Abstract.
In this study, we analyze clustering of infant deaths within families living in a rural part of western Burkina Faso. The study included 9,220 infants, born between 1993 and 2009 in Nouna Health and Demographic Surveillance System (HDSS). A clustering of infant deaths in families was explored by calculating observed versus expected number of infant deaths within families for a given family size. In addition, risk ratios were calculated for infant death depending on the vital status of the previous sibling. We observed 470 infant deaths, yielding an overall infant mortality risk of 51/1,000 births. Clustering of infant deaths within families was observed (P = 0.004). In smaller families, the mortality of firstborns was higher than for the following siblings. The infant mortality risk was higher when the preceding sibling died in infancy (P = 0.03). The study supports the hypothesis of infant death clustering existing within rural families in West Africa. Further studies are needed to shed more light on these findings with the goal to develop effective interventions directed toward the families who already lost a child.
Introduction
Globally, infant mortality has decreased from an estimated 63 deaths per 1,000 live births in 1990 to 32 deaths per 1,000 live births in 2015.1 However, the risk of a child dying before completing the first year of life in 2015 was highest in the WHO African Region (55 per 1,000 live births), more than five times higher than in the WHO European Region (10 per 1,000 live births).1 Progress is needed to meet the Sustainable Development Goal of Good Health and Well-being (SDG 3) on infant survival, particularly in high-mortality countries of sub-Saharan Africa (SSA).2,3 To achieve the SDG of an under-five mortality risk of a maximum 25 deaths per 1,000 live births by 2030, a total of 47 countries need to make substantial progress, 34 are located in SSA, among them Burkina Faso.3
In societies with high mortality and high fertility, there is evidence that mortality increases with family size and that clustering of deaths occurs within families.4–7 High correlation in infant mortality among siblings is partly attributed to short birth intervals.8–10 In many countries, sufficient birth spacing has been promoted through mother–child health programs, as this is perceived to be beneficial for the health and well-being of mothers and children.11 Death clustering has been understood as a phenomenon in which greater heterogeneity exists in the distribution of child deaths between families than would be expected if deaths were distributed randomly. Investigating this issue in Kenya, Omariba et al.6 showed that the death of the immediately preceding child had a substantial and significant effect on the probability of death of the next child in the family even after adjustment for child-level variables (e.g. multiple birth, birth order, birth interval, and maternal age) and family-level factors (e.g. maternal/paternal education, ethnicity, and religion).
Until now, the topic of infant death clustering has rarely been analyzed and mostly been considered with retrospective birth history data from Demographic and Health Surveys (DHSs). Health and Demographic Surveillance Systems (HDSSs) have the advantage that data are continuously collected over a long time, thereby accounting for all births and deaths occurring within the study area.12
It is the aim of this study to investigate clustering of infant mortality with regard to the following questions: 1) is there infant clustering within certain families? 2) Is the birth order of a child associated with mortality? 3) Is the mortality risk of a child higher, if the directly preceding sibling died in infancy?
Materials and methods
Study area.
The Nouna HDSS, a member of the International Network for the Demographic Evaluation of Populations and their Health (INDEPTH),13,14 is located in a rural area of North-Western Burkina Faso and comprises about 90,000 people in 2010, living in the semi-urban town of Nouna and 58 surrounding villages. Since 1993, its population is under continuous demographic surveillance. Most inhabitants live from subsistence farming. All households in the study area are visited three times per year to register vital events such as births and deaths, and in- and out-migration.12,13,15 Health services in the HDSS area consist of one district hospital in Nouna town and 18 peripheral health centers.
Study population.
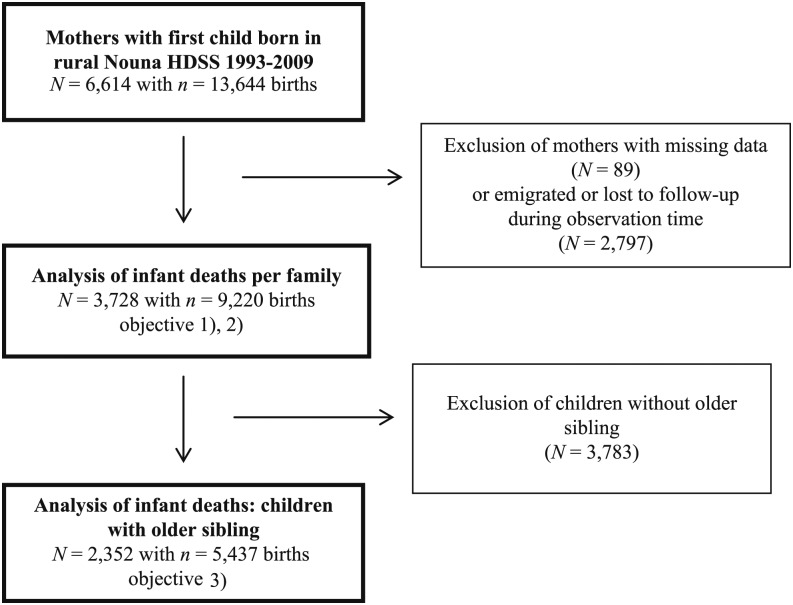
In this analysis, we considered infant deaths, that is deaths that occurred between birth and the first birthday, of children born in the calendar period 1993–2009 within the rural part of Nouna HDSS (excluding the town of Nouna). Children were included if the complete birth history of the mother was available. This implies that the first child of a mother was born in the HDSS after January 1, 1993, and the mother stayed within the study area from that time onward. Mothers who emigrated out of the study area were excluded from analysis because the information about the vital status of all her children could not be ensured. The inclusion criteria in Figure 1 were set to investigate families (mothers are considered to constitute the family-level) with continuous birth order.
Figure 1.
Flowchart of participant inclusion and exclusion criteria, rural Nouna Health and Demographic Surveillance System (HDSS), 1993–2009.
There were 6,614 mothers whose first child was born in the rural area of Nouna HDSS between 1993 and 2009. Of these, 3,728 mothers with 9,220 children fulfilled the inclusion criteria for objectives 1) and 2) of living within the study area for the full observation period. Concerning objective 3), the first child had to be excluded from the analysis because considered children had to have at least one older sibling, which left 2,352 mothers with 5,437 children for analysis.
Statistical analysis.
To investigate possible clustering of infant deaths within families, objective 1), the expected number of families with i infant deaths (EXPij) per family size j was estimated under the assumption of no clustering as follows:
with , where is the number of infant deaths in families with size j and is the number of children in families of size j. This is compared with the observed number of i infant deaths in families of size j (OBSij). To assess whether statistically significant infant death clustering exists, we calculated as follows:
To avoid very small numbers we combined two or more infant deaths within a family into one group. This yields a value with 10 degrees of freedom.
To evaluate if the order of the child is associated with the infant mortality risk (objective [3]), we calculated how often infant death occurred in the kth child of a family, stratified by total number of live births of a family. Twins and multiples were assigned the same birth order.
For objective 3), we calculated infant mortality risks for the subgroup of 5,437 children with existing older sibling, and estimated the mortality risk ratio of both groups, where the previous sibling died or did not die as infant. If the kth child had preceding twins, one of which died and the other survived, this child was assigned as “older sibling died.”
All analyses were generated using SAS/STAT® Software, Version 9.4 of the SAS System for Windows.16
Results
The mean number of children per family in our analysis for the observation period January 1, 1993, until December 31, 2009, was 2.5 [median = 2, range 1–10]. It must be noted that the end of observation date was before the end of the reproductive phase for many women in the study; therefore, this number must not be interpreted as the mean number of births per woman. With 470 observed infant deaths in 9,220 births, the overall infant mortality risk was 51.0 per 1,000 live births (95% confidence interval [CI]: 46.5–55.5). The dataset included 222 multiples (108 twins and three triplets), from which 32 twin siblings died.
Table 1 summarizes live births and infant mortality in the study population by family size. In total, 3,311 (88.8%) families experienced no infant death. Of the 470 infant deaths, 21.7% occurred in families with two and more infant deaths. The observed and the expected (in italics) numbers of infant deaths per family are shown. For example, among the 390 families with four live births, there were 86 infant deaths. Among these, we observed 317 families with no infant death, 61 families with one death, 11 families with two deaths, and one family with three deaths of four births, whereas only 6.5 families were expected to experience two or more deaths, given “overall mortality in families with four children.”
Table 1.
Distribution of infant deaths per family, rural Nouna Health and Demographic Surveillance System, 1993–2009
| No. of live births per family | Infant deaths per family | No. of families | Infant deaths | Mortality risk per 1,000 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | * | ||||||
| 1 | OBS | 1,305 | 46 | – | – | – | – | 1,351 | 46 | – | 34.1 (24.4–43.7) |
| EXP | 1,305.0 | 46.0 | – | – | – | – | |||||
| 2 | OBS | 801 | 72 | 5 | – | – | 5 | 878 | 82 | 5.5 | 46.7 (36.8–56.6) |
| EXP | 798.0 | 78.1 | 1.9 | – | – | 1.9 | |||||
| 3 | OBS | 532 | 99 | 7 | 0 | – | 7 | 638 | 113 | 0.1 | 59.0 (48.5–69.6) |
| EXP | 531.5 | 100.2 | 6.3 | 0.0 | – | 6.3 | |||||
| 4 | OBS | 317 | 61 | 11 | 1 | 0 | 12 | 390 | 86 | 6.9 | 55.1 (43.8–66.5) |
| EXP | 310.9 | 72.6 | 6.3 | 0.2 | 0.0 | 6.5 | |||||
| 5 | OBS | 226 | 42 | 8 | 1 | 1 | 10 | 278 | 65 | 7.0 | 46.8 (35.7–57.9) |
| EXP | 218.8 | 53.7 | 5.3 | 0.2 | 0.0 | 5.5 | |||||
| 6 | OBS | 87 | 26 | 9 | 0 | 0 | 9 | 122 | 44 | 4.2 | 60.1 (42.9–77.3) |
| EXP | 84.1 | 32.3 | 5.2 | 0.4 | 0.0 | 5.6 | |||||
| 7–10 | OBS | 43 | 22 | 6 | 0 | 0 | 6 | 71 | 34 | 2.4 | 65.8 (44.4–87.1) |
| EXP | 47.3 | 19.8 | 3.5 | 0.4 | 0.0 | 3.9 | |||||
| Total | – | 3,311 | 368 | 46 | 2 | 1 | 49 | 3,728 | 470 | 26.1 | 51.0 (46.5–55.5) |
OBS = observed number of infant deaths; EXP = Expected number of infant deaths; estimated by binominal distribution given row total. test based on entries in shaded cells.
* Combined groups with deaths for calculating the statistics.
The overall chi-square test statistic was 26.1 with 10 degrees of freedom and the corresponding chi-squared test results in a P-value of 0.004.
Table 2 shows the birth order of the deceased infants, stratified by total number of live births (objective 2). For example, among all families with four live births, we observed 86 deaths in total, of which we found 31 deaths of the first child, 23 deaths of the second child, and so on. For smaller families (≤ 4 live births), the mortality of firstborns seemed to be higher than that for the following siblings, whereas for larger families no clear pattern was seen.
Table 2.
Infant deaths (N = 470) stratified by birth order of a child, rural Nouna Health and Demographic Surveillance System, 1993–2009
| No. of live births per family | Birth order of deceased infants per family | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| 1 | OBS | 46 | – | – | – | – | – | – |
| Percent | 100.0 | – | – | – | – | – | – | |
| 2 | OBS | 55 | 27 | – | – | – | – | – |
| Percent | 67.1 | 32.9 | – | – | – | – | – | |
| 3 | OBS | 50 | 43 | 20 | – | – | – | – |
| Percent | 44.6 | 37.5 | 17.9 | – | – | – | – | |
| 4 | OBS | 31 | 23 | 19 | 13 | – | – | – |
| Percent | 36.1 | 26.7 | 22.1 | 15.1 | – | – | – | |
| 5 | OBS | 16 | 12 | 26 | 7 | 4 | – | – |
| Percent | 24.6 | 18.5 | 40.0 | 10.8 | 6.2 | – | – | |
| 6 | OBS | 7 | 10 | 7 | 11 | 8 | 1 | – |
| Percent | 15.9 | 22.7 | 15.9 | 25.0 | 18.2 | 2.3 | – | |
| 7–10 | OBS | 4 | 7 | 7 | 5 | 4 | 6 | 1 |
| Percent | 11.8 | 20.6 | 20.6 | 14.7 | 11.8 | 17.7 | 2.9 | |
OBS = observed number of infant deaths; Percent = row percentages.
Regarding research question 3), children with an existing older sibling were analyzed. We observed 5,437 children, where 258 infant deaths occurred. To investigate whether a child had a higher infant mortality risk if the preceding sibling died as an infant, a cross-classification of infant deaths (Yi) by survival status of the preceding child (Yi−1) is presented in Table 3. The observed conditional probabilities p1 and p0 of an infant death given that his/her preceding sibling had died or survived, respectively, are as follows:
Table 3.
Distribution of infants by survival status of index and previous child for 5,437 children with an existing older sibling in rural Nouna Health and Demographic Surveillance System, 1993–2009
| Index child | ||||
|---|---|---|---|---|
| Previous child | Deceased | Alive | All | |
| Deceased | No | 24 | 305 | 329 |
| % | 7.3 | 92.7 | 100 | |
| Alive | No | 234 | 4,874 | 5,108 |
| % | 4.6 | 95.4 | 100 | |
| All | No | 258 | 5,179 | 5,437 |
Children whose older sibling died in infancy were 1.6 times more likely to die in the first year of life than children whose older sibling survived (RR = 1.58; 95% CI: 1.1–2.5; P = 0.03).
Discussion
The present study showed a significant clustering of infant mortality within families in the rural area of the Nouna HDSS and children whose older sibling died in infancy were at significantly increased risk to die in their first year of life. Our results suggest that being the first child in the family may be a risk factor to die in infancy.
In the study area, several risk factors for infant mortality have been identified in previous studies: age of the mother at birth of the child, death of the mother, being a twin, insufficient birth spacing, being born in the rainy season, specific areas of residence, ethnicity, and distance to the nearest health center.10,17–20 A recent follow-up study in the Nouna HDSS study area showed that the previously identified risk factors for infant mortality decreased over time, but infant mortality has remained unacceptably high,21 supporting the idea for further investigations into the risks of infant mortality. Household wealth, which is suspected to play a major role in infant death clustering,22 was recently analyzed in the Nouna HDSS, but was found to not affect infant and child mortality in the rural Nouna HDSS.23
The finding of this study is in line with other literature, where mortality clustering was found in SSA22. Kuate-Defo and Diallo22 stated that infant and early childhood mortality levels in Africa are ascribed to a concentration of child mortality within particular families. They also claimed the survival status of the preceding child as the principal determinant of mortality concentration which is in line with a recent study from Bangladesh, where the authors found that the risk of under-five death was significantly higher in children whose mothers reported a previous death of a sibling.24
The finding that mortality risk of firstborns was higher than that for the following siblings in smaller families was in line with the study results of Van Malderen et al.9 who found that in 13 African countries, the first child and the fifth or later in birth order had a higher risk of death. Also a large study in India found that infant mortality risk was higher when the preceding sibling had died as an infant, as compared with when the preceding sibling survived.4 They found that the pattern of effects shows no obvious relation with the socioeconomic status of the families and highlight the role of short birth intervals.
In a study in Kenya, the authors investigated with DHS data in detail why mortality risks for infants differ between families.6 Omariba et al.6 examined the extent of death clustering by analyzing the sequence of births and deaths in a family and found also substantial clustering of infant deaths in certain families, whereas most families did not experience any death, similar to our results. The authors report that the risk of death for siblings close in age is more likely than for those further apart. They suspected that there is a causal process in which the death of an immediately previous child increases the risk of death of the next child in the family. Few families contributing to the high percentage of infant death were also determined in a study in Nigeria with high risk of infant death showing that if there was prior neonatal death in a family, then the probability of death for index neonate is seven times more likely, than neonates from families with no previous neonatal death.25
The reasons for infant death clustering in Nouna HDSS are still unclear. Possible reasons among other within-family risks are mother’s level of education, insufficient economic resources, parent’s attitude toward health or care-seeking behavior, ethnicity, and accessibility of health center.4,6 Edvinsson and Janssens26 underline that because of the complex phenomenon related to high-risk mothers, adequate methods have to be developed and large datasets are needed. In a recent review, van Dijk27 emphasized that early-life mortality clustering usually occurs in a limited number of high-mortality families, which is in line with the findings from our article. It has to be underlined that families play a more important role for death clustering than communities. Still unknown is whether the same characteristics put infants and children at risk in both high- and low-risk families, or if there are specific explanations for mortality in high-risk families. These questions are essential for making progress in the field of early-life mortality clustering in families. In addition, it has been reported that fathers may also play an important role and should therefore be considered in more detail. This might be especially important with regard to health policy. Moreover, van Dijk27 argues that the timing of death is related to the cause. Post-neonatal deaths may be more strongly related to factors such as childcare and other exogenous characteristics such as e.g. wasting, diarrhoea, and respiratory diseases, whereas perinatal deaths are assumed to be related to factors experienced during pregnancy and to health and genetic problems in affected families. Further research on the causes of death in relation to time of death in high-mortality families may help to disentangle the mechanisms of death clustering of children.
Strengths and limitations.
It is an advantage of this study to be based on an HDSS site that continuously collected data for 17 years and provides data on mothers with a continuous and complete birth order. However, only mothers who got their first child in Nouna HDSS could be considered and mothers who migrated out of the HDSS area or already had their first child when they moved to the study area or when the HDSS was initiated had to be excluded from analysis. Another limitation is that perinatal deaths are underreported in countries of SSA, which is also true for the Nouna HDSS.12 Reasons are that the households are only visited every 4 months, and that women might not want to report early deaths for cultural reasons.
It should be noted that the test we used to test for clustering within families is in fact conservative because it simply tests the departure from the binomial distribution. In our data, we observe a departure in a particular direction, pointing to more families with zero infant deaths or with many deaths, and less families with one death than expected.
Conclusions.
The study investigates clustering of infant deaths within families in the rural Nouna HDSS. Being born as first child and the infant death of a previous sibling are important risk factors for infant mortality. Because it is difficult to uncover the mechanisms associated with the death of a previous sibling and clustering of infant deaths in certain families, further analytical studies are needed to investigate these findings and to develop interventions to identify and support particularly vulnerable families. Interventions might be directed toward families who already lost a child, to encourage care-seeking.
Acknowledgments:
We would like to thank the staff of the Centre de Recherche en Santé de Nouna, who are responsible for all data collection and entry processes in the Health and Demographic Surveillance System.
REFERENCES
- 1.GHO, WHO , 2017. Global Health Observatory (GHO) Data: Infant Mortality. Available at: http://www.who.int/gho/child_health/mortality/neonatal_infant/en/. Accessed October 2018.
- 2.Bryce J, Victora CG, Black RE, 2013. The unfinished agenda in child survival. Lancet 382: 1049–1059. [DOI] [PubMed] [Google Scholar]
- 3.United Nations , 2015. The Millennium Development Goals Report 2015. Available at: http://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf. Accessed October 2018.
- 4.Arulampalam W, Bhalotra S, 2008. The linked survival prospects of siblings: evidence for the Indian states in population. Popul Stud 62: 171–190. [DOI] [PubMed] [Google Scholar]
- 5.Ikamari L, 2000. Sibling mortality correlation in Kenya. J Biosoc Sci 32: 265–278. [DOI] [PubMed] [Google Scholar]
- 6.Omariba W, Rajulton F, Beaujot R, 2008. Correlated mortality risks of siblings in Kenya: the role of state dependence. Demographic Res 18: 311–336. [Google Scholar]
- 7.Ranjan M, Dwivedi LK, Mishra R, 2018. Caste differentials in death clustering in central and eastern Indian states. J Biosoc Sci 50: 254–274. [DOI] [PubMed] [Google Scholar]
- 8.Ronsmans C, 1996. Birth spacing and child survival in rural Senegal. Int J Epidemiol 25: 989–997. [DOI] [PubMed] [Google Scholar]
- 9.Van Malderen C, Van Oyen H, Speybroeck N, 2013. Contributing determinants of overall and wealth-related inequality in under-5 mortality in 13 African countries. J Epidemiol Community Health 67: 667–676. [DOI] [PubMed] [Google Scholar]
- 10.Becher H, Müller O, Jahn A, Gbangou A, Kynast-Wolf G, Kouyaté B, 2004. Risk factors of infant and child mortality in rural Burkina Faso. Bull World Health Organ 82: 265–273. [PMC free article] [PubMed] [Google Scholar]
- 11.Lartey ST, Khanam R, Takahashi S, 2016. The impact of household wealth on child survival in Ghana. J Health Popul Nutr 35: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sié A, Louis VR, Gbangou A, Müller O, Niamba L, Stieglbauer G, Ye M, Kouyate B, Sauerborn R, Becher H, 2010. The health and demographic surveillance System (HDSS) in Nouna, Burkina Faso, 1993–2007. Glob Health Action Sep 14; 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.INDEPTH , 2018. An International Network of DSS Sites Involved in Demographic and Health Research in Developing Countries. Available at: http://www.indepth-network.org. Accessed October 2018.
- 14.Sankoh O, Byass P, 2012. The INDEPTH Network: filling vital gaps in global epidemiology. Int J Epidemiol 41: 579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Becher H, Kouyaté B, 2005. Health Research in Developing Countries: A Collaboration between Burkina Faso and Germany. Heidelberg, Germany: Springer. [Google Scholar]
- 16.SAS, Copyright © 2013 SAS Institute Inc., Cary, NC.
- 17.Jahn A, Kynast-Wolf G, Kouyaté B, Becher H, 2006. Multiple pregnancy in rural Burkina Faso: frequency, survival, and use of health services. Acta Obstet Gynecol Scand 85: 26–32. [DOI] [PubMed] [Google Scholar]
- 18.Kynast-Wolf G, Hammer GP, Müller O, Kouyatü B, Becher H, 2006. Season of death and birth predict patterns of mortality in Burkina Faso. Int J Epidemiol 35: 427–435. [DOI] [PubMed] [Google Scholar]
- 19.Hammer GP, Some F, Müller O, Kynast-Wolf G, Kouyatü B, Becher H, 2006. Pattern of cause-specific childhood mortality in a malaria endemic area of Burkina Faso. Malar J 5: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schoeps A, Gabrysch S, Niamba L, Sié A, Becher H, 2011. The effect of distance to health-care facilities on childhood mortality in rural Burkina Faso. Am J Epidemiol 173: 492–498. [DOI] [PubMed] [Google Scholar]
- 21.Schoeps A, Kynast-Wolf G, Nesbitt R, Müller O, Sié A, Becher H, 2015. Decreasing disparities in infant survival using surveillance data from Burkina Faso. Am J Trop Med Hyg 92: 1038–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuate-Defo B, Diallo K, 2002. Geography of child mortality clustering within African families. Health Place 8: 93–117. [DOI] [PubMed] [Google Scholar]
- 23.Schoeps A, Souares A, Niamba L, Diboulo E, Kynast-Wolf G, Müller O, Sié A, Becher H, 2014. Childhood mortality and its association with household wealth in rural and semi-urban Burkina Faso. Trans R Soc Trop Med Hyg 108: 639–647. [DOI] [PubMed] [Google Scholar]
- 24.Abir T, Agho KE, Page AN, Milton AH, Dibley MJ, 2015. Risk factors for under-5 mortality: evidence from Bangladesh Demographic and Health Survey, 2004–2011. BMJ Open 5: e006722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mishra R, Ranjan M, 2015. Linkages Among Sibling Survival and Death Clustering in Nigeria: A Panel Data Analysis. Available at: http://uaps2015.princeton.edu/abstracts/151590. Accessed October 2018.
- 26.Edvinsson S, Janssens A, 2012. Clustering of deaths in families: infant and child mortality in historical perspective. Biodemography Soc Biol 58: 75–86. [DOI] [PubMed] [Google Scholar]
- 27.van Dijk IK, 2018. Early-life mortality clustering in families: a literature review. Popul Stud (Camb), May 4: 1–21. [DOI] [PubMed] [Google Scholar]