomechanics. True measured resection could then be performed and a ‘balanced’ knee may then be possible.
Footnotes
ICMJE Conflict of interest statement: None declared.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Sheth NP, Husain A, Nelson CL. Surgical techniques for total knee arthroplasty: measured resection, gap balancing, and hybrid. J Am Acad Orthop Surg 2017;25:499–508. [DOI] [PubMed] [Google Scholar]
- 2. Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty 2009;24:560–569. [DOI] [PubMed] [Google Scholar]
- 3. Verstraete MA, Meere PA, Salvadore G, Victor J, Walker PS. Contact forces in the tibiofemoral joint from soft tissue tensions: implications to soft tissue balancing in total knee arthroplasty. J Biomech 2017;58:195-202. [DOI] [PubMed] [Google Scholar]
- 4. Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR. A targeted approach to ligament balancing using kinetic sensors. J Arthroplasty 2017;32(7):2127-2132. [DOI] [PubMed] [Google Scholar]
- 5. Babazadeh S, Stoney JD, Lim K, Choong PF. The relevance of ligament balancing in total knee arthroplasty: how important is it? A systematic review of the literature. Orthop Rev (Pavia) 2009;1:e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nowakowski AM, Majewski M, Müller-Gerbl M, Valderrabano V. Development of a force-determining tensor to measure ‘physiologic knee ligament gaps’ without bone resection using a total knee arthroplasty approach. J Orthop Sci 2011;16:56–63. [DOI] [PubMed] [Google Scholar]
- 7. Tanaka K, Muratsu H, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M. Soft tissue balance measurement in anterior cruciate ligament-resected knee joint: cadaveric study as a model for cruciate-retaining total knee arthroplasty. J Orthop Sci 2007;12:149–153. [DOI] [PubMed] [Google Scholar]
- 8. Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res 1990;255:215–227. [PubMed] [Google Scholar]
- 9. Victor J. A comparative study on the biomechanics of the native human knee joint and total knee arthroplasty. Doctoral thesis, 2009. https://core.ac.uk/download/pdf/34437230.pdf (date last accessed 25 October 2018).
- 10. Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res 1985;192:13–22. [PubMed] [Google Scholar]
- 11. Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 2010;468:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Luyckx T, Peeters T, Vandenneucker H, Victor J, Bellemans J. Is adapted measured resection superior to gap-balancing in determining femoral component rotation in total knee replacement? J Bone Joint Surg Br 2012;94:1271–1276. [DOI] [PubMed] [Google Scholar]
- 13. Babazadeh S, Dowsey MM, Stoney JD, Choong PF. Gap balancing sacrifices joint-line maintenance to improve gap symmetry: a randomized controlled trial comparing gap balancing and measured resection. J Arthroplasty 2014;29:950–954. [DOI] [PubMed] [Google Scholar]
- 14. Berger RA, Rubash HE, Seel MJ, Thompson W, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 1993;286:40-47. [PubMed] [Google Scholar]
- 15. Griffin FM, Insall JN, Scuderi GR. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 2000;15:970–973. [DOI] [PubMed] [Google Scholar]
- 16. Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res 1996;331:35–46. [DOI] [PubMed] [Google Scholar]
- 17. Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res 1995;321:168-172. [PubMed] [Google Scholar]
- 18. Nagamine R, Miura H, Inoue Y, et al. Reliability of the anteroposterior axis and the posterior condylar axis for determining rotational alignment. J Orthop Sci 1998;3:194-198. [DOI] [PubMed] [Google Scholar]
- 19. Schnurr C, Nessler J, König DP. Is referencing the posterior condyles sufficient to achieve a rectangular flexion gap in total knee arthroplasty? Int Orthop 2009;33:1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yau WP, Chiu KY, Tang WM. How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: an in vivo study. J Arthroplasty 2007;22:1042–1048. [DOI] [PubMed] [Google Scholar]
- 21. Daines BK, Dennis DA. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg 2014;6:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whiteside LA, Saeki K, Mihalko WM. Functional medial ligament balancing in total knee arthroplasty. Clin Orthop Relat Res 2000;380:45–57. [DOI] [PubMed] [Google Scholar]
- 23. Dennis DA, Fehring TK. P.F.C. Sigma RP knee system surgical technique. First ed. Warsaw: DePuy Orthopaedics, 2007. [Google Scholar]
- 24. Insall J, Ranawat CS, Scott WN, Walker P. Total condylar knee replacement: preliminary report. Clin Orthop Relat Res 1976;120:149–154. [PubMed] [Google Scholar]
- 25. Kaipel M, Gergely I, Sinz K, Neumann C, Sinz G. Femoral rotation in ligament balanced knee arthroplasty: a prospective clinical study. J Arthroplasty 2013;28:1103–1106. [DOI] [PubMed] [Google Scholar]
- 26. Whiteside LA, Kasselt MR, Haynes DW. Varus-valgus and rotational stability in rotationally unconstrained total knee arthroplasty. Clin Orthop Relat Res 1987;219:147–157. [PubMed] [Google Scholar]
- 27. Van Damme G, Defoort K, Ducoulombier Y, Van Glabbeek F, Bellemans J, Victor J. What should the surgeon aim for when performing computer-assisted total knee arthroplasty? J Bone Joint Surg Am 2005;87–A:52–58. [DOI] [PubMed] [Google Scholar]
- 28. Martin JW, Whiteside LA. The influence of joint line position on knee stability after condylar knee arthroplasty. Clin Orthop Relat Res 1990;259:146–156. [PubMed] [Google Scholar]
- 29. Hungerford DS. Measured resection: a valuable tool in TKA. Orthopedics 2008;31:941-944. [DOI] [PubMed] [Google Scholar]
- 30. Ries MD, Haas SB, Windsor RE. Soft-tissue balance in revision total knee arthroplasty. J Bone Joint Surg Am 2003;85–A:S38–42. [DOI] [PubMed] [Google Scholar]
- 31. Lombardi AV, Jr, Berend KR, Leith JR, Mangino GP, Adams JB. Posteriorstabilized constrained total knee arthroplasty for complex primary cases. J Bone Joint Surg Am 2007;89:S90–S102. [DOI] [PubMed] [Google Scholar]
- 32. Bellemans J, Ries MD, Victor J. Total knee arthroplasty: a guide to get better performance. Heidelberg: Springer Medizin Verlag, 2005. [Google Scholar]
- 33. Roth JD, Howell SM, Hull ML. Native knee laxities at 0°, 45°, and 90° of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Joint Surg [Am] 2015;97:1678–1684. [DOI] [PubMed] [Google Scholar]
- 34. Smith CR, Vignos MF, Lenhart RL, Kaiser J, Thelen DG. The influence of component alignment and ligament properties on tibiofemoral contact forces in total knee replacement. J Biomech Eng 2016;138:021017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kwak DS, Kong CG, Han SH, Kim DH, In Y. Development of a pneumatic tensioning device for gap measurement during total knee arthroplasty. Clin Orthop Surg 2012;4:188–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Asano H, Muneta T, Sekiya I. Soft tissue tension in extension in total knee arthroplasty affects postoperative knee extension and stability. Knee Surg Sports Traumatol Arthrosc 2008;16:999–1003. [DOI] [PubMed] [Google Scholar]
- 37. Yagishita K, Muneta T, Ikeda H. Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty 2003;18:313–320. [DOI] [PubMed] [Google Scholar]
- 38. Heesterbeek PJC, Haffner N, Wymenga AB, Stifter J, Ritschl P. Patient-related factors influence stiffness of the soft tissue complex during intraoperative gap balancing in cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:2760-2768. [DOI] [PubMed] [Google Scholar]
- 39. Kamat YD, Aurakzai KM, Adhikari AR. Computer navigation of soft tissues in total knee replacement. J Knee Surg 2013;26:145–150. [DOI] [PubMed] [Google Scholar]
- 40. Nagai K, Muratsu H, Takeoka Y, Tsubosaka M, Kuroda R, Matsumoto T. The influence of joint distraction force on the soft-tissue balance using modified gap-balancing technique in posterior-stabilized total knee arthroplasty. J Arthroplasty 2017;32:2995-2999. [DOI] [PubMed] [Google Scholar]
- 41. Ten Ham AM, Heesterbeek PJC, van der Schaaf DB, Jacobs WCH, Wymenga AB. Flexion and extension laxity after medial, mobile-bearing unicompartmental knee arthroplasty: a comparison between a spacer-and a tension-guided technique. Knee Surg Sports Traumatol Arthrosc 2013;21:2447–2452. [DOI] [PubMed] [Google Scholar]
- 42. Chow JC, Breslauer L. The use of intraoperative sensors significantly increases the patient-reported rate of improvement in primary total knee arthroplasty. Orthopedics 2017;40:e648-651. [DOI] [PubMed] [Google Scholar]
- 43. D’Angelo F, Puricelli M, Binda T, Surace MF, Floridi C, Cherubino P. The use of an electronic system for soft tissue balancing in primary total knee arthroplasties: clinical and radiological evaluation. Surg Technol Int 2015;26:261–268. [PubMed] [Google Scholar]
- 44. Elmallah RK, Mistry JB, Cherian JJ, et al. Can we really ‘feel’ a balanced total knee arthroplasty? J Arthroplasty 2016;31:102–105. [DOI] [PubMed] [Google Scholar]
- 45. Meneghini RM, Ziemba-Davis MM, Lovro LR, Ireland PH, Damer BM. Can intraoperative sensors determine the ‘target’ ligament balance? Early outcomes in total knee arthroplasty. J Arthroplasty 2016;31:2181–2187. [DOI] [PubMed] [Google Scholar]


