Abstract.
Stigma has been associated with health-related outcomes such as medication adherence and quality of life (QOL) in patients with tuberculosis (TB); however, the mechanisms via which TB-related stigma interferes with specific outcomes are unclear. This study aimed to determine whether depressive symptoms were one of the mechanisms that mediated the associations between TB-related stigma and both medication adherence and QOL in patients with TB. A cross-sectional survey was conducted between October 1, 2013, and March 31, 2014, in Hubei Province, central China, and data were collected from 1,342 patients with TB, using a structured questionnaire that measured TB-related stigma, depressive symptoms, medication adherence, and QOL. Multiple imputation was used to account for missing data. Structural equation modeling was performed to assess the mediating effect of depressive symptoms on the associations of TB-related stigma with medication adherence and QOL. Mediation analyses showed that depressive symptoms partially mediated the association between TB-related stigma and medication adherence (standardized indirect effect = −0.16, 95% bias-corrected confidence interval [CI] [−0.19, −0.13], P < 0.01). Moreover, depressive symptoms fully mediated the association between TB-related stigma and QOL (standardized indirect effect = −0.17, 95% bias-corrected CI [−0.21, −0.14], P < 0.01). The results suggest that depressive symptoms played a key role in the relationships among TB-related stigma, medication adherence, and QOL in patients with TB. Therefore, the alleviation of depressive symptoms could be an important strategy for improving medication adherence and QOL in patients with TB.
Introduction
Patients with tuberculosis (TB) are now able to enjoy improved health because of the implementation of therapeutic regimens recommended by the World Health Organization.1 However, to obtain optimal benefits from this treatment, patients are required to maintain strict adherence to TB medication regimens. Unfortunately, poor medication adherence is common in patients with TB, which increases the risk of morbidity, mortality, and drug resistance, potentially reducing patients’ quality of life (QOL).2–4
Factors associated with TB medication adherence and QOL have been explored in previous studies. For instance, a systematic review of qualitative studies reported that similar factors affected medication adherence and QOL, including health conditions, demographic factors, and psychosocial factors such as stigma.5 Stigma is both an important predictor of medication adherence and a factor affecting QOL.6–12 Goffman posited that stigma was a social process that reduced individuals “from a whole and usual person to a tainted, discounted one.”13 During this process, patients tend to conceal their symptoms and withdraw from interpersonal contact for fear of discrimination, thereby isolating themselves to avoid negative public attitudes, and this could affect medication adherence.14 Furthermore, TB-related stigma is known to lead to poor self-esteem and lack of self-confidence, which are common symptoms of depression, and therefore threaten emotional, mental, and physical well-being and interfere with QOL in patients with TB.15
Depressive symptoms also constitute a significant barrier to medication adherence and QOL. The prevalence of depressive symptoms in patients with TB has been reported to be approximately 16.8–70.0%.15–18 It is possible that participants’ ethnicity, gender, age, and location influence the likelihood of experiencing depressive status. In addition, the variation in reported prevalence of depression may be due to the fact that different tools were used for measuring depression, and that various states of depression were mixed together, including the diagnosed major depression disorder, self-reported depression, and nonspecific depressive states. Consequently, it is difficult to compare the reported results in the previous studies. The presence of depression exerts an adverse effect on the ability to cope with stress, treatment side effects, and daily life.19 Depressed individuals are unlikely to seek care promptly or adhere to medication regimens consistently or precisely.20 In addition, when patients with TB are in a depressive status, they experience severe psychological distress, which interferes with their QOL, comprising a person’s physical, psychological, and emotional well-being.5 Several recent studies have demonstrated negative associations between depressive symptoms and specific health-related outcomes, such as medication adherence and QOL in patients with TB.21–23
As mentioned previously, although previous studies have linked stigma with depressive symptoms and medication adherence/QOL separately, these variables have not been examined simultaneously to determine the interrelationships among them. Most previous studies involving regression analysis have only explored the direct relationships between variables; therefore, the pathways reflecting their effects on medication adherence and QOL in patients with TB remain unclear. However, mediation analysis could also identify complex indirect relationships between variables and explain the mechanism or process via which the variables affect each other.24
We conducted a cross-sectional study to estimate the associations of TB-related stigma with medication adherence and QOL in patients with TB, and, more importantly, determine whether depressive symptoms mediated these associations. To our knowledge, this was the first study to examine whether depressive symptoms were a mediator of the impact of stigma on both medication adherence and QOL in patients with TB. Based on the theory and empirical findings described previously, we hypothesized that depressive symptoms would mediate the associations between TB-related stigma and medication adherence/overall QOL among patients with TB in China.
Methods
Ethics statement.
Ethical approval was provided by the Human Research Ethics Committee, Huazhong University of Science and Technology, Wuhan, China. Each participant was voluntary and provided written informed consent before participating in the study.
Participants and sampling.
A cross-sectional study was conducted between October 1, 2013, and March 31, 2014, in Hubei Province, central China. Participants were recruited via multistage stratified sampling. Counties across Hubei Province were divided into three categories based on their levels of economic development (i.e., upper, middle, and lower), and a county was randomly selected from each category. Thereafter, patients with TB who attended TB clinics at the study sites in the selected counties were recruited as participants. The inclusion criterion was a diagnosis of active TB, based on national TB program guidelines, and the exclusion criterion was the presence of psychosis. In total, 1,430 patients with TB were recruited and completed a structured, self-administered questionnaire anonymously. Of the 1,430 questionnaires collected, 88 were directly deleted because of logical errors or a large amount of missing data. In addition, approximately 4% of questionnaires had missing data for the TB-related stigma scale, and the level of missingness was less than or equal to 2% for other variables. Thus, multiple imputation was used to account for missing data,25,26 and eventually, 1,342 TB patients were included in the analysis.
Measurement instruments.
The questionnaire consisted of five sections: Demographic Characteristics, TB-Related Stigma, Depressive Symptoms, Medication Adherence, and QOL. The demographic characteristics included age, gender, educational level, marital status, religious beliefs, and history of previous TB treatment.
Tuberculosis-related stigma was measured using the TB-Related Stigma scale by our research group. A detailed description of the development of the scale was available in our previous study.27 Briefly, the original item pool was formulated through literature review and in-depth interview. Then, the appropriate items were selected to form the first draft of the scale through group discussion and expert evaluation. The first draft was piloted among 15 patients with TB and finally the TB-Related Stigma scale was developed. The scale consists of nine items divided between three subscales (Negative Experience, Emotional Reactions, and Coping Style). Responses for the items are provided using a four-point Likert scale ranging from 0 (strongly disagree) to 3 (strongly agree). The item scores are summed to provide a total score (range: 0–27), and higher scores indicate greater stigma. The overall Cronbach’s alpha was 0.88 for the scale. The deletion of any individual item would have lowered the scale’s internal consistency, as all of the items demonstrated alpha values of more than 0.85. Overall, these results demonstrate good internal consistency for the TB-Related Stigma scale among patients with TB. The English version of the scale and its evaluation were shown in the Supplement Tables.
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression (CES-D) Scale which is a commonly used self-report measure of depressive symptoms in research and clinical settings.28 The scale consists of 20 items divided between four subscales: Depressive Mood, Somatic Symptoms, Interpersonal Relationships, and Positive Affect. Responses for the items are provided using a four-point Likert scale ranging from 0 (not at all) to 3 (almost daily). The item scores are summed to provide a total score (range: 0–60). The CES-D has been widely used in China,29 and in the present study, the scale demonstrated high internal consistency (Cronbach’s alpha = 0.86).
Medication adherence was measured using the 8-item Morisky Medication Adherence Scale (MMAS-8). The scale was developed by Morisky in 2008 and was a structured self-reported medication adherence measure.30 Response choices are yes/no for items 1 through 7 and the last item is answered using a five-point Likert scale. Total scores range from 0 to 8, and higher scores indicate stricter medication adherence. The MMAS-8 has been used extensively in China31 with good reliability and validity. In our study, the scale showed good internal consistency (Cronbach’s alpha = 0.79).
Quality of life was measured using a 6-item scale that was developed by Phillips in 2002.32 The scale included six items pertaining to physical health, psychological health, economic circumstances, work, family relationships, and relationships with nonfamily associates. Participants were asked to rate the extent to which six characteristics reflected circumstances in their lives during the preceding month. Responses were provided using a five-point Likert scale ranging from 1 (very poor) to 5 (excellent). Higher scores indicated higher QOL levels. In the present study, the six items scale showed good internal consistency (Cronbach’s alpha = 0.81).
Statistical analysis.
Data were analyzed using the Statistical Analysis System (SAS) 9.4 for Windows (SAS Institute, Inc., Cary, NC) and AMOS (version 17.0; IBM, Seoul, Korea) software packages. The missing values were filled by SAS multiple imputation procedure. We calculated descriptive statistics for participants’ demographic characteristics. Structural equation modeling (SEM) was performed to assess the mediating effect of depressive symptoms on the associations of TB-related stigma with medication adherence and QOL in patients with TB. The maximum likelihood method was used to perform parameter estimations. In addition, 95% confidence intervals (CIs) were calculated using bootstrapping with 1,000 resamples for all effects,33 which were considered statistically significant if the 95% CI did not include zero. The following fit indices were used to evaluate goodness of fit for the model: root mean square error of approximation (RMSEA), the goodness-of-fit index (GFI), the adjusted GFI (AGFI), the comparative fit index (CFI), and the Tucker–Lewis index (TLI). Goodness-of-fit index, AGFI, CFI, and TLI values greater than 0.90 and RMSEA values less than 0.08 indicated adequate goodness of fit.34,35 All differences were assessed using two-tailed tests, and the significance level was set at P < 0.05.
Results
Demographic characteristics and descriptions of the study variables.
The participants’ mean age was 47.56 (standard deviation = 17.05) years, and 67.44% of participants were men. In addition, 57.23% of participants were educated to at least secondary school level, and most of the participants were married (78.46%) (Table 1).
Table 1.
Demographic characteristics of study sample (N = 1,342)
| Characteristics categories | N | % |
|---|---|---|
| Gender | ||
| Male | 905 (67.44) | 67.44 |
| Female | 437 (32.56) | 32.56 |
| Education | ||
| Primary or less | 574 (42.77) | 42.77 |
| Secondary | 540 (40.24) | 40.24 |
| High school or higher (above) | 228 (16.99) | 16.99 |
| Marital status | ||
| Single | 231 (17.21) | 17.21 |
| Separated/divorced/widowed | 58 (4.33) | 4.33 |
| Married | 1,053 (78.46) | 78.46 |
| Religious beliefs | ||
| No | 1,162 (86.59) | 86.59 |
| Yes | 180 (13.41) | 13.41 |
| History of prior antituberculosis treatment | ||
| No | 1,174 (87.48) | 87.48 |
| Yes | 168 (12.52) | 12.52 |
Tuberculosis-related stigma was negatively correlated with medication adherence (r = −0.31, P < 0.01) and QOL (r = −0.22, P < 0.01). In addition, depressive symptoms were negatively correlated with medication adherence (r = −0.38, P < 0.001) and QOL (r = −0.51, P < 0.01) and positively correlated with TB-related stigma (r = 0.28, P < 0.01) (Table 2).
Table 2.
Descriptive statistics and correlations between variables
| Variables | Mean (standard deviation) | TB-related stigma | Depressive symptoms | Medication adherence |
|---|---|---|---|---|
| TB-related stigma | 9.27 (4.25) | – | – | – |
| Depressive symptoms | 15.84 (8.26) | 0.28** | – | – |
| Medication adherence | 6.06 (1.95) | −0.31** | −0.38** | – |
| Quality of life | 18.98 (3.16) | −0.22** | −0.51** | 0.31** |
TB = tuberculosis; **P < 0.01.
Assessment of the mediating effect of depressive symptoms on medication adherence.
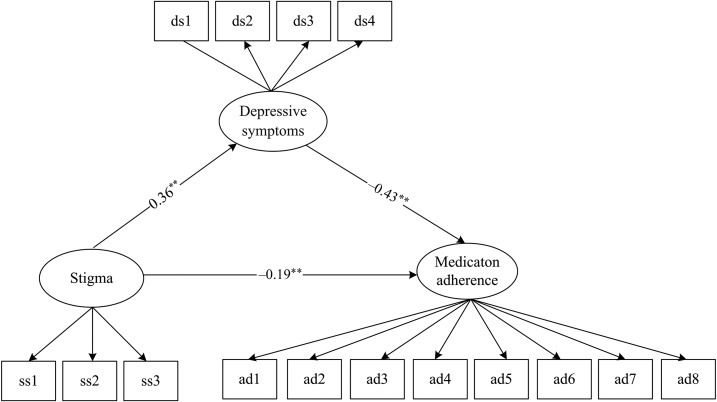
As shown in Figure 1, SEM was performed in AMOS 17.0 to assess the mediating effect of depressive symptoms on the relationship between stigma and medication adherence, controlling for gender and age. The fit indices for model 1 indicated that the model fits the data well (GFI = 0.97; AGFI = 0.94; TLI = 0.93; CFI = 0.95; RMSEA = 0.05; Figure 1). Stigma was positively associated with depressive symptoms (standard error [SE] = 0.09, standardized coefficient [β] = 0.36, P < 0.01) and negatively associated with medication adherence (SE = 0.01, β = −0.19, P < 0.01). In addition, depressive symptoms were negatively associated with medication adherence (SE < 0.01, β = −0.43, P < 0.01). Depressive symptoms partially mediated the relationship between stigma and medication adherence (standardized indirect effect: −0.16, 95% bias-corrected CI [−0.19, −0.13], P < 0.01) (Table 3, Figure 1).
Figure 1.
Mediation model for medication adherence (model 1). Note: Structural equation modeling was conducted in AMOS 17.0 to test the mediating effect of depressive symptoms on the relationship between stigma and medication adherence. All the coefficients in the figure were standardized. Model was adjusted for age and gender. **P < 0.01; goodness-of-fit index (GFI) = 0.97; adjusted GFI = 0.94; Tucker–Lewis index = 0.93; comparative fit index = 0.95; root mean square error of approximation = 0.05. Questionnaire items of the Morisky Medication Adherence Scale-8 labeled ad1, ad2, ad3, ad4, ad5, ad6, ad7, and ad8. Three dimensions of the Tuberculosis-Related Stigma scale labeled ss1, ss2, and ss3. Four subscales of the Center for Epidemiologic Studies Depression scale labeled ds1, ds2, ds3, and ds4.
Table 3.
Parameter estimates from model 1
| Paths | Coefficient | Standard error | Standardized coefficient (β) | 95% confidence interval | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Adherence ← stigma | −0.04 | 0.01 | −0.19** | −0.26 | −0.12 |
| Adherence ← depressive symptoms | −0.03 | < 0.01 | −0.43** | −0.50 | −0.36 |
| Adherence ← age | −0.01 | < 0.01 | −0.06* | −0.12 | −0.01 |
| Adherence ← gender | −0.04 | 0.02 | −0.09* | −0.12 | −0.01 |
| Depressive symptoms ← stigma | 0.99 | 0.09 | 0.36** | 0.31 | 0.42 |
| Depressive symptoms ← age | 0.02 | 0.01 | 0.11** | 0.06 | 0.17 |
| Depressive symptoms ← gender | 1.19 | 0.21 | 0.15** | 0.09 | 0.20 |
Adherence = medication adherence; *P < 0.05, **P < 0.01.
Assessment of the mediating effect of depressive symptoms on QOL.
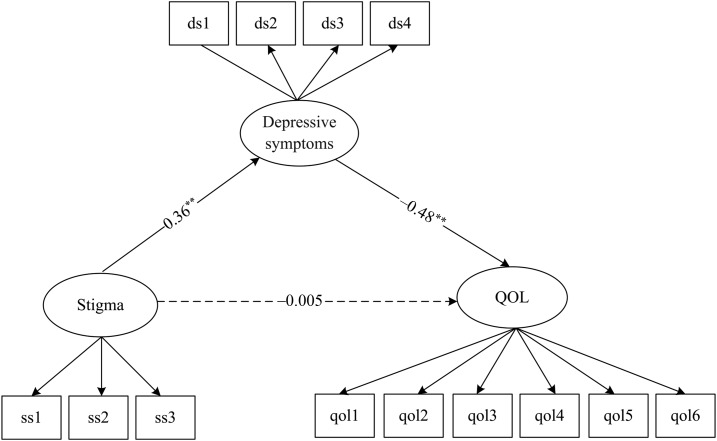
The fit indices for the model 2 also suggested that the model fits the data well (GFI = 0.94; AGFI = 0.91; TLI = 0.91; CFI = 0.93; RMSEA = 0.07). Stigma was a significant predictor of depressive symptoms (SE = 0.09, β = 0.36, P < 0.01), and depressive symptoms were negatively associated with QOL (SE = 0.01, β = −0.48, P < 0.01). However, the direct effect of stigma on QOL was nonsignificant (SE = 0.02, β = −0.005, P = 0.88). Depressive symptoms fully mediated the relationship between stigma and QOL (standardized indirect effect = −0.17, 95% bias-corrected CI [−0.21, −0.14], P < 0.01) (Table 4, Figure 2).
Table 4.
Parameter estimates from model 2
| Paths | Coefficient | Standard error | Standardized coefficient(β) | 95% confidence interval | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| QOL ← stigma | −0.002 | 0.02 | −0.005 | −0.08 | 0.06 |
| QOL ← depressive symptoms | −0.09 | 0.01 | −0.48** | −0.54 | −0.41 |
| QOL ← age | −0.01 | < 0.01 | −0.16** | −0.21 | −0.11 |
| QOL ← gender | −0.07 | 0.04 | −0.05 | −0.10 | 0.01 |
| Depressive symptoms ← stigma | 0.97 | 0.09 | 0.36** | 0.31 | 0.41 |
| Depressive symptoms ← age | 0.02 | 0.01 | 0.11** | 0.06 | 0.17 |
| Depressive symptoms ← gender | 1.18 | 0.20 | 0.14** | 0.10 | 0.20 |
QOL = quality of life; *P < 0.05, **P < 0.01.
Figure 2.
Mediation model for quality of life (QOL) (model 2) Note: All the coefficients in the figure were standardized. Model was adjusted for age and gender, **P < 0.01; goodness-of-fit index (GFI) = 0.94; adjusted GFI = 0.91; Tucker–Lewis index = 0.91; comparative fit index = 0.93; root mean square error of approximation = 0.07. The arrow with the dotted line represents the effect between stigma and QOL that is not statistically significant (standardized estimates: β = −0.005, P = 0.88). Questionnaire items of QOL labeled qol1, qol2, qol3, qol4, qol5, and qol6. Three dimensions of the Tuberculosis-Related Stigma scale labeled ss1, ss2, and ss3. Four subscales of the Center for Epidemiologic Studies Depression scale labeled ds1, ds2, ds3, and ds4.
Discussion
The study examined the associations among TB-related stigma, depressive symptoms, and medication adherence/QOL in patients with TB simultaneously. To our knowledge, this was the first study to perform mediation analyses to examine these complex relationships in patients with TB. The key finding was that depressive symptoms partially mediated the relationship between TB-related stigma and medication adherence and fully mediated the relationship between TB-related stigma and QOL, which provided strong evidence to support the study hypothesis.
Our findings were consistent with previous studies which have linked depressive symptoms with TB-related stigma and medication adherence/QOL separately.10,12,22,36 More importantly, the results of the mediation analyses suggested that depressive symptoms at least partially explained the associations between TB-related stigma and both medication adherence and QOL. Two previous studies showed that depressive symptoms mediated the relationship between HIV-related stigma and medication adherence in people living with human immunodeficiency virus infection and acquired immune deficiency syndrome,37,38 which provided evidence to support our research.
This study focused on the complex relationships among TB-related stigma, depressive symptoms, and medication adherence/QOL in patients with TB. Depressive symptoms may be a reaction to negative life events such as TB infection, stigma, and side effects of some drugs during the treatment.39 Therefore, reducing the impact of negative psychological stress factors such as the alleviation of stigma may be an effective way to relieve depressive symptoms among patients with TB. Moreover, our study demonstrated the possible mechanism via which TB-related stigma affected adherence and QOL in patients with TB. Coping with TB-related stigma may be a way to relieve depressive symptoms in patients with TB and ultimately reduce the negative health outcomes caused by depression. Clinical health-care providers should consider the interconnected relationships among stigma, depressive symptoms, and poor medication adherence in patients with TB and enhance interventions designed to reduce stigmatization and depression in clinical practice, which will ultimately help to achieve better health outcomes.10
One of the strengths of the study was that SEM was performed to examine mediating variables. The assessment of mediation has been used widely to open the “black box” in epidemiological studies. Our mediation analysis was based on SEM, which takes into account measurement errors and is more robust than the regression model.40,41 The use of SEM allowed us to disentangle the pathways linking stigma to medication adherence and QOL.
The study was subject to several limitations which should be acknowledged. First, the analysis of cross-sectional data limited the scope for inference of causality in the relationships between the study variables; therefore, future research should use longitudinal designs to validate the current findings. Second, the CES-D scale which was used in our study is a commonly used self-report measure of depressive symptoms and this scale cannot be used as a diagnostic tool. Participants for this study did not have clinical diagnosis of depression. Therefore, pay attention to this when generalizing our results. Moreover, although the results demonstrated the effects of two interconnected factors (i.e., stigma and depressive symptoms), other variables, such as self-efficacy and social support, could have affected treatment adherence; therefore, future research should examine alternative potential mechanisms underlying the associations among TB-related stigma, medication adherence, and QOL.
Conclusion
Overall, the study showed strong associations among TB-related stigma, depressive symptoms, and medication adherence/QOL in patients with TB and indicated that depressive symptoms represented a mechanism via which TB-related stigma influenced medication adherence and QOL in patients with TB. Therefore, the findings could enhance health-care workers’ understanding of strategies for coping with TB-related stigma, depressive symptoms, and treatment adherence difficulties in patients with TB.
Supplementary Material
Acknowledgments:
We thank the Center for Disease Control and Prevention of Hubei Province for their support. We also appreciate all study participants who have been involved and contributed to the procedure of data collection.
Note: Supplemental tables appears at www.ajtmh.org.
REFERENCES
- 1.World Health Organization , 2016. Global Tuberculosis Report 2016. Geneva, Switzerland: WHO. [Google Scholar]
- 2.Woith WM, Larson JL, 2008. Delay in seeking treatment and adherence to tuberculosis medications in Russia: a survey of patients from two clinics. Int J Nurs Stud 45: 1163–1174. [DOI] [PubMed] [Google Scholar]
- 3.Tachfouti N, Slama K, Berraho M, Nejjari C, 2012. The impact of knowledge and attitudes on adherence to tuberculosis treatment: a case-control study in a Moroccan region. Pan Afr Med J 12: 52. [PMC free article] [PubMed] [Google Scholar]
- 4.Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J, 2007. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med 4: e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kastien-Hilka T, Rosenkranz B, Bennett B, Sinanovic E, Schwenkglenks M, 2016. How to evaluate health-related quality of life and its association with medication adherence in pulmonary tuberculosis—designing a prospective observational study in South Africa. Front Pharmacol 7: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Link BG, Phelan JC, 2006. Stigma and its public health implications. Lancet 367: 528–529. [DOI] [PubMed] [Google Scholar]
- 7.Chang SH, Cataldo JK, 2014. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. Int J Tuberc Lung Dis 18: 168–173. [DOI] [PubMed] [Google Scholar]
- 8.Anand T, Kumar DA, Sharma N, Saha R, Krishnamurthy L, Singh SV, Ingle GK, 2014. Perception of stigma towards TB among patients on DOTS & patients attending general OPD in Delhi. Indian J Tuberc 61: 35–42. [PubMed] [Google Scholar]
- 9.Sabawoon W, Sato H, Kobayashi Y, 2012. Delay in the treatment of pulmonary tuberculosis: a report from Afghanistan. Environ Health Prev Med 17: 53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peddireddy V, 2016. Quality of life, psychological interventions and treatment outcome in tuberculosis patients: the indian scenario. Front Psychol 7: 1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kastien-Hilka T, Abulfathi A, Rosenkranz B, Bennett B, Schwenkglenks M, Sinanovic E, 2016. Health-related quality of life and its association with medication adherence in active pulmonary tuberculosis—a systematic review of global literature with focus on South Africa. Health Qual Life Outcomes 14: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y, Ehiri J, Tang S, Li D, Bian Y, Lin H, Marshall C, Cao J, 2013. Factors associated with patient, and diagnostic delays in Chinese TB patients: a systematic review and meta-analysis. BMC Med 11: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goffman E, 1963. Stigma: Notes on the Management of Spoiled Identity. New York, NY: Simon & Schuster. [Google Scholar]
- 14.McArthur E, Bali S, Khan AA, 2016. Socio-cultural and knowledge-based barriers to tuberculosis diagnosis for women in Bhopal, India. Indian J Community Med 41: 62–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duko B, Gebeyehu A, Ayano G, 2015. Prevalence and correlates of depression and anxiety among patients with tuberculosis at WolaitaSodo University Hospital and Sodo Health Center, WolaitaSodo, south Ethiopia, cross sectional study. BMC psychiatry 15: 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sagili KD, Satyanarayana S, Chadha SS, 2016. Is knowledge regarding tuberculosis associated with stigmatising and discriminating attitudes of general population towards tuberculosis patients? Findings from a community based survey in 30 districts of India. PLoS One 11: e0147274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee LY, Tung HH, Chen SC, Fu CH, 2017. Perceived stigma and depression in initially diagnosed pulmonary tuberculosis patients. J Clin Nurs 26: 4813–4821. [DOI] [PubMed] [Google Scholar]
- 18.Singh L, Pardal PK, Prakash J, 2015. Psychiatric morbidity in patients of pulmonary tuberculosis-an observational study. Ind Psychiatry J 24: 168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mason PH, Sweetland AC, Fox GJ, Halovic S, Nguyen TA, Marks GB, 2016. Tuberculosis and mental health in the Asia-Pacific. Australas Psychiatry 24: 553–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pan SW, Yen YF, Feng JY, Su VYF, Kou YR, Su WJ, 2015. The risk of depressive disorder among contacts of tuberculosis patients in a TB-endemic area: a population-based cohort study. Medicine 94: e1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dos Santos APC, Lazzari TK, Silva DR, 2017. Health-related quality of life, depression and anxiety in hospitalized patients with tuberculosis. Tuberc Respir Dis (Seoul) 80: 69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kehbila J, Ekabe CJ, Aminde LN, Noubiap JJN, Fon PN, Monekosso GL, 2016. Prevalence and correlates of depressive symptoms in adult patients with pulmonary tuberculosis in the southwest region of Cameroon. Infect Dis Poverty 5: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pachi A, Bratis D, Moussas G, Tselebis A, 2013. Psychiatric morbidity and other factors affecting treatment adherence in pulmonary tuberculosis patients. Tuberc Res Treat 2013: 489865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shapiro-Mendoza CK, 2014. Commentary: mediation and moderation analyses: a novel approach to exploring the complex pathways between maternal medical conditions, preterm birth and associated newborn morbidity risk. Int J Epidemiol 43: 815–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harel O, Mitchell EM, Perkins NJ, Cole SR, Tchetgen Tchetgen EJ, Sun B, Schisterman EF, 2018. Multiple imputation for incomplete data in epidemiologic studies. Am J Epidemiol 187: 576–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee KJ, Carlin JB, 2012. Recovery of information from multiple imputation: a simulation study. Emerg Themes Epidemiol 9: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang TT, Tong YQ, YIn XX, Lu ZX, Gong YH, 2016. Evaluation of Morisky medication aherence scale and family APGAR applied to patients with tuberculosis. Chin J Social Med 33: 580–582. [Google Scholar]
- 28.Radloff LS, 1977. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1: 385–401. [Google Scholar]
- 29.Zhang J, Sun W, Kong Y, Wang C, 2012. Reliability and validity of the center for epidemiological studies depression scale in 2 special adult samples from rural China. Compr Psychiatry 53: 1243–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morisky DE, Ang A, Krousel-Wood M, Ward HJ, 2008. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 10: 348–354. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Yan J, You LM, Yang Q, Liu B, Jin S, Zhou J, Lin C, Monrisky DE, 2014. Translation and validation of a Chinese version of the 8-item Morisky medication adherence scale in myocardial infarction patients. J Eval Clin Pract 20: 311–317. [DOI] [PubMed] [Google Scholar]
- 32.Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M, 2002. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet 360: 1728–1736. [DOI] [PubMed] [Google Scholar]
- 33.Preacher KJ, Hayes AF, 2008. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 40: 879–891. [DOI] [PubMed] [Google Scholar]
- 34.Hu L, Bentler PM, 1999. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6: 1–55. [Google Scholar]
- 35.Kenny DA, McCoach DB, 2003. Effect of the number of variables on measures of fit in structural equation modeling. Struct Equ Model 10: 333–351. [Google Scholar]
- 36.Li CT, Chu KH, Reiher B, Kienene T, Chien LY, 2017. Evaluation of health-related quality of life in patients with tuberculosis who completed treatment in Kiribati. J Int Med Res 45: 610–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mitzel LD, Vanable PA, Brown JL, Bostwick RA, Sweeney SM, Carey MP, 2015. Depressive symptoms mediate the effect of HIV-related stigmatization on medication adherence among HIV-infected men who have sex with men. AIDS Behav 19: 1454–1459. [DOI] [PubMed] [Google Scholar]
- 38.Rao D, Feldman BJ, Fredericksen RJ, Crane PK, Simoni JM, Kitahata MM, Crane HM, 2012. A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS Behav 16: 711–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ambaw F, Mayston R, Hanlon C, Alem A, 2015. Depression among patients with tuberculosis: determinants, course and impact on pathways to care and treatment outcomes in a primary care setting in southern Ethiopia—a study protocol. BMJ Open 5: e007653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hafeman DM, Schwartz S, 2009. Opening the black box: a motivation for the assessment of mediation. Int J Epidemiol 38: 838–845. [DOI] [PubMed] [Google Scholar]
- 41.Brunner J, Austin PC, 2009. Inflation of type I error rate in multiple regression when independent variables are measured with error. Can J Stat 37: 33–46. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.