Abstract
Morrison County Community-Based Care Coordination is a collaborative, cross-sector effort in Little Falls, Minnesota, that began in 2014 to reduce the use and abuse of opioids among patients at the local hospital and clinic and within the broader local rural community. As of March 2018, 453 clinic patients discontinued use of controlled substances (a reduction of 44 952 doses each month), and law enforcement stakeholders have reported a decrease in drug crimes related to the sale of narcotics.
The following analysis describes the Morrison County Community-Based Care Coordination intervention and its implementation and examines the evaluation results, sustainability, and public health significance of the project.
INTERVENTION
Morrison County Community-Based Care Coordination is one of 15 Accountable Communities for Health (ACHs) in Minnesota funded through a State Innovation Model cooperative agreement awarded to the state by the Centers for Medicare and Medicaid Innovation. The aim of Morrison County ACH was to reduce opioid analgesic use and abuse among patients at St Gabriel’s Hospital and Family Medical Center (FMC) in Little Falls, Minnesota; to change opioid prescribing practices among providers; and to raise awareness throughout the community about the prevention of opioid use and addiction and about treatment options.
PLACE AND TIME
Morrison County ACH is located in rural central Minnesota in Little Falls (population 8300), which is the seat of Morrison County (population 33 000). The ACH began in 2014, with seed funding ending in 2017. The work of the program continues through reimbursement and additional grant and foundation funding.
PERSON
Morrison County ACH targets patients of St Gabriel’s Hospital and FMC (clinic) who use one or more controlled substances to help manage chronic pain, clinic physicians who prescribe opioids and other controlled substances, and the broader Morrison County community.
PURPOSE
Morrison County ACH came together to address growing concerns about narcotics use and abuse in the community, as evidenced by the high number of emergency department visits to St Gabriel’s for therapeutic drug monitoring (an International Classification of Diseases, Ninth Revision, code applied to many visits during which patients sought narcotics for uncontrolled pain1), the high volume of clinic Medicaid patients with eight to 20 narcotics prescriptions filled monthly between January and August of 2014, and concerns expressed by law enforcement about overdoses in the community.2
IMPLEMENTATION
The core of Morrison County ACH is an interdisciplinary Controlled Substance Care Team (Care Team), which consists of a social worker, a nurse, two physicians, and a pharmacist. Any patient receiving care at St Gabriel’s Hospital and FMC who uses a controlled substance (i.e., opioid analgesic, benzodiazepine, or stimulant) is required to work with the Care Team. The Care Team works in consultation with the patient and his or her own physician to establish a Controlled Substance Care Plan to (1) taper or maintain the patient’s dosage or (2) discontinue narcotic prescriptions entirely. The Care Team also monitors patients’ narcotics use to ensure care plan adherence (including urine drug screens), addresses any social determinants of health that might contribute to overuse of controlled substances (e.g., housing, transportation, food access, employment), and treats opioid use disorders with a medication-assisted treatment program involving buprenorphine.
The physicians on the Care Team work closely with other FMC family practice providers to encourage compliance with the Centers for Disease Control and Prevention recommendation to limit narcotic prescriptions to a maximum of 90 morphine milligram equivalents per day for certain chronic conditions. Providers are also encouraged to recommend alternatives to narcotics (e.g., physical or occupational therapy) to further reduce controlled substance use among patients.
The ACH leverages a volunteer collaborative, the Morrison County Prescription Drug Task Force, to (1) raise community awareness about the prevention of opioid use and addiction by providing education for medical and nonmedical service providers, patients, and the general community and (2) facilitate community-wide collaboration on preventing and treating prescription drug abuse. The Task Force is multidisciplinary and includes stakeholders from county public health and social services, law enforcement, the Little Falls school district, the county attorney, the local pharmacy, the Controlled Substance Care Team, and others. Among other accomplishments, the Task Force has worked to provide individuals with opioid use disorder who are incarcerated at the county jail with buprenorphine treatment through St Gabriel’s. In addition, through the deliberations of the Task Force, local law enforcement now alerts the Care Team when prescription narcotics are found in the possession of a person for whom they were not prescribed. The Care Team then contacts the patient to whom the narcotics were prescribed and works to avoid future prescription diversion by the individual. (Diverting patients are not criminally charged; some are offered treatment, drug court, care coordination, or a combination of the three).
EVALUATION
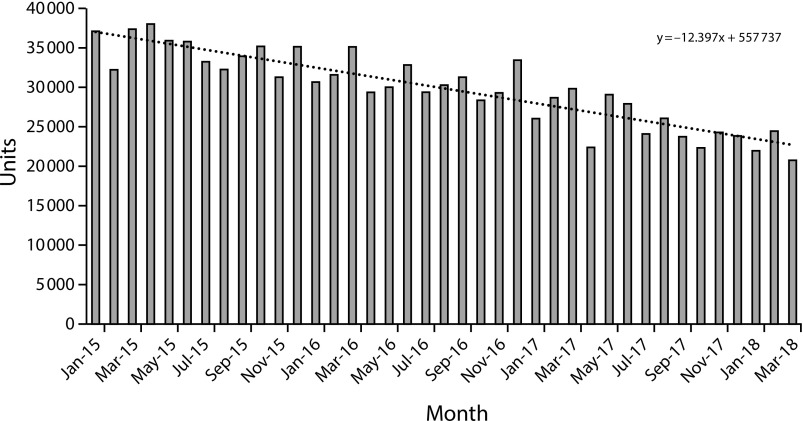
After six months of launching the Controlled Substance Care Team, visits for therapeutic drug monitoring went from being the top emergency department visit type at St Gabriel’s to being absent from the top 20 visit types.3 As of March 2018, 453 FMC patients had been tapered off controlled substances out of the more than 1500 patients that were using them. The number of monthly units of narcotics was down by 34 641, benzodiazepines by 8208, and stimulants by 2103 from January 2015 to March 2018—a reduction of 44 952 doses each month.4 Data from the local pharmacy in Little Falls reflect this reduction, with a clear downward trend in Schedule 2 units filled from January 2015 through March 2018 (Figure 1).4 (“In the absence of data predating the intervention, we were unable to identify whether the reductions in patients using controlled substances and the number of Schedule 2 units being filled during the study period can be uniquely attributed to the intervention of the Controlled Substance Care Team”). In addition, St Gabriel’s had 64 active medication-assisted treatment patients as of July 2018.
FIGURE 1—
Schedule 2 Units Filled Each Month, Coburn’s Pharmacy, Little Falls, MN, January 2015–March 2018
Changes are also being felt in the broader Morrison County community through the efforts of the Prescription Drug Task Force. Both city and county law enforcement partners report that drug crimes from narcotics sales have decreased because of factors including fewer extra pills being available for diversion. In addition, initial results point to decreased jail time and reduced recidivism among county jail inmates who engage in medication-assisted treatment through St Gabriel’s: among 36 patients surveyed who received buprenorphine between May 2016 and March 2018 while incarcerated, all saw a subsequent reduction in average days incarcerated.
ADVERSE EFFECTS
We observed no adverse effects or unintended consequences from Morrison County ACH.
SUSTAINABILITY
Given the success of Morrison County ACH, the community is committed to sustaining its work. The community has secured a combination of foundation funding, additional federal grants, and new state funding, and the ACH continues to receive support from FMC through reimbursement for care coordination for certain patients enrolled in Minnesota Health Care Programs, along with reinvestment from partnering agencies and organizations. Morrison County ACH is also working to replicate its model: St Gabriel’s Health Foundation supported 2017 state legislation providing $1 million to allow eight other Minnesota communities to replicate the ACH’s approach with technical assistance from St Gabriel’s.5 In addition, St Gabriel’s received a $293 000 State Targeted Response Grant from the US Substance Abuse and Mental Health Services Administration making St Gabriel’s an Extension for Community Healthcare Outcomes (ECHO) Hub.6 As an ECHO Hub, St Gabriel’s will provide statewide e-learning sessions on topics such as prescribing practices, community collaboration, and the establishment and management of a rural buprenorphine clinic.
PUBLIC HEALTH SIGNIFICANCE
Morrison County ACH has been critical in alleviating the burden of opioid use and abuse in the Morrison County area, and the ACH’s efforts to work across disciplines and sectors to simultaneously address the needs of both individuals and the broader community supported its effectiveness. Others attempting to replicate the Morrison County model should note the critical role that meaningful interdisciplinary and cross-sector collaboration has played in improving individual and population health in the community.
ACKNOWLEDGMENTS
The authors would like to thank Christina Worrall of the State Health Access Data Assistance Center (University of Minnesota, School of Public Health) for reviewing early drafts of the article.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed for this study because the data used were all publicly available or obtained in aggregate.
REFERENCES
- 1.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 2.Bell H, Devine K. Morrison County opioid program. 2017. Available at: https://www.acponline.org/system/files/documents/about_acp/chapters/mn/morrison_county_opioid_program_september_2017.pdf. Accessed May 3, 2018.
- 3.Devine K, Bell H. Morrison County Drug Task Force: battling opioid addiction in greater Minnesota. Minnesota Physician. November. 2016;8:24–25. [Google Scholar]
- 4.CHI St Gabriel’s Health. Controlled Substance Care Team. April 2018. Available at: https://www.chistgabriels.com/wp-content/uploads/2018/04/CSCT.pdf. Accessed May 3, 2018.
- 5.Minnesota Department of Health. Programs & initiatives in communities: opioid abuse community prevention pilot projects. Available at: http://www.health.state.mn.us/divs/healthimprovement/programs-initiatives/in-communities/opioidgrant.html. Accessed September 11, 2018.
- 6.Minnesota Department of Health. State targeted response to the opioid crisis grants. Available at: https://mn.gov/dhs/assets/str-project-descriptions_tcm1053-334424.pdf. Accessed September 11, 2018.