Abstract
Several studies have shown that epitope vaccines exhibit substantial advantages over conventional vaccines. However, epitope vaccines are associated with limited immunity, which can be overcome by conjugating antigenic epitopes with built-in adjuvants (e.g., some carrier proteins or new biomaterials) with special properties, including immunologic specificity, good biosecurity and biocompatibility, and the ability to vastly improve the immune response of epitope vaccines. When designing epitope vaccines, the following types of built-in adjuvants are typically considered: (1) pattern recognition receptor ligands (i.e., toll-like receptors); (2) virus-like particle carrier platforms; (3) bacterial toxin proteins; and (4) novel potential delivery systems (e.g., self-assembled peptide nanoparticles, lipid core peptides, and polymeric or inorganic nanoparticles). This review primarily discusses the current and prospective applications of these built-in adjuvants (i.e., biological carriers) to provide some references for the future design of epitope-based vaccines.
Keywords: Built-in adjuvants, Epitope-based vaccines, Biological carriers, Nanoparticles
Introduction
Vaccination is a major preventive measure designed to establish specific immune defenses (i.e., antibody or cellular immunity) to protect individuals from infectious diseases. In 1796, the British rural doctor, Edward Jenner, conducted a scientific study on the prevention of smallpox in humans and demonstrated that vaccination with vaccinia virus could prevent smallpox, from which the terms vaccinology and immunology originated (Negahdaripour et al., 2017b). Traditional vaccines typically include inactivated or attenuated vaccines derived by reducing the virulence of the pathogen by physical or chemical methods (Skwarczynski & Toth, 2011a; Karch & Burkhard, 2016). Due to the continuous progress of science and technology (i.e., immunology and molecular biology), subunit vaccines based on short, specific pathogen fragments have undergone increased development to compensate for the shortcomings of traditional vaccines, including low biosafety (reversion to virulence), inefficient cultivation of pathogens, and the occurrence of allergies and autoimmunity (Skwarczynski & Toth, 2014). Moreover, epitope-based vaccines play an important role in current vaccine research and exhibit several advantages over conventional vaccines, including high specificity, good safety, ease of production and storage, and stability. As a result of these advantages, epitope-based vaccines have become an area of growing interest in the field of vaccine research (Skwarczynski & Toth, 2014; Hajighahramani et al., 2017; Nezafat et al., 2016, 2017).
Since antigenic peptides are easily degraded by proteases in the body, it is difficult for the receptors expressed on the immune cells to identify antigen epitopes, and they do not generate a strong immune response to pathogens. An epitope-based vaccine with a reasonable design is composed of epitope peptide/s, a delivery system, and an adjuvant (Rueckert & Guzman, 2012). For multi-epitope vaccines, since the traditional carriers and adjuvants are associated with poor efficacy, vaccine designs with built-in adjuvants have been proposed. Therefore, a built-in adjuvant exhibiting both the functions of a transmission system and a traditional adjuvant, is constructed within the vaccine to improve the immunogenicity of epitope peptides by stimulating the innate immune response required for an adaptive immune response. To achieve this goal, the epitopes are regularly fused with adjuvant proteins (e.g., toll-like receptor (TLR) ligands and proteins that can spontaneously assemble into virus-like particles (VLPs)) or displayed on the surface of some particular biomaterials (e.g., liposomes, gold nanoparticles, and poly(lactic-co-glycolic acid) (PLGA)) and the immunogenicity of the epitopes are significantly increased by this immune complex (Chen et al., 2017; Rueda et al., 2017; Kitaoka et al., 2017; Karuturi et al., 2017). This review primarily introduces the methods for applying built-in adjuvants in the design of epitope-based vaccines, including a few new delivery systems (e.g., dendrimers, self-assembled peptide nanoparticles (SAPNs), and hyperbranched polyglycerol (hbPG)) (Busseron et al., 2013; Glaffig et al., 2015; Indelicato, Burkhard & Twarock, 2017).
Survey Methodology
In this paper, we reviewed articles related to the built-in adjuvants of epitope-based vaccines. All references in this review paper were retrieved using search engines, such as PubMed, Google Scholar. Keywords, including epitope vaccine, built-in adjuvants, biological carriers, and nanoparticles (NPs) were used to search for relevant references.
Major Immunological Concepts of Epitope-Based Subunit Vaccines
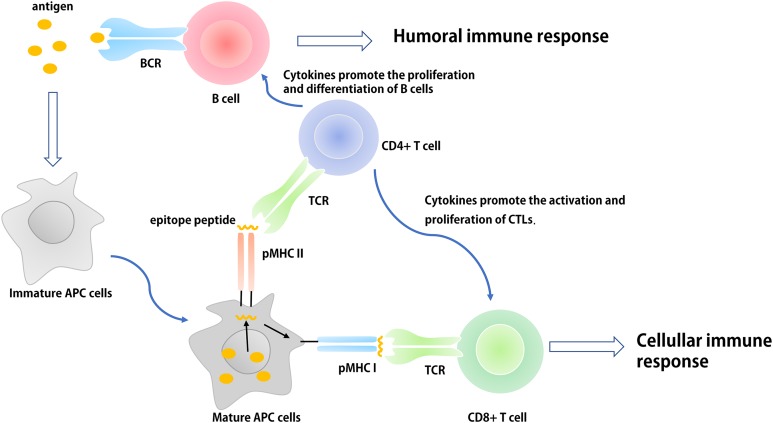
Epitope-based subunit vaccines are typically composed of multiple epitopes derived from one or more pathogenic microorganisms (Azmi et al., 2014; Nezafat et al., 2017). These epitopes are generally composed of B cell epitopes, cytotoxic T cell (CTL) epitopes, and helper T cell (Th) epitopes. B cells identify thymus-dependent antigen through B-cell receptors (BCRs) expressed on their surface. The activation of B cells and the transfer of signals following activation requires two signals: (1) the BCR-specific receptor directly identifies B cell epitopes of the pathogen; and (2) the interaction between multiple co-stimulators on the surface of Th cells and B cells. In addition, activated B cells expressing a variety of cytokine receptors can proliferate in response to cytokines secreted by activated Th cells. The interaction between the specific T cell receptor and the antigen peptide-major histocompatibility complex is known as antigen recognition, which is the first signal required for T cell activation. The interaction between many of the co-stimulatory molecules expressed on the surface of T cells and antigen presentation cells (APCs) (e.g., dendritic cells (DCs)) facilitates the complete activation of T cells. Activated Th1 cells secrete a variety of cytokines (e.g., IL-2, TNF-β, and IFN-γ) some of which (e.g., IL-2) induce non-professional or professional APCs to express co-stimulatory molecules that provide the second signal for the activation of CTLs (Moyle & Toth, 2013; Skwarczynski & Toth, 2014). These cytokines can also promote the activation and proliferation of Th1, Th2, CTL, and natural killer cells, and expand the cellular immune response. Th2 cells further promote the proliferation and differentiation of B cells and assist the humoral immune response by producing cytokines (e.g., IL-4, IL-5, IL-10, and IL-13) and establishing CD40-CD40L connections with B cells (Fig. 1). However, the individual specific epitopes of pathogenic microorganisms are often unable to induce adequate CTL and antibody responses due to a lack of appropriately activated Th cells and pathogen-derived molecules. Therefore, when designing epitope-based vaccines, researchers typically concatenate antigen-specific B cell or CTL epitopes with Th-cell epitopes with appropriate flexible linkers (e.g., GPGPG and EAAK) (Wang et al., 2011, 2018a; Nezafat et al., 2015).
Figure 1. The basic process of immune response in vivo.
The antigen is ingested and processed by immature antigen-presenting cells (e.g., DCs), APCs becomes mature under the action of immune-stimulating molecules. Mature APCs can express antigen information on its surface in the form of antigen peptide-MHC molecular complex and present it to T cells. After recognizing this complex, T cells are activated, proliferated, and differentiated into different subtypes of effector T cells (CD4+ and CD8+) to participate in the regulation of antigen-specific humoral and cellular immune responses.
Innate immune cells (e.g., monocyte-macrophages and DCs) recognize different pathogens through pattern recognition receptors (PRRs). Their antigen-presenting and cytokine regulation effects initiate adaptive immune responses, influence the intensity and type of an adaptive immune response, and participate in the generation of immunological memory. In the design of epitope-based vaccines, researchers generally regard the application of built-in adjuvants as an important platform used to provide suitable Th-cell epitopes for specific pathogens or pathogen related molecular patterns (PAMPs) to activate the innate immune response. Thus, some molecular adjuvants or carriers with no infectious and toxic components can be used as built-in adjuvants to facilitate the presentation of pathogen epitopes to the immune system (Moyle & Toth, 2013; Foged, 2011; Shirbaghaee & Bolhassani, 2016).
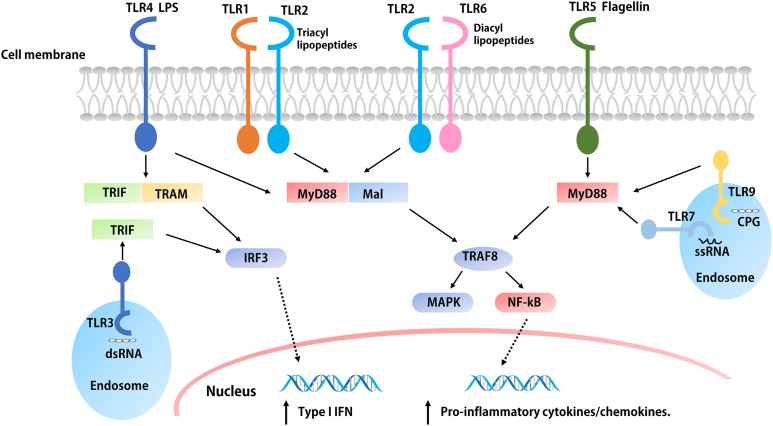
Toll-like Receptor Agonists as Built-in Adjuvants
The development of immunotherapeutic vaccines based on T cell immune responses is essential for the prevention and control of cancer and viral diseases. To achieve this goal, researchers must identify a built-in adjuvant that can stimulate strong Th1 immune responses (Felzmann, Gadner & Holter, 2002). One of the strategies for designing epitope-based vaccines is to use TLR ligands as adjuvants that can polarize CD4+ Th cells and induce CTL responses (Van Der Burg et al., 2006). TLRs are a type of PRR that can both induce an innate immune response and activate the adaptive immune system following PAMP activation (Allison, Benoist & Chervonsky, 2011). To date, researchers have discovered 10 TLRs, termed TLR1–TLR10 (Table 1). TLR ligands are expressed by different microorganisms; for example, bacteria harbor a variety of TLR ligands, including TLR2 (macrophage-activating lipoprotein 2 (MALP-2)); TLR4 (e.g., LPS, HSP, and HBHA), TLR5 (e.g., flagellin), and TLR9 (CpG DNA) ligands (Zhu et al., 2010). The role of TLR10 is to inhibit rather than activate the immune system, and its ligands are poorly understood (Jiang et al., 2016). The extracellular portion of the TLR is activated after binding to an appropriate ligand, and the conformational changes cause convergence of downstream molecules, which triggers associated signaling pathways and induces the up-regulation and activation of cytokines, chemokines, and other costimulatory factors (Dowling & Dellacasagrande, 2016) (Fig. 2). Thus, TLR ligands are promising candidates for the development of novel built-in vaccine adjuvants, which can enhance the immunogenicity of epitope-based vaccines. According to the different biological characteristics of various TLRs, appropriate PAMPs are often selected as the molecular binding proteins of epitope peptides to be used as immune adjuvants (Basto & Leitao, 2014). In this review, several TLR ligands that are often used as built-in adjuvants for epitope vaccines are introduced.
Table 1. Different subtypes of TLRs and their identified PAMPs.
| TLRs | PAMPs | Biological activity | Reference |
|---|---|---|---|
| TLR2/TLR6 TLR2/TLR1 | The lipoproteins of bacteria or mycoplasma. Lipopeptide (MALP-2), Peptidogl, ycan (PGN) | Activate intracellular signal NF-KB, induce adhesion molecules and inflammatory cytokines. | Zhu et al. (2010), Basto & Leitao (2014), Kaisho & Akira (2002) |
| TLR4 | Lipopolysaccharides(LPS), Heat shock protein (HSP), β-defensin, Heparin-binding hemagglutinin(HBHA) | Induce the expression of adhesion molecules and inflammatory cytokines. | Reed et al. (2016), Kaisho & Akira (2002) |
| TLR5 | Gram-negative bacteria flagellin | The potent proinflammatory activity by inducing NF-KB activation, and expression of IL-8 and inducible NO synthase in intestinal epithelial cells. | Kaisho & Akira (2002), Moyle (2017) |
| TLR3 | Double-stranded RNA (ds RNA), Poly(I:C) | Induce IL-12 production and DC maturation and elevate CD40 expression on APCs. | Kaisho & Akira (2002), Cheng et al. (2018) |
| TLR7/TLR8 | Single-stranded RNA (ssRNA) | Induce the expression of adhesion molecules and inflammatory cytokines | Vasilakos & Tomai (2013) |
| TLR9 | CpG DNA, Hemozoin, Herpes simplex virus DNA | Production of Th1 cytokines and promotion of cytotoxic activity of NK cells. | Zhu et al. (2010), Kaisho & Akira (2002) |
Note:
The biological activities of TLRs agonists that can activate the immune system.
Figure 2. The signaling pathways of TLRs.
The extracellular parts of TLRs are activated after binding with ligands, and the conformation changes lead to convergence of downstream molecules, which triggers the signaling pathway and induced the up-regulation and activation of cytokines, chemokines, and other co-stimulatory factors. With the exception of TLR3, all TLRs initiate MyD88 through the expressed MyD88 or simultaneous bridging MAL, and then activate the NF-kB and MAPK through tandem reactions, which induces the production of pro-inflammatory cytokines such as IL-1, IL-6, TNF-α, etc. The overexpression of both TRIF and TRAM or TRIF alone initiated the TRIF dependent pathway, the TRIF dependent pathway activates IFN regulatory factors and mediates the production of type I IFNs. In addition, the activation of TLR4 is related to both pathways.
Lipopeptides
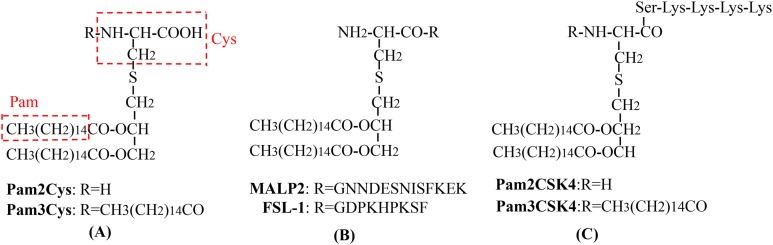
As a lipopeptide derived from mycoplasma and a potential agonist of TLR2/6 heterodimers in DCs (Takeda et al., 2018), MALP-2 is the most widely studied TLR2 adjuvant and has attracted great interest as a novel and efficient built-in adjuvant for vaccines against infectious diseases (McDonald et al., 2014; Muhlradt et al., 1997). MALP-2 has been used in phase I and II trials involving pancreatic cancer patients (Schmidt et al., 2007). McDonald et al. (2014) constructed a variety of self-adjuvating MUC1-MALP-2 conjugate vaccine candidates and demonstrated that the vaccine candidates could induce a high level of humoral immunity without the participation of an external adjuvant and Th epitopes in animal models. Fibroblast stimulating lipopeptide-1 (FSL-1; Pam2CGDPKHPKSF) and synthetic lipopeptide, Pam2CSK4, derived from the LP44 lipoprotein of Mycoplasma salivarium can activate macrophages as a TLR2/TLR6 ligand (Kurkjian et al., 2017; Liu et al., 2016). Liu et al. (2016) used FSL-1 as a built-in adjuvant and synthesized a new type of self-adjuvating (glyco) lipopeptide cancer vaccine. Recently, the TLR2/6 ligand, Pam2CSK4, was used as a Th2 polarizing adjuvant in the study of Leishmania major and Brugia malayi murine vaccines (Halliday et al., 2016). In addition, Pam2CSK4 is also used as an adjuvant for major outer membrane protein antigen of Chlamydia trachomatis to stimulate a robust immune response and induce effective protection against C. muridarum (Cheng et al., 2014a). The Braun Escherichia coli lipoprotein is a prototype composed of the three acylated lipoproteins from the outer membrane of gram-negative bacteria, and some of its synthetic lipopeptides act as TLR2 stimulators (e.g., Pam3CSK4) (Basto & Leitao, 2014; Arai, Inuki & Fujimoto, 2018). Cai et al. (2017) designed and synthesized an HIV-1 glycopeptide immunogen containing a V3 glycan-dependent neutralizing epitope, a universal T helper epitope (P30), and a lipopeptide (Pam3CSK4). After administering the glycopeptide immunogen to rabbits without any additional adjuvants, a glycan-dependent antibody can be produced in a short period of time, and the induced serum antibodies can recognize a wide-range of HIV-1 gp120s across different clades (Cai et al., 2017). Pam2Cys and Pam3Cys are also molecular adjuvants used in vaccines (Zaman & Toth, 2013; McDonald, Byrne & Payne, 2015; Nalla et al., 2015) (Table 2; Fig. 3). Synthetic lipopeptides and their analogues play an important role in the study of built-in adjuvants for epitope-based vaccines. However, compared with mature protein carriers for conjugated vaccines, TLR ligands (e.g., lipopeptides and monophosphoryl lipid A derivatives) are still in their early stages as potential vaccine carriers (Li & Guo, 2018). However, since their interaction with TLRs has been thoroughly studied and understood, the prospective development of epitope-based vaccines using TLR ligands as built-in adjuvants is foreseeable. At present, one of the major challenges is obtaining a sufficient number of vaccines for clinical research since the structure of these lipopeptides, as well as their synthesis and binding to target antigens is highly complex. Semi-total and aminoalkyl glucosaminide 4-phosphates (AGPs) synthesis are important methods that can be used to solve this problem (Li & Guo, 2018; Persing et al., 2002). AGPs have a less-complex structure that allows for synthesis to be easier, more efficient, and elicit immunostimulatory activity in preclinical studies. For example, a Hepatitis B vaccine based on AGP has been approved for use in Argentina (Dupont et al., 2006). A second challenge is how to make full use of all aspects of the multicomponent vaccine structure through reasonable considerations in vaccine design, which can be optimized through structure-activity relationship analysis and molecular modeling (Jin et al., 2007).
Table 2. Various lipopeptides that can be used as build-in adjuvants.
| Name | Natural analogues | Biological activity or structure | Reference |
|---|---|---|---|
| MALP2 | The M161Ag lipoprotein of Mycoplasma fermentans | The agonistic ligand of the TLR2/6 heterodimer. Induces production of inflammatory cytokines from macrophages, monocytes and DCs. MALP2s, a short form of MALP2, lacks the last eight amino acids of the full length MALP2 (Pam2-CGNNDESNISFKEK). As an adjuvant capable of inducing DC maturation, MALP2s can be used in antitumor immunotherapy. |
Takeda et al. (2018), McDonald et al. (2014) |
| FSL-1 | The LP44 lipoprotein from Mycoplasma salivarium | FSL-1 (Pam2CGDPKHPKSF) contains the structure of diacylglycerol similar to Pam2CSK4, which play a key role in immune cell maturation and Th2 immunization and induces the expression of inflammatory cytokines, such as monocyte chemotactic protein (MCP)-1, IL-6, IL-8 and tumor necrosis factor (TNF)-α by monocytes/macrophages. | Liu et al. (2016), Kurkjian et al. (2017) |
| Pam3CSK4 | The Braun lipoprotein in Escherichia coli | Pam3CSK4 is the first mimicking lipopeptide that contains three highly lipophilic tails and six amino acids and can activates the TLR2/1 signaling pathway. | Basto & Leitao (2014), Arai, Inuki & Fujimoto (2018) |
| Pam2CSK4 | The LP44 lipoprotein from Mycoplasma salivarium | The palmityl tail on the N-terminal of cysteine of Pam3CSK4 has been shown to be an dispensable part of TLR2 activation. Removing this lipophilic tail forms a highly effective Pam2CSK4. | Halliday et al. (2016), Arai, Inuki & Fujimoto (2018) |
| Pam3Cys | The Braun lipoprotein in Escherichia coli | Modulation of APC Migration and Antigen Internalization. More efficient than CpG and resiquimod (TLR9 andTLR7/8 ligands). The enantiopure Pam3Cys derivatives that contained R-configured glycerol can induce cytokines and antibody production in mice when administered with antigens. The antigen-specific CTL cells induced by S-epimers were significantly higher in mice. Vaccines containing Pam3Cys can reduce the burden of breast tumors in mice and induce the production of CTLs. |
Zaman & Toth (2013), McDonald, Byrne & Payne (2015) |
| Pam2Cys | Cytoplasmic membrane of Mycoplasma fermentans | Compared with Pam3Cys, Pam2Cys have higher solubility characteristics and is a more potential stimulus factor splenocytes and macrophages. The activity of the natural R isomer of Pam2Cys is 100 times that of S isomer. Dependent on the palm acylated cysteine lipid head group activates downstream signals and activate TLR2 on DC’s and trigger maturation of DCs. | Zaman & Toth (2013), Nalla et al. (2015) |
Note:
The biological activities or structures of various lipopeptides and their natural analogues.
Figure 3. The chemical structures of different TLR2-targeting Pam lipopeptides.
(A) Pam2Cys and Pam3Cys lipopeptides. (B) MALP-2 and FSL-1 lipopeptides. (C) Pam2CSK4 and Pam3CSK4 lipopeptides.
Heat shock proteins
Heat shock proteins (HSPs) are a type of cellular companion protein produced by biological cells that are stimulated by environmental stressors and can be divided into several families, each of which is composed of different members (Juwono & Martinus, 2016; Craig, 2018; Pearl, Prodromou & Workman, 2008; Tang et al., 2005; Bolhassani & Rafati, 2008) (Table 3). HSPs can be internalized by APCs through receptor-mediated endocytosis and can also promote the activity of some cytokines, chemokines, and co-stimulatory molecules through the NF-κB signaling pathway, since HSPs are the molecular chaperones of the antigen epitopes in the APC-MHC I delivery pathway (Robert, 2003; Zachova, Krupka & Raska, 2016). HSPs affect the immune system in different ways because they can act as carriers of antigens, molecular chaperones, and ligands for related receptors (e.g., TLR4) (Moyle, 2017). Among the HSPs, HSP60 obtained from gram-negative bacteria has the ability to stimulate cells of both the innate and acquired immune system, functions as a linker between immune cells, and coordinates immunological activities. Therefore, HSP60 appears to be a promising potential component of subunit vaccines designed to provide protection from infections with gram-negative bacteria (Bajzert et al., 2018). In addition, some researchers have confirmed murine HSP110 (mHSP110) to be a biological adjuvant that significantly enhances the immune response of C57BL/6 mice to the E749–57 or E711–20 epitopes of h-2d restricted human papilloma virus (HPV) (Ding et al., 2013). In addition, the Gp96-peptide complex is considered to be a highly effective stimulator of MHC I-mediated antigen presentation; this strategy makes full use of the built-in adjuvant function and antigen transfer ability of Gp96 to induce cytotoxic immunity against widespread viral or tumor antigens (Strbo et al., 2013).
Table 3. Several major types of heat shock proteins.
| HSP family/members | Intracellular localization | Biological function | Reference |
|---|---|---|---|
| HSP60/HSP58, HSP60, HSP65 | Mitochondrion cytoplasm | It plays a role in the folding of proteins in the mitochondrial matrix. Hsp60 can affect T cell response in two ways: as a ligand of toll-like receptor 2 signalling and as an antigen. |
Juwono & Martinus (2016), Bajzert et al. (2018) |
| HSP70/HSP68, HSP70, HSP72, HSP73 | Cytoplasm or nucleus Mitochondrion Endoplasmic reticulum |
It plays a role in different cell processes, from protein folding to protein complex decomposition and cell membrane protein transfer. Almost every protein that is not folded into its original state has multiple accessible Hsp70 binding sites. It is most commonly used as an adjuvant and protective antigen. | Craig (2018), Cheng et al. (2014b) |
| HSP90/HSP83, HSP84, HSP87, HSP90, Gp96 | Cytoplasm or nucleus Endoplasmic reticulum Golgiosome |
HSP90 regulates the stability of client proteins, activates intracellular division of labor, participates in the regulation of multiple signaling pathways and cell cycle processes, and plays an important role in carcinogenic signal transduction, anti-apoptosis, metastasis, stress injury, autoimmune and other diseases treatment. HSP90 can promote the correct assembly, folding, or restoring the normal conformation of the damaged protein, prevent the wrong folding and aggregation of the protein and also promote the processing of MHC I antigen through the generation and assembly of the antigen determinant cluster of 26s protease complex. | Pearl, Prodromou & Workman (2008), Strbo et al. (2013) |
| HSP110 | Cytoplasm or nucleus | HSP110 has a strong molecular chaperone function and can present antigen peptides to APCs to activate specific antitumor cellular immunity. Moreover, HSP110 can also up-regulate the expression of MHC-II, CD40 and costimulatory molecules of APC, thus enhancing the antigen-presenting ability of APC. | Tang et al. (2005), Ding et al. (2013) |
| Small HSPs/HSP22 HSP23, HSP26, HSP27, HSP28, αβ-crystallin |
Cytoplasm or nucleus Mitochondrion |
Stable cytoskeleton Heme catabolism or antioxygenic property Actin dynamics |
Bolhassani & Rafati (2008) |
Note:
The intracellular localizations and biological functions of several major types of heat shock proteins.
Mycobacterial HSP70 (mHSP70) is widely used as an intramolecular adjuvant for epitope-based vaccines, and the carboxyl terminal polypeptide binding area (HSP70 aa 359–610) of mHSP70 has a stimulating epitope that can combine with the CD40 receptor to stimulate the production of Th1-polarizing cytokines (e.g., IL-12, TNF-α, and NO) to induce DC maturation (Wang et al., 2002; Suzue et al., 1997; Suzue & Young, 1996). Compared with the T cell epitopes of other proteins, the HSP70 T cell epitope can be efficiently processed by APCs, so that the polypeptide binding region of HSP70 has higher affinity with MHC molecules (Basu et al., 2001; Castellino et al., 2000). The single HSP70, which does not fuse with other exogenous epitopes, only induces a very weak cellular and humoral immune response. Some studies have shown that removing the amino end of HSP70 (ATPase domain) and retaining only its carboxyl end (polypeptide binding region) as an antigen can produce a large amount of IL-12, TNF-α, NO, and chemokines (Fu et al., 2013). In contrast, neither the ATPase domain nor native HSP70 can induce such a powerful immune response (Cheng et al., 2014b; Li et al., 2006; Ge et al., 2006). For example, the fusion of the hantavirus glycoprotein (GP) and nucleocapsid protein with the carboxyl end of HSP70 can induce a more specific immune response (Cheng et al., 2014b). The major antigenic segment of the Japanese encephalitis virus E protein can fuse with the amino terminus of the peptide binding domain of HSP70, which can induce a more effective immune response than the major antigenic segment of the E protein alone (Ge et al., 2006). HSP70s and HSP90s have been also found to act as carriers of tumor-derived peptides, adjuvants for antigen presentation, and can target the innate immune system by inducing anti-tumor immune responses (Shevtsov & Multhoff, 2016).
Heparin-binding hemagglutinin
With regards to Mycobacterium tuberculosis antigens, several Mycobacterium lipid and glycolipid antigens (e.g., mycolic acid, lipoarabinomannan, glucose monomycolate) can be recognized by specific T cells by the CD1 antigen-presentation pathway in humans, suggesting the possible application of Mycobacterium tuberculosis lipid molecules in subunit vaccine preparation (Moody et al., 2000). Dascher et al. (2003) developed a vaccine which included lipids from Mycobacterium tuberculosis that were incorporated into liposomes with an adjuvant; the studies using a guinea pig aerosol tuberculosis challenge model demonstrated that lipid antigens play an important role in the immune response to tuberculosis infection, potentially through the production of CD1-restricted T cells. In addition, the Mycobacterium tuberculosis 6-kilodalton early secreted antigenic target protein (ESAT-6) is considered to be an important mediator in mycobacterial virulence, has strong antigenicity, and can induce a protective Th1 immune response against Mycobacterium tuberculosis (Pandey et al., 2018). Khader et al. (2007) vaccinated mice with an ESAT-6 peptide (amino acids 1–20 of ESAT-6) in an adjuvant composed of MPLA, trehalose dicorynomycolate, and dimethyl dioctadecylammonium bromide. The vaccination was found to induce antigen-specific T cells that produced IFN-γ, T cells that persisted in the central lymphoid organs, and antigen-specific IL-17-producing T cells that persisted in the lung (Khader et al., 2007). Recently, heparin-binding hemagglutinin (HBHA), a component of Mycobacterium tuberculosis, has been closely investigated for its strong immune potential, which can stimulate the migration of DCs and promote the expression of a variety of surface molecules (e.g., CD40, CD80, and CD86), MHC I and MHC II molecules, as well as inflammatory cytokines (e.g., IL-6, IL-12, IL-1β, and TNF-α) in a TLR4-dependent manner (Jung et al., 2011; Eraghi et al., 2017). For example, HBHA can induce immunological protection against Mycobacterium tuberculosis by stimulating the production of IFN-γ, IL-2, and IL-17-coexpressing CD4+ T cells (Fukui et al., 2015). As an effective immune adjuvant, HBHA can induce a strong Th1 cell immune response and plays an important role in the research of multi-epitope vaccines for immunotherapy (i.e., tumor vaccines). It has also been reported that the amino acid sequence of the epitope for the MAP1611 immunization region of the Mycobacterium avium subsp., paratuberculosis multiple antigenic peptide (MAP), is connected to the conservative amino acid sequence of HBHA. In addition, this recombinant subunit vaccine exhibited good immunogenicity and was identified to have a no allergenicity as predicted by employing a hybrid approach using the AlgPred program (Rana, Rub & Akhter, 2014; Rana & Akhter, 2016). Some researchers have designed a multi-epitope vaccine that includes CTL epitopes of Wilms tumor-1 and HPV E7 antigens, helper T lymphocyte epitopes of the tetanus toxin fragment C (TTFrC) and HLA PADRE, and HBHA as the intramolecular adjuvant of epitope-based vaccines and is connected with appropriate linkers to enhance the effect of this recombinant multiple-epitope vaccine against cancer (Nezafat et al., 2014, 2015). As a built-in adjuvant with a powerful immune enhancement effect, HBHA is rarely used in epitope vaccine research and is worthy of further study in the development of antiviral and cancer epitope-based vaccines.
Bacterial flagellin
Flagellins are TLR5 and NOD receptor ligands that can activate both innate and acquired immune cells (Huleatt et al., 2008; Wang et al., 2014; Hajam et al., 2017). Both the N- and C-terminals of flagellin are composed of conservative alpha helices that function as TLR5 recognition sites, and the portion between the N- and C-terminals comprises a highly variable flagellin antigen region (Murthy et al., 2004). It has been found that deletion of part of the highly variable region of flagellin disables the ability of the host to produce antibodies against bacterial flagellum but does not affect its adjuvant activity (Deng et al., 2017). Therefore, researchers typically replace this region with exogenous antigen epitopes (e.g., the HPV prophylactic peptide vaccine) (Nempont et al., 2008; Negahdaripour et al., 2017a). For example, replacing the FliC variable region with the M2e protein of influenza A does not obstruct TLR signaling pathways (Smith et al., 2003; Deng et al., 2017). A truncated flagellin (tFL) with deletion of the hypervariable regions was used as a carrier by chemical conjugation with a malaria antigen M.RCAg-1 (M312), and compared with the physical mixture of M312 and tFL, the conjugates M312-PEG-tFL elicited higher M312-specific antibody titers (Guo et al., 2018). In addition, two HPV epitopes and some universal Th epitopes have been linked to the different flagellin positions via different linkers, and the optimal construction of a multiepitope vaccine was screened using protein structure analysis, modeling, optimization, and an evaluation of immunogenicity (Negahdaripour et al., 2018). In addition, four copies of the ectodomain of matrix protein 2 (f4M2e) of the influenza A virus (IAV), H1, HA2 domain (fHApr8), or H3 HA2 domain (fHAaichi) were used to replace the high immunogenicity region of flagellin, and the fusion proteins were crosslinked with propionate (DTSSP) to form protein NPs, thereby retaining the agonist activity of FliC to TLR5, and ability to assist the epitope protein in stimulating the immune response against IAV (Deng et al., 2017). The combination of flagellin with multiple copies of HPV L2 neutralization epitopes have demonstrated a strong broad spectrum anti-HPV effect without the participation of other adjuvants, thus demonstrating a significant advantage of this strategy in enhancing the cross-protection of the HPV vaccine (Kalnin et al., 2014, 2017; Gambhira et al., 2007). In addition, Ajamian et al. (2018) found that inserting the HIV gp41607–683 (MPER) into a flagellin-based scaffold could significantly enhance the immunogenicity of gp41607–683 in a TLR5-dependent manner and induce strong humoral responses specific to MPER in a mouse model. Various flagellin antigen fusion proteins have been studied in human clinical trials. Furthermore, flagellin is also commonly used as an antigen skeleton of SAPN-based vaccines (El et al., 2017), for which the associated content is described below.
Outer membrane vesicles
Outer membrane vesicles (OMVs) are naturally secreted on the surface of most gram-negative bacteria, and the vesicle membrane typically consists of lipopolysaccharide (LPS), glycerophospholipids, and outer membrane proteins (OMPs) (Tan et al., 2018). Due to their intact outer membrane and periplasmic contents, OMVs possess good intrinsic stimulation ability and strong immunoreactivity, which can induce strong humoral and cellular immune responses. In addition to research focused on the possibility of using OMVs as candidate antigens for vaccine development, there is growing interest in the application of OMVs as a self-adjuvant for immunostimulatory molecules. This function is mediated by the interaction between the OMV-associated PAMPs and the TLRs expressed on the surface of APCs, thus enhancing the immune response to exogenous antigens (Gnopo et al., 2017). OMVs can also even be used as a mucosal transporter to transport antigens to the mucosal barriers (Jang et al., 2004). In addition, designed glycoengineered OMVs, which can display the O-antigen and surface glycans from different bacteria could be used as bacterial vaccine platforms to prevent bacterial infections (Valguarnera & Feldman, 2017). In addition, plasmids can be transported into OMVs to further modify the intracavity content, including LPS functionality and attenuate toxicity (Tan et al., 2018). Hekmat et al. (2018) developed a novel hepatitis C virus (HCV) therapeutic vaccine candidate, rC/N-NMB OMVs, formulated as a targeted synthesized recombinant fusion protein consisting of a truncated core and NS3 (rC/N) of HCV as a bipartite antigen accompanied by Neisseria meningitidis serogroup B OMVs (NMB OMVs), has the ability to induce Th1, Th2, and Th17 immune responses. Compared with MF59 and Freund adjuvant, NMB OMVs can significantly increase the level of Th1 immune responses (Hekmat et al., 2018). Liu et al. (2018) have demonstrated OMVs from flagellin-deficient Salmonella Typhimurium can serve as an adjuvant when combined with OMPs from different Salmonella serotypes, and enhances the cross-protection capacity of this combined vaccine. Additionally, novel vaccine adjuvant OMVs have been reported, which can serve as delivery carriers to improve vaccine safety and protective efficacy. ClyA is a 34 kDa pore-forming toxin enriched on OMVs, for which exogenous antigens are fused at the C terminus of ClyA to produce ClyA-antigen fusion proteins on OMVs (Kim et al., 2008). Chen et al. (2010) demonstrated that rOMVs carrying ClyA-GFP fusion proteins could induce a high level of anti-GFP IgG titers in mice, which was similar to that of GFP adjuvanted with alum. Rappazzo et al. (2016) immunized mice with ClyA-M2e4xHet OMVs displaying an influenza-derived antigen, M2e4xHet, which was associated with 100% survival following subsequent influenza challenge. In addition to ClyA, other prospective proteins also have the potential to display an antigen of interest, such as the hemoglobin protease (Hbp) autotransporter platform (Daleke-Schermerhorn et al., 2014). Jong et al. (2014) introduced a mutation to preserve the integrity of Hbp to avoid cleavage following translocation to the outer membrane. Kuipers et al. (2015) demonstrated that rOMVs displaying the pneumococcal antigens, pneumococcal surface protein A and pneumolysin, by the Hbp system could prevent pneumococcal colonization. Although some obstacles to the development of OMV adjuvants remain (e.g., large number of clinical and preclinical assessments, and limited knowledge of the OMV manufacturing process), we believe that the use of OMVs as an epitope-based vaccine delivery system would also be of great value in controlling all types of pathogen infections due to their comprehensive immune potency, higher safety, and substantial mucosal delivery efficacy (Tan et al., 2018).
In addition, generalized modules for membrane antigens (GMMA) as an OMV technology are outer membrane particles consisting of outer membrane lipids, OMPs, and soluble periplasmic components (Gerke et al., 2015). GMMA are derived from gram-negative bacteria (i.e., Salmonella and Shigella) which are genetically modified (deletion of the tolR gene) to enhance the associated advantages of being cost-effective with high-production yields. Further gene deletions (i.e., the late acyltransferases genes HtrB175 and MsbB) resulted in GMMA with penta-acylated LPS with no possibility of infection (Rossi et al., 2014). Due to the self-adjuvanting properties of GMMA that deliver innate immune signaling through PAMPs (i.e., TLR ligands), many studies have shown that GMMA vaccines can simultaneously deliver surface polysaccharides and OMPs to the immune system and display greater immunogenicity compared to glycoconjugate vaccines (Micoli et al., 2018; MacLennan, Martin & Micoli, 2014). Moreover, it has been demonstrated that the GMMA technique can be used as a carrier to display the salmonella LPS O-antigen to the immune system. It is envisaged that GMMA could also be considered as a built-in adjuvant platform for epitope-based vaccines against pathogens other than gram-negative bacteria. More importantly, clinical trials (currently under way with Shigella sonnei GMMA vaccines) are required to further assess the safety and tolerance of this vaccine platform in humans.
Salmonella porin
Salmonella Typhi expresses a variety of porins. While the major S. Typhi OmpC and OmpF porins can be expressed constitutively, the expression of other porins (e.g., OmpS1 and OmpS2) is relatively low in vitro and during potential infection (Perez-Toledo et al., 2017). Both the major and minor S. Typhi porins can effectively activate the innate immune system through the TLR2 and TLR4 signaling pathways, resulting in the increased expression of costimulatory molecules and cytokines in DCs and B cells (Moreno-Eutimio et al., 2013; Cervantes-Barragan et al., 2009). Due to such immune-activating properties, some of these porins have been used as potential vaccine adjuvants. Perez-Toledo et al. (2017) have shown that the S. Typhi porins, OmpC and OmpF, are multipurpose vaccine adjuvants, which can be used to polarize the T cell response toward a Th1/Th17 profile and enhance the antibody response generated toward T-dependent and T-independent antigens with poor immunogenicity. In addition, Leclerc et al. (2013) used malva mosaic virus NPs as a vaccine platform to improve the stability of the M2e peptide of influenza A in conjunction with OmpC purified from Salmonella typhi as an adjuvant; their data demonstrate that OmpC increased the immune response to the M2e peptide and provided protection against a heterosubtypic influenza strain in a mouse model. Moreover, Moreno-Eutimio et al. (2013) investigated the immunogenic and protective capacities of the OmpS1 and OmpS2 porins and determined that these porins can be potent inducers of the innate immune response, exhibiting adjuvant properties that can promote increased antibody titers and long-term antibody responses when co-immunized with antigens.
β-Defensin
β-Defensins are antimicrobial peptides involved in the innate immune response of the host and are responsible for stimulating innate and adaptive immune responses by recruiting naïve T cells and immature DCs through interactions with corresponding immune receptors (e.g., CCR6 or TLRs) (Narula et al., 2018). Kim et al. (2018) have concluded that human β-defensin 2 can induce the primary antiviral innate immune response and may also mediate the induction of antigen-specific immune response against a conjugated antigen. Using immunoinformatic methods, a multi-epitope vaccine for dengue was developed that included Tc and Th cell epitopes with β-defensin included as a molecular adjuvant at the N-terminal of the construct (Ali et al., 2017). Similarly, researchers developed an anti-chikungunya multi-epitope vaccine that included B cell and T cell-binding epitopes and IFN-γ inducing epitopes with β-defensin added as a built-in adjuvant (Narula et al., 2018).
Virus-like Particles as Built-in Adjuvant Platforms
Hepatitis B virus core antigen
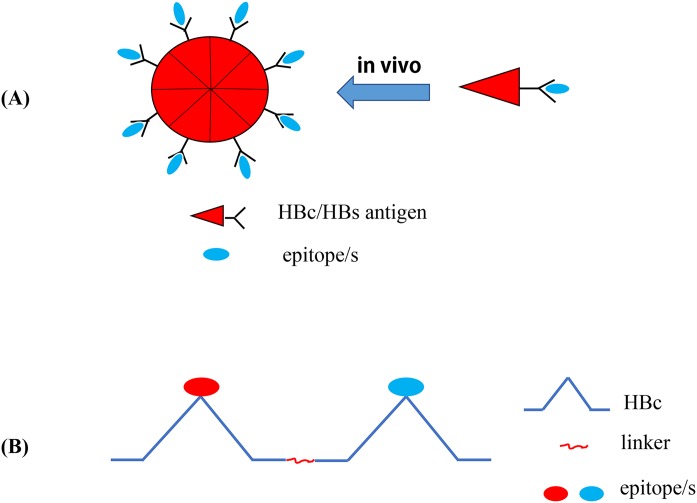
Hepatitis B virus core antigen can act both as a Th cell-dependent or Th cell-independent antigen (Roose et al., 2013), and the Th-priming effects of HBcAg can easily transfer the adaptive response to the inserted related epitopes (Milich et al., 1987). In addition, the nanoscale structure of HBcAg can be more effectively identified and processed by APCs (Lee et al., 2009; Ong, Tan & Ho, 2017). Therefore, HBcAg has been used as an vaccine carrier for several exogenous pathogens (e.g., hepatitis B, C, and E virus, influenza virus, foot-and-mouth disease virus, Human enterovirus 71, coxsackievirus A16, and C. trachomatis), and the immunogenicity of recombinant HBc-based VLP vaccines against pathogens has also been verified in animal models (Dai et al., 2016; Su et al., 2013; Zheng et al., 2016; Chu et al., 2016; Zhu et al., 2016; Wu et al., 2017; Jiang et al., 2017). VLPs are the self-assembled structural proteins of most viruses and can stimulate the immune response in the absence of an adjuvant by exposing pathogen epitopes and simulating the structure of natural viruses (Plummer & Manchester, 2011; Yang et al., 2016). In addition, VLPs can stimulate an innate immune response by activating PRRs (e.g., TLRs) (Shirbaghaee & Bolhassani, 2016). In addition, the autoantigen molecules displayed by HBcAg VLPs can escape immune tolerance and produce specific auto-antibodies (Long et al., 2014). Due to these advantages, the HBc is often used as a powerful carrier protein and built-in adjuvant to display exogenous epitopes (Chen et al., 2017; Jiang et al., 2017; Roose et al., 2013; Liang et al., 2018). In general, researchers will insert pathogen epitopes into the HBcAg major immunogenic region (MIR; HBcAg aa 78–82 in the spike tip of HBV), which does not affect the self-assembly of the fusion protein into VLP NPs, to generate immune activation; therefore, antigen epitopes will be presented on the surface of the particles (Wang et al., 2017a; Chen et al., 2017) (Fig. 4A). As the main insertion site of exogenous epitopes, MIR can significantly enhance the immunogenicity of such epitopes (Dai et al., 2016; Reynolds et al., 2015). Recently, Wu et al. (2017) developed a novel vaccine against chickenpox and hand-foot-mouth disease by constructing three VLPs with HBcAg used as a carrier protein, and epitopes derived from varicella-zoster virus-gE, EV71 (enterovirus71)-VP1, and EV71-VP2 were displayed by HBcAg. This study also fully demonstrated the significant potential of HBcAg as a carrier protein for epitope vaccines used in multivalent epitope vaccine research (Wu et al., 2017). The tandem core (TC) contains two HBcAg molecules that are connected by the appropriate linker and has two independent MIRs which can individually accommodate multiple exogenous antigens (Fig. 4B). This VLP platform is associated with beneficial prospects for the development of multivalent vaccines (Roose et al., 2013). Alejandro et al. inserted the four conserved antigenic regions of the matrix protein 2 ectodomain and hemagglutinin stalk of an existing IAV into the MIR region of TC, thereby constructing a VLP vaccine called Tandiflu1, which can induce the production of cross-protective antibodies (Ramirez et al., 2018).
Figure 4. Recombinant HBc-based VLPs or HBs-based VLPs.
(A) (1) The HBc proteins naturally form the dimers, the building blocks that forms the VLPs. It takes about 60 such dimers (i.e., 120 copies of HBc) to form a HBc-based VLP. The results showed that there were about 40 amino acid residues inserted into the N-terminal of HBc. In the MIR region of HBc, 50 or 100 amino acid residues can be inserted, and as many as 100 or more residues at the C-terminal do not interfere with the formation of particles. (2) Hepatitis B surface antigen (HBsAg) can also self-assemble into highly organized viroid particles with a diameter of 22 nm. These HBs-derived VLPs contain about 100 HBsAg molecules and provide a unique opportunity to display multiple exogenous epitopes. (B) Hepatitis B virus tandem core platform. The two replicas of HBc protein are linked together by covalent bonds through flexible amino acid sequences so that the fused dimers can be folded correctly and assembled into HBc particles. In the assembled HBc particles, the four helix bundles formed at each dimer interface appear on the surface as prominent “spikes”. The tip of the spike is the preferred site for inserting foreign sequences for bivalent vaccine.
Hepatitis B virus surface antigen
The tertiary structure of hepatitis B virus surface antigen (HBsAg) can form a highly conserved hydrophilic loop. Additionally, it has been reported that the existing immunity to HBsAg does not impede the immune response to foreign epitopes carried by HBsAg particles, which is often used as a carrier to insert exogenous antigens into the external hydrophilic loop or the end of the HBsAg N- or C-terminal (Bellier & Klatzmann, 2013). Czarnota et al. (2016) inserted a highly conserved epitope (amino acid residues 412–425) of the HCV E2 GP into the hydrophobic loop of HBsAg, and the chimeric protein was then expressed in an unconventional Leishmania tarentolae expression system and independently assembled into VLPs, which demonstrated high immunogenicity and induced cross-reactive antibodies against HCV (Czarnota et al., 2016). Wei et al. (2018) also used HBsAg to display neutralizing HCV epitopes to obtain chimeric HCV–HBV VLPs as a novel strategy for developing a bivalent prophylactic HCV–HBV epitope vaccine (Wei et al., 2018). The envelope protein domain III (EDIII) of dengue viruses (DENV) contains good serotype-specificity and cross-reactive epitopes. Ramasamy et al. (2018) fused the EDIII of all four DENV serotypes with four copies of HBsAg and expressed the construct in the P. pastoris GS115 strain to obtain a tetravalent VLP vaccine termed DSV4, which has a high immunogenicity and produces effective and persistent neutralizing antibodies against all four DENV serotypes in mice.
Phage-based VLPs
The over-expression of the single-chain dimer coat proteins (CPs) of MS2 and PP7 RNA phages in bacteria can spontaneously assemble into recombinant MS2 or PP7 VLPs containing 90 dimer copies and 90 exogenous epitopes. In addition, for the Qβ bacteriophage, 180 copies of single-chain dimer capsid proteins can spontaneously assemble into a VLP; thus, at least 180 exogenous epitopes can be displayed on the surface of a Qβ VLP (Basu et al., 2018). Recent reports have shown that the Qβ bacteriophage contains TLR ligands that can enhance Qβ-VLP-induced T cell-independent and -dependent Ab reactions, including a germinal center reaction via of TLR/MyD88 signaling in B cells (Tian et al., 2018). This VLP platform which contains no viral genome can be used in the future as a carrier system for the administration of safe vaccines against many pathogens (Pumpens et al., 2016). Basu et al. (2018) described potential B cell epitopes located on the envelope proteins of Zika virus on the surface of a highly immunogenic bacteriophage VLP platform (MS2, PP7, and Qβ), and evaluated the immunogenicity of these VLPs in mice. Zhai et al. (2017) also displayed consensus peptides from HPV L2 and tandem HPV31/16L2 peptides on the surface of bacteriophage MS2 VLPs. These MS2-L2 VLPs can induce high antibody titers in mice and are cost-effective vaccine candidates against HPV; however, HPV vaccines with greater cross-protection should be further evaluated to prevent more types of HPV (Zhai et al., 2017). Recently, Qβ VLPs have been applied as carriers for the development of carbohydrate-based anticancer vaccines (Sungsuwan, Wu & Huang, 2017). Additionally, researchers have developed a size-exclusion chromatography-based purification method for an VLP-based influenza A vaccine derived from the MS2 phage that displays an epitope from the extracellular domain of the IAV matrix two protein. Moreover, the purification procedure provides an improved strategy for the future large-scale production of VLP-based epitope vaccines (Lagoutte et al., 2016).
Tobacco mosaic virus
Tobacco mosaic virus (TMV) is a widely studied and identified filamentous plant virus. TMV particles are hollow with tubular rods (300 nm length × 18 nm diameter) consisting of about 2,130 CP subunits encase a single-stranded, plus-sense RNA genome (Culver, 2002). As an antigen carrier, TMV has two important functions: (1) due to the architecture and size of TMV, TMV carrying antigen epitopes is robustly and readily taken up by DCs, leading to the activation of key surface markers (Smith et al., 2007); and (2) TMV also provides adjuvant effects, due to either repetitive antigen displayed on the surfaces of TMV or the presence of non-functional viral RNA that is important for inducing cellular-mediated immunity (Banik et al., 2015). Kemnade et al. (2014) demonstrated that TMV is capable of boosting TMV-induced antigen-specific T cell responses, but does not induce neutralizing self-immunity. In addition, since TMV is not a human pathogen, it is intrinsically secure (Liu et al., 2013). These findings further confirm that TMV has great potential as an epitope-based vaccine vector. McCormick et al. (2006) fused well-characterized T cell epitopes that provide protection against tumor challenge in mice into a TMV CP and demonstrated that C57BL/6 mice inoculated with TMV displayed significantly improved protection against tumor challenge in both the EG.7-Ova and B16 melanoma models. Moreover, Zhao et al. (2015) reported that when efficient copper (I)-catalyzed azide–alkyne cycloaddition reaction was performed for the conjugation of the small molecule estriol (E3) onto TMV capsid, TMV can induce a strong and long-term antibody response. Furthermore, Banik et al. (2015) developed a multivalent subunit vaccine against tularemia using a TMV-based delivery platform and demonstrated TMV can serve as a suitable built-in adjuvant for multiple protective antigens (PAs) of F. tularensis, as well as induce cell-mediated immune responses and long-lasting humoral immunity against tularemia.
Papaya mosaic virus
As a member of the potexvirus family, papaya mosaic virus (PapMV) displays a flexible rod-like structure composed of 1,400 subunits of the viral CP assembled around a positive-strand RNA (Lacasse et al., 2008). Since PapMV-based VLPs comprised of PapMV CPs assembled around an ssRNA can efficiently trigger an innate immune response, they can be used as a vaccine adjuvant platform. Following phagocytosis, PapMV-based VLPs can reach the endosome of immune cells and release ssRNA, which engages and activates TLR7 (Therien et al., 2017). The direct fusion of antigenic peptides to the open reading frame (ORF) of the PapMV CP can lead to the formation of chimeric VLPs that can trigger a humoral or CTL response against the fused antigen (Bolduc et al., 2018). Additionally, Carignan et al. (2015) have shown that the fusion of a short M2e (sM2e) epitope (nine amino acids) to the N-terminus of the PapMV CP allows for the assembly of highly immunogenic VLPs. This group further demonstrated that an intramuscular injection of PapMV-sM2e VLPs is sufficient to induce a powerful anti-M2e humoral response that protects mice against subsequent challenge with influenza A. Similarly, Bolduc et al. (2018) have developed a PapMV-based VLP vaccine candidate capable of inducing robust and broad protection against two different influenza A strains (H1N1 and H3N2). Lacasse et al. (2008) have shown that PapMV VLPs carrying the H-2b-restricted dominant p33 CTL epitope from the lymphocytic choriomeningitis virus can induce DC maturation and cross-presentation of the p33 CTL epitope, which triggers a protective antiviral T cell response. Furthermore, Therien et al. (2017) engineered a PapMV-based VLP platform with a SrtA receptor motif and allowed SrtA to attach to the long peptides of the VLPs. This approach was found to be more versatile than the fusion of only small peptides to the ORF of the PapMV CP. Therefore, PapMV NPs with SrtA-conjugated peptide antigens may represent a promising tool in vaccine design against various diseases (Therien et al., 2017).
Keyhole Limpet Hemocyanin and Bovine Serum Albumin
Keyhole limpet hemocyanin (KLH) and bovine serum albumin (BSA) are easily identified by the immune system as non-self components, which is useful for enhancing the immunogenicity of small antigens or a low antigen dose. KLH and BSA are easily processed APCs and can recruit Th cells to assist in antigen uptake (Mora et al., 2017). These characteristics of KLH and BSA have promoted their frequent use as epitope carrier proteins. For example, researchers have developed the novel epitope peptide vaccine, Aβ3-10-KLH, by coupling the B cell epitope, Aβ3-10, from amyloid-β peptide (Aβ) with KLH, for the potential treatment and prevention of Alzheimer’s disease (AD) (Ding et al., 2016, 2017a). In another study, an anti-PCSK9 (proprotein convertase subtilisin/kexin type 9) peptide vaccine using KLH as the carrier protein was shown to produce long-lasting anti-PCSK9 antibodies and is considered to be the primary vaccine for the treatment of dyslipidemia in the future (Kawakami et al., 2018). In addition, a short peptide (UPK3A 65-84) from Uroplakin 3A (UPK3A) covalently coupled with KLH and CpG as adjuvant was found to be an immunotherapeutic vaccine for bladder cancer (Izgi et al., 2015). In addition, BSA is often used as a carrier protein for small antigens in glycoconjugate vaccines (Prasanphanich et al., 2015). For example, Cai et al. (2013) combined a synthesized MUC1 glycopeptide with BSA or three different T-helper cell epitopes of TTox and demonstrated a beneficial effect. Furthermore, the immune complex formed by coupling the synthetic trisaccharide Galα(1,3)Galβ(1,4)GlcNAcα of Trypanosoma cruzi with BSA as a carrier protein was reported to be a vaccine candidate for Chagas disease (Schocker et al., 2016).
Bacterial Toxin Proteins
Heat-labile toxins and cholera toxin
Heat-labile toxins (HLTs) are produced by some enterotoxigenic E. coli strains and can be fused with other antigenic proteins to function as an adjuvant (Da et al., 2011; Luiz et al., 2015; Hu et al., 2014) (Table 4). HLTs and cholera toxins (CTs) are highly homologous, consisting of five subunit-Bs and one subunit-A, and are members of the bacterial protein toxin AB5 family. Subunit-A is a toxic subunit, noncovalently bound to the B pentamer and has ADP ribosyltransferase activity, whereas subunit-B is a nontoxic receptor-binding subunit (Lencer, Hirst & Holmes, 1999). Generally, non-toxic HLTs (e.g., subunit-B and mutant forms of HLT) also act as immune adjuvants to activate DCs, B cells, and T cells, regulate epitope specificity, and improve the immune response (Batista et al., 2014; Rodrigues et al., 2011). The fusion of the HLT B subunit (HLTB) with the linear B cell epitope of the outer membrane protein (OmpC) of Aeromonas hydrophila can stimulate the production of neutralizing antibodies against this linear epitope and generate a Th2 type mixed auxiliary T cell immune response (Sharma et al., 2017). The two epitopes of the Zairian Ebola virus GP1 protein, which can be recognized by neutralizing antibodies, were coupled with HLTB protein to form recombinant antigen HLTB-EBOV expressed in plant tissues, and immunizing mice with the recombinant antigen presented by the plant induced a higher level of IgA and IgG responses (Rios-Huerta et al., 2017). The CT subunit-B (CTB) can be used as a powerful adjuvant to generate mucosal immunity due to its strong affinity to the GM1 ganglioside receptor which is primarily located on mucosal epithelial cells (i.e., M cells) (Pinkhasov et al., 2010). The multivalent epitope-based vaccine against Helicobacter pylori, CWAE, and an anti-atherosclerosis multi-epitope vaccine have been developed using CTB as intramolecular adjuvant (Tourani, Karkhah & Najafi, 2017; Guo et al., 2017).
Table 4. Summary of several bacterial toxin build-in adjuvants listed in this paper.
| Objective | Advantages and characteristics | Application example | Reference |
|---|---|---|---|
| Heat labile toxins (HLT) |
|
|
Rodrigues et al. (2011), Sharma et al. (2017), Rios-Huerta et al. (2017) |
| Cholera toxin (CT) |
|
|
Guo et al. (2017), Tourani, Karkhah & Najafi (2017) |
| Diphtheria toxin (DT) |
|
|
Tobias et al. (2017), Zhang et al. (2016) |
| Tetanus toxoid (TT) |
|
|
Saadi, Karkhah & Nouri (2017), Broker (2016), Arcuri et al. (2017) |
| Anthrax toxin |
|
|
Wesche et al. (1998), Shaw & Starnbach (2008), Chandra et al. (2006) |
Note:
The advantages and characteristics and some application examples of several bacterial toxin build-in adjuvants.
Diphtheria toxin
The carrier protein cross-reacting material 197 (CRM197) is an inactivated and non-toxic form of diphtheria toxin (DTT) created using an enzymatic reaction, and has been successfully applied in many vaccines against infectious diseases because it can effectively combine and present peptides (Caro-Aguilar et al., 2013) (Table 4). Moreover, CRM can rapidly activate CD4+ T cells by generating a multitude of Th1 and Th2 cytokines, thereby promoting the proliferation of B cells and regulating the level of antibody production (Kamboj et al., 2001). Several short B cell epitopes (P4, P6, and P7) on the Her-2/neu protein were combined with the polyepitope peptide, P467, using CRM197 as a carrier protein to conjugate with this complex epitope, demonstrated a strong anti-tumor response (Tobias et al., 2017). The function of DTT is to assist the enzyme active region (C-domain) in passing through the endocytosis membrane, and there are no associated risks when the transmembrane domain of DTT is used as the protein carrier for exogenous antigen (Ladokhin, 2013; Malito et al., 2012). Xu et al. (2017) developed a vascular endothelial growth factor (VEGF)-based antigen DTT-VEGF consisting of the receptor-binding domain of VEGF and DTT stimulated neutralizing antibody response and induced type 1 immune response as well as anti-tumor CTLs in mice, and their data demonstrated that DTT is an effective antigen carrier to break immune self-tolerance and DTT-VEGF has potential to be used a promising cancer vaccine. In addition, DTT contains four Th cell epitopes (aa 69–88, 119–138, 129–148, and 149–168) and the 89–96 amino acid residues form a turn-helix-turn structure that is completely exposed to the surface, which may be a potential site for the insertion of exogenous epitopes (Diethelm-Okita et al., 2000). For individuals who have been previously vaccinated with the DTT vaccine, the Th cell epitopes based on the DTT vaccine will induce a rapid CD4+ memory T cell response (Fraser et al., 2014). For example, a TNF-α epitope has been coupled to the insertion site of DTT to develop an anti-TNF-α vaccine, DTNF, demonstrating the potential advantage of a DTT-based epitope vaccine gainst autoimmune diseases (Zhang et al., 2016).
Tetanus toxoid
Since tetanus toxoid (TT) is a carrier protein possessing multiple CD4+ Th cell epitopes and is associated memory Th subsets, it can be recognized by APCs and presented to CD4+ Th cells (Table 4). As mentioned previously, these Th cells can provide the second signal required for B cell activation (Van Der Heiden et al., 2017; Da et al., 2017). Recently, it has been reported that a new type of anti-gastrin vaccine using TT as a carrier protein for multiple complex antigens can significantly enhance the immunogenicity of the vaccine (He et al., 2018). Jarzab et al. (2018) used TT as the carrier protein for the several synthetic linear or cyclic OmpC epitope peptides and demonstrated that cyclic peptide conjugated to TT as a potential candidate gainst shigellosis. Helper epitopes selected from TTFrC are typically associated with the target epitope to stimulate a CD4+ T cell response (e.g., anti-brucellosis and anti-atherosclerosis multi-epitope vaccines) (Saadi, Karkhah & Nouri, 2017; Tourani, Karkhah & Najafi, 2017). TT is also commonly used as a carrier protein for glycoconjugate vaccines (Broker, 2016). For example, the Vi polysaccharide of typhoid has been combined with TT via chemical bonding to compare the immunogenicity with that of diphtheria toxoid (DT) and CRM197 as a carrier protein (Arcuri et al., 2017).
Anthrax toxin
The lethal toxin produced by Bacillus anthracis is a bipartite toxin consisting of PA as the cell binding moiety and lethal factor (LF) as the effector component. PA has the inherent ability to transport the enzymatically active LF across the host cell membrane into the cytoplasm, leading to the death of the host cell (Liu et al., 2017). PA binds to receptors on host cells, and the resulting PA heptopolymer can bind to three LF molecules. Subsequently, the entire toxin complex is endocytosed by cells. PA undergoes conformational changes due to endocytosis-associated acidification, resulting in transmembrane pores which can facilitate the translocation of LF molecules from the endosome into the cytosol (Shaw & Starnbach, 2008; Arora, Misra & Sajid, 2017). The N-terminal (the first 255 amino acids) of LF (PA binding region) termed LFn, retains PA-binding and translocation capabilities but has no toxic activity. LFn has been used to transfer foreign proteins and peptides into the cytoplasm, where they are processed through the MHC class I antigen presentation pathway, and subsequently induce CTL responses. However, it has been reported that LFn (as a fusion protein) cannot transfer all proteins into the cytoplasm (Wesche et al., 1998). Shaw & Starnbach (2008) fused two epitopes (one CD4+ T-cell epitope and one restricted epitope by MHC-I) from chicken ovalbumin (Ova) to LFn and demonstrated that this recombinant protein induced both Ova-specific CD4+ T cell and Ova-specific CD8+ T cell responses in mice. Additionally, Chandra et al. (2006) demonstrated that the anthrax toxin system can be used as an ESAT-6 delivery carrier of to induce CTL response against tuberculosis by the ability of LFn to deliver genetically fused ESAT-6 into the cytosol.
Other Potential Co-Delivery Systems of Epitope-Based Vaccines
Multiple antigenic peptide
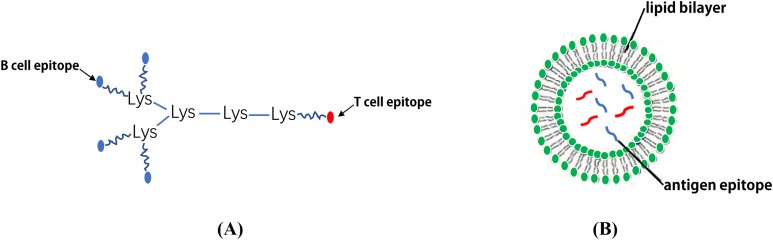
Although the synthesis of long linear peptides with one or more epitopes can promote their presentation on MHC I and II molecules and enhance their immunogenicity, these vaccines continue to fail to demonstrate adequate efficacy or improve the overall survival rate (Simanovich et al., 2017). To solve this problem, epitopes can be displayed on a MAP system which contains a core matrix of lysine residues that form a scaffold (Tam, 1988). Currently, the most common strategy is to couple a number of epitope peptides to the dendritic polylysine-scaffold using standard solid phase chemistry (Moyle et al., 2006; Horvath et al., 2004) (Fig. 5A). It has been reported that the MAP-based vaccine, (B4T(thi)), which is composed of four copies of B cell epitopes (amino acid (aa) residues 136–154 of the FMDV VP1 protein) which are linked to a T cell epitope (aa residues 21–35 of the FMDV non-structural protein 3A) via thioether bonds can significantly induce an immune response against FMDV (Cubillos et al., 2012). Moreover, Wen et al. (2016) designed a novel tetra-branched MAP vaccine, M2e-MAP, which combines four copies of M2e with a foreign Th epitope to provide cross-protection against influenza viruses and may serve as a promising platform for influenza vaccine development. The immunogenicity of both adjuvanted and non-adjuvanted MAP vaccines composed of three conserved HCV envelope peptides (E1 peptide (aa 315–323) and E2 peptide (aa 412–419 and aa 516–531)) were studied. The results showed that the three HCV envelope MAP peptides exhibit strong immunogenicity and produce higher levels of neutralizing antibodies (Abdelhafez et al., 2017). Tumor vaccines based on MAP may also be an effective way to treat and prevent certain types of cancer (Simanovich et al., 2017).
Figure 5. The schematic diagram of MAP system and LCP nanoparticles.
(A) MAP epitope vaccine based on lysine scaffold. (B) The LCP nanoparticles.
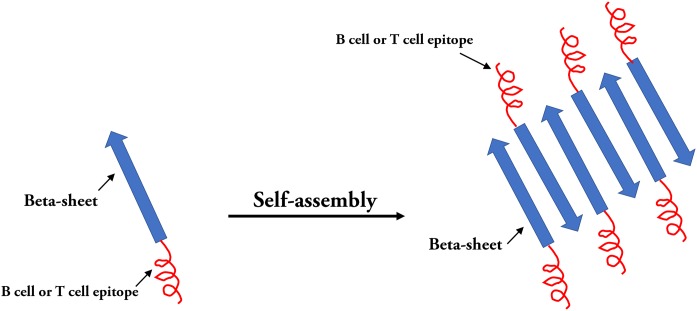
Self-assembled peptide nanoparticles
In the field of epitope vaccine research, natural self-assembled particles that are often used by researchers are proteins derived from viruses (HBsAg or HBcAg (mentioned above) and (TMV) capsid proteins) (Lopez-Sagaseta et al., 2016). With the development of advanced molecular machinery and the construction of sophisticated instruments and materials at an atomic level, a wide-range of materials are being used in SAPN systems (Yang et al., 2012). The SAPN complex is primarily dependent on the selection of suitable building blocks. In the SAPN β-sheets, both polar and hydrophobic amino acids are arranged in an alternating pattern, and self-assembly can occur spontaneously under suitable conditions (Mandal, Nasrolahi & Parang, 2014) (Fig. 6). Indelicato, Burkhard & Twarock (2017) designed a mathematical procedure for the structural classification of a specific class of SAPNs, which provides a toolkit for a systematic exploitation of SAPNs and predicting the density of epitopes on the SAPN surface. In addition, epitopes can be integrated on the surface of peptide NPs by synthesizing in the SAPN system (Friedrich, Beasley & Rudra, 2016). In addition, monomeric peptides containing self-assembled regions and epitopes can be produced by high throughput expression in vitro (El et al., 2014). Recent studies have shown that the SAPN malaria vaccine, FMP014, based on flagellin can be produced by replacing the D0 and D1 regions of bacterial flagellin with repeated sequences of several antigenic epitope regions (e.g., αTSR and circumsporozoite protein (PfCSP) of Plasmodium falciparum) (Seth et al., 2017). In addition, a vaccine was reported to be constructed by combining two conserved influenza virus antigens, M2e and Helix C, with SAPNs as the carrier and flagellin as the self-assembled adjuvant, and the experimental results from animal models show that the SAPN vaccine demonstrates substantial potential for the prevention and control of influenza viruses (Karch et al., 2017). A novel peptide-based SAPN HPV16 vaccine may also be a promising method of improving the efficacy of cervical cancer vaccines and can be used as a useful reference for the study of virus-related diseases and specific tumor immunotherapy (Tang et al., 2012).
Figure 6. Self-assembled peptides nanoparticles (SAPNs).
Systematic self-assembling peptides (β-sheet nanofiber vaccine) with antigen epitopes.
Lipid core peptide
As a form of vaccine delivery, the lipid core peptide (LCP) system allows for lipid amino acids in water with a poly-lysine core to combine with exogenous epitopes to form NPs displaying a polydispersity of 0.3–0.5 (Skwarczynski & Toth, 2011b). It appears that the key to self-assembly into small NPs is to ensure there is a proper balance between the composition of hydrophilic and hydrophobic components (Schulze et al., 2017). In the process of vaccine development, antigen epitopes are surrounded by phospholipid bimolecular layers, thus avoiding the degradation of antigenic peptides by enzymes (Azmi et al., 2014) (Fig. 5B). Using the LCP vector system, the B cell epitope, J14, on the M protein of Streptococcus pyogenes and the epitope peptides of the SfbI protein can be coupled (Zaman et al., 2012, 2011; Moyle et al., 2014). One study demonstrated that an LCP system using BPPCysMPEG as a mucosal adjuvant was more effective at presenting synthetic epitope peptides (Schulze et al., 2017; Olive et al., 2007). Noushin et al. combined the antigen site of pre-fusion respiratory syncytial virus (RSV) F GP (Ø and II (B cell epitopes)) with PADRE (T helper cell epitope) using the LCP delivery system and found that the LCP constructs could induce a high level of RSV-specific antibodies (Jaberolansar et al., 2017). In addition, Nirmal et al. coated the group A streptococcus (GAS) lipopeptide-based vaccine candidate (LCP-1) on the surface of PLGA to form NPs that induced a high antibody response, suggesting that the PLGA-based LCP delivery system may be a promising method in vaccine research (Marasini et al., 2016). Due to several advantageous properties, lipid-based antigen complexes can effectively stimulate both humoral and cellular immune responses. Therefore, lipid-based delivery systems represent potential efficient vaccine adjuvants (Kabiri et al., 2018). For example, several liposome vaccines are currently being investigated in clinical studies (Table 5).
Table 5. Different investigational built-in adjuvants for epitope-based vaccines.
| Build-in adjuvant | Disease | Clinical phase | Reference |
|---|---|---|---|
| Gp96 | Late stage melanoma | Pilot | Shevtsov & Multhoff (2016) |
| Metastatic colon carcinoma | Phase I | Mazzaferro et al. (2003) | |
| Gastric carcinoma | Phase I | Shevtsov & Multhoff (2016) | |
| Pancreatic carcinoma | Phase I | Maki et al. (2007) | |
| Hodgkin lymphoma | Phase I | Shevtsov & Multhoff (2016) | |
| Glioblastoma | Phase I–II | Bloch & Parsa (2014) | |
| HSP70 | Malignant melanoma | Phase I | Shevtsov & Multhoff (2016) |
| Chronic lymphatic leukemia | Phase I | Shevtsov & Multhoff (2016) | |
| Advanced solid tumors | Pilot | Guzhova et al. (2013) | |
| Glioblastoma | Phase I | Guzhova et al. (2013) | |
| HIV | Phase I | SenGupta et al. (2004) | |
| Bacterial flagellin | Bacterial diarrhea and Guillain–Barré syndrome | Phase I | Moyle (2017) |
| Influenza A virus | Phase I/II | Taylor et al. (2011, 2012) | |
| Dengue viruses/Zika virus | Preclinical | Liu et al. (2015) | |
| Respiratory syncytial virus | Preclinical | Liu et al. (2015) | |
| MALP-2 | Pancreatic cancer | Phase I/II | Schmidt et al. (2007) |
| HBcAg | P. falciparum | Phase I | Roose et al. (2013) |
| Influenza A virus | Phase I | Roose et al. (2013) | |
| Hepatitis B virus | Licensed | Effio & Hubbuch (2015) | |
| Qβ VLP | Melanoma | Phase I, II, IIa | Goldinger et al. (2012) |
| Persistent allergic asthma | Phase II | Beeh et al. (2013) | |
| Hypertension | Phase I | Ambühl et al. (2007) | |
| Nicotine dependence | Phase I | Cornuz et al. (2008) | |
| Alzheimer’s disease | Phase I/IIa | Winblad et al. (2012) | |
| SAPNs | Hepatitis B | Phase III | Shirbaghaee & Bolhassani (2016) |
| Cervix cancer | Phase III | Shirbaghaee & Bolhassani (2016) | |
| Parvovirus porcine infection | Phase I/II | Kushnir, Streatfield & Yusibov (2012) | |
| Influenza A | Phase I/II | Kushnir, Streatfield & Yusibov (2012) | |
| Malaria | Phase III | Kushnir, Streatfield & Yusibov (2012) | |
| Alzheimer’s disease | Phase II | Lopez-Sagaseta et al. (2016) | |
| Malignant melanoma | Phase II | Lopez-Sagaseta et al. (2016) | |
| Liposome | Influenza | Phase I/II | Tandrup et al. (2016) |
| Streptococcus mutans | Phase I | Tandrup et al. (2016) | |
| Neisseria meningitides | Phase I | Tandrup et al. (2016) | |
| HIV | Phase I | Tandrup et al. (2016) | |
| Mycobacterium tuberculosis | Phase I | Tandrup et al. (2016) | |
| PLGA | Hepatitis B | Clinical trial | Yang et al. (2016) |
| HIV | Phase I | Bolhassani et al. (2014) | |
| Solid tumors | Preclinical | Bolhassani et al. (2014) | |
| Cervix cancer | Phase II/III | Bolhassani et al. (2014) | |
| Hepatitis C | Preclinical | Bolhassani et al. (2014) | |
| Chitosan | RSV | Preclinical | Bolhassani et al. (2014) |
| Tuberculosis | Preclinical | Bolhassani et al. (2014) | |
| Allergy | Preclinical | Bolhassani et al. (2014) | |
| Gold nanoparticle | Influenza | Clinical trial | Vartak & Sucheck (2016), Zhao et al. (2014) |
| HIV | Clinical trial | Vartak & Sucheck (2016), Zhao et al. (2014) | |
| RSV | Clinical trial | Vartak & Sucheck (2016), Zhao et al. (2014) | |
| Foot-and-mouth disease | Clinical trial | Vartak & Sucheck (2016), Zhao et al. (2014) | |
| Malaria | Clinical trial | Vartak & Sucheck (2016), Zhao et al. (2014) |
Note:
The clinical phases of various built-in adjuvants and their applications in the treatment of different diseases.
Polymeric and inorganic nanoparticles
Some polymers exhibit good stability and biocompatibility, and can encapsulate and carry antigens to target cells (Negahdaripour et al., 2017b), such as PLGA, thermo-responsive synthetic polymers, and N-(2-hydroxypropyl) methacrylamide (HPMA) (Li, Zhou & Huang, 2017). Thus, these polymers are often used as organic biological carriers to present multiple epitopes to the immune system (Tam, 1988). Multi-alkyne-functionalized hbPG is a globular polymer with multiple branches that displays good biocompatibility and is not immunogenic; its multi-functional dendrimer-like structure provides sufficient space to present multivalent antigens (Glaffig et al., 2014). Based on these characteristics, B cell epitopes of the tumor-associated antigen, MUC1, glycopeptide, and the T cell epitopes of the tetanus toxin, P2, can be coupled in series to each branch of the hbPG; moreover, these nanoscale branched spheres can express the glycopeptide on its surface, resulting in enhanced exposure of the antigens to the immune system (Glaffig et al., 2014, 2015). Currently, various vaccines based on polymer NPs are being tested in preclinical and clinical trials, including those for tuberculosis, cancer, and HIV (Table 5).
Nanoparticles based on the conjugation of peptide epitopes and polymers display highly promising self-adjuvant properties; however, their lack of biodegradability may lead to serious deficiencies (Skwarczynski et al., 2010). Chitosan is a non-toxic, muco-adhesive, and biodegradable natural polymer that can be recognized by a variety of receptors (e.g., mannose receptors, TLR2, C-type lectin receptor, Dectin-1, and leukotriene B4 receptors) on the surface of APCs (Li et al., 2013). Chitosan NPs are typically prepared by interacting with anionic crosslinkers, antigens or polymers; anionic tripoly-phosphate was typically used as a crosslinking agent in previous studies (Prego et al., 2010). However, Nevagi et al. (2018) developed a novel chitosan NPs-based vaccine delivery system produced by the conjugation of a short anionic polymer (PGA) to a peptide antigen possessing a conserved B cell epitope derived from GAS and a universal Th epitope to form NPs with trimethyl chitosan via ionic interactions. The GAS peptide antigen-based chitosan NPs were formulated without the use of a crosslinking agent and evaluated in mice upon intranasal administration; such studies have determined that NPs can induce specific mucosal and systemic opsonic antibodies (Nevagi et al., 2018).
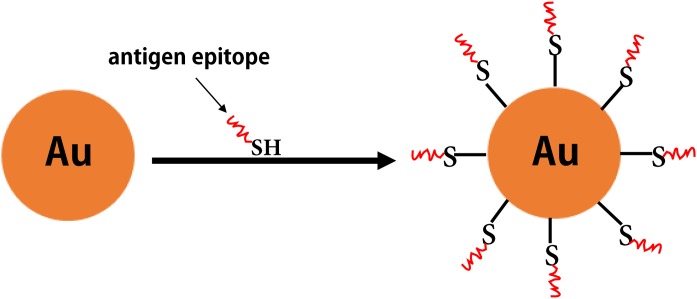
Some inorganic materials (e.g., gold, aluminum hydroxide, and carbon nanotubes) also have excellent biological properties (e.g., good biocompatibility, as well as ease of modification and processing). Among these, gold NPs have attracted increased attention as antigen carriers in vaccine research (Negahdaripour et al., 2017b) (Fig. 7). Compared with other inorganic NPs, gold NPs have been widely investigated in clinical studies for epitope-based vaccine delivery (e.g., influenza, HIV, and Malaria) (Table 5). For example, the Cap protein of porcine ring type 2 is used to directly react with AuNPs via a unique cysteine sulfhydryl group to form Cap-AuNPs, which expose neutralized epitopes to the outer surface of gold NPs, and mice immunized with Cap-AuNP showed that Cap-AuNP could efficiently activate T lymphocytes and balance the immune response of Th1 and Th2 cells (Ding et al., 2017b). Recently, researchers have developed a variety of gold nano-vaccines against influenza viruses that are associated with favorable application prospects (Tao et al., 2017; Wang, Zhu & Wang (2017b)). Wang et al. (2018b) coupled recombinant trimetric influenza A/Aichi/2/68 (H3N2) HA onto the surface of AuNPs and used flagellin as a built-in adjuvant to develop a FliC-coupled AuNP-HA nano-vaccine. These studies indicate that there is promising future for polymeric and inorganic NPs in vaccine development.
Figure 7. The inorganic nanoparticles.
The formation of gold nanoparticles carrying antigen epitopes.
Conclusions
With the expansion of knowledge in the fields of immunology and pathogenic biology, a new era of vaccine science has been established. Such advances have provided a basis for the development of various epitope-based vaccines that have been extensively studied due to their unique advantages, particularly the ability to overcome the safety problems associated with traditional vaccines. To overcome the obstacles associated with epitope-based vaccines (e.g., enzymatic degradation), facilitate recognition by the target cells of the immune system more efficiently, as well as maintain and enhance the efficiency and immunoreactivity of the constructed vaccines, the development of novel built-in adjuvants is a key step in the design of epitope-based vaccines. It is essential to optimize the subunit vaccine antigen design and understand the trends in adjuvant applications, including target antigen processing and its in vivo presentation. To efficiently separate the constructed multi-epitope domains, flexible linkers are often used (e.g., GPGPG and EAAK). The lack of suitable linkers in epitope-based vaccines may lead to the production of novel structural regions which may interfere with the immunogenicity of exogenous epitopes. In this review, we briefly introduced several commonly used built-in adjuvants (e.g., TLR ligands, VLPs, and several bacterial toxin proteins) with different features and several new potential co-delivery systems for epitope-based antigens. These systems are capable of forming NPs, have no immunogenicity or toxicity, and can display antigen epitopes on the surface of the particles, including MAP, SAPNs, LCP, and polymeric or inorganic nanomaterials. Additionally, carrier proteins with epitopes can serve as chaperones and stimulate the production of immune-related factors, possess CTL and Th-cell epitopes required to generate a humoral and cellular immune response, or spontaneously assemble into VLPs. The majority of built-in adjuvants (e.g., HSP70, flagellin, and Chitosan) mentioned in this review are already in clinical trials (Table 5). The carbohydrate-based conjugate vaccines were prepared using TT, DT, meningococcus B outer membrane protein complex (OMPC), and other proteins (e.g., KLH) used as the carrier molecules (Pichichero, 2013). Additionally, these protein carriers have achieved great success. For example, a range of glycoconjugate vaccines against infectious diseases (e.g., Haemophilus influenzae type B, Neisseria meningitidis and pneumonia) have been licensed for clinical use (Astronomo & Burton, 2010). There are some approved VLP-based vaccines currently on the market, including recombinant HBV, hepatitis E virus, and HPV vaccines. Several VLP vaccines for different diseases are also being tested in clinical trials (Negahdaripour et al., 2017b). However, the clinical development of HBc-based VLPs for prophylactic vaccines is likely to experience little growth in the next few years. This is because for HBV-infected patients, the use of HBV particles as an immunogen may lead to poor responses. Thus, it is particularly important to develop alternative VLPs, such as hepadnaviral or plant virus-derived VLPs (e.g., TMV-based VLPs), some of which could be tested in future clinical trials (Roose et al., 2013). Although some adjuvants are currently used in vaccines licensed for human use, they are usually used as mixtures with antigens. In comparison, antigen-adjuvant fusion can significantly improve immunogenicity and display greater potential to induce an antigen-specific immune response. Based on clinical studies of conjugate vaccines, it is difficult to conclude which built-in adjuvant has a greater influence on vaccine immunogenicity. This is because, in addition to adjuvants and selected epitopes, there are other parameters that affect the immunogenicity of epitope vaccines, including conjugation chemistry, the presence of a spacer, and degree of conjugation. The development of future multivalent epitope-based vaccines is primarily dependent on future advances in research involving built-in adjuvants, which have the characteristics of being easily obtained, good biological safety, and a high efficiency for displaying epitopes. In the future, we hope to see the marketing approval of several multiepitope-adjuvant fusion vaccines, as well as increased interest in the field of built-in adjuvants.
Funding Statement
This work was supported by the National Key Research and Development Program (2017YFD0500902), the Key R&D Program of Gansu Province of China (Grant No. 17YF1NA070) and the National Pig Industrial System of China (CARS-36-06B). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Huiyun Chang, Email: changhuiyun@caas.cn.
Yongguang Zhang, Email: zhangyongguang@caas.cn.
Additional Information and Declarations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Yao Lei conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Furong Zhao performed the experiments, contributed reagents/materials/analysis tools, authored or reviewed drafts of the paper.
Junjun Shao performed the experiments, contributed reagents/materials/analysis tools.
Yangfan Li performed the experiments.
Shifang Li performed the experiments.
Huiyun Chang conceived and designed the experiments, authored or reviewed drafts of the paper, approved the final draft.
Yongguang Zhang conceived and designed the experiments, approved the final draft.
Data Availability
The following information was supplied regarding data availability:
This is a review article and did not generate raw data.
References
- Abdelhafez et al. (2017).Abdelhafez TH, Bader EDN, Tabll AA, Mashaly MM, Dawood RM, Yassin NA, El-Awady MK. Mice antibody response to conserved nonadjuvanted multiple antigenic peptides derived from E1/E2 regions of hepatitis C virus. Viral Immunology. 2017;30(5):359–365. doi: 10.1089/vim.2016.0123. [DOI] [PubMed] [Google Scholar]
- Ajamian et al. (2018).Ajamian L, Melnychuk L, Jean-Pierre P, Zaharatos GJ. DNA vaccine-encoded flagellin can be used as an adjuvant scaffold to augment HIV-1 gp41 membrane proximal external region immunogenicity. Viruses. 2018;10(3):100. doi: 10.3390/v10030100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali et al. (2017).Ali M, Pandey RK, Khatoon N, Narula A, Mishra A, Prajapati VK. Exploring dengue genome to construct a multi-epitope based subunit vaccine by utilizing immunoinformatics approach to battle against dengue infection. Scientific Reports. 2017;7(1):9232. doi: 10.1038/s41598-017-09199-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison, Benoist & Chervonsky (2011).Allison JP, Benoist C, Chervonsky AV. Nobels: toll pioneers deserve recognition. Nature. 2011;479(7372):178–178. doi: 10.1038/479178a. [DOI] [PubMed] [Google Scholar]
- Ambühl et al. (2007).Ambühl PM, Tissot AC, Fulurija A, Maurer P, Nussberger J, Sabat R, Nief V, Schellekens C, Sladko K, Roubicek K, Pfister T, Rettenbacher M, Volk H-D, Wagner F, Müller P, Jennings GT, Bachmann MF. A vaccine for hypertension based on virus-like particles: preclinical efficacy and phase I safety and immunogenicity. Journal of Hypertension. 2007;25(1):63–72. doi: 10.1097/HJH.0b013e32800ff5d6. [DOI] [PubMed] [Google Scholar]
- Arai, Inuki & Fujimoto (2018).Arai Y, Inuki S, Fujimoto Y. Site-specific effect of polar functional group-modification in lipids of TLR2 ligands for modulating the ligand immunostimulatory activity. Bioorganic and Medicinal Chemistry Letters. 2018;28(9):1638–1641. doi: 10.1016/j.bmcl.2018.03.042. [DOI] [PubMed] [Google Scholar]
- Arcuri et al. (2017).Arcuri M, Di Benedetto R, Cunningham AF, Saul A, MacLennan CA, Micoli F. The influence of conjugation variables on the design and immunogenicity of a glycoconjugate vaccine against Salmonella Typhi. PLOS ONE. 2017;12(12):e189100. doi: 10.1371/journal.pone.0189100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora, Misra & Sajid (2017).Arora G, Misra R, Sajid A. Model systems for pulmonary infectious diseases: paradigms of anthrax and tuberculosis. Current Topics in Medicinal Chemistry. 2017;17(18):2077–2099. doi: 10.2174/1568026617666170130111324. [DOI] [PubMed] [Google Scholar]
- Astronomo & Burton (2010).Astronomo RD, Burton DR. Carbohydrate vaccines: developing sweet solutions to sticky situations? Nature Reviews Drug Discovery. 2010;9(4):308–324. doi: 10.1038/nrd3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azmi et al. (2014).Azmi F, Ahmad FA, Skwarczynski M, Toth I. Recent progress in adjuvant discovery for peptide-based subunit vaccines. Human Vaccines & Immunotherapeutics. 2014;10(3):778–796. doi: 10.4161/hv.27332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajzert et al. (2018).Bajzert J, Gorczykowski M, Galli J, Stefaniak T. The evaluation of immunogenic impact of selected bacterial, recombinant Hsp60 antigens in DBA/2J mice. Microbial Pathogenesis. 2018;115:100–111. doi: 10.1016/j.micpath.2017.12.001. [DOI] [PubMed] [Google Scholar]
- Banik et al. (2015).Banik S, Mansour AA, Suresh RV, Wykoff-Clary S, Malik M, McCormick AA, Bakshi CS, Murthy AK. Development of a multivalent subunit vaccine against Tularemia using tobacco mosaic virus (TMV) based delivery system. PLOS ONE. 2015;10(6):e130858. doi: 10.1371/journal.pone.0130858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basto & Leitao (2014).Basto AP, Leitao A. Targeting TLR2 for vaccine development. Journal of Immunology Research. 2014;2014(6):1–22. doi: 10.1155/2014/619410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu et al. (2001).Basu S, Binder RJ, Ramalingam T, Srivastava PK. CD91 is a common receptor for heat shock proteins gp96, hsp90, hsp70, and calreticulin. Immunity. 2001;14:303–313. doi: 10.1016/s1074-7613(01)00111-x. [DOI] [PubMed] [Google Scholar]
- Basu et al. (2018).Basu R, Zhai L, Contreras A, Tumban E. Immunization with phage virus-like particles displaying Zika virus potential B-cell epitopes neutralizes Zika virus infection of monkey kidney cells. Vaccine. 2018;36(10):1256–1264. doi: 10.1016/j.vaccine.2018.01.056. [DOI] [PubMed] [Google Scholar]
- Batista et al. (2014).Batista MT, Souza RD, Ferreira EL, Robinette R, Crowley PJ, Rodrigues JF, Brady LJ, Ferreira LC, Ferreira RC. Immunogenicity and in vitro and in vivo protective effects of antibodies targeting a recombinant form of the Streptococcus mutans P1 surface protein. Infection and Immunity. 2014;82(12):4978–4988. doi: 10.1128/IAI.02074-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeh et al. (2013).Beeh K-M, Kanniess F, Wagner F, Schilder C, Naudts I, Hammann-Haenni A, Willers J, Stocker H, Mueller P, Bachmann MF, Renner WA. The novel TLR-9 agonist QbG10 shows clinical efficacy in persistent allergic asthma. Journal of Allergy and Clinical Immunology. 2013;131(3):866–874. doi: 10.1016/j.jaci.2012.12.1561. [DOI] [PubMed] [Google Scholar]
- Bellier & Klatzmann (2013).Bellier B, Klatzmann D. Virus-like particle-based vaccines against hepatitis C virus infection. Expert Review of Vaccines. 2013;12(2):143–154. doi: 10.1586/erv.13.10. [DOI] [PubMed] [Google Scholar]
- Bloch & Parsa (2014).Bloch O, Parsa AT. Heat shock protein peptide complex-96 (HSPPC-96) vaccination for recurrent glioblastoma: a phase II, single arm trial. Neuro-Oncology. 2014;16(5):758–759. doi: 10.1093/neuonc/nou054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolduc et al. (2018).Bolduc M, Baz M, Laliberte-Gagne ME, Carignan D, Garneau C, Russel A, Boivin G, Savard P, Leclerc D. The quest for a nanoparticle-based vaccine inducing broad protection to influenza viruses. Nanomedicine: Nanotechnology, Biology and Medicine. 2018;14(8):2563–2574. doi: 10.1016/j.nano.2018.08.010. [DOI] [PubMed] [Google Scholar]
- Bolhassani et al. (2014).Bolhassani A, Javanzad S, Saleh T, Hashemi M, Aghasadeghi MR, Sadat SM. Polymeric nanoparticles: potent vectors for vaccine delivery targeting cancer and infectious diseases. Human Vaccines & Immunotherapeutics. 2014;10(2):321–332. doi: 10.4161/hv.26796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolhassani & Rafati (2008).Bolhassani A, Rafati S. Heat-shock proteins as powerful weapons in vaccine development. Expert Review of Vaccines. 2008;7(8):1185–1199. doi: 10.1586/14760584.7.8.1185. [DOI] [PubMed] [Google Scholar]
- Broker (2016).Broker M. Potential protective immunogenicity of tetanus toxoid, diphtheria toxoid and cross reacting material 197 (CRM197) when used as carrier proteins in glycoconjugates. Human Vaccines & Immunotherapeutics. 2016;12(3):664–667. doi: 10.1080/21645515.2015.1086048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busseron et al. (2013).Busseron E, Ruff Y, Moulin E, Giuseppone N. Supramolecular self-assemblies as functional nanomaterials. Nanoscale. 2013;5(16):7098–7140. doi: 10.1039/c3nr02176a. [DOI] [PubMed] [Google Scholar]
- Cai et al. (2013).Cai H, Chen MS, Sun ZY, Zhao YF, Kunz H, Li YM. Self-adjuvanting synthetic antitumor vaccines from MUC1 glycopeptides conjugated to T-cell epitopes from tetanus toxoid. Angewandte Chemie International Edition. 2013;52(23):6106–6110. doi: 10.1002/anie.201300390. [DOI] [PubMed] [Google Scholar]
- Cai et al. (2017).Cai H, Orwenyo J, Giddens JP, Yang Q, Zhang R, LaBranche CC, Montefiori DC, Wang LX. Synthetic three-component HIV-1 V3 glycopeptide immunogens induce glycan-dependent antibody responses. Cell Chemical Biology. 2017;24(12):1513–1522.e4. doi: 10.1016/j.chembiol.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carignan et al. (2015).Carignan D, Therien A, Rioux G, Paquet G, Gagne ML, Bolduc M, Savard P, Leclerc D. Engineering of the PapMV Vaccine platform with a shortened M2e peptide leads to an effective one dose influenza vaccine. Vaccine. 2015;33(51):7245–7253. doi: 10.1016/j.vaccine.2015.10.123. [DOI] [PubMed] [Google Scholar]
- Caro-Aguilar et al. (2013).Caro-Aguilar I, Ottinger E, Hepler RW, Nahas DD, Wu C, Good MF, Batzloff M, Joyce JG, Heinrichs JH, Skinner JM. Immunogenicity in mice and non-human primates of the Group A Streptococcal J8 peptide vaccine candidate conjugated to CRM197. Human Vaccines & Immunotherapeutics. 2013;9(3):488–496. doi: 10.4161/hv.23224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellino et al. (2000).Castellino F, Boucher PE, Eichelberg K, Mayhew M, Rothman JE, Houghton AN, Germain RN. Receptor-mediated uptake of antigen/heat shock protein complexes results in major histocompatibility complex class I antigen presentation via two distinct processing pathways. Journal of Experimental Medicine. 2000;191(11):1957–1964. doi: 10.1084/jem.191.11.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes-Barragan et al. (2009).Cervantes-Barragan L, Gil-Cruz C, Pastelin-Palacios R, Lang KS, Isibasi A, Ludewig B, Lopez-Macias C. TLR2 and TLR4 signaling shapes specific antibody responses to Salmonella typhi antigens. European Journal of Immunology. 2009;39(1):126–135. doi: 10.1002/eji.200838185. [DOI] [PubMed] [Google Scholar]
- Chandra et al. (2006).Chandra S, Kaur M, Midha S, Bhatnagar R, Banerjee-Bhatnagar N. Evaluation of the ability of N-terminal fragment of lethal factor of Bacillus anthracis for delivery of Mycobacterium T cell antigen ESAT-6 into cytosol of antigen presenting cells to elicit effective cytotoxic T lymphocyte response. Biochemical and Biophysical Research Communications. 2006;351(3):702–707. doi: 10.1016/j.bbrc.2006.10.099. [DOI] [PubMed] [Google Scholar]
- Chen et al. (2017).Chen Q, Li W, Wang P, Shao H, Ding Y, Wang W, Cen D, Cai Y, Xue X, Zhang L, Zhu G. Induction of humoral and cellular immune responses in mice by multiepitope vaccines composing of both T and B lymphocyte epitopes of MAGE-A3 which are recombined into HBcAg. Protein & Peptide Letters. 2017;24(10):947–954. doi: 10.2174/0929866524666170621094921. [DOI] [PubMed] [Google Scholar]
- Chen et al. (2010).Chen DJ, Osterrieder N, Metzger SM, Buckles E, Doody AM, DeLisa MP, Putnam D. Delivery of foreign antigens by engineered outer membrane vesicle vaccines. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(7):3099–3104. doi: 10.1073/pnas.0805532107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng et al. (2014a).Cheng C, Pal S, Tifrea D, Jia Z, De la Maza LM. A vaccine formulated with a combination of TLR-2 and TLR-9 adjuvants and the recombinant major outer membrane protein elicits a robust immune response and significant protection against a Chlamydia muridarum challenge. Microbes and Infection. 2014a;16(3):244–252. doi: 10.1016/j.micinf.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng et al. (2018).Cheng L, Wang Q, Li G, Banga R, Ma J, Yu H, Yasui F, Zhang Z, Pantaleo G, Perreau M, Zurawski S, Zurawski G, Levy Y, Su L. TLR3 agonist and CD40-targeting vaccination induces immune responses and reduces HIV-1 reservoirs. Journal of Clinical Investigation. 2018;128(10):4387–4396. doi: 10.1172/JCI99005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng et al. (2014b).Cheng L, Yu L, Wu X, Li K, Wang F, Zhang L, Ye W, Li P, Zhang F, Xu Z. Induction of specific humoral and cellular immune responses in a mouse model following gene fusion of HSP70C and Hantaan virus Gn and S0.7 in an adenoviral vector. PLOS ONE. 2014b;9(2):e88183. doi: 10.1371/journal.pone.0088183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu et al. (2016).Chu X, Li Y, Long Q, Xia Y, Yao Y, Sun W, Huang W, Yang X, Liu C, Ma Y. Chimeric HBcAg virus-like particles presenting a HPV 16 E7 epitope significantly suppressed tumor progression through preventive or therapeutic immunization in a TC-1-grafted mouse model. International Journal of Nanomedicine. 2016;11:2417–2429. doi: 10.2147/IJN.S102467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornuz et al. (2008).Cornuz J, Zwahlen S, Jungi WF, Osterwalder J, Klingler K, van Melle G, Bangala Y, Guessous I, Müller P, Willers J, Maurer P, Bachmann MF, Cerny T. A vaccine against nicotine for smoking cessation: a randomized controlled trial. PLOS ONE. 2008;3(6):e2547. doi: 10.1371/journal.pone.0002547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig (2018).Craig EA. Hsp70 at the membrane: driving protein translocation. BMC Biology. 2018;16(1):11. doi: 10.1186/s12915-017-0474-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cubillos et al. (2012).Cubillos C, De la Torre BG, Barcena J, Andreu D, Sobrino F, Blanco E. Inclusion of a specific T cell epitope increases the protection conferred against foot-and-mouth disease virus in pigs by a linear peptide containing an immunodominant B cell site. Virology Journal. 2012;9(1):66. doi: 10.1186/1743-422X-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culver (2002).Culver JN. Tobacco mosaic virus assembly and disassembly: determinants in pathogenicity and resistance. Annual Review of Phytopathology. 2002;40(1):287–308. doi: 10.1146/annurev.phyto.40.120301.102400. [DOI] [PubMed] [Google Scholar]
- Czarnota et al. (2016).Czarnota A, Tyborowska J, Peszynska-Sularz G, Gromadzka B, Bienkowska-Szewczyk K, Grzyb K. Immunogenicity of Leishmania-derived hepatitis B small surface antigen particles exposing highly conserved E2 epitope of hepatitis C virus. Microbial Cell Factories. 2016;15(1):62. doi: 10.1186/s12934-016-0460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da et al. (2011).Da HVP, Conceicao FR, Dellagostin OA, Doolan DL. Non-toxic derivatives of LT as potent adjuvants. Vaccine. 2011;29(8):1538–1544. doi: 10.1016/j.vaccine.2010.11.091. [DOI] [PubMed] [Google Scholar]
- Da et al. (2017).Da SAR, Paul S, Sidney J, Weiskopf D, Dan JM, Phillips E, Mallal S, Crotty S, Sette A, Lindestam AC. Definition of human epitopes recognized in tetanus toxoid and development of an assay strategy to detect exvivo tetanus CD4+ T cell responses. PLOS ONE. 2017;12(1):e169086. doi: 10.1371/journal.pone.0169086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai et al. (2016).Dai S, Zhuo M, Song L, Chen X, Yu Y, Zang G, Tang Z. Lentiviral vector encoding ubiquitinated hepatitis B core antigen induces potent cellular immune responses and therapeutic immunity in HBV transgenic mice. Immunobiology. 2016;221(7):813–821. doi: 10.1016/j.imbio.2016.01.015. [DOI] [PubMed] [Google Scholar]
- Daleke-Schermerhorn et al. (2014).Daleke-Schermerhorn MH, Felix T, Soprova Z, Ten HC, Vikstrom D, Majlessi L, Beskers J, Follmann F, De Punder K, Van Der Wel NN, Baumgarten T, Pham TV, Piersma SR, Jimenez CR, Van Ulsen P, De Gier JW, Leclerc C, Jong WS, Luirink J. Decoration of outer membrane vesicles with multiple antigens by using an autotransporter approach. Applied and Environmental Microbiology. 2014;80(18):5854–5865. doi: 10.1128/AEM.01941-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dascher et al. (2003).Dascher CC, Hiromatsu K, Xiong X, Morehouse C, Watts G, Liu G, McMurray DN, LeClair KP, Porcelli SA, Brenner MB. Immunization with a mycobacterial lipid vaccine improves pulmonary pathology in the guinea pig model of tuberculosis. International Immunology. 2003;15:915–925. doi: 10.1093/intimm/dxg091. [DOI] [PubMed] [Google Scholar]
- Deng et al. (2017).Deng L, Kim JR, Chang TZ, Zhang H, Mohan T, Champion JA, Wang B. Protein nanoparticle vaccine based on flagellin carrier fused to influenza conserved epitopes confers full protection against influenza A virus challenge. Virology. 2017;509:82–89. doi: 10.1016/j.virol.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diethelm-Okita et al. (2000).Diethelm-Okita BM, Okita DK, Banaszak L, Conti-Fine BM. Universal epitopes for human CD4+ cells on tetanus and diphtheria toxins. Journal of Infectious Diseases. 2000;181(3):1001–1009. doi: 10.1086/315324. [DOI] [PubMed] [Google Scholar]
- Ding et al. (2016).Ding L, Meng Y, Zhang HY, Yin WC, Yan Y, Cao YP. Active immunization with the peptide epitope vaccine Aβ3-10-KLH induces a Th2-polarized anti-Aβ antibody response and decreases amyloid plaques in APP/PS1 transgenic mice. Neuroscience Letters. 2016;634:1–6. doi: 10.1016/j.neulet.2016.09.050. [DOI] [PubMed] [Google Scholar]
- Ding et al. (2017a).Ding L, Meng Y, Zhang HY, Yin WC, Yan Y, Cao YP. Prophylactic active immunization with a novel epitope vaccine improves cognitive ability by decreasing amyloid plaques and neuroinflammation in APP/PS1 transgenic mice. Neuroscience Research. 2017a;119:7–14. doi: 10.1016/j.neures.2017.01.003. [DOI] [PubMed] [Google Scholar]
- Ding et al. (2013).Ding Z, Ou R, Ni B, Tang J, Xu Y. Cytolytic activity of the human papillomavirus type 16 E711-20 epitope-specific cytotoxic T lymphocyte is enhanced by heat shock protein 110 in HLA-A*0201 transgenic mice. Clinical and Vaccine Immunology. 2013;20(7):1027–1033. doi: 10.1128/CVI.00721-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding et al. (2017b).Ding P, Zhang T, Li Y, Teng M, Sun Y, Liu X, Chai S, Zhou E, Jin Q, Zhang G. Nanoparticle orientationally displayed antigen epitopes improve neutralizing antibody level in a model of porcine circovirus type 2. International Journal of Nanomedicine. 2017b;12:5239–5254. doi: 10.2147/IJN.S140789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling & Dellacasagrande (2016).Dowling JK, Dellacasagrande J. Toll-like receptors: ligands, cell-based models, and readouts for receptor action. Methods in Molecular Biology. 2016;1390:3–27. doi: 10.1007/978-1-4939-3335-8_1. [DOI] [PubMed] [Google Scholar]
- Dupont et al. (2006).Dupont J, Altclas J, Lepetic A, Lombardo M, Vazquez V, Salgueira C, Seigelchifer M, Arndtz N, Antunez E, Von Eschen K, Janowicz Z. A controlled clinical trial comparing the safety and immunogenicity of a new adjuvanted hepatitis B Vaccine with a standard hepatitis B vaccine. Vaccine. 2006;24(49–50):7167–7174. doi: 10.1016/j.vaccine.2006.06.053. [DOI] [PubMed] [Google Scholar]
- Effio & Hubbuch (2015).Effio CL, Hubbuch J. Next generation vaccines and vectors: designing downstream processes for recombinant protein-based virus-like particles. Biotechnology Journal. 2015;10(5):715–727. doi: 10.1002/biot.201400392. [DOI] [PubMed] [Google Scholar]
- El et al. (2014).El BK, Zhou Y, Dasgupta D, Cobb D, Dubey JP, Burkhard P, Lanar DE, McLeod R. Effectiveness of a novel immunogenic nanoparticle platform for Toxoplasma peptide Vaccine in HLA transgenic mice. Vaccine. 2014;32(26):3243–3248. doi: 10.1016/j.vaccine.2014.03.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El et al. (2017).El BK, Zhou Y, Paulillo SM, Raman SK, Karch CP, Roberts CW, Lanar DE, Reed S, Fox C, Carter D, Alexander J, Sette A, Sidney J, Lorenzi H, Begeman IJ, Burkhard P, McLeod R. Protein nanovaccine confers robust immunity against Toxoplasma. NPJ Vaccines. 2017;2(1):24. doi: 10.1038/s41541-017-0024-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eraghi et al. (2017).Eraghi V, Derakhshandeh A, Hosseini A, Motamedi-Boroojeni A. In silico design and expression of a novel fusion protein of HBHA and high antigenic region of FAP-P of Mycobacterium avium subsp. paratuberculosis in Pichia pastoris. Molecular Biology Research Communications. 2017;6:161–168. doi: 10.22099/mbrc.2017.26522.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felzmann, Gadner & Holter (2002).Felzmann T, Gadner H, Holter W. Dendritic cells as adjuvants in antitumor immune therapy. Onkologie. 2002;25(5):456–464. doi: 10.1159/000067441. [DOI] [PubMed] [Google Scholar]
- Foged (2011).Foged C. Subunit vaccines of the future: the need for safe, customized and optimized particulate delivery systems. Therapeutic Delivery. 2011;2(8):1057–1077. doi: 10.4155/tde.11.68. [DOI] [PubMed] [Google Scholar]
- Fraser et al. (2014).Fraser CC, Altreuter DH, Ilyinskii P, Pittet L, LaMothe RA, Keegan M, Johnston L, Kishimoto TK. Generation of a universal CD4 memory T cell recall peptide effective in humans, mice and non-human primates. Vaccine. 2014;32(24):2896–2903. doi: 10.1016/j.vaccine.2014.02.024. [DOI] [PubMed] [Google Scholar]
- Friedrich, Beasley & Rudra (2016).Friedrich BM, Beasley D, Rudra JS. Supramolecular peptide hydrogel adjuvanted subunit Vaccine elicits protective antibody responses against West Nile virus. Vaccine. 2016;34(46):5479–5482. doi: 10.1016/j.vaccine.2016.09.044. [DOI] [PubMed] [Google Scholar]
- Fu et al. (2013).Fu F, Tian H, Li X, Lang Y, Tong G, Liu S, Li H, Wang W, Li X, Chen X. C-terminal heat shock protein 70 of Mycobacterium tuberculosis as a molecular adjuvant for DNA vaccination with the porcine circovirus type 2 ORF2 (capsid) gene in mice. Veterinary Journal. 2013;195(2):244–247. doi: 10.1016/j.tvjl.2012.06.005. [DOI] [PubMed] [Google Scholar]
- Fukui et al. (2015).Fukui M, Shinjo K, Umemura M, Shigeno S, Harakuni T, Arakawa T, Matsuzaki G. Enhanced effect of BCG vaccine against pulmonary Mycobacterium tuberculosis infection in mice with lung Th17 response to mycobacterial heparin-binding hemagglutinin adhesin antigen. Microbiology and Immunology. 2015;59(12):735–743. doi: 10.1111/1348-0421.12340. [DOI] [PubMed] [Google Scholar]
- Gambhira et al. (2007).Gambhira R, Karanam B, Jagu S, Roberts JN, Buck CB, Bossis I, Alphs H, Culp T, Christensen ND, Roden RB. A protective and broadly cross-neutralizing epitope of human papillomavirus L2. Journal of Virology. 2007;81(24):13927–13931. doi: 10.1128/JVI.00936-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge et al. (2006).Ge F, Qiu Y, Gao X, Yang Y, Chen P. Fusion expression of major antigenic segment of JEV E protein-hsp70 and the identification of domain acting as adjuvant in hsp70. Veterinary Immunology and Immunopathology. 2006;113(3–4):288–296. doi: 10.1016/j.vetimm.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Gerke et al. (2015).Gerke C, Colucci AM, Giannelli C, Sanzone S, Vitali CG, Sollai L, Rossi O, Martin LB, Auerbach J, Di Cioccio V, Saul A. Production of a Shigella sonnei vaccine based on generalized modules for membrane antigens (GMMA), 1790GAHB. PLOS ONE. 2015;10(8):e134478. doi: 10.1371/journal.pone.0134478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaffig et al. (2014).Glaffig M, Palitzsch B, Hartmann S, Schüll C, Nuhn L, Gerlitzki B, Schmitt E, Frey H, Kunz H. A fully synthetic glycopeptide antitumor vaccine based on multiple antigen presentation on a hyperbranched polymer. Chemistry-A European Journal. 2014;20(15):4232–4236. doi: 10.1002/chem.201400256. [DOI] [PubMed] [Google Scholar]
- Glaffig et al. (2015).Glaffig M, Palitzsch B, Stergiou N, Schull C, Strassburger D, Schmitt E, Frey H, Kunz H. Enhanced immunogenicity of multivalent MUC1 glycopeptide antitumour vaccines based on hyperbranched polymers. Organic & Biomolecular Chemistry. 2015;13(40):10150–10154. doi: 10.1039/c5ob01255d. [DOI] [PubMed] [Google Scholar]
- Gnopo et al. (2017).Gnopo Y, Watkins HC, Stevenson TC, DeLisa MP, Putnam D. Designer outer membrane vesicles as immunomodulatory systems–reprogramming bacteria for vaccine delivery. Advanced Drug Delivery Reviews. 2017;114:132–142. doi: 10.1016/j.addr.2017.05.003. [DOI] [PubMed] [Google Scholar]
- Goldinger et al. (2012).Goldinger SM, Dummer R, Baumgaertner P, Mihic-Probst D, Schwarz K, Hammann-Haenni A, Willers J, Geldhof C, Prior JO, Kündig TM, Michielin O, Bachmann MF, Speiser DE. Nano-particle vaccination combined with TLR-7 and -9 ligands triggers memory and effector CD8+ T-cell responses in melanoma patients. European Journal of Immunology. 2012;42(11):3049–3061. doi: 10.1002/eji.201142361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo et al. (2018).Guo F, Liu Y, Zhang C, Wang Q, Wang L, Gao Y, Bi J, Wang H, Su Z. Prompt and robust humoral immunity elicited by a conjugated chimeric malaria antigen with a truncated flagellin. Bioconjugate Chemistry. 2018;29(3):761–770. doi: 10.1021/acs.bioconjchem.7b00320. [DOI] [PubMed] [Google Scholar]
- Guo et al. (2017).Guo L, Yang H, Tang F, Yin R, Liu H, Gong X, Wei J, Zhang Y, Xu G, Liu K. Oral immunization with a multivalent epitope-based vaccine, based on NAP, urease, HSP60, and HpaA, provides therapeutic effect on H. pylori infection in Mongolian gerbils. Frontiers in Cellular and Infection Microbiology. 2017;7:349. doi: 10.3389/fcimb.2017.00349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzhova et al. (2013).Guzhova IV, Shevtsov MA, Abkin SV, Pankratova KM, Margulis BA. Intracellular and extracellular Hsp70 chaperone as a target for cancer therapy. International Journal of Hyperthermia. 2013;29(5):399–408. doi: 10.3109/02656736.2013.807439. [DOI] [PubMed] [Google Scholar]
- Hajam et al. (2017).Hajam IA, Dar PA, Shahnawaz I, Jaume JC, Lee JH. Bacterial flagellin-a potent immunomodulatory agent. Experimental and Molecular Medicine. 2017;49(9):e373. doi: 10.1038/emm.2017.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajighahramani et al. (2017).Hajighahramani N, Nezafat N, Eslami M, Negahdaripour M, Rahmatabadi SS, Ghasemi Y. Immunoinformatics analysis and in silico designing of a novel multi-epitope peptide vaccine against Staphylococcus aureus. Infection, Genetics and Evolution. 2017;48:83–94. doi: 10.1016/j.meegid.2016.12.010. [DOI] [PubMed] [Google Scholar]
- Halliday et al. (2016).Halliday A, Turner JD, Guimaraes A, Bates PA, Taylor MJ. The TLR2/6 ligand PAM2CSK4 is a Th2 polarizing adjuvant in Leishmania major and Brugia malayi murine vaccine models. Parasites & Vectors. 2016;9(1):96. doi: 10.1186/s13071-016-1381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He et al. (2018).He Q, Gao H, Gao M, Qi S, Yang K, Zhang Y, Wang J. Immunogenicity and safety of a novel tetanus toxoid-conjugated anti-gastrin Vaccine in BALB/c mice. Vaccine. 2018;36(6):847–852. doi: 10.1016/j.vaccine.2017.12.054. [DOI] [PubMed] [Google Scholar]
- Hekmat et al. (2018).Hekmat S, Sadat SM, Aslani MM, Mahdavi M, Bolhassani A, Asgar HF, Ghahari S, Aghasadeghi MR, Siadat SD. Truncated core/NS3 fusion protein of HCV adjuvanted with outer membrane vesicles of Neisseria meningitidis serogroup B: potent inducer of the murine immune system. Iranian Biomedical Journal. 2018 doi: 10.29252/.23.4.235. Epub ahead of print 3 October 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath et al. (2004).Horvath A, Olive C, Karpati L, Sun HK, Good M, Toth I. Toward the development of a synthetic group a streptococcal vaccine of high purity and broad protective coverage. Journal of Medicinal Chemistry. 2004;47(16):4100–4104. doi: 10.1021/jm040041w. [DOI] [PubMed] [Google Scholar]
- Hu et al. (2014).Hu JC, Mathias-Santos C, Greene CJ, King-Lyons ND, Rodrigues JF, Hajishengallis G, Ferreira LC, Connell TD. Intradermal administration of the type II heat-labile enterotoxins LT-IIb and LT-IIc of enterotoxigenic Escherichia coli enhances humoral and CD8+ T cell immunity to a co-administered antigen. PLOS ONE. 2014;9(12):e113978. doi: 10.1371/journal.pone.0113978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huleatt et al. (2008).Huleatt JW, Nakaar V, Desai P, Huang Y, Hewitt D, Jacobs A, Tang J, McDonald W, Song L, Evans RK, Umlauf S, Tussey L, Powell TJ. Potent immunogenicity and efficacy of a universal influenza Vaccine candidate comprising a recombinant fusion protein linking influenza M2e to the TLR5 ligand flagellin. Vaccine. 2008;26(2):201–214. doi: 10.1016/j.vaccine.2007.10.062. [DOI] [PubMed] [Google Scholar]
- Indelicato, Burkhard & Twarock (2017).Indelicato G, Burkhard P, Twarock R. Classification of self-assembling protein nanoparticle architectures for applications in vaccine design. Royal Society Open Science. 2017;4(4):161092. doi: 10.1098/rsos.161092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izgi et al. (2015).Izgi K, Iskender B, Sakalar C, Arslanhan A, Saraymen B, Canatan H. Evaluation of two different adjuvants with immunogenic uroplakin 3A-derived peptide for their ability to evoke an immune response in mice. European Cytokine Network. 2015;26:46–56. doi: 10.1684/ecn.2015.0365. [DOI] [PubMed] [Google Scholar]
- Jaberolansar et al. (2017).Jaberolansar N, Chappell KJ, Watterson D, Bermingham IM, Toth I, Young PR, Skwarczynski M. Induction of high titred, non-neutralising antibodies by self-adjuvanting peptide epitopes derived from the respiratory syncytial virus fusion protein. Scientific Reports. 2017;7(1):11130. doi: 10.1038/s41598-017-10415-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang et al. (2004).Jang MH, Kweon MN, Iwatani K, Yamamoto M, Terahara K, Sasakawa C, Suzuki T, Nochi T, Yokota Y, Rennert PD, Hiroi T, Tamagawa H, Iijima H, Kunisawa J, Yuki Y, Kiyono H. Intestinal villous M cells: an antigen entry site in the mucosal epithelium. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(16):6110–6115. doi: 10.1073/pnas.0400969101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarzab et al. (2018).Jarzab A, Witkowska D, Ziomek E, Setner B, Czajkowska A, Dorot M, Szewczuk Z, Gamian A. Cyclic OmpC peptidic epitope conjugated to tetanus toxoid as a potential Vaccine candidate against shigellosis. Vaccine. 2018;36(31):4641–4649. doi: 10.1016/j.vaccine.2018.06.037. [DOI] [PubMed] [Google Scholar]
- Jiang et al. (2017).Jiang P, Cai Y, Chen J, Ye X, Mao S, Zhu S, Xue X, Chen S, Zhang L. Evaluation of tandem Chlamydia trachomatis MOMP multi-epitopes Vaccine in BALB/c mice model. Vaccine. 2017;35(23):3096–3103. doi: 10.1016/j.vaccine.2017.04.031. [DOI] [PubMed] [Google Scholar]
- Jiang et al. (2016).Jiang S, Li X, Hess NJ, Guan Y, Tapping RI. TLR10 is a negative regulator of both MyD88-dependent and -independent TLR signaling. Journal of Immunology. 2016;196(9):3834–3841. doi: 10.4049/jimmunol.1502599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin et al. (2007).Jin MS, Kim SE, Heo JY, Lee ME, Kim HM, Paik SG, Lee H, Lee JO. Crystal structure of the TLR1-TLR2 heterodimer induced by binding of a tri-acylated lipopeptide. Cell. 2007;130(6):1071–1082. doi: 10.1016/j.cell.2007.09.008. [DOI] [PubMed] [Google Scholar]
- Jong et al. (2014).Jong WS, Daleke-Schermerhorn MH, Vikstrom D, Ten HC, De Punder K, Van Der Wel NN, Van De Sandt CE, Rimmelzwaan GF, Follmann F, Agger EM, Andersen P, De Gier JW, Luirink J. An autotransporter display platform for the development of multivalent recombinant bacterial vector vaccines. Microbial Cell Factories. 2014;13(1):162. doi: 10.1186/s12934-014-0162-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung et al. (2011).Jung ID, Jeong SK, Lee CM, Noh KT, Heo DR, Shin YK, Yun CH, Koh WJ, Akira S, Whang J, Kim HJ, Park WS, Shin SJ, Park YM. Enhanced efficacy of therapeutic cancer vaccines produced by co-treatment with Mycobacterium tuberculosis heparin-binding hemagglutinin, a novel TLR4 agonist. Cancer Research. 2011;71(8):2858–2870. doi: 10.1158/0008-5472.CAN-10-3487. [DOI] [PubMed] [Google Scholar]
- Juwono & Martinus (2016).Juwono J, Martinus RD. Does Hsp60 provide a link between mitochondrial stress and inflammation in diabetes mellitus? Journal of Diabetes Research. 2016;2016(3):8017571–8017576. doi: 10.1155/2016/8017571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabiri et al. (2018).Kabiri M, Sankian M, Hosseinpour M, Tafaghodi M. The novel immunogenic chimeric peptide vaccine to elicit potent cellular and mucosal immune responses against HTLV-1. International Journal of Pharmaceutics. 2018;549(1–2):404–414. doi: 10.1016/j.ijpharm.2018.07.069. [DOI] [PubMed] [Google Scholar]
- Kaisho & Akira (2002).Kaisho T, Akira S. Toll-like receptors as adjuvant receptors. Biochimica et Biophysica Acta. 2002;1589(1):1–13. doi: 10.1016/S0167-4889(01)00182-3. [DOI] [PubMed] [Google Scholar]
- Kalnin et al. (2017).Kalnin K, Chivukula S, Tibbitts T, Yan Y, Stegalkina S, Shen L, Cieszynski J, Costa V, Sabharwal R, Anderson SF, Christensen N, Jagu S, Roden RBS, Kleanthous H. Incorporation of RG1 epitope concatemers into a self-adjuvanting Flagellin-L2 vaccine broaden durable protection against cutaneous challenge with diverse human papillomavirus genotypes. Vaccine. 2017;35(37):4942–4951. doi: 10.1016/j.vaccine.2017.07.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalnin et al. (2014).Kalnin K, Tibbitts T, Yan Y, Stegalkina S, Shen L, Costa V, Sabharwal R, Anderson SF, Day PM, Christensen N, Schiller JT, Jagu S, Roden RB, Almond J, Kleanthous H. Low doses of flagellin-L2 multimer Vaccines protect against challenge with diverse papillomavirus genotypes. Vaccine. 2014;32(28):3540–3547. doi: 10.1016/j.vaccine.2014.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamboj et al. (2001).Kamboj KK, King CL, Greenspan NS, Kirchner HL, Schreiber JR. Immunization with Haemophilus influenzae type b-CRM(197) conjugate vaccine elicits a mixed Th1 and Th2 CD(4+) T cell cytokine response that correlates with the isotype of antipolysaccharide antibody. Journal of Infectious Diseases. 2001;184(7):931–935. doi: 10.1086/323342. [DOI] [PubMed] [Google Scholar]
- Karch & Burkhard (2016).Karch CP, Burkhard P. Vaccine technologies: from whole organisms to rationally designed protein assemblies. Biochemical Pharmacology. 2016;120:1–14. doi: 10.1016/j.bcp.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karch et al. (2017).Karch CP, Li J, Kulangara C, Paulillo SM, Raman SK, Emadi S, Tan A, Helal ZH, Fan Q, Khan MI, Burkhard P. Vaccination with self-adjuvanted protein nanoparticles provides protection against lethal influenza challenge. Nanomedicine. 2017;13(1):241–251. doi: 10.1016/j.nano.2016.08.030. [DOI] [PubMed] [Google Scholar]
- Karuturi et al. (2017).Karuturi B, Tallapaka SB, Yeapuri P, Curran SM, Sanderson SD, Vetro JA. Encapsulation of an EP67-conjugated CTL peptide vaccine in nanoscale biodegradable particles increases the efficacy of respiratory immunization and affects the magnitude and memory subsets of vaccine-generated mucosal and systemic CD8(+) T cells in a diameter-dependent manner. Molecular Pharmaceutics. 2017;14(5):1469–1481. doi: 10.1021/acs.molpharmaceut.6b01088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawakami et al. (2018).Kawakami R, Nozato Y, Nakagami H, Ikeda Y, Shimamura M, Yoshida S, Sun J, Kawano T, Takami Y, Noma T, Rakugi H, Minamino T, Morishita R. Development of vaccine for dyslipidemia targeted to a proprotein convertase subtilisin/kexin type 9 (PCSK9) epitope in mice. PLOS ONE. 2018;13(2):e191895. doi: 10.1371/journal.pone.0191895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemnade et al. (2014).Kemnade JO, Seethammagari M, Collinson-Pautz M, Kaur H, Spencer DM, McCormick AA. Tobacco mosaic virus efficiently targets DC uptake, activation and antigen-specific T cell responses in vivo. Vaccine. 2014;32(33):4228–4233. doi: 10.1016/j.vaccine.2014.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khader et al. (2007).Khader SA, Bell GK, Pearl JE, Fountain JJ, Rangel-Moreno J, Cilley GE, Shen F, Eaton SM, Gaffen SL, Swain SL, Locksley RM, Haynes L, Randall TD, Cooper AM. IL-23 and IL-17 in the establishment of protective pulmonary CD4+ T cell responses after vaccination and during Mycobacterium tuberculosis challenge. Nature Immunology. 2007;8(4):369–377. doi: 10.1038/ni1449. [DOI] [PubMed] [Google Scholar]
- Kim et al. (2008).Kim JY, Doody AM, Chen DJ, Cremona GH, Shuler ML, Putnam D, DeLisa MP. Engineered bacterial outer membrane vesicles with enhanced functionality. Journal of Molecular Biology. 2008;380(1):51–66. doi: 10.1016/j.jmb.2008.03.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim et al. (2018).Kim J, Yang YL, Jang SH, Jang YS. Human beta-defensin 2 plays a regulatory role in innate antiviral immunity and is capable of potentiating the induction of antigen-specific immunity. Virology Journal. 2018;15(1):124. doi: 10.1186/s12985-018-1035-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitaoka et al. (2017).Kitaoka M, Naritomi A, Kawabe Y, Kamihira M, Kamiya N, Goto M. Transcutaneous pollinosis immunotherapy using a solid-in-oil nanodispersion system carrying T cell epitope peptide and R848. Bioengineering & Translational Medicine. 2017;2(1):102–108. doi: 10.1002/btm2.10048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuipers et al. (2015).Kuipers K, Daleke-Schermerhorn MH, Jong WS, Ten HC, Van Opzeeland F, Simonetti E, Luirink J, De Jonge MI. Salmonella outer membrane vesicles displaying high densities of pneumococcal antigen at the surface offer protection against colonization. Vaccine. 2015;33(17):2022–2029. doi: 10.1016/j.vaccine.2015.03.010. [DOI] [PubMed] [Google Scholar]
- Kushnir, Streatfield & Yusibov (2012).Kushnir N, Streatfield SJ, Yusibov V. Virus-like particles as a highly efficient vaccine platform: diversity of targets and production systems and advances in clinical development. Vaccine. 2012;31(1):58–83. doi: 10.1016/j.vaccine.2012.10.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurkjian et al. (2017).Kurkjian CJ, Guo H, Montgomery ND, Cheng N, Yuan H, Merrill JR, Sempowski GD, Brickey WJ, Ting JP. The toll-like receptor 2/6 agonist, FSL-1 lipopeptide, therapeutically mitigates acute radiation syndrome. Scientific Reports. 2017;7(1):17355. doi: 10.1038/s41598-017-17729-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacasse et al. (2008).Lacasse P, Denis J, Lapointe R, Leclerc D, Lamarre A. Novel plant virus-based vaccine induces protective cytotoxic T-lymphocyte-mediated antiviral immunity through dendritic cell maturation. Journal of Virology. 2008;82(2):785–794. doi: 10.1128/JVI.01811-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladokhin (2013).Ladokhin AS. pH-triggered conformational switching along the membrane insertion pathway of the diphtheria toxin T-domain. Toxins (Basel) 2013;5(8):1362–1380. doi: 10.3390/toxins5081362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagoutte et al. (2016).Lagoutte P, Mignon C, Donnat S, Stadthagen G, Mast J, Sodoyer R, Lugari A, Werle B. Scalable chromatography-based purification of virus-like particle carrier for epitope based influenza A vaccine produced in Escherichia coli. Journal of Virological Methods. 2016;232:8–11. doi: 10.1016/j.jviromet.2016.02.011. [DOI] [PubMed] [Google Scholar]
- Leclerc et al. (2013).Leclerc D, Rivest M, Babin C, Lopez-Macias C, Savard P. A novel M2e based flu vaccine formulation for dogs. PLOS ONE. 2013;8(10):e77084. doi: 10.1371/journal.pone.0077084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2009).Lee BO, Tucker A, Frelin L, Sallberg M, Jones J, Peters C, Hughes J, Whitacre D, Darsow B, Peterson DL, Milich DR. Interaction of the hepatitis B core antigen and the innate immune system. Journal of Immunology. 2009;182(11):6670–6681. doi: 10.4049/jimmunol.0803683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lencer, Hirst & Holmes (1999).Lencer WI, Hirst TR, Holmes RK. Membrane traffic and the cellular uptake of cholera toxin. Biochimica et Biophysica Acta (BBA)–Molecular Cell Research. 1999;1450(3):177–190. doi: 10.1016/s0167-4889(99)00070-1. [DOI] [PubMed] [Google Scholar]
- Li & Guo (2018).Li Q, Guo Z. Recent advances in toll like receptor-targeting glycoconjugate vaccines. Molecules. 2018;23(7):1583. doi: 10.3390/molecules23071583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2013).Li X, Min M, Du N, Gu Y, Hode T, Naylor M, Chen D, Nordquist RE, Chen WR. Chitin, chitosan, and glycated chitosan regulate immune responses: the novel adjuvants for cancer vaccine. Clinical and Developmental Immunology. 2013;2013(7378):387023–387028. doi: 10.1155/2013/387023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2006).Li X, Yang X, Li L, Liu H, Liu J. A truncated C-terminal fragment of Mycobacterium tuberculosis HSP70 gene enhanced potency of HBV DNA Vaccine. Vaccine. 2006;24(16):3321–3331. doi: 10.1016/j.vaccine.2006.01.012. [DOI] [PubMed] [Google Scholar]
- Li, Zhou & Huang (2017).Li L, Zhou M, Huang Y. Synergistic enhancement of anticancer therapeutic efficacy of HPMA copolymer doxorubicin conjugates via combination of ligand modification and stimuli-response srategies. International Journal of Pharmaceutics. 2017;536(1):450–458. doi: 10.1016/j.ijpharm.2017.12.018. [DOI] [PubMed] [Google Scholar]
- Liang et al. (2018).Liang P, Yi Y, Su QD, Qiu F, Fan XT, Lu XX, Bi SL. Efficient humoral and cellular immune responses induced by a chimeric virus-like particle displaying the epitope of EV71 without adjuvant. Biomedical and Environmental Sciences. 2018;31:343–350. doi: 10.3967/bes2018.045. [DOI] [PubMed] [Google Scholar]
- Liu et al. (2017).Liu S, Ma Q, Fattah R, Bugge TH, Leppla SH. Anti-tumor activity of anthrax toxin variants that form a functional translocation pore by intermolecular complementation. Oncotarget. 2017;8(39):65123–65131. doi: 10.18632/oncotarget.17729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu et al. (2015).Liu G, Song L, Beasley DWC, Putnak R, Parent J, Misczak J, Li H, Reiserova L, Liu X, Tian H, Liu W, Labonte D, Duan L, Kim Y, Travalent L, Wigington D, Weaver B, Tussey L. Immunogenicity and efficacy of flagellin-envelope fusion dengue vaccines in mice and monkeys. Clinical and Vaccine Immunology. 2015;22(5):516–525. doi: 10.1128/CVI.00770-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu et al. (2018).Liu Q, Tan K, Yuan J, Song K, Li R, Huang X, Liu Q. Flagellin-deficient outer membrane vesicles as adjuvant induce cross-protection of Salmonella Typhimurium outer membrane proteins against infection by heterologous Salmonella serotypes. International Journal of Medical Microbiology. 2018;308(7):796–802. doi: 10.1016/j.ijmm.2018.06.001. [DOI] [PubMed] [Google Scholar]
- Liu et al. (2013).Liu R, Vaishnav RA, Roberts AM, Friedland RP. Humans have antibodies against a plant virus: evidence from tobacco mosaic virus. PLOS ONE. 2013;8(4):e60621. doi: 10.1371/journal.pone.0060621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu et al. (2016).Liu Y, Zhang W, He Q, Yu F, Song T, Liu T, Zhang Z, Zhou J, Wang PG, Zhao W. Fully synthetic self-adjuvanting MUC1-fibroblast stimulating lipopeptide 1 conjugates as potential cancer vaccines. Chemical Communications. 2016;52(72):10886–10889. doi: 10.1039/c6cc04623a. [DOI] [PubMed] [Google Scholar]
- Long et al. (2014).Long Q, Huang W, Yao Y, Yang X, Sun W, Jin X, Li Y, Chu X, Liu C, Peng Z, Ma Y. Virus-like particles presenting interleukin-33 molecules: immunization characteristics and potentials of blockingIL-33/ST2 pathway in allergic airway inflammation. Human Vaccines & Immunotherapeutics. 2014;10(8):2303–2311. doi: 10.4161/hv.29425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Sagaseta et al. (2016).Lopez-Sagaseta J, Malito E, Rappuoli R, Bottomley MJ. Self-assembling protein nanoparticles in the design of vaccines. Computational and Structural Biotechnology Journal. 2016;14:58–68. doi: 10.1016/j.csbj.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luiz et al. (2015).Luiz WB, Rodrigues JF, Crabb JH, Savarino SJ, Ferreira LC. Maternal vaccination with a fimbrial tip adhesin and passive protection of neonatal mice against lethal human enterotoxigenic Escherichia coli challenge. Infection and Immunity. 2015;83(12):4555–4564. doi: 10.1128/IAI.00858-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLennan, Martin & Micoli (2014).MacLennan CA, Martin LB, Micoli F. Vaccines against invasive Salmonella disease: current status and future directions. Human Vaccines & Immunotherapeutics. 2014;10(6):1478–1493. doi: 10.4161/hv.29054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maki et al. (2007).Maki RG, Livingston PO, Lewis JJ, Janetzki S, Klimstra D, Desantis D, Srivastava PK, Brennan MF. A phase I pilot study of autologous heat shock protein vaccine HSPPC-96 in patients with resected pancreatic adenocarcinoma. Digestive Diseases and Sciences. 2007;52(8):1964–1972. doi: 10.1007/s10620-006-9205-2. [DOI] [PubMed] [Google Scholar]
- Malito et al. (2012).Malito E, Bursulaya B, Chen C, Lo SP, Picchianti M, Balducci E, Biancucci M, Brock A, Berti F, Bottomley MJ, Nissum M, Costantino P, Rappuoli R, Spraggon G. Structural basis for lack of toxicity of the diphtheria toxin mutant CRM197. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(14):5229–5234. doi: 10.1073/pnas.1201964109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal, Nasrolahi & Parang (2014).Mandal D, Nasrolahi SA, Parang K. Self-assembly of peptides to nanostructures. Organic and Biomolecular Chemistry. 2014;12(22):3544–3561. doi: 10.1039/c4ob00447g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marasini et al. (2016).Marasini N, Khalil ZG, Giddam AK, Ghaffar KA, Hussein WM, Capon RJ, Batzloff MR, Good MF, Skwarczynski M, Toth I. Lipid core peptide/poly(lactic-co-glycolic acid) as a highly potent intranasal vaccine delivery system against Group A streptococcus. International Journal of Pharmaceutics. 2016;513(1–2):410–420. doi: 10.1016/j.ijpharm.2016.09.057. [DOI] [PubMed] [Google Scholar]
- Mazzaferro et al. (2003).Mazzaferro V, Coppa J, Carrabba MG, Rivoltini L, Schiavo M, Regalia E, Mariani L, Camerini T, Marchiano A, Andreola S, Camerini R, Corsi M, Lewis JJ, Srivastava PK, Parmiani G. Vaccination with autologous tumor-derived heat-shock protein gp96 after liver resection for metastatic colorectal cancer. Clinical Cancer Research. 2003;9:3235–3245. [PubMed] [Google Scholar]
- McCormick et al. (2006).McCormick AA, Corbo TA, Wykoff-Clary S, Nguyen LV, Smith ML, Palmer KE, Pogue GP. TMV-peptide fusion vaccines induce cell-mediated immune responses and tumor protection in two murine models. Vaccine. 2006;24(40–41):6414–6423. doi: 10.1016/j.vaccine.2006.06.003. [DOI] [PubMed] [Google Scholar]
- McDonald, Byrne & Payne (2015).McDonald DM, Byrne SN, Payne RJ. Synthetic self-adjuvanting glycopeptide cancer vaccines. Frontiers in Chemistry. 2015;3:60. doi: 10.3389/fchem.2015.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald et al. (2014).McDonald DM, Wilkinson BL, Corcilius L, Thaysen-Andersen M, Byrne SN, Payne RJ. Synthesis and immunological evaluation of self-adjuvanting MUC1-macrophage activating lipopeptide 2 conjugate vaccine candidates. Chemical Communications. 2014;50(71):10273–10276. doi: 10.1039/c4cc03510k. [DOI] [PubMed] [Google Scholar]
- Micoli et al. (2018).Micoli F, Rondini S, Alfini R, Lanzilao L, Necchi F, Negrea A, Rossi O, Brandt C, Clare S, Mastroeni P, Rappuoli R, Saul A, MacLennan CA. Comparative immunogenicity and efficacy of equivalent outer membrane vesicle and glycoconjugate vaccines against nontyphoidal Salmonella. Proceedings of the National Academy of Sciences of the United States of America. 2018;115(41):10428–10433. doi: 10.1073/pnas.1807655115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milich et al. (1987).Milich DR, McLachlan A, Thornton GB, Hughes JL. Antibody production to the nucleocapsid and envelope of the hepatitis B virus primed by a single synthetic T cell site. Nature. 1987;329(6139):547–549. doi: 10.1038/329547a0. [DOI] [PubMed] [Google Scholar]
- Moody et al. (2000).Moody DB, Ulrichs T, Muhlecker W, Young DC, Gurcha SS, Grant E, Rosat JP, Brenner MB, Costello CE, Besra GS, Porcelli SA. CD1c-mediated T-cell recognition of isoprenoid glycolipids in Mycobacterium tuberculosis infection. Nature. 2000;404(6780):884–888. doi: 10.1038/35009119. [DOI] [PubMed] [Google Scholar]
- Mora et al. (2017).Mora D, Salman MD, Myrick CA, Rhyan JC, Miller LA, Saetre EM, Eckery DC. Evaluation of antibody response to an adjuvanted hapten-protein vaccine as a potential inhibitor of sexual maturation for farmed Atlantic salmon. Fish & Shellfish Immunology. 2017;71:255–263. doi: 10.1016/j.fsi.2017.08.038. [DOI] [PubMed] [Google Scholar]
- Moreno-Eutimio et al. (2013).Moreno-Eutimio MA, Tenorio-Calvo A, Pastelin-Palacios R, Perez-Shibayama C, Gil-Cruz C, Lopez-Santiago R, Baeza I, Fernandez-Mora M, Bonifaz L, Isibasi A, Calva E, Lopez-Macias C. Salmonella Typhi OmpS1 and OmpS2 porins are potent protective immunogens with adjuvant properties. Immunology. 2013;139(4):459–471. doi: 10.1111/imm.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyle (2017).Moyle PM. Biotechnology approaches to produce potent, self-adjuvanting antigen-adjuvant fusion protein subunit vaccines. Biotechnology Advances. 2017;35(3):375–389. doi: 10.1016/j.biotechadv.2017.03.005. [DOI] [PubMed] [Google Scholar]
- Moyle et al. (2014).Moyle PM, Dai W, Zhang Y, Batzloff MR, Good MF, Toth I. Site-specific incorporation of three toll-like receptor 2 targeting adjuvants into semisynthetic, molecularly defined nanoparticles: application to group a streptococcal vaccines. Bioconjugate Chemistry. 2014;25(5):965–978. doi: 10.1021/bc500108b. [DOI] [PubMed] [Google Scholar]
- Moyle et al. (2006).Moyle PM, Olive C, Ho MF, Good MF, Toth I. Synthesis of a highly pure lipid core peptide based self-adjuvanting triepitopic group A streptococcal vaccine, and subsequent immunological evaluation. Journal of Medicinal Chemistry. 2006;49(21):6364–6370. doi: 10.1021/jm060475m. [DOI] [PubMed] [Google Scholar]
- Moyle & Toth (2013).Moyle PM, Toth I. Modern subunit vaccines: development, components, and research opportunities. ChemMedChem. 2013;8(3):360–376. doi: 10.1002/cmdc.201200487. [DOI] [PubMed] [Google Scholar]
- Muhlradt et al. (1997).Muhlradt PF, Kiess M, Meyer H, Sussmuth R, Jung G. Isolation, structure elucidation, and synthesis of a macrophage stimulatory lipopeptide from Mycoplasma fermentans acting at picomolar concentration. Journal of Experimental Medicine. 1997;185:1951–1958. doi: 10.1084/jem.185.11.1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy et al. (2004).Murthy KG, Deb A, Goonesekera S, Szabo C, Salzman AL. Identification of conserved domains in Salmonella muenchen flagellin that are essential for its ability to activate TLR5 and to induce an inflammatory response in vitro. Journal of Biological Chemistry. 2004;279(7):5667–5675. doi: 10.1074/jbc.M307759200. [DOI] [PubMed] [Google Scholar]
- Nalla et al. (2015).Nalla N, Pallavi P, Reddy BS, Miryala S, Naveen KV, Mahboob M, Halmuthur MS. Design, synthesis and immunological evaluation of 1,2,3-triazole-tethered carbohydrate-Pam3Cys conjugates as TLR2 agonists. Bioorganic & Medicinal Chemistry. 2015;23(17):5846–5855. doi: 10.1016/j.bmc.2015.06.070. [DOI] [PubMed] [Google Scholar]
- Narula et al. (2018).Narula A, Pandey RK, Khatoon N, Mishra A, Prajapati VK. Excavating chikungunya genome to design B and T cell multi-epitope subunit vaccine using comprehensive immunoinformatics approach to control chikungunya infection. Infection, Genetics and Evolution. 2018;61:4–15. doi: 10.1016/j.meegid.2018.03.007. [DOI] [PubMed] [Google Scholar]
- Negahdaripour et al. (2017a).Negahdaripour M, Eslami M, Nezafat N, Hajighahramani N, Ghoshoon MB, Shoolian E, Dehshahri A, Erfani N, Morowvat MH, Ghasemi Y. A novel HPV prophylactic peptide vaccine, designed by immunoinformatics and structural vaccinology approaches. Infection, Genetics and Evolution. 2017a;54:402–416. doi: 10.1016/j.meegid.2017.08.002. [DOI] [PubMed] [Google Scholar]
- Negahdaripour et al. (2017b).Negahdaripour M, Golkar N, Hajighahramani N, Kianpour S, Nezafat N, Ghasemi Y. Harnessing self-assembled peptide nanoparticles in epitope vaccine design. Biotechnology Advances. 2017b;35(5):575–596. doi: 10.1016/j.biotechadv.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negahdaripour et al. (2018).Negahdaripour M, Nezafat N, Eslami M, Ghoshoon MB, Shoolian E, Najafipour S, Morowvat MH, Dehshahri A, Erfani N, Ghasemi Y. Structural vaccinology considerations for in silico designing of a multi-epitope vaccine. Infection, Genetics and Evolution. 2018;58:96–109. doi: 10.1016/j.meegid.2017.12.008. [DOI] [PubMed] [Google Scholar]
- Nempont et al. (2008).Nempont C, Cayet D, Rumbo M, Bompard C, Villeret V, Sirard JC. Deletion of flagellin’s hypervariable region abrogates antibody-mediated neutralization and systemic activation of TLR5-dependent immunity. Journal of Immunology. 2008;181(3):2036–2043. doi: 10.4049/jimmunol.181.3.2036. [DOI] [PubMed] [Google Scholar]
- Nevagi et al. (2018).Nevagi RJ, Khalil ZG, Hussein WM, Powell J, Batzloff MR, Capon RJ, Good MF, Skwarczynski M, Toth I. Polyglutamic acid-trimethyl chitosan-based intranasal peptide nano-vaccine induces potent immune responses against group A streptococcus. Acta Biomaterialia. 2018;80:278–287. doi: 10.1016/j.actbio.2018.09.037. [DOI] [PubMed] [Google Scholar]
- Nezafat et al. (2017).Nezafat N, Eslami M, Negahdaripour M, Rahbar MR, Ghasemi Y. Designing an efficient multi-epitope oral vaccine against Helicobacter pylori using immunoinformatics and structural vaccinology approaches. Molecular BioSystems. 2017;13(4):699–713. doi: 10.1039/c6mb00772d. [DOI] [PubMed] [Google Scholar]
- Nezafat et al. (2014).Nezafat N, Ghasemi Y, Javadi G, Khoshnoud MJ, Omidinia E. A novel multi-epitope peptide vaccine against cancer: an in silico approach. Journal of Theoretical Biology. 2014;349:121–134. doi: 10.1016/j.jtbi.2014.01.018. [DOI] [PubMed] [Google Scholar]
- Nezafat et al. (2016).Nezafat N, Karimi Z, Eslami M, Mohkam M, Zandian S, Ghasemi Y. Designing an efficient multi-epitope peptide vaccine against Vibrio cholerae via combined immunoinformatics and protein interaction based approaches. Computational Biology and Chemistry. 2016;62:82–95. doi: 10.1016/j.compbiolchem.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Nezafat et al. (2015).Nezafat N, Sadraeian M, Rahbar MR, Khoshnoud MJ, Mohkam M, Gholami A, Banihashemi M, Ghasemi Y. Production of a novel multi-epitope peptide vaccine for cancer immunotherapy in TC-1 tumor-bearing mice. Biologicals. 2015;43(1):11–17. doi: 10.1016/j.biologicals.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Olive et al. (2007).Olive C, Schulze K, Sun HK, Ebensen T, Horvath A, Toth I, Guzman CA. Enhanced protection against Streptococcus pyogenes infection by intranasal vaccination with a dual antigen component M protein/SfbI lipid core peptide Vaccine formulation. Vaccine. 2007;25(10):1789–1797. doi: 10.1016/j.vaccine.2006.11.031. [DOI] [PubMed] [Google Scholar]
- Ong, Tan & Ho (2017).Ong HK, Tan WS, Ho KL. Virus like particles as a platform for cancer vaccine development. PeerJ. 2017;5(Suppl 1):e4053. doi: 10.7717/peerj.4053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey et al. (2018).Pandey H, Fatma F, Yabaji SM, Kumari M, Tripathi S, Srivastava K, Tripathi DK, Kant S, Srivastava KK, Arora A. Biophysical and immunological characterization of the ESX-4 system ESAT-6 family proteins Rv3444c and Rv3445c from Mycobacterium tuberculosis H37Rv. Tuberculosis (Edinb) 2018;109:85–96. doi: 10.1016/j.tube.2018.02.002. [DOI] [PubMed] [Google Scholar]
- Pearl, Prodromou & Workman (2008).Pearl LH, Prodromou C, Workman P. The Hsp90 molecular chaperone: an open and shut case for treatment. Biochemical Journal. 2008;410(3):439–453. doi: 10.1042/BJ20071640. [DOI] [PubMed] [Google Scholar]
- Perez-Toledo et al. (2017).Perez-Toledo M, Valero-Pacheco N, Pastelin-Palacios R, Gil-Cruz C, Perez-Shibayama C, Moreno-Eutimio MA, Becker I, Perez-Tapia SM, Arriaga-Pizano L, Cunningham AF, Isibasi A, Bonifaz LC, Lopez-Macias C. Salmonella typhi porins OmpC and OmpF are potent adjuvants for T-dependent and T-independent antigens. Frontiers in Immunology. 2017;8(2):230. doi: 10.3389/fimmu.2017.00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persing et al. (2002).Persing DH, Coler RN, Lacy MJ, Johnson DA, Baldridge JR, Hershberg RM, Reed SG. Taking toll: lipid A mimetics as adjuvants and immunomodulators. Trends in Microbiology. 2002;10:S32–S37. doi: 10.1016/s0966-842x(02)02426-5. [DOI] [PubMed] [Google Scholar]
- Pichichero (2013).Pichichero ME. Protein carriers of conjugate vaccines: characteristics, development, and clinical trials. Human vaccines & immunotherapeutics. 2013;9(12):2505–2523. doi: 10.4161/hv.26109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkhasov et al. (2010).Pinkhasov J, Alvarez ML, Pathangey LB, Tinder TL, Mason HS, Walmsley AM, Gendler SJ, Mukherjee P. Analysis of a cholera toxin B subunit (CTB) and human mucin 1 (MUC1) conjugate protein in a MUC1-tolerant mouse model. Cancer Immunology, Immunotherapy. 2010;59(12):1801–1811. doi: 10.1007/s00262-010-0906-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plummer & Manchester (2011).Plummer EM, Manchester M. Viral nanoparticles and virus-like particles: platforms for contemporary vaccine design. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology. 2011;3(2):174–196. doi: 10.1002/wnan.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasanphanich et al. (2015).Prasanphanich NS, Song X, Heimburg-Molinaro J, Luyai AE, Lasanajak Y, Cutler CE, Smith DF, Cummings RD. Intact reducing glycan promotes the specific immune response to lacto-N-neotetraose-BSA neoglycoconjugates. Bioconjugate Chemistry. 2015;26(3):559–571. doi: 10.1021/acs.bioconjchem.5b00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prego et al. (2010).Prego C, Paolicelli P, Diaz B, Vicente S, Sanchez A, Gonzalez-Fernandez A, Alonso MJ. Chitosan-based nanoparticles for improving immunization against hepatitis B infection. Vaccine. 2010;28(14):2607–2614. doi: 10.1016/j.vaccine.2010.01.011. [DOI] [PubMed] [Google Scholar]
- Pumpens et al. (2016).Pumpens P, Renhofa R, Dishlers A, Kozlovska T, Ose V, Pushko P, Tars K, Grens E, Bachmann MF. The true story and advantages of RNA phage capsids as nanotools. Intervirology. 2016;59(2):74–110. doi: 10.1159/000449503. [DOI] [PubMed] [Google Scholar]
- Ramasamy et al. (2018).Ramasamy V, Arora U, Shukla R, Poddar A, Shanmugam RK, White LJ, Mattocks MM, Raut R, Perween A, Tyagi P, De Silva AM, Bhaumik SK, Kaja MK, Villinger F, Ahmed R, Johnston RE, Swaminathan S, Khanna N. A tetravalent virus-like particle vaccine designed to display domain III of dengue envelope proteins induces multi-serotype neutralizing antibodies in mice and macaques which confer protection against antibody dependent enhancement in AG129 mice. PLOS Neglected Tropical Diseases. 2018;12(1):e0006191. doi: 10.1371/journal.pntd.0006191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez et al. (2018).Ramirez A, Morris S, Maucourant S, D’Ascanio I, Crescente V, Lu IN, Farinelle S, Muller CP, Whelan M, Rosenberg W. A virus-like particle vaccine candidate for influenza A virus based on multiple conserved antigens presented on hepatitis B tandem core particles. Vaccine. 2018;36(6):873–880. doi: 10.1016/j.vaccine.2017.12.053. [DOI] [PubMed] [Google Scholar]
- Rana & Akhter (2016).Rana A, Akhter Y. A multi-subunit based, thermodynamically stable model vaccine using combined immunoinformatics and protein structure based approach. Immunobiology. 2016;221(4):544–557. doi: 10.1016/j.imbio.2015.12.004. [DOI] [PubMed] [Google Scholar]
- Rana, Rub & Akhter (2014).Rana A, Rub A, Akhter Y. Proteome-scale identification of outer membrane proteins in Mycobacterium avium subspecies paratuberculosis using a structure based combined hierarchical approach. Molecular BioSystems. 2014;10(9):2329–2337. doi: 10.1039/c4mb00234b. [DOI] [PubMed] [Google Scholar]
- Rappazzo et al. (2016).Rappazzo CG, Watkins HC, Guarino CM, Chau A, Lopez JL, DeLisa MP, Leifer CA, Whittaker GR, Putnam D. Recombinant M2e outer membrane vesicle vaccines protect against lethal influenza A challenge in BALB/c mice. Vaccine. 2016;34(10):1252–1258. doi: 10.1016/j.vaccine.2016.01.028. [DOI] [PubMed] [Google Scholar]
- Reed et al. (2016).Reed SG, Hsu F-C, Carter D, Orr MT. The science of vaccine adjuvants: advances in TLR4 ligand adjuvants. Current Opinion in Immunology. 2016;41:85–90. doi: 10.1016/j.coi.2016.06.007. [DOI] [PubMed] [Google Scholar]
- Reynolds et al. (2015).Reynolds TD, Buonocore L, Rose NF, Rose JK, Robek MD. Virus-like vesicle-based therapeutic vaccine vectors for chronic hepatitis B virus infection. Journal of Virology. 2015;89(20):10407–10415. doi: 10.1128/JVI.01184-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rios-Huerta et al. (2017).Rios-Huerta R, Monreal-Escalante E, Govea-Alonso DO, Angulo C, Rosales-Mendoza S. Expression of an immunogenic LTB-based chimeric protein targeting Zaire ebolavirus epitopes from GP1 in plant cells. Plant Cell Reports. 2017;36(2):355–365. doi: 10.1007/s00299-016-2088-6. [DOI] [PubMed] [Google Scholar]
- Robert (2003).Robert J. Evolution of heat shock protein and immunity. Developmental and Comparative Immunology. 2003;27(6–7):449–464. doi: 10.1016/s0145-305x(02)00160-x. [DOI] [PubMed] [Google Scholar]
- Rodrigues et al. (2011).Rodrigues JF, Mathias-Santos C, Sbrogio-Almeida ME, Amorim JH, Cabrera-Crespo J, Balan A, Ferreira LC. Functional diversity of heat-labile toxins (LT) produced by enterotoxigenic Escherichia coli: differential enzymatic and immunological activities of LT1 (hLT) AND LT4 (pLT) Journal of Biological Chemistry. 2011;286(7):5222–5233. doi: 10.1074/jbc.M110.173682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roose et al. (2013).Roose K, De Baets S, Schepens B, Saelens X. Hepatitis B core-based virus-like particles to present heterologous epitopes. Expert Review of Vaccines. 2013;12(2):183–198. doi: 10.1586/erv.12.150. [DOI] [PubMed] [Google Scholar]
- Rossi et al. (2014).Rossi O, Pesce I, Giannelli C, Aprea S, Caboni M, Citiulo F, Valentini S, Ferlenghi I, MacLennan CA, D’Oro U, Saul A, Gerke C. Modulation of endotoxicity of Shigella generalized modules for membrane antigens (GMMA) by genetic lipid A modifications: relative activation of TLR4 and TLR2 pathways in different mutants. Journal of Biological Chemistry. 2014;289(36):24922–24935. doi: 10.1074/jbc.M114.566570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueckert & Guzman (2012).Rueckert C, Guzman CA. Vaccines: from empirical development to rational design. PLoS Pathogens. 2012;8(11):e1003001. doi: 10.1371/journal.ppat.1003001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueda et al. (2017).Rueda F, Eich C, Cordobilla B, Domingo P, Acosta G, Albericio F, Cruz LJ, Domingo JC. Effect of TLR ligands co-encapsulated with multiepitopic antigen in nanoliposomes targeted to human DCs via Fc receptor for cancer vaccines. Immunobiology. 2017;222(11):989–997. doi: 10.1016/j.imbio.2017.06.002. [DOI] [PubMed] [Google Scholar]
- Saadi, Karkhah & Nouri (2017).Saadi M, Karkhah A, Nouri HR. Development of a multi-epitope peptide vaccine inducing robust T cell responses against brucellosis using immunoinformatics based approaches. Infection, Genetics and Evolution. 2017;51:227–234. doi: 10.1016/j.meegid.2017.04.009. [DOI] [PubMed] [Google Scholar]
- Schmidt et al. (2007).Schmidt J, Welsch T, Jager D, Muhlradt PF, Buchler MW, Marten A. Intratumoural injection of the toll-like receptor-2/6 agonist ‘macrophage-activating lipopeptide-2′ in patients with pancreatic carcinoma: a phase I/II trial. British Journal of Cancer. 2007;97(5):598–604. doi: 10.1038/sj.bjc.6603903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schocker et al. (2016).Schocker NS, Portillo S, Brito CR, Marques AF, Almeida IC, Michael K. Synthesis of Galalpha(1,3)Galbeta(1,4)GlcNAcalpha-, Galbeta(1,4)GlcNAcalpha- and GlcNAc-containing neoglycoproteins and their immunological evaluation in the context of Chagas disease. Glycobiology. 2016;26:39–50. doi: 10.1093/glycob/cwv081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulze et al. (2017).Schulze K, Ebensen T, Chandrudu S, Skwarczynski M, Toth I, Olive C, Guzman CA. Bivalent mucosal peptide vaccines administered using the LCP carrier system stimulate protective immune responses against Streptococcus pyogenes infection. Nanomedicine: Nanotechnology, Biology and Medicine. 2017;13(8):2463–2474. doi: 10.1016/j.nano.2017.08.015. [DOI] [PubMed] [Google Scholar]
- SenGupta et al. (2004).SenGupta D, Norris PJ, Suscovich TJ, Hassan-Zahraee M, Moffett HF, Trocha A, Draenert R, Goulder PJR, Binder RJ, Levey DL, Walker BD, Srivastava PK, Brander C. Heat shock protein-mediated cross-presentation of exogenous HIV antigen on HLA class I and class II. Journal of Immunology. 2004;173(3):1987–1993. doi: 10.4049/jimmunol.173.3.1987. [DOI] [PubMed] [Google Scholar]
- Seth et al. (2017).Seth L, Bingham FK, Kaba SA, Musser DM, Emadi S, Matyas GR, Beck Z, Alving CR, Burkhard P, Lanar DE. Development of a self-assembling protein nanoparticle Vaccine targeting Plasmodium falciparum circumsporozoite protein delivered in three army liposome formulation adjuvants. Vaccine. 2017;35(41):5448–5454. doi: 10.1016/j.vaccine.2017.02.040. [DOI] [PubMed] [Google Scholar]
- Sharma et al. (2017).Sharma M, Dash P, Sahoo PK, Dixit A. Th2-biased immune response and agglutinating antibodies generation by a chimeric protein comprising OmpC epitope (323–336) of Aeromonas hydrophila and LTB. Immunologic Research. 2017;66(1):187–199. doi: 10.1007/s12026-017-8953-8. [DOI] [PubMed] [Google Scholar]
- Shaw & Starnbach (2008).Shaw CA, Starnbach MN. Both CD4+ and CD8+ T cells respond to antigens fused to anthrax lethal toxin. Infection and Immunity. 2008;76(6):2603–2611. doi: 10.1128/IAI.01718-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevtsov & Multhoff (2016).Shevtsov M, Multhoff G. Heat shock protein-peptide and HSP-based immunotherapies for the treatment of cancer. Frontiers in Immunology. 2016;7:171. doi: 10.3389/fimmu.2016.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirbaghaee & Bolhassani (2016).Shirbaghaee Z, Bolhassani A. Different applications of virus-like particles in biology and medicine: vaccination and delivery systems. Biopolymers. 2016;105(3):113–132. doi: 10.1002/bip.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simanovich et al. (2017).Simanovich E, Brod V, Rahat MM, Drazdov E, Walter M, Shakya J, Rahat MA. Inhibition of tumor growth and metastasis by EMMPRIN multiple antigenic peptide (MAP) vaccination is mediated by immune modulation. OncoImmunology. 2017;6(1):e1261778. doi: 10.1080/2162402X.2016.1261778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skwarczynski & Toth (2011a).Skwarczynski M, Toth I. Peptide-based subunit nanovaccines. Current Drug Delivery. 2011a;8(3):282–289. doi: 10.2174/156720111795256192. [DOI] [PubMed] [Google Scholar]
- Skwarczynski & Toth (2011b).Skwarczynski M, Toth I. Lipid-core-peptide system for self-adjuvanting synthetic vaccine delivery. Methods in Molecular Biology. 2011b;751:297–308. doi: 10.1007/978-1-61779-151-2_18. [DOI] [PubMed] [Google Scholar]
- Skwarczynski & Toth (2014).Skwarczynski M, Toth I. Recent advances in peptide-based subunit nanovaccines. Nanomedicine. 2014;9(17):2657–2669. doi: 10.2217/nnm.14.187. [DOI] [PubMed] [Google Scholar]
- Skwarczynski et al. (2010).Skwarczynski M, Zaman M, Urbani CN, Lin IC, Jia Z, Batzloff MR, Good MF, Monteiro MJ, Toth I. Polyacrylate dendrimer nanoparticles: a self-adjuvanting vaccine delivery system. Angewandte Chemie International Edition. 2010;49(33):5742–5745. doi: 10.1002/anie.201002221. [DOI] [PubMed] [Google Scholar]
- Smith et al. (2003).Smith KD, Andersen-Nissen E, Hayashi F, Strobe K, Bergman MA, Barrett SL, Cookson BT, Aderem A. Toll-like receptor 5 recognizes a conserved site on flagellin required for protofilament formation and bacterial motility. Nature Immunology. 2003;4(12):1247–1253. doi: 10.1038/ni1011. [DOI] [PubMed] [Google Scholar]
- Smith et al. (2007).Smith ML, Corbo T, Bernales J, Lindbo JA, Pogue GP, Palmer KE, McCormick AA. Assembly of trans-encapsidated recombinant viral vectors engineered from tobacco mosaic virus and Semliki Forest virus and their evaluation as immunogens. Virology. 2007;358(2):321–333. doi: 10.1016/j.virol.2006.08.040. [DOI] [PubMed] [Google Scholar]
- Strbo et al. (2013).Strbo N, Garcia-Soto A, Schreiber TH, Podack ER. Secreted heat shock protein gp96-Ig: next-generation vaccines for cancer and infectious diseases. Immunologic Research. 2013;57(1–3):311–325. doi: 10.1007/s12026-013-8468-x. [DOI] [PubMed] [Google Scholar]
- Su et al. (2013).Su Q, Yi Y, Guo M, Qiu F, Jia Z, Lu X, Meng Q, Bi S. Construction and immunological evaluation of truncated hepatitis B core particles carrying HBsAg amino acids 119-152 in the major immunodominant region (MIR) Biochemical and Biophysical Research Communications. 2013;439(1):84–89. doi: 10.1016/j.bbrc.2013.08.024. [DOI] [PubMed] [Google Scholar]
- Sungsuwan, Wu & Huang (2017).Sungsuwan S, Wu X, Huang X. Evaluation of virus-like particle-based tumor-associated carbohydrate immunogen in a mouse tumor model. Methods in Enzymology. 2017;597:359–376. doi: 10.1016/bs.mie.2017.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzue & Young (1996).Suzue K, Young RA. Adjuvant-free hsp70 fusion protein system elicits humoral and cellular immune responses to HIV-1 p24. Journal of Immunology. 1996;156:873–879. [PubMed] [Google Scholar]
- Suzue et al. (1997).Suzue K, Zhou X, Eisen HN, Young RA. Heat shock fusion proteins as vehicles for antigen delivery into the major histocompatibility complex class I presentation pathway. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(24):13146–13151. doi: 10.1073/pnas.94.24.13146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda et al. (2018).Takeda Y, Azuma M, Funami K, Shime H, Matsumoto M, Seya T. Type I interferon-independent dendritic cell priming and antitumor T cell activation induced by a Mycoplasma fermentans lipopeptide. Frontiers in Immunology. 2018;9:496. doi: 10.3389/fimmu.2018.00496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam (1988).Tam JP. Synthetic peptide vaccine design: synthesis and properties of a high-density multiple antigenic peptide system. Proceedings of the National Academy of Sciences of the United States of America. 1988;85:5409–5413. doi: 10.1073/pnas.85.15.5409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan et al. (2018).Tan K, Li R, Huang X, Liu Q. Outer membrane vesicles: current status and future direction of these novel vaccine adjuvants. Frontiers in Microbiology. 2018;9:783. doi: 10.3389/fmicb.2018.00783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandrup et al. (2016).Tandrup SS, Foged C, Korsholm KS, Rades T, Christensen D. Liposome-based adjuvants for subunit vaccines: formulation strategies for subunit antigens and immunostimulators. Pharmaceutics. 2016;8(1):7. doi: 10.3390/pharmaceutics8010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang et al. (2005).Tang D, Khaleque MA, Jones EL, Theriault JR, Li C, Wong WH, Stevenson MA, Calderwood SK. Expression of heat shock proteins and heat shock protein messenger ribonucleic acid in human prostate carcinoma in vitro and in tumors in vivo. Cell Stress Chaperones. 2005;10:46–58. doi: 10.1379/CSC-44R.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang et al. (2012).Tang J, Yin R, Tian Y, Huang Z, Shi J, Fu X, Wang L, Wu Y, Hao F, Ni B. A novel self-assembled nanoparticle vaccine with HIV-1 Tat49-57/HPV16 E749-57 fusion peptide and GM-CSF DNA elicits potent and prolonged CD8+ T cell-dependent anti-tumor immunity in mice. Vaccine. 2012;30(6):1071–1082. doi: 10.1016/j.vaccine.2011.12.029. [DOI] [PubMed] [Google Scholar]
- Tao et al. (2017).Tao W, Hurst BL, Shakya AK, Uddin MJ, Ingrole RS, Hernandez-Sanabria M, Arya RP, Bimler L, Paust S, Tarbet EB, Gill HS. Consensus M2e peptide conjugated to gold nanoparticles confers protection against H1N1, H3N2 and H5N1 influenza A viruses. Antiviral Research. 2017;141:62–72. doi: 10.1016/j.antiviral.2017.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor et al. (2012).Taylor DN, Treanor JJ, Sheldon EA, Johnson C, Umlauf S, Song L, Kavita U, Liu G, Tussey L, Ozer K, Hofstaetter T, Shaw A. Development of VAX128, a recombinant hemagglutinin (HA) influenza-flagellin fusion vaccine with improved safety and immune response. Vaccine. 2012;30(39):5761–5769. doi: 10.1016/j.vaccine.2012.06.086. [DOI] [PubMed] [Google Scholar]
- Taylor et al. (2011).Taylor DN, Treanor JJ, Strout C, Johnson C, Fitzgerald T, Kavita U, Ozer K, Tussey L, Shaw A. Induction of a potent immune response in the elderly using the TLR-5 agonist, flagellin, with a recombinant hemagglutinin influenza-flagellin fusion vaccine (VAX125, STF2.HA1 SI) Vaccine. 2011;29(31):4897–4902. doi: 10.1016/j.vaccine.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Therien et al. (2017).Therien A, Bedard M, Carignan D, Rioux G, Gauthier-Landry L, Laliberte-Gagne ME, Bolduc M, Savard P, Leclerc D. A versatile papaya mosaic virus (PapMV) vaccine platform based on sortase-mediated antigen coupling. Journal of Nanobiotechnology. 2017;15(1):54. doi: 10.1186/s12951-017-0289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian et al. (2018).Tian M, Hua Z, Hong S, Zhang Z, Liu C, Lin L, Chen J, Zhang W, Zhou X, Zhang F, DeFranco AL, Hou B. B cell-intrinsic MyD88 signaling promotes initial cell proliferation and differentiation to enhance the germinal center response to a virus-like particle. Journal of Immunology. 2018;200(3):937–948. doi: 10.4049/jimmunol.1701067. [DOI] [PubMed] [Google Scholar]
- Tobias et al. (2017).Tobias J, Jasinska J, Baier K, Kundi M, Ede N, Zielinski C, Wiedermann U. Enhanced and long term immunogenicity of a Her-2/neu multi-epitope vaccine conjugated to the carrier CRM197 in conjunction with the adjuvant Montanide. BMC Cancer. 2017;17(1):177. doi: 10.1186/s12885-017-3098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourani, Karkhah & Najafi (2017).Tourani M, Karkhah A, Najafi A. Development of an epitope-based vaccine inhibiting immune cells rolling and migration against atherosclerosis using in silico approaches. Computational Biology and Chemistry. 2017;70:156–163. doi: 10.1016/j.compbiolchem.2017.08.016. [DOI] [PubMed] [Google Scholar]
- Valguarnera & Feldman (2017).Valguarnera E, Feldman MF. Glycoengineered outer membrane vesicles as a platform for vaccine development. Methods in Enzymology. 2017;597:285–310. doi: 10.1016/bs.mie.2017.06.032. [DOI] [PubMed] [Google Scholar]
- Van Der Burg et al. (2006).Van Der Burg SH, Bijker MS, Welters MJ, Offringa R, Melief CJ. Improved peptide vaccine strategies, creating synthetic artificial infections to maximize immune efficacy. Advanced Drug Delivery Reviews. 2006;58(8):916–930. doi: 10.1016/j.addr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Van Der Heiden et al. (2017).Van Der Heiden M, Duizendstra A, Berbers G, Boots A, Buisman AM. Tetanus Toxoid carrier protein induced T-helper cell responses upon vaccination of middle-aged adults. Vaccine. 2017;35(42):5581–5588. doi: 10.1016/j.vaccine.2017.08.056. [DOI] [PubMed] [Google Scholar]
- Vartak & Sucheck (2016).Vartak A, Sucheck SJ. Recent advances in subunit vaccine carriers. Vaccines. 2016;4(2):12. doi: 10.3390/vaccines4020012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilakos & Tomai (2013).Vasilakos JP, Tomai MA. The use of Toll-like receptor 7/8 agonists as vaccine adjuvants. Expert Review of Vaccines. 2013;12(7):809–819. doi: 10.1586/14760584.2013.811208. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2018).Wang Y, Alahdal M, Ye J, Jing L, Liu X, Chen H, Jin L, Cao R. Inhibition of RM-1 prostate carcinoma and eliciting robust immune responses in the mouse model by using VEGF-M2-GnRH3-hinge-MVP vaccine. Genes & Immunity. 2018;2018:1–10. doi: 10.1038/s41435-017-0005-9. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2017a).Wang W, Feng F, Lv J, Xie Z, Chen J, Zhang L, Li W. Major immunodominant region of hepatitis B virus core antigen as a delivery vector to improve the immunogenicity of the fusion antigen ROP2-SAG1 multiepitope from Toxoplasma gondii in Mice. Viral Immunology. 2017a;30(7):508–515. doi: 10.1089/vim.2016.0135. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2014).Wang BZ, Gill HS, He C, Ou C, Wang L, Wang YC, Feng H, Zhang H, Prausnitz MR, Compans RW. Microneedle delivery of an M2e-TLR5 ligand fusion protein to skin confers broadly cross-protective influenza immunity. Journal of Controlled Release. 2014;178:1–7. doi: 10.1016/j.jconrel.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2002).Wang Y, Kelly CG, Singh M, McGowan EG, Carrara AS, Bergmeier LA, Lehner T. Stimulation of Th1-polarizing cytokines, C-C chemokines, maturation of dendritic cells, and adjuvant function by the peptide binding fragment of heat shock protein 70. Journal of Immunology. 2002;169(5):2422–2429. doi: 10.4049/jimmunol.169.5.2422. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2018b).Wang C, Zhu W, Luo Y, Wang BZ. Gold nanoparticles conjugating recombinant influenza hemagglutinin trimers and flagellin enhanced mucosal cellular immunity. Nanomedicine: Nanotechnology, Biology and Medicine. 2018b;14(4):1349–1360. doi: 10.1016/j.nano.2018.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Zhu & Wang (2017b).Wang C, Zhu W, Wang BZ. Dual-linker gold nanoparticles as adjuvanting carriers for multivalent display of recombinant influenza hemagglutinin trimers and flagellin improve the immunological responses in vivo and in vitro. International Journal of Nanomedicine. 2017b;12:4747–4762. doi: 10.2147/IJN.S137222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2011).Wang H, Su X, Zhang P, Liang J, Wei H, Wan M, Wu X, Yu Y, Wang L. Recombinant heat shock protein 65 carrying PADRE and HBV epitopes activates dendritic cells and elicits HBV-specific CTL responses. Vaccine. 2011;29(12):2328–2335. doi: 10.1016/j.vaccine.2010.12.124. [DOI] [PubMed] [Google Scholar]
- Wei et al. (2018).Wei S, Lei Y, Yang J, Wang X, Shu F, Wei X, Lin F, Li B, Cui Y, Zhang H, Wei S. Neutralization effects of antibody elicited by chimeric HBV S antigen viral-like particles presenting HCV neutralization epitopes. Vaccine. 2018;36(17):2273–2281. doi: 10.1016/j.vaccine.2018.03.036. [DOI] [PubMed] [Google Scholar]
- Wen et al. (2016).Wen F, Ma JH, Yu H, Yang FR, Huang M, Zhou YJ, Li ZJ, Wang XH, Li GX, Jiang YF, Tong W, Tong GZ. A novel M2e-multiple antigenic peptide providing heterologous protection in mice. Journal of Veterinary Science. 2016;17(1):71–78. doi: 10.4142/jvs.2016.17.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesche et al. (1998).Wesche J, Elliott JL, Falnes PO, Olsnes S, Collier RJ. Characterization of membrane translocation by anthrax protective antigen. Biochemistry. 1998;37(45):15737–15746. doi: 10.1021/bi981436i. [DOI] [PubMed] [Google Scholar]
- Winblad et al. (2012).Winblad B, Andreasen N, Minthon L, Floesser A, Imbert G, Dumortier T, Maguire RP, Blennow K, Lundmark J, Staufenbiel M, Orgogozo J-M, Graf A. Safety, tolerability, and antibody response of active Abeta immunotherapy with CAD106 in patients with Alzheimer’s disease: randomised, double-blind, placebo-controlled, first-in-human study. Lancet Neurology. 2012;11(7):597–604. doi: 10.1016/S1474-4422(12)70140-0. [DOI] [PubMed] [Google Scholar]
- Wu et al. (2017).Wu Y, Zhu R, Xu L, Li Y, Li S, Yu H, Li S, Zhu H, Cheng T, Xia N. A novel combined vaccine based on monochimeric VLP co-displaying multiple conserved epitopes against enterovirus 71 and varicella-zoster virus. Vaccine. 2017;35(20):2728–2735. doi: 10.1016/j.vaccine.2017.03.065. [DOI] [PubMed] [Google Scholar]
- Xu et al. (2017).Xu A, Zhang L, Chen Y, Lin Z, Li R. Immunogenicity and efficacy of a rationally designed vaccine against vascular endothelial growth factor in mouse solid tumor models. Cancer Immunology, Immunotherapy. 2017;66(2):181–192. doi: 10.1007/s00262-016-1928-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2016).Yang L, Li W, Kirberger M, Liao W, Ren J. Design of nanomaterial based systems for novel vaccine development. Biomaterials Science. 2016;4(5):785–802. doi: 10.1039/c5bm00507h. [DOI] [PubMed] [Google Scholar]
- Yang et al. (2012).Yang Y, Ringler P, Muller SA, Burkhard P. Optimizing the refolding conditions of self-assembling polypeptide nanoparticles that serve as repetitive antigen display systems. Journal of Structural Biology. 2012;177(1):168–176. doi: 10.1016/j.jsb.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachova, Krupka & Raska (2016).Zachova K, Krupka M, Raska M. Antigen cross-presentation and heat shock protein-based vaccines. Archivum Immunologiae et Therapiae Experimentalis. 2016;64(1):1–18. doi: 10.1007/s00005-015-0370-x. [DOI] [PubMed] [Google Scholar]
- Zaman et al. (2012).Zaman M, Abdel-Aal AB, Fujita Y, Phillipps KS, Batzloff MR, Good MF, Toth I. Immunological evaluation of lipopeptide group A streptococcus (GAS) vaccine: structure-activity relationship. PLOS ONE. 2012;7(1):e30146. doi: 10.1371/journal.pone.0030146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaman et al. (2011).Zaman M, Skwarczynski M, Malcolm JM, Urbani CN, Jia Z, Batzloff MR, Good MF, Monteiro MJ, Toth I. Self-adjuvanting polyacrylic nanoparticulate delivery system for group A streptococcus (GAS) vaccine. Nanomedicine: Nanotechnology, Biology and Medicine. 2011;7(2):168–173. doi: 10.1016/j.nano.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Zaman & Toth (2013).Zaman M, Toth I. Immunostimulation by synthetic lipopeptide-based vaccine candidates: structure-activity relationships. Frontiers in Immunology. 2013;4:318. doi: 10.3389/fimmu.2013.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai et al. (2017).Zhai L, Peabody J, Pang YS, Schiller J, Chackerian B.TumbanE. A novel candidate HPV vaccine: MS2 phage VLP displaying a tandem HPV L2 peptide offers similar protection in mice to Gardasil-9. Antiviral Research. 2017;147:116–123. doi: 10.1016/j.antiviral.2017.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2016).Zhang L, Wang J, Xu A, Zhong C, Lu W, Deng L, Li R. A rationally designed TNF-α epitope-scaffold immunogen induces sustained antibody response and alleviates collagen-induced arthritis in mice. PLOS ONE. 2016;11(9):e0163080. doi: 10.1371/journal.pone.0163080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao et al. (2015).Zhao X, Chen L, Luckanagul JA, Zhang X, Lin Y, Wang Q. Enhancing antibody response against small molecular hapten with tobacco mosaic virus as a polyvalent carrier. ChemBioChem. 2015;16(9):1279–1283. doi: 10.1002/cbic.201500028. [DOI] [PubMed] [Google Scholar]
- Zhao et al. (2014).Zhao L, Seth A, Wibowo N, Zhao C-X, Mitter N, Yu C, Middelberg APJ. Nanoparticle vaccines. Vaccine. 2014;32(3):327–337. doi: 10.1016/j.vaccine.2013.11.069. [DOI] [PubMed] [Google Scholar]
- Zheng et al. (2016).Zheng D, Chen S, Qu D, Chen J, Wang F, Zhang R, Chen Z. Influenza H7N9 LAH-HBc virus-like particle vaccine with adjuvant protects mice against homologous and heterologous influenza viruses. Vaccine. 2016;34(51):6464–6471. doi: 10.1016/j.vaccine.2016.11.026. [DOI] [PubMed] [Google Scholar]
- Zhu et al. (2010).Zhu Q, Egelston C, Gagnon S, Sui Y, Belyakov IM, Klinman DM, Berzofsky JA. Using 3 TLR ligands as a combination adjuvant induces qualitative changes in T cell responses needed for antiviral protection in mice. Journal of Clinical Investigation. 2010;120(2):607–616. doi: 10.1172/JCI39293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu et al. (2016).Zhu R, Liu J, Chen C, Ye X, Xu L, Wang W, Zhao Q, Zhu H, Cheng T, Xia N. A highly conserved epitope-vaccine candidate against varicella-zoster virus induces neutralizing antibodies in mice. Vaccine. 2016;34(13):1589–1596. doi: 10.1016/j.vaccine.2016.02.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability:
This is a review article and did not generate raw data.